1. Introduction
Cerebral palsy (CP) is a non-progressive neurological disorder that affects muscle control, movement, and coordination [
1]. According to the CDC, CP is the leading cause of motor impairment in children, affecting ~1 in 345 children in the US [
2]. The symptoms of brain injury might change during a lifetime, meaning the individual can improve function to a certain degree, but they might also experience reduced motor function during their life [
3]. Regardless of the level of impairment, therapeutic exercises are essential to either improve a skill or prevent loss of function. During childhood, one of the early and most robust predictors of limitations in everyday activity and participation restrictions is the limited ability to manipulate objects with the hand. Therefore, improving manual skills becomes one of the most important treatment goals for children with CP to increase independence in daily living skills [
4]. Unfortunately, the quality and volume of training do not often meet the demand for children with CP due to the space and personnel costs associated with inpatient care and the transportation and access issues associated with outpatient rehabilitation. Telerehabilitation is a third approach to rehabilitation designed in part to address the challenges posed by in person care. Remote assessment, treatment, and monitoring using telecommunications equipment, expand rehabilitation opportunities by improving access to patients and limiting costs to providers. Remote assessment is particularly challenging in children with CP due to difficulties collecting valid, objective measures of motor function, particularly in younger children[
5].
A critical aspect of providing remote rehabilitation is the ability to assess improvements over time. This is especially important in this target population, where changes in motor performance might be small and hard to detect by clinicians and caregivers[
6]. In addition, younger and cognitively impaired children with CP might not be able to self-report improvement or deterioration. Assessments of hand function that show progress over time play an important role in clinical decision making for therapists and also serve to keep children engaged and motivated to participate in therapy. Clinical assessments utilizing standardized activities such as the Melbourne Assessment[
7], Box and Blocks Test[
8], the Assisting Hand Assessment[
9] and the Jebsen Taylor Test of Hand Function[
10], are used extensively in clinical and research settings to evaluate the impairment level and functional level of upper extremity of children with CP. They provide high levels of reliability and ecological validity. This said, these tests require children to be present in the clinic, limiting their accessibility to children with mobility and transportation issues. They also are unable to provide immediate feedback to children as they perform home exercise programs. Standardized computer-based assessments can provide objective and instantaneous evaluation of the upper extremity function and make remote and more frequent monitoring possible. However, to be feasible, these assessments need to accommodate the bodies and cognitive perceptual / abilities of the children being tested. They also need to collect data that is related to real world function.
Studies show that camera-based motion capture systems are reliable and effective for the provision of upper extremity therapies for children with CP in the laboratory setting [
11,
12,
13]. A higher degree of precision is required to perform standardized assessments in order for tests to be sufficiently reliable and valid for measuring progress and facilitating clinical decision making by therapists. Systems that utilize gesture recognition require usable anthropometric data for transformation into a hand model that can be used for kinematic measurement. Hand shape and size affect these measurements[
14]. To date, no acceptable range of hand sizes for utilization in camera-based motion capture has been established.
Technology based motor assessment requires a degree of direction following and attention beyond those of traditionally standardized assessments[
15]. Complex sensorimotor transformations are also necessary for users to understand the translation of physical movement to on-screen movement [
16]. All of these abilities are impacted by both the neuropathology associated with CP and the developmental process. There are no established guidelines describing an ideal age range or minimum age for the collection of valid, camera-based motor performance data in children with CP.
Rehabilitation Technologies for Hand and Arm (R3THA™) uses exergame technologies and cloud powered data analytics to provide personalized and adaptive hand and arm rehabilitation activities for individuals with chronic brain injuries. R3THA (‘ree-tha’) employs infrared motion capture and adaptive learning algorithms to assess hand function, tailors over 20 different hand exercises to individual impairments, and tracks progress over time. Therapists can use it in person or via remote telerehabilitation sessions, and individuals can use it for home exercise programs. A previous iteration of this approach, the Home-based Virtual Rehabilitation System (HoVRS), developed by New Jersey Institute of Technology (NJIT), was originally designed for studying individuals recovering from stroke [
17,
18,
19,
20,
21].
R3THA is specifically designed to work without wearable sensors attached to the hand. It uses an infrared camera, Leap Motion Controller (LMC), to capture kinematic measures. The LMC has two infrared light emitting diodes (LEDs) that collect images transmitted via USB to the LMC’s tracking software, which analyzes and transforms the images into three-dimensional representations of these images[
18]. This allows for real time, camera-based estimation of wrist and finger angles and position measures without an expensive and cumbersome wearable apparatus. The reliability and validity of kinematic measures of wrist and finger function collected by the LMC capturing finger/wrist joint data have been validated in our previous research studies with individuals with stroke[
19]. R3THA also provides a comprehensive assessment protocol (R3THA-AP), which collects a battery of kinematic measures to provide objective, standardized, and detailed information for clinicians, end-users, and caregivers. Kinematic measurements from R3THA-AP have demonstrated clinically acceptable levels of reliability as well moderate to strong correlations with clinical measures of motor control in persons with stroke, which suggests that the R3THA-AP can generate the meaningful remote assessments necessary for effective telerehabilitation in this population[
19]. In order to establish that the R3THA-AP will be able to meet the needs of children with CP in a similar fashion we conducted two proof of concept studies to evaluate the following aspects of the R3THA-AP in a group of children with hemiplegia.
- 1)
Explore the relationship between R3HTA-AP measurements data and children’s ages and upper extremity size.
- 2)
Evaluate the validity of R3HTA-AP by correlating its kinematic measurements with clinical assessments.
2. Study #1: Explore the relationship between R3HTA-AP measurements data and children’s ages and upper extremity size.
2.1. Materials and Methods
2.1.1. Study Participants
Both studies were approved by the Internal Review Board of the New Jersey Institute of Technology. Children were recruited at a summer camp located in suburban New Jersey, USA. Children from across the US attend this summer camp, traveling to New Jersey for the four-week duration of the camp. Parents and children were informed about the study on the first day of camp. Potential participants were pre-screened by a camp Occupational Therapist (OT) and an on-site study coordinator. Consent and assent were completed with parents and children.
Participants were selected for both studies based on the following inclusion criteria: 1) Children with CP or hemiplegia due to brain injury, 2) Aged 3 – 18, 3) Gross Motor Function Classification System level of I – IV, 4) No severe arm weakness and tone, 5) Able to follow verbal instructions, 6) No visual problems that make it difficult for them to interact with the entire computer screen.
2.1.2. Study Protocol
To prepare for the study, study therapists were trained to use the R3THA-AP a week before the summer camp started. After the consent and assent, participants’ motor function was evaluated using clinical assessments and R3THA-AP based kinematic assessments during the week of the camp, by four licensed OTs.
2.1.3. Data collection
2.1.3.1. Demographic Data
Demographic information, such as participants' age, gender, and side of hemiplegia, was gathered before the study commenced. Participants’ upper extremity size was measured from the tip of the middle finger to the elbow crease.
2.1.3.2. R3THA Assessment
R3THA-AP (Assessment Protocol) collects a battery of kinematic measurements to assess the range of motion and control of movements of hand and arm. It measures the following:
Table 1.
R3THA-AP kinematic measurement and description.
Table 1.
R3THA-AP kinematic measurement and description.
| R3THA-AP Subtest Items |
Descriptions |
| Hand Open/Close Range (cm) |
The participant fully opens and then fully closes their hand. The Hand Open Range value is calculated by measuring the difference in the average distance between the fingertips and the center of the palm across all four fingers in these two positions. A larger value indicates a greater hand opening range. |
| Hand Open/Close Trace Error Rate (%) |
The participant controls a cursor that moves up and down by opening and closing their hand. The participant attempts to trace an irregular wave which moves on the screen from left to right at a constant speed. Accuracy is calculated as the root mean square error between the cursor position and the corresponding target point on the wave. Root mean square error is calculated to quantify the differences in cued movement and actual participant movement (smaller error = better performance). The smaller the value, the better control of hand opening. |
| Wrist Extension/Flexion Range (deg) |
The participant extends and flexes their wrist against gravity with their forearm in a fixed position. Angular difference between these two positions is reported as the wrist pitch range. |
| Wrist Extension/Flexion Trace Error Rate (%) |
The participant controls a cursor that moves up and down by flexing and extending their wrist. Task and accuracy values are calculated. |
| Pronation/Supination Range (deg) |
The participant moves and holds their hand in pronation and supination with their elbow fixed. Range is calculated. |
| Pronation/Supination Trace Error Rate (%) |
The participant controls a cursor that moves up and down by pronating and supinating their hand. Task and accuracy calculations were performed. |
2.1.4. Statistical Analysis
We explored the relationship between R3THA-AP’s measurements and children’s age and upper extremity size using Spearman rank-order correlation. Linear regression analysis was utilized to determine the correlation between upper extremity size and percentage of the valid R3THA-AP. The statistical data analyses were conducted using R 4.1.0, and a custom-written script in MATLAB software (MathWorks, MA, v.R2022b).
2.2. Results
2.2.1. Participants
A total of 36 participants between the ages of 3 to 18 years old were recruited to evaluate the usability of R3THA-AP with children with CP with wide range of age and hand size. Consent and assent were obtained from each participant prior to being enrolled in the study. The demographic characteristics are listed in
Table 2. No safety issues were reported, and none of the participants experienced any side effects during the study.
2.2.2. Data Validation Analysis
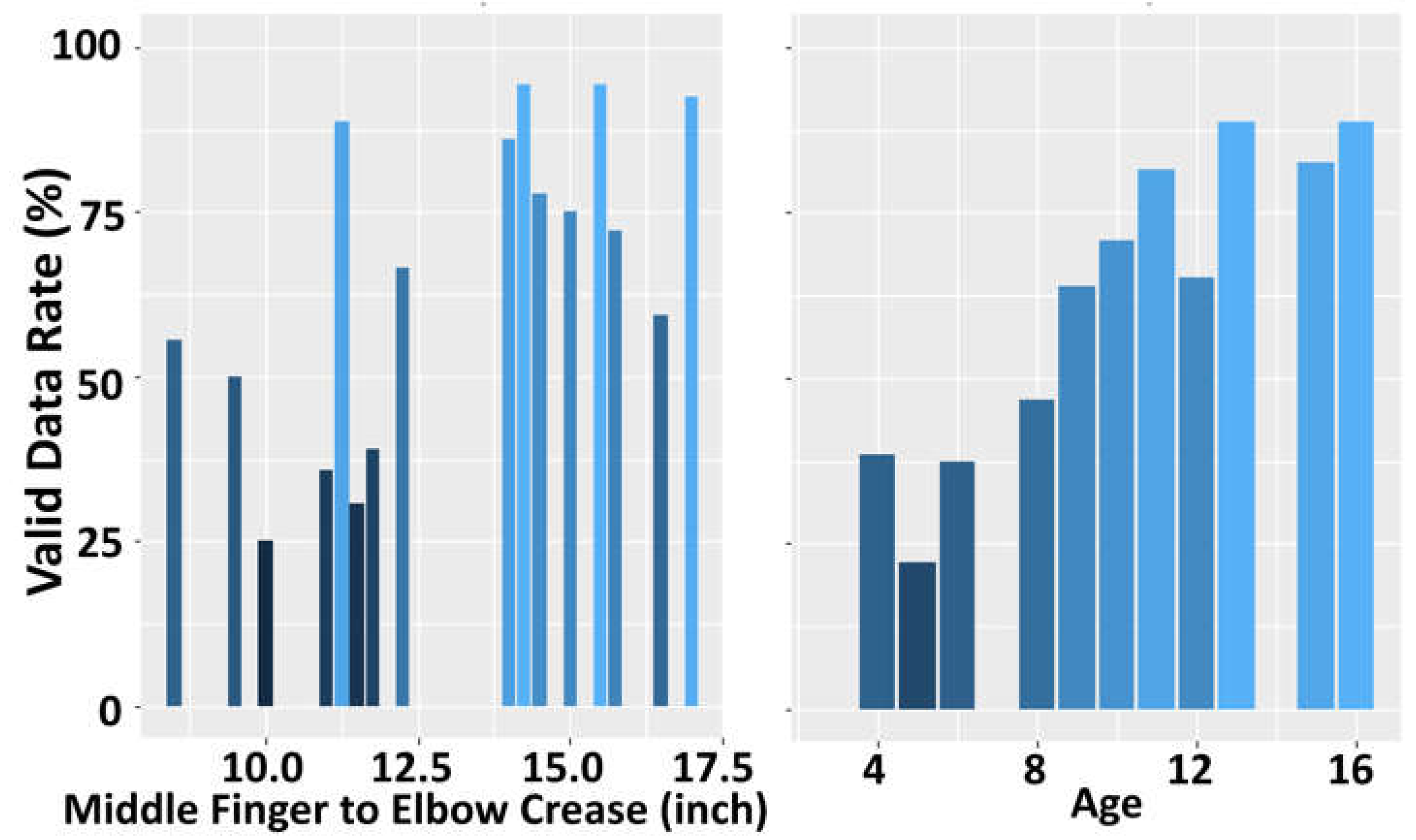
During the study, if the system is unable to track the participant's hand for a specific subtest, the corresponding R3THA-AP subtest item score were recorded as null. The R3THA-AP valid data rate was calculated as the percentage of non-null R3THA-AP kinematic measurements relative to the total number of subtests. R3THA-AP’s valid data rate collected from participants aged 8 and older is 40% higher than participants aged 7 and younger. The valide data rate is statistically significantly correlated with age (Spearman’s ρ = 0.94, p-val <0.001), and moderately correlated with upper extremity size (Spearman’s ρ = 0.602, p-val =0.013) (
Figure 1).
3. Study #2: Evaluate the validity of R3HTA-AP by correlating its kinematic measurements with clinical assessments.
3.1. Materials and Methods
3.1.1. Study Participants
3.1.2. Study Protocol
To prepare for the study, study therapists were trained to use the R3THA-AP a week before the summer camp started. After the consent and assent, participants’ motor function was evaluated using clinical assessments and R3THA-AP based kinematic assessments during camp by four licensed OTs.
3.1.3. Data Collection
3.1.3.1. Demographic Data
Demographic information, such as participants' age, gender, and side of hemiplegia, was gathered before training commenced.
3.1.3.2. Clinical Assessments
The Melbourne Assessment 2 (MA2): MA2 is a 14 item criterion-referenced test for evaluating four elements of upper limb movement quality in children with a neurological impairment aged 2.5 to 15 years: (i) Range of movement, (ii) Accuracy of reach and placement, (iii) Dexterity of grasp, release and manipulation and (iv) Fluency of movement [
22]. MA2 performance is video recorded and scored after performance is complete.
Box and Block Test (BBT): BBT is a standardized activity level test used to measure the gross manual dexterity of [
23,
24]. The subject is given 60 seconds to move as many blocks as possible over a partition to the other side, using one hand. Subjects perform the test with both hands. The Box and Blocks Index is calculated by subtracting the more impaired hand score from the less impaired hand score.
2.3.3. R3THA Assessment
See section 2.1.3.2
2.4. Statistical Analysis
The values for kinematic measures, along with MA2 and BBT, were analyzed to explore the relationship between the kinematic measurements provided by LMC and the level of impairment assessed clinically. Linear regression analysis was utilized to determine the correlation between clinical assessments and each kinematic measurement from R3THA-AP.
3.2. Results
3.2.1. Participants
R3THA-AP data set of 21 participants from study 1 was used for this study. These 21 participants was selected based on the following criteria: 1) age at 8 years or older, 2) validiat data rate is at 65% or above.
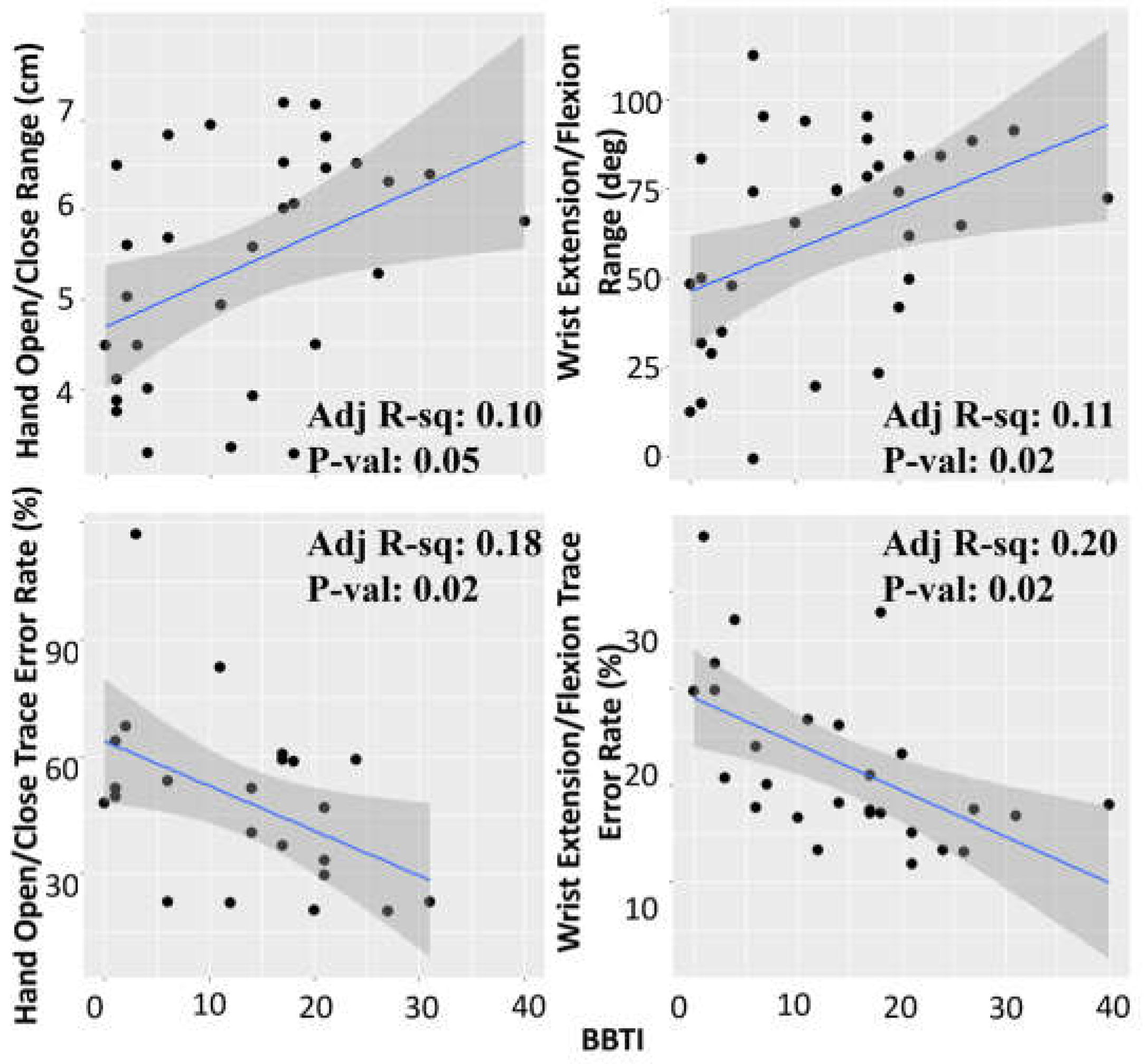
3.2.1.1. Correlation Between Box and Blocks Test and R3THA-AP
The Hand Open/Close range and Wrist Pitch range show a positive correlation with BBTI (
Figure 3). Hand Open/Close tracing error and Wrist Pitch tracing error show a negative correlation with BBTI (higher BBTI score, less trace error = higher accuracy). The two measures of pronation / supination did not demonstrate statistically significant correlations with BBT scores.
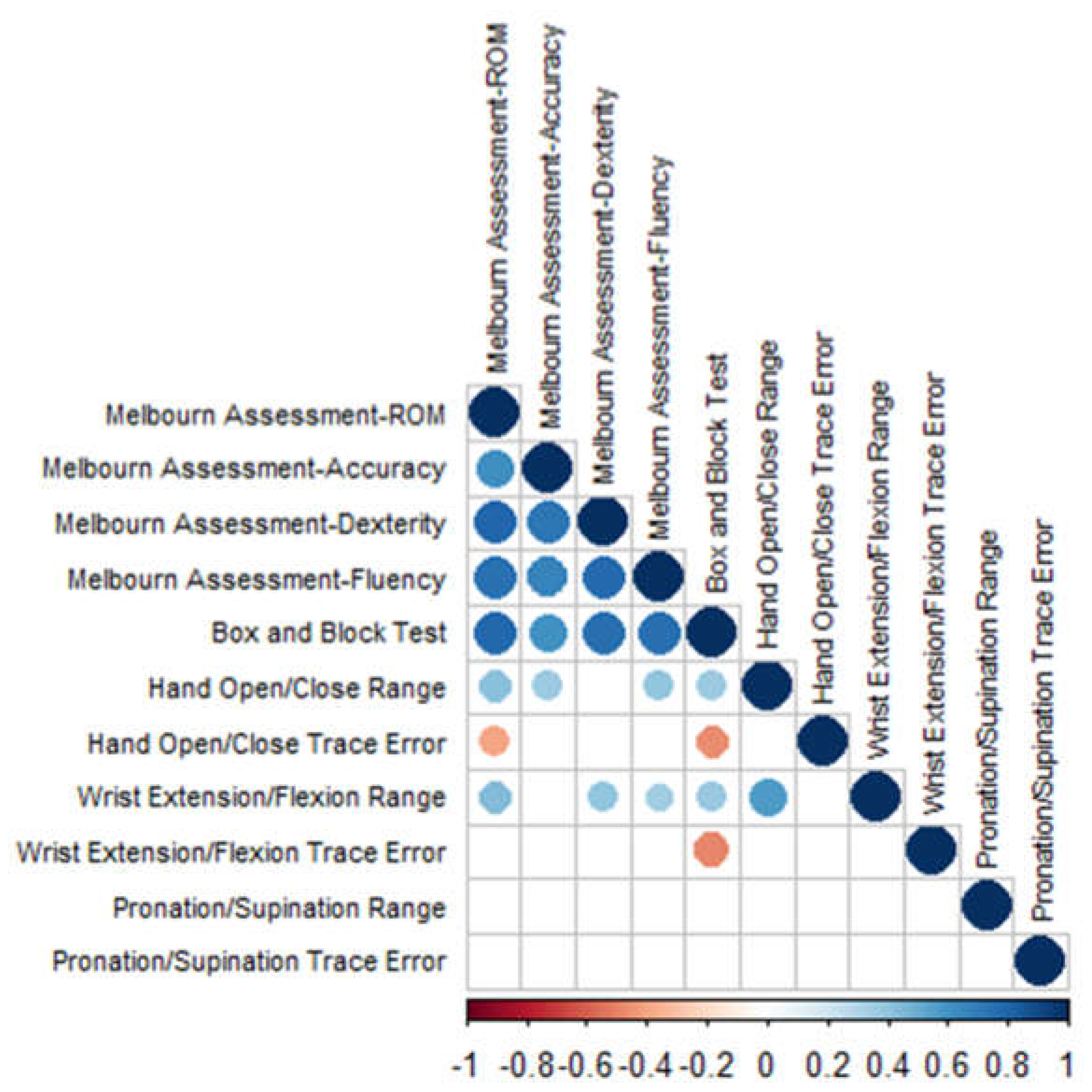
3.2.1. Correlation Analysis
The correlation matrix between the pair of each kinematics measurement from R3THA-AP and BBT and all four categories of MA2 are shown in
Figure 2. Only the significant correlated pair (p≤0.05) are illustrated in circles.
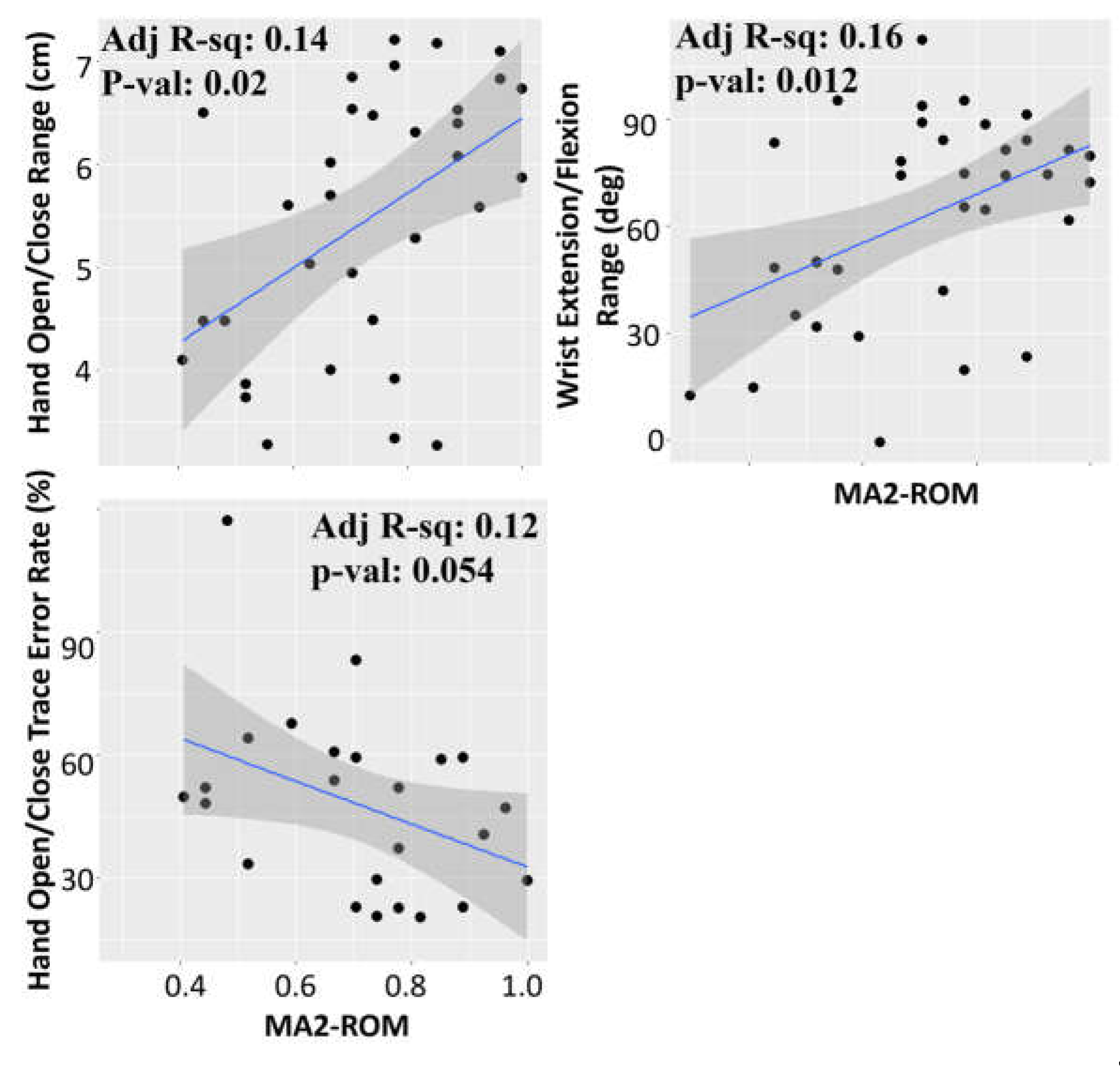
3.2.1.2. Correlation Between MA2-ROM and R3THA-AP
Hand Open Range, Wrist Pitch Range, and Wrist Extension/Flexion Accuracy demonstrated statistically significant correlations with
MA2-ROM (
Figure 4).
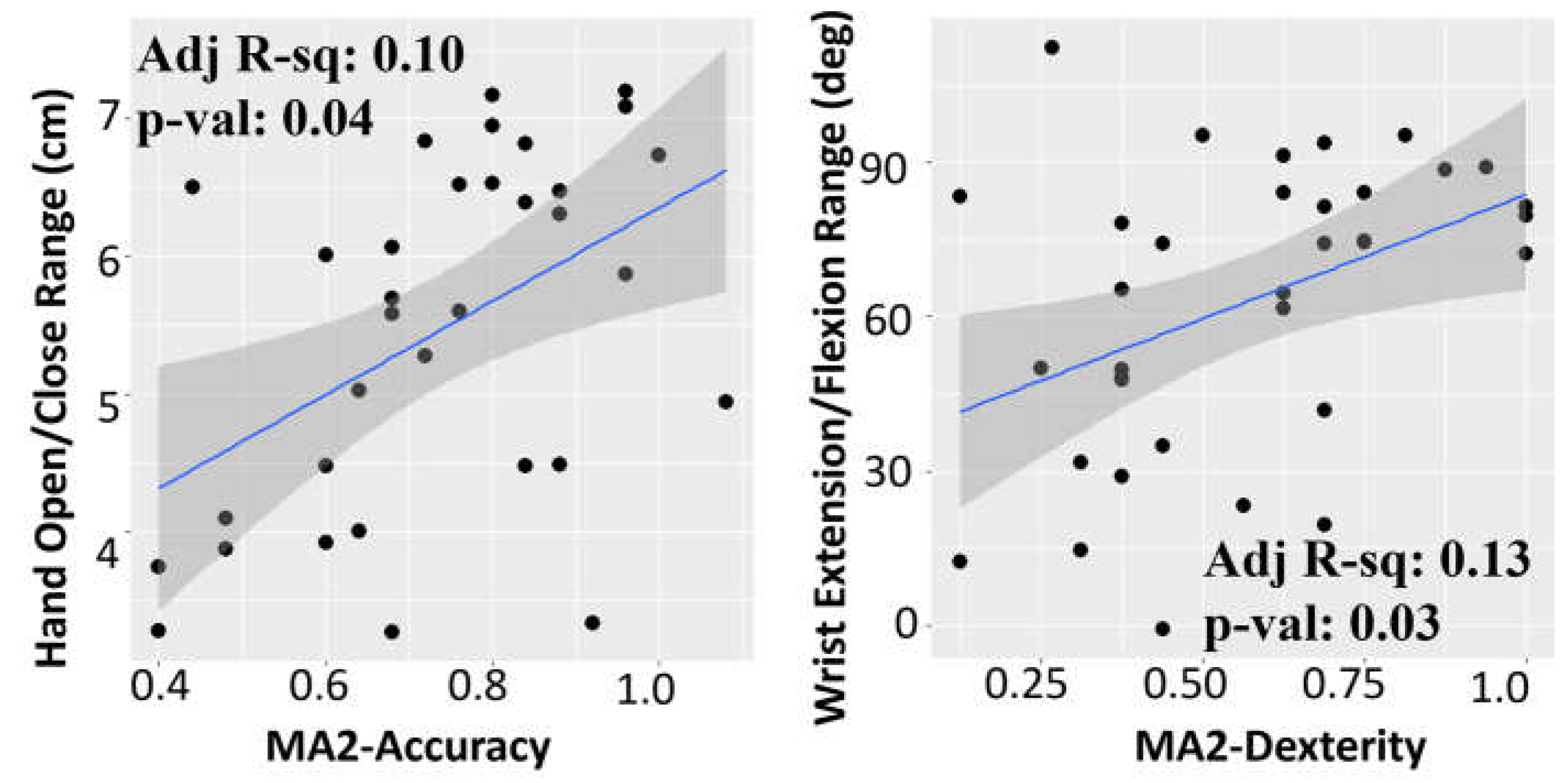
3.2.1.3. R3THA-AP with MA2-Accuracy and MA2-Dexterity
R3THA’s Hand Open Range demonstrated statistically significant correlations with MA2-Accuracy. R3THA’s Wrist Extension/Flexion Range measurement demonstrated a statistically significant correlation with MA2-Dexterity (
Figure 5).
4. Discussion
Our study found that age was a stronger predictor of the ability to collect usable kinematic data with the R3THA than upper extremity size in a group of children with CP. While age and upper extremity size were highly correlated with each, the ability to collect valid kinematic data did not increase linearly with upper extremity size or demonstrate a clear bench mark which is consistent with findings of a study of measurement characteristics of the LMC by Chan [
25]. However, the findings from this study suggest that age 8 might be a suitable benchmark for achieving usable measurements with the R3THA-AP. These findings are congruent with the findings of a systematic review by Martinie [
26] and consistent with neurodevelopmental literature which states that, children typically have developed the functional visual and cognitive skills necessary to manipulate, organize, and prioritize objects and actions, along with the ability to concentrate by the age of 8 [
27].
The R3THA-AP was able to collect valid measurements of finger and wrist movement in a majority of the children tested in Study One, which is consistent with the published literature[
28]. However, the number of valid data sets for the measures of pronation/supination range and trace was quite low and we did not find correlations between R3THA based measures of pronation / supination with clinical measures of motor function in Study Two. This could be due to the characteristic of the upper extremity impairment of children with CP. An excessive inward rotation of the forearm, known as hyper forearm pronation, is common in children with CP, particularly in those with spastic types of CP [
29]. The motion capture camera used by R3THA faces challenges in tracking and assessing the hand in this position because it relies on the visibility of all five fingers to recognize a hand. When the hand is in a hyper-pronated position, it becomes difficult for the camera to detect it accurately if the camera is placed on a table. These findings are consistent with those described by Smeragliuolo, who cited problems with LMC based measures of pronation / supination [
28]. Future work of the ability to rotate the camera to directly face the palm or utilize an array of multiple cameras to improve the ability to track pronation / supination movements is part of the development / future study plan for R3THA.
In study two, four of the six measurements provided by the R3THA-AP had demonstrated statistically significant correlations with activity based clinical assessments. Sub-items of R3THA-AP measurements, such as hand range of motion, hand open/close trace error, wrist flexion/extension range and trace error show a correlation with BBT as well as ROM, Accuracy and Dexterity measures produced by the MA2. This suggests that R3THA based measurements may provide valid assessments of motor skills and abilities in children with CP. To date, there are no published studies of correlations between camera- based measures of wrist and finger kinematics and the BBT or elements of the MA2.
To date, the measurement of distal kinematics has been the primary focus of the R3THA-AP. The current R3THA-AP battery does not contain a test of shoulder / range of motion or hand transport kinematics. There is a rich literature addressing proximal upper extremity function in children with cerebral palsy [
26,
30,
31] and a growing literature supporting the feasibility of using camera based measures to evaluate hand transport kinematics[
31,
32,
33]. In order to provide a comprehensive assessment protocol, future development and study of the R3THA-AP will include tests of the ability to move the hand and arm through three-dimensional space.
5. Conclusions
This study found that age was a stronger predictor of the ability to collect usable kinematic data with the R3THA-AP than upper extremity size in a group of children with CP. Measurements of hand opening and wrist range of motion and measurements of wrist and finger tracking movements, provided by the R3THA-AP demonstrated statistically significant correlations with standardized, activity-based clinical assessments, suggesting that the system is capable of generating the valid remote assessments necessary for effective telerehabilitation.
6. Patent
Eriksson M., Qiu Q., Cronce A., MontJohnson A., inventors; NeuroTechR3 Inc., assignee. SYSTEM AND METHOD FOR PERFORMING REHABILITATION EXERCISES. US patent application 63538935. 2023, September 18
Author Contributions
Conceptualization, M.E., Q.Q., A.G., A.M., S.A.; methodology Q.Q., A.M.; software, A.G., Q.Q.; formal analysis, Q.Q.; investigation, M.E., G.F., A.M. and Q.Q.; curation, Q.Q., A.G., M.E. writing—original draft preparation, Q.Q., A.M.; writing—review and editing, M.E., A.G., G.F., A.M., S.A; project administration, M.E. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Study protocol was approved by the Internal Review Board of the New Jersey Institute of Technology.
Informed Consent Statement
Informed consent and assent were obtained from all participants involved in the study.
Data Availability Statement
De-identified data will be supplied by the corresponding author if requested in writing.
Acknowledgments
The authors would like to thank the Intensive Therapeutics staff, particularly Scott Matthews, Executive Director; Alexandra Clayton, OT; Brielle Hassa, OT; Lauren Armenti, OT; and Emma Przyhocky, OT, who assisted with recruitment for the study and assessment administration described in this paper. The authors would like to thank Dr. JenFu Cheng, board-certified in both Physical Medicine and Rehabilitation and Pediatric Rehabilitation Medicine, who assisted with advice on the development of technology solutions for neurorehabilitation for children with Cerebral Palsy.
Conflicts of Interest
Ashley Mont, Amanda Gross, Qinyin Qiu, and Mee Eriksson are cofounders and employees of NeuroTechR3 Inc.
References
- Pasquale, J. Accardo MD. Capute and Accardo's neurodevelopmental disabilities in infancy and childhood2008.
- Durkin MS, Benedict RE, Christensen D, Dubois LA, Fitzgerald RT, Kirby RS, Maenner MJ, Van Naarden Braun K, Wingate MS, Yeargin-Allsopp M. Prevalence of Cerebral Palsy among 8-Year-Old Children in 2010 and Preliminary Evidence of Trends in Its Relationship to Low Birthweight. Paediatr Perinat Epidemiol. 2016;30(5):496-510. Epub 20160523. [CrossRef] [PubMed]
- Blair, E. Epidemiology of the cerebral palsies. Orthop Clin North Am. 2010;41(4):441-55. hPubMed ttps://doi.org/10.1016/j.ocl.2010.06.004. [PubMed]
- Plasschaert VFP, Vriezekolk JE, Aarts PBM, Geurts ACH, Van den Ende CHM. Interventions to improve upper limb function for children with bilateral cerebral palsy: a systematic review. Dev Med Child Neurol. 2019;61(8):899-907. Epub 20190110. [CrossRef] [PubMed]
- Dostie R, Gaboury I, Cinar E, Camden C. Acceptability of pediatric telerehabilitation interventions provided by physical therapists and occupational therapists—A scoping review. Physical & Occupational Therapy In Pediatrics. 2022;42(6):615-34. [CrossRef]
- Meyns P, Roman de Mettelinge T, van der Spank J, Coussens M, Van Waelvelde H. Motivation in pediatric motor rehabilitation: A systematic search of the literature using the self-determination theory as a conceptual framework. Developmental neurorehabilitation. 2018;21(6):371-90.
- Randall M, Johnson L, Reddihough D. The melbourne assessment 2. Melbourne: Royal Children’s Hospital. 1999.
- Jongbloed-Pereboom M, Nijhuis-van der Sanden MW, Steenbergen B. Norm scores of the box and block test for children ages 3–10 years. The American Journal of Occupational Therapy. 2013;67(3):312-8. [CrossRef]
- Krumlinde-Sundholm L, Eliasson A-C. Development of the Assisting Hand Assessment: a Rasch-built measure intended for children with unilateral upper limb impairments. Scandinavian Journal of Occupational Therapy. 2003;10(1):16-26. [CrossRef]
- Araneda R, Ebner-Karestinos D, Paradis J, Saussez G, Friel KM, Gordon AM, Bleyenheuft Y. Reliability and responsiveness of the Jebsen-Taylor Test of Hand Function and the Box and Block Test for children with cerebral palsy. Developmental Medicine & child neurology. 2019;61(10):1182-8. [CrossRef]
- Tarakci E, Arman N, Tarakci D, Kasapcopur O. Leap Motion Controller-based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial. J Hand Ther. 2020;33(2):220-8 e1. Epub 20190419. [CrossRef] [PubMed]
- Avcil E, Tarakci D, Arman N, Tarakci E. Upper extremity rehabilitation using video games in cerebral palsy: a randomized clinical trial. Acta Neurol Belg. 2021;121(4):1053-60. Epub 20200611. [CrossRef] [PubMed]
- de Oliveira JM, Fernandes RC, Pinto CS, Pinheiro PR, Ribeiro S, de Albuquerque VH. Novel Virtual Environment for Alternative Treatment of Children with Cerebral Palsy. Comput Intell Neurosci. 2016;2016:8984379. Epub 20160614. [CrossRef] [PubMed]
- Chan A, Halevi T, Memon N, editors. Leap motion controller for authentication via hand geometry and gestures. Human Aspects of Information Security, Privacy, and Trust: Third International Conference, HAS 2015, Held as Part of HCI International 2015, Los Angeles, CA, USA, August 2-7, 2015 Proceedings 3; 2015: Springer.
- Laufer Y, Weiss PTL. Virtual reality in the assessment and treatment of children with motor impairment: a systematic review. Journal of Physical Therapy Education. 2011;25(1):59-71. [CrossRef]
- Abtahi P, Hough SQ, Landay JA, Follmer S, editors. Beyond being real: A sensorimotor control perspective on interactions in virtual reality. Proceedings of the 2022 CHI Conference on Human Factors in Computing Systems; 2022.
- Qiu Q, Cronce A, Fluet G, Patel J, Merians A, Adamovich S. Home-based virtual rehabilitation for upper extremity functional recovery post-stroke. Journal of Alternative Medicine Research, suppl Special Issue: Innovations and challenges in the use of virtual reality technologies for rehabilitation. 2018;10(1):27-35. [PubMed]
- Qiu Q, Cronce A, Patel J, Fluet GG, Mont AJ, Merians AS, Adamovich SV. Development of the Home based Virtual Rehabilitation System (HoVRS) to remotely deliver an intense and customized upper extremity training. J Neuroeng Rehabil. 2020;17(1):155. Epub 20201123. [CrossRef] [PubMed]
- MontJohnson A, Cronce A, Qiu Q, Patel J, Eriksson M, Merians A, Adamovich S, Fluet G. Laboratory-Based Examination of the Reliability and Validity of Kinematic Measures of Wrist and Finger Function Collected by a Telerehabilitation System in Persons with Chronic Stroke. Sensors (Basel). 2023;23(5). Epub 20230228. [CrossRef] [PubMed]
- Fluet G, Qiu Q, Patel J, Mont A, Cronce A, Yarossi M, Merians A, Adamovich S. Virtual Rehabilitation of the Paretic Hand and Arm in Persons With Stroke: Translation From Laboratory to Rehabilitation Centers and the Patient's Home. Front Neurol. 2021;12:623261. Epub 20210128. [CrossRef] [PubMed]
- Fluet GG, Qiu Q, Patel J, Cronce A, Merians AS, Adamovich SV. Autonomous Use of the Home Virtual Rehabilitation System: A Feasibility and Pilot Study. Games Health J. 2019;8(6):432-8. [CrossRef] [PubMed]
- Bourke-Taylor, H. Melbourne Assessment of Unilateral Upper Limb Function: construct validity and correlation with the Pediatric Evaluation of Disability Inventory. Dev Med Child Neurol. 2003;45(2):92-6. [CrossRef] [PubMed]
- Jongbloed-Pereboom M, Nijhuis-van der Sanden MW, Steenbergen B. Norm scores of the box and block test for children ages 3-10 years. Am J Occup Ther. 2013;67(3):312-8. [CrossRef] [PubMed]
- Mathiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther. 1985;39(6):386-91. [CrossRef] [PubMed]
- Chan A, Halevi T, Memon N, editors. Leap Motion Controller for Authentication via Hand Geometry and Gestures. Human Aspects of Information Security, Privacy, and Trust; 2015 2015//; Cham: Springer International Publishing.
- Martinie O, Mercier C, Gordon AM, Robert MT. Upper Limb Motor Planning in Individuals with Cerebral Palsy Aged between 3 and 21 Years Old: A Systematic Review. Brain Sci. 2021;11(7). Epub 20210712. [CrossRef] [PubMed]
- Middle Childhood (6-8 years of age). National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention: https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/middle.html; 2021.
- Smeragliuolo AH, Hill NJ, Disla L, Putrino D. Validation of the Leap Motion Controller using markered motion capture technology. J Biomech. 2016;49(9):1742-50. Epub 20160408. [CrossRef] [PubMed]
- Choi JY, Rha DW, Kim SA, Park ES. The Dynamic Thumb-in-Palm Pattern in Children with Spastic Cerebral Palsy and Its Effects on Upper Limb Function. Children (Basel). 2020;8(1). Epub 20201231. [CrossRef] [PubMed]
- Francisco-Martinez C, Prado-Olivarez J, Padilla-Medina JA, Diaz-Carmona J, Perez-Pinal FJ, Barranco-Gutierrez AI, Martinez-Nolasco JJ. Upper limb movement measurement systems for cerebral palsy: a systematic literature review. Sensors. 2021;21(23):7884. [CrossRef]
- Tung JY, Lulic T, Gonzalez DA, Tran J, Dickerson CR, Roy EA. Evaluation of a portable markerless finger position capture device: accuracy of the Leap Motion controller in healthy adults. Physiological measurement. 2015;36(5):1025. [CrossRef]
- Vysocký A, Grushko S, Oščádal P, Kot T, Babjak J, Jánoš R, Sukop M, Bobovský Z. Analysis of precision and stability of hand tracking with leap motion sensor. Sensors. 2020;20(15):4088. [CrossRef]
- Guna J, Jakus G, Pogačnik M, Tomažič S, Sodnik J. An analysis of the precision and reliability of the leap motion sensor and its suitability for static and dynamic tracking. Sensors. 2014;14(2):3702-20. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).