1. Introduction
The integration of robotic devices into healthcare settings for rehabilitation is rapid advancing, offering significant benefit for both therapists and patients [
1]. With the aging population in the United States projected to double, the demand for rehabilitation services due to age-related disorders is increasing [
2]. Meanwhile, stroke remains a leading cause of disability in the United States [
3]. These factors underscore the need for innovative solutions, and robotic devices present a promising answer. These devices can assist with daily living tasks and enhance therapy sessions, enabling patients to engage in repetitive rehabilitation movements that promote motor function recovery and reduce dependence on compensatory methods [
4]. By facilitating high-intensity training and incorporating machine learning techniques, robotic systems complement traditional therapy, offering patients the autonomy to self-train independently while providing valuable support to therapists [
5].
In stroke rehabilitation, primary goals include motor function recovery, improved movement coordination, and prevention of secondary complications like muscle atrophy and spasticity [
6]. To achieve these goals, robotics serves as invaluable tools in achieving these objectives, delivering quality treatment efficiently and cost-effectively [
1]. The application of robotics in rehabilitation applications spans various contexts and is characterized by diverse technical distinctions [
7]. They allow for precise and quantitative assessment of patient performance [
4], addressing both biomechanical and clinical aspects to alleviate movement impairments and facilitate task completion [
6].
Robotic systems in rehabilitation are generally categorized into two main types based on their technical differences: end-effector systems and exoskeleton systems [
5]. End-effector systems use manipulators to provide assistive or resistive forces, which can guide passive or active movement to improve positioning and movement patterns. Exoskeleton systems, on the other hand, attach directly to the limb joint axes and use electromagnetic motors to facilitate movements at multiple joints. The flexibility in setting up these devices is also important for their adaptation to diverse rehabilitation environments, often shared with various equipment and mobility aids [
6]. Configuring these devices for individual patients can be time-consuming, especially for those with complex designs [
9]. Many robotic systems incorporate feedback mechanisms, such as kinesthetic and tactile feedback, to promote correct movement patterns [
10].
Robotic aids serve different purposes, ranging from shared therapeutic systems in clinics to individual-use systems in home environments, assisting with activities of daily living [
6]. Development efforts focus on enhancing the functionality and usability of these devices. They can vary in complexity from single-purpose to multi-purpose, allowing patients greater control over limb movements and enabling them to replicate therapist-guided exercises independently [
9]. However, the high cost of these devices often makes them financially inaccessible for many patients [
11]. Some solutions involve using industrial robots to reduce cost, although these may lack the finesse and responsiveness of human limbs. Back-drivable devices, allowing user-generated movement in passive states, enable range of motion measurement and promote safety by not restricting user movements [
9].
For a rehabilitation robotic device, assisting patients in performing rehabilitation exercises is a critical function, whether through manual interaction with therapists or self-training sessions. Factors influencing the selection of a specific rehabilitation robot include cost, appearance, weight, adaptability, safety, size, and practicality. According to Riener et al. [
6], robots should appear “human-friendly” and behave accordingly, emphasizing safety, compactness, friendliness, quietness, and compliance to mimic the therapist’s hand during manual therapy, thus enhancing user comfort and natural interaction [
12]. “Ease of use” is critical for the adoption and success of robotic devices in rehabilitation settings [
8]. Robotic devices also offer potential solutions to this challenge, serving assistive roles for daily living tasks or aiding therapy sessions [
7]. These devices reduce labor intensity, increase repeatability, and minimize observation errors [
13] compared to manual therapy, facilitating high-intensity, reproducible therapy sessions. Despite their promising prospects, global clinical adoption of robotic aids in rehabilitation remains limited due to space constraints, cost concerns, and efficacy considerations [
11]. Safety and patient comfort are also paramount, given the close interaction with patients, emphasizing adaptability to human limbs and maximizing patient attention and effort during training [
9]. Despite their promise, challenges persist, potentially undermining representation of recovery outcomes [
5].
Although robot systems have long been investigated in rehabilitation settings, their efficacy is hampered by limitations such as inefficient processing of patient data and logistical challenges for patients, such as travel time to rehabilitation centers. Addressing these shortcomings, the integration of cyber-physical systems into rehabilitation emerges as a transformative solution [
15,
16]. Unlike standalone robots, cyber-physical systems leverage network connectivity and real-time data processing to enhance the efficiency and convenience of robot-based rehabilitation, addressing challenges such as inefficient patient data processing and logistical issues like travel time to rehabilitation centers [
17,
18]. By seamlessly integrating sensors, actuators, and computational algorithms, cyber-physical systems empower therapists to treat patients more effectively by providing actionable insights derived from comprehensive data analysis. This enables therapists to tailor treatment plans precisely to each patient’s unique needs, leading to improved outcomes.
Moreover, cyber-physical systems facilitate remote monitoring and intervention, allowing therapists to oversee patient progress and adjust treatment protocols without the need for in-person visits. This not only saves patients valuable time and resources but also ensures continuity of care, particularly for individuals residing in remote or underserved areas. Additionally, cyber-physical systems enable collaborative decision-making by facilitating communication and information sharing among healthcare professionals, further enhancing the quality and efficacy of rehabilitation services. Overall, the integration of CPS into rehabilitation represents a significant leap forward in leveraging technology to optimize patient care and outcomes.
Overall, the integration of cyber-physical systems into rehabilitation can mark a significant advancement in the field, offering comprehensive solutions to address the limitations of standalone robot systems. By harnessing the power of network connectivity and real-time data processing, cyber-physical systems enhance the efficiency and convenience of robot-based rehabilitation while empowering therapists to deliver more personalized and effective care. Through remote monitoring and intervention, cyber-physical systems enable seamless collaboration among healthcare professionals and ensure continuity of care for patients, ultimately leading to improved outcomes. As technology continues to evolve, the integration of cyber-physical systems into rehabilitation holds immense promise for revolutionizing the way we approach patient care and rehabilitation therapy.
2. Platform Structure of Proposed Cyber-Physical Rehabilitation System
To construct a cyber-physical rehabilitation system for patients and therapists, distinct subsystems interacting with individual users must be implemented. On the patient’s side, an exoskeleton connected to the server for assistance is essential, while the therapist’s side requires a robotic device with sufficient degrees-of-freedom tailored to the targeted affected body part. Bridging the patients and the therapist sides, a cloud server is necessary to integrate the subsystems for designated tasks. On the patient’s side, the subsystem must facilitate interaction with the remote therapist, execute assigned rehab activities, and assist the patient in their daily activities. Conversely, on the therapist’s side, a mechanism is required to accurately replicate the patient’s motions, enabling the therapist to assess the progress of their rehabilitation.
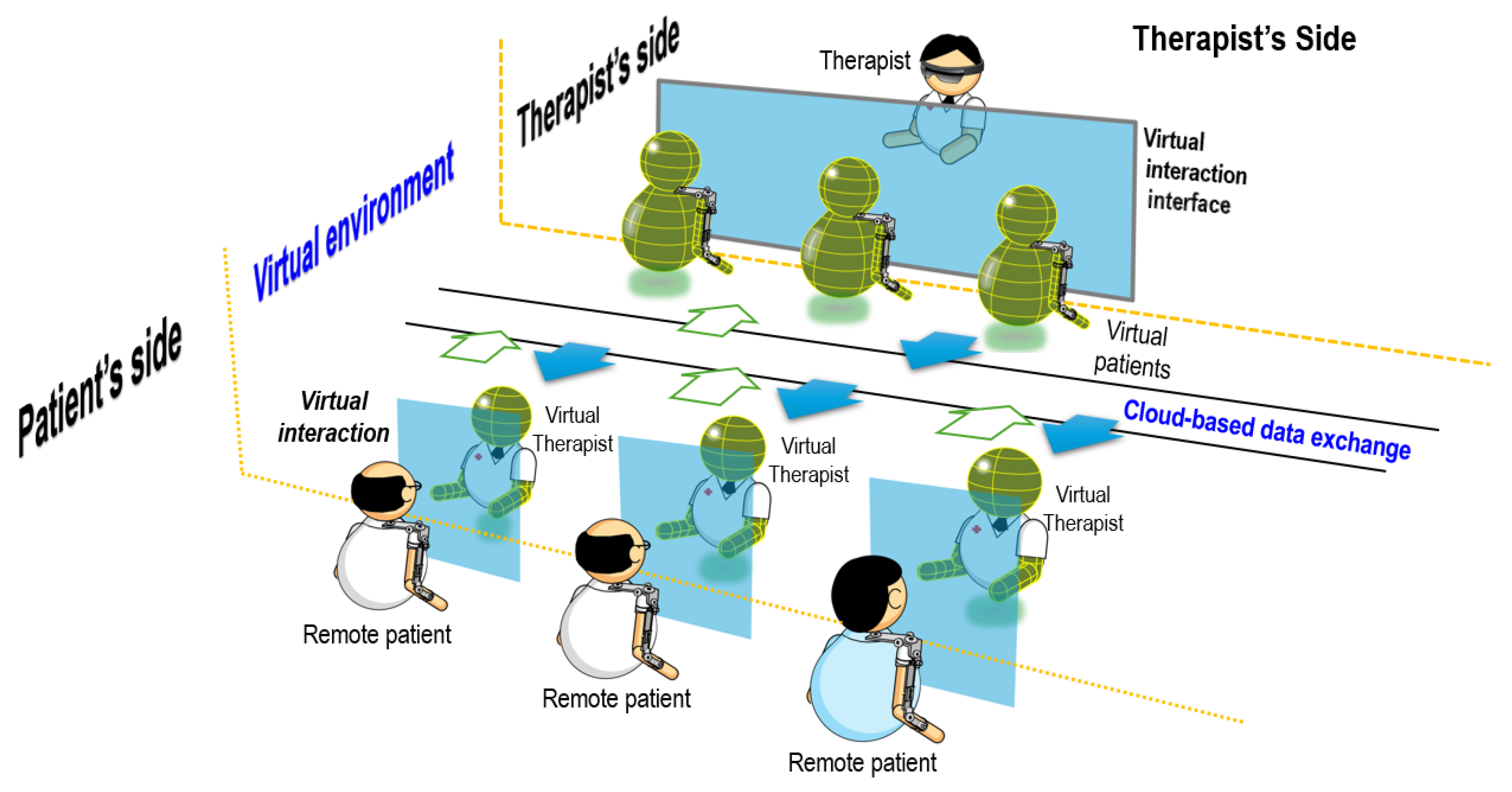
Figure 1 illustrates the overall system of the cyber-physical system used for rehabilitation.
2.1. Traditional Rehabilitation Sessions
In a rehabilitation session focused solely on motor skill recovery for brain-injured patients, the therapist follows a structured process aimed at facilitating optimal recovery and functional improvement. The session typically begins with an assessment of the patient’s current motor abilities, including range of motion, muscle strength, coordination, and motor control. This assessment helps the therapist understand the extent of the patient’s impairment and tailor the rehabilitation plan accordingly. Once the assessment is complete, the therapist develops a personalized rehabilitation program targeting specific motor skills that need improvement. This program includes a variety of exercises and activities designed to promote neuroplasticity and enhance motor learning.
During the session, the therapist typically provides hands-on guidance and instruction to ensure the patient performs each exercise correctly and safely. They may use manual techniques, verbal cues, visual demonstrations, and tactile feedback to help the patient understand and execute the movements effectively. The therapist also monitors the patient’s progress closely, adjusting the intensity and complexity of the exercises as the patient’s abilities improve. Throughout the session, the therapist emphasizes the importance of repetition and consistency in motor skill rehabilitation. They encourage the patient to practice the exercises regularly, both during therapy sessions and independently at home, to maximize the benefits of rehabilitation. The therapist also educates the patient about proper body mechanics, strategies for overcoming movement limitations, and techniques for preventing injury.
At the end of the session, the therapist evaluates the patient’s performance and progress, noting any improvements or areas of concern. They may discuss goals for future sessions, modifications to the rehabilitation plan, and strategies for overcoming challenges. The therapist also provides feedback and encouragement to motivate the patient to continue their rehabilitation efforts outside of therapy sessions.
2.2. Exoskeleton Subsystem on Patient’s Side
Relearning motor skills for a brain-injured patient is a critical aspect of rehabilitation, and incorporating exoskeleton technology can greatly enhance this process. Exoskeletons offer a promising tool for these patients as they provide targeted assistance and feedback to aid in motor relearning. By supporting weakened or impaired limbs, exoskeletons facilitate the execution of movements, allowing patients to engage in repetitive and task-specific exercises essential for motor recovery. One of the key benefits of exoskeletons is their ability to provide precise assistance tailored to the individual needs of stroke patients. These devices can be programmed to support specific joint movements, providing assistance where it is most needed while allowing patients to actively participate in the rehabilitation process. By assisting with movement initiation, maintaining proper alignment, and providing resistance during exercises, exoskeletons help patients relearn motor skills more effectively.
Moreover, exoskeletons can offer real-time feedback, enabling patients to better understand and refine their movements. Through sensors embedded in the device, patients receive immediate feedback on their joint angles, muscle activity, and performance metrics. This feedback loop enhances proprioception and kinesthetic awareness, allowing patients to make adjustments and corrections to their movements in real-time, leading to more precise and controlled motor relearning. Exoskeleton on the patient’s side can fulfill dual roles. It serves to aid the therapist in conducting rehabilitation activities while also assisting the patient in performing daily tasks. Additionally, exoskeletons promote neuroplasticity by providing intensive and repetitive training, which is essential for rewiring neural pathways in the brain. By engaging in repetitive movements facilitated by the exoskeleton, patients stimulate neuroplastic changes in the brain, promoting motor learning and recovery. This enables patients to rehabilitate at their own pace, adapting the process to their individual needs and abilities. This adaptive process allows the brain to reorganize and form new connections, leading to improvements in movement control, coordination, and motor function over time. Exoskeletons can also facilitate the transition from rehabilitation to daily life activities. By training in a supportive and controlled environment with the exoskeleton, patients can gradually regain the confidence and skills necessary to perform activities of daily living independently. This transition is crucial for promoting functional independence and improving overall quality of life for stroke survivors.
When not utilized for rehabilitation within a cyber-physical system, the exoskeleton on the patient’s side serves as a tool for replicating instructions from the therapist. Additionally, it can memorize the assigned rehab activities and ensure the patient focuses on specific motions designated by the therapist. By doing so, the patient can save time typically spent traveling between the clinic or medical center and their residence. Furthermore, through motion capturing functionality, the exoskeleton can record the patient’s progress for self-assessment or evaluation by the therapist.
For therapists, the utilization of exoskeleton technology offers the advantage of remote monitoring and supervision. Therapists can remotely observe and assess their patients’ progress in real-time, providing timely feedback and adjusting rehabilitation plans as needed. This remote monitoring capability not only enhances the efficiency of therapy sessions but also allows therapists to oversee multiple patients simultaneously, optimizing their time and resources. For patients, the use of exoskeletons provides increased motivation and engagement in the rehabilitation process. The visual and tangible feedback provided by the exoskeleton reinforces progress and achievements, encouraging patients to continue their efforts. Additionally, the ability to monitor their own progress through recorded data promotes autonomy and self-management, empowering patients to take an active role in their recovery journey.
2.3. Robotic Subsystem on Therapist’s Side
In a cyber-physical system where an exoskeleton is worn by the patient and a robot is utilized on the therapist’s side to replicate the patient’s motion in real-time, the robot serves several essential functions and offers distinct advantages. The robot on the therapist’s side accurately mimics the patient’s movements, providing the therapist with a real-time visual representation of the patient’s motor abilities. This enables the therapist to closely monitor the patient’s progress and make immediate adjustments to the rehabilitation program as needed. By replicating the patient’s motion with precision, the robot allows the therapist to remotely assess the effectiveness of exercises and interventions, ensuring that the rehabilitation plan is tailored to the patient’s specific needs and capabilities. The robot also facilitates hands-on guidance and assistance from the therapist, even in remote or virtual settings. Through the use of force feedback and control mechanisms, the therapist can interact with the patient’s movements in real-time, providing tactile cues and corrections to improve technique and optimize motor learning. This interactive aspect of the robot’s function enhances the therapeutic relationship between the therapist and patient, fostering trust, engagement, and collaboration in the rehabilitation process.
Additionally, the robot’s ability to replicate the patient’s motion offers significant advantages in terms of scalability and accessibility. Therapists can remotely supervise and guide multiple patients simultaneously, maximizing their efficiency and reach. This scalability allows for more widespread access to specialized rehabilitation services, particularly in underserved or remote areas where access to rehabilitation facilities may be limited. Furthermore, the use of robotics in rehabilitation reduces the physical demands on therapists, minimizing the risk of fatigue and injury while increasing their capacity to provide high-quality care to a larger number of patients. Overall, the robot’s function in replicating the patient’s motion in real-time within a cyber-physical system enhances the effectiveness, efficiency, and accessibility of motor rehabilitation interventions. By providing accurate feedback, facilitating hands-on guidance, and enabling remote supervision, the robot contributes to improved outcomes and enhanced patient-centered care in rehabilitation settings.
2.4. Cloud Server between Patients and Therapists
In such a cyber-physical system where patients interact with therapists through exoskeletons and robots, a central server plays a crucial role in facilitating communication, data exchange, and coordination between the patient and therapist subsystems. The server serves as the backbone of the system, managing information flow, processing commands, and ensuring seamless interaction between all components involved.
The server facilitates real-time communication between the patient’s exoskeleton and the therapist’s robot. It acts as a centralized hub, receiving input from the patient’s exoskeleton regarding their movements and transmitting this data to the therapist’s robot, which then replicates the movements in real-time. Conversely, the server also receives feedback from the therapist’s robot regarding any adjustments or interventions made during the session, which is relayed back to the patient’s exoskeleton to provide immediate feedback or corrections. Additionally, the server stores and manages patient data, including historical rehabilitation sessions, progress reports, and personalized rehabilitation plans. Centralized storage allows therapists to access and review patient information from any location, enabling continuity of care and informed decision-making. Moreover, the server may incorporate algorithms or machine learning techniques to analyze patient data and generate insights or recommendations to optimize rehabilitation strategies based on individual progress and preferences. The server also facilitates remote monitoring and supervision by therapists, allowing them to observe and interact with patients in real-time, regardless of their physical location. Through secure connections and encrypted communication protocols, therapists can access the system from anywhere with internet connectivity, providing flexibility and accessibility in delivering rehabilitation services. This remote monitoring capability enhances the efficiency of therapy sessions, reduces the need for in-person appointments, and enables therapists to oversee multiple patients simultaneously, maximizing their time and resources. Overall, the server in a patient-therapist cyber-physical system acts as a central hub for communication, data management, and remote supervision. By facilitating real-time interaction, storing patient data, and enabling remote monitoring, the server enhances the effectiveness, efficiency, and accessibility of motor rehabilitation interventions, ultimately improving patient outcomes and quality of care.
3. Operation Modes of Proposed Cyber-Physical System
Depending on the tasks at hand, the server and the subsystems can operate in different modes, including data-collection mode, rehabilitation mode, and assistive mode. The first mode, the data-collection mode, enables the system to collect human motion data on the client side and store them on the server. In the second mode, the rehabilitation mode, the client-side system generates rehabilitation motions with force feedback and control compensation to guide the assistive device along the required trajectory. This allows the device to mimic the therapist’s prescribed rehab activities. Meanwhile, a device on the therapist’s side tracks the patient’s motion trajectory to monitor their performance. The server collects all necessary information from both sides, enabling corresponding trajectories to be replicated. If the therapist is unavailable in rehabilitation sessions, the server can still generate the required trajectories for rehab activities. The third mode, the assistive mode, enables the platform to provide assistance in the patient’s daily activities. Here, the predetermined trajectories for corresponding motions ensure the assistive device can apply the necessary force, required motion prediction and force compensation on the patient’s side.
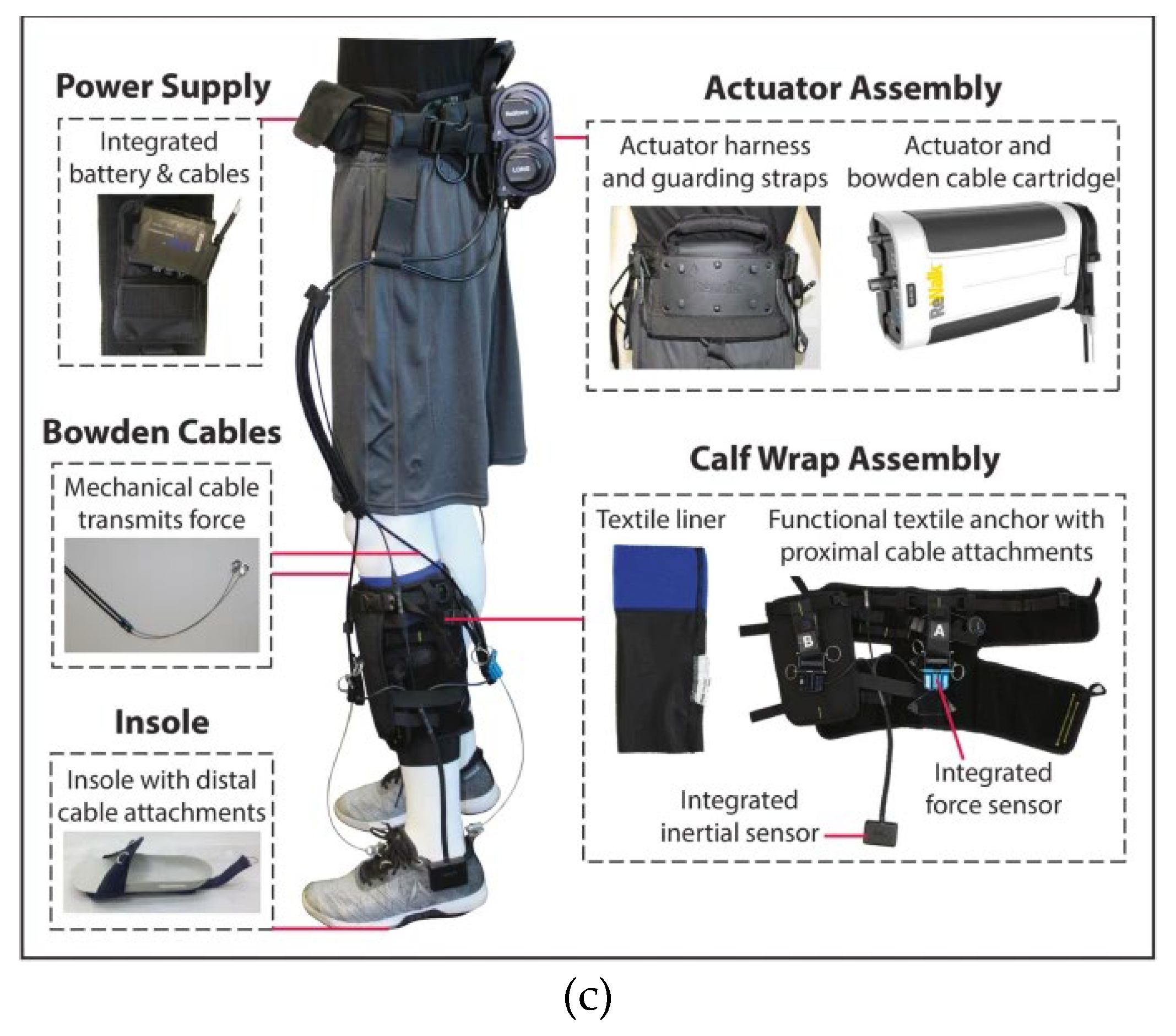
Figure 2.
Schematic diagram of the assistive exoskeleton device.
Figure 2.
Schematic diagram of the assistive exoskeleton device.
3.1. Data-Collection Mode
To ensure the cyber-physical system effectively facilitates patient-therapist interactions, it is imperative that the robots on both sides possess robust data-collection capabilities. On the therapist’s side, the robot functions as a joystick, recording the precise movements utilized during rehabilitation sessions. This recorded data is then stored by the server, enabling therapists to access and review the specific motions prescribed for each patient’s rehabilitation regimen. By maintaining a comprehensive record of rehabilitation exercises, therapists can tailor treatment plans to individual patients’ needs and monitor progress over time. Conversely, on the patient’s side, the exoskeleton serves as a primary data-collection tool, capturing the exercises performed by the patient during rehabilitation sessions. This data is invaluable for assessing the patient’s progress and adherence to prescribed exercises. The collected data can also be leveraged to model the movement patterns of the patient, enabling the exoskeleton to anticipate and provide assistance for intended motions. By analyzing movement data over time, therapists can gain insights into the effectiveness of rehabilitation interventions and make informed decisions regarding treatment adjustments.
Furthermore, the data collected by the robots in the cyber-physical system can be utilized for various purposes beyond assessment and modeling. For example, machine learning algorithms can be applied to analyze movement patterns and identify trends indicative of progress or areas for improvement. Additionally, the data can be anonymized and aggregated to contribute to research efforts aimed at advancing rehabilitation science and optimizing patient outcomes.
In summary, robust data-collection capabilities are essential for the effective operation of a rehabilitation cyber-physical system in facilitating patient-therapist interactions and supporting rehabilitation efforts. By recording and analyzing joint movements, the robots enable therapists to tailor treatment plans, monitor patient progress, and provide targeted assistance, ultimately enhancing the quality and efficacy of motor rehabilitation interventions.
3.2. Rehabilitation Mode
In the rehabilitation mode, or training mode [
28], of the cyber-physical system, there are two distinct functions aimed at optimizing patient-therapist interaction and facilitating self-paced rehabilitation. The therapist-patient interaction function enables virtual engagement between the therapist and patient during the rehabilitation session, fostering real-time communication and guidance. Through the system, the therapist applies instructions via the robot on their side, which in turn prompts the exoskeleton worn by the patient to generate corresponding motions. This interactive process allows the therapist to remotely guide the patient through rehabilitation exercises, providing verbal cues, visual demonstrations, and tactile feedback as needed. Crucially, force feedback from the patient’s side ensures that the therapist can gauge the resistance and muscular response, facilitating accurate assessment and adjustment of the rehabilitation program. This virtual interaction type enhances accessibility to therapy sessions, enabling patients to receive guidance and support from therapists regardless of geographical constraints or physical limitations.
Concurrently, the self-paced rehabilitation function allows patients to engage in rehabilitation activities autonomously, according to their own pace and schedule. The exoskeleton not only facilitates real-time motion following based on therapist instructions but also allows patients to initiate and perform rehabilitation exercises independently. This flexibility enables patients to engage in rehabilitation sessions at their convenience, whether during scheduled therapy sessions or self-directed practice sessions. By empowering patients to take control of their rehabilitation journey, this function of rehabilitation mode promotes self-efficacy, motivation, and active participation in the recovery process. Additionally, the exoskeleton’s ability to generate designated motions at any time provides patients with continuous access to rehabilitation exercises, fostering consistency and adherence to the prescribed treatment plan.
3.3. Assistive Mode
In the assistive mode of the cyber-physical system, the exoskeleton plays an important role in providing necessary assistance to guide the patient’s motion, allowing them to perform activities independently. This assistance is based on the ongoing motion detected by the exoskeleton, enabling the patient to carry out tasks without requiring external assistance. The implementation of exoskeletons includes various mechanisms tailored to specific needs, particularly focusing on lightweight and cost-effective designs for upper limb activities. Over the past decade, numerous research groups have proposed diverse designs to facilitate daily activities involving upper limbs, while similar efforts have been directed towards developing exoskeletons for lower limb mobility and functionality across different activities. Regardless of the type, a common requirement for assistive exoskeletons is their ability to predict ongoing motions and provide the necessary support.
One essential aspect of the assistive exoskeleton is its independence from fixed stations, necessitating wireless connectivity to the server for operational commands and stand-alone power supply. This ensures mobility and flexibility in usage, allowing patients to move freely without constraints imposed by stationary devices. In instances where network connection is unavailable, the onboard controller should be capable of detecting common motions and providing assistance autonomously to ensure patient safety and basic functionality. Additionally, even if specific motions cannot be recognized by the onboard controller, the exoskeleton should still offer support to maintain essential functions. When connected to the network, computation for motion prediction can be shifted to an online processor linked to a motion library, expanding the range of applicable motions that the assistive exoskeleton can support. Furthermore, careful consideration must be given to power storage capacity to ensure sufficient operational time for patients to carry out required functions effectively.
The assistive mode of the cyber-physical system comprises both offline and connected components, offering flexibility in usage based on the availability of network connectivity. Through wireless communication and onboard processing capabilities, the assistive exoskeleton provides patients with necessary support for independent motion execution, contributing to enhanced mobility and functionality in various activities of daily living.
4. Required Techniques for Rehabilitation Cyber-Physical Systems
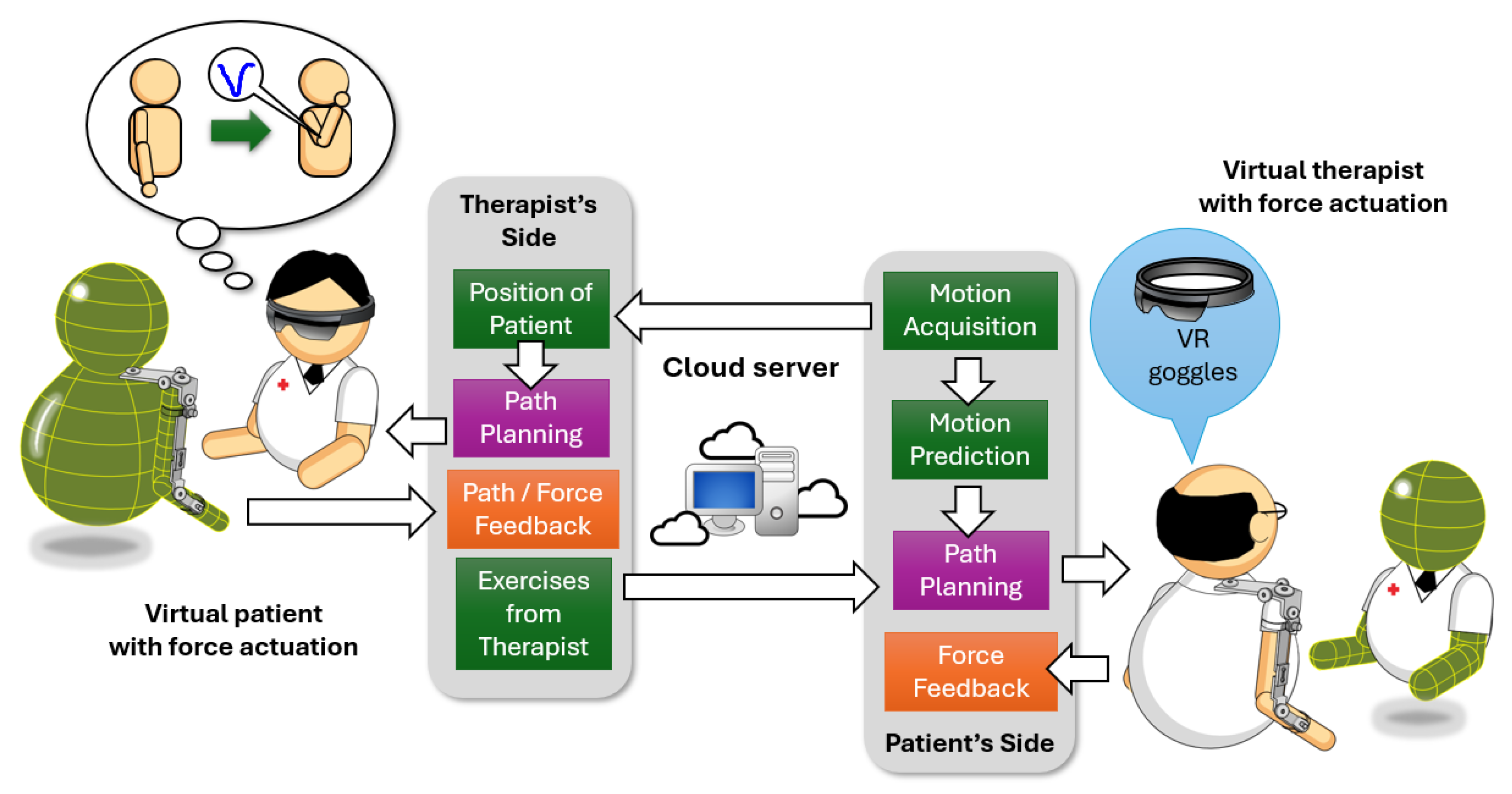
Effective rehabilitation relies heavily on the interactions between patients and therapists, encompassing oral, visual, and tactile communications, particularly regarding force responses in affected areas. A wearable robotic system on the patient’s side serves a dual purpose: as an interactive tool emulating therapist-guided activities, enabling patients to feel applied forces during rehabilitation, and as a daily activity aid, assisting with arm movements. On the therapist’s side, a robotic device replicates the patient’s motions with corresponding force and position feedback, aiding therapists in guiding required activities. The cloud-based server facilitates communication between patients and therapists, enabling the exchange of 3D images, voices, and force feedback. Virtual reality headsets further enhance interaction by immersing patients and therapists in a shared virtual environment. To implement such a cyber-physical system used for rehabilitation as well as assistance for daily activities, several techniques need to be developed. In this study, we focused on the system developed at West Virginia University.
4.1. Mechanism of Robot Mechanisms
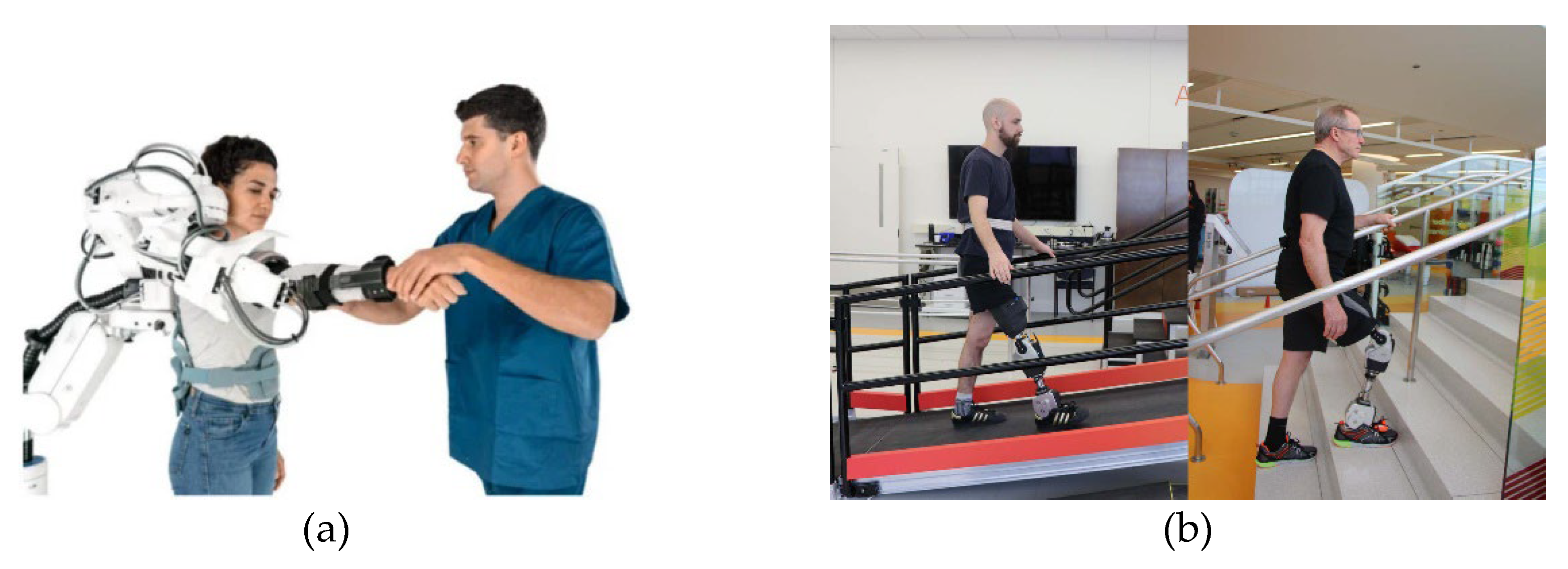
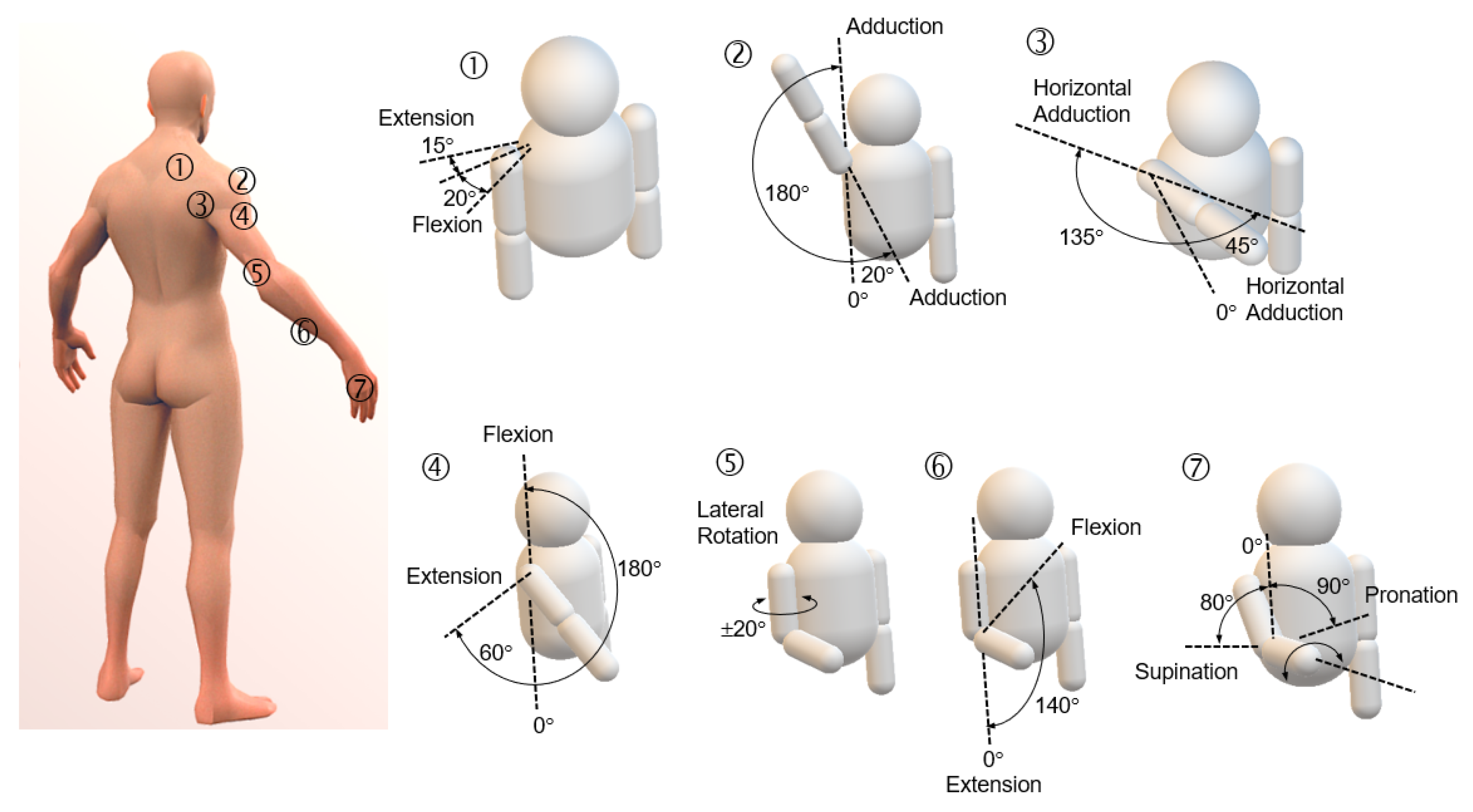
A rehabilitation cyber-physical system should incorporate two essential robotic mechanisms: one designed for the patient’s use and the other for the therapist’s utilization. The exoskeleton utilized empowered by patients is governed by the degree of freedom (DOF), which is a critical factor. For upper limbs, the total DOFs is typically 11 [
19] for each arm, excluding the palm. However, some studies have simplified the mechanism to focus on dominant joints, reducing the DOFs to 5 [
20], as shown in
Figure 3a. In case of lower limbs, the exoskeleton typically features 7-DOFs for each leg [
21,
22,
23]. Consequently, both the robots and exoskeletons used by therapist and patients must possess identical number of DOFs to facilitate rehabilitation activities effectively. Recent innovations, such as the Open Source Leg, as illustrated in
Figure 3b, developed by the Nerobionics Lab, allow users to program prosthetic legs using provided APIs, offering flexibility to adapt the robot to diverse operating environments [
24]. The reprogrammable feature of exoskeletons can offer the advantage of customization to better align with the patient’s habitual movements during daily activities.
Figure 3.
(
a) A Float upper limb exoskeleton for rehabilitation fabricated by Rehab Technologies Lab [
20]. (
b) An Open Source Leg developed by the Neurobionics Lab [
24]. (
c) A ReWalk ReStore™ exosuit that consists of an actuator assembly, calf wrap assembly, and shoe insole. [
25].
Figure 3.
(
a) A Float upper limb exoskeleton for rehabilitation fabricated by Rehab Technologies Lab [
20]. (
b) An Open Source Leg developed by the Neurobionics Lab [
24]. (
c) A ReWalk ReStore™ exosuit that consists of an actuator assembly, calf wrap assembly, and shoe insole. [
25].
Despite advancements, existing designs still encounter limitations concerning mobility due to constraints related to power sources and bulky control units. Efforts have been made to redistribute loadings to alternative locations; however, these restrictions impede usability due to weight and available power. Lightweight exosuit systems tailored [
25], as shown in
Figure 3c, for elderly and stroke patients have been proposed to address mobility and versability issues, yet further development is required. Although many current systems are bulky and heavy, they provide sufficient driving force and DOFs to support the force required by patients. These systems often incorporate more powerful processing units to ensure efficient operation and processing of tasks.
Figure 4 illustrates the simplified 7-DOFs associated with a single human arm.
Considering the various considerations outlined, an optimal exoskeleton mechanism for patient use should ideally prioritize characteristics such as lightweight construction, extended operational duration, ample driving force, and reprogrammable functionality to accommodate individualized needs. While existing designs may not fully meet these criteria, it is imperative to incorporate these factors into the future development of rehabilitation exoskeletons. Additionally, advancements in materials science, battery technology, and software programming may contribute to addressing these challenges and ultimately enhance the efficacy and usability of exoskeleton devices in rehabilitation settings.
The robotic mechanism on the therapist’s side functions as a real-time playback system, facilitating observation of the patient’s rehabilitation activities. In the clinical settings, therapists often manually guide patient’s movements to ensure adherence to prescribed exercises [
27]. Thus, this robotic mechanism also serves as a joystick, providing both force and position feedback obtained from the patient’s side [
28]. Accurate control of force and position within this multi-axial system is critical for enabling therapists to closely monitor patients’ movements. Furthermore, this device doubles as a playback tool for patient exercises during self-rehabilitation sessions. It records and replays exercises, aiding patients in reviewing patient progress and providing feedback. This versatility enhances the efficiency and effectiveness of rehabilitation sessions, both in clinical setting and during the independent patient practice. Additionally, the device’s role in recording exercises for self-rehabilitation sessions empowers patients to engage in structured rehabilitation activities outside of clinical sessions, promoting continuity of case of progress tracking.
4.2. Motion Acquisition
Motion acquisition is essential for a rehabilitation cyber-physical system, translating physical movements into digital data for interpretation and interaction by other users. Some rehabilitation systems use computer vision techniques, typically confined to fixed locations and lacking mobility, such as those equipped with RGB-D cameras or specialized motion capturing setups [
29,
30]. These systems capture the patient’s motion holistically and reduce the need for wiring individual sensors, making maintenance easier. However, for applications requiring mobility, like exoskeletons in rehabilitation activities, motion acquisition sensors must be integrated directly into the wearable device to ensure seamless movement and data capture.
To effectively monitor and support rehabilitation activities, various sensors are used for motion acquisition in a cyber-physical system. These sensors capture and relay detailed information about the patient’s movements, enabling precise and adaptive assistance. The key types of sensors used for motion acquisition include:
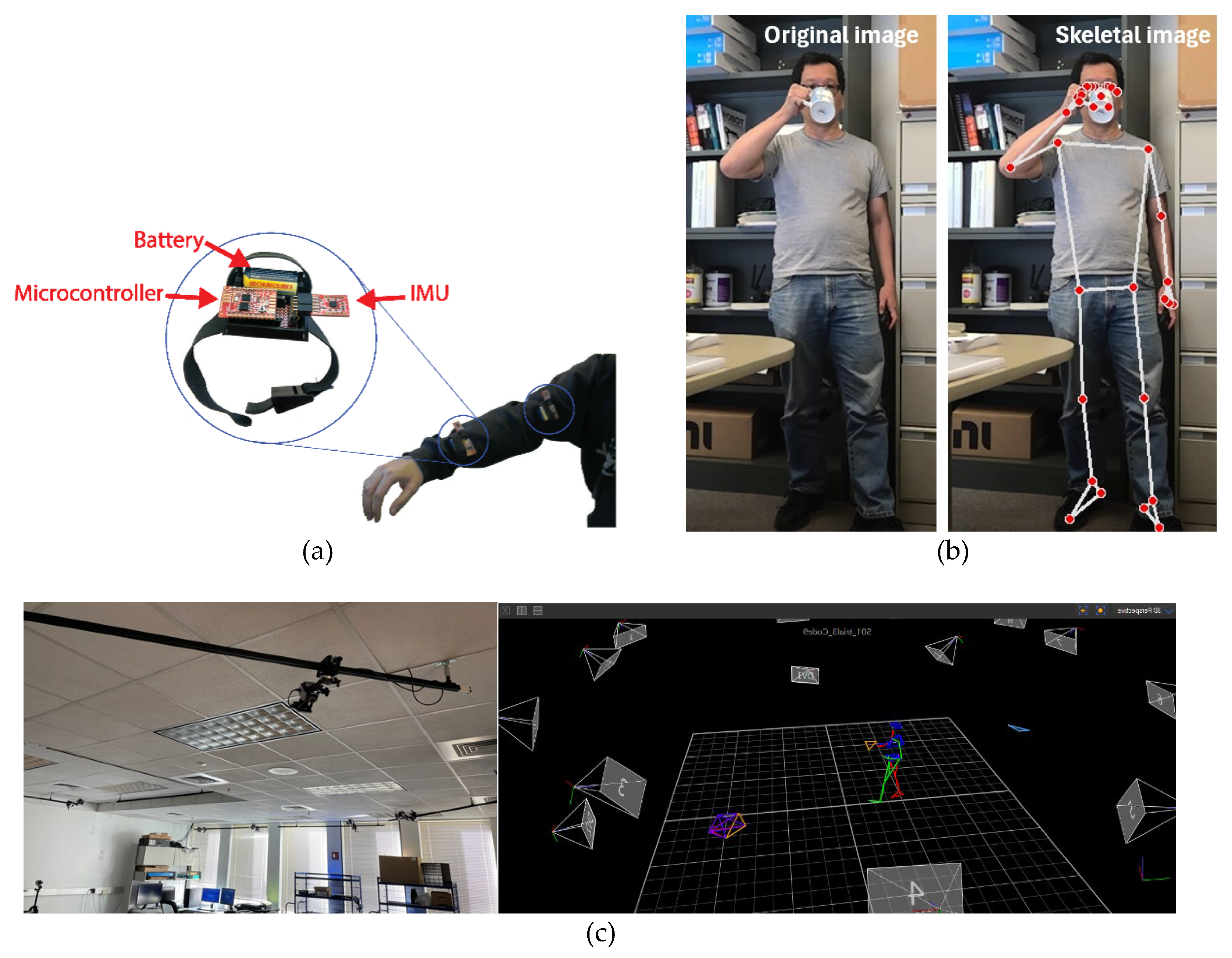
Inertial Measurement Units (IMUs): IMUs are widely used due to their versatility and cost-effectiveness. They typically combine accelerometers, gyroscopes, and sometimes magnetometers to measure linear acceleration, angular velocity, and orientation [
31]. These sensors are particularly useful for tracking dynamic movements of body segments, providing real-time data on joint angles, velocities, and accelerations [
32,
33,
34].
Figure 5a shows a wearable IMU setup for arm motion acquisition. However, IMUs can be susceptible to noise and drift, necessitating the use of algorithms like Kalman filters and sensor fusion techniques to enhance accuracy [
35].
Force Sensing Arrays (FSRs): FSRs measure the force or pressure applied to specific areas of the body and have been widely applied to the exoskeleton of lower limb applications [
36,
37]. These sensors are critical for understanding the external forces acting on the patient during rehabilitation exercises or the force the patient applies to specific areas. FSRs consist of a grid of force-sensitive resistors that change resistance in response to pressure, providing data on the magnitude and distribution of forces. This information ensures that patients perform exercises correctly and safely, adjusting the level of assistance provided by the robotic system.
Motion Capture Systems: These systems, including RGB-D cameras and marker-based setups, provide highly accurate and detailed motion data. RGB-D cameras combine traditional RGB imaging with depth sensing to capture three-dimensional movements without wearable sensors [
38,
39]. Marker-based systems use reflective markers on the body tracked by cameras. These systems are often used in clinical and research settings where high precision is required, but their fixed setup limits mobility and practicality for everyday use [
40].
Figure 5b displays the skeletal information obtained from a motion capture using an RGB-D camera, processed with the open-source MediaPipe framework.
Figure 5c illustrates a VICON motion capture system set up in a lab environment with 16 cameras, along with the rendered motion animation.
Additional Sensors and Techniques: Other sensors, such as electromyography (EMG) sensors, monitor muscle activity by measuring electrical signals generated by muscle contractions. This provides insight into the patient’s muscle activation patterns and neuromuscular function. Combining data from multiple sensor types offers a comprehensive understanding of the patient’s movements and condition [
41,
42].
Figure 5 illustrates the common methods used for capturing human motion. The integration of these sensors into exoskeletons enables real-time monitoring of the patient’s movements and progress during rehabilitation. By capturing and analyzing kinematic data, therapists can tailor interventions and exercises to each patient’s specific needs, optimizing the effectiveness of the rehabilitation process. Moreover, the mobility afforded by wearable exoskeletons allows for rehabilitation activities to be conducted in various settings, including home environments, increasing accessibility and convenience for patients.
For effective motion recognition, the motion acquisition devices must be integrated on the patient’s side. These sensors typically capture joint angles, which are then translated into movements of individual body parts for interpretation by the control unit. The data collected includes positions, velocities, and accelerations, along with patient-specific body information. When adequately modeled, this kinematic information helps the control unit identify the type of ongoing motions [
43]. However, while IMUs offer valuable kinematic data, they do not provide measurements of the force or pressure applied to specific body parts. Therefore, additional sensors capable of measuring pressure or force may be necessary on the exoskeleton.
Forces and pressure information integrated with motion acquisition play an essential role in gait analysis for specific postures of the human body. Additionally, force and gesture information aid the control unit in responding to the patient’s movements and intentions. Gesture information derived from motion acquisition measurements enables the rehabilitation system to understand the patient’s intended actions and identify any difficulties encountered during exercises [
44,
45]. This information is particularly valuable when the exoskeleton device is utilized in assistive mode, allowing the control unit to predict ongoing motions and provide appropriate assistance accordingly. Integrating such sensors enhances the exoskeleton’s ability to provide tailored assistance based on both motion and force feedback, optimizing the rehabilitation process.
4.3. Motion Recognition
One key advantage of using cyber-physical system for both rehabilitation and assistance is the ability of the exoskeleton device to prevent further injuries caused by minor accidents, such as fall or muscle misuse. Consequently, recognizing patient’s motions and providing timely, appropriate assistance is important. To achieve this, the cyber-physical system must not only identify the motions being performed by the patient but also predict these motions based on partial movement of observed joints.
After the signals are collected by the sensors, they need to be sent to the control unit for analysis and determination of the type of captured motion. Before the data can be analyzed, sensor fusion combines data from multiple sensors and is typically used to improve motion recognition accuracy. Algorithms commonly utilized in sensor fusion include the Kalman filter, particle filter, and complementary filter. The Kalman filter is adept at estimating the state of a dynamic system by amalgamating measurements from various sensors while accommodating noise and inaccuracies [
47,
48]. It finds particular utility in real-time motion tracking applications. In contrast, the particle filter was developed to address non-linear and non-Gaussian systems, making it suitable for processing data pertaining to intricate motion patterns [
49,
50]. To mitigate the computational burden on the control unit, a complementary filter was introduced [
51]. This filter simplifies the Kalman filter process, rendering it suitable for applications where computational resources are limited. By combining the strengths of different sensors and filter algorithms, sensor fusion optimizes motion recognition accuracy, facilitating more effective control and assistance in rehabilitation scenarios.
Once the collected motion data is adequately processed, it can be used by the system to identify the type of motions. Recently, various machine learning and deep learning methods have been proposed for this purpose showing promising results [
19]. These methods include support vector machines (SVM) [
52], random forests, K-nearest neighbors (KNN) [
53], convolutional neural networks (CNNs) [
54], recurrent neural networks (RNNs) [
55], and autoencoders, etc. Among these methods, SVMs are effective in classification tasks, making them suitable for distinguishing between different types of movements. They work by finding the hyperplane that best separates the data into different classes. Random Forests ensemble learning method combines multiple decision trees to improve classification accuracy, which is robust against overfitting and can handle large datasets with many features. KNN classifies a motion by comparing it to the most similar instances in the dataset. This method is simple and effective, especially for smaller datasets or less complex motion patterns. CNNs are widely used for processing spatial data and have been highly successful in image and video recognition tasks. In motion recognition, CNNs can process time-series data from sensors to identify complex patterns in human movement. RNNs, particularly Long Short-Term Memory (LSTM) networks [
56], are designed to handle sequential data. They are well-suited for capturing temporal dependencies in motion data, making them ideal for recognizing continuous movements over time. Autoencoders are used for unsupervised learning tasks. They can learn efficient representations of motion data, which can then be used for clustering similar movements or detecting anomalies in motion patterns. To further accelerate the computation processes of these machine learning and deep learning methods, efficient data processing techniques are employed to better capture the distinct characteristics of various human motions.
Combining different algorithms can leverage the strengths of each method. For example, a system might use CNNs to extract features from raw sensor data and then apply an SVM for classification. Alternatively, RNNs can be used to model temporal dependencies, with a Kalman filter applied to refine the motion estimates. These methods help create systems that can monitor patient progress, predict upcoming movements, and provide necessary assistance, ultimately enhancing the rehabilitation experience and outcomes for patients.
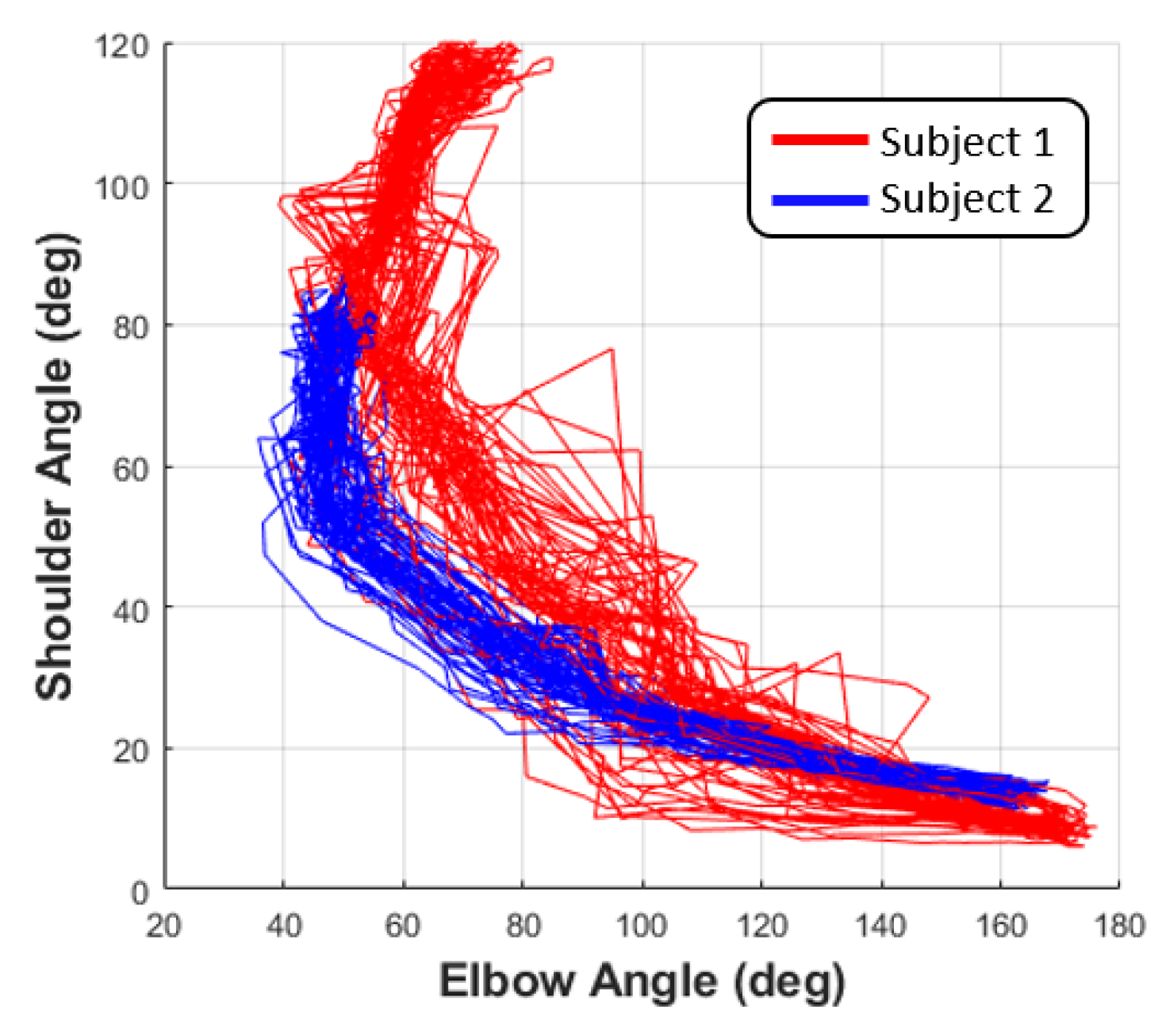
Figure 6 illustrates a drinking water motion that can be performed similarly by individuals on their own and can also exhibit similarities across different individuals [
57].
Figure 6 illustrates the self-similarity and cross-similarity observed in a drinking motion.
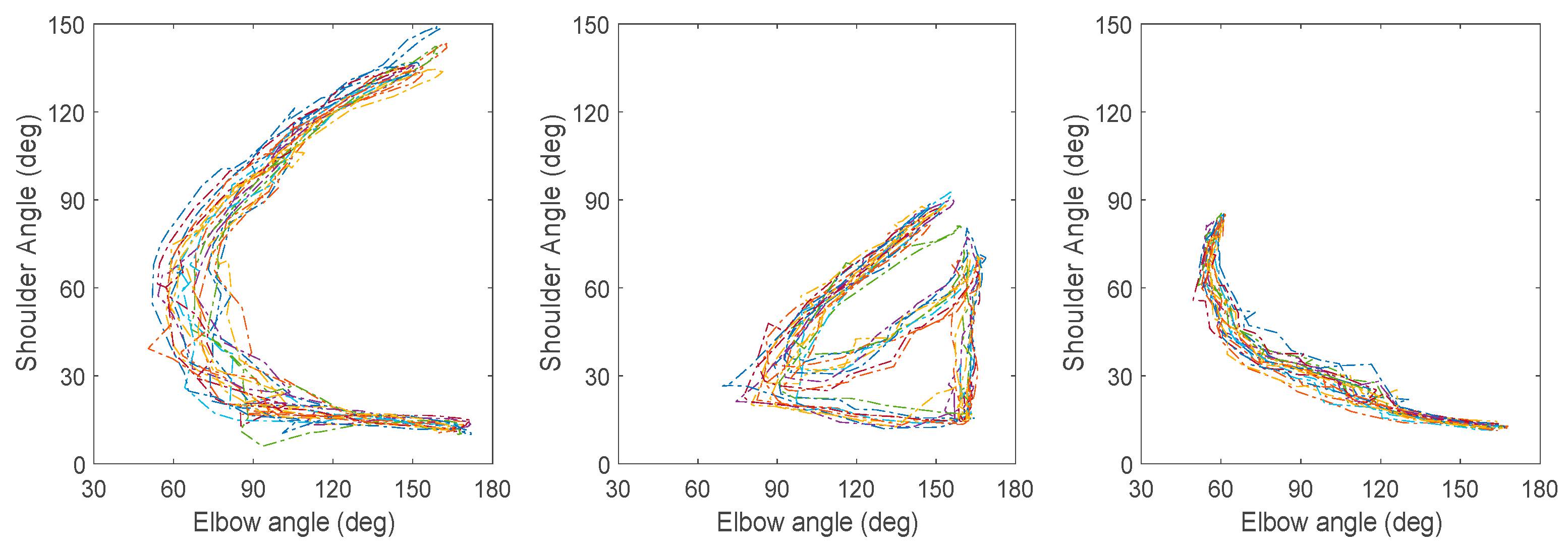
Figure 7 demonstrates the three selected motions used in motion prediction model utilizing CNNs. With the help of these innovative modeling techniques, some results suggest that the accuracy rate can exceed 97% for selected self-similar motions. Additionally, the type of an ongoing motion can be determined after the initial one-third of the motion is performed [
57]. This approach enables the exoskeleton device to respond appropriately and adopt suitable trajectories to assist patients in their daily activities. However, these approaches require a large dataset of recorded motions performed by stroke patients in different phases to ensure the model can precisely predict the types of ongoing motions. Human motion recognition in rehabilitation research activities relies on advanced algorithms that process sensor data to identify and interpret various physical movements. These algorithms are critical for developing effective rehabilitation systems that can monitor patient progress and provide appropriate assistance.
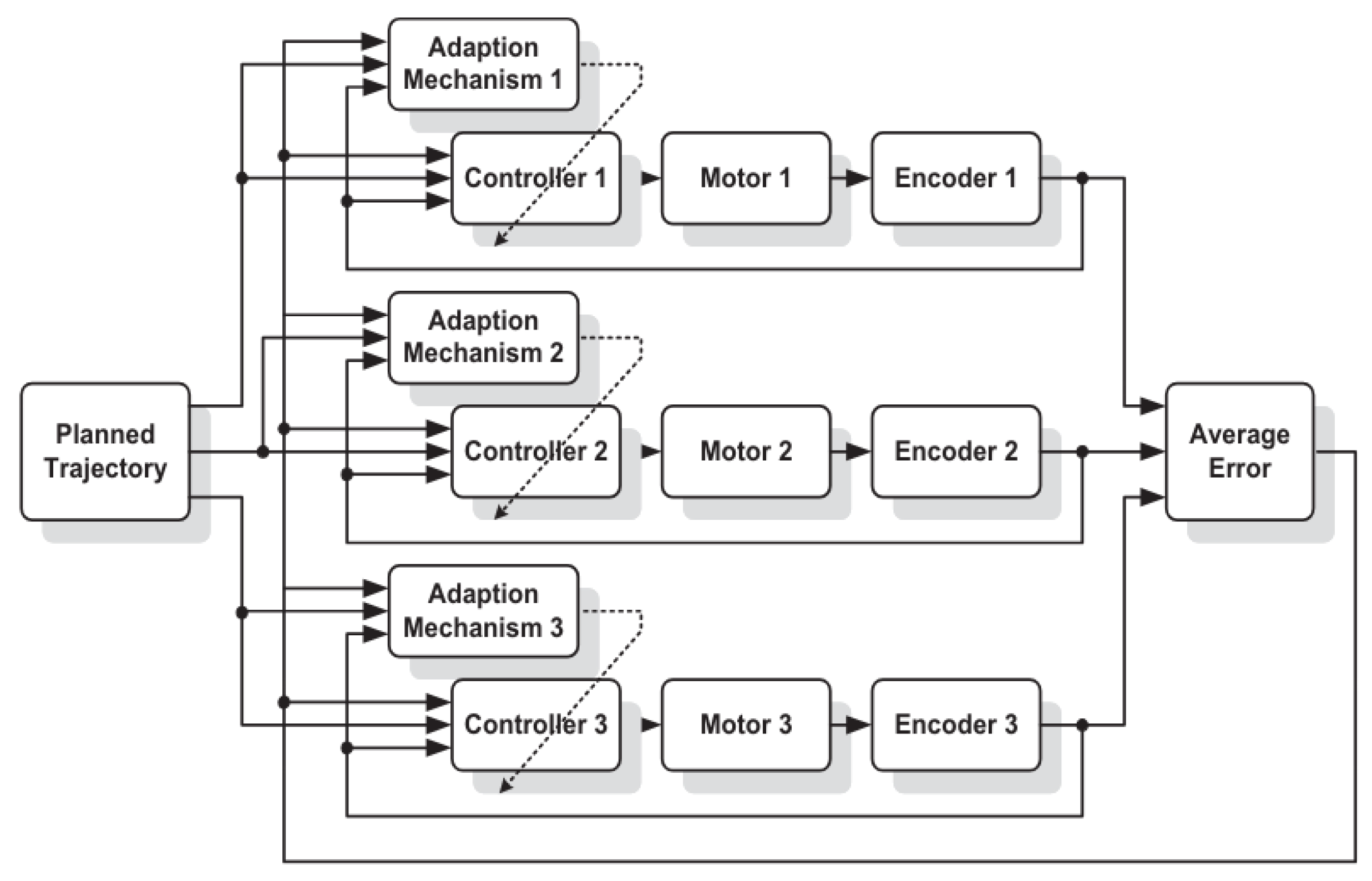
4.4. Controller Implementation Based on the Mechanism
Regarding the controllers for the robotics system used in a rehabilitation cyber-physical system, multiaxial control strategies are essential. The exoskeleton employed by the patients can exhibit significant nonlinearity due to varying inertia and stiffness based on the patient’s response. The cross-coupled dynamics among involved joints further complicates the control scheme. Additionally, different actuation components used in the exoskeletons influence the selection of controller types. To address these challenges, various types of controllers used for multiaxial systems have been proposed by researchers to adapt to different scenarios effectively.
For assistive exoskeletons and social robots, synchronizing the movements of individual joints to generate a designated motion is critical. Additionally, joint movements are interdependent due to the varying loads each joint experiences during motion execution. Depending on the complexity of the motion involved, the corresponding mechanism and control strategy can be adjusted accordingly. For example, a bionic ankle can be simplified to 2-DOFs. In this case, impedance control, combining linear controller and feedforward controller, has been proposed to compensate the 2D motion tracking of dorsiflexion and plantar flexion [
58]. For a polycentric knee exoskeleton using an electro-hydraulic actuator, a simple 1-DOF mechanism has been proposed and compensated by a sliding-mode controller to address the disturbances [
59]. For upper limb rehabilitation, the exoskeleton suit typically involves more DOFs, requiring multiaxial controllers that coordinate the overall movement of the arm. For example, linear controllers that treat movements along other axes as disturbances have been commonly adopted to simplify the complexity of controller synthesis [
60]. In addition to position feedback, force feedback is crucial for exoskeleton or robotic system to accurately follow the designated trajectories of all joints [
61]. To account for the interdependent relationship among involved joints, a multiaxial adaptive robust controller (ARC) [
62] has been proposed to compensate for the movements of both shoulder and elbow joints, addressing uncertainties caused by these movements [
26,
35]. As shown in
Figure 8, the ARC controller accounts for varying system parameters due to external disturbances and synchronization errors, enhancing tracking performance. Additionally, a robust adaptive integral terminal sliding mode control strategy has been developed to handle unknown but bounded dynamic uncertainties in the nonlinear system of upper limb exoskeletons, ensuring effective passive rehabilitation movements [
63].
Overall, while various control strategies have been proposed for exoskeleton suits used in rehabilitation, accurate dynamic models for lower and upper limbs still need to be developed. In particular, factors such as body size, age, types of motions, and recovery status require further investigation to enhance the control of exoskeletons and robotic devices on the therapist’s side. Recent developments in artificial intelligence can enhance human motion prediction, thereby improving control strategies for the multiaxial movements in both rehabilitation and daily activities [
64,
65,
66].
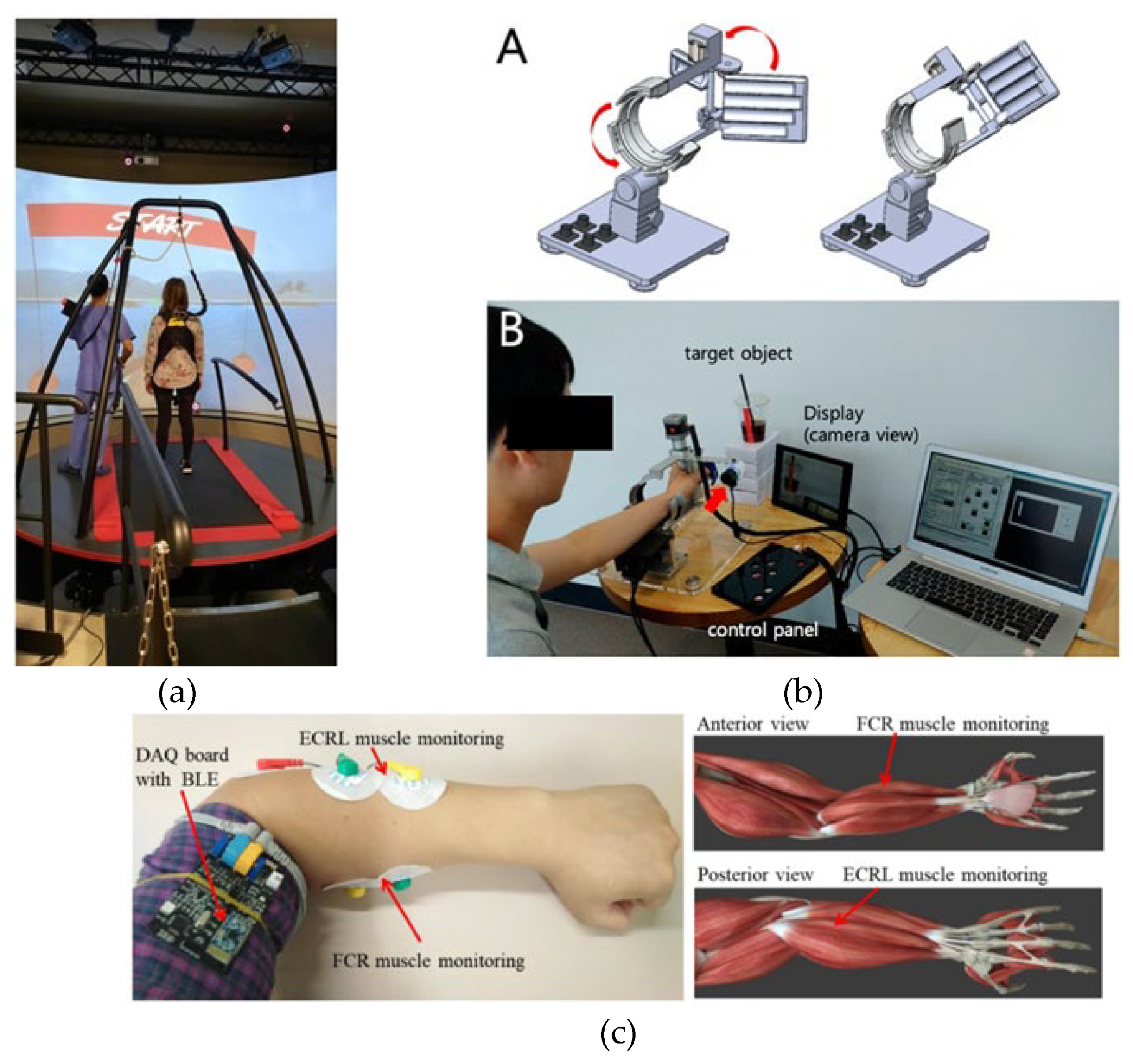
4.5. Virtual Interaction
Virtual interaction between therapists and patients in rehabilitation activities, which became feasible in the past decade, is a game-changing approach that exploits technology to enhance the rehabilitation process, making it more accessible, efficient, and tailored to individual needs. This method includes various levels of interaction, from immersive virtual reality environments and emulated interaction using robots to video/audio conferencing, providing patients with the means to communicate with their therapists without the constraints of travel.
Immersive virtual reality environments are particularly noteworthy for their ability to simulate real-world scenarios aimed at improving motor skills and cognitive functions. Within these virtual environments, therapists can possibly deliver traditional rehabilitation activities while also customizing the surroundings to suit each patient’s specific requirements [
67,
68]. Although this type of virtual interaction requires additional robotic devices to facilitate physical interactions, it can offer an experience that closely mimics on-site session. This level of customization ensures that the rehabilitation exercises are not only effective but also engaging, helping to maintain the patient’s interest and motivation, which is critical for long-term success [
69]. Moreover, the use of virtual reality enables therapists to remotely guide and monitor patients’ progress in real-time, a significant advantage of rehabilitation cyber-physical systems. By leveraging virtual reality technology, therapists can provide immediate feedback and adjustments to the patient’s exercises, enhancing the overall rehabilitation experience. This real-time interaction bridges the physical distance between therapists and patients, allowing for continuous support and guidance regardless of geographical location. By integrating technology into rehabilitation practices, virtual interaction facilitates seamless communication and collaboration between therapists and patients. It breaks down barriers to access and fosters a more personalized approach to rehabilitation, ultimately improving patient outcomes and enhancing the overall quality of care.
Figure 9 showcases various rehabilitation tools that utilize virtual reality, incorporating different types of sensors or robotic devices.
Telemedicine offers an alternative avenue for therapists to remotely engage with patients if virtual reality environments are not feasible. Through video calls and digital communication platforms, therapists can provide guidance and feedback, particularly advantageous for patients facing mobility challenges or residing in geographically remote areas. Wearable sensors and mobile apps serve as remote monitoring tools, tracking patients’ progress and vital signs in real-time and furnishing therapists with continuous data for informed treatment decisions and exercise adjustments.
The integration of cyber-physical systems in rehabilitation augments physical processes with digital control and computation, contributing not only to physical rehabilitation but also injury prevention by ensuring safe and correct movement execution. Exoskeletons within these systems offer physical support and resistance, enabling patients to execute movements beyond their individual capabilities. Data on patients’ movements collected by the system are transmitted to therapists, who can then provide real-time feedback and adjustments, bridging the gap of virtual interaction. Therapists can observe patients’ movements as they perform exercises and offer corrections or encouragement promptly, facilitating accelerated learning and movement improvement compared to traditional rehabilitation methods.
The immediate feedback loop established through virtual interaction enables therapists to personalize treatment plans based on individual patient needs, enhancing the effectiveness of rehabilitation interventions. Moreover, virtual interaction significantly enhances the accessibility of rehabilitation resources, particularly for patients in remote areas or with limited transportation access. This approach also holds promise for reducing healthcare costs by minimizing the need for frequent in-person visits. The flexibility of scheduling virtual rehabilitation sessions also allows for integration into patients’ daily routines, fostering greater adherence to the rehabilitation program.
4.6. Security and Network Connection
The demanding nature of real-time data transmission and processing in cyber-physical systems used for rehabilitation presents significant challenges, particularly regarding bandwidth and network connection requirements for the required activities. Reliability and security are the major paramount considerations, ensuring the protection of personal medical records and the delivery of high-quality rehabilitation services.
Bandwidth Requirements: cyber-physical system for rehabilitation often involves the real-time transmission of sensor data, video feeds, planned trajectories of joints, and control signals between the patient, therapist, and the cyber-physical system infrastructure. This data can be substantial, especially when considering high-resolution video streams or data from multiple sensors integrated into the system. As a result, high bandwidth is essential to ensure smooth and timely communication between all components of the system.
Latency: Low latency is critical for cyber-physical system used in rehabilitation to enable real-time interaction between the patient and the system. Any delay in data transmission or processing can impact the effectiveness of therapy sessions, particularly in scenarios where precise timing is crucial for providing feedback or adjusting therapy parameters. Therefore, network connections with minimal latency are necessary to maintain the responsiveness of the system. In cases where latency cannot be eliminated, digital lift technique may become necessary to minimize the volume of data transferred, facilitating real-time synchronization with reduced resolution. Any loss in resolution can then be compensated locally by the control unit.
Reliability: Rehabilitation cyber-physical system must operate reliably to ensure uninterrupted therapy sessions and patient safety. Network connections should be stable and resilient to fluctuations or interruptions, as even brief outages can disrupt therapy sessions and compromise patient progress. Redundancy and failover mechanisms may be implemented to mitigate the risk of network failures.
Security: Given the sensitive nature of patient data involved in rehabilitation cyber-physical system, robust security measures are essential to protect confidentiality and integrity. Secure communication protocols, data encryption, and access control mechanisms should be implemented to safeguard patient information and prevent unauthorized access or tampering.
Scalability: As the number of users and devices connected to the cyber-physical system infrastructure grows, the network must be scalable to accommodate increased demand without sacrificing performance. Scalable network architecture and provisioning strategies can help ensure that the system can support the evolving needs of rehabilitation facilities and accommodate future expansion.
Compatibility: Rehabilitation cyber-physical system may involve integration with existing healthcare IT systems, electronic health records (EHRs), and other medical devices. Compatibility with diverse hardware and software platforms is essential to facilitate seamless data exchange and interoperability across different components of the healthcare ecosystem.
Deploying cyber-physical systems for rehabilitation in both patients’ residences and medical facilities requires meticulous attention to several critical factors. In medical facilities, cyber-physical system deployment must consider the integration with existing medical equipment and systems, ensuring interoperability and minimizing disruptions to current workflows. The system should be scalable to accommodate multiple users and adaptable to various rehabilitation needs. Continuous monitoring and maintenance are essential to ensure the system’s reliability and effectiveness. In patients’ residences, the system should be user-friendly and require minimal setup to ensure ease of use. It should be designed to operate on commonly available home internet connections, with fail-safes in place to handle connectivity issues. Providing technical support and training for both patients and caregivers is crucial to ensure effective use and troubleshooting of the system.
Collaborative efforts between healthcare providers, technology vendors, network specialists, and cybersecurity experts are necessary to design and deploy robust and reliable cyber-physical system solutions for rehabilitation activities. These collaborations will help address the unique challenges of each deployment setting and ensure that the systems are tailored to meet the specific needs of both medical professionals and patients.
5. Implementation of Cyber-Physical System for Rehabilitation
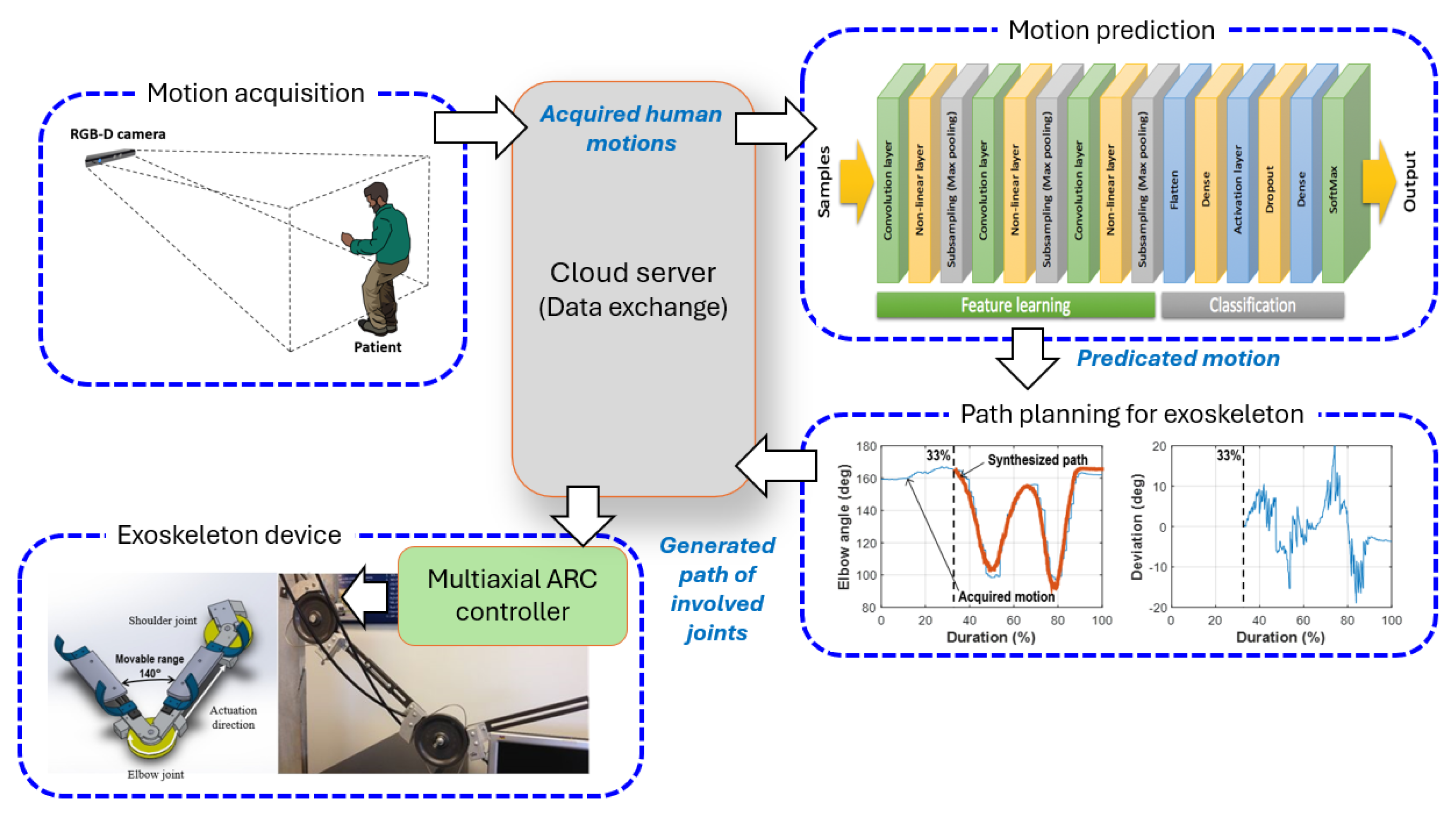
Although the technologies described in the previous sections have been developed individually, a comprehensive cyber-physical rehabilitation system has yet to be realized commercially. To validate the concept of the proposed cyber-physical rehabilitation system, several experimental systems were realized separately. These include an exoskeleton device that drives human arm motion [
26], a motion prediction model that forecasts arm movements and generates required trajectories for involved joints [
57], and a cloud-based control system that transfers the motion to a standalone server and sends the trajectories to a robotic device. Integrating these systems allows for the creation of a prototype of a cyber-physical rehabilitation system.
Figure 10 illustrates a conceptual integration of an exoskeleton system designed to mimic three human right arm motions. Communication between the system components was facilitated through the exchange of acquired information. In this integrated system, the motion acquisition was achieved using an RGB-D camera. The acquired motion information was sent to a motion prediction model to identify the type of on-going motion. The results from the motion prediction model were used to synthesize the trajectories of the involved joints. Once the trajectories were synthesized, a multiaxial controller compensated for the exoskeleton to perform the corresponding motion. This system focused on the patient’s side, and while the number of motions that the prediction model can recognize is limited, the accuracy rate is exceptionally high at over 95% for the included motions. Notably, the system can predict an on-going motion within the first 33% of the total cycle [
57]. The acquired motion data and the generated joint trajectories were exchanged via a cloud-based file server. The proposed controller effectively compensated for the disturbances caused by the synchronization of involved joints [
73]. To implement the therapist-patient interaction, a joystick type with force feedback is required to replace the parts of the motion prediction model and the path planning of joints. This allows the therapist to directly interact with and adjust the patient’s movements in real-time, enhancing the precision and effectiveness of the rehabilitation process.
A video conference service was used to test the virtual interaction in this implementation. During the testing, it was observed that the latency introduced by the video conferencing platform varied between 100 to 200 milliseconds. While this delay was within an acceptable range for general communication, it posed challenges for real-time motion synchronization and feedback in the rehabilitation process. To mitigate the impact of this latency, additional buffering and prediction algorithms need to be incorporated to ensure smoother interaction and more accurate control of the exoskeleton. This approach helped to maintain the efficacy of the virtual interaction despite the inherent delays of the video conferencing service. In addition to the communication delay, delays caused by data exchange present another significant issue in this study. Network latency and cloud drive delays can further complicate the real-time interaction required for effective rehabilitation. These delays arise from the time taken to transfer data between the local system and the cloud servers, as well as the processing time on these servers. Such latencies can affect the synchronization of motion data and the timely execution of control commands, necessitating the implementation of advanced buffering and prediction algorithms to compensate for these delays and maintain the system’s overall performance.
This prototype demonstrates the potential of integrating various technological components into a cohesive cyber-physical rehabilitation system, paving the way for future developments that could offer comprehensive, real-time, and personalized therapy solutions.
6. Conclusions
The integration of cyber-physical systems into rehabilitation offers a transformative approach that significantly enhances the quality, efficiency, and accessibility of therapeutic interventions. This paper has discussed various aspects of cyber-physical systems in rehabilitation, including the use of robotic exoskeletons, machine learning for motion prediction, and virtual reality environments. By enabling precise, high-intensity training and offering real-time feedback, these technologies support the recovery process for patients, particularly those recovering from strokes.
Key benefits of cyber-physical systems in rehabilitation include the ability to perform repetitive and consistent therapeutic exercises, which are important for motor function recovery. The incorporation of machine learning or deep learning algorithms allows for accurate motion prediction and personalized therapy plans, ensuring that exercises are both effective and engaging. Additionally, virtual reality environments create immersive scenarios that maintain patient motivation and interest, further contributing to successful rehabilitation outcomes. Despite the significant advantages, the deployment of cyber-physical systems in rehabilitation comes with challenges, particularly concerning bandwidth and network connection requirements. Ensuring reliable, low-latency, and secure communication is paramount for the effective operation of these systems. Moreover, considerations for scalability, compatibility, and data management are essential for integrating cyber-physical systems into both medical facilities and patient residences.
Future research and development should focus on addressing these challenges, enhancing the robustness of cyber-physical systems, and expanding the range of motions and therapeutic activities they can support. Collaborative efforts among healthcare providers, technology developers, and network specialists will be crucial in advancing cyber-physical systems technologies and maximizing their potential benefits for rehabilitation. In conclusion, the advancement of cyber-physical systems in rehabilitation represents a promising frontier in healthcare, offering innovative solutions that can significantly improve patient outcomes and streamline therapeutic processes. As technology continues to evolve, cyber-physical systems will undoubtedly play a pivotal role in shaping the future of rehabilitation.
Author Contributions
Conceptualization and methodology, Marvin Cheng; formal analysis, Marvin Cheng; investigation, writing—original draft preparation, Marvin Cheng; writing—review and editing, Hugo Camargo and Ezzat Bakhoum.
Funding
This research received no external funding.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors express their gratitude to Po-Lin Huang, Hao-Chun Chu, Reza Shisheie, and Lei Jiang for fabricating the individual experimental platforms.
Conflicts of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Díaz, I.; Gil, J.J.; Sánchez, E. Lower-Limb Robotic Rehabilitation: Literature Review and Challenges. J. Robot. 2011, 2011, 1–11. [CrossRef]
- Krebs, H., Dipietro, L., Levy-Tzedek, S., Fasoli, S., Rykman-Berland, A., Zipse, J., Fawcett, J., Stein, J., Poizner, H., Lo, A., Volpe, B., & Hogan, N. (2008). A paradigm shift for rehabilitation robotics: Therapeutic robots enhance clinician productivity in facilitating patient recovery. Institute of Electrical and Electronics Engineers, 27(4), 1-26. [CrossRef]
- Beckelhimer, S. C., Dalton, A. E., Richter, C. A., Hermann, V., & Page, S. J. (2011). Brief Report—Computer-based rhythm and timing training in severe, stroke-induced arm hemiparesis. American Journal of Occupational Therapy, 65, 96–100. [CrossRef]
- Linder, S.M.; Rosenfeldt, A.B.; Bay, R.C.; Sahu, K.; Wolf, S.L.; Alberts, J.L. Improving Quality of Life and Depression After Stroke Through Telerehabilitation. Am. J. Occup. Ther. 2015, 69. [CrossRef]
- Kwakkel, G., Kollen, B. J., & Krebs, H. I. (2008). Effects of robot-assisted therapy on upper limb recover after stroke: A systematic review. Neurorehabilitation and Neural Repair, 22(2), 111-121. [CrossRef]
- Riener, R.; Nef, T.; Colombo, G. Robot-aided neurorehabilitation of the upper extremities. Med Biol. Eng. Comput. 2005, 43, 2–10. [CrossRef]
- Yang, C.-L.; Lin, K.-C.; Chen, H.-C.; Wu, C.-Y.; Chen, C.-L. Pilot Comparative Study of Unilateral and Bilateral Robot-Assisted Training on Upper-Extremity Performance in Patients With Stroke. Am. J. Occup. Ther. 2012, 66, 198–206. [CrossRef]
- Klamroth-Marganska, V., Blanco, J., Campen, K., Curt, A., Dietz, V., Ettlin, T., Felder, M., Fellinghauer, B., Guidali, M., Kollmar, A., Luft, A., Nef, T., Schuster-Amft, C., Stahel, W., & Riener, R. (2014). Three-dimensional, task-specific robot therapy of the arm after stroke: A multicenter, parallel-group randomized trial. Lancet Neurology, 13, 159-66. [CrossRef]
- Maciejasz, P.; Eschweiler, J.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabilitation 2014, 11, 3–3. [CrossRef]
- Senanayake, C. and Senanayake, S.M.N.A. (2009). Emerging robotics devices for therapeutic rehabilitation of the lower extremity. In IEEE/ASME International Conference on Advanced Intelligent Mechatronics, 2009, pp. 1142-1147. [CrossRef]
- Stein, J. (2012). Robotics in rehabilitation: Technology as destiny. American Journal of Physical Medicine and Rehabilitation. 91(Suppl), 199-203. [CrossRef]
- Zinn, M.; Roth, B.; Khatib, O.; Salisbury, J.K. A New Actuation Approach for Human Friendly Robot Design. Int. J. Robot. Res. 2004, 23, 379–398. [CrossRef]
- Krebs, H.; Hogan, N. Therapeutic Robotics: A Technology Push. Proc. IEEE 2006, 94, 1727–1738. [CrossRef]
- Lo, A.C.; Guarino, P.D.; Richards, L.G.; Haselkorn, J.K.; Wittenberg, G.F.; Federman, D.G.; Ringer, R.J.; Wagner, T.H.; Krebs, H.I.; Volpe, B.T.; et al. Robot-Assisted Therapy for Long-Term Upper-Limb Impairment after Stroke. New Engl. J. Med. 2010, 362, 1772–1783. [CrossRef]
- Stevens, T.; McGinnis, R.S.; Hewgill, B.; Choquette, R.H.; Tourville, T.W.; Harvey, J.; Lachapelle, R.; Beynnon, B.D.; Toth, M.J.; Skalka, C. A Cyber-Physical System for Near Real-Time Monitoring of At-Home Orthopedic Rehabilitation and Mobile-Based Provider-Patient Communications to Improve Adherence: Development and Formative Evaluation. JMIR Hum. Factors 2020, 7, e16605. [CrossRef]
- Feng, J.; Zhu, F.; Li, P.; Davari, H.; Lee, J. Development of An Integrated Framework for Cyber-Physical System (CPS)-Enabled Rehabilitation System. Int. J. Progn. Heal. Manag. 2021, 12. [CrossRef]
- Haque, S.A.; Aziz, S.M.; Rahman, M. Review of Cyber-Physical System in Healthcare. Int. J. Distrib. Sens. Networks 2014, 10. [CrossRef]
- Qiu, H.; Qiu, M.; Liu, M.; Memmi, G. Secure Health Data Sharing for Medical Cyber-Physical Systems for the Healthcare 4.0. IEEE J. Biomed. Heal. Informatics 2020, 24, 2499–2505. [CrossRef]
- Cheng, M. H., Huang, P. L., Chu, H. C., Peng, L. H., & Bakhoum, E. (2018, November). Virtual interaction between patients and occupational therapists using an assistive robotic device with cyber-physical system. In ASME International Mechanical Engineering Congress and Exposition (Vol. 52026, p. V003T04A074). American Society of Mechanical Engineers. [CrossRef]
- Buccelli, S.; Tessari, F.; Fanin, F.; De Guglielmo, L.; Capitta, G.; Piezzo, C.; Bruschi, A.; Van Son, F.; Scarpetta, S.; Succi, A.; et al. A Gravity-Compensated Upper-Limb Exoskeleton for Functional Rehabilitation of the Shoulder Complex. Appl. Sci. 2022, 12, 3364. [CrossRef]
- Xinyi, Z., Haoping, W., Yang, T., Zefeng, W., & Laurent, P. (2015, July). Modeling, simulation & control of human lower extremity exoskeleton. In 2015 34th Chinese Control Conference (CCC) (pp. 6066-6071). IEEE. [CrossRef]
- Esquenazi, A.; Talaty, M.; Packel, A.P.; Saulino, M. The ReWalk Powered Exoskeleton to Restore Ambulatory Function to Individuals with Thoracic-Level Motor-Complete Spinal Cord Injury. Am. J. Phys. Med. Rehabilitation 2012, 91, 911–921. [CrossRef]
- Talaty, M., Esquenazi, A., & Briceno, J. E. (2013, June). Differentiating ability in users of the ReWalk TM powered exoskeleton: An analysis of walking kinematics. In 2013 IEEE 13th international conference on rehabilitation robotics (ICORR) (pp. 1-5). IEEE. [CrossRef]
- Azocar, A.F.; Mooney, L.M.; Duval, J.-F.; Simon, A.M.; Hargrove, L.J.; Rouse, E.J. Design and clinical implementation of an open-source bionic leg. Nat. Biomed. Eng. 2020, 4, 941–953. [CrossRef]
- Awad, L.N.; Esquenazi, A.; Francisco, G.E.; Nolan, K.J.; Jayaraman, A. The ReWalk ReStore™ soft robotic exosuit: a multi-site clinical trial of the safety, reliability, and feasibility of exosuit-augmented post-stroke gait rehabilitation. J. Neuroeng. Rehabilitation 2020, 17, 80. [CrossRef]
- Cheng, M. H., Jiang, L., Mou, Q., Wheeler, S., Banta, L., Shisheie, R., & Bakhoum, E. (2016, July). Design, fabrication, and control of twisted actuated robotic device. In 2016 American Control Conference (ACC) (pp. 1215-1220). IEEE. [CrossRef]
- Calderita, L.V.; Manso, L.J.; Bustos, P.; Suárez-Mejías, C.; Fernández, F.; Bandera, A. THERAPIST: Towards an Autonomous Socially Interactive Robot for Motor and Neurorehabilitation Therapies for Children. JMIR Rehabilitation Assist. Technol. 2014, 1, e1. [CrossRef]
- Song, A.; Wu, C.; Ni, D.; Li, H.; Qin, H. One-Therapist to Three-Patient Telerehabilitation Robot System for the Upper Limb after Stroke. Int. J. Soc. Robot. 2016, 8, 319–329. [CrossRef]
- Wang, P.; Li, W.; Ogunbona, P.; Wan, J.; Escalera, S. RGB-D-based human motion recognition with deep learning: A survey. Comput. Vis. Image Underst. 2018, 171, 118–139. [CrossRef]
- Faria, D. R., Premebida, C., & Nunes, U. (2014, August). A probabilistic approach for human everyday activities recognition using body motion from RGB-D images. In The 23rd IEEE international symposium on robot and human interactive communication (pp. 732-737). IEEE. [CrossRef]
- von Marcard, T.; Pons-Moll, G.; Rosenhahn, B. Human Pose Estimation from Video and IMUs. IEEE Trans. Pattern Anal. Mach. Intell. 2016, 38, 1533–1547. [CrossRef]
- Ribeiro, P.M.S.; Matos, A.C.; Santos, P.H.; Cardoso, J.S. Machine Learning Improvements to Human Motion Tracking with IMUs. Sensors 2020, 20, 6383. [CrossRef]
- Guidolin, M., Petrea, R. A. B., Roberto, O., Reggiani, M., Menegatti, E., & Tagliapietra, L. (2021, March). On the accuracy of imus for human motion tracking: A comparative evaluation. In 2021 IEEE International Conference on Mechatronics (ICM) (pp. 1-6). IEEE. [CrossRef]
- Tsilomitrou, O.; Gkountas, K.; Evangeliou, N.; Dermatas, E. Wireless Motion Capture System for Upper Limb Rehabilitation. Appl. Syst. Innov. 2021, 4, 14. [CrossRef]
- Cheng, M., & Bakhoum, E. (2021, November). Tracking Control Design and Implementation of Multiaxial Controller for Social Robotic Devices. In ASME International Mechanical Engineering Congress and Exposition (Vol. 85611, p. V07AT07A025). American Society of Mechanical Engineers. [CrossRef]
- Rathore, A., Wilcox, M., Ramirez, D. Z. M., Loureiro, R., & Carlson, T. (2016, August). Quantifying the human-robot interaction forces between a lower limb exoskeleton and healthy users. In 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC) (pp. 586-589). IEEE. [CrossRef]
- Chen, B.; Zi, B.; Wang, Z.; Qin, L.; Liao, W.-H. Knee exoskeletons for gait rehabilitation and human performance augmentation: A state-of-the-art. Mech. Mach. Theory 2019, 134, 499–511. (https://www.sciencedirect.com/science/article/abs/pii/S0094114X1831992X). [CrossRef]
- Ye, M.; Yang, C.; Stankovic, V.; Stankovic, L.; Kerr, A. A Depth Camera Motion Analysis Framework for Tele-rehabilitation: Motion Capture and Person-Centric Kinematics Analysis. IEEE J. Sel. Top. Signal Process. 2016, 10, 877–887. [CrossRef]
- Xu, Y.; Tong, M.; Ming, W.-K.; Lin, Y.; Mai, W.; Huang, W.; Chen, Z. A Depth Camera–Based, Task-Specific Virtual Reality Rehabilitation Game for Patients With Stroke: Pilot Usability Study. JMIR Serious Games 2021, 9, e20916. [CrossRef]
- Rodrigues, T.B.; Salgado, D.P.; Catháin, C..; O’connor, N.; Murray, N. Human gait assessment using a 3D marker-less multimodal motion capture system. Multimedia Tools Appl. 2019, 79, 2629–2651. [CrossRef]
- Yin, Y.H.; Fan, Y.J.; Xu, L.D. EMG and EPP-Integrated Human–Machine Interface Between the Paralyzed and Rehabilitation Exoskeleton. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 542–549. [CrossRef]
- Bi, L.; Feleke, A.-.-G.; Guan, C. A review on EMG-based motor intention prediction of continuous human upper limb motion for human-robot collaboration. Biomed. Signal Process. Control. 2019, 51, 113–127. [CrossRef]
- Kim, H.; Miller, L.M.; Fedulow, I.; Simkins, M.; Abrams, G.M.; Byl, N.; Rosen, J. Kinematic Data Analysis for Post-Stroke Patients Following Bilateral Versus Unilateral Rehabilitation With an Upper Limb Wearable Robotic System. IEEE Trans. Neural Syst. Rehabilitation Eng. 2012, 21, 153–164. [CrossRef]
- Tognetti, A.; Lorussi, F.; Bartalesi, R.; Quaglini, S.; Tesconi, M.; Zupone, G.; De Rossi, D. Wearable kinesthetic system for capturing and classifying upper limb gesture in post-stroke rehabilitation. J. Neuroeng. Rehabilitation 2005, 2, 8–8. [CrossRef]
- Zhou, H.; Hu, H. Human motion tracking for rehabilitation—A survey. Biomed. Signal Process. Control. 2008, 3, 1–18. [CrossRef]
- VICON. (n.d.). A simple motion capture system delivering powerful results. Retrieved from https://www.vicon.com/resources/case-studies/a-simple-motion-capture-system-delivering-powerful-results/.
- Sasiadek, J. Sensor fusion. Annu. Rev. Control. 2002, 26, 203–228. [CrossRef]
- Zhao, H.; Wang, Z. Motion Measurement Using Inertial Sensors, Ultrasonic Sensors, and Magnetometers With Extended Kalman Filter for Data Fusion. IEEE Sensors J. 2011, 12, 943–953. [CrossRef]
- Rigatos, G.G. Extended Kalman and Particle Filtering for sensor fusion in motion control of mobile robots. Math. Comput. Simul. 2010, 81, 590–607. [CrossRef]
- Yuan, J.; Chen, H.; Sun, F.; Huang, Y. Multisensor Information Fusion for People Tracking With a Mobile Robot: A Particle Filtering Approach. IEEE Trans. Instrum. Meas. 2015, 64, 2427–2442. [CrossRef]
- Fourati, H. Heterogeneous Data Fusion Algorithm for Pedestrian Navigation via Foot-Mounted Inertial Measurement Unit and Complementary Filter. IEEE Trans. Instrum. Meas. 2014, 64, 221–229. [CrossRef]
- Sidenbladh, H. (2004, August). Detecting human motion with support vector machines. In Proceedings of the 17th International Conference on Pattern Recognition, 2004. ICPR 2004. (Vol. 2, pp. 188-191). IEEE. [CrossRef]
- Wang, P., Zhang, Y., & Jiang, W. (2021, June). Application of K-Nearest neighbor (knn) algorithm for human action recognition. In 2021 IEEE 4th Advanced Information Management, Communicates, Electronic and Automation Control Conference (IMCEC) (Vol. 4, pp. 492-496). IEEE. [CrossRef]
- Tu, Z.; Xie, W.; Qin, Q.; Poppe, R.; Veltkamp, R.C.; Li, B.; Yuan, J. Multi-stream CNN: Learning representations based on human-related regions for action recognition. Pattern Recognit. 2018, 79, 32–43. [CrossRef]
- Martinez, J., Black, M. J., & Romero, J. (2017). On human motion prediction using recurrent neural networks. In Proceedings of the IEEE conference on computer vision and pattern recognition (pp. 2891-2900). [CrossRef]
- Majd, M.; Safabakhsh, R. Correlational Convolutional LSTM for human action recognition. Neurocomputing 2020, 396, 224–229. [CrossRef]
- Cheng, M. H., Huang, P. L., Chu, H. C., & McKenzie Jr, E. A. (2019, November). Motion Estimation and Path Planning for Assistive Robotic Devices. In ASME International Mechanical Engineering Congress and Exposition (Vol. 59407, p. V003T04A073). American Society of Mechanical Engineers. [CrossRef]
- Zhao, S.; Liang, W.; Wang, K.; Ren, L.; Qian, Z.; Chen, G.; Lu, X.; Zhao, D.; Wang, X.; Ren, L. A Multiaxial Bionic Ankle Based on Series Elastic Actuation With a Parallel Spring. IEEE Trans. Ind. Electron. 2023, 71, 7498–7510. [CrossRef]
- Lee, T.; Lee, D.; Song, B.; Baek, Y.S. Design and Control of a Polycentric Knee Exoskeleton Using an Electro-Hydraulic Actuator. Sensors 2019, 20, 211. [CrossRef]
- González-Mendoza, A.; Quiñones-Urióstegui, I.; Salazar-Cruz, S.; Perez-Sanpablo, A.-I.; López-Gutiérrez, R.; Lozano, R. Design and Implementation of a Rehabilitation Upper-limb Exoskeleton Robot Controlled by Cognitive and Physical Interfaces. J. Bionic Eng. 2022, 19, 1374–1391. [CrossRef]
- Frisoli, A.; Salsedo, F.; Bergamasco, M.; Rossi, B.; Carboncini, M.C. A force-feedback exoskeleton for upper-limb rehabilitation in virtual reality. Appl. Bionics Biomech. 2009, 6, 115–126. [CrossRef]
- Cheng, M.H.; Li, Y.J.; Bakhoum, E.G. Controller Synthesis of Tracking and Synchronization for Multiaxis Motion System. IEEE Trans. Control. Syst. Technol. 2013, 22, 378–386. [CrossRef]
- Riani, A.; Madani, T.; Benallegue, A.; Djouani, K. Adaptive integral terminal sliding mode control for upper-limb rehabilitation exoskeleton. Control. Eng. Pr. 2018, 75, 108–117. [CrossRef]
- Xiong, D.; Zhang, D.; Zhao, X.; Zhao, Y. Deep Learning for EMG-based Human-Machine Interaction: A Review. Ieee/caa J. Autom. Sin. 2021, 8, 512–533. [CrossRef]
- Wan, S.; Qi, L.; Xu, X.; Tong, C.; Gu, Z. Deep Learning Models for Real-time Human Activity Recognition with Smartphones. Mob. Networks Appl. 2019, 25, 743–755. [CrossRef]
- Su, H.; Qi, W.; Li, Z.; Chen, Z.; Ferrigno, G.; De Momi, E. Deep Neural Network Approach in EMG-Based Force Estimation for Human–Robot Interaction. IEEE Trans. Artif. Intell. 2021, 2, 404–412. [CrossRef]
- Powell, M. O., Elor, A., Teodorescu, M., & Kurniawan, S. (2020). Openbutterfly: Multimodal rehabilitation analysis of immersive virtual reality for physical therapy. American Journal of Sports Science and Medicine, 8(1), 23-35. http://article.scisportsscience.com/pdf/ajssm-8-1-5.pdf.
- Chatterjee, K.; Buchanan, A.; Cottrell, K.; Hughes, S.; Day, T.W.; John, N.W. Immersive Virtual Reality for the Cognitive Rehabilitation of Stroke Survivors. IEEE Trans. Neural Syst. Rehabilitation Eng. 2022, 30, 719–728. [CrossRef]
- Herrera, V.; Vallejo, D.; Castro-Schez, J.J.; Monekosso, D.N.; Reyes, A.d.L.; Glez-Morcillo, C.; Albusac, J. Rehab-Immersive: A framework to support the development of virtual reality applications in upper limb rehabilitation. SoftwareX 2023, 23. [CrossRef]
- Cellini, R.; Paladina, G.; Mascaro, G.; Lembo, M.A.; Facciale, A.L.; Ferrera, M.C.; Fonti, B.; Pergolizzi, L.; Buonasera, P.; Bramanti, P.; et al. Effect of Immersive Virtual Reality by a Computer Assisted Rehabilitation Environment (CAREN) in Juvenile Huntington’s Disease: A Case Report. Medicina 2022, 58, 919. [CrossRef]
- Nam, H.S.; Hong, N.; Cho, M.; Lee, C.; Seo, H.G.; Kim, S. Vision-Assisted Interactive Human-in-the-Loop Distal Upper Limb Rehabilitation Robot and its Clinical Usability Test. Appl. Sci. 2019, 9, 3106. [CrossRef]
- Zhao, S.; Liu, J.; Gong, Z.; Lei, Y.; OuYang, X.; Chan, C.C.; Ruan, S. Wearable Physiological Monitoring System Based on Electrocardiography and Electromyography for Upper Limb Rehabilitation Training. Sensors 2020, 20, 4861. [CrossRef]
- Jiang, L., Shisheie, R., Cheng, M. H., & Bakhoum, E. (2015). Controller synthesis for assistive robotic device using twisted-string actuation. In 2015 American Control Conference (pp. 2248-2253). Chicago, IL, July 1 – 3, 2015. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).