Submitted:
09 September 2024
Posted:
10 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Review of the Literature
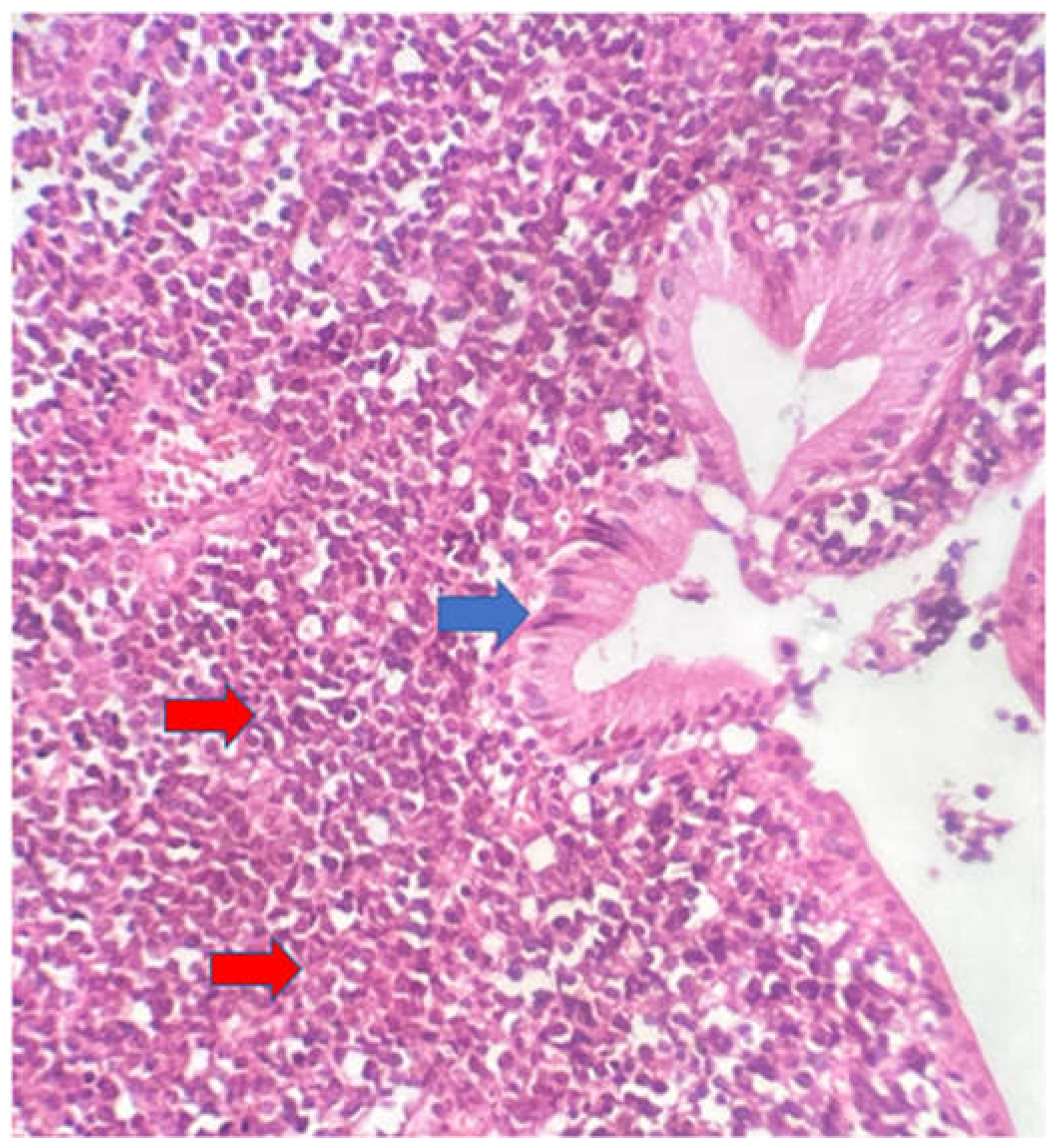
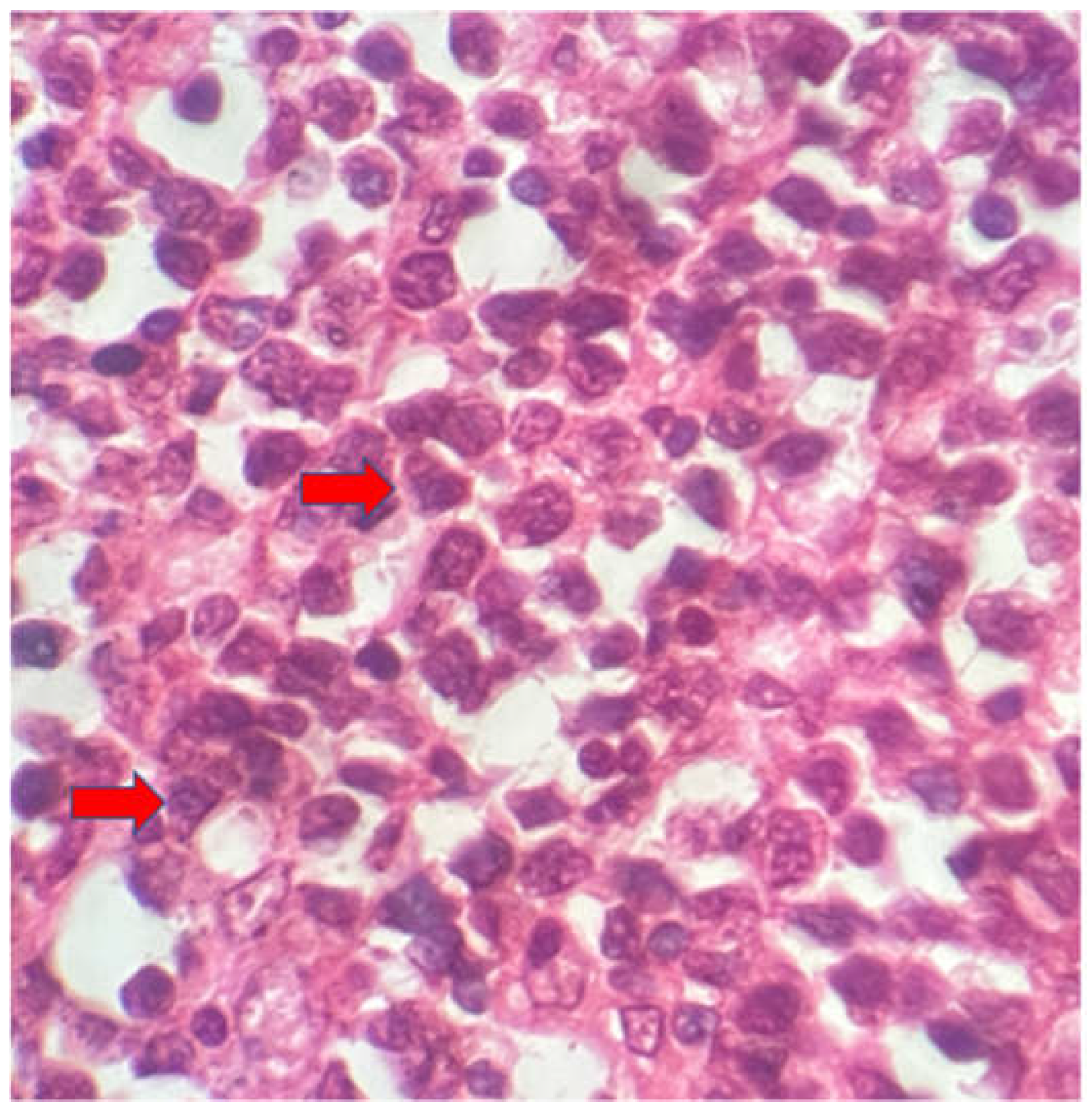
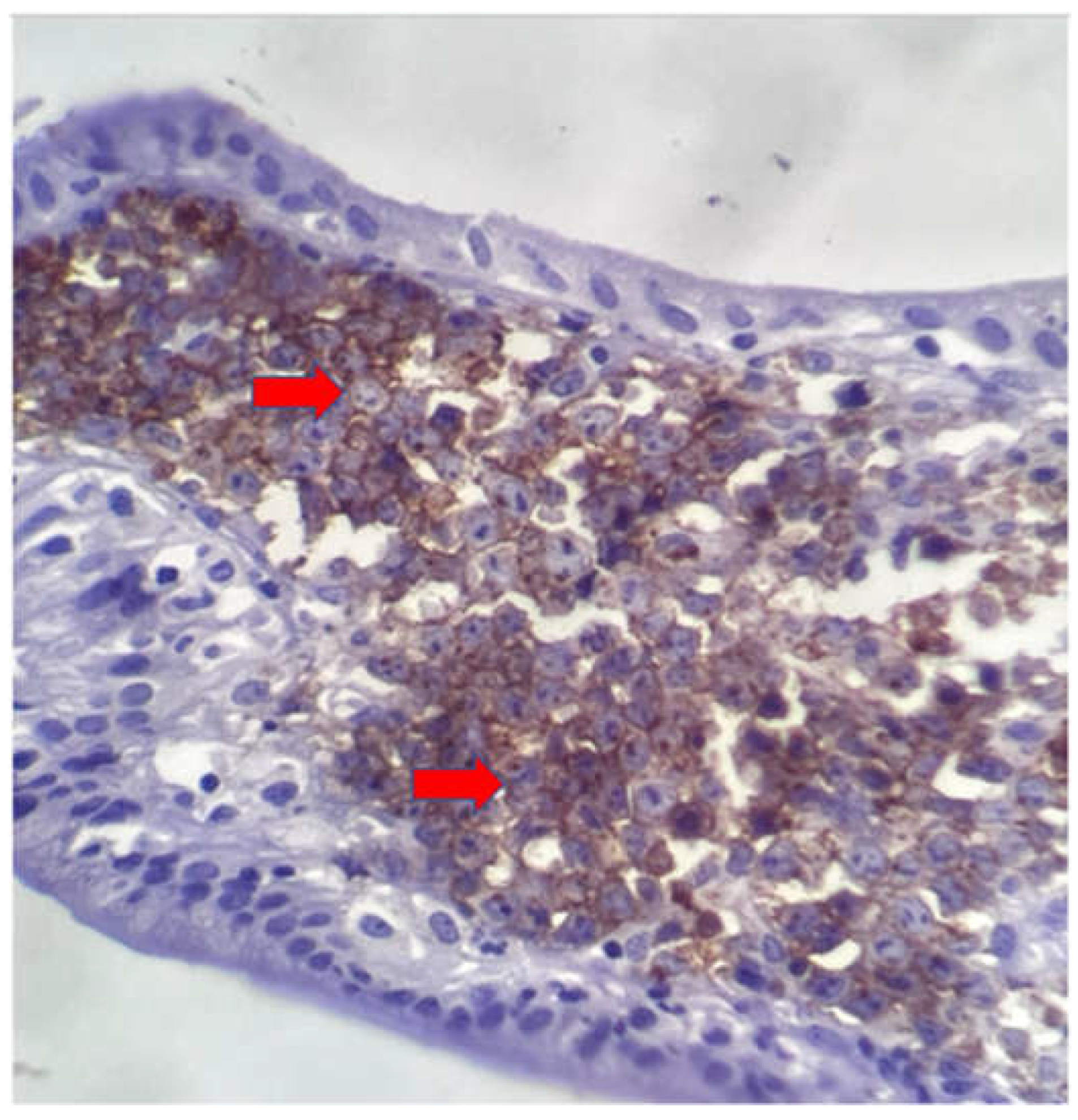
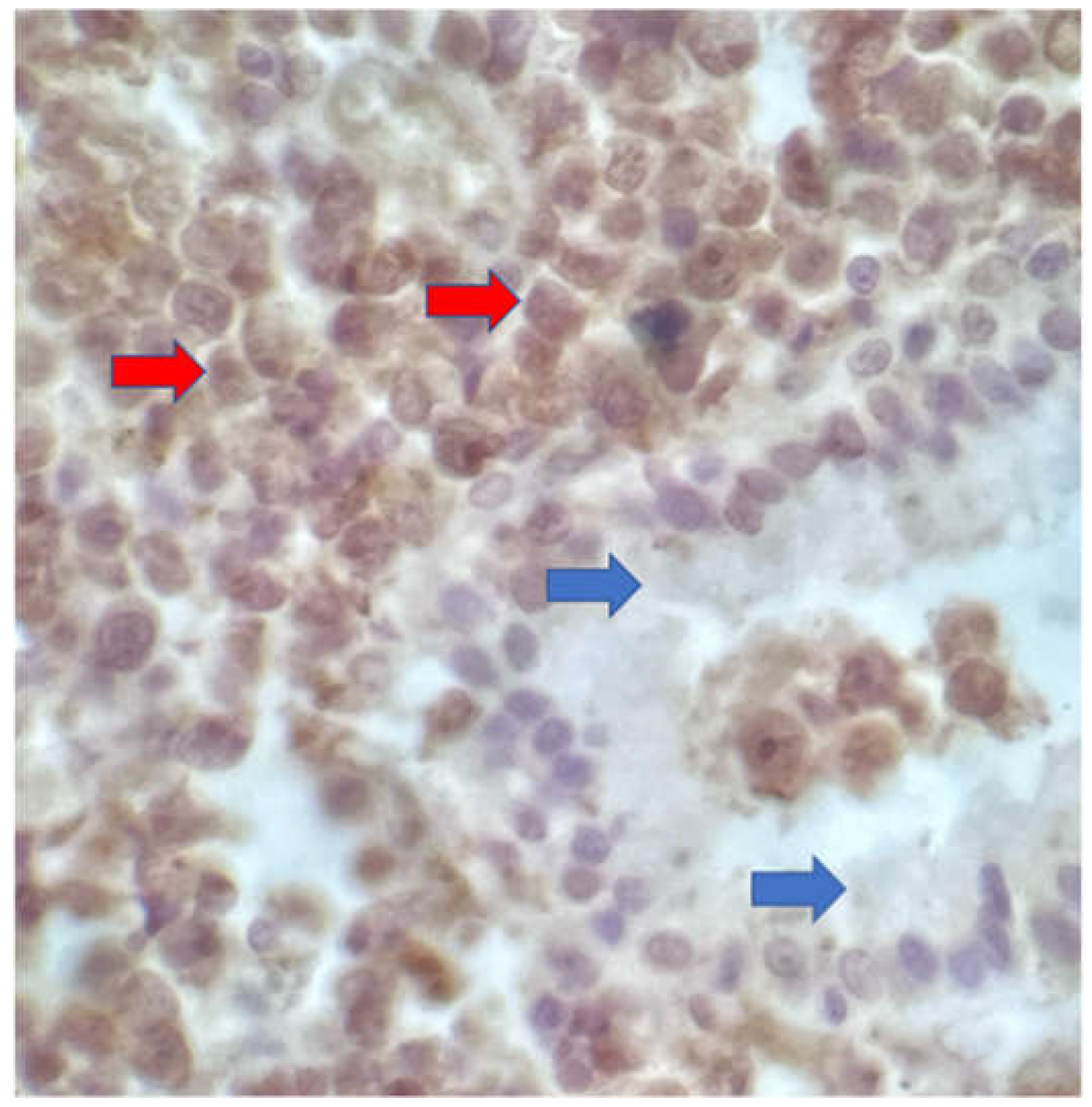
3. Case Description
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hosoda, K.; et al. Gallbladder Burkitt’s lymphoma mimicking gallbladder cancer: A case report. World J Gastroenterol 2022, 28, 675. [Google Scholar] [CrossRef]
- Yasuma, T.; Yanana, M. Primary sarcoma of the gallbladder--report of three cases. Acta Pathol Jpn 1971, 28, 285–304. [Google Scholar] [CrossRef]
- Jelic, T.M.; et al. Primary, extranodal, follicular non-Hodgkin lymphoma of the gallbladder: case report and a review of the literature. Leuk Lymphoma 2004, 45, 381–387. [Google Scholar] [CrossRef]
- Ono, A.; et al. Primary malignant lymphoma of the gallbladder: a case report and literature review. Br J Radiol 2009, 82, e15–e19. [Google Scholar] [CrossRef]
- Ayub, A.; et al. Primary non-Hodgkin's lymphoma of the gallbladder: A population-based analysis. Anticancer Res. 2017, 37, 2581–2586. [Google Scholar] [CrossRef]
- Mani, H.; et al. Gall bladder and extrahepatic bile duct lymphomas: clinicopathological observations and biological implications. Am J Surg Pathol. 2010, 34, 1277–1286. [Google Scholar] [CrossRef]
- Doherty, B.; Palmer, W.; Cvinar, J.; Sadek, N. A Rare Case of Systemic Adult Burkitt Lymphoma Presenting as Acute Acalculous Cholecystitis. ACG Case Rep J 2019, 6, e00048. [Google Scholar] [CrossRef]
- Repine, T.B.; DeArmond, G.; López, J.D. Unusual sites of metastatic malignancy: Case 2. Burkitt's lymphoma involving the gallbladder. J Clin Oncol. 2004, 22, 5014–5015. [Google Scholar] [CrossRef]
- Balonga, C.; et al. Burkitt's lymphoma: Unusual localization. Rev Esp Enf Digest. 1996, 88, 439–441. [Google Scholar]
- Centers for Disease Control and Prevention. Revised classification system for human immunodeficiency virus infection in children less than 13 years of age. MMWR Morb Mortal Wkly Rep. 1994, 43, 1–10. Available online: https://www.sandiegocounty.gov/content/dam/sdc/hhsa/programs/phs/documents/rr4312.pdf (accessed on 11 May 2024).
- Brasil, Ministério da Saúde, Coordenação Geral de Vigilância do HIV/AIDS e Hepatites Virais - CGAHV/DATHI/SVSA/MS. Protocolo Clínico e Diretrizes Terapêuticas para Manejo da Infecção Pelo HIV em Crianças e Adolescentes: Módulos 1 e 2. 2023. Available online: https://portaldeboaspraticas.iff.fiocruz.br/atencao-recem-nascido/pcdt-para-manejo-da-infeccao-pelo-hiv-em-criancas-e-adolescentes/ (accessed on 11 May 2024).
- Khoury, J.D.; et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: Myeloid and histiocytic/dendritic neoplasms. Leukemia 2022, 36, 1703–1719. [Google Scholar] [CrossRef]
- Gulley, M.L.; et al. Guidelines for interpreting EBER in situ hybridization and LMP1 immunohistochemical tests for detecting Epstein-Barr virus in Hodgkin lymphoma. Am J Clin Pathol. 2002, 117, 259–267. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases, 11th edition (ICD 11). Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 11 May 2024).
- Murphy, S.B. Classification, staging and end results of treatment of childhood non-Hodgkin’s lymphomas: Dissimilarities from lymphomas in adults. Semin. Oncol. 1980, 7, 332–339. [Google Scholar]
- Canellos, G.P.; et al. The m-BACOD combination chemotherapy regimen in the treatment of diffuse large cell lymphoma. In: Seminars in Hematology. Semin Hematol. 1987, 24, 2–7. [Google Scholar]
- Reiter, A.; et al. Non-Hodgkin's lymphomas of childhood and adolescence: results of a treatment stratified for biologic subtypes and stage--a report of the Berlin-Frankfurt-Münster Group. J Clin Oncol. 1995, 13, 359–372. [Google Scholar] [CrossRef]
- Brasil, Ministério da Saúde, Coordenação Nacional de DST e AIDS. Guia de tratamento clínico da infecção pelo HIV em crianças. 2001. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/073_03Guia_tratamento.pdf (accessed on 11 May 2024).
- Crombie, J.; LaCasce, A. The treatment of Burkitt lymphoma in adults. Blood. 2021, 11, 743–750. [Google Scholar] [CrossRef]
- Carbone, A.; Vaccher, E.; Gloghini, A. Hematologic cancers in individuals infected by HIV. Blood 2022, 139, 995–1012. [Google Scholar] [CrossRef]
- Dawson, I.M.; Cornes, J.S.; Morson, B.C. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961, 80–89. [Google Scholar] [CrossRef]
- Lewin, K.J.; Ranchod, M.; Dorfman, R.F. Lymphomas of the gastrointestinal tract. A study of 117 cases presenting with gastrointestinal disease. Cancer 1978, 42, 673–707. [Google Scholar] [CrossRef]
- Lin, Y.; et al. Clinical presentation of gastric Burkitt lymphoma presenting with paraplegia and acute pancreatitis: A case report. World J Gastroenterol. 2021, 27, 7844–7854. [Google Scholar] [CrossRef]
- Biggar, R.J.; Frisch, M.; Goedert, J.J. Risk of cancer in children with AIDS. JAMA 2000, 284, 205–209. [Google Scholar] [CrossRef]
- Caselli, D.; Klersy, C.; de Martino, M.; Gabiano, C.; Galli, L.; Tovo, P.; Aricò, M.; Italian register for HIV infection in children. Human immunodeficiency virus–related cancer in children: Incidence and treatment outcome—Report of the Italian register. J. Clin. Oncol. 2000, 18, 3854–3861. [Google Scholar] [CrossRef]
- Chiappini, E.; et al. Pediatric human immunodeficiency virus infection and cancer in the highly active antiretroviral treatment (HAART) era. Cancer Lett. 2014, 347, 38–45. [Google Scholar] [CrossRef]
- Simard, E.P.; Shiels, M.S.; Bhatia, K.; Engels, E.A. Long-term cancer risk among people diagnosed with AIDS during childhood. Cancer Epidemiol Biomarkers Prev. 2012, 21, 148–154. [Google Scholar] [CrossRef]
- Pollock, B.H.; et al. Risk factors for pediatric human immunodeficiency virus–related malignancy. JAMA 2003, 289, 2393–2399. [Google Scholar] [CrossRef]
- Zicari, S.; et al. Immune activation, inflammation, and non-AIDS co-morbidities in HIV-infected patients under long-term ART. Viruses 2019, 11, 200. [Google Scholar] [CrossRef]
- Shindiapina, P.; et al. Immunology of EBV-related lymphoproliferative disease in HIV-positive individuals. Front. Oncol. 2020, 10, 1723. [Google Scholar] [CrossRef]
- Verdu-Bou, M.; et al. Clinical and Therapeutic Implications of Epstein–Barr Virus in HIV-Related Lymphomas. Cancers (Basel). 2021, 13, 5534. [Google Scholar] [CrossRef]
- Hatano, Y.; et al. Virus-driven carcinogenesis. Cancers (Basel). 2021, 13, 2625. [Google Scholar] [CrossRef]
- Gougeon, M.; Montagnier, L. Programmed Cell Death as a Mechanism of CD4 and CD8 T Cell Deletion in AIDS: Molecular Control and Effect of Highly Active Antiretroviral Therapy. Ann N. Y. Acad. Sci. 1999, 887, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Chanock, S.J.; Pizzo, P.A. Infection prevention strategies for children with cancer and AIDS: Contrasting dilemmas. J. Hosp. Infect. 1995, 30, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Geel, J.A.; et al. Prognostic factors affecting survival in children and adolescents with HIV and Hodgkin lymphoma in South Africa. Leuk Lymphoma 2021, 62, 2854–2863. [Google Scholar] [CrossRef] [PubMed]
- Chiappini, E.; et al. Cancer rates after year 2000 significantly decrease in children with perinatal HIV infection: A study by the Italian Register for HIV Infection in Children. J Clin Oncol. 2007, 25, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Orem, J.; et al. Clinical characteristics, treatment and outcome of childhood Burkitt’s lymphoma at the Uganda Cancer Institute. Trans R Soc Trop Med Hyg. 2011, 105, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Stefan, D.C.; Stones, D.; Newton, R. Burkitt lymphoma in South African children: One or two entities? Transfus Apher Sci. 2011, 44, 191–194. [Google Scholar] [CrossRef]
- Abrahão, R.; et al. Chronic medical conditions and late effects following non-Hodgkin lymphoma in HIV-uninfected and HIV-infected adolescents and young adults: A population-based study. Br J Haematol. 2020, 190, 371–384. [Google Scholar] [CrossRef]
- Singh, E.; et al. , J. HIV-associated malignancies in children. Curr Opin HIV AIDS 2017, 12, 77. [Google Scholar] [CrossRef]
- Katumba, R.G.; et al. Cancer in Youth Living With HIV (YLWHIV): A Narrative Review of the Access to Oncological Services Among YLWHIV and the Role of Economic Strengthening in Child Health. Front Public Health 2020, 8, 409. [Google Scholar] [CrossRef]
- Duarte, N.L.; et al. Incidence and Clinical Description of Lymphomas in Children and Adolescents with Vertical Transmission of HIV in Rio de Janeiro, Brazil, in Pre-and Post-Combined Antiretroviral Therapy Eras: A Multicentric Hospital-Based Survival Analysis Study. Cancers (Basel). 2022, 14, 6129. [Google Scholar] [CrossRef]
- Duarte, N.L.; et al. Prognostic Factors in Children and Adolescents with Lymphomas and Vertical Transmission of HIV in Rio de Janeiro, Brazil: A Multicentric Hospital-Based Survival Analysis Study. Cancers (Basel). 2023, 15, 2292. [Google Scholar] [CrossRef]
- Chiappini, E.; et al. Real-world analysis of survival and clinical events in a cohort of Italian perinatally HIV-1 infected children from 2001 to 2018. Front Pediatr. 2021, 9, 665764. [Google Scholar] [CrossRef]
- de Martino, M.; et al. Reduction in mortality with availability of antiretroviral therapy for children with perinatal HIV-1 infection. JAMA 2000, 284, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Álvaro-Meca, A.; et al. Epidemiologic trends of cancer diagnoses among HIV-infected children in Spain from 1997 to 2008. Pediatr. Infect. Dis. J. 2011, 30, 764–768. [Google Scholar] [CrossRef]
- Carrasco, I.; et al. Innate and adaptive abnormalities in youth with vertically acquired HIV through a multicentre cohort in Spain. J. Int. AIDS Soc. 2021, 24, e25804. [Google Scholar] [CrossRef]
- Chhabra, S.; et al. Malignancy and all-cause mortality; incidence in adolescents and young adults living with perinatally acquired HIV. J. Virus Erad. 2020, 6, 30–33. [Google Scholar] [CrossRef] [PubMed]
- Kato, H.; et al. Primary non-Hodgkin’s lymphoma of the gallbladder diagnosed by laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2008, 15, 659–663. [Google Scholar] [CrossRef]
- Gupta, P.; et al. Imaging-based algorithmic approach to gallbladder wall thickening. World J Gastroenterology 2020, 26, 6163–6181. [Google Scholar] [CrossRef] [PubMed]
- Gascoyne, R.D. Establishing the diagnosis of lymphoma: from initial biopsy to clinical staging. Oncology (Williston Park) 1998, 12, 11–16. [Google Scholar]
- Carbone, A.; et al. HIV-associated Hodgkin lymphoma. Curr Opin HIV AIDS. 2009, 4, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Carbone, A.; Gloghini, A. AIDS-related lymphomas: from pathogenesis to pathology. Br J Haematol. 2005, 130, 662–670. [Google Scholar] [CrossRef]
- Cesarman, E. Gammaherpesvirus and lymphoproliferative disorders in immunocompromised patients. Cancer Lett. 2011, 305, 163–174. [Google Scholar] [CrossRef]
- Hijlkema, S.H.; et al. A longitudinal and cross-sectional study of Epstein-Barr virus DNA load: a possible predictor of AIDS-related lymphoma in HIV-infected patients. Infect Dis (Lond). 2018, 50, 847–852. [Google Scholar] [CrossRef] [PubMed]
- Gloghini, A.; Dolcetti, R.; Carbone, A. Lymphomas occurring specifically in HIV-infected patients: from pathogenesis to pathology. Semin Cancer Biol. 2013, 23, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Shindiapina, P.; et al. Immunology of EBV-related lymphoproliferative disease in HIV-positive individuals. Front Oncol. 2020, 30, 1723. [Google Scholar] [CrossRef] [PubMed]
- Verdu-Bou, M.; et al. Clinical and therapeutic implications of Epstein–Barr virus in HIV-related lymphomas. Cancers (Basel). 2021; 5534, 13. [Google Scholar] [CrossRef]
- Westmoreland, K.D.; et al. Hodgkin lymphoma, HIV, and Epstein–Barr virus in Malawi: Longitudinal results from the Kamuzu Central Hospital lymphoma study. Pediatr. Blood Cancer 2017, 64, e26302. [Google Scholar] [CrossRef]
- Newton, R.; et al. A case-control study of human immunodeficiency virus infection and cancer in adults and children residing in Kampala, Uganda. Int J Cancer 2001, 92, 622–627. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




