1. Introduction
Understanding the relationship between the mental health index and ESG-Environmental, Social, and Governance factors in Italian regions is crucial for several reasons. This complex approach provides a comprehensive view of the factors influencing mental health, which is essential for developing effective public health strategies and policies. This detailed analysis can lead to targeted interventions, improved healthcare systems, and ultimately, better mental health outcomes for the population. The importance of this relationship is examined through various lenses: the environmental impact on mental health, social determinants of health, and the role of governance in health outcomes. The environment significantly impacts mental health, influencing both direct and indirect pathways. Clean air, green spaces, and low levels of pollution are directly associated with improved mental health outcomes. In contrast, high pollution levels, poor air quality, and limited access to green spaces can exacerbate mental health issues such as anxiety and depression. Analysing the mental health index in relation to environmental factors allows policymakers to identify specific environmental risks and develop strategies to mitigate these risks. For instance, regions with higher pollution levels can be targeted for environmental clean-up initiatives, while urban areas lacking green spaces can be prioritized for the development of parks and recreational areas. Moreover, climate change and its associated phenomena, such as extreme weather events, have been linked to mental health issues. In Italy, regions prone to natural disasters like floods and landslides often experience heightened stress and anxiety among residents. By examining the mental health index alongside environmental factors, policymakers can better understand the psychological impacts of climate change and develop resilience-building strategies to support affected communities. This could include enhancing infrastructure to withstand extreme weather, providing mental health support services post-disaster, and integrating climate resilience into urban planning. Social determinants, including education, employment, income inequality, and social support networks, play a critical role in shaping mental health outcomes. Regions with higher levels of education and employment typically exhibit better mental health indices. This is because employment provides not only financial stability but also a sense of purpose and social interaction, which are vital for mental well-being. Conversely, unemployment and underemployment are associated with increased stress, anxiety, and depression. Analyzing the mental health index in relation to social factors helps identify regions where social inequalities may be contributing to poor mental health. For instance, areas with high youth unemployment rates (NEET: Not in Education, Employment, or Training) may benefit from targeted employment programs and vocational training. Furthermore, regions with significant income inequality may require policies aimed at reducing the wealth gap, such as progressive taxation and social welfare programs. Understanding these social dynamics allows for the creation of complex policies that address both economic and mental health needs simultaneously. Family and community support are also crucial social determinants. Strong social support networks can buffer against mental health issues, providing emotional and practical support during times of stress. Regions with high levels of social cohesion and community engagement often report better mental health outcomes. By examining these factors, policymakers can promote community-building initiatives, encourage civic participation, and support organizations that foster social connections. This approach recognizes that mental health is not just an individual issue but a community concern that benefits from collective action. Governance plays a pivotal role in determining the quality and accessibility of mental health services. Effective governance ensures that mental health policies are well-implemented and that resources are allocated efficiently to meet the needs of the population. Regions with robust healthcare systems, transparent governance, and active community engagement typically show better mental health indices. Analyzing the mental health index in relation to governance factors highlights the importance of policy coherence and integration across different sectors. For example, mental health cannot be improved solely through healthcare interventions; it requires coordinated efforts across education, employment, housing, and environmental policies. Regions with well-coordinated governance structures that integrate these various sectors often see more significant improvements in mental health outcomes. Moreover, governance impacts the social determinants of health. Policies that ensure fair employment practices, adequate housing, and accessible education contribute to the overall well-being of the population. Transparent and accountable governance also fosters trust in public institutions, which is essential for the successful implementation of mental health initiatives. In contrast, regions with poor governance may experience resource misallocation, corruption, and inefficiency, leading to gaps in mental health services and support.
The relationship between mental health and ESG factors underscores the need for integrated policy approaches. Policymakers must recognize that mental health is influenced by a complex interplay of environmental, social, and governance factors. Effective mental health policies should, therefore, be comprehensive, addressing multiple determinants simultaneously. For instance, an integrated policy approach might include environmental initiatives to reduce pollution and increase green spaces, social policies to improve education and employment opportunities, and governance reforms to enhance the efficiency and transparency of healthcare systems. By addressing these factors collectively, policymakers can create an environment that supports mental well-being. Furthermore, integrated policies can help identify and address the unique needs of different regions. Italy's diverse regions have varying environmental, social, and governance contexts, requiring tailored interventions. For example, rural areas may need more focus on improving healthcare accessibility and employment opportunities, while urban areas might benefit from initiatives to reduce pollution and enhance social cohesion. By considering regional specificities, integrated policies can be more effective in promoting mental health. The use of predictive analytics in examining the relationship between mental health and ESG factors can provide valuable insights for future planning. Machine learning algorithms can identify patterns and predict trends, allowing policymakers to anticipate and address potential mental health issues proactively. This forward-thinking approach can lead to more efficient resource allocation and better-prepared mental health services. For example, predictive models can identify regions at high risk of mental health crises due to environmental degradation or economic downturns. Policymakers can then prioritize these areas for intervention, ensuring that support services are in place before issues escalate. Additionally, predictive analytics can help evaluate the potential impact of different policy interventions, guiding decision-making to maximize positive outcomes.
Longitudinal studies examining the relationship between mental health and ESG factors are essential for understanding the long-term effects of various determinants. Mental health is influenced by cumulative experiences and conditions over time, making it important to track changes and identify trends. Longitudinal data can reveal how environmental changes, social policies, and governance reforms impact mental health over extended periods. Such studies can also help identify lag effects, where the impact of certain determinants on mental health may not be immediate but becomes evident over time. For instance, improvements in air quality may lead to gradual enhancements in mental health, or the benefits of educational policies might take years to manifest fully. Understanding these dynamics is crucial for developing effective long-term strategies.
Analysing the relationship between mental health and ESG factors also involves ethical considerations. Researchers and policymakers must ensure that interventions are equitable and do not disproportionately benefit certain groups while neglecting others. Vulnerable populations, such as low-income individuals, migrants, and those with pre-existing mental health conditions, should be prioritized in mental health policies. Ethical governance requires transparency, accountability, and community involvement in decision-making processes. Engaging communities in developing and implementing mental health initiatives ensures that policies are culturally appropriate and meet the needs of those they aim to serve. Additionally, protecting individual rights and promoting social justice are fundamental principles that should guide mental health policies. Analysing the relationship between the mental health index and ESG factors in Italian regions is of paramount importance. This comprehensive approach provides insights into the multifaceted determinants of mental health, guiding the development of effective and targeted policies. By considering environmental, social, and governance factors collectively, policymakers can create holistic strategies that promote mental well-being and address regional disparities. Integrated policy approaches, predictive analytics, longitudinal studies, and ethical considerations are all essential components of a robust mental health strategy. Ultimately, this analysis can lead to improved public health outcomes, reduced inequalities, and a healthier, more resilient population.
The article continues as follows: the second section presents the analysis of the scientific literature, the third section analyses the trends and regional distribution of the mental health, the fourth section presents the clustering with the k-Means algorithm, the fifth section analyses the predictions through the use of machine learning, the sixth section considers economic policies to increase mental health in light of ESG principles, the seventh section presents the conclusions.
2. Literature Review
Below we present a detailed analysis of the reference literature capable of capturing the relationships between the mental health index and the ESG model. Since the ESG model is composed of three elements, each of which is particularly relevant in determining mental health conditions, we have decided to divide the literature into three parts. We thus present an analysis of the literature relating to the relationships between mental health and the environment, social issues, and governance. The deep connections of the three elements of the ESG model for mental health are highlighted.
Environment and Mental Health. Amerio et al. (2020) explore the psychological impacts of the COVID-19 lockdown, focusing specifically on how the built environment of homes affects mental health. This study is crucial as it reflects the immediate responses of individuals confined to their homes during lockdowns, revealing significant stressors like lack of space, inadequate housing quality, and the absence of natural light, all of which can exacerbate feelings of anxiety and depression. The research stresses the need for urban planning and housing policies to consider mental health impacts, advocating for designs that incorporate elements promoting psychological well-being, such as access to green spaces and enhanced indoor environments. Barouki et al. (2021) address the broader context of the COVID-19 pandemic in relation to global environmental changes. This paper calls for an integrated research approach to understand the links between environmental degradation, climate change, and pandemic outbreaks, highlighting how these global challenges can influence mental health. The study proposes developing new frameworks for public health that incorporate environmental sustainability, suggesting that mitigating climate change and environmental degradation could also improve mental health outcomes. Brouwers et al. (2020) delve into the complexities of mental health disclosure in the workplace. Through focus groups involving multiple stakeholders, including employees with mental health issues and their employers, the study explores the fears and prejudices surrounding mental health disclosure. The findings reveal that stigma remains a significant barrier, impacting employees' decisions to disclose their mental health conditions, which can affect their access to support and accommodations. This study underscores the importance of fostering a workplace culture that is inclusive and supportive of mental health to improve employee well-being and productivity. Callaghan et al. (2021) review the literature on the impact of urban green spaces on mental health, providing evidence that access to such spaces can significantly reduce stress, enhance mood, and improve overall mental well-being. The review advocates for urban planning that prioritizes green spaces not just for their ecological benefits but also for their mental health benefits. This is particularly pertinent in urban settings where concrete dominates and natural landscapes are limited, pointing to a need for cities to integrate more nature into their landscapes as a public health measure. Charlson et al. (2021) conduct a scoping review to examine the existing research on the effects of climate change on mental health. This study highlights an emerging area of concern, noting that climate-related stressors such as extreme weather events and long-term climate shifts can lead to a range of mental health issues, including anxiety, depression, and post-traumatic stress disorder. The review calls for more research into interventions that can mitigate these impacts and suggests integrating mental health considerations into climate adaptation strategies. Choe et al. (2020) investigate whether natural environments enhance the effectiveness of Mindfulness-Based Stress Reduction (MBSR) programs. Their findings suggest that conducting MBSR sessions in natural settings can augment the benefits of mindfulness practices, enhancing not only mental health and well-being but also increasing individuals' connection to nature. This research underscores the potential synergistic effects of combining psychological interventions with environmental exposure, proposing a holistic approach to mental health that incorporates biophilic design in therapeutic practices. Comtesse et al. (2021) introduce the concept of ecological grief as a response to environmental changes. This paper explores whether feelings of grief tied to environmental degradation, such as loss of biodiversity or climate change, represent a mental health risk or a functional emotional response. The authors suggest that while ecological grief can contribute to mental health challenges, it also fosters a deeper connection and commitment to environmental stewardship. Recognizing ecological grief in mental health frameworks can lead to better support systems that address both the emotional and environmental dimensions of this grief. Dzhambov et al. (2021) focus on the mental health benefits of indoor and outdoor greenery during the COVID-19 quarantine. Their study confirms that exposure to green spaces, even when experienced indoors through views or houseplants, can serve as a vital health resource, mitigating stress and boosting mood during extended periods of isolation. This research supports urban and architectural designs that integrate natural elements into living spaces, emphasizing green infrastructure as essential for public health. Hobbs et al. (2021) present data from New Zealand examining the association between unhealthy environments and mental health. This study utilizes nationally representative data to link environmental factors such as pollution, noise, and lack of green spaces with increased psychological distress. The findings argue for policy interventions that prioritize environmental health as a component of public health, suggesting that improving environmental quality can directly enhance community mental health outcomes. Ingle et al. (2020) tackle the often overlooked topic of mental health in the context of climate change. Their discussion stresses the “invisible injustice” that climate change represents, particularly for vulnerable populations who face the greatest mental health risks from climate-induced stressors yet have the least resources to cope. They argue for the urgent integration of mental health support into climate change adaptation strategies, emphasizing that addressing this invisible injustice is crucial for sustainable development and equity. Jiang et al. (2020) focus on the mental and physical health impacts of environmental risk perceptions among migrant construction workers in China. Their study highlights how perceptions of environmental risks—such as pollution and hazardous working conditions—can significantly influence workers' health outcomes. This research underscores the importance of improving working environments and providing better health education and protections to mitigate these adverse effects. Li et al. (2022) investigate the link between environmental noise exposure and mental health in a population-based longitudinal study. Their findings demonstrate a clear association between higher levels of noise exposure and increased risks of mental health issues. This study calls for urban planning and public health policies that consider noise reduction as a critical factor in promoting mental health. Liu et al. (2020) explore the mental health benefits of natural outdoor environments and neighborhood social cohesion using multilevel structural equation modeling. Their research provides empirical support for the positive impacts of green spaces on mental health, mediated by enhanced social cohesion. These findings advocate for urban designs that incorporate green spaces as a strategy to foster community interaction and mental well-being. Marazziti et al. (2021) explore the complex interplay between climate change, environmental pollution, the COVID-19 pandemic, and mental health. This article highlights how these global crises exacerbate mental health issues, pointing to increased rates of anxiety, depression, and other psychological disorders. The authors argue for urgent international cooperation to address these intersecting challenges, suggesting that mitigating environmental and health crises could also alleviate their profound psychological impacts. Marzukhi et al. (2020) present a theoretical framework for understanding the bidirectional associations between the urban physical environment and mental health. Their work explores how urban design and environmental quality both influence and are influenced by the mental health of urban residents. This framework calls for urban planning that not only considers the physical needs of residents but also their psychological well-being, advocating for environments that promote mental health. Ortuño-Sierra et al. (2021) focus on adolescent mental health in relation to environmental and behavioral factors. This article brings together various studies that underscore the critical role of both physical and social environments in shaping adolescent well-being. It highlights the need for supportive environments that foster healthy psychological development during this vulnerable stage of life. Ribeiro et al. (2021) analyze the mental health outcomes associated with exposure to nature during the COVID-19 lockdown in Portugal and Spain. Their comparative study demonstrates that access to natural environments during lockdowns significantly mitigated the mental health impacts of the pandemic, supporting the notion that urban green spaces are not just recreational amenities but essential components of public health infrastructure. Sameroff and Seifer (2021) discuss how environmental risks accumulate to impact child mental health negatively. They provide a comprehensive review of factors such as poverty, neighborhood violence, and lack of access to quality education, which compound over time to exert a profound impact on children's psychological development. This work underscores the need for early interventions that address these environmental risks to prevent long-term mental health issues. Schwartz et al. (2023) explore the emerging concept of climate change anxiety and propose environmental activism as a potential buffer against the mental health impacts of this anxiety. The study suggests that engagement in proactive environmental behaviors can alleviate feelings of helplessness and depression associated with the climate crisis, thus serving a dual purpose: improving mental health and the environment. Tang et al. (2022) provide an analysis of how social capital and the built environment influence mental health among elderly populations in urban China. Their findings indicate that strong social networks and well-designed urban environments significantly enhance mental health, pointing to the need for community-centered urban planning and social policies that foster social interaction and accessibility. Thoma et al. (2021) discuss the field of clinical ecopsychology, which examines the direct impacts of the environmental and climate crisis on mental health. Their work advocates for integrating ecological variables into clinical psychological practice, proposing that understanding these impacts is crucial for developing effective mental health interventions in an era of environmental change. Van Kamp et al. (2022) investigate the long-term effects of environmental quality on mental health from early childhood to adulthood. Their longitudinal approach underscores the lasting impacts of early environmental exposures on mental health, advocating for improvements in environmental quality as a preventive strategy against mental health disorders. Wutich et al. (2020) review the critical links between water security and mental health. They argue that water insecurity can lead to severe psychological stress and mental health issues, advocating for urgent water policy reforms to address this underrecognized water-related stressor. Yue et al. (2022) explore how the built environment influences mental health among older adults China. They find that perceived environmental attributes, such as safety, accessibility, and aesthetic quality, mediate the relationship between the physical environment and mental health, suggesting that improving these perceptions can significantly enhance mental well-being. A synthesis of the literature by macro-themes is presented in
Table 1.
Social Issues and Mental Health. Abbas et al. (2021) explore the pivotal role of social media during the early stages of the COVID-19 pandemic. This study highlights how social media platforms served as critical sources of information, tools for crisis management, and means for maintaining social connections amidst physical distancing measures. However, the authors also discuss the mental health challenges exacerbated by the spread of misinformation and the overload of often anxiety-inducing news, suggesting a need for strategies to leverage social media positively while mitigating its negative impacts on mental health. Argyriadis et al. (2023) report on the barriers to accessing quality healthcare for the LGBTQIA+ community, with a particular focus on gender discrimination and socio-cultural stigmas. Their mixed-method study emphasizes the mental health disparities faced by LGBTQIA+ individuals and calls for inclusive health policies that address these inequities directly. Armbruster and Klotzbücher (2020) discuss the psychological effects of the COVID-19 lockdown in Germany. Their paper examines how social distancing measures have led to increased feelings of isolation and stress, impacting mental health across the population. The findings underscore the importance of developing support systems that can be mobilized during such public health crises to mitigate adverse mental health outcomes. Bedaso et al. (2021) focus on the relationship between social support and mental health issues during pregnancy through a systematic review and meta-analysis. Their findings reveal that strong social support networks are crucial in reducing the risk of mental health problems among pregnant women, highlighting the need for targeted support services for expectant mothers. Braghieri et al. (2022) delve into the complex relationship between social media use and mental health. They provide evidence that prolonged use of social media can have detrimental effects on mental health, suggesting a need for awareness and educational programs to help individuals manage their social media consumption effectively. Brouwers (2020) addresses the issue of social stigma associated with mental illness and its impact on unemployment. He argues that stigma is a significant barrier preventing people with mental health issues from seeking employment and calls for societal and policy changes to reduce stigma and support employment among this population. Chaturvedi (2020) discusses the critical need for mental health rehabilitation services during the COVID-19 crisis. This brief article emphasizes the psychological impacts of the pandemic and the importance of integrating mental health services in all crisis response strategies to support affected individuals. Coyne et al. (2020) present findings from an eight-year longitudinal study on the impacts of social media use on mental health. Their research indicates that excessive social media use can lead to adverse mental health outcomes, providing a data-backed basis for recommending limits and mindful usage of social media platforms. Disney and McPherson (2020) explore the intersection of refugee mental health and employment. Their paper provides insights into the unique challenges faced by refugees in securing employment and accessing mental health services, advocating for specialized support systems that address these specific needs. Facmhn and Bhullar, N. (2020) discuss the effects of social isolation on mental health during the pandemic. This brief report highlights the psychological toll of isolation and the critical need for community-based interventions to support mental well-being during extended periods of social distancing. Fisher et al. (2021) discuss the role of social work in mental health in their book, emphasizing the complexities and vital importance of observing and understanding mental health within social work practice. The text provides an in-depth look at the methodologies and interventions that social workers use to support mental health, showcasing the essential link between practice and outcome in social work. Ganesan et al. (2021) explore the significant mental health impacts of COVID-19-related quarantine, isolation, and lockdown policies. Their study highlights increased rates of anxiety, depression, and suicide due to these restrictive measures, calling for urgent mental health interventions and policy adjustments to mitigate these effects. Girdhar et al. (2020) focus on the mental health issues faced by the elderly during the COVID-19 pandemic. Their research discusses the unique vulnerabilities of the elderly, including isolation and the fear of illness, recommending targeted mental health support and resources for this demographic. Gislason et al. (2021) examine the social and ecological determinants of mental health among children and youth amidst the climate crisis. Their study calls for an integrated approach that considers environmental justice and mental health support in response to climate change. Gorczynski et al. (2021) address mental health literacy and cultural competence in elite sports. Their article underscores the need for comprehensive mental health education and culturally competent practices among sports professionals to improve athlete well-being and performance. Gupta and Agrawal (2021) provide a qualitative analysis of the mental health concerns of college students during the COVID-19 pandemic. Their study reveals the profound anxiety and uncertainty faced by students, emphasizing the need for robust mental health support in educational settings. Mukhtar (2020) discusses the mental health of Pakistanis during the COVID-19 pandemic. The study highlights the psychological distress caused by the pandemic and the importance of culturally appropriate mental health interventions in the Pakistani context. Newman and Zainal (2020) highlight the importance of maintaining social connections for mental health among older adults. They argue that social connections are crucial for mitigating the impacts of aging and isolation on mental health, advocating for community and social strategies to support these connections. Nurunnabi et al. (2020) analyze the mental health and well-being of individuals in higher education during the COVID-19 pandemic across G20 countries. Their study underscores the significant mental health challenges faced by students and faculty, calling for international cooperation to address these issues in the educational sector. O’reilly (2020) examines the dual impact of social media on adolescent mental health. This study explores how social media can both positively and negatively affect young people's mental health, suggesting a need for guidance and education to help adolescents navigate these platforms healthily. Ogbe et al. (2020) offer a comprehensive review of interventions for survivors of intimate partner violence, focusing on the role of social support and mental health outcomes. Their study highlights the effectiveness of community and social support networks in mitigating the psychological impacts of violence, emphasizing the need for integrated services that address both immediate safety and long-term mental health needs. Okoro et al. (2024) explore the potential of technology in enhancing mental health advocacy. Their systematic review suggests that digital platforms can significantly extend the reach and effectiveness of mental health advocacy, making support more accessible and reducing stigma. Ollivier al. (2021) discuss the mental health challenges faced by new mothers during the COVID-19 pandemic. The study sheds light on the acute stress and isolation experienced by new parents, underlining the importance of targeted support and resources to help them navigate the complexities of parenthood during such unprecedented times. Pancani et al. (2021) analyze the mental health impacts of forced social isolation during Italy's COVID-19 lockdown. Their findings illustrate the significant psychological toll of lockdown measures, with social isolation leading to increased anxiety and depression, highlighting the critical need for strategies to maintain social connections even under restrictive conditions. Stogner et al. (2020) examine the specific stresses faced by police officers during the COVID-19 pandemic. The study underscores the high levels of stress and the need for resilience strategies tailored to law enforcement personnel, who face both the usual risks of their jobs and the additional pressures of the pandemic. Sujarwoto et al. (2023) delve into the issue of social media addiction and its impact on mental health among university students in Indonesia during the pandemic. Their findings highlight the double-edged sword of social media, which, while providing a vital connection, also poses risks of addiction that can exacerbate mental health issues. Thakur (2020) offers a unique perspective on the mental health of high school students during the pandemic. This viewpoint piece reflects on the significant educational and psychological disruptions faced by students, advocating for more robust mental health supports within educational settings. Valdez et al. (2020) utilize social media data to analyze mental health trends in the U.S. during the COVID-19 pandemic. Their study provides real-time insights into public mental health, suggesting that social media can be a powerful tool for monitoring and responding to community mental health needs during crises. Ventriglio et al. (2021) explore the mental health challenges associated with urbanization. The study discusses how rapid urban growth can lead to increased mental health issues due to environmental stressors, social fragmentation, and inadequate infrastructure, calling for urban planning that prioritizes mental well-being. A synthesis of the literature by macro-themes is presented in
Table 2.
Governance and Mental Health. Arensman et al. (2022) detail the protocol for the MENTUPP intervention, aimed at improving mental health in workplace settings. This pilot study represents a proactive approach to mental health promotion and intervention, emphasizing the necessity of tailored mental health resources in occupational environments to enhance overall workplace health. Bjørnshagen and Ugreninov (2021) explore the labour market inclusion of young people with mental health issues in Norway. Their study highlights the barriers to employment faced by this demographic and suggests that inclusive employment policies can significantly improve mental health outcomes and economic participation. Cao et al. (2022) analyze how mental health affects job satisfaction, with a focus on the mediating roles of psychological and social capital. The findings underline the complex interplay between an individual's mental health status and their perceptions of job satisfaction, suggesting that enhancing psychological resources could bolster job satisfaction and performance. Cheng et al. (2022) investigate the impact of management practices on entrepreneurial behaviors among college students, using complex adaptive system theory. Their research provides insights into how educational and organizational environments can cultivate entrepreneurial skills and mental resilience among students. Cvenkel (2020) discusses workplace well-being and the role of governance and sustainability in promoting health. This book emphasizes the strategic importance of integrating well-being into corporate governance to enhance both employee health and organizational performance. Fletcher et al. (2020) provide a case study on the integration of a peer respite into a public mental health system. This study exemplifies a community-based approach to mental health care, highlighting the benefits of peer support services in enhancing mental health outcomes and community integration. Hassan et al. (2022) examine the relationship between social media use, consumer behavior, and mental health. Their findings suggest that social media can influence mental well-being and consumer habits, pointing to the need for awareness and interventions to manage the potential negative impacts of digital consumption. Hogg et al. (2021) review workplace interventions aimed at reducing depression and anxiety in small and medium-sized enterprises. This systematic review confirms the effectiveness of targeted workplace interventions in reducing mental health issues, advocating for their broader implementation. Hogg et al. (2023) discuss strategies for supporting employees with mental illness and reducing stigma in the workplace. The study emphasizes the importance of fostering an inclusive and supportive workplace culture to enhance mental health outcomes. Ipsen et al. (2020) argue for the concurrent management of mental health and organizational performance. Their discussion points to the mutual benefits of addressing these aspects together, suggesting that improving mental health at work can lead to better organizational outcomes. Jain et al. (2021) explore the role of occupational health services in managing psychosocial risks and promoting mental health at work. Their study highlights the crucial function of occupational health professionals in identifying and mitigating workplace stressors, advocating for proactive approaches to enhance worker well-being. Looi et al. (2020) discuss the need for an overhaul of corporate governance in mental healthcare in Australia. They argue that current governance structures are inadequate to address the mental health needs of the population effectively, calling for comprehensive reforms to better integrate mental health services within the healthcare system. Lu et al. (2020) analyze the impact of occupational hazards on the mental health and job stress of factory workers and miners. Their research uses propensity score analysis to quantify the effects of hazardous working conditions, underscoring the need for improved occupational health standards and protective measures. Martin et al. (2020) conduct a randomized control trial to evaluate mental health interventions for small-to-medium enterprise owners. The study compares self-administered and telephone-supported interventions, finding that tailored mental health support can significantly reduce stress and improve well-being among entrepreneurs. McLeod et al. (2020) address the lack of evidence in global prison health care governance and its impact on health equity. They highlight the critical gaps in healthcare provision within prison systems and the disproportionate mental health burdens faced by incarcerated populations. Moncrieff (2022) presents a Marxist analysis of the mental health system. This theoretical paper critiques the economic underpinnings of the mental health industry, arguing that profit motives often overshadow the needs of patients, leading to inadequate care and support. Nguyen et al. (2021) discuss the challenges of integrating mental health services into primary care in Vietnam. They describe the systemic barriers and propose solutions to enhance the accessibility and effectiveness of mental health care, emphasizing the importance of community-based approaches. Pavlista et al. (2021) explore the barriers and drivers of psychosocial risk assessments in German micro and small-sized enterprises. Their study reveals that while there is awareness of the importance of mental health at work, many businesses lack the resources and knowledge to implement effective risk management strategies. Piao et al. (2022) investigate how environmental, social, and corporate governance (ESG) activities influence employee psychological well-being. Their research supports the notion that companies that invest in ESG practices not only contribute to environmental and social good but also benefit from improved employee mental health. Salameh et al. (2020) examine the mental health outcomes of the COVID-19 pandemic alongside economic collapse in a developing country. They detail how the dual crises exacerbate mental health issues, stressing the urgent need for comprehensive public health interventions to address these intertwined challenges. Shohaieb et al. (2022) analyze the relationship between corporate governance and diversity management, focusing on how transparency in governance impacts diversity policies. Their study underscores the importance of clear, accountable governance structures in fostering inclusive workplace environments that support mental health. Spitzmueller (2020) discusses the remaking of community mental health services in the context of contested institutional logics and organizational change. This book chapter explores how different organizational models and management strategies can significantly influence the effectiveness of mental health services in community settings. Vella et al. (2021) present a systematic review and meta-synthesis of mental health position statements in sport. Their work assesses the scope and quality of current mental health initiatives in sports, calling for more comprehensive policies to support athletes' mental well-being. Vinberg and Danielsson (2021) explore how COVID-19 has impacted managers of micro-sized enterprises, particularly in terms of business operations, work-life balance, and mental well-being. Their study highlights the intense stress experienced by small business owners during the pandemic and suggests strategies to support these individuals' mental health. Visentin et al. (2020) discuss the challenges faced by small business owners regarding mental health. The article points out the unique pressures small business owners face and the need for targeted mental health interventions within this group. Vito (2020) examines how variations in organizational culture and leadership influence mental health and welfare services for children. The study compares different agencies to understand how organizational practices can better support mental health outcomes for vulnerable populations. Weirauch et al. (2023) evaluate the effects of holacracy, a decentralized governance model, on person-organization fit and job satisfaction. Their research suggests that holacracy can enhance job satisfaction by aligning organizational structures more closely with employees' needs and expectations, potentially improving mental health outcomes. Wu et al. (2021) outline best practices for supporting mental health in the workplace. This article in the provides evidence-based recommendations for organizations to foster a supportive environment that promotes mental well-being and mitigates work-related stress. Yang et al. (2021) investigate how workers' perceptions of their work values affect their physical and mental health in China. The study illustrates the link between value alignment and health outcomes, emphasizing the need for organizations to understand and address the values and expectations of their workforce to enhance well-being. Yi et al. (2022) analyze the relationship between occupational stress, mental health, and work ability among coal chemical workers in Xinjiang. This study highlights the severe impacts of high-stress environments on mental health and underscores the necessity for targeted mental health support and occupational safety improvements in high-risk industries. A synthesis of the literature by macro-themes is presented in
Table 3.
3. Trend and Regional Distributions
Below we present a static analysis relating to the ISTAT-BES findings regarding the trend of the mental health index in the Italian regions. The analysis is conducted in order to create rankings, capture the changes detected in the medium term and also analyze the distribution of the mental health index at macro-regional level in order to identify the existence of a gap between Centre-North Italy and southern Italy.
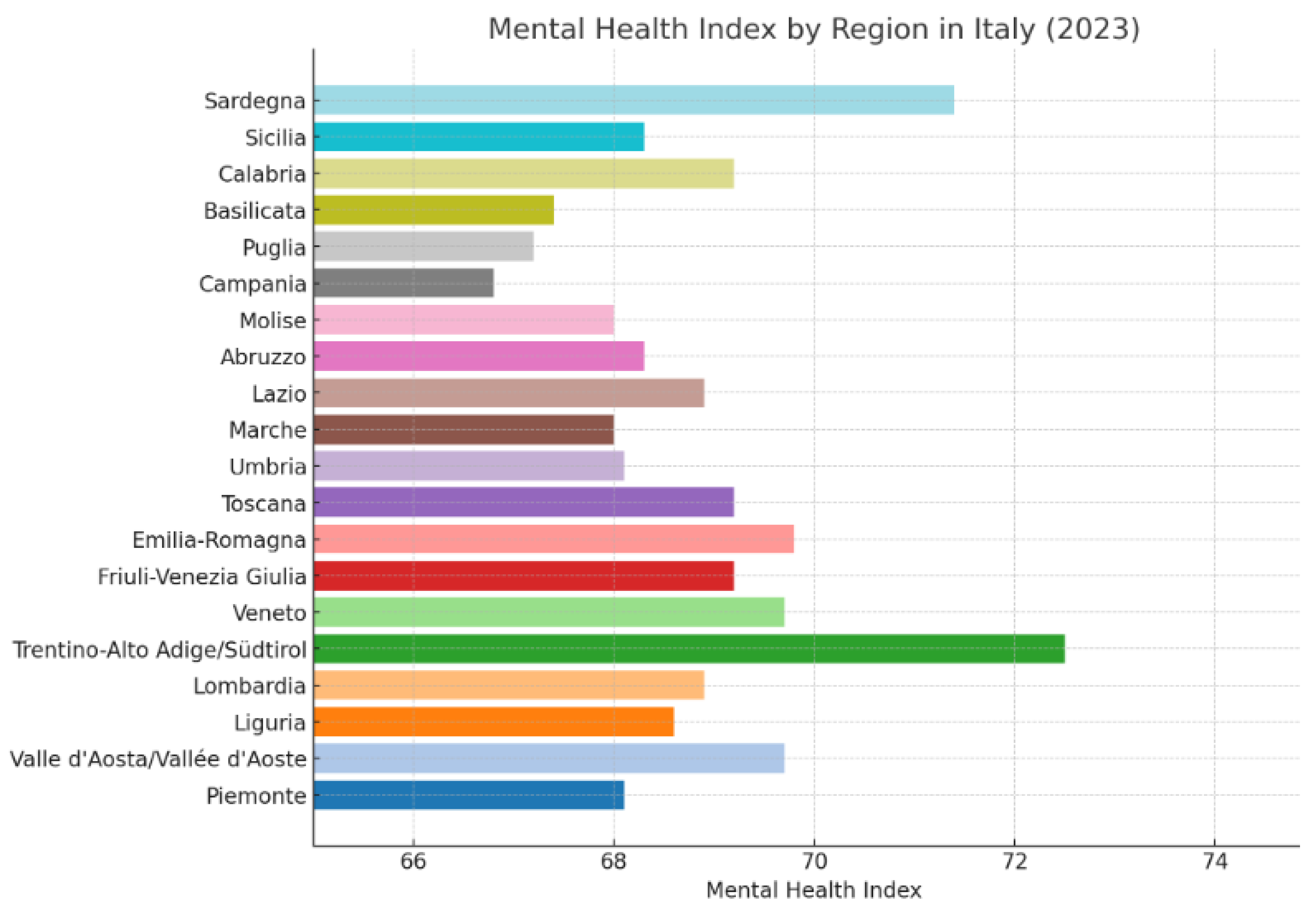
The Mental Health Index across the Italian regions in 2023. The mental health index across various Italian regions in 2023 presents a diverse landscape, reflecting both the geographical and socio-economic variance throughout Italy. Notably, Trentino-Alto Adige/Südtirol achieves the highest index at 72.5, which could be attributed to its robust healthcare infrastructure and high standard of living. On the other end of the spectrum, Campania records the lowest index at 66.8, potentially indicating regional challenges in public health resources and access to mental health services. In northern Italy, regions generally show a stronger mental health index, with Lombardia at 68.9 and Liguria at 68.6, closely followed by Piemonte and Valle d'Aosta/Vallée d'Aoste with 68.1 and 69.7 respectively. This trend may reflect the better economic conditions and higher availability of healthcare services in the north compared to the south of Italy. The exception here is Veneto, matching Valle d'Aosta/Vallée d'Aoste with a score of 69.7, suggesting that even within the more affluent northern areas, there are significant regional variations. The central Italian regions display moderate scores with Toscana and Friuli-Venezia Giulia both scoring 69.2. Emilia-Romagna slightly exceeds these figures with a 69.8 index, indicating a slightly better mental health status which might be linked to its well-established healthcare systems and innovative health policy initiatives. Both Umbria and Marche record scores around the median, with 68.1 and 68 respectively, indicating a standard deviation consistent with central Italian averages. In southern Italy and the islands, the mental health indices reflect a more challenging scenario. While Sardegna shows a relatively high index at 71.4, likely due to its unique demographic and geographic characteristics, regions like Puglia, Basilicata, and Calabria report lower scores of 67.2, 67.4, and 69.2 respectively. These numbers might reflect the socio-economic difficulties prevalent in the southern part of Italy, including higher rates of unemployment and lower GDP per capita, which are known to influence mental health negatively. The index for Sicilia stands at 68.3, aligning closely with the national trend but still below the northern and some central regions. This could be indicative of the ongoing economic struggles and the impacts of less accessible healthcare services. Abruzzo and Molise, often overlooked in broader economic plans, post similar scores at 68.3 and 68, mirroring the overall challenges faced by less economically robust regions. Overall, the mental health index across Italian regions in 2023 highlights the influence of economic stability, access to quality healthcare, and regional policies on mental well-being. It underscores the need for targeted mental health strategies that address the specific needs of each region, particularly focusing on improving healthcare access in the southern regions to bridge the gap with the north. The disparity in indices could serve as a crucial pointer for policymakers to allocate resources more efficiently and foster a balanced approach to mental health across the country (
Figure 1).
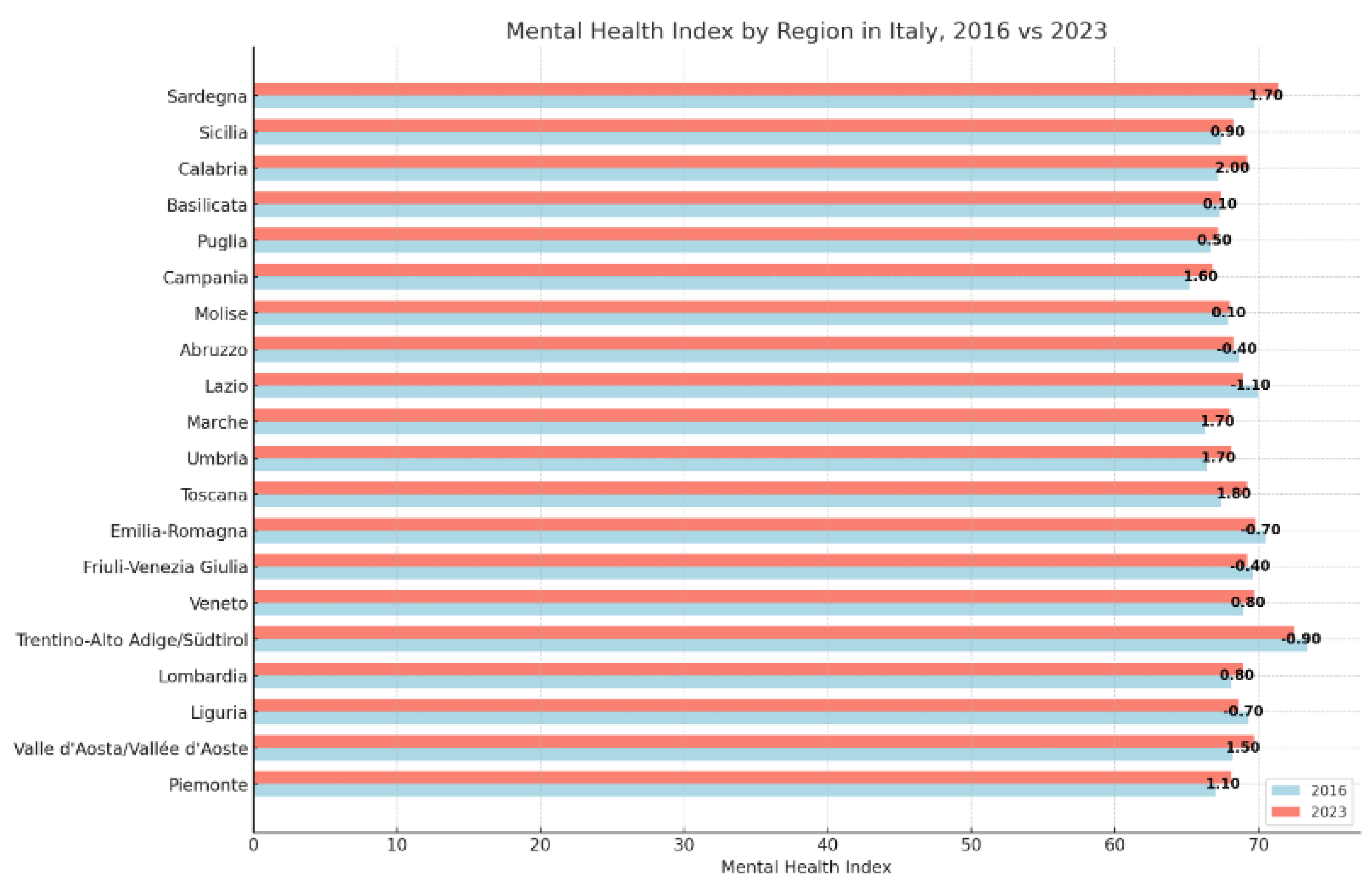
The Mental Health Index across the Italian regions between 2016 and 2023. The data on mental health indices across Italian regions from 2016 to 2023 reveals both positive and negative trends, with variations in absolute and percentage changes that offer insights into regional developments in mental health care and societal wellbeing. Regions such as Toscana, Umbria, and Marche show notable improvements, with Toscana’s index increasing by 1.80 points or 2.67 percent. Both Umbria and Marche mirrored this rise, each increasing by 1.70 points or 2.56 percent. These increases may reflect enhanced healthcare policies, greater public awareness of mental health issues, and improved access to mental health services. Calabria presents the highest percentage increase among all regions, with a 2.00 point rise translating to a nearly 3 percent improvement. This significant change could be associated with targeted regional health initiatives and possibly improved socioeconomic conditions, which often correlate with better mental health outcomes. Conversely, regions like Trentino-Alto Adige/Südtirol, Emilia-Romagna, and Lazio experienced declines in their mental health indices. Trentino-Alto Adige/Südtirol, despite having one of the highest indices in both years, saw a decrease of 0.90 points or 1.23 percent. Emilia-Romagna and Lazio similarly faced reductions of 0.70 and 1.10 points, respectively, which might suggest shifts in regional health priorities, economic challenges, or rising mental health burdens that have not been adequately addressed. Interestingly, Liguria and Friuli-Venezia Giulia also recorded slight declines, which might indicate stagnation in mental health improvements or challenges in maintaining the quality of mental health services. Abruzzo's slight decline of 0.40 points or 0.58 percent further underscores the nuanced regional differences in the evolution of mental health support. In the south, Campania and Sardegna made substantial gains, with increases of 1.60 and 1.70 points, respectively. These improvements could be attributed to concerted efforts to enhance healthcare infrastructure and access to mental health services in these historically underserved regions. The data underscores the complexity of mental health evolution across Italy, influenced by a myriad of factors including economic conditions, healthcare service availability, and regional policies. The overall trend indicates that while some regions have made significant advances, others are either stagnating or regressing, highlighting the need for a more uniform approach to mental health across the country. Policymakers might use this information to target specific areas for improvement and to tailor interventions that address both regional disparities and specific mental health challenges (
Figure 2).
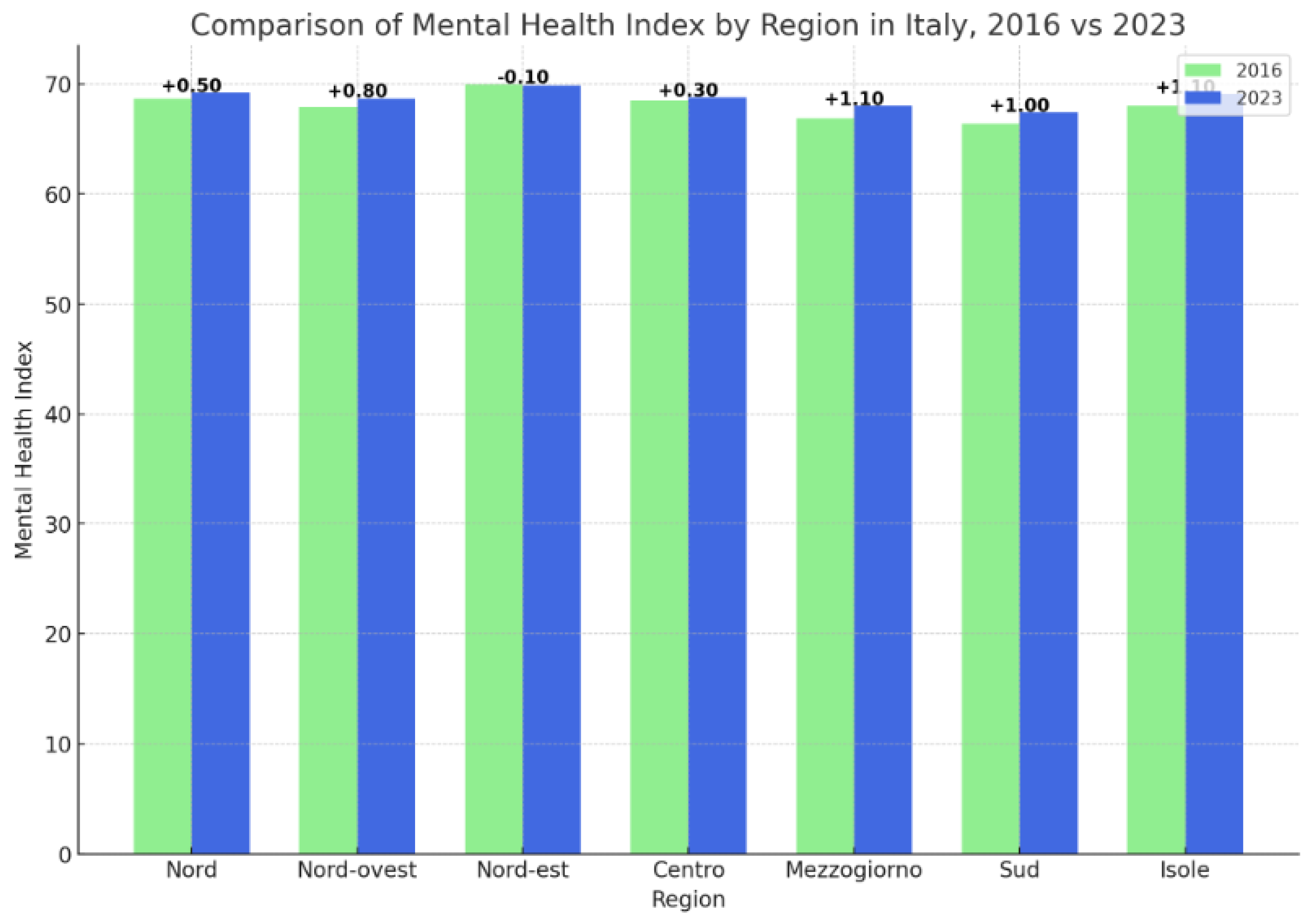
The Mental Health Index across the Italian macro-regions between 2016 and 2023. Analyzing the mental health index data from various regions of Italy over the period from 2016 to 2023 reveals nuanced regional trends that reflect broader socio-economic and healthcare dynamics. The data is segmented into several geographical categories: North, North-west, North-east, Central, Mezzogiorno, South, and Islands, , each displaying unique trends in mental health progression or regression. The North region shows a slight improvement in its mental health index, moving from 68.7 in 2016 to 69.2 in 2023, which translates to a modest increase of 0.50 points or 0.73 percent. This increment, although minimal, suggests a steady enhancement in mental health resources or perhaps better economic stability, which is often linked to improved general wellbeing. Contrastingly, the Northwest, another segment of the North, records a more noticeable improvement from 67.9 to 68.7, marking an 0.80-point or 1.18 percent increase. This might indicate targeted interventions or improved healthcare services that have begun to bear fruit over the seven-year period. However, the North-east region slightly regresses, with a decrease of 0.10 points or 0.14 percent, marking it as an outlier in the northern part of Italy where other regions are witnessing growth. This could be indicative of either economic challenges, reduced healthcare funding, or perhaps shifts in population demographics adversely impacting overall mental health scores. The Central Italy sees a minor rise from 68.5 in 2016 to 68.8 in 2023, an increase of 0.30 points or 0.44 percent. This suggests a stable but slow progression in mental health initiatives, possibly reflecting cautious but steady enhancements in both public health policy and service delivery. In contrast, the southern regions of Italy, particularly Mezzogiorno and South, display more significant improvements. Mezzogiorno's index rises from 66.9 to 68, a gain of 1.10 points or 1.64 percent, and South from 66.4 to 67.4, up by 1.00 point or 1.51 percent. These improvements are notable as they indicate a closing of the gap with more affluent northern regions, possibly due to increased health funding, better accessibility to mental health services, or successful regional programs aimed at enhancing public health. The Islands including Sicily and Sardinia, also show substantial growth, with their index climbing from 68 to 69.1, an increase of 1.10 points or 1.62 percent. This may reflect improvements in local healthcare infrastructures, increased tourism contributing to better economic conditions, or specific regional policies targeting mental health improvements. Overall, the data from 2016 to 2023 underscores a generally positive trend in mental health indices across Italy, with more pronounced gains in historically lower-performing southern regions and islands. This indicates ongoing efforts to address disparities in mental health access and quality across the country, though challenges remain in ensuring uniform progress across all regions (
Figure 3).
Territorial inequalities in terms of mental health index. Analyzing the data concerning the Mental Health Index in Italian regions from 2016 to 2023, a nuanced picture emerges that suggests a partial North-South divide, though with significant improvements in the South and Islands. In the North, represented by three subsets (North, North-West, North-East), the changes in mental health indices are relatively modest. The North's overall index rises slightly from 68.7 to 69.2, a modest increase of 0.50 points or 0.73 percent. The North-West shows a bit more improvement, with an increase from 67.9 to 68.7, translating to a 0.80 point or 1.18 percent rise. Interestingly, the North-East actually experiences a slight decline, with its index decreasing by 0.10 points or -0.14 percent, indicating a stagnation or minor retreat in mental health status. The Central region also shows modest improvement, with the index moving from 68.5 to 68.8, a gain of 0.30 points or 0.44 percent. This suggests stable, albeit slow, progress in mental health outcomes. In contrast, the southern regions, including Mezzogiorno, South, and the Islands, display more substantial improvements. Mezzogiorno's index rises from 66.9 to 68, an increase of 1.10 points or 1.64 percent, which is the highest percentage increase across all regions. Similarly, the South shows a significant improvement, with its index increasing from 66.4 to 67.4, marking a 1.00 point or 1.51 percent rise. The Islands also see a notable increase from 68 to 69.1, a rise of 1.10 points or 1.62 percent. These figures suggest that while the North and Center have relatively stable or slightly improving mental health indices, the more substantial improvements are seen in the South and Islands. This could indicate a reduction in the historical mental health disparities between the northern and southern parts of Italy. The larger increases in the South and Islands might be a result of targeted healthcare initiatives, increased investment in mental health services, or broader socio-economic improvements in these regions. Therefore, while a North-South divide in mental health indices still exists, with the North generally starting from a higher baseline, the gap appears to be narrowing due to more pronounced gains in the South and Islands. This trend is encouraging as it suggests efforts to balance regional disparities in mental health are making an impact, particularly in historically underserved areas.
4. Clusterization with k-Means Algorithms
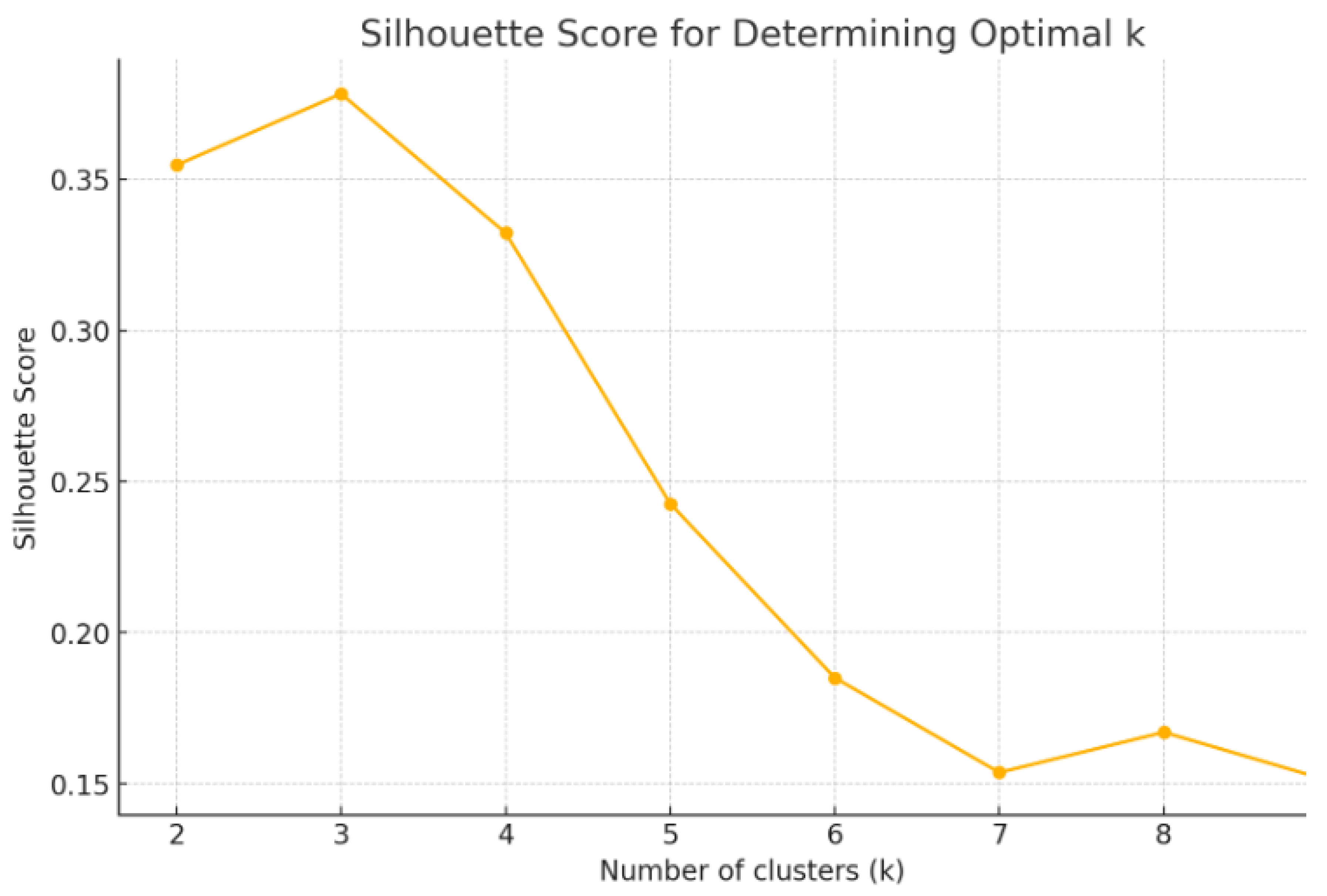
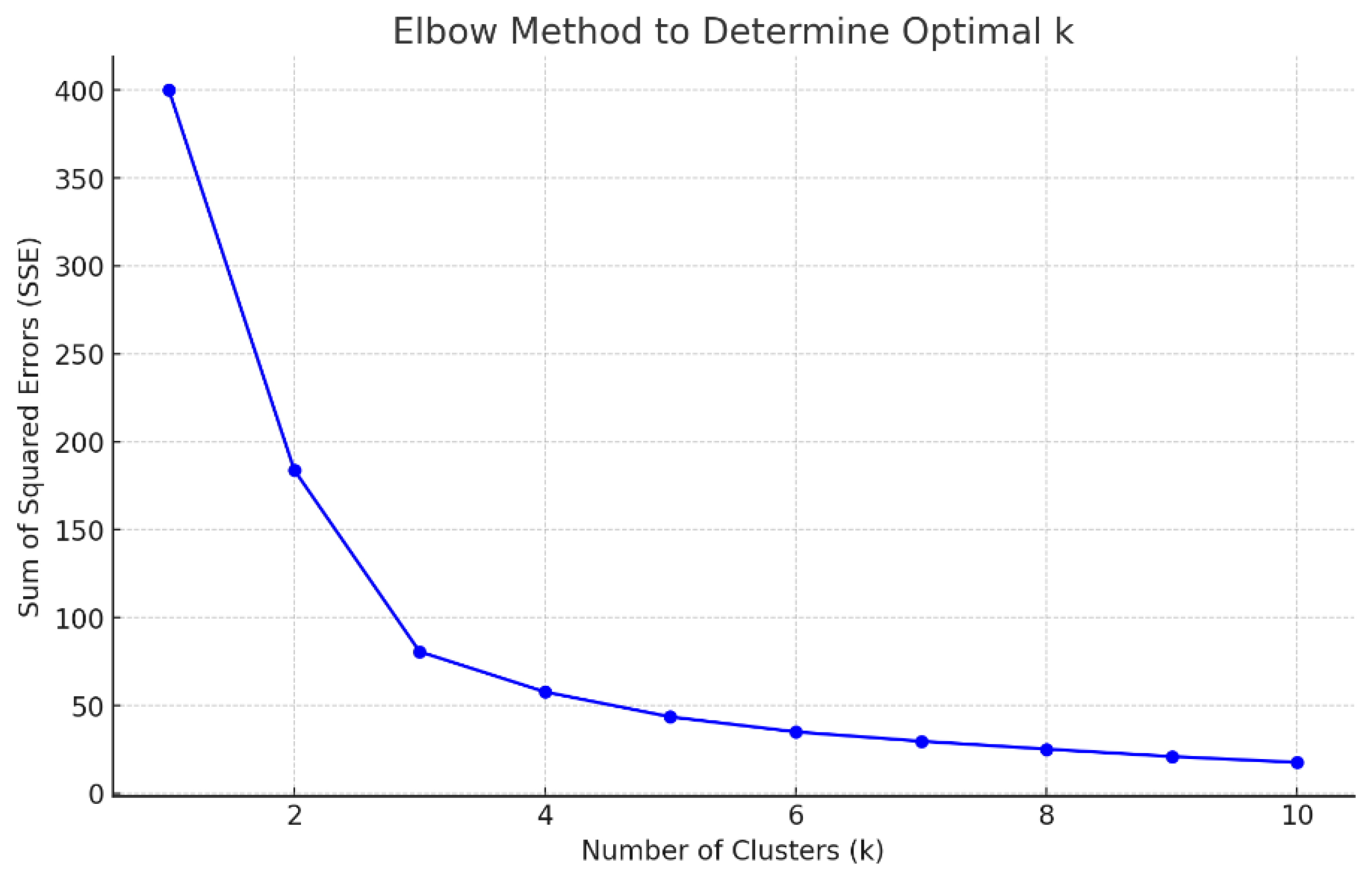
Below we present a clustering with k-Means algorithm. Since the k-Means algorithm is an unsupervised algorithm, it is necessary to use methods and indicators to identify the optimal number of clusters. In the following analysis we therefore present the clustering with the k-Means algorithm based on two optimization criteria, namely the Silhouette Coefficient and the Elbow Method. The results obtained will then be compared to choose the optimization method that is best able to efficiently represent the cluster structure of the Italian regions by value of the Mental Health Index.
In the following part, we analyze a clusterization with k-Means algorithm optimized with the Silhouette Coefficient. Performing a clusterization using the k-Means algorithm, optimized with the Silhouette Coefficient, can be beneficial for a variety of reasons, particularly when dealing with complex datasets such as those measuring variables like mental health indices across different regions. The Silhouette Coefficient measures how similar an object is to its own cluster compared to other clusters. It ranges from -1 to +1, where a high value indicates that objects are well-matched to their own cluster and poorly matched to neighboring clusters. By optimizing the number of clusters (k) based on the Silhouette Coefficient, it is possible to ensure that the clustering solution maximizes internal similarity and minimizes external similarity, providing a more meaningful and statistically significant clustering outcome (
Figure 4).
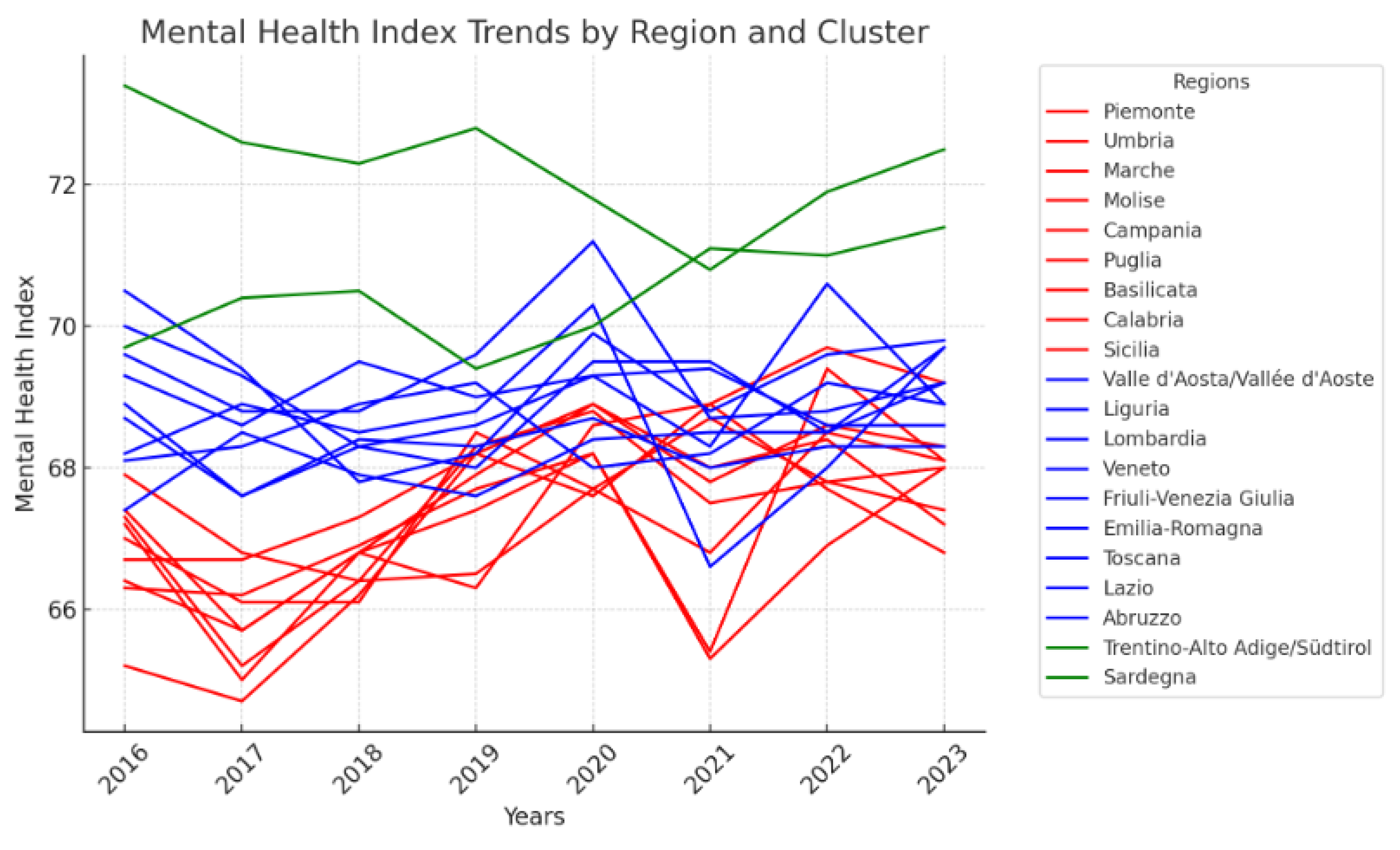
The k-Means clustering algorithm, set with k=3, groups the Italian regions into three distinct clusters based on their mental health index trends from 2016 to 2023:
Cluster 0: encapsulates a diverse group of regions, primarily from the southern part of Italy, including Piemonte, Umbria, Marche, Molise, Campania, Puglia, Basilicata, Calabria, and Sicilia. These regions generally exhibit moderate mental health indices with some fluctuations over the years. The presence of many southern regions in this cluster might reflect the economic challenges and limited healthcare infrastructure that are characteristic of southern Italy. These factors can contribute to variable mental health outcomes and suggest a need for targeted interventions to improve healthcare accessibility and quality in these areas. The inclusion of regions like Piemonte and Umbria, which are not in the southern part of Italy, indicates that while geographical location often correlates with health outcomes, other factors such as local policies, economic conditions, and social issues also play significant roles.
Cluster 1: represents regions with relatively stable and higher mental health indices, suggesting a better overall mental health landscape compared to Cluster 0. This cluster includes Valle d'Aosta/Vallée d'Aoste, Liguria, Lombardia, Veneto, Friuli-Venezia Giulia, Emilia-Romagna, Toscana, Abruzzo, and Lazio. These regions are predominantly located in the northern and central parts of Italy, areas generally associated with stronger economic performance and better healthcare systems. The stability and higher indices observed in these regions could be attributed to more effective public health policies, higher investment in health care, and greater social awareness about mental health. Additionally, these areas typically enjoy higher levels of education and income, which are known to positively impact mental health.
Cluster 2: includes just two regions, Trentino-Alto Adige/Südtirol and Sardegna, which are noted for the highest and most stable mental health indices across all regions considered. The exceptional performance of these regions could be linked to several factors. For Trentino-Alto Adige/Südtirol, high autonomy in local governance allows for tailored health policies and significant investment in public health services, while Sardegna's insular nature might contribute to unique social and economic dynamics that protect against some of the stressors present on the mainland. These regions also benefit from robust local economies and effective social services, which support overall well-being (
Figure 5).
In summary, the clustering reveals a clear pattern where regions in northern and central Italy tend to have better mental health outcomes compared to the south, underscoring the influence of economic disparities on health. However, the standout performance of regions like Trentino-Alto Adige/Südtirol and Sardegna in Cluster 2 also highlights how specific regional policies and unique geographic or economic contexts can significantly enhance mental health outcomes. This analysis underscores the importance of considering local conditions and tailored approaches in addressing mental health challenges across different regions.
To have further proof of the validity of the clustering with the k-Means algorithm optimized with the Silhouette Coefficient it is also necessary to compare the results obtained with the application of the clustering with the k-Means algorithm optimized with the Elbow method. The application of Elbow's method leads to the identification of a number of clusters equal to k=3 (
Figure 6).
The application of the k-Means algorithm optimized with the Elbow Method shows the presence of an optimal number of clusters equal to three. As can be seen, the result of the clustering carried out with the k-Means algorithm optimized with the Silhouette coefficient and the clustering with k-Means algorithm optimized with the Elbow method both lead to the same result. The optimal number of clusters is therefore recognized at k=3.
5. Predictions Using Machine Learning Algorithms
Below we present a comparison between eleven machine-learning algorithms for predicting the value of the mental health index in Italian regions. The algorithms are evaluated based on their performance in terms of R-Squared, MAE-Mean Absolute Error, MSE-Mean Squared Error, RMSE-Root Mean Squared Error. The machine learning algorithms used for prediction are given below i.e.: Linear Regression, Polynomial Regression, Decision Tree, Random Forest, Gradient Boosting, XGBoost, SVR-Support Vector Regression, Neural Network, Ridge Regression, Lasso Regression, Elastic Net Regression. Following the analysis based on the statistical indicators, to better control the predictive efficiency, we also use cross-validation. Finally, the best algorithms will be used both to estimate 2023, which is already present in the original time series, and to estimate 2024, i.e. the following year compared to the reference dataset (
Table 4).
Based on the results shown in the table, the best algorithm for predicting mental health index depends on which aspect of performance is considered most critical. The best performing algorithms are indicated below:
Linear Regression: Shows an R-squared of 1.0, indicating perfect predictive ability on the test set. However, this result is highly suspect as it may indicate extreme overfitting, especially with perfectly linear or very simple data.
Ridge Regression: With an R-squared of 0.981 and very low errors (MAE, MSE, RMSE), Ridge Regression appears to provide good overall performance without the extremes of overfitting shown by simple linear regression.
Polynomial Regression: Demonstrated a good R-squared of 0.953 and relatively low errors. This suggests it can model the complexity and non-linearities in the data well.
Support Vector Regression (SVR): With an R-squared of 0.947 and moderate errors, SVR provides another valid option that generally works well with different types of datasets, especially in non-linear cases or with moderately sized datasets.
If the priority is accuracy and generalization capability while avoiding the risk of overfitting, both Ridge Regression and Polynomial Regression are excellent choices. Support Vector Regression could also be considered for its balance between performance and the ability to handle non-linearities.
Cross validation. Below we present a cross validation to verify the efficiency of the best performing machine learning algorithms. Cross-validation is a powerful tool for ensuring the reliability and robustness of predictive models. It not only helps in selecting the best model among various candidates but also ensures that the chosen model is truly capable of generalizing well to new and unseen data. We perform 10-fold cross-validation for Linear Regression, Ridge Regression, Polynomial Regression, and Support Vector Regression (SVR) to evaluate their performance across multiple subsets of the data. We present in the following table 5 the results of the 10-fold cross-validation for Linear Regression, Ridge Regression, Polynomial Regression, and Support Vector Regression (SVR), showing the average values for R-squared, Mean Absolute Error (MAE), and Mean Squared Error (MSE):
Based on these results it is possible to notice that:
Linear Regression shows perfect R-squared values (1.0) across all folds, suggesting a potential overfitting or perfect linear relation in the dataset, which might not generalize well to new, unseen data.
Ridge Regression provides robust results with high R-squared values close to 1 and low error metrics, indicating a stable model with good generalization capabilities.
Polynomial Regression also exhibits excellent R-squared values close to 1, with low MAE and MSE, indicating strong predictive power and the ability to capture more complex patterns in the data.
SVR displayed variable performance with a much lower average R-squared and significantly higher error values, suggesting it may not be the best fit for this particular dataset or might require more parameter tuning.
Given these results, both Ridge Regression and Polynomial Regression emerge as strong candidates due to their high performance and low error rates, making them suitable for predicting the mental health index effectively. These models are recommended for deployment based on their demonstrated accuracy and reliability in the cross-validation process. Below we therefore present a prediction using data from 2004 to 2022 to predict 2023. Since 2023 is part of the historical series of the data analyzed it is possible to easily calculate the percentage variables between the actual values detected and the values predicted by the algorithms in order to obtain an evaluation of predictive efficiency (
Table 6).
The data provided gives an interesting insight into the mental health index across different regions of Italy for the year 2023, comparing historical data with predictions from two different statistical models: Ridge Regression and Polynomial Regression. This comprehensive analysis can help us understand regional variations in mental health metrics and the potential accuracy and utility of different predictive models. Firstly, it's noteworthy that the predictions for 2023 made by the Ridge Regression model show slight variations from the historical data. These changes are quantified as percentage variations between the predicted and actual data. For example, in regions such as Liguria and Lazio, there are minute positive variations indicating a slightly better mental health index than the historical data. Conversely, regions like Trentino-Alto Adige, Friuli-Venezia Giulia, and Sardegna exhibit minor negative deviations. Such variations, although minimal, are crucial for understanding the dynamic nature of mental health across regions and can guide targeted interventions. The Polynomial Regression model, however, presents an entirely different scenario with zero variation from the historical data in nearly all regions. This uniformity might suggest that the model is possibly overfitting the data, capturing noise rather than underlying trends, or it might simply imply that the historical data patterns are well-established and expected to continue unchanged. This highlights an essential aspect of predictive modeling in mental health: the complexity and potentially stable nature of influencing factors that might not change significantly over short periods. Moreover, the average percentage variation across all regions for Ridge Regression is -0.0021%, while it stands at 0.0000% for Polynomial Regression, suggesting a very stable overall mental health index prediction from the latter. This stability might be comforting but also raises questions about the sensitivity of the models to small yet significant changes in mental health indicators. The specific choice of Ridge versus Polynomial Regression is also of interest. Ridge Regression is known for its ability to handle multicollinearity among predictor variables by imposing a penalty on the size of coefficients. This can be particularly useful in complex datasets like those involving mental health, where many interlinked factors may contribute to the outcome. On the other hand, Polynomial Regression can model non-linear relationships which might be more reflective of the real-world scenarios where mental health outcomes are influenced by non-linearly interacting variables. It is also essential to consider the real-world application of such predictive models. For policymakers, understanding regional variations in mental health can help in allocating resources more efficiently and designing interventions tailored to specific needs. For instance, regions with slight deteriorations might require increased mental health services or public health campaigns to address emerging issues.
Once the validity of the algorithms used and the prediction compared with the historical reference data have been ensured, we can try to predict 2024 to verify the future trends by region. Below are the results in the following
Table 7:
The provided data for the mental health index predictions for 2024 across various regions in Italy, utilizing Ridge and Polynomial Regression models, offers a nuanced view into how these statistical tools can be employed to forecast mental health trends. Each region displays unique trends, with predictions varying slightly between the two models. This analysis not only informs us about the expected changes in mental health indices but also illuminates the efficacy and differences of the two regression techniques. Ridge Regression, known for its robustness in handling multicollinearity by imposing a penalty on the coefficients of the predictors, has shown varied changes across regions. For instance, Emilia-Romagna shows a significant positive variation of 0.45%, suggesting an improvement in the mental health index. Conversely, Sardegna and Lombardia predict a decline, albeit minimal. This variance underscores Ridge Regression's sensitivity to underlying data trends, allowing for subtle fluctuations in the dataset to be captured effectively. On the other hand, Polynomial Regression, which models relationships through higher-degree polynomials and can capture non-linear patterns, presents predictions that are generally in close agreement with those of Ridge Regression but with slightly rounded variations. For instance, in Basilicata, Polynomial Regression predicts a slightly higher improvement than Ridge Regression. Such small discrepancies might indicate Polynomial Regression's ability to detect and model subtle non-linear dynamics in the data which Ridge Regression might overlook. Comparatively, some regions like Campania and Puglia show no change or minimal decrease in the mental health index according to Polynomial Regression, reflecting a potential stability in those areas' mental health conditions. This stability could be interpreted as either a saturation in the potential for improvement or simply a temporary plateau in ongoing mental health dynamics. The differences in prediction between the two models for regions like Trentino-Alto Adige and Molise, which both models predict improvements, can be significant for regional health administrations. These predictions could influence the strategic planning of mental health resources, interventions, and policies to either capitalize on positive trends or counteract negative ones. From an average perspective, both models predict a very slight overall positive change in the mental health index with an average increase of 0.09% for Ridge and 0.10% for Polynomial Regression. This overall minimal change suggests that while there are regional variations, the broader national mental health landscape is expected to remain relatively stable. Such predictive modeling is crucial for preemptive health management, especially in tailoring public health initiatives and resource allocation to address anticipated mental health needs. It allows policymakers and health administrators to visualize potential future scenarios and adjust their strategies accordingly. For instance, areas predicted to experience a decline might need more robust mental health services and early intervention programs. In conclusion, the analysis of the 2024 mental health index predictions through Ridge and Polynomial Regression models not only showcases the practical application of these statistical tools in public health planning but also highlights the regional disparities in mental health trends across Italy. These insights are essential for targeted health interventions, efficient resource allocation, and ultimately, for enhancing the well-being of the population.
6. ESG Oriented Policies to Improve Mental Health
Below we present some economic policy interventions that could be useful for improving mental health conditions by making the environment, the social situation and governance more efficient.
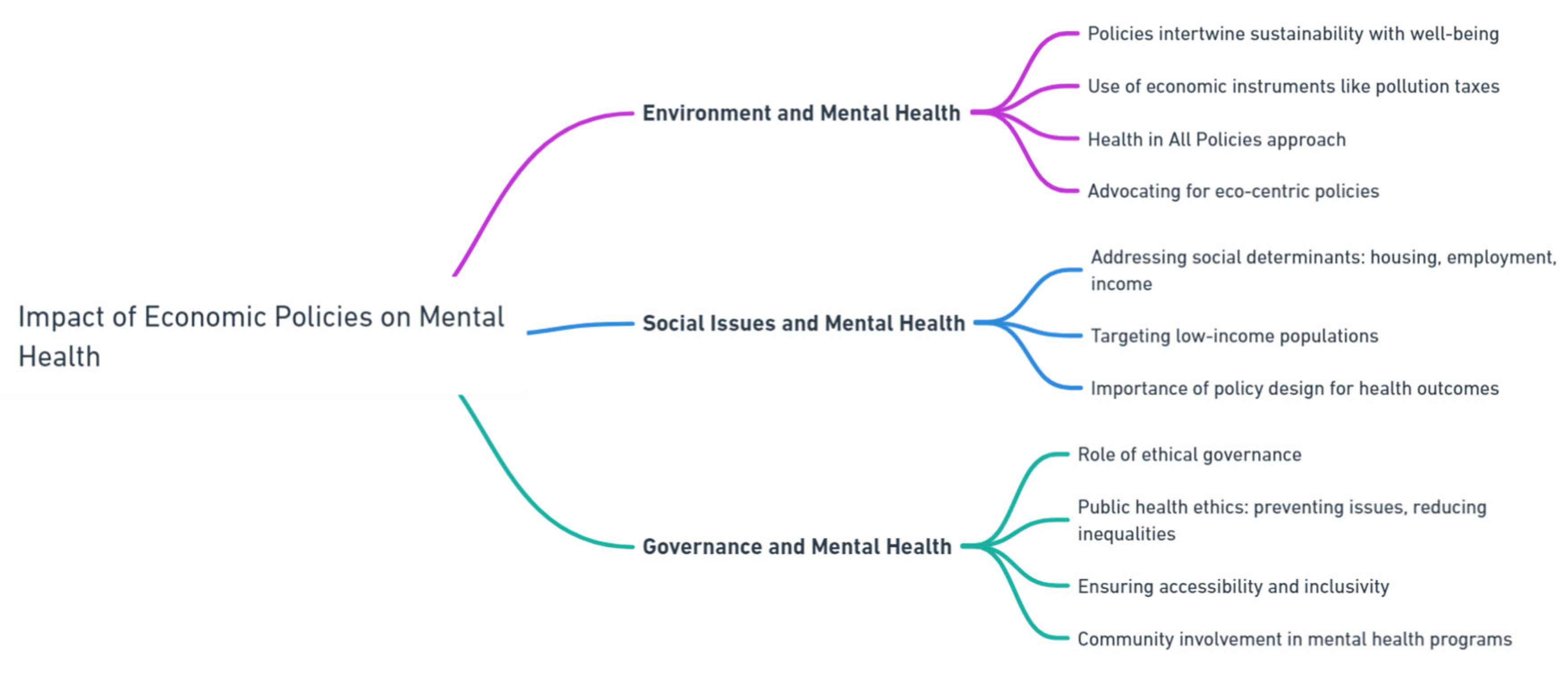
Environment and Mental Health. Economic policies that intertwine environmental sustainability with mental health typically employ strategies that both protect the environment and enhance public well-being. Policies using economic instruments, such as pollution taxes or subsidies for green practices, directly contribute to a healthier environment, thereby improving mental health outcomes. For instance, integrating environmental considerations into fiscal policies and budgeting processes can help mitigate environmentally harmful practices, promoting a healthier living space that benefits mental well-being. The concept of "Health in All Policies" further supports this integration by ensuring that all public policy considerations account for their impact on health, facilitating a comprehensive approach to environmental and mental health. Additionally, advocating for eco-centric policies fosters a societal shift towards deeper environmental connections and care, which is also beneficial for mental health. Such policies not only achieve environmental goals but also enhance public health by creating cleaner, healthier environments that reduce mental health stressors (Warford, 1995); (Guidotti, 2018); (Petrie, 2022); (Younes, 2018); (Gorobets, 2014).
Social Issues and Mental Health. Economic policies that address social issues can significantly impact mental health by altering social determinants of health such as housing, employment, and income. Research shows that economic and social policies targeting low-income populations often yield both mental and physical health benefits, although these effects can diminish over time. Policies aimed at enhancing housing stability, increasing employment opportunities, and providing income supplementation have been shown to improve mental health outcomes. Such policies not only target economic betterment but inadvertently promote mental well-being, emphasizing the interdependence of economic stability and health. For instance, Osypuk et al. (2014) reviewed various U.S. social and economic policies and found that interventions in housing and neighborhood, employment, family strengthening, and income supplementation documented significant mental health benefits. This review highlights the importance of designing social policies with health outcomes in mind, targeting broader segments of the population, and considering family caregiving responsibilities to avoid unintended health consequences.
Governance and Mental Health. Public and ethical governance plays a vital role in promoting mental health by guiding the development and implementation of policies with a strong ethical foundation. Ethical governance in public health ensures mental health initiatives respect individual rights, promote social justice, and address broader social determinants. For example, public health ethics prioritize preventing mental health issues and reducing inequalities by influencing policies that affect social, economic, and environmental factors linked to mental health. Ethical considerations in policy implementation also demand that interventions do not disproportionately affect vulnerable populations, enhance rather than restrict personal autonomy, and maintain transparency and accountability. This approach involves integrating cultural sensitivity and ensuring inclusivity, making mental health programs accessible to all community segments, including minority and underserved groups. Moreover, it emphasizes community involvement in planning and executing mental health initiatives, ensuring that programs respect and respond to community values and experiences. Collectively, these governance practices ensure that mental health policies are not only effective but also equitable and respectful of individual and community rights, fostering an environment where all community members can achieve better mental health outcomes (Cratsley and Radden, 2019); (Kass, 2001); (Bonnie and Zelle, 2019) (
Figure 7).
7. Conclusions
This comprehensive study on the determinants of mental health across Italian regions from 2004 to 2023 provides a nuanced understanding of how environmental, social, and governance (ESG) factors influence mental health outcomes. Using a machine learning approach, the research delves into the static analysis of regional trends, clustering with k-Means algorithm, and a comparative evaluation of eleven machine learning algorithms to predict the mental health index. The findings reveal significant insights into the intricate relationships between mental health and various ESG determinants. First and foremost, environmental factors have a profound impact on mental health. The study finds that regions with cleaner air, more green spaces, and lower pollution levels generally exhibit better mental health outcomes. Conversely, high pollution, poor air quality, and limited access to nature exacerbate mental health issues like anxiety and depression. This underscores the importance of environmental policies aimed at reducing pollution and increasing green spaces. The research also highlights the mental health impacts of climate change and natural disasters, such as floods and landslides, which are particularly pertinent for regions prone to such events. Policymakers are urged to develop resilience-building strategies, including infrastructure improvements and mental health support services, to mitigate these effects. Social determinants are equally critical in shaping mental health outcomes. Higher levels of education and employment correlate with better mental health indices, as employment provides financial stability, social interaction, and a sense of purpose. In contrast, high unemployment and income inequality are linked to increased stress and mental health issues. The study suggests that targeted employment programs, vocational training, and policies to reduce income inequality, such as progressive taxation and social welfare programs, can significantly improve mental health. Moreover, strong social support networks and community engagement play a vital role in buffering against mental health issues. Regions with high social cohesion and active community participation report better mental health outcomes, emphasizing the need for policies that promote community building and civic participation. Governance is another pivotal factor influencing mental health. Regions with robust healthcare systems, transparent governance, and active community engagement tend to have better mental health indices. Effective governance ensures that mental health policies are well-implemented and resources are allocated efficiently. The study highlights the importance of policy coherence across various sectors, including education, employment, housing, and environmental policies, to achieve significant improvements in mental health outcomes. Transparent and accountable governance fosters public trust, which is essential for the successful implementation of mental health initiatives.
The research also identifies substantial regional disparities in mental health indices across Italy. Northern regions generally have higher mental health indices compared to the South, reflecting better economic conditions and healthcare services. However, there are significant improvements in some southern regions and islands, indicating efforts to address these disparities. The clustering analysis using the k-Means algorithm groups Italian regions into three clusters based on their mental health indices, showing that while geographic location is a major factor, local policies, economic conditions, and social issues also play crucial roles. This highlights the need for tailored interventions that address specific regional needs. Predictive analytics prove to be a valuable tool in examining the relationship between mental health and ESG factors. Among the machine learning algorithms evaluated, Linear Regression, Ridge Regression, and Polynomial Regression demonstrate strong predictive capabilities. These models can identify patterns and predict trends, allowing policymakers to anticipate and address potential mental health issues proactively. By using predictive models, policymakers can allocate resources more efficiently and ensure mental health services are prepared for future challenges. The study advocates for an integrated policy approach that addresses multiple determinants simultaneously, combining environmental initiatives, social policies, and governance reforms to create a holistic strategy for mental health. Ethical considerations are paramount in developing mental health policies. Interventions must be equitable and prioritize vulnerable populations, such as low-income individuals, migrants, and those with pre-existing mental health conditions. Ethical governance ensures transparency, accountability, and community involvement in decision-making processes. Engaging communities in the development and implementation of mental health initiatives ensures that policies are culturally appropriate and meet the needs of those they aim to serve. This approach enhances personal autonomy, inclusivity, and respect for cultural values, fostering an environment where all community members can achieve better mental health outcomes. The study suggests several economic policy interventions to improve mental health conditions by making the environment, social situation, and governance more efficient. For environmental improvements, policies such as pollution taxes, subsidies for green practices, and integrating environmental considerations into fiscal policies are recommended. For social improvements, enhancing housing stability, increasing employment opportunities, and providing income supplementation are suggested to target economic betterment and promote mental well-being. Governance policies should ensure ethical governance in public health, promoting social justice and addressing broader social determinants through inclusive and transparent policymaking.
8. Declarations
Data Availability Statement. The data presented in this study are available on request from the corresponding author.
Funding. The authors received no financial support for the research, authorship, and/or publication of this article.
Declaration of Competing Interest. The authors declare that there is no conflict of interests regarding the publication of this manuscript. In addition, the ethical issues, including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication.
References
- Abbas, J.; Wang, D.; Su, Z.; Ziapour, A. The Role of Social Media in the Advent of COVID-19 Pandemic: Crisis Management, Mental Health Challenges and Implications. Risk Manag. Heal. Policy 2021, 14, 1917–1932. [Google Scholar] [CrossRef]
- Amerio, A.; Brambilla, A.; Morganti, A.; Aguglia, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Costanza, A.; Signorelli, C.; et al. COVID-19 Lockdown: Housing Built Environment’s Effects on Mental Health. Int. J. Environ. Res. Public Heal. 2020, 17, 5973. [Google Scholar] [CrossRef]
- Arensman, E.; O’connor, C.; Leduc, C.; Griffin, E.; Cully, G.; Dhálaigh, D.N.; Holland, C.; Van Audenhove, C.; Coppens, E.; Tsantila, F.; et al. Mental Health Promotion and Intervention in Occupational Settings: Protocol for a Pilot Study of the MENTUPP Intervention. Int. J. Environ. Res. Public Heal. 2022, 19, 947. [Google Scholar] [CrossRef]
- Argyriadis, A.; Fradelos, E.C.; Argyriadi, A.; Ziegler, E.; Kaba, E. Advancing Access to Quality LGBTQIA+ Health Care: Gender Discrimination, Socio-Cultural, and Mental Health Issues: A Mixed-Method Study. Int. J. Environ. Res. Public Heal. 2023, 20, 4767. [Google Scholar] [CrossRef]
- Armbruster, S.; Klotzbücher, V. (2020). Lost in lockdown? COVID-19, social distancing, and mental health in Germany (No. 2020-04). Diskussionsbeiträge.
- Barouki, R.; Kogevinas, M.; Audouze, K.; Belesova, K.; Bergman, A.; Birnbaum, L.; Boekhold, S.; Denys, S.; Desseille, C.; Drakvik, E.; et al. The COVID-19 pandemic and global environmental change: Emerging research needs. Environ. Int. 2021, 146, 106272–106272. [Google Scholar] [CrossRef]
- Bedaso, A., Adams, J., Peng, W., & Sibbritt, D. (2021). The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reproductive health, 18, 1-23.
- Bjørnshagen, V.; Ugreninov, E. Labour market inclusion of young people with mental health problems in Norway. Alter 2021, 15, 46–60. [Google Scholar] [CrossRef]
- Bonnie, R.; Zelle, H. (2019). Ethics in Mental Health Care: A Public Health Perspective. The Oxford Handbook of Public Health Ethics. [CrossRef]
- Braghieri, L., Levy, R. E., & Makarin, A. (2022). Social media and mental health. American Economic Review, 112(11), 3660-3693.
- Brouwers, E.P.M. Social stigma is an underestimated contributing factor to unemployment in people with mental illness or mental health issues: position paper and future directions. BMC Psychol. 2020, 8, 1–7. [Google Scholar] [CrossRef]
- Brouwers, E.P.M.; Joosen, M.C.W.; van Zelst, C.; Van Weeghel, J. To Disclose or Not to Disclose: A Multi-stakeholder Focus Group Study on Mental Health Issues in the Work Environment. J. Occup. Rehabilitation 2020, 30, 84–92. [Google Scholar] [CrossRef]
- Callaghan, A.; McCombe, G.; Harrold, A.; McMeel, C.; Mills, G.; Moore-Cherry, N.; Cullen, W. The impact of green spaces on mental health in urban settings: a scoping review. J. Ment. Heal. 2020, 30, 179–193. [Google Scholar] [CrossRef]
- Cao, X.; Zhang, H.; Li, P.; Huang, X. The Influence of Mental Health on Job Satisfaction: Mediating Effect of Psychological Capital and Social Capital. Front. Public Heal. 2022, 10, 797274. [Google Scholar] [CrossRef]
- Charlson, F. , Ali, S., Benmarhnia, T., Pearl, M., Massazza, A., Augustinavicius, J., & Scott, J. G. (2021). Climate change and mental health: a scoping review. International journal of environmental research and public health, 18(9), 4486.
- Chaturvedi, S.K. Covid-19, Coronavirus and Mental Health Rehabilitation at Times of Crisis. J. Psychosoc. Rehabilitation Ment. Heal. 2020, 7, 1–2. [Google Scholar] [CrossRef]
- Cheng, Y.; Zhang, J.; Liu, Y. The Impact of Enterprise Management Elements on College Students’ Entrepreneurial Behavior by Complex Adaptive System Theory. Front. Psychol. 2022, 12, 769481. [Google Scholar] [CrossRef]
- Choe, E.Y.; Jorgensen, A.; Sheffield, D. Does a natural environment enhance the effectiveness of Mindfulness-Based Stress Reduction (MBSR)? Examining the mental health and wellbeing, and nature connectedness benefits. Landsc. Urban Plan. 2020, 202, 103886. [Google Scholar] [CrossRef]
- Comtesse, H.; Ertl, V.; Hengst, S.M.C.; Rosner, R.; Smid, G.E. Ecological Grief as a Response to Environmental Change: A Mental Health Risk or Functional Response? Int. J. Environ. Res. Public Heal. 2021, 18, 734. [Google Scholar] [CrossRef]
- Coyne, S.M.; Rogers, A.A.; Zurcher, J.D.; Stockdale, L.; Booth, M. Does time spent using social media impact mental health?: An eight year longitudinal study. Comput. Hum. Behav. 2020, 104, 106160. [Google Scholar] [CrossRef]
- Cratsley, K. , & Radden, J. (2019). Public mental health ethics. Developments in Neuroethics and Bioethics. [CrossRef]
- Cvenkel, N. Well-Being in the Workplace: Governance and Sustainability Insights to Promote Workplace Health; Springer Science and Business Media LLC: Dordrecht, GX, Netherlands, 2020. [Google Scholar]
- Disney, L.; McPherson, J. Understanding Refugee Mental Health and Employment Issues: Implications for Social Work Practice. J. Soc. Work. Glob. Community 2020, 5, 2. [Google Scholar] [CrossRef]
- Dzhambov, A.M.; Lercher, P.; Browning, M.H.E.M.; Stoyanov, D.; Petrova, N.; Novakov, S.; Dimitrova, D.D. Does greenery experienced indoors and outdoors provide an escape and support mental health during the COVID-19 quarantine? Environ. Res. 2021, 196, 110420. [Google Scholar] [CrossRef]
- FACMHN, K. U. A. R. P. , & Bhullar, N. (2020). Life in the pandemic: Social isolation and mental health.
- Fisher, M.; Newton, C.; Sainsbury, E. Mental Health Social Work Observed; Informa UK Limited: London, United Kingdom, 2021. [Google Scholar]
- Fletcher, E. , Barroso, A., & Croft, B. (2020). A case study of a peer respite's integration into a public mental health system. Journal of health care for the poor and underserved, 31(1), 218-234.
- Ganesan, B.; Al-Jumaily, A.; Fong, K.N.K.; Prasad, P.; Meena, S.K.; Tong, R.K.-Y. Impact of Coronavirus Disease 2019 (COVID-19) Outbreak Quarantine, Isolation, and Lockdown Policies on Mental Health and Suicide. Front. Psychiatry 2021, 12, 565190. [Google Scholar] [CrossRef]
- Girdhar, R. , Srivastava, V., & Sethi, S. (2020). Managing mental health issues among elderly during COVID-19 pandemic. Journal of geriatric care and research, 7(1), 32-5.
- Gislason, M.K.; Kennedy, A.M.; Witham, S.M. The Interplay between Social and Ecological Determinants of Mental Health for Children and Youth in the Climate Crisis. Int. J. Environ. Res. Public Heal. 2021, 18, 4573. [Google Scholar] [CrossRef]
- Gorczynski, P.; Currie, A.; Gibson, K.; Gouttebarge, V.; Hainline, B.; Castaldelli-Maia, J.M.; Mountjoy, M.; Purcell, R.; Reardon, C.L.; Rice, S.; et al. Developing mental health literacy and cultural competence in elite sport. J. Appl. Sport Psychol. 2020, 33, 387–401. [Google Scholar] [CrossRef]
- Gorobets, A. Eco-centric policy for sustainable development. J. Clean. Prod. 2014, 64, 654–655. [Google Scholar] [CrossRef]
- Guidotti, T.L. Sustainability and health: notes toward a convergence of agendas. J. Environ. Stud. Sci. 2018, 8, 357–361. [Google Scholar] [CrossRef]
- Gupta, R.; Agrawal, R. Are the concerns destroying mental health of college students?: A qualitative analysis portraying experiences amidst COVID-19 ambiguities. Anal. Soc. Issues Public Policy 2021, 21, 621–639. [Google Scholar] [CrossRef]
- Hassan, H.; Hsbollah, H.M.; Mohamad, R. Examining the interlink of social media use, purchase behavior, and mental health. Procedia Comput. Sci. 2022, 196, 85–92. [Google Scholar] [CrossRef]
- Hobbs, M.; Kingham, S.; Wiki, J.; Marek, L.; Campbell, M. Unhealthy environments are associated with adverse mental health and psychological distress: Cross-sectional evidence from nationally representative data in New Zealand. Prev. Med. 2021, 145, 106416. [Google Scholar] [CrossRef]
- Hogg, B.; Medina, J.C.; Gardoki-Souto, I.; Serbanescu, I.; Moreno-Alcázar, A.; Cerga-Pashoja, A.; Coppens, E.; Tóth, M.D.; Fanaj, N.; Greiner, B.A.; et al. Workplace interventions to reduce depression and anxiety in small and medium-sized enterprises: A systematic review. J. Affect. Disord. 2021, 290, 378–386. [Google Scholar] [CrossRef]
- Hogg, B.; Moreno-Alcázar, A.; Tóth, M.D.; Serbanescu, I.; Aust, B.; Leduc, C.; Paterson, C.; Tsantilla, F.; Abdulla, K.; Cerga-Pashoja, A.; et al. Supporting employees with mental illness and reducing mental illness-related stigma in the workplace: an expert survey. Eur. Arch. Psychiatry Clin. Neurosci. 2023, 273, 739–753. [Google Scholar] [CrossRef]
- Ingle, H. E. , & Mikulewicz, M. (2020). Mental health and climate change: tackling invisible injustice. The Lancet Planetary Health, 4(4), e128-e130.
- Ipsen, C.; Karanika-Murray, M.; Nardelli, G. Addressing mental health and organisational performance in tandem: A challenge and an opportunity for bringing together what belongs together. Work. Stress 2020, 34, 1–4. [Google Scholar] [CrossRef]
- Jain, A.; Hassard, J.; Leka, S.; Di Tecco, C.; Iavicoli, S. The Role of Occupational Health Services in Psychosocial Risk Management and the Promotion of Mental Health and Well-Being at Work. Int. J. Environ. Res. Public Heal. 2021, 18, 3632. [Google Scholar] [CrossRef]
- Jiang, Y.; Luo, H.; Yang, F. Influences of Migrant Construction Workers’ Environmental Risk Perception on Their Physical and Mental Health: Evidence from China. Int. J. Environ. Res. Public Heal. 2020, 17, 7424. [Google Scholar] [CrossRef]
- Kass, N.E. An Ethics Framework for Public Health. Am. J. Public Heal. 2001, 91, 1776–1782. [Google Scholar] [CrossRef]
- Li, A.; Martino, E.; Mansour, A.; Bentley, R. Environmental Noise Exposure and Mental Health: Evidence From a Population-Based Longitudinal Study. Am. J. Prev. Med. 2022, 63, e39–e48. [Google Scholar] [CrossRef]
- Looi, J.C.; Allison, S.; Bastiampillai, T. Commonwealth of common mental health: the need for a comprehensive overhaul of corporate governance in mental healthcare in Australia. Australas. Psychiatry 2020, 28, 300–302. [Google Scholar] [CrossRef]
- Marazziti, D. , Cianconi, P., Mucci, F., Foresi, L., Chiarantini, I., & Della Vecchia, A. (2021). Climate change, environment pollution, COVID-19 pandemic and mental health. Science of the total environment, 773, 145182.
- Martin, A. , Kilpatrick, M., Scott, J., Cocker, F., Dawkins, S., Brough, P., & Sanderson, K. (2020). Protecting the mental health of small-to-medium enterprise owners: a randomized control trial evaluating a self-administered versus telephone supported intervention. Journal of Occupational and Environmental Medicine, 62(7), 503-510.
- Marzukhi, M.A.; Ghazali, N.M.; Leh, O.L.H.; Yakob, H. A Bidirectional Associations between Urban Physical Environment and Mental Health: A theoretical framework. Environ. Proc. J. 2020, 5, 167. [Google Scholar] [CrossRef]
- McLeod, K.E.; Butler, A.; Young, J.T.; Southalan, L.; Borschmann, R.; Sturup-Toft, S.; Dirkzwager, A.; Dolan, K.; Acheampong, L.K.; Topp, S.M.; et al. Global Prison Health Care Governance and Health Equity: A Critical Lack of Evidence. Am. J. Public Heal. 2020, 110, 303–308. [Google Scholar] [CrossRef]
- Moncrieff, J. The Political Economy of the Mental Health System: A Marxist Analysis. Front. Sociol. 2022, 6, 771875. [Google Scholar] [CrossRef]
- Mukhtar, S. Pakistanis’ mental health during the COVID-19. Asian journal of psychiatry 2020, 51, 102127. [Google Scholar] [CrossRef]
- Newman, M.G.; Zainal, N.H. The value of maintaining social connections for mental health in older people. Lancet Public Heal. 2020, 5, e12–e13. [Google Scholar] [CrossRef]
- Nguyen, T. , Tran, T., Tran, H., Tran, T. D., & Fisher, J. (2021). Challenges in integrating mental health into primary care in Vietnam. In Innovations in global mental health (pp. 1249-1269). Cham: Springer International Publishing.
- Nurunnabi, M.; Almusharraf, N.; Aldeghaither, D. Mental health and well-being during the COVID-19 pandemic in higher education: Evidence from G20 countries. J. Public Heal. Res. 2020, 9, 60–68. [Google Scholar] [CrossRef]
- O’reilly, M. Social media and adolescent mental health: the good, the bad and the ugly. J. Ment. Heal. 2020, 29, 200–206. [Google Scholar] [CrossRef]
- Ogbe, E. , Harmon, S., Van den Bergh, R., & Degomme, O. (2020). A systematic review of intimate partner violence interventions focused on improving social support and/mental health outcomes of survivors. PLoS one, 15(6), e0235177.
- Okoro, Y.O.; Ayo-Farai, O.; Maduka, C.P.; Okongwu, C.C.; Sodamade, O.T. The role of technology in enhancing mental health advocacy: a systematic review. Int. J. Appl. Res. Soc. Sci. 2024, 6, 37–50. [Google Scholar] [CrossRef]
- Ollivier, R.; Aston, M.; Price, S.; Sim, M.; Benoit, B.; Joy, P.; Iduye, D.; Nassaji, N.A. Mental Health & Parental Concerns during COVID-19: The Experiences of New Mothers Amidst Social Isolation. Midwifery 2021, 94, 102902–102902. [Google Scholar] [CrossRef]
- Ortuño-Sierra, J.; Lucas-Molina, B.; Inchausti, F.; Fonseca-Pedrero, E. Special Issue on Mental Health and Well-Being in Adolescence: Environment and Behavior. Int. J. Environ. Res. Public Heal. 2021, 18, 2975. [Google Scholar] [CrossRef]
- Osypuk, T.L.; Joshi, P.; Geronimo, K.; Acevedo-Garcia, D. Do Social and Economic Policies Influence Health? A Review. Curr. Epidemiology Rep. 2014, 1, 149–164. [Google Scholar] [CrossRef]
- Pancani, L.; Marinucci, M.; Aureli, N.; Riva, P. Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown. Front. Psychol. 2021, 12, 663799. [Google Scholar] [CrossRef]
- Pavlista, V. , Angerer, P., & Diebig, M. (2021). Barriers and drivers of psychosocial risk assessments in German micro and small-sized enterprises: a qualitative study with owners and managers. BMC public health, 21, 1-12.
- Petrie, M. Integrating Economic and Environmental Policy. Policy Q. 2022, 18, 10–17. [Google Scholar] [CrossRef]
- Piao, X.; Xie, J.; Managi, S. Environmental, social, and corporate governance activities with employee psychological well-being improvement. BMC Public Heal. 2022, 22, 1–12. [Google Scholar] [CrossRef]
- Ribeiro, A.I.; Triguero-Mas, M.; Santos, C.J.; Gómez-Nieto, A.; Cole, H.; Anguelovski, I.; Silva, F.M.; Baró, F. Exposure to nature and mental health outcomes during COVID-19 lockdown. A comparison between Portugal and Spain. Environ. Int. 2021, 154, 106664–106664. [Google Scholar] [CrossRef]
- Salameh, P.; Hajj, A.; A Badro, D.; Selwan, C.A.; Aoun, R.; Sacre, H. Mental Health Outcomes of the COVID-19 Pandemic and a Collapsing Economy: Perspectives from a Developing Country. Psychiatry Res. 2020, 294, 113520–113520. [Google Scholar] [CrossRef]
- Sameroff, A. J. , & Seifer, R. (2021). Accumulation of environmental risk and child mental health. In Children of poverty (pp. 233-258). Routledge.
- Schwartz, S.E.O.; Benoit, L.; Clayton, S.; Parnes, M.F.; Swenson, L.; Lowe, S.R. Climate change anxiety and mental health: Environmental activism as buffer. Curr. Psychol. 2023, 42, 16708–16721. [Google Scholar] [CrossRef]
- Shohaieb, D.; Elmarzouky, M.; Albitar, K. Corporate governance and diversity management: evidence from a disclosure perspective. Int. J. Account. Inf. Manag. 2022, 30, 502–525. [Google Scholar] [CrossRef]
- Spitzmueller, M. C. (2020). Remaking “community” mental health: Contested institutional logics and organizational change. In Human Service Organizations and the Question of Impact (pp. 11-33). Routledge.
- Stogner, J. , Miller, B. L., & McLean, K. (2020). Police stress, mental health, and resiliency during the COVID-19 pandemic. American journal of criminal justice, 45, 718-730.
- Saputri, R.A.M.; Yumarni, T. Social Media Addiction and Mental Health Among University Students During the COVID-19 Pandemic in Indonesia. Int. J. Ment. Heal. Addict. 2021, 1–15. [Google Scholar] [CrossRef]
- Tang, S. , Lee, H. F., & Feng, J. (2022). Social capital, built environment and mental health: a comparison between the local elderly people and the ‘laopiao’in urban China. Ageing & Society, 42(1), 179-203.
- Thakur, A. Mental Health in High School Students at the Time of COVID-19: A Student’s Perspective. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1309–1310. [Google Scholar] [CrossRef]
- Thoma, M.V.; Rohleder, N.; Rohner, S.L. Clinical Ecopsychology: The Mental Health Impacts and Underlying Pathways of the Climate and Environmental Crisis. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Valdez, D.; Thij, M.T.; Bathina, K.; A Rutter, L.; Bollen, J. Social Media Insights Into US Mental Health During the COVID-19 Pandemic: Longitudinal Analysis of Twitter Data. J. Med Internet Res. 2020, 22, e21418. [Google Scholar] [CrossRef]
- van Kamp, I.; Waye, K.P.; Kanninen, K.; Gulliver, J.; Bozzon, A.; Psyllidis, A.; Boshuizen, H.; Selander, J.; Hazel, P.v.D.; Brambilla, M.; et al. Early environmental quality and life-course mental health effects: The Equal-Life project. Environ. Epidemiology 2022, 6, e183. [Google Scholar] [CrossRef]
- Vella, S.A.; Schweickle, M.J.; Sutcliffe, J.T.; Swann, C. A systematic review and meta-synthesis of mental health position statements in sport: Scope, quality and future directions. Psychol. Sport Exerc. 2021, 55, 101946. [Google Scholar] [CrossRef]
- Ventriglio, A.; Torales, J.; Castaldelli-Maia, J.M.; De Berardis, D.; Bhugra, D. Urbanization and emerging mental health issues. CNS Spectrums 2021, 26, 43–50. [Google Scholar] [CrossRef]
- Vinberg, S.; Danielsson, P. Managers of micro-sized enterprises and Covid-19: impact on business operations, work-life balance and well-being. Int. J. Circumpolar Heal. 2021, 80, 1959700. [Google Scholar] [CrossRef]
- Visentin, D.C.; Cleary, M.; Minutillo, S. Small Business Ownership and Mental Health. Issues Ment. Heal. Nurs. 2020, 41, 460–463. [Google Scholar] [CrossRef]
- Vito, R. Key variations in organizational culture and leadership influence: A comparison between three children’s mental health and child welfare agencies. Child. Youth Serv. Rev. 2020, 108, 104600. [Google Scholar] [CrossRef]
- Warford, J.J. Environment, health, and sustainable development: the role of economic instruments and policies. . 1995, 73, 387–95. [Google Scholar]
- Weirauch, L.; Galliker, S.; Elfering, A. Holacracy, a modern form of organizational governance predictors for person-organization-fit and job satisfaction. Front. Psychol. 2023, 13, 1021545. [Google Scholar] [CrossRef]
- Wu, A.M.; Roemer, E.C.; Kent, K.B.; Ballard, D.W.P.; Goetzel, R.Z. Organizational Best Practices Supporting Mental Health in the Workplace. J. Occup. Environ. Med. 2021, 63, E925–E931. [Google Scholar] [CrossRef]
- Wutich, A. , Brewis, A., & Tsai, A. (2020). Water and mental health. Wiley Interdisciplinary Reviews: Water, 7(5), e1461.
- Yang, F.; Jiang, Y.; Pu, X. Impact of Work Value Perception on Workers’ Physical and Mental Health: Evidence from China. Healthcare 2021, 9, 1059. [Google Scholar] [CrossRef]
- Yi, X.; Yang, J.; Gao, X.; Li, F. The relationship between occupational stress, mental health and work ability of coal chemical workers in Xinjiang. Front. Psychiatry 2022, 13, 903534. [Google Scholar] [CrossRef]
- Younes, M. 1694b Health in all policies as a sustainable development strategy. In Proceedings of the Occupational and Environmental Medic 32nd Triennial Congress of the International Commission on Occupational Health (ICOH), Dublin, Ireland, 29th April to 4th May 2018; p. 602. [Google Scholar]
- Yue, Y.; Yang, D.; Owen, N.; Van Dyck, D. The built environment and mental health among older adults in Dalian: The mediating role of perceived environmental attributes. Soc. Sci. Med. 2022, 311, 115333. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).