Submitted:
17 June 2024
Posted:
18 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Physical Exercise
3.1. GAD
3.1.1. Physical Exercise as an Adjuvant to Pharmacotherapy
3.1.2. Yoga
3.2. SAD
3.2.1. Resistance and Aerobic Exercise
3.2.2. Yoga
3.3. PTSD
3.3.1. Resistance and Aerobic Exercise
3.3.2. Yoga
3.4. Panic Disorder
3.4.1. Resistance and Aerobic Exercise
3.4.2. Yoga
3.5. Conclusion
| Author, year of publication | Study design | Intervention | Participant count | Population characteristics | |
| Cox et al. (2000) |
Randomized controlled trial | Exercise on either a treadmill (jogging) or a stationary stepper (stepping) at either low intensity (50% predicted VO2 max) or high intensity (75% predicted VO2 max) for 30 minutes. | Total: 24 | -Male university students -Average age of 28.3 years -Engage in vigorous physical activity 3 times per week for 30–60 minutes -Recreational exercisers, not highly trained athletes |
|
| Mccarthy et al. (2017) |
Unblinded observational study with a waiting period and baseline control data collection | Trauma-sensitive yoga sessions are 90 minutes every seven days for eight weeks, consisting of Hatha yoga with various postures, sensory awareness, breath awareness, and guided meditation. Home practice was also encouraged. | Total: 30 | -Mean age of 63.5 years -The majority of participants were males -All participants had a diagnosis of PTSD -The majority of participants had relatively severe PTSD symptoms |
|
| Whitworth et al. (2019) |
Randomized controlled trial | The intervention included three 30-minute high-intensity resistance exercise sessions per week for 3 weeks, led by a certified personal trainer, with exercises tailored to the individual's eight-repetition maximum and limited interpersonal interaction. | Total: 30 | -Participants were non-treatment-seeking urban-dwelling adults The mean age of participants was 29.10 years -73.3% of the sample were female -Participants were aged between 18 and 45 years -Participants had exposure to a recent traumatic event within the past 2 years -Participants had a positive screen for PTSD and anxiety -Participants could not be undergoing any trauma-focused therapies at the time of the study -Participants on psychoactive medications for other conditions had to be on a stable dose for at least 6 months before the study |
|
| Ma et al. (2017) |
Randomized experimental design with purposive sampling | A home-based exercise program includes 30 minutes of exercise daily, 5 days per week for 3 months, a pocket-size book, a logbook, a DVD with exercise demonstrations, and regular communication with the research team. | Total: 86 | Among participants, 23 (27.8%) were diagnosed with OCD, 24 (28.9%) with panic disorder (PD), 4 (7.5%) with social phobia (SP), 2 (2.4%) with post-traumatic stress disorder (PTSD), 28 (33.7%) with GAD, and 2 (2.4%) with specific phobias. Participants reported a moderate-to-high level of anxiety, more than half were married, and those with OCD had more years of education and lower trait anxiety levels compared to other anxiety disorders. |
|
| Broman-Fulks et al. (2004) |
Randomized controlled trial | High-intensity aerobic exercise and low-intensity walking exercise, each completed for six 20-minute sessions over two weeks, with the high-intensity exercise aiming to achieve heart rates between 60% and 90% of the individual's age-adjusted predicted maximal heart rate. | Total: 54 | -Participants were 54 students, predominantly women (41 out of 54) -The age range of participants was 18-51, with a mean age of 21.17 -Participants had to achieve a score of 25 or more on the Anxiety Sensitivity Index, be at least 18 years old, and be in good general health to be included in the study -Exclusion criteria included health conditions that would prevent aerobic exercise, current involvement in psychotherapy or use of psychotropic medication, and current participation in an aerobic exercise program |
|
| Broman-Fulks et al. (2015) |
Randomized controlled trial | Participants received either aerobic or resistance training, which included two sets of each exercise to exhaustion with weights they could perform at least 10 repetitions and 2 minutes of rest between sets. | Total: 77 | -Female: 60% -Caucasian: 85% |
|
| Plag et al. (2020) |
Randomized controlled trial | High-intensity interval training (HIIT) every second day for 12 days and Lower-intensity exercise training (LIT) every second day for 12 days. | Total: 33 | -The study included 33 patients with generalized anxiety disorder (GAD). -The sample consisted of 24 women and 9 men, with a higher percentage of women in the HIIT and LIT groups. |
|
| Lucibello et al. (2019) |
Randomized controlled trial | Nine-week moderate-intensity exercise group: 3 weekly exercise sessions involving cycling at 70-75% of HR maximum for 27.5 minutes each session. | Total: 54 | -Young adults aged 18-30 years old -Majority of female participants -Participants recruited from McMaster University -Participants engaged in no more than one hour of moderate-to-vigorous physical activity per week for the past six months -The study focused on the effects of aerobic exercise training on physical performance and mental functioning |
|
| Ströhle et al. (2009) |
Crossover design, within-subject design | Treadmill walking for 30 minutes at 70% VO2 max and a bolus injection of CCK-4 (25 lg for patients, 50 lg for healthy subjects) dissolved in 2 ml 0.9% saline. | Total: 24 | -Patients with panic disorder and healthy age-and sex-matched control subjects | |
| Gaudlitz et al. (2015) |
Randomized, double-blind, controlled | -Exercise Group: Endurance training on a treadmill three times a week for 8 weeks for 30 minutes each time. -Control Group: Light exercises, light stretching, and simple yoga-based exercises three times a week for 8 weeks for 30 minutes each time. |
Total: 58 |
-Patients with panic disorder (PD) with or without agoraphobia -Aged between 18-70 -All patients were Caucasian -Exclusion of patients with severe mental disorders, acute suicidal tendencies, epilepsy, pregnancy, or breastfeeding |
|
| Wedekind et al. (2010) |
Randomized controlled trial | Paroxetine 20mg capsules daily for 10 weeks, Aerobic exercise for 45 minutes 3 times a week for 10 weeks, Relaxation training similar to Autogenic Training once daily for increasing durations up to 20 minutes by the end of the study. | Total: 75 |
Patients with panic disorder with or without agoraphobia, aged between 19 and 52 years on average, with a majority being female (70%) | |
| Herring et al. (2011) |
Randomized controlled trial | The study participants received interventions were Resistance Exercise Training (RET) and Aerobic Exercise Training (AET), both involving 2 weekly sessions for 6 weeks. RET sessions lasted approximately 46 minutes and 40 seconds, focusing on resistance exercises for the legs, while AET sessions consisted of 16 minutes of continuous leg cycling. | Total: 30 |
-Patients aged between 18-37 years -Patients with a primary DSM-IV diagnosis of Generalized Anxiety Disorder (GAD) |
|
| Yi et al.(2022) |
Randomized controlled trial | 12-week yoga intervention consisting of 6 45-minute sessions held once every 2 weeks | Total: 94 |
-Women with symptoms of post-traumatic stress disorder (PTSD) following a motor vehicle accident (MVA) |
|
| Streeter et al. (2010) |
Randomized controlled trial | Yoga intervention (60-minute sessions 3 times a week for 12 weeks, taught by certified Iyengar yoga instructors with consistent presentation of weekly posture sequences) and Walking intervention (60-minute sessions 3 times a week for 12 weeks, matched for metabolic demands with the yoga intervention) | Total: 34 |
-Participants aged 18-45 years old with no current Axis I diagnosis -Nonpsychoactive medications were allowed if the dosage was stable for at least 1 month;- Individuals with recent yoga practice, active psychotherapy, certain medical conditions, recent medication affecting the GABA system, tobacco use, high alcohol consumption, and contraindications to MRI evaluation were excluded. -Women were obligated to use birth control and had to have negative pregnancy tests. |
|
| Javnbakht et al. (2009) |
Randomized controlled trial | Twice-weekly yoga classes of 90 minutes duration for two months, consisting of Ashtanga yoga exercises (Iyengar method) | Total: 34 |
-New female patient referrals without documented psychological disorders or specialist recommendation for yoga therapy -Exclusion of cases with a history of psychiatric disorders, drug abuse, and previous yoga practice |
|
| Jazaieri et al. (2012) |
Randomized controlled trial | The study participants received mindfulness-Based Stress Reduction (MBSR) and Aerobic Exercise (AE) interventions. MBSR included eight weekly 2.5-hour group classes, a 1-day meditation retreat, and daily home practice. AE included a 2-month gym membership with at least two individual AE sessions and one group AE session per week. | Total: 56 |
-Participants with Social Anxiety Disorder (SAD) randomised to MBSR or AE: -52% female, -41% Caucasian, -mean age 32.8 Healthy control group: -52.1% female, -56.3% Caucasian, -mean age 33.9 Untreated group with generalised SAD: -44.8% female, -48.3% Caucasian, -mean age 32.3 |
|
| Fetzner et al. (2015) | Randomized controlled trial | Standardized aerobic exercise program on a stationary bicycle for six 20-minute sessions over two weeks at 60-80% heart rate reserve, supervised by certified personal trainers in a private laboratory exercise room. | Total: 33 |
- Participants were primarily women (76%) - Participants reported being Caucasian (79%), Canadian First Nations (9%), Asian (6%), and Latino (3%) - Participants were employed full-time (46%), students (24%), employed part-time (12%), on medical leave from their occupation (6%), or unemployed (6%) |
|
| Lundt et al. (2019) | Observational study with elements of randomization and control | Yoga therapy is provided in yoga classes, 60 minutes each, once a week for 8 weeks, including body and breathing activities and meditation. | Total: 70 |
The majority of the participants were women - All participants were of German nationality - 90% of the participants had secondary and higher education - The most common tumour diagnosis among participants was breast cancer - The average time since primary diagnosis was 24 months - A portion of the participants had experienced recurrence or were diagnosed with metastases |
|
| Gordon et al. (2020) | Randomized controlled trial | The intervention consisted of an eight-week RET program conducted twice weekly, with progressive resistance and various exercises. These included barbell squat, barbell bench press, hexagon bar deadlift, seated dumbbell shoulder lateral raise; barbell bent over rows, dumbbell lunges, seated dumbbell curls, and abdominal crunches. Participants also underwent a three-week familiarisation process before starting the whole intervention. | Total: 44 | - Participants meeting the criteria for AGAD - Participants not excluded if in treatment for anxiety, depression, or other mental health disorders |
|
| O'Sullivan et al. (2023) | Randomized controlled trial | Eight-week, twice-weekly resistance exercise training (RET) intervention including exercises such as barbell back squat, barbell bench press, hexagon bar deadlift, seated dumbbell shoulder lateral raise, barbell bent over rows, dumbbell lunges, seated dumbbell curls, and abdominal crunches. Sessions were one-on-one and lasted approximately 25 minutes. The resistance was progressively increased as participants completed two sets of 8-12 repetitions. Load adjustments were made based on performance. | Total: 55 | -36 female participants out of a total of 55 participants -Participants with and without subclinical Generalized Anxiety Disorder (AGAD) and Major Depressive Disorder (AMDD) -Participants recruited via posters, emails, and word of mouth -Participants stratified by sex and AGAD status -Participants not excluded for previous engagement in resistance exercise training -Participants were asked about their involvement in a formalized resistance exercise training program to quantify training age |
|
| Tully et al. (2015) | Observational study | Primary depression cognitive behavioural therapy (CBT), Primary generalized anxiety disorder (GAD) CBT, Community exercise program once per week for 1 hour, including aerobic training, resistance training, and flexibility/balance exercises for 12 weeks | Total: 29 |
HF patients under psychiatric management with comorbid depression and generalized anxiety disorder | |
| Doria et al. (2015) | Non-controlled longitudinal study | SKY therapy for six months, including an intense workshop with 10 sessions over two weeks followed by weekly follow-up classes, consisting of five sequential breathing exercises with specific techniques like Ujjayi, Nadi Shodana, Kapalabati, Bhastrika, and Sudarshan Kriya. | Total: 69 | The population consisted of both men and women. -The majority of the participants were women. -The study included individuals with mental disorders, specifically anxiety and depression. |
|
| Simon et al. (2020) | Prospective randomized controlled trial | Kundalini yoga and Cognitive Behavioral Therapy for Generalized Anxiety Disorder, delivered in groups of 4 to 6 participants by 2 instructors during twelve 120-minute sessions with 20 minutes of daily homework. Kundalini yoga includes physical postures, breathing techniques, relaxation exercises, meditation, mindfulness practices, yoga theory, philosophy, and psychology. Cognitive Behavioral Therapy provides psychoeducation, cognitive restructuring, progressive muscle relaxation, worry exposures, in vivo exposure exercises, and targeted metacognitions. | Total: 226 | -Participants were adults aged 18 years or older The majority of participants were female (69.9%) -Participants had a primary diagnosis of Generalized Anxiety Disorder (GAD) -Exclusions included various mental health conditions and a history of more than 5 yoga or CBT sessions in the past 5 years |
|
| Szuhany et al. (2022) | Randomized controlled trial | Cognitive Behavioral Therapy (CBT) for 12 weeks, Yoga (Kundalini Yoga) for 12 weeks, Stress education for 12 weeks | Total: 226 |
-Participants were 226 men and women - 70% of the participants were female - Exclusion criteria included various mental health conditions such as posttraumatic stress disorder, substance use disorders, eating disorders, etc. - Participants self-reported their age, gender, race, and ethnicity |
|
| Goldin et al. (2013) | Randomized controlled trial | Mindfulness-Based Stress Reduction (MBSR) and aerobic exercise (AE) stress reduction program for 8 weeks. MBSR included eight weekly 2.5-hour group classes, a 1-day meditation retreat, and daily home practice. AE included 2-month gym memberships requiring at least two individual AE sessions and one group AE session per week. | Total: 56 |
Participants with generalized Social Anxiety Disorder (SAD) who met DSM-IV criteria for primary generalized SAD and had various comorbidities, including generalized anxiety disorder, major depressive disorder, specific phobia, dysthymia, panic disorder, agoraphobia, and obsessive-compulsive disorder. | |
| Herring et al. (2015) | Randomized controlled trial | Resistance exercise training (RET) and aerobic exercise training (AET) were conducted twice weekly for six weeks. | Total: 26 | - Sedentary women - Diagnosed with Generalized Anxiety Disorder (GAD) - Young adults with insufficient sleep and irregular sleep patterns |
|
| Herring et al. (2011) | Randomized controlled trial | Resistance Exercise Training (RET) involves lower-body weightlifting with two weekly sessions, and Aerobic Exercise Training (AET) involves dynamic leg cycling with two weekly sessions. | Total: 30 |
-Primary diagnosis of Generalized Anxiety Disorder (GAD) -Not undergoing concurrent psychiatric or psychological therapy other than medication -Anxiety Disorders Interview Schedule (ADIS-IV) clinician severity rating of at least 4 |
|
| Rosenbaum et al. (2014) | Randomized controlled trial | Three 30-minute resistance-training sessions per week, pedometer-based walking program, weekly supervised exercise sessions, two unsupervised home-based exercise sessions, individualized exercise intensity, increase in load based on RPE, provision of pedometer and exercise diary, adjustments based on physical activity levels and PTSD symptom severity, designed concerning ACSM guidelines. Usual care involves psychotherapy, pharmaceutical interventions, and group therapy. | Total: 81 |
-84% of the participants were male -Mean baseline BMI was 30.5, with the majority of participants being overweight or obese |
|
| Jazaieri et al. (2016) | Randomized controlled trial | The study participants received Mindfulness-based stress reduction (MBSR) for 8 weeks and Aerobic exercise (AE) for 8 weeks, including specific components for each intervention. | Total: 47 |
- 53% females - Predominantly Caucasian (45%) and Asian (45%) - Diagnosed with generalized social anxiety disorder |
|
| Fetzner et al. (2014) | Randomized controlled trial | A 2-week intervention involving six 20-minute aerobic exercise sessions on a stationary bicycle at 60-80% heart rate reserve, supervised by certified personal trainers. Participants were divided into three groups: one receiving interoceptive prompts (IP), another a distraction task, and the third with no specific prompts or distractions during exercise. | Total: 33 |
-Participants were primarily women (76%) -Participants reported being Caucasian (79%), Canadian First Nations (9%), Asian (6%), and Latino (3%) -Participants were employed full-time (46%), students (24%), employed part-time (12%), on medical leave from their occupation (6%), or unemployed (6%) |
|
| Javed et al. (2022) | case report | Yoga Practice Module (Pranayam, asanas, suryatrataka, OM kara meditation) for 30 minutes daily in the early morning at home; Dietary recommendations emphasizing specific food choices and preparation guidelines. | 1 | -32 years old, married male -Symptoms started at the age of 12 -No history of psychological trauma -Had caring parents and was a good performer in school |
|
| Broocks et al. (1998) | Randomized controlled trial | The intervention(s) that the study participants received were regular aerobic exercise (running) and clomipramine (112.5 mg/day) for a 10-week treatment protocol. | Total: 46 |
Patients with moderate to severe panic disorder with or without agoraphobia, outpatients, patients with no concomitant physical disorders or current substance abuse, and patients required to discontinue psychotropic medication at least 3 weeks before baseline. Young patients with no contraindications for aerobic or other forms of exercise. | |
| Carter et al. (2013) | Randomized controlled trial | Sudarshan Kriya Yoga (SKY) intervention is adapted for veterans and includes cyclical breathing at different rates, joint mobility exercises, warrior values, mild yoga stretches, Yoga Nidra, and guided meditation. Participants were encouraged to maintain a daily 30-minute yoga breath practice | Total: 25 | -The study population consists of male -Vietnam veterans - The average age of the participants is 58 years - The participants are classified as disabled due to service-related PTSD |
|
| Martin et al. (2016) | Randomized controlled trial | Participants received a 75-minute yoga intervention weekly for 12 weeks or twice weekly for 6 weeks, designed by a licensed psychologist and a certified Kripalu yoga instructor. The intervention included trauma-sensitive elements, simple poses progressing over time, and components of Dialectical Behavior Therapy. | Total: 38 |
-Female participants The majority of participants were white (52.6%) -Nearly half of the participants had previously taken a yoga class -Average body mass index was in the overweight range |
|
| Sree et al. (2024) | Randomized controlled trial | Integrated yoga sessions lasting 60 minutes, five days a week, for 12 weeks, including loosening exercises, sun salutations, physical postures, breathing practices, and anapana meditation. | Total: 64 |
Individuals diagnosed with panic disorder, gender distribution with 54.7% male and 45.3% female participants, majority of participants were literate, predominantly from semi-urban areas, majority of participants were unmarried, about 45.3% of participants were employed | |
| Vorkapic et al. (2014) | Randomized controlled trial | Group 1 (G1-Yoga): Yoga classes twice a week, 50 minutes each, for 2 months. Group 2 (G2-CBT + Yoga): Yoga practice and CBT sessions twice a week, 100 minutes (yoga once a week for 50 minutes, CBT once a week for 50 minutes), for 2 months. | Total: 20 |
-Both male and female participants -Diagnosed with panic disorder (DSM IV), with or without agoraphobia -Exclusion criteria: severe pulmonary disease, heart condition, high blood pressure -Inclusion criteria: subjects with depression (comorbidity) or using antidepressant or anxiolytic drugs |
|
| Huberty et al. (2020) | randomized feasibility trial | Intervention low dose (LD): 60 minutes per week of online yoga for 12 weeks. Intervention moderate dose (MD): 150 minutes weekly online yoga for 12 weeks. Stretch and tone control group (STC): 60 minutes weekly of online stretching/toning exercises for 12 weeks. |
Total: 90 |
-Participants were predominantly White (86%) -Most participants earned $61,000 per year or more -A majority of participants were college-educated -The average gestational age at the time of stillbirth was 30 weeks |
|
| Ensari et al. (2019) | A randomized, counterbalanced, within-subjects design | Participants received a 40-minute session of guided yoga or a light stretching protocol. The yoga session included vinyasa style yoga, while the stretching protocol involved minimal movement. Peak RPE was assessed after the session. | Total: 18 | -The sample further had clinically meaningful levels of generalized anxiety symptoms, measured by the Spielberger Trait Anxiety Inventory(TAI). | |
| Van Der Kolk et al. (2014) | Randomized controlled trial | The intervention was a 10-week trauma-informed yoga program consisting of breathing exercises, postures, and mindfulness meditation, offered as a weekly 1-hour class. | Total: 101 |
-Women with chronic, treatment-resistant PTSD -Adult women -Participants from the United States -Relatively well-educated women -Employed women |
|
| Participant age | Summary | Limitations | Main findings | ||
| 20-36.6 years | The study explores the delayed anxiolytic effect of acute aerobic exercise, the impact of exercise intensity and mode on state anxiety, and the need for further research on factors influencing state anxiety reduction post-exercise. | -The study should have thoroughly investigated the exercise mode as a determinant of the anxiolytic effect. -The sample size of 24 male university students may limit the generalizability of the findings. -The study did not explore the impact of age and gender on the anxiolytic effect of exercise. -The indirect estimation of submaximal target intensities could have confounded the results. -The study suggests further research to explore additional factors influencing the anxiolytic effects of exercise. |
-The study demonstrated a delayed anxiolytic effect of an acute bout of exercise, with a reduction in state anxiety observed 30 and 60 minutes following the cessation of exercise. -The association between state anxiety and exercise mode was not supported, indicating that differences in exercise mode did not significantly impact state anxiety levels. -The association between state anxiety and exercise intensity was not supported, suggesting that exercising at 75% predicted VO2 max did not result in lower post-exercise state anxiety levels than 50% predicted VO2 max. |
||
| 63.5 years | Yoga as an adjuvant treatment shows significant benefits in reducing symptoms of combat-related PTSD and improving the quality of life for military veterans. | -Small number of subjects - Unblinded approach to the investigation -Limited generalizability to younger populations -Lack of data on between-session practice and long-term retention of benefits -Lack of follow-up data -Lack of a double-blind approach |
Yoga intervention led to significant improvements in psychometric assessments, with reduced PTSD symptoms and a majority of participants achieving PCL scores below the diagnostic cut-off point. | ||
| 18–45 years | The research explores the feasibility of a high-intensity resistance exercise intervention for reducing post-traumatic stress symptoms in non-treatment-seeking adults with PTSD and anxiety, finding the intervention to be feasible and potentially beneficial, with further research needed to confirm the results. | -Small sample size -Unblinded assessor may introduce bias -Reliance on self-report measures instead of diagnostic interviews -Lack of a delayed follow-up period to assess long-term effects |
-High-intensity resistance exercise intervention was feasible and well-tolerated, with significant beneficial effects on symptoms of avoidance, hyperarousal, sleep quality, and hazardous alcohol use. | ||
| 40.11 years (mean) | The study evaluated the effects of a home-based exercise program on anxiety levels and metabolic functions in patients with anxiety disorders in Taiwan, showing significant improvements in various indicators and suggesting positive effects on both mental and physical health. | -The 3-month duration of the follow-up test may not capture all long-term effects -Reliance on self-report instruments could limit data accuracy |
The HB exercise program improved body mass index, high-density lipoprotein cholesterol levels, moderate exercise levels in the experimental group, and reduced state and trait anxiety levels. The program also positively impacted metabolic indicators and anxiety levels in Taiwanese adults with anxiety disorders. | ||
| 18–51 years | The study discusses the importance of anxiety sensitivity as a precursor to panic disorder. It also highlights the effectiveness of aerobic exercise as a treatment for anxiety disorders. It shows that high-intensity exercise leads to more rapid reductions in anxiety sensitivity compared to low-intensity exercise. | -Lack of assessment of participants' previous exercise experiences -Lack of assessment of perceptions of effort and physiological sensations experienced during exercise -Lack of assessment of changes in participants' exercise habits between post-treatment and follow-up -Limited generalizability due to strict selection criteria |
-Both high-intensity and low-intensity exercise reduced anxiety sensitivity, but high-intensity exercise led to more rapid reductions and had more treatment responders than low-intensity exercise. -High-intensity exercise was more effective in reducing fear of anxiety-related bodily sensations compared to low-intensity exercise. -The study highlights the potential of high-intensity aerobic exercise in reducing anxiety sensitivity and fear of anxiety-related sensations. |
||
| 19.19-20.12 mean years old in subgroup | The study discusses the prevalence of anxiety disorders, the benefits of physical exercise as an intervention for anxiety, and the effects of aerobic exercise and resistance training on anxiety sensitivity and CO2 reactivity. It also highlights the lack of observable effects on distress tolerance and discomfort intolerance. | -The study sample consisted of non-selected young adults, limiting the generalizability of the findings to at-risk or clinical populations. -The intensity of the exercise interventions was relatively homogenous and moderate, suggesting a need to explore the effects of a broader range of exercise intensities on anxiety vulnerability factors. -Further research is needed to investigate if resistance training exercises engaging larger muscle groups could have a more significant impact on anxiety sensitivity and other vulnerability factors. -Comparisons with other established treatments like CBT in varying dosages would provide insights into the efficacy of aerobic exercise and resistance training for anxiety-vulnerable populations. -Longitudinal studies of longer duration and follow-up studies are necessary to assess exercise interventions' long-term effects and durability on anxiety vulnerability factors. |
-Physical exercise is effective in reducing anxiety vulnerability factors like anxiety sensitivity (AS) and reactivity to CO2 challenges. -Both aerobic exercise and resistance training led to significant decreases in AS scores. -Aerobic exercise reduced reactivity to CO2 challenges more effectively than resistance training. -Neither exercise had observable effects on distress tolerance (DT) or discomfort intolerance (DI). |
||
| 41.03 years (mean) | The research demonstrates that high-intensity interval training (HIIT) is highly effective and fast-acting in treating generalized anxiety disorder (GAD), potentially complementing traditional treatment approaches. | -Small sample size -Lack of assessment of training-related exhaustion -Short follow-up period limits the ability to assess long-term efficacy |
-HIIT and LIT showed moderate to significant effects, with HIIT being about twice as effective as LIT. -HIIT was highly influential, fast-acting, and could complement first-line treatments for GAD. -Aerobic exercise was confirmed as a beneficial treatment option for GAD, showing significant effects on core symptoms and comorbid depression. |
||
| 18–30 years | The research examines the impact of exercise on state anxiety in young adults, highlighting the benefits of regular physical activity in managing stress. It focuses on the differences in anxiety reduction between high and low-anxious individuals through a nine-week exercise intervention. | -Predominantly female sample -Single-state anxiety measure post-exercise -Non-exercise control group -Lack of physiological data collection at each time point -Single measure of state anxiety change once per week The majority of participants were female. -Lack of measure of sedentary behaviour |
-The exercise group with high anxiety at baseline showed increased reductions in state anxiety following acute exercise as training progressed. In contrast, no significant training effects were observed for the exercise subgroup with low baseline anxiety. -Regular physical activity, particularly moderate-intensity aerobic exercise, was influential in managing state anxiety in young adults, with more significant reductions observed in individuals with higher levels of anxiety. |
||
| Patients: 31.9 years; Healthy control subjects: 30.8 years | The research demonstrates that a single bout of mild to moderate aerobic exercise has acute anti panic and anxiolytic effects, reducing panic attack frequency and CCK-4-induced symptoms in patients with panic disorder. This suggests a potential therapeutic application of exercise in managing panic disorder. | -The study did not investigate the duration of the protective effects of a single bout of exercise. -The study used a 30-minute exercise protocol, which may differ from longer durations used in other studies. -This study needed to fully characterise the optimum dosage (duration and intensity) and frequency of exercise treatment for panic disorder. |
-The study's main finding was that 30 minutes of mild to moderate aerobic exercise had an acute anti panic and anxiolytic activity, reducing panic attack frequency and CCK-4-induced symptoms. -The study suggests that a single exercise bout may be used in the treatment of panic disorder. -Further research is needed to determine the optimal dosage, duration, intensity, and exercise frequency for treating panic disorder. |
||
| 18–70 years | The research demonstrates that regular aerobic exercise provides an additional benefit to cognitive behavioural therapy in patients with panic disorder, leading to improved anxiety symptoms and increased effectiveness of treatment. | -Possible relaxation effects in the control group -Need for larger sample size and more sophisticated statistical strategies -Further research is needed to refine the design of the active control group |
Aerobic exercise had a significant anxiolytic effect and enhanced the effectiveness of cognitive-behavioural therapy in individuals with panic disorder, suggesting it as a promising additional therapeutic option. | ||
| 19–52 years | The research discusses a randomized controlled trial comparing the efficacy of aerobic exercise combined with paroxetine to relaxation combined with paroxetine or placebo in the treatment of panic disorder. While paroxetine was superior to placebo, aerobic exercise did not show significant differences from relaxation training in most efficacy measures. The paper concludes that regular aerobic exercise may still be a valuable tool in the treatment of panic disorder, especially for patients who are unwilling to take medication. | -The study design did not allow for actual double-blind conditions regarding exercise and relaxation. -The study did not show exercise superior to the control group, contradicting previous findings. -The study did not compare exercise directly to other established treatments like SSRIs or CBT. -The study did not include patients with significant depression, limiting the generalizability of the findings. -The study had a small sample size, which may affect the generalizability of the results. -The study did not investigate the long-term effects of exercise on panic disorder. -The study did not explore the potential interaction effects between exercise and medication. -The study did not assess the impact of exercise on different subtypes of panic disorder. |
Patients in all treatment groups showed improvement in primary and secondary efficacy measures, with paroxetine treatment demonstrating significantly better improvement than placebo. Regular aerobic exercise was not superior to relaxation training, but it can still be a helpful tool in combination with cognitive behavioural therapies for panic disorder. | ||
| 18–39 years | The research presents a randomized controlled trial demonstrating that exercise training, particularly resistance exercise training, is a feasible and effective short-term treatment option for reducing worry symptoms and promoting remission in sedentary women diagnosed with Generalized Anxiety Disorder (GAD), suggesting the need for further research in this area. | -Small sample size -Short treatment duration -Predominantly young-adult sample -Need for more and better clinical trials -Encouragement for continued investigation of mechanisms explaining antianxiety effects of exercise |
Exercise training, especially resistance exercise training (RET), can reduce worry symptoms among GAD patients and lead to higher remission rates than a waitlist control. RET and aerobic exercise training (AET) showed moderate reductions in worry symptoms. | ||
| 40.8–42.1 years (mean) | The paper demonstrates that a 12-week yoga intervention can effectively reduce psychological distress and improve PTSD symptoms in women who have experienced motor vehicle accidents. | -Small sample size -Evaluation of only one type of yoga, which may not be the most beneficial -Reliance on self-report data, which can be influenced by patient expectations and biases |
-The yoga intervention significantly reduced PTSD symptoms, anxiety, and depression in women who survived motor vehicle accidents. -The study showed that yoga had a positive impact on reducing intrusion and avoidance symptoms in women with PTSD following MVA. -The results suggest that a 12-week yoga practice can effectively reduce psychological distress in women with PTSD following MVA. |
||
| 18–45 years | The study demonstrates that yoga is associated with more significant improvements in mood and anxiety compared to walking, with positive correlations between increased thalamic GABA levels and improved mood/anxiety, suggesting a potential role of GABA in mediating the effects of yoga on mood and anxiety, warranting further research. | -Small sample size in the yoga group -Lack of significant increase in thalamic GABA levels in the yoga group -Potential limitation due to the use of a single MRI scanner -Lack of baseline differences between experienced yoga practitioners and controls in a previous study -The study did not explore the long-term effects of yoga intervention -The study did not investigate the effects of different types of yoga interventions -The study did not consider the potential impact of individual differences in response to yoga interventions |
-Yoga intervention led to more significant improvements in mood and anxiety compared to walking exercise -Increased thalamic GABA levels were associated with improved mood and decreased anxiety -Positive correlation found between acute increases in thalamic GABA levels and improvements in mood/anxiety scales |
||
| 22–40 years | The study discusses the perception of yoga as a stress management tool for alleviating depression and anxiety disorders, evaluates the influence of yoga on relieving symptoms of depression and anxiety in women, and concludes that participation in a two-month yoga class can significantly reduce anxiety levels in women with anxiety disorders, highlighting the effectiveness of yoga in managing and reducing stress. | -Limited to a female population -Small sample sizes -Lack of particular practice in the control group -Short study duration -Lack of mixed-gender sample |
Yoga is effective in reducing state and trait anxiety in women and can be considered as a complementary or alternative therapy for anxiety disorders. The potential of yoga in treating anxiety in women is significant and could be an important therapeutic option. | ||
| 16.4 to 49.2 years old for study participants, 24.1 to 43.7 years old for healthy controls | The study compares the effectiveness of Mindfulness-Based Stress Reduction (MBSR) and Aerobic Exercise (AE) in treating social anxiety disorder (SAD) in adults, finding both interventions to be equally effective in producing meaningful changes in symptoms and well-being. | -The study examined two alternative interventions for adults with SAD, and while they produced modest clinically significant changes, they did not reach the same level as traditional treatments. -The chronicity of SAD and the comparison to the untreated SAD group suggest that future research should continue to explore alternative interventions such as MBSR and AE for SAD. -Future research may benefit from examining the potential enhancement of treatment outcomes with a combination of MBSR and AE or the addition of MBSR or AE to traditional treatments for SAD. |
Both MBSR and AE were effective in reducing social anxiety and depression and increasing subjective well-being immediately post-intervention and at 3 months post-intervention. Participants in both interventions showed improvements in clinical symptoms and well-being compared to an untreated SAD group. | ||
| -Mean age of 36.9 years | The paper discusses the potential benefits of aerobic exercise for individuals with PTSD, highlights the need for further research to confirm these benefits, presents a study evaluating the effects of a brief aerobic exercise program on PTSD symptoms, and concludes that aerobic exercise may be a valuable adjunct to traditional psychotherapy for individuals with PTSD. | -Follow-up clinical interviews were not performed - Nearly half of the sample did not complete the monthly follow-up - Individuals with physical health conditions co-occurring with PTSD were excluded - Additional activity during the study was not controlled for - Study groups differed in fitness capacity - Absence of a nonactive control group |
-Regular aerobic exercise has mental health benefits for individuals with anxiety disorders and can reduce symptoms of PTSD. -Aerobic exercise was shown to significantly reduce PTSD symptoms over the treatment period and maintain these gains at one-month follow-up. -The study supports the clinical application of aerobic exercise for individuals with PTSD, indicating its potential as an adjunct to traditional psychotherapy protocols. |
||
| -The average age of the participants was 58 years, with a range from 24 to 80 years | The paper discusses the common symptoms of anxiety, depression, and fatigue in cancer patients and the potential of yoga therapy to alleviate these symptoms, emphasizing the need for further research to confirm the promising results. | -Based on an observational design -Causality cannot be attributed to yoga therapy -Small sample size -Elevated symptom levels not part of inclusion criteria -A high percentage of female participants -Generalizability limited by education levels -The therapy period may have been too short |
The main findings of the study include a significant reduction in symptoms of anxiety, depression, and fatigue six months after the end of yoga therapy compared to baseline. Additionally, most patients continued practicing yoga on their own, with many attributing benefits to helping with anxiety and concerns about the future. | ||
| - Young adults aged 18-40 | Ecologically valid resistance exercise training effectively improved AGAD status. It reduced worry and anxiety symptoms in young adults with elevated worry indicative of AGAD, suggesting it is a potential alternative or augmentation therapy for anxiety disorders. | -Small sample size -Lack of attention-matched control condition -Lack of follow-up assessment -Lack of time-matched control condition -Lack of anonymous clinical interviews assessing baseline AGAD status -Insufficient power for detecting small-to-moderate reductions in worry symptoms -Potential benefit from attention and social interaction in the RET intervention -Lack of exploration of sex-related response differences to RET and potential mediators/moderators of response -Lack of sustainability assessment for reductions in symptoms |
RET significantly improved AGAD status with a Number Needed to Treat (NNT) of 3 and led to significant reductions in worry and anxiety symptoms, supporting its efficacy as an alternative or augmentation therapy for anxiety disorders among young adults with AGAD. | ||
| 18-40 years | The article demonstrates the effectiveness of resistance exercise training in reducing depressive symptoms among young adults at risk for elevated depressive symptoms. The authors highlight RET as a promising treatment for mild or subclinical depression and as a potential intervention for individuals with clinically meaningful anxiety. | -Lack of an attention-control condition -Absence of post-intervention follow-ups -Need for long-term follow-ups to assess maintenance of depressive symptom reductions -Lack of control for the use of contraceptive medications -Unclear inter-individual variation in depressive symptom responses to RET -Small sample size for a pilot efficacy trial -Use of QIDS for diagnosing depression status in the AMDD sample -Uncertainty about the effect of RET on depressive symptoms among young adults with clinically meaningful MDD with or without comorbid GAD |
Resistance exercise training (RET) led to significant, clinically meaningful, and large-magnitude reductions in depressive symptoms among young adults, supporting RET as a promising treatment for mild depression, in alignment with WHO and ACSM guidelines. | ||
| 61.1 mean years old in Primary depression treatment group 57.6 mean years old in Primary GAD treatment group |
The article discusses the effective treatment of comorbid depression and generalized anxiety disorder in heart failure patients using cognitive behavioural therapy, exercise, and psychotropic medication, with significant improvements in symptoms observed. | -The study is an exploratory investigation not designed to prove treatment efficacy. -The use of anxiety questionnaires may have elicited more referrals for patients with comorbid GAD and depression. -The study may not reflect comorbidity rates in other earlier-stage CVD populations. -Depression and anxiety disorders are frequently under-recognized. -Treatment was not allocated according to a randomization process but based on consultation and patient preference. -The current HFSMP was only government-funded for one session per week. -Patients were excluded from the analyses if meeting the criteria for alcohol or substance abuse or personality disorders. -The sample size, low statistical power, width of standard deviations, and number of statistical analyses should be considered when interpreting the findings. |
-The primary GAD CBT group showed a significant reduction in PHQ symptoms compared to the primary depression CBT group. -Participation in the exercise program was associated with significantly reducing PHQ-somatic symptoms. -The primary GAD CBT group had a lower average number of cardiac hospital readmissions compared to the primary depression CBT group. |
||
| 25-64 years old | The paper discusses the efficacy of Sudarshan Kriya Yoga (SKY) in significantly reducing anxiety and depression scores in patients suffering from these disorders, with a focus on stable patients participating in the study. | -Need for replication on a more significant clinical sample in a controlled trial to further investigate the effectiveness of the SKY Protocol | -SKY therapy significantly reduces Anxiety and Depression scores, especially after the initial treatment, leading to a long plateau phase. -The study verified that SKY therapy in a controlled environment significantly reduces Anxiety and Depression levels in patients across different groups. -The reduction in scores is particularly evident after the initial intensive SKY treatment, followed by a gradual decrease towards null anxiety/depression scores. |
||
| 31.1 mean years old | The article discusses the commonality and impact of generalized anxiety disorder (GAD), the need for alternative interventions like yoga, the efficacy of Kundalini yoga for GAD, and the superiority of CBT as a first-line treatment for GAD. | -Findings may not generalize to community settings -Results for Kundalini yoga may not apply to all yoga types -Mediation analysis did not examine lagged associations |
The study's main findings indicate that both Kundalini yoga and CBT were more effective than stress education for treating generalized anxiety disorder, with CBT being superior to Kundalini yoga. (confidence: 90) | ||
| 20-46 years old | The study explores the impact of treatment preferences for CBT or yoga on outcomes and engagement in patients with Generalized Anxiety Disorder. | -predominantly White and well-educated sample, limiting generalizability -specific form of yoga used may not represent all types of yoga -differences in public perceptions of yoga versus structured class may have influenced results -inability to differentiate effects of preference versus intervention within subjects -suggestion for future use of doubly randomized preference control trials. |
-Both yoga and CBT were more effective than stress education in treating GAD, with CBT being more effective than yoga. Matching treatment preference did not significantly improve treatment outcomes, and dropout rates were higher for yoga compared to CBT. | ||
| 32.87 mean years old in MBSR group 32.88 mean years old in AE group |
The paper investigates the effectiveness of Mindfulness-Based Stress Reduction (MBSR) in reducing emotional reactivity and enhancing emotion regulation in patients with social anxiety disorder (SAD) compared to aerobic exercise (AE). It uses functional magnetic resonance imaging to study the neural correlates of attention regulation of negative self-beliefs. | -The study is limited to a single emotion regulation strategy and one type of anxiety-inducing probe, suggesting a need to compare multiple methods for different probes in future studies. -The fixed order of only four autobiographical situations may limit the generalizability of the findings, indicating the potential benefit of using a random sequence of more diverse life situations in future research. -Future analyses should explore whether baseline behavioural and neural signals during emotion regulation can predict the optimal treatment for individuals, suggesting a need for moderator analysis. -Further investigation into the underlying mechanisms of how MBSR and AE work, including whether changes in brain responses predict long-term clinical outcomes, is recommended, indicating the importance of mediator analysis. |
-MBSR led to more significant reductions in negative emotion and increases in attention-related brain regions compared to AE. -MBSR was associated with decreased emotional reactivity and increased behavioural self-regulation and emotion regulation. -Greater meditation practice in MBSR was linked to enhanced brain responses in attention regions. |
||
| 18–37 years old | Short-term exercise training improves sleep outcomes among GAD patients, especially for RET and weekend sleep. The study suggests that exercise can be an effective nonpharmacologic therapy for improving sleep in individuals with GAD. | -Small sample size -Low exercise dose, particularly for aerobic exercise training -Reliance on self-report diary measure of sleep -Lack of objective measurement of sleep -Need for future studies to explore more intense exercise stimulus and dose-response relations with sleep |
Short-term exercise training improves sleep outcomes among GAD patients, especially for resistance exercise training (RET) and weekend sleep. Improved sleep may be associated with reduced clinical severity among GAD patients. Exercise, particularly resistance training, can lead to significant improvements in sleep initiation, continuity, and reductions in time spent in bed and hypersomnia among young women with GAD. | ||
| 18-37 years old | The paper demonstrates that short-term exercise training, including resistance exercise training, can improve signs and symptoms associated with GAD, particularly irritability, anxiety, low vigour, and pain, highlighting the potential of exercise as a feasible treatment option for GAD. Further research is needed to explore the efficacy of exercise training compared to other treatments for GAD. | -Small sample size -Limited generalizability -Focus only on sedentary women -Lack of long-term follow-up -Absence of investigation into underlying mechanisms -Lack of comparison with other treatments |
Both RET and AET resulted in improvements in signs and symptoms associated with GAD, with RET showing significant reductions in anxiety-tension and irritability and larger effect sizes for various symptoms compared to AET. | ||
| Participants aged from 23 to 73 years. |
The study demonstrates that a 12-week exercise program, in addition to usual care, significantly improves mental health outcomes and physical health measures in in-patients with primary PTSD, supporting the use of structured exercise as an augmentation strategy for PTSD treatment. | -The study did not record potential confounding factors like chronic pain or fibromyalgia. -Data on pharmacological therapy were not recorded, which is acknowledged as a limitation. -Difficulty in accurately recording medication usage due to changes in regimes. -Variability in supervised session attendance due to the geographical location of the hospital. -Poor rate of exercise diary completion limited the exploration of dose-response associations. |
-The exercise intervention significantly reduced PTSD symptoms compared to usual care. -The intervention group showed improvements in depressive symptoms, waist circumference, sleep quality, and sedentary time compared to the usual care group. -The study demonstrated that a 12-week exercise program, in addition to usual care, can lead to improvements in both mental health outcomes and physical health outcomes for in-patients with primary PTSD. |
||
| Age range: 23–53 years, mean age 33.3 years |
The article examines how pre-treatment social anxiety severity moderates the impact of mindfulness-based stress reduction (MBSR) and aerobic exercise (AE) for generalized social anxiety disorder. The authors found that both interventions produced equivalent reductions in weekly social anxiety symptoms but were influenced by pre-treatment social anxiety severity levels. | -Small sample size for moderator analyses -Need for future studies with larger sample sizes to replicate and extend findings -Lack of examination of MBSR and AE within other anxiety disorders for generalizability -Lack of direct comparison of MBSR and AE to gold-standard treatments |
Pre-treatment social anxiety severity moderates the impact of mindfulness-based stress reduction (MBSR) and aerobic exercise (AE) on social anxiety symptoms. MBSR is more effective for patients with lower pre-treatment social anxiety severity, while AE is more effective for patients with higher pre-treatment social anxiety severity. Tailoring treatment recommendations based on pre-treatment social anxiety severity could enhance intervention effectiveness. | ||
| mean age of 36.9 years | The article discusses the therapeutic effects of aerobic exercise for individuals with PTSD and related disorders, supporting its clinical application for improving mental health outcomes. | -Follow-up clinical interviews were not performed -Nearly half of the sample did not complete the monthly follow-up -Individuals with physical health conditions co-occurring with PTSD were excluded -Additional activity during the study was not controlled for -Study groups differed in fitness capacity -Absence of a nonactive control group |
Regular aerobic exercise has mental health benefits for individuals with anxiety disorders and can reduce symptoms of PTSD. Aerobic exercise was effective in reducing PTSD symptoms over the treatment period and maintaining these gains at one-month follow-up. The study supports the clinical application of aerobic exercise for individuals with PTSD stemming from various traumas. | ||
| 32 years old | The article presents a case report where a patient with social anxiety disorder and paruresis-specific social phobia showed significant improvement after practising yoga and meditation under supervision, highlighting the potential benefits of yoga in such cases. | -Single case report limits generalizability -Lack of control group -Self-reported symptoms may introduce bias -Long-term effects not explored -Need for more extensive controlled studies for validation |
-Yoga practices led to significant improvements in multiple parameters related to Social Anxiety Disorder and paruresis, as evidenced by reduced scores on various scales and improved quality of life. | ||
| age range 18–50 years | Regular aerobic exercise alone is associated with significant clinical improvement in patients who have panic disorder, but it is less effective than treatment with clomipramine. | The short duration of the study (10 weeks) may not be sufficient to fully evaluate the effects of exercise. -Lack of actual double-blind conditions due to the nature of comparing a behavioural treatment approach with medication intake -Possibility of nonspecific effects such as increased social interaction contributing to the beneficial effect of exercise -The study does not address the long-term effects or risk of relapse associated with regular exercise in panic disorder -The study does not explore potential subgroups of patients who may respond preferentially to exercise -The study does not investigate the combination of exercise and drug treatment to assess potential potentiating of treatment effects |
The main findings suggest that exercise and clomipramine were effective in treating panic disorder, with clomipramine being more effective than exercise. | ||
| 58 (average) years old | The article explores the potential benefits of Sudarshan Kriya Yoga (SKY) in reducing symptom severity in Vietnam veterans with treatment-resistant PTSD, indicating that yoga breath techniques may offer a valuable adjunctive treatment for this population. | -small sample size -lack of blinding -use of a wait-list control -difficulty in determining responsible components of the intervention -need for more extensive studies with more diverse populations -challenges in adapting and disseminating multi-component yoga programs to veterans -difficulty in maintaining improvements due to lack of participant commitment |
-The study showed significant reductions in PTSD symptoms in both the SKY Intervention group and the Control group at the 6-month follow-up, indicating the potential benefits of the yoga intervention for veterans with chronic PTSD. | ||
| 20-65 years | The article discusses the impact of a yoga intervention on physical activity, self-efficacy, and motivation in women with PTSD symptoms, highlighting the importance of understanding the psychological mechanisms behind physical activity behaviour change. It also highlights the potential benefits of yoga on mental health. | -The study focused on women with subthreshold or full PTSD, limiting its generalizability to men or other mental health populations. -The study had a small sample size, which may have limited the ability to detect significant changes in relevant constructs. -The purpose of the parent study was to investigate the effect of the yoga intervention on PTSD symptoms and not necessarily to promote continued physical activity in participants. -The study may have lacked statistical power to detect medium effect sizes. -The study should have addressed the utility of other forms of physical activity beyond yoga, such as flexibility and strength training. -The study suggested that future research should aim to better understand the growth of psychological determinants during and after a yoga intervention to develop more targeted interventions for individuals with mental health disorders |
-The yoga intervention did not lead to significant changes in physical activity or self-efficacy but resulted in a substantial decrease in external motivation. -While there was a trend towards increased leisure-time physical activity in the yoga group, it did not reach statistical significance. -The control group significantly decreased amotivation scores during the study. |
||
| 18-35 years old | The article provides compelling evidence that yoga can significantly improve anxiety symptoms and quality of life in individuals with panic disorder, offering a valuable complementary or alternative approach to traditional treatments. | -Participants were all diagnosed with panic disorder and recruited from a single location, limiting generalizability. -Further research with more extensive and diverse samples is needed to confirm the generalizability of the findings. -Lack of investigation into the specific mechanisms by which yoga reduces anxiety and improves quality of life. |
The yoga group exhibited a significant reduction in anxiety levels and improvements in quality of life compared to the control group, suggesting yoga is a valuable complementary or alternative approach to traditional treatments for anxiety disorders. | ||
| 18-60 years old | The study explores the therapeutic benefits of yoga in reducing panic-related symptoms in patients with panic disorder, both when practised alone and in combination with cognitive-behavioural therapy. | -Need for further research to explore the mechanisms through which mind-body practices improve mental health -Transparency regarding potential conflicts of interest |
The study demonstrated significant reductions in anxiety levels, panic-related beliefs, and panic-related body sensations in patients with panic disorder, with the combination of yoga and CBT showing more significant improvements compared to yoga alone. | ||
| ≥18 years of age | The study is a feasibility trial that aimed to determine the feasibility, acceptability, and preliminary efficacy of a 12-week home-based, online yoga intervention with varying doses for women who have experienced stillbirth. Results showed significant decreases in PTSD and depression and improvements in self-rated health at post-intervention. | -Inconsistencies with the software used to track participation -Sample not necessarily representative of the population of women who have had stillbirths in the US -High number of dropouts -The study was a feasibility study, and the sample size was not powered to determine the efficacy |
The study found significant decreases in PTSD and depression and improvements in self-rated health at post-intervention for both intervention groups, with the moderate dose group reporting the prescribed minutes of yoga to be too much. There was also a significant difference in depression scores and grief intensity between the moderate dose and control groups. | ||
| 22.1 mean years old | The study investigates the efficacy of yoga for improving cognitive and physical anxiety symptoms in high-anxious women, exploring the possible dissociation between mental and physical symptoms of anxiety among women with anxiety sensitivity. It also aims to assess the immediate and delayed anxiolytic effects of yoga in response to an anxiety-inducing CO2-inhalation task in women with high anxiety sensitivity. | -Small sample size -Control condition might not have been the most appropriate choice -Lack of comparison between individuals with high vs low AS |
-The study did not find significant differences between the effects of yoga and light stretching on anxiety symptoms. -Physical activity, regardless of the specific type, showed an overall reduction in cognitive anxiety symptoms. -The study suggests a dissociation between cognitive and physical symptoms of anxiety in women with anxiety sensitivity |
||
| 18-58 years old | The study demonstrates that a 10-week, weekly yoga program can significantly reduce PTSD symptoms in women with chronic treatment-resistant PTSD, highlighting the importance of body awareness and somatic regulation in the treatment of PTSD. | -Need for replication with different populations and in various cultural settings -Further investigation into the mechanisms of mindfulness meditation and their extension to yoga -Importance of dismantling the components of yoga to study their specific contributions |
Yoga significantly reduced PTSD symptomatology in women with chronic treatment-resistant PTSD, with effect sizes comparable to traditional psychotherapeutic and pharmacologic approaches. | ||
4. Virtual Reality (VR)
4.1. PTSD
4.2. SAD
4.3. GAD
4.4. Phobias
| Author, year of publication | Study design | Intervention | Participant count | Population characteristics |
| Mclay et al. (2014) |
Retrospective observational study, non-controlled, single-site | Virtual Reality Graded Exposure Therapy (VR-GET) consists of weekly to biweekly sessions with a psychologist, with a fixed number of sessions (5, 10, 15, or 20) in the open-label study and a fixed 10-week treatment duration in the randomized trial. The therapy included graded VR exposure, physiologic monitoring, and skills training. | Total: 28 | -Active-duty service members -Participants with PTSD related to service in Iraq or Afghanistan -Participants who completed neuropsychological testing and self-report measures of PTSD, depression, and generalised anxiety |
| Beidel et al. (2017) |
Randomized controlled trial | Trauma Management Therapy (TMT) with Virtual Reality Exposure Therapy (VRET) was conducted three times per week for five weeks, followed by group treatment twice-weekly for the first two weeks and then once weekly, totalling 43.5 hours of treatment for each patient. The individual exposure therapy component of TMT used an intensive flooding approach. | Total: 92 |
-Iraq and Afghanistan veterans and active duty military personnel with combat-related PTSD |
| Anderson et al. (2013) |
Randomized controlled trial | Virtual Reality Exposure Therapy (VRE) for 8 sessions with up to 120 minutes of exposure and Exposure Group Therapy (EGT) for 8 sessions with up to 120 minutes of exposure. | Total: 97 | Participants with social anxiety disorder, mostly women, ethnically diverse sample, the majority reported completing college, 43.2% reported an annual income of $50,000 or more, 43.2% reported being “married”, the majority did not have a comorbid diagnosis |
| Anderson et al. (2005) |
An open clinical trial with a treatment manual, homogenous inclusion/exclusion criteria, independent assessment, and a behavioural avoidance test | Cognitive-behavioural treatment using virtual reality for exposure therapy for eight sessions, including anxiety management training and exposure therapy using a virtual audience. | Total: 10 | -Predominantly female -Married -Well-educated -Middle-to-upper class -Self-identified as either Caucasian or African-American -Met criteria for social phobia or panic disorder with agoraphobia -Most participants met the criteria for another anxiety disorder |
| Bouchard et al. (2016) |
Randomized controlled trial | Individual CBT with exposure either in virtuo or in vivo for 14 weekly 60-minute sessions. Therapists were graduate students experienced in CBT for anxiety disorders. | Total: 59 |
-French-speaking individuals -Aged 18 to 65 years diagnosed with SAD according to DSM-5 criteria, excluding those with specific conditions or receiving concurrent psychotherapy. |
| Rubin et al. (2021) |
Randomized Controlled Trial | VRET with attention guidance training (AGT) -two 45-minute sessions over one week, including psychoeducation, public speaking exposures, and specific instructions to focus on audience members' faces with feedback on gaze behaviour. | Total: 21 |
-Participants were fluent in English -Participants had a Personal Report of Public Speaking Anxiety > 98 -Participants had a Leibowitz Social Anxiety Scale > 30 -Participants had a Peak fear ≥ 50 on the behavioural approach task during the baseline public speaking challenge -Participants met DSM-5 Criteria for Social Anxiety Disorder |
| Pitti et al. (2015) |
Randomized controlled trial | CBT for 11 sessions, Paroxetine at a mean dose of 22.60 mg/day, Virtual reality exposure for 4 sessions, in addition to CBT sessions | Total: 99 | -Patients with agoraphobia, mostly female -Mostly having agoraphobia with panic disorder The majority of patients were chronic cases. -Exclusion criteria included psychotic symptoms, bipolar disorders, high suicide risk, heart disease, neurological disease, or ophthalmologic disease |
| Kim et al. (2022) |
Randomized controlled trial | Eight sessions of virtual reality self-training (VRS) over 2 weeks in three different environments with increasing difficulty levels. | Total: 52 |
Participants were diagnosed with SAD according to DSM-5 criteria, with a Liebowitz social anxiety scale-self report (LSAS) score of more than 30. |
| Zainal et al. (2021) |
Randomized controlled trial | Self-guided VRE for social anxiety disorder, including exposure scenarios related to an informal dinner party and a formal job interview, with increasing levels of anxiety-inducing situations, along with between-session in vivo exposure therapy homework. The VRE included a virtual therapist, SUDS ratings, and cutting-edge technology. Sessions were held twice a week for 50–60 minutes each. | Total: 44 |
-Majority female (77.3%) -Diverse racial and ethnic backgrounds -Varied educational attainment |
| Malbos (2013) |
Randomized Controlled Trial | VRET alone for one group and VRET combined with cognitive therapy for another group. VRET sessions involved exposure to nine different virtual environments related to agoraphobic fears for 50–60 minutes each. Cognitive therapy for the combined group included psychoeducation, anxiety acceptance, cognitive restructuring, positive self-statements, and relapse prevention. Participants were instructed not to practice voluntary self-exposure between sessions. | Total: 19 |
-Participants were predominantly Caucasian -Mix of educational backgrounds -Most were married or in a de facto relationship, and most worked or studied full-time. -Some participants had co-morbid disorders such as major depression, social phobia, and specific phobia. |
| Powers et al. (2013) |
within-subjects incomplete repeated measures design with random starting order and rotation counterbalancing | Participants conversed with an actor/operator in either VR or in vivo environments. The VR conversation involved using a virtual environment through a stereovision head-mounted display (HMD) and noise-cancellation headphones. The facilitator used a microphone headset to speak with the participant. | Total: 26 |
-The study included 26 undergraduate participants, primarily females (73.1%). -The majority of participants were Non-Hispanic White (76.9%), with smaller percentages being Black (11.5%), Hispanic (7.7%), and Asian (3.8%). -Participants were recruited from an undergraduate psychology course and received extra credit for their participation. -Participants scored similarly to college students in previous studies on measures of social anxiety and general anxiety. |
| Wang et al. (2020) |
randomized controlled trial | Participants with GAD were randomly assigned to either a virtual nature (VN) or a virtual abstract painting (VAP) group. | Total: 77 | -Participants with GAD -Normal body mass index (BMI) between 18.5 and 24 kg/m2. |
| Wald et al. (2003) | Case study | Three sessions of VRET after a 7-day baseline | Total: 7 | - Seven adults with a specific phobia diagnosis, consisting of six females and one male, all possessing valid driver's licenses, reporting a longstanding history of driving fear and avoidance, with three participants having a history of being in a motor vehicle accident. |
| Kampmann et al. (2016) | Randomized controlled trial | Participants received VRET or iVET for ten 90-minute sessions scheduled twice weekly, without any homework assignments and with exposure elements based on protocols without cognitive components. | Total: 60 |
Participants diagnosed with social anxiety disorder, 63.3% women, were recruited through various sources; exclusion criteria included factors like recent psychotherapy for SAD, current use of certain medications, history of psychosis, current suicidal intentions, substance dependence, severe cognitive impairment, and insufficient command of the Dutch language. |
| Tortella-Feliu et al. (2010) | Randomized trial | Virtual Reality Exposure Therapy (VRET), Computer-aided exposure with a therapist (CAE-T), Self-administered computer-aided exposure (CAE-SA) | Total: 60 | -Diverse community-based sample -Participants with specific phobia related to fear of flying -Participants meeting DSM-IV criteria for specific phobia |
| Participant age | Summary | Limitations | Main findings | |
| 34.07 average years old | The study investigates the effectiveness of Virtual Reality Graded Exposure Therapy (VR-GET) on PTSD, depression, anxiety, and neuropsychological functioning, showing significant reductions in PTSD and anxiety severity and improvements on the emotional Stroop test, but no significant changes in depression or other neuropsychological measures. | -Participants were allowed to decline neuropsychological testing, potentially affecting the completeness of the data. -The small sample size may have limited the ability to detect relationships between PTSD and neuropsychological impairment consistently. -Larger studies are needed to determine the efficacy of the treatment modality in other areas. -The study suggests that VR-GET may be more effective for treating PTSD specifically. |
-VR-GET treatment led to significant reductions in PTSD and anxiety severity, along with improvements in the emotional Stroop test. -Changes in the emotional Stroop test did not correlate with changes in self-reported PTSD symptoms. -The study supports the use of VR-GET as a treatment for PTSD, indicating benefits may be focused on specific areas. |
|
| 37.67 mean years old in TMT group 33.26 mean years old in EXP group |
The article demonstrates the effectiveness of VRET in significantly reducing PTSD symptoms, with positive results maintained at the six-month follow-up. | -Dropout rate differences between TMT and EXP groups -Baseline differences despite randomization -Lack of comparison with different exposure models |
-VRET resulted in significant decreases in PTSD symptoms as assessed by the CAPS and PCL-M. -TMT, which includes VRET plus a group treatment for anger, depression, and social isolation, showed additional benefits in enhancing social and emotional functioning compared to VRET plus a psychoeducation control condition. -Both VRET and TMT led to significant decreases in depression and anger, with TMT specifically enhancing social functioning. Both interventions: -All treatment gains were maintained at the six-month follow-up. -42%-50% of each group demonstrated reliable and clinically significant changes in PTSD symptoms, with all but one participant showing at least reliable change. The relapse rate was meager at 4.5%. |
|
| 19-69 years old | The article compares VRET to exposure group therapy and a waitlist for social anxiety disorder, showing significant improvements in both active treatments compared to the wait list, with virtual reality exposure therapy being equally effective as exposure group therapy. | -Difficulty in equating two treatments delivered in different formats -Need for comparison with another individually administered treatment to equate factors -Challenge in comparing similar treatments delivered across different modalities -Limited generalizability due to specific inclusion criteria -Lower comorbidity rate in the sample compared to typical individuals with social anxiety disorder -Underrepresentation of ethnic/racial diversity in treatment efficacy research |
-Virtual reality exposure therapy effectively treats social fears and maintains improvement for at least 1 year. -Virtual reality exposure therapy is equally effective as exposure group therapy. -Virtual reality exposure therapy is effective for reducing symptoms of social anxiety disorder and public speaking fears, with changes in behavior observed in the real world. -Improvement in fear of negative evaluation was not immediate post-treatment but was observed at follow-up. -Both virtual reality exposure therapy and exposure group therapy showed similar improvements across various outcome measures and process variables. |
|
| not mentioned | The study discusses a study that used CBT with virtual reality (VR) for exposure therapy to treat public-speaking anxiety, showing significant improvement in self-report measures of public-speaking anxiety post-treatment and at follow-up. | -Should not include individuals whose primary diagnosis is panic disorder -The addition of physiological monitoring would improve the assessment -Future work could isolate the effect of VR on treatment response -Disadvantages include cost and the inability of the VR to match the idiosyncratic fears or elicit anxiety for some patients |
-Participants experienced significant reductions in public-speaking anxiety post-treatment, with maintained improvements at follow-up. -Most participants showed improvement in fear of public speaking measures and reported feeling significantly better and satisfied with the treatment. -Audience members rated participants as performing better and less anxious at post-treatment compared to pre-treatment. |
|
| 18–65 years old | The study discusses the advantages and effectiveness of using virtual reality in CBT for social anxiety disorder, highlighting the positive outcomes of CBT with virtual exposure compared to traditional CBT. | -Lack of clinical evaluations by independent assessors -Study focused on individual CBT, not group format -Need for replication with a larger sample -In vivo exposures did not precisely match in virtual scenarios |
-CBT with in virtual exposure and in vivo exposure showed improvements in primary and secondary outcome measures compared to the waiting list. -Conducting exposure in VR was more effective than in vivo exposure on specific outcome measures. -VR was significantly more practical for therapists than in vivo exposure. |
|
| 18–65 years old | The study discusses the development and testing of a VRET protocol for social anxiety disorder, focusing on modifying visual attention and gaze patterns during exposure therapy. Results show a reduction in fear of public speaking and general symptoms of social anxiety across both intervention groups. | -Lack of a non-socially anxious group at baseline for comparison -Absence of assessment of presence during treatment, potentially impacting efficacy -Clinicians not being blind to the treatment condition during follow-up assessments -Potential limitation of non-interactive public speaking challenges in the efficacy of social exposures |
-Attention can be modified within and during VRET. -Modifying visual gaze avoidance may be causally linked to reduced social anxiety. -The intervention had a significant overall effect on symptoms of social anxiety. |
|
| 39 mean years old | The study compares the efficacy of different treatments for agoraphobia, with combined treatments showing more significant improvements overall. Still, the superiority of virtual reality exposure in combination with therapy remains uncertain. | -Difficulty in determining phobic stimuli for each individual -Lack of determination of differential efficacy in groups not treated with psych drugs -Uncertainty regarding efficacy based on the acute or chronic nature of agoraphobia -Need for further data to confirm differential efficacy |
-Combined treatments involving both psychological therapy and psychodrug therapy were more effective in reducing agoraphobia symptoms compared to treatment with psychodrugs alone. -Virtual reality exposure showed more significant improvement in confronting phobic stimuli, but doubts remain about its superiority over traditional psychological treatments. -At follow-up, both combined treatment groups continued to improve over time, with no significant differences. |
|
| 19–30 years old | The study discusses virtual reality self-training (VRS) as a potential tool to reduce social anxiety in individuals with SAD before formal treatment. It highlights improvements in attention to social stimuli and emotional cues based on functional changes in the visual cortices and thalamus. VRS is suggested as a first intervention option for individuals with SAD who avoid society or are reluctant to receive formal treatment. | -Small sample size -Lack of a healthy control group -Insufficient evidence to support the interpretation of negative bias due to the lack of valence ratings on the faces used in the task -Order effects due to the tasks not being counterbalanced - Potential influence of regular visits to the VR clinic on the results |
-The VRS program led to significant improvements in anxiety, avoidance, distress, and negative self-evaluation for the self, associated with functional changes in the visual cortices and thalamus. -No changes were observed in regions related to negative self-beliefs in the fMRI results. |
|
| 18–53 years old | The study tests the efficacy of self-guided virtual reality exposure therapy for SAD in comparison to a waitlist control group, demonstrating significant reductions in SAD severity, job interview anxiety, and trait worry. This results in promising outcomes for the use of self-guided VRE as a potential treatment for individuals with SAD. | -Small sample size -Use of a waitlist control group could inflate effect sizes -Lack of a behavioral avoidance task to assess the real-life transfer of VRE gains -Potential benefit from human contact with research assistant |
-The self-guided VRE was effective in reducing SAD severity, job interview anxiety, and trait worry compared to the waitlist control group, with moderate-to-large effect sizes. | |
| 24–72 years old | The study evaluates the independent effect of VRET for agoraphobia compared to VRET combined with cognitive therapy. | -Participants were well-educated, which may not represent the general agoraphobic population. -The small sample size limited the ability to conclude group differences. -Lack of a waiting list group and an in vivo exposure group limits the ability to determine the absolute efficacy of the treatments. |
-VRET showed a positive effect on agoraphobia symptoms. -Cognitive therapy did not provide significant additional benefits. -The isolated effects of VRET were not significantly less than those of combined VRET with cognitive therapy. -No significant differences between the two groups were found at the 3-month follow-up. |
|
| 20.42 mean years old | The study explores the use of virtual reality technology for exposure therapy in social anxiety, showing that VR conversations increased fear ratings compared to baseline and in vivo conversations, indicating potential usefulness for future treatment of social anxiety. | -Participants were not selected based on social anxiety scores for this feasibility pilot study. -Presence would be enhanced if participants did not meet the facilitator/actor controlling the avatar before the conversation and if the actor also controlled the avatar from another room. -Small sample size does not permit analysis of multiple dimensions of presence. -The study does not indicate if real-time interaction is superior to standard VRET for social anxiety. -Participants were given course credit, which may affect generalizability. -Control over the actor's use of facial expressions, gestures, and gaze was not verified. -Future studies should incorporate additional measures of distress. -Future studies may help determine the optimal content choices for social anxiety exposures. -Habituation/extinction could not be measured, as participants only completed each conversation condition once. |
-VR conversations elicited higher fear ratings compared to in vivo conversations. -In vivo, conversations were rated as more realistic than VR conversations. -The technology allowing real-time interaction in VR may be beneficial for treating social anxiety in future studies. |
|
| 50–75 years old | The study explores the effects of virtual exercise therapy on patients with generalized anxiety disorder, comparing the impact of natural landscapes versus abstract paintings on stress relief, restorative quality, and satisfaction levels. | -The study only examined the effects of a single 20-minute virtual exercise period on psychological responses in patients with GAD without considering the impact of long-term exercise. -The study used a 270-angle virtual environment instead of a 360-angle virtual environment, potentially limiting the degree of immersion experienced by participants. -The psychological responses to an acute bout of exercise might be moderated by age, and the study only included middle-aged and older participants, suggesting a need for further research on different age groups in patients with GAD. |
-Patients with GAD experienced higher levels of stress relief, restorative quality, and satisfaction when exercising in a virtual environment with natural landscapes compared to abstract paintings. -Both groups showed increased alpha activity post-exercise, indicating a more relaxed state after cycling in the virtual environment. -The study suggests that exercising in a virtual natural environment can be an effective method to address clinical psychological and psychological issues in patients with GAD. |
|
| 31-57 years old | VRET shows promise in treating driving phobia by reducing anxiety and avoidance symptoms, though additional in vivo exposure therapy may be needed for some individuals. | -Cost-effectiveness due to the current cost of virtual reality technology -Limited accessibility to therapists and clients -Lack of realism for some individuals -Inability to target specific individual driving fears effectively -Insufficiency of VRET as a standalone treatment for all patients -Recommendation for VRET to be used as an initial step followed by in vivo exposure therapy -Need for further research on the effectiveness and limitations of VRET |
-VRET showed promising results in reducing driving anxiety and avoidance in individuals with driving phobia. -The efficacy of VRET was demonstrated through improvements in phobic-related symptoms, decreased peak anxiety, and the elimination of diagnostic criteria for driving phobia in some patients. - While VRET may not be sufficient for all patients, it could be a valuable initial step in treatment, followed by in vivo exposure therapy. |
|
| 18-65 years old | The study investigates the efficacy of VRET as a standalone treatment for individuals with SAD by simulating social verbal interaction in various virtual social situations relevant to treating individuals with SAD. The study includes 60 participants with a mean age of 36.9 years, predominantly women, who were randomly assigned to VRET, individual in vivo exposure therapy (iVET), or a waiting-list control group. The results suggest that VRET with extensive verbal interaction can effectively reduce complaints of generalized social anxiety disorder. | -Absence of homework exercises in both treatment conditions -Social situations in exposure exercises were not identical in both treatment conditions -Need for improvement in technological and psychological aspects of virtual social interactions |
The main findings include the effectiveness of both VRET and iVET in reducing various symptoms of social anxiety, with iVET showing more significant improvements in certain areas compared to VRET. | |
| 38 mean years old in CAE-T group 36.24 mean yeras old in CAE-SA group 36.89 mean yeras old in VRET group |
The study compared the efficacy of three computer-based exposure treatments for fear of flying (VRET, CAE-T, CAE-SA) and found them all effective in reducing fear of flying, with no significant differences between them. The results suggest that therapist involvement can be minimized during computer-based treatments. | -Small number of participants in each treatment condition - The absence of a behavioral avoidance test at the initial assessment. - The absence of a control group. |
-The three computer-based exposure treatments were equally effective in reducing fear of flying, with no significant differences. The self-administered treatment (CAE-SA) did not have higher attrition rates, indicating good acceptability and adherence. The study suggests that therapist involvement can be minimised during computer-based therapies. | |
5. Mindfulness
5.1. MBI and Classical Treatment
5.2. SAD
5.3. GAD
5.4. Conclusion
| Author, year of publication | Study design | Intervention | Participant count | Population characteristics | |
| Hoge et al. (2017) | Randomized, controlled, parallel design, non-blinded, prospective clinical trial | MBSR intervention included 8 weekly group classes, a retreat day, and daily home practice assignments guided by audio recordings, including breath awareness, body scan, and gentle Hatha yoga. Stress Management Education (SME) was didactic and provided information on stress-related topics like time management, nutrition, exercise, and sleep. | Total: 57 | -Individuals with Generalized Anxiety Disorder (GAD) -56% women - Inclusion criteria based on DSM-IV criteria for GAD and HAMA score of 20 or above -No significant differences in gender, race, or age between treatment groups |
|
| Kim (2010) |
Non-controlled trial with pre-post design | MBCT program for panic disorder patients, consisting of eight weekly sessions lasting about 90 minutes each. | Total: 31 | -Patients with panic disorder -Gender distribution: 57% male, 43% female -Mean duration of illness of 22.4 months -Mean educational level of 14.0 years -Marital status: 70% married, 30% unmarried -Occupational status: 44% employed, 56% unemployed -Religion: 52% declared, 48% undeclared |
|
| Sado et al. (2018) |
Single-arm study with a pre-post comparison design | Participants received an 8-week MBCT program consisting of meditation, yoga, sharing experiences, psychoeducation, and daily home practice, led by a psychiatrist and a nurse/clinical psychologist, with modifications for anxiety disorders. The program included 8 weekly 2-hour-long sessions and 2 monthly boosters. | Total: 14 | -Female: 71.4% -Average treatment duration at the start of the intervention: 13.4 years -Pharmacotherapy rate: 93% (71.4% antidepressants, 50.0% benzodiazepines) |
|
| Jiang (2022) |
Randomized, controlled, noninferiority trial with blinding and computer-generated randomization | Participants received either Mindfulness-based cognitive therapy adapted for treating GAD (MBCT-A) or Cognitive behavioral therapy designed to treat GAD (CBT-A). MBCT-A involved individual precourse orientation, 8 weekly group classes, one "retreat in silence" day, daily homework guided by audio recordings, and various mindfulness practices. CBT-A is aimed at changing or challenging dysfunctional thoughts related to generalized anxiety and introducing participants to various relaxation techniques. | Total: 138 | -Adult patients with GAD -24.6% of screened participants were successfully recruited -17.9% did not attend any intervention sessions -84.1% and 81.2% attendance rates for MBCT-A and CBT-A groups, respectively |
|
| Goldin et al. (2010) |
Pre-post intervention study design | MBSR intervention: 2.5-hour once-weekly small-group format for eight sessions, plus one half-day meditation retreat, with meditation CDs for home practice and daily monitoring form for recording practices. Participants attended most classes and completed several weekly hours of home meditation practice. | Total: 16 | Patients diagnosed with SAD according to DSM-IV criteria, with a diverse racial background and college-educated, middle-aged individuals. |
|
| Goldin et al. (2016) |
Randomized controlled trial, controlled, longitudinal, diagnostic study design, ethical considerations | Cognitive-Behavioral Group Therapy (CBGT) and Mindfulness-Based Stress Reduction (MBSR) | Total: 108 |
-55.6% female -The racial distribution of the population was 43.5% Caucasian, 39% Asian, 9.3% Hispanic, and 8.3% other ethnicities -Patients met the criteria for a principal diagnosis of SAD based on the DSM-IV-TR and the ADIS-IV-L |
|
| Koszycki et al. (2007) |
Randomized controlled trial | MBSR: 8-week mindfulness-based stress reduction program based on mindfulness meditation practices. CBGT: 12 weekly sessions of cognitive-behavioral group therapy. |
Total: 68 |
-Patients with DSM-IV SAD -Mixed-gender distribution -Presence of concurrent psychiatric disorders and medication use -Variability in the age of onset of SAD between treatment groups |
|
| Shikatani et al. (2014) | Randomized controlled trial | Cognitive restructuring and mindfulness strategies, each lasting approximately 40 minutes | Total: 56 | - Majority female participants - Age range from 17 to 53 years with a mean age of 24.5 years - Diverse ethnic and cultural background, with the majority being White/European - Exclusion of individuals with a history of CBT or mindfulness-based treatment |
|
| Koszycki et al. (2016) | Randomized controlled trial | Mindfulness-Based Intervention for Social Anxiety Disorder (MBI-SAD) with 12-weekly 2-hour group sessions, led by a psychologist, including psychoeducation, formal mindful meditations, mindful exposure, and compassion-based meditations. | Total: 39 | -Participants were men and women aged 18 years and older -Exclusion criteria included a history of psychosis, bipolar disorder, substance use disorders, psychotic features of affective disorder, and high suicide risk -Comorbidities were allowed as long as SAD was the primary disorder -Participants with depressive disorders scoring 24 or higher on the Montgomery-A ˚sberg Depression Rating Scale were excluded -Participants with an established meditation practice or regular yoga practice were excluded |
|
| Koszycki et al. (2020) | Participants received either a Mindfulness-Based Intervention for Social Anxiety Disorder (MBI-SAD) or Cognitive Behavioral Group Therapy (CBGT) for 12 weekly group sessions. The MBI-SAD included elements from Kabat-Zinn's MBSR curriculum, psychoeducation, mindfulness orientation, mindful attitudes review, raisin exercise, body scan, mindful exposure, and compassion-based meditations. Sessions were structured with homework assignments, cognitive restructuring, self-directed exposure, in-session exposures, and subsequent week's homework. The MBI-SAD sessions are led by qualified therapists. Participants engaged in formal meditation practice for an average of 4.97 days per week. | Total: 97 |
-Participants with at least moderately severe social anxiety symptoms The majority of participants were medication-free -A significant portion of participants had received counseling or psychotherapy in the past |
||
| Wong et al. (2016) | Randomized Controlled Trial (RCT) | 8-week mindfulness-based cognitive therapy (MBCT) course and psychoeducation based on CBT principles, involving weekly 2-hour sessions with up to 15 participants and daily homework exercises. | Total: 182 | -Majority of women (79%) -Participants diagnosed with GAD and scored 19 or above on the Beck Anxiety Inventory - Participants needed to understand Cantonese |
|
| Spinhoven et al. (2022) | Pragmatic randomized controlled trial | Mindfulness-Based Cognitive Therapy (MBCT) in 8 weekly 2-hour group sessions consisting of 4–8 participants, with homework assignments between sessions covering various topics. | Total: 136 |
- Mean age of 40.8 years, with a range from 18 to 73 - 58.1% female participants - Most prevalent anxiety disorders: panic disorder, obsessive-compulsive disorder, generalized anxiety disorder - Nearly half had a single anxiety disorder, 25% had two or more - No significant differences in sociodemographic or clinical variables between MBCT and CBT-RP participants |
|
| Participant age | Summary | Limitations | Main findings | ||
| -Mean age 39 years | The study explores the impact of mindfulness meditation on occupational functioning and healthcare utilisation in individuals with GAD, highlighting its potential benefits and discussing possible mechanisms of action. | -Small sample size -Reliance on self-report measures -High drop-out rate during the follow-up period -High variability in absenteeism rates -Study not powered to detect significant differences in work-related outcomes -Post-hoc correction for the main result was needed |
-Participation in MBSR was associated with a significant decrease in partial work days missed for adults with GAD -Greater home mindfulness meditation practice among MBSR participants was linked to less work loss and fewer mental health professional visits. -Mindfulness meditation was found to have a beneficial effect on occupational functioning. |
||
| -Mean age 41.2 years | The study discusses the effectiveness of MBCT as an adjunct to pharmacotherapy in treating patients with panic disorder, showing improvements in anxiety assessments, panic disorder severity, anxiety sensitivity, phobia, and worry. It suggests that MBCT can affect the clinical course of panic disorder by improving key factors, and concludes that further studies are needed to confirm these findings. | -Small sample size -Non-controlled study design -Absence of reporting the Mindful Attention and Awareness Scale (MAAS) -Uncertainty regarding the significant improvement of anxiety in panic disorder patients derived from pharmacotherapy or MBCT |
-HAM-A and PDSS scores significantly decreased at the 2nd, 4th, and 8th weeks compared to baseline, indicating a reduction in anxiety symptoms in patients with panic disorder -The Panic Disorder Severity Scale (PDSS) scores significantly reduced throughout the MBCT program, suggesting an improvement in the core symptoms of panic disorder -Anxiety assessments such as HAM-A and BAI were significantly improved after the MBCT program, aligning with previous studies showing the effectiveness of MBCT in relieving anxiety symptoms |
||
| -Mean age: 45.0 | The study evaluates the feasibility and effectiveness of MBCT for anxiety disorders in a Japanese setting, demonstrating statistically significant improvements in the State-Trait Anxiety Inventory (STAI)- state at every evaluation point. | -Small sample size -Inability to conduct subgroup analyses between different types of anxiety disorders -Lack of generalizability due to the small sample size and single-arm pre-post design -Need for future randomized controlled studies to accurately evaluate effectiveness |
-The study involved 14 patients with anxiety disorders, showing statistically significant improvements in the State-Trait Anxiety Inventory (STAI)-state at every evaluation point. -Significant improvements were observed in disease-specific scales, with the MIA (AAC) score showing significant improvements at the 2-month follow-up. -The MBCT intervention demonstrated sustained efficacy post-treatment, with significant improvements in both STAI-state and STAI-trait, indicating potential for addressing anxiety symptoms from early stages. |
||
| -Mean age 35.94 years | The study compares the efficacy of group mindfulness-based cognitive therapy (MBCT-A) with group cognitive behavioural therapy (CBT-A) for treating GAD and finds that MBCT-A is noninferior to CBT-A in improving symptoms of anxiety in GAD patients. | - Lack of a no-treatment control or wait-list control - Failure to record specific reasons for screen failure during recruitment - Absence of data collection on mindfulness exercises in the MBCT-A group or behavior exercises in the CBT-A group. Unclear which components of the interventions led to positive effects. Treatment time between the two groups |
-MBCT-A was noninferior to CBT-A in reducing anxiety symptoms in GAD patients, both interventions showed long-term benefits, and both are considered valuable treatment options for patients with GAD. | ||
| Age range 21-49 | The study discusses the effectiveness of MBSR in reducing symptoms of stress, anxiety, and depression, particularly in patients with SAD. The authors compare its effectiveness with cognitive-behavioural group therapy (CBGT) in improving mood, functionality, and quality of life in patients with generalised SAD. | -Lack of a control group or active comparison clinical intervention -Examination of only breath-focused attention, neglecting other important mindfulness practices -Need for randomized clinical trial methodology with multiple groups -Use of experimental paradigms with a variety of emotional probes and regulation strategies -Consideration of self-report measures of mindfulness -Analysis of individual differences at baseline -Investigation of how mindfulness practice in the health care provider interacts with the individual receiving health care |
-MBSR completers showed improvements in anxiety, depression symptoms, and self-esteem. -Breath-focused attention led to decreased negative emotion experience, reduced amygdala activity, and increased activity in attention-related brain regions. -Post-MBSR, there was a reduction in negative emotion, specifically when implementing breath-focused attention. | ||
| -Mean age 32.7 years | The study aimed to compare the treatment outcome and mediators of cognitive-behavioural group therapy (CBGT) and mindfulness-based stress reduction (MBSR) in patients with social anxiety disorder, showing both treatments produced significant improvements with common and specific mediators. | -Underrepresentation of African Americans in the sample -Focus solely on group therapy, not individual therapy -Modification of MBSR from its standard implementation -Lack of inclusion of computer tasks to complement traditional outcome indices -Need for experimental dismantling studies to examine treatment-specific mechanisms |
- Both CBGT and MBSR were effective in reducing social anxiety symptoms and shared similar underlying psychological mechanisms of change. | ||
| -Mean age of 37.6 years for CBGT group and 38.9 years for MBSR group | The study discusses a randomised trial comparing MBSR to CBGT for SAD, showing that while CBGT was more effective in reducing core symptoms, MBSR may still be a useful alternative intervention for some patients with SAD. | -Lack of a control comparison group -Infrequent assessments, limiting the ability to assess the time course of treatment effects -Recruitment primarily via media advertisement may not represent typical treatment-seeking populations -Limited impact of psychiatric comorbidity due to low rate and limited specific concurrent disorders -Reliance on self-report for verifying compliance with practices and homework |
-CBGT was significantly more effective than MBSR in reducing core symptoms of SAD, as indicated by lower scores on specific scales measuring social anxiety. -Response and remission rates were also significantly greater with CBGT. |
||
| -Age ranged from 17 to 53 years, with a mean age of 24.5 years | The study discusses the impact of cognitive restructuring and mindfulness strategies on post-event processing (PEP) and affect in social anxiety disorder (SAD), examining their efficacy in reducing PEP and improving affect in individuals with SAD, while also investigating the cognitive processes involved. | -Different lengths of the strategies may have influenced the results and comparability between conditions. -The structured and artificial nature of the PEP induction may limit the generalizability of the findings to real-life situations. -The brief duration and lack of homework component in the cognitive restructuring and mindfulness strategies may have limited their effectiveness in inducing cognitive changes. - The short follow-up period of one day may not have been sufficient to capture lasting changes in cognitive processes. - The measures used to assess mindfulness and decentering may not have been sensitive enough to detect subtle changes over a short timeframe. |
Cognitive restructuring and mindfulness strategies effectively reduced post-event processing (PEP) and improved affect compared to the control condition. Participants in these conditions reported decreased PEP, improved state affect, and greater skin conductance level (SCL) reductions compared to the control condition. Changes in cognitive processes predicted reduced PEP at follow-up. | ||
| 41.00 mean years old in MBI-SAD 38.33 mean years old in WL |
The study evaluated the feasibility and initial efficacy of a 12-week group mindfulness-based intervention for social anxiety disorder, which showed superiority over the waitlist control group in improving various outcomes. This suggests that integrating self-compassion and mindful exposure is a promising intervention for SAD. | -WL control does not account for nonspecific factors contributing to outcomes -Small sample size, predominantly female white participants, limits generalizability -Self-selected sample may be more receptive to mindfulness training -Recruitment mainly from the community via media advertisement may not generalize to treatment-seeking samples -Unclear extent of improvement due to therapist factors or the intervention itself -Follow-up only extended to 3 months, long-term benefits beyond this period unknown |
The MBI-SAD intervention demonstrated significant improvements in social anxiety symptom severity, depression, and social adjustment compared to the waitlist control group. Additionally, it enhanced self-compassion and facets of mindfulness, with these treatment gains being maintained at the 3-month follow-up. | ||
| -Participants aged 18–65 years | The study compared the efficacy of MBI-SAD and CBGT for social anxiety disorder, finding that while CBGT was more effective in reducing social anxiety severity, MBI-SAD showed comparable improvements in other well-being indices. Both interventions increased levels of mindfulness and self-compassion, suggesting overlapping psychological mechanisms. | -The study did not include a nonspecific control condition -High attrition rates in group therapies for SAD -Lack of consensus on determining noninferiority margins -Recruitment primarily via advertisement may limit generalizability -Participant demographics skewed towards Caucasian, well-educated individuals |
The main findings recommend that CBGT is more effective than MBI-SAD in reducing social anxiety severity. Still, both interventions have comparable effects on other well-being measures, with CBGT showing increased levels of mindfulness and self-compassion. | ||
| -Age range: 21-65 | The article discusses the effectiveness of MBCT and psychoeducation compared to usual care in reducing anxiety symptoms in patients with GAD, with psychoeducation showing additional benefits in reducing worry and depressive symptoms. It suggests further exploration of patient populations suitable for each intervention. | -Outcome measures based on self-reported questionnaires; lack of clinician-rated instruments or diagnostic interviews; comparison with usual care group limited to 3 months; potential selection bias in recruited participants; uncertainty regarding the reasons for differences between interventions and usual care. | - Both MBCT and psychoeducation were superior to usual care in reducing anxiety symptoms in participants with GAD. -BAI scores significantly decreased in MBCT and psychoeducation groups at 2 and 5 months after baseline assessment. |
||
| -Mean age of 40.8 years, with a range from 18 to 73 | The article presents a pragmatic randomized controlled trial comparing the effectiveness of MBCT with CBT-RP for treatment-refractory anxiety disorders, showing MBCT to be more effective in reducing anxiety and related symptoms compared to CBT-RP. | -Treatment-refractory anxiety disorder definition is not well-defined in the literature. -Lack of concealment of treatment allocation for participants during pre-treatment and subsequent assessments may introduce attrition bias. -Sample size limitations prevented the analysis of facets of mindfulness skills and difficulties in emotion regulation. -MBCT therapists' competence and adherence were rated as 'advanced beginner', potentially affecting treatment outcomes. -Lack of data on prior experience with mindfulness or meditation. -Absence of data on prior treatment history before admission to the center or the treatment format of the first-line CBT at the center. |
-MBCT was more effective than CBT-RP in reducing anxiety, avoidance, difficulties in emotion regulation, and worry while also increasing mindfulness skills. -The effects of MBCT were somewhat diminished at the 6-month follow-up. -The study concludes that MBCT is a promising intervention for individuals with anxiety disorders who did not respond well to first-line psychological treatment. |
||
6. TMS
6.1. Mechanism of Action
6.2. GAD
6.3. SAD
6.4. PTSD
6.5. Conclusion
| Autor, year of publication | Study design | Intervention | Participant count | Population characteristics |
| Cohen et al. (2004) | Randomized, double-blind, placebo-controlled trial | Low-frequency (1 Hz) rTMS for 10 daily sessions over 2 weeks; High-frequency (10 Hz) rTMS for 10 daily sessions over 2 weeks | Total: 29 | Patients with PTSD, 17 men and 7 women, various types of trauma experienced the mean time elapsed since trauma was 5.4 years |
| Watts et al. (2012) | Randomized controlled trial, double-blind, sham-controlled, pre-post design | Repetitive transcranial magnetic stimulation (rTMS) at 1 Hz to the right dorsolateral prefrontal cortex (DLPRC) for 10 sessions, delivered at 90% of the motor threshold for 20 minutes per day, with each 1-minute cycle consisting of a 20-second stimulation train with a 40-second intertrain interval | Total: 20 | - Largely white men in their early 50s - Participants had typically experienced combat trauma several decades earlier |
| Grisaru et al. (1998) | Open study with one session of slow TMS involving ten PTSD patients | Participants received one session of slow transcranial magnetic stimulation (TMS) with specific parameters: 30 pulses of 1 m/sec each, 15 to each side of the motor cortex, using a Magstim 200 stimulator with an intensity of 100% of machine capacity, a frequency of 0.3 Hz, and a field intensity of 2.5 T, over a total duration of 35 minutes. | Total: 10 | For patients diagnosed with PTSD, Traumatic events leading to PTSD included accidents, assault, and combat reactions. Some patients were drug-free, while others were treated with fluoxetine or fluvoxamine |
| Isserles et al. (2013) | Double-blind randomized controlled trial | Deep Transcranial Magnetic Stimulation (DTMS) after script-driven imagery of either the traumatic experience or a positive experience, followed by script-driven imagery of a neutral event. The DTMS sessions consisted of 42, 20 Hz trains of 2 s each, with a 20 s inter-train interval, totaling 1680 pulses per session. Participants received three weekly treatment sessions for 4 weeks, totaling 12 sessions. The script-driven imagery procedure recorded physiological responses (heart rate and skin conductance). | Total: 30 | The study population consists of adults with resistant PTSD |
| Boggio et al. (2010) | Randomized, Double-blind, Placebo-controlled, Phase II trial | Active 20 Hz rTMS of the right DLPFC, active 20 Hz rTMS of the left DLPFC, or sham rTMS, administered for 10 sessions over 2 weeks, 5 days per week. | Total: 30 | -patients with DSM-IV-diagnosed PTSD - Traumatic events associated with PTSD included assaults, sexual abuse, death or severe disease of a relative, and psychological distress/perceived physical harm - Most of the study subjects (21 of 30) were female - There were no significant differences in demographic and clinical scores at baseline across the 3 groups of treatment |
| Wang et al. (2022) | A randomized, double-blind, controlled trial | Participants received either single-site stimulation over the right dorsolateral prefrontal cortex (dlPFC) with 1500 pulses per session, or single-site stimulation over the right posterior parietal cortex (PPC) with 1500 pulses per session. Repeatable dual-site ccPAS (rds-ccPAS) over the right dlPFC and right PPC with 1500 pulses per session, or rds-ccPAS over the right dlPFC. and right PPC with 750 pulses per session. The intervention consisted of 10 sessions of 1 Hz rTMS. | Total: 71 | - Patients with Generalized Anxiety Disorder (GAD) |
| Dilkov et al. (2017) | A randomized, double-blind, controlled trial with a placebo-controlled design | High-frequency rTMS (20 Hz) to the right DLPFC for the ACTIVE group, with specific parameters: 5 sessions a week for the first 4 weeks, reduced to 3 times/week during the 5th week, and twice a week during the 6th week. | Total: 50 | - The age range of participants was 18 to 65 years old. - The gender distribution was 52% male and 48% female. - Participants from the Canadian site were older than those from the Bulgarian site, with differences in scores for HRDS and HARS. |
| Huang et al. (2018) | Randomized, double-blind, placebo-controlled pilot study | 1 Hz rTMS over the right parietal lobe for 10 consecutive days at 90% of resting motor threshold intensity. Sham rTMS was also administered over the same area with the same parameters. | Total: 36 | Participants were recruited from neurology outpatient clinics of Xuanwu Hospital, with specific exclusion criteria and restrictions on medication use. |
| Diefenbach et al. (2016) | Randomized, double-blind, sham-controlled trial with a parallel group | Repetitive transcranial magnetic stimulation (rTMS) targeted at the right dorsolateral prefrontal cortex (DLPFC) at a frequency of 1 Hz for 15 minutes (900 pulses/session) with an intensity of 90% of the resting motor threshold for a total of 30 sessions over 6 weeks (5 days/week). Some participants received sham rTMS using the Neuronetics XPLOR coil. | Total: 25 | - Diagnosed with GAD as the principal or coprincipal disorder - Participants were well-matched on demographic variables and most clinical variables, with the active group having more severe anxiety and worry - Responder status was significantly higher in the active group compared to the sham group after treatment |
| Wang et al. (2022) | Randomized controlled trial, double-blind, controlled, parallel design, non-placebo-controlled, multi-site, prospective, interventional | Single-site stimulation over the right dlPFC with 1500 pulses per session, single-site stimulation over the right PPC with 1500 pulses per session. RDS-ccPAS over the right dlPFC and right PPC with 1500 pulses per session, rds-ccPAS over the right dlPFC and right PPC with 750 pulses per session. Stimulation intensity was 90% of the resting motor threshold. | Total: 50 | - Participants with GAD - Inclusion criteria: Stable medication use for at least 4 weeks, diagnosis of GAD, Clinical Global Impression-Severity score of 4 or greater, HAM-A score greater than 14, HAM-D score of 22 or less - Exclusion criteria: Presence of neurologic disorders, unstable medical conditions, other psychiatric diseases or substance use disorders within the last 6 months, pregnancy or breastfeeding, contraindications for rTMS - All participants underwent resting-state EEG recordings - Baseline demographics, including age, sex, education, employment status, clinical variables, and RMT values, did not differ between groups |
| Diefenbach et al. (2016) | Randomized controlled trial (RCT), double-blind, intention-to-treat analysis, pre-treatment, post-treatment, and 3-month follow-up | 30 daily sessions (5 days/week) of low-frequency rTMS stimulation to the right DLPFC using the NeuroStar TMS Therapy System, with stimulation parameters of 1 Hz, 900 pulses/session, at 90% resting motor threshold. The right DLPFC point for stimulation was identified using a structural MRI scan and located using a frameless stereotactic neuronavigation system. | Total: 25 | - Predominantly women (84.6% in the active group, 66.7% in the sham group) |
| Assaf et al. (2018) | The study design includes a cross-sectional observational study (Study I) and a randomized-controlled trial (Study II) involving individuals with GAD and healthy controls. Study II is a controlled trial with active and sham rTMS interventions. | Active and sham repetitive transcranial magnetic stimulation (rTMS) targeting the right dorsolateral prefrontal cortex for 30 sessions. | Total: 51 | - Individuals diagnosed with GAD and healthy controls - Some individuals with GAD had comorbid anxiety or depressive disorders - Participants were matched on age, gender, race, and estimated IQ - A majority of individuals with GAD were undergoing pharmacological treatments |
| Leuchter et al. (2022) | The study design is a randomized controlled trial that blinds the subjects and research staff. | The intervention(s) that the study participants received were in vivo spider exposure followed by iTBS for three sessions administered to either active (vmPFC) or control (vertex) treatment sites and iTBS stimulation at 100% of the subject's RMT. | Total: 22 | - Individuals with spider phobia |
| Tomita et al. (2024) | randomized controlled trial | Participants received neodymium magnet stimulation on the right frontopolar area (rFPA) for 20 minutes. | Total: 23 | - The study included young adults with social anxiety tendencies, consisting of 12 women and 11 men, who were university students in 2022. The participants were Japanese, right-handed, and reported no psychological disorders, hearing problems, or neurological or cardiovascular illnesses. Furthermore, they reported no poor physical condition, lack of sleep, medication within 24 hours, or alcohol and caffeine consumption within 12 hours before the experiment. |
| Minervini et al. (2023) | Single-blind randomized controlled trial | Transcranial magnetic stimulation (TMS) on both the left and right DLPFC with low frequency (1 Hz) and high frequency (10 Hz) stimulation, totaling 300 pulses each, with specific durations and intervals between trains. | Total: 13 | - Mix of male and female participants, including individuals of Hispanic, Asian, and Caucasian ethnicities, with a mix of left-handed and right-handed participants. |
| Participant age | Summary | Limitations | Main findings | |
| age range 22-68 years old | The study presents the therapeutic effects of high-frequency repetitive transcranial magnetic stimulation (rTMS) of the right dorsolateral prefrontal cortex in PTSD patients, showing greater efficacy compared to slow-frequency or sham stimulation. | - Some patients did not complete the treatment course. - Development of manic episodes and rage attacks in some patients. - Controversy and uncertainty regarding cortisol levels and HPA axis in PTSD patients. - A small sample size leads to the preliminary nature of the study. |
- High-frequency rTMS (10 Hz) over the right dorsolateral prefrontal cortex significantly improved PTSD core symptoms and anxiety symptoms in patients with PTSD. | |
| Participants were mainly in their early 50s | The study presents the efficacy of rTMS for PTSD, showing that 1 Hz rTMS to the right DLPRC resulted in significant improvements in PTSD and depressive symptoms compared to sham treatment, supporting the effectiveness of right-sided rTMS for PTSD. | -Small sample size. -Homogenous patient population. |
- rTMS at 1 Hz to the right DLPRC showed significant improvements in core PTSD and depressive symptoms compared to sham treatments - Right-sided rTMS treatments were effective for PTSD - 10 sessions of 1 Hz rTMS to the right DLPRC had therapeutic effects for PTSD greater than sham rTMS |
|
| age range 21-53 years old | The study evaluates the clinical effect of slow TMS on PTSD symptoms, finding it effective in lowering core symptoms and highlighting TMS as a safe and tolerable intervention, marking the first exploration of TMS as a treatment for PTSD. | - The study was an open study with a limited number of participants. - Only one single TMS session was conducted at a slow frequency. - Some participants were receiving medication, which could have influenced the results. - The possibility of a placebo effect was acknowledged, casting some doubt on the results. - Future research is needed to determine the importance of lateralization, exact coil placement, stimulus intensity, and frequency for PTSD treatment. - Blinding of the study is suggested for future empirical studies. |
- TMS was effective in lowering core symptoms of PTSD, such as avoidance, anxiety, and somatization. - TMS was found to be a safe and tolerable intervention with indications of therapeutic efficacy for PTSD patients. - TMS led to significant improvement in PTSD core symptoms, particularly avoidance, in a short-term and transient manner. |
|
| 49 mean years old in group A 40.5 mean years old in group B 40.4 mean years old in Group C |
The study discusses the debilitating nature of PTSD induced by traumatic experiences, introduces the use of DTMS combined with brief exposure as a potentially effective treatment for resistant PTSD patients, and presents significant improvements in PTSD symptoms with this approach, suggesting the need for further validation through multi-center studies. | - Small sample size - Lack of a fourth control group receiving sham stimulation following sham exposure - The challenge to the broadly accepted theory by Koenigs and Grafman regarding the role of mPFC in PTSD |
- DTMS after exposure to the traumatic event script led to significant improvement in the intrusive component of the CAPS scale. - Combining brief script-driven exposure with DTMS showed therapeutic effects in PTSD patients. - The treatment effect was clinically and statistically significant, especially in the CAPS-Intrusive scores. |
|
| Age range 18- 64 years old | The study investigated the efficacy of high-frequency rTMS on PTSD symptoms, comparing right and left DLPFC stimulation. The right rTMS showed a more significant effect on core PTSD symptoms and anxiety relief compared to the left rTMS, which was more effective in improving depression symptoms. Right and left DLPFC stimulation were safe and not associated with cognitive worsening. The results suggest that high-frequency rTMS of the right DLPFC may be the optimal treatment strategy for PTSD. | The study's limitations include potential issues with the blinding method in the sham rTMS group, which could introduce bias or affect the interpretation of results. There is also a general limitation related to using the sham method in rTMS studies. Acknowledging the possibility of ineffective blinding further adds to the study's limitations. | - Both active 20 Hz rTMS of left and right DLPFC induced a significant decrease in PTSD symptoms, with right rTMS showing a more substantial effect. - Right rTMS led to a significant reduction in anxiety, while left rTMS resulted in a substantial improvement in mood. - The improvements in PTSD symptoms were long-lasting, remaining significant at the 3-month follow-up. |
|
| Age range 18-60 years old | Frontoparietal rds-ccPAS may be a better treatment option for GAD. | - Small sample size - Lack of comparison between dual-site stimulation with 1500 ccPAS pulses and single-site stimulation with 3000 pulses - Ideal control would have been dual-site sham stimulation - Uncertainty regarding the EEG system's correspondence with cortical areas |
The main findings suggest that frontoparietal rds-ccPAS with a between-site interval of 100 ms provided better benefits for patients with GAD compared to single-site protocols, showing more significant improvements in anxiety, depression, and insomnia symptoms, along with higher response rates and remission rates. | |
| age range 23-57 years old | Repetitive transcranial magnetic stimulation (rTMS) shows promise as a treatment option for patients with GAD who do not respond to pharmacotherapies, leading to a significant reduction in anxiety symptoms as measured by the Hamilton Anxiety Rating Scale (HARS). | A small sample size of the ACTIVE group and the SHAM procedure may limit the generalizability of the results. - Lack of proper blinding in the study, potentially leading to bias in the results. - Inability to generalize findings from the Bulgarian ACTIVE group to the Canadian population due to demographic and clinical differences. - The relatively small sample size (N = 5) in the Canadian site may have influenced the results. |
The main findings indicate that high-frequency rTMS applied to the right DLPFC significantly reduced anxiety symptoms, with the ACTIVE group showing clinical improvement and remission in HARS scores. | |
| 42.35 mean years old in GAD group 39.75 mean years old in the HC group |
1 Hz rTMS on the right parietal lobe is effective for improving anxiety and insomnia symptoms in comorbid GAD and insomnia, potentially through modulating attention and emotion processing. | - Parameters of rTMS stimulation for optimal effects in GAD patients are unknown. - Lack of clarity on the stimulation frequency, intensity, and duration of treatment. - Uncertainty about the generalizability of the findings to a larger population. - The study did not investigate the long-term effects of rTMS treatment on comorbid GAD and insomnia. - The study did not explore the potential impact of different rTMS protocols on treatment outcomes. |
- Repetitive transcranial magnetic stimulation (rTMS) on the right parietal lobe improved both anxiety and insomnia symptoms in patients with comorbid GAD and insomnia. - There was a positive correlation between the improvement of anxiety and insomnia symptoms. - rTMS was shown to be an effective treatment for comorbid GAD and insomnia. |
|
| age range 5-18 years old | The study presents the results of the first RCT investigating the efficacy of rTMS for GAD. The results show significant improvements in anxiety, worry, and depressive symptoms in the active group compared to the sham group, with higher response and remission rates in the active group. The findings suggest that rTMS may modify neural activity in the stimulation site, providing preliminary evidence for its effectiveness in treating GAD symptoms. | - Small sample size - High attrition rates - Preliminary nature of the results - Lack of long-term follow-up data - Unclear optimal treatment parameters for GAD - Potential placebo response in individuals with GAD - Need for further research to establish rTMS mechanisms of action - Importance of exploring biological mechanisms of anxiety improvements following rTMS - Need for future research to investigate relapse risk and maintenance rTMS - Importance of identifying efficacious dosing schedules that are more acceptable and feasible - Potential bias due to unequal distribution of anxiety symptoms in the randomization process - Unclear biological process underlying the mechanism by which inhibitory stimulation led to increased DLPFC activation during decision-making - Lack of clarity on the impact and predictors of neuromodulation on transdiagnostic biological and behavioral constructs |
The study's main findings include preliminary evidence supporting the efficacy of repetitive transcranial magnetic stimulation (rTMS) in treating GAD, with higher response and remission rates in the active rTMS group compared to the sham group. Changes in proper DLPFC activation during decision-making tasks correlated significantly with improvements in worry symptoms. | |
| age range 18-60 years old | Frontoparietal rds-ccPAS may be a better treatment option for GAD, showing more significant improvements in anxiety, depression, and insomnia compared to single-site stimulation. | - Small sample size - Lack of sham control group - Lack of equal-pulse single-site stimulation for comparison - Potential bias due to the absence of a sham control group - Need for replication in a larger sample size - Need for further research to confirm the findings |
- Frontoparietal rds-ccPAS-1500 induced more significant improvements in anxiety, depression, and insomnia symptoms compared to rds-ccPAS-750 and single-site stimulation. - More patients responded to treatment with rds-ccPAS-1500 than with single-site stimulation, with these differences persisting until the 3-month follow-up. - The study suggests that frontoparietal rds-ccPAS may be a more effective treatment option for GAD. |
|
| age range 29-59 years old | The study investigates the use of rTMS to improve emotion regulation in patients with GAD, showing significant improvements in self-reported emotion regulation difficulties in the active rTMS group, focusing on the association between emotion regulation improvements and clinical outcomes. | - Small sample size - Unclear relationship between emotion regulation improvements and symptom improvements - Need for future research with more extensive and better-matched samples - Need to investigate if emotion regulation improvements mediate treatment effects of rTMS on clinical symptoms |
Compared to the sham group, the active group demonstrated significant improvements in self-reported emotion regulation, particularly in goal-directed behaviors and impulse control. The study supports the clinical effects of DLPFC neuromodulation in patients with GAD. | |
| The study discusses the neural mechanisms underlying cognitive deficits associated with intolerance of uncertainty in individuals with GAD and how repetitive transcranial magnetic stimulation (rTMS) may effectively treat GAD by modulating neural networks. It outlines the neural abnormalities in GAD, the impact of rTMS on neural architecture, and the potential treatment targets for rTMS in GAD. The study also highlights the importance of understanding the neural circuits involved in decision-making under uncertainty and the role of neuromodulation in altering these circuits. The results suggest that GAD is associated with specific alterations in neural connectivity, particularly in regions like the dorsal anterior cingulate cortex (dACC), subgenual anterior cingulate cortex (sgACC), anterior insula (AI), and dorsolateral prefrontal cortex (DLPFC). The findings indicate that rTMS treatment can normalize functional connectivity patterns in these regions, potentially improving worry symptoms. The paper concludes by emphasizing the significance of these results for optimizing rTMS treatments for GAD. | - Over half of the patients with GAD also met the criteria for other anxiety or depressive disorders, limiting the specificity of the results. - Most GAD patients were undergoing pharmacological treatments, which could have secondary effects that were not assessed. - Study II had a small number of GAD patients undergoing active or sham rTMS treatment, with a liberal statistical threshold, making the results preliminary and necessitating replication with a larger sample. - The FC analyses included the sample used to identify ROIs, potentially affecting independence. |
- Individuals with GAD demonstrated impaired prefrontal cortex (PFC) functional connectivity during high uncertainty conditions. - Active rTMS treatment led to normalization of functional connectivity in specific brain regions and was associated with improvements in worry symptoms. - The study highlights the potential of rTMS in modulating neural networks and improving symptoms in individuals with generalized anxiety disorder. |
||
| 18+ (eligibility criteria) | The study discusses the feasibility and potential efficacy of using rTMS stimulation of vmPFC to augment exposure therapy for spider phobia, supporting the idea that rTMS may enhance exposure therapy for specific phobias. | - Small sample size - Homogeneous study population - Brief treatment duration compared to conventional standards - Control condition may not have been entirely inert - Substantial average delay between exposures and TMS - Large difference in pre-treatment baseline SCL between groups - Limited power due to small sample size - Potential bias due to recruitment methods - Methodological limitations in the study design - Lack of generalizability due to the specific population studied |
The study aimed to examine the feasibility and potential benefit of using rTMS stimulation of the ventromedial prefrontal cortex (vmPFC) to augment the efficacy of exposure therapy for spider phobia. Regardless of group, all subjects showed significant improvement in fear of spiders and skin conductance levels during the behavioral avoidance test. Subjects who received vmPFC stimulation tolerated lower treatment intensity, and there was a significant correlation between treatment intensity, distress improvement, and physiological measures. | |
| 20.81 mean years old | The study investigates the effects of transcranial static magnetic field stimulation (tSMS) on individuals with SAD, aiming to suppress rFPA activation and reduce self-focused attention (SFA) during a speech task, with promising results suggesting the potential clinical application of tSMS for treating SAD. | - Need for a larger sample size to validate the effectiveness of tSMS - Lack of investigation in clinical populations - Unclear duration of the effects of tSMS - Potential for long-lasting effects with multiple sessions of tSMS - Need to investigate remote effects of tSMS on other brain regions - Comparison of results between triple tSMS and single magnet system |
The main findings include the effectiveness of tSMS in decreasing rFPA activity, reducing SFA to bodily sensations, and increasing detached mindfulness perspective in individuals with high social anxiety tendencies. | |
| The participants' age range is 18-65 years old. |
The paper explores how social exclusion can induce pain-related sensations, the use of Cyberball to analyze social exclusion and the impact of transcranial magnetic stimulation on the DLPFC in influencing feelings of exclusion. | - Small sample size - Limited number of questions in the questionnaire - Focus only on the DLPFC, suggesting the need to explore other brain regions - Cyberball game parameters could be modified for a more comprehensive study - Replicability and generalizability concerns due to the small sample size and specific focus on DLPFC - Demand characteristics in participant responses could influence results |
- Excitation of the right DLPFC increased feelings of social exclusion - The right DLPFC plays a crucial role in processing social exclusion and social pain - Manipulation of brain activity in the DLPFC, especially the right DLPFC, significantly impacted perceptions of social exclusion |
|
6.5.1. Neurostimulation – Not Only rTMS and TMS
7. Electroconvulsive Therapy
8. Biofeedback
8.1. GAD
8.2. SAD
8.3. PTSD
8.4. Conclusion
| Autor, year of publication | Study design | Intervention | Participant count | Population characteristics |
| Rice et al. (1993) | Randomized controlled trial | The study participants' interventions were frontal EMG biofeedback, biofeedback to increase EEG alpha, biofeedback to decrease EEG alpha, and a pseudo meditation control condition, each consisting of 8 sessions. | Total: 45 | - Participants recruited from students and staff at SUNY-Albany and the community The average age of participants was 27.4 - 22 males and 23 females participated - 18 out of 45 participants were students |
| Wang et al. (2022) | Randomized controlled trial, double-blind, controlled, parallel design, non-placebo-controlled, multi-site, prospective, interventional | Single-site stimulation over the right dlPFC with 1500 pulses per session, single-site stimulation over the right PPC with 1500 pulses per session. RDS-ccPAS over the right dlPFC and right PPC with 1500 pulses per session, rds-ccPAS over the right dlPFC and right PPC with 750 pulses per session. Stimulation intensity was 90% of the resting motor threshold. | Total: 50 | - Participants with Generalized Anxiety Disorder (GAD) - Inclusion criteria: Stable medication use for at least 4 weeks, diagnosis of GAD, Clinical Global Impression-Severity score of 4 or greater, HAM-A score greater than 14, HAM-D score of 22 or less - Exclusion criteria: Presence of neurologic disorders, unstable medical conditions, other psychiatric diseases or substance use disorders within the last 6 months, pregnancy or breastfeeding, contraindications for rTMS - All participants underwent resting-state EEG recordings - Baseline demographics, including age, sex, education, employment status, clinical variables, and RMT values, did not differ between groups |
| Polak et al. (2015) | Randomized controlled trial (RCT) with two parallel groups | Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) with complementary breathing biofeedback using the RespiFit device introduced during the first session and continued throughout the exposure therapy sessions, mainly when focusing on emotional hotspots. | Total: 8 | - Patients with chronic PTSD - 6 females and 2 males in the study - Participants experienced single-event traumata such as motor vehicle accidents, sexual or physical abuse |
| Gerlach et al. (2004) | Randomized controlled trial with repeated measures analysis | Participants received veridical heart rate sounds presented in private or public condition while being evaluated by observers for 4 minutes. | Total: 64 | - Participants with social phobia and controls without any current psychiatric disorders were recruited - Social phobic participants did not differ from controls in terms of age, educational level, or male-to-female ratio The majority of the social phobic participants were diagnosed with generalized social phobia, with some having co-morbid diagnoses |
| Silver et al. (1995) | Controlled comparative study design | The study participants' interventions were Biofeedback, Relaxation Training, and Eye Movement Desensitization and Reprocessing (EMDR). Biofeedback and Relaxation Training were provided during treatment in the PTSD Program, while EMDR had limited availability due to therapist training and required at least one session. | Total: 100 | - Male Vietnam War veterans - Average time in combat of 12.5 months |
| Nilsson et al. (2011) | Randomized single experimental intervention | Audio feedback with cognitive preparation (CP) before listening to and evaluating a taped recording of their speech performance. The CP involved predicting in detail what they would hear on the audiotape, forming an image of themselves giving the speech, and listening to the audio recording as though they were listening to a stranger. | Total: 40 | - The study's population consists of 40 socially anxious undergraduate students with a gender distribution of 37 females and 3 males. |
| Nilsson et al. (2016) | Randomized controlled experiment | Audio feedback (AF) with reduced self-focus (RS) intervention | Total: 41 | - Socially anxious individuals - Students at Kristianstad Highschool in Sweden - 27 female and 14 male participants - Participants scoring 17 or higher on the FNE questionnaire |
| Hou et al. (2020) | Randomized controlled open-label | Neurofeedback training of alpha activity over the parietal lobe in GAD, with assessments at baseline, two weeks, and four weeks after treatment. | Total: 26 | - Female patients diagnosed with GAD and experiencing symptoms of anxiety trait, depressive symptoms, and insomnia |
| Dadashi et al. (2015) | The study design is a quasi-experimental study with pre-test and post-test with two groups. | Fifteen 30-minute alpha training sessions and fifteen 30-minute theta brain training sessions in the occipital area using neurofeedback training. | Total: 28 | Patients diagnosed with GAD, with an education level of at least up to the third grade of junior high school |
| Scheinost et al. (2013) | Controlled trial with a parallel design | Real-time functional magnetic resonance imaging (rt-fMRI) neurofeedback (NF) involving manipulation of orbitofrontal cortex (OFC) activity based on visual cues and feedback, with participants having four scanning sessions over 3 weeks and 10 functional runs during each session to control their brain activity. | Total: 20 | Subjects with high contamination-related anxiety, exclusion of individuals with a history of neuropsychiatric disorder or currently using medication (other than antibiotics or birth control), all included subjects had a score of X8 on the Padua Inventory-Washington State University Revision - Contamination Obsessions and Washing Compulsions subscale, total of 20 subjects included in the final analysis with 4 females in each group. |
| Participant age | Summary | Limitations | Main findings | |
| Mean 27.4 years old | The study discusses the effectiveness of different forms of biofeedback treatments, including frontal EMG biofeedback and EEG alpha biofeedback, in reducing anxiety symptoms in individuals with generalized anxiety disorder. | - Small sample size - Low statistical power due to small sample sizes - Brief treatment duration of 8 sessions - Not all subjects had diagnosable levels of GAD |
- All treated subjects experienced significant reductions in trait anxiety and psychophysiological symptoms. - Only the alpha-increase biofeedback group showed significant reductions in heart rate reactivity to stressors. - The decrease in self-reported anxiety was sustained at the 6-week post-treatment assessment. |
|
| The age range of participants: 18 to 60 years | Frontoparietal rds-ccPAS may be a better treatment option for GAD, showing more significant improvements in anxiety, depression, and insomnia compared to single-site stimulation. | - Small sample size - Lack of comparison between dual-site stimulation with 1500 ccPAS pulses and single-site stimulation with 3000 pulses - Ideal control would have been dual-site sham stimulation - Uncertainty regarding the EEG system's correspondence with cortical areas |
- Frontoparietal rds-ccPAS-1500 induced more significant improvements in anxiety, depression, and insomnia symptoms compared to rds-ccPAS-750 and single-site stimulation. - More patients responded to treatment with rds-ccPAS-1500 than with single-site stimulation, with these differences persisting until the 3-month follow-up. - The study suggests that frontoparietal rds-ccPAS may be a more effective treatment option for GAD. |
|
| The age range of participants: 25–57 years |
Breathing biofeedback as an adjunct to exposure in cognitive behavioral therapy shows promise in hastening the reduction of PTSD symptoms. | - Small sample size - Missing values of one patient who was lost to follow-up measurement - Breathing rates or parameters were not recorded during sessions in either condition - Results were limited by the fact that breathing biofeedback was not compared to TF-CBT without biofeedback - Need for future research with larger sample sizes to draw more definite conclusions on the effectiveness of breathing biofeedback addition to exposure in CBT and the effect on reduction in no-shows and non-response in TF-CBT - Need for future research to examine the underlying acute physiological processes and changes during breathing biofeedback to gain more insight into the exact working mechanisms involved and improve the efficiency of this additional treatment |
Breathing biofeedback showed a trend towards a significantly faster reduction in PTSD symptoms compared to regular TF-CBT, as measured by the Impact of Event Scale-Revised (IES-R) and confirmed by the mixed model analysis. | |
| The study discusses the theoretical model of social phobia, the impact of providing non-veridical feedback of a heart rate increase, and the differences in heart rates and reported anxiety between social phobics and controls. It also discusses the induction of social anxiety in social phobics when making an anxiety symptom public. | - Differences in heart rate in the social phobic groups between the counterbalanced experimental groups without a clear explanation. - Significantly different levels of social anxiety and depression in the two experimental social phobia groups, with no explanation other than chance. |
Social phobics experienced more anxiety and worry when their heart rate was made public compared to when it was private. Social phobics reported higher levels of anxiety and worry about their heart rate in public condition compared to controls. The visibility of anxiety symptoms, such as heart rate, can significantly increase anxiety levels in social phobics. | ||
| The age range of participants: 2-20 years |
The study discusses the effectiveness of EMDR, Relaxation Training, and Biofeedback in treating PTSD among Vietnam War veterans, with EMDR being the most effective treatment, significantly improving symptoms compared to the Control group and outperforming the other treatments. | - Reliance on patient self-report data - Variability in experience levels in treatments and PTSD - Exposure to trauma events in EMDR but not in the other two treatments - Lack of blinding of clinicians and subjects to the comparative treatment research - Small sample size for some treatment groups - Potential bias and expectancy effects due to the Control group being treated before EMDR was introduced - Need for replication with more significant numbers and extension to other treatment techniques and populations |
EMDR was the most effective additional treatment for PTSD symptoms, outperforming Relaxation Training and Biofeedback. | |
| 26.5 mean years old | The study discusses the potential of audio feedback with cognitive preparation as a treatment intervention for social phobia, highlighting its benefits in reducing negative self-evaluations and anxiety in socially anxious individuals. | - Small sample size - Analogue study - Gender bias towards females - Concerns about using FNE as a screening instrument - Use of a one-item measure for state anxiety - Lack of a control condition with no audio feedback - Lack of comparison of audio feedback alone against no feedback at all |
- Audio feedback with cognitive preparation (AFeCP) led to less negative self-ratings after the first speech, and these effects generalized to the evaluation of the second speech. - The study demonstrated that AFeCP was beneficial for socially anxious individuals in reducing negative self-evaluations and decreasing anxiety. - The results align with previous research on the effectiveness of cognitive preparation in enhancing the effects of feedback interventions. |
|
| The age range of participants: 18-19 years | The study explores the use of reduced self-focus as an intervention for social anxiety, showing that AF with RS leads to improved voice evaluations in socially anxious individuals, indicating the potential of RS as a promising intervention for social anxiety. | - small sample size - analogue study - need for comparisons with the entire CP package - need for comparison of different kinds of self-focus - need for replication with a clinical sample |
- AF with RS led to improved voice evaluations compared to AF-only after the first speech, and this improvement was maintained in the assessment of the second speech. - Positive speech evaluations were linked to reductions in performance anxiety. - RS, as a component of cognitive preparation, showed promising results in improving voice evaluation in socially anxious individuals, suggesting its potential as an intervention for social anxiety treatment. |
|
| Neurofeedback training of alpha activity over the parietal lobe is efficacious in improving anxiety traits and depressive symptoms in female patients with GAD. | - Only a time effect emerged for the questionnaire - No significant difference in the grouping factors of the two groups - Small sample size - Limited to female subjects - Short follow-up time |
The main findings of the study indicate that neurofeedback training targeting alpha activity over the parietal lobe effectively improves anxiety traits and depressive symptoms in patients with GAD. | ||
| The age range of participants: 18–50 years | The study investigates the effects of increasing alpha and theta brain wave amplitude in the occipital area on reducing symptoms of GAD and improving the global functioning level in patients with GAD. Neurofeedback training targeting alpha and theta waves effectively lowered GAD symptoms and enhanced functioning levels. | Cultural differences do not influence the study results significantly. - Subjects' scores being different at the beginning, affecting the comparison between control and experimental groups - Absence of a placebo treatment group and control group due to limitations of the sample and ethical concerns |
- Increase of alpha and theta brain waves amplitude in the occipital area can lead to an increase in global functioning level and a reduction in symptoms of generalized anxiety disorder in patients with GAD. - Neurofeedback training can effectively increase alpha and theta brain waves amplitude and reduce symptoms of GAD. - The study confirms brain functional changes related to alpha wave amplitude following neurofeedback training sessions. |
|
| The study demonstrates the use of fMRI neurofeedback to alter brain connectivity and reduce contamination anxiety, with observed lasting modifications in brain functional architecture, supporting the potential of neurofeedback as a clinically helpful therapy for anxiety. | - The study was limited to two NF sessions, so the optimal number of sessions for the intervention is unknown. - The study did not include patients with OCD, so the generalizability of the findings to this population is uncertain. - The study focused on contamination anxiety, so the applicability of the results to other forms of anxiety is unclear. - The study did not investigate the long-term effects of more than several days post-training. - The study did not explore the persistence of changes induced by rt-fMRI NF in various contexts beyond contamination anxiety. |
- The study used fMRI neurofeedback to alter brain connectivity and reduce contamination anxiety. - Neurofeedback training led to lasting changes in brain connectivity numerous days after the completion of training. - The training increased subjects' control over contamination anxiety even days after the training sessions. |
||
9. Other Methods
9.1. EMDR (Eye Movement Desensitization and Reprocesing)
9.2. VNS (Vagus Nerve Stimulation)
9.3. MDMA as a Therapeutic Adjunct to Psychotherapy
9.4. Cryotherapy
9.4.1. Temperature-Based Therapies in Anxiety-Provoking Medical Situations
9.4.2. Conclusion
9.5. Hyperbaric Therapy
9.5.1. Conclusion
10. Herbal Treatment
10.1. Lavender Oil
10.2. Cannabidiol
10.3. Kava Kava
10.4. Valeriana
10.5. Chamomile
10.6. Conclusion
| Author, year of publication | Herb, dosageform and total daily dose |
Study design | Dosage, total duration of administration | First test group | Second test group | Third test group |
| Kasper et al. (2014) | Lavender Oil, capsules, 160 mg | randomized, double-blind, double-dummy,reference- and placebo- controlled | 1x160mg/day for 10 weeks | Lavender oil capsules, 128 adults (18-65 years old), 121 adults completed | 20 mg paroxetine 137 adults (18-65 years old) 132 adults completed |
placebo, 136 adults (18-65 years old) 135 adults completed |
| Crippa et al. (2010) |
Cannabis sativa, capsules, 400 mg, | double- blind, placebo controlled | 400 mg acute administration in two sessions | CBD capsules, 10 men (20-33 years old) |
placebo 10 (20-33 years old) |
|
| Savage et al. (2023) |
Piper methysticum (Kava), tablets, 240 mg | sub-study, double- blinded, placebo- controlled | 2x120mg/day for 8 weeks | Kava tablets 20 adults (18-65 years old) 9 adults completed |
placebo, 17 adults (18-65 years old) 8 adults completed |
|
| Roh et al. (2019) |
Valerian root (Valeriana), capsules, 300 mg |
double-blinded, randomized, placebo-controlled clinical trial | 3x100 mg/day for 4 weeks | Valeriana capsules, 34 adults (18-65 years old) 29 adults completed |
placebo 30 adults (18-65 years old) 23 adults completed |
|
| Keefe et al. (2018) |
Chamomile, capsules, 500 mg |
open-label clinical trial |
500 mg/day for 8 weeks | Chamomile capsules, 45 adults (>18 years old) 45 adults completed |
- | |
| H. Woelk e al. (2007) |
Ginkgo biloba, tablets 480 mg, 240 mg |
randomized, double-blind, placebo-controlled trial |
3x2 tablets of 40 mg/ day or 3x2 tablets of 80 mg/ day for 4 weeks |
Ginkgo Biloba capsules, 40 mg 36 adults (18-70 years old) 35 adults completed |
Ginkgo Biloba capsules, 80 mg 34 adults (18-70 years old) 32 adults completed |
Placebo 37 adults (18-70 years old) 37 adults completed |
| S Akhondzadeh et al.(2001) |
Passiflora incarnata (Passionflower) | pilot double-blind randomized controlled trial |
45 drops a day for 4 weeks | Passiflora drops, 45 drops a day 18 adults (19-47 years old) 16 adults completed |
Oxazepam 30 mg/day plus Passiflora drops 18 adults (19-47 years old) 16 adults completed |
Placebo 36 adults (19-47 years old) 32 adults completed |
| Majeed et al. |
Ashwagandha root, 500 mg | randomized, double-blind, placebo-controlled study | 12.5 mg withanolides/day for 60 days | Ashwagandha root extract with 95% piperine capsules 27 adults 25 adults completed |
Placebo 27 adults 15 adults completed |
|
| Author, year of publication | Method of data collecting | Outcomes | Adverse events/ side effects | Limitations | Overall effect | |
| Kasper et al. (2014) | Hamilton Anxiety Rating Scale (HAM-A) | Reduction in HAMA total score in Silexan group and paroxetine group | 48 adverse events, mostly Gastrointestinal disorders, infections, and nervous system disorders in all groups |
no significant limitations | positive | |
| Crippa et al. (2010) |
SPECT imaging Visual Analogue Mood Scale (VAMS) |
Significant reduction in VAMS anxiety score reduced ECD uptake in the left parahippocampal gyrus, hippocampus, inferior temporal gyrus and increased ECD uptake in the right posterior cingulate gyrus |
no major side effects | small sample size without a sample of control subjects lower sensitivity of the SPECT technique absence of absolute quantitative estimates of rCBF when SPECT tracers are used |
positive | |
| Savage et al. (2023) |
proton magnetic resonance spectroscopy (H-MRS) Hamilton Anxiety Rating Scale (HAM-A) |
Reduction in GABA concentration in dorsal anterior cingulate in Kava group A positive correlation between HAMA scores and GABA concentration level at baseline, but no significant relation to treatment |
no significantly different between Kava and placebo groups dizziness and headache of mild severity (1 case) in Kava group |
a sample size attrition of 46% from baseline to the second time point (n = 8 kava; n = 9 placebo) the risk of measurement errors due to requirement of high amounts of data modelling to expose GABA peaks MRI scan environment as a influencing factor in anxiety level in participants |
positive | |
| Roh et al. (2019) |
electroencephalography (EEG) | significantly greater increases in frontal brain region alpha coherence across four electrode pairs and significantly greater decreases in theta coherence across another four electrodes pairs in the VRE group |
atypical chest pain (1 case) in VRE group mild gastrointestinal problem (1 case) in placebo group |
volume conduction problems which caused pseudo-correlation recordings from neighboring electrodes small sample size as a problem in detecting all differences in psychological variables relatively small VRE dose which leads to negative findings on psychological scales |
positive | |
| Keefe et al. (2018) |
morning salivary cortisol a subject- report measure of GAD symptomatology (GAD-7) subject-report questionnaire Mao Expectancy of Treatment Effects (METE) |
increases in morning salivary cortisol and the diurnal cortisol slope improving the total score of GAD-7 and METE |
not mentioned | small sample size lack of placebo group predicted changes in cortisol due to higher baseline GAD-7 scores It is hard to determine whether GAD symptom improvement leads to changes in cortisol or cortisol changes precede GAD symptom improvement, or they occur relatively simultaneously |
positive | |
| H. Woelk e al. (2007) |
Hamilton Anxiety Rating Scale (HAM-A) Clinician’s global judgement, operationalized by the Clinical global impression of change CGI-C |
Reduction in HAMA total score in all three treatment groups during the early phase Patients in both Ginkgo Biloba groups felt better than in placebo groups |
nine adverse events were reported, three for each treatment group. mild gastroenteritis, moderate pain in the context of pre-existing osteoarthritis of the lumbar spine and moderate to severe tachycardia with hypertension in placebo group moderate to severe gastroenteritis, moderate sinusitis and mild pruritus in Ginkgo Biloba 40 mg group moderate to severe gastroenteritis, moderate sinusitis and mild pruritus,(1 case) in Ginkgo Biloba 80 mg group systolic blood pressure drop from a median 130 to 122.5 mmHg and from 137.5 to 130 mmHg in two Ginkgo Biloba groups |
small sample size difficulty in reliable sample size calculation due to small amount of data to estimate the potential effect size of Ginkgo Biloba Participants fulfilled diagnostic criteria for both GAD and adjustment disorder with anxious mood (ADWAM) |
positive | |
| S Akhondzadeh et al.(2001) |
Hamilton Anxiety Rating Scale (HAM-A) | Significant reduction in HAM-A score from the baseline. No significant difference was observed between Passiflora and oxazepam group | In Passiflora drop: Dizziness (7 cases) Drowsiness (6) Confusion (4) Ataxia (2) Allergic reaction (2) Impairment of job performance (8) |
small- sample size short time of duration (4 weeks) |
positive | |
| Majeed et al. |
perceived stress scale (PSS) measure of GAD symptomatology (GAD-7) Quality-of-Life questionnaire (QOL) Cambridge Neuropsychological Test Automated Battery (CANTAB) analysis, salivary cortisol, urinary dopamine, serotonin, and antioxidant markers |
improving the total score of PSS, GAD-7, QOL in ARE group significant improvement in multitasking, concentration, and decision taking time in CATNAB in ARE group greater reduction in the morning salivary cortisol and an increase in urinary serotonin in ARE group Serum levels of NO, GSH, and MDA were not significantly different |
any incidence of adverse events | Patients were healthy adults with mild to moderate stress in southern India Small sample size Short time of duration (60 days) |
positive | |
11. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Collaborators GDaIIaP. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211-59. PubMed PMID: 28919117; PubMed Central PMCID: PMC5605509. [CrossRef]
- Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655-79. PubMed PMID: 21896369. [CrossRef]
- Kessler RC. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatr Scand Suppl. 2003(417):19-27. PubMed PMID: 12950433. [CrossRef]
- Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety. 2008;25(1):72-90. PubMed PMID: 17146763. [CrossRef]
- Peng L, Morford KL, Levander XA. Benzodiazepines and Related Sedatives. Med Clin North Am. 2022;106(1):113-29. PubMed PMID: 34823725. [CrossRef]
- Anagha K, Shihabudheen P, Uvais NA. Side Effect Profiles of Selective Serotonin Reuptake Inhibitors: A Cross-Sectional Study in a Naturalistic Setting. Prim Care Companion CNS Disord. 2021;23(4). Epub 20210729. PubMed PMID: 34324797. [CrossRef]
- Hedman E, Andersson E, Ljótsson B, Axelsson E, Lekander M. Cost effectiveness of internet-based cognitive behaviour therapy and behavioural stress management for severe health anxiety. BMJ Open. 2016;6(4):e009327. Epub 20160425. PubMed PMID: 27113231; PubMed Central PMCID: PMC4854011. [CrossRef]
- Bijl RV, de Graaf R, Hiripi E, Kessler RC, Kohn R, Offord DR, et al. The prevalence of treated and untreated mental disorders in five countries. Health Aff (Millwood). 2003;22(3):122-33. PubMed PMID: 12757277. [CrossRef]
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219-29. PubMed PMID: 22818936; PubMed Central PMCID: PMC3645500. [CrossRef]
- Wedekind D, Broocks A, Weiss N, Engel K, Neubert K, Bandelow B. A randomized, controlled trial of aerobic exercise in combination with paroxetine in the treatment of panic disorder. World J Biol Psychiatry. 2010;11(7):904-13. PubMed PMID: 20602575. [CrossRef]
- Lucibello KM, Parker J, Heisz JJ. Examining a training effect on the state anxiety response to an acute bout of exercise in low and high anxious individuals. J Affect Disord. 2019;247:29-35. Epub 20181223. PubMed PMID: 30640027. [CrossRef]
- Estevao C. The role of yoga in inflammatory markers. Brain Behav Immun Health. 2022;20:100421. Epub 20220201. PubMed PMID: 35199049; PubMed Central PMCID: PMC8842003. [CrossRef]
- Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med. 2010;16(11):1145-52. Epub 20100819. PubMed PMID: 20722471; PubMed Central PMCID: PMC3111147. [CrossRef]
- Javnbakht M, Hejazi Kenari R, Ghasemi M. Effects of yoga on depression and anxiety of women. Complement Ther Clin Pract. 2009;15(2):102-4. Epub 20090320. PubMed PMID: 19341989. [CrossRef]
- O'Shea M, Capon H, Skvarc D, Evans S, McIver S, Harris J, et al. A pragmatic preference trial of therapeutic yoga as an adjunct to group cognitive behaviour therapy versus group CBT alone for depression and anxiety. J Affect Disord. 2022;307:1-10. Epub 20220315. PubMed PMID: 35301041. [CrossRef]
- Lundt A, Jentschke E. Long-Term Changes of Symptoms of Anxiety, Depression, and Fatigue in Cancer Patients 6 Months After the End of Yoga Therapy. Integr Cancer Ther. 2019;18:1534735418822096. PubMed PMID: 30791735; PubMed Central PMCID: PMC7240880. [CrossRef]
- Broman-Fulks JJ, Berman ME, Rabian BA, Webster MJ. Effects of aerobic exercise on anxiety sensitivity. Behav Res Ther. 2004;42(2):125-36. PubMed PMID: 14975776. [CrossRef]
- Cox RH, Thomas TR, Davis JE. Delayed Anxiolytic Effect Associated with an Acute Bout of Aerobic Exercise. Journal of Exercise Physiology Online. 2000;3(4).
- Broman-Fulks JJ, Kelso K, Zawilinski L. Effects of a Single Bout of Aerobic Exercise Versus Resistance Training on Cognitive Vulnerabilities for Anxiety Disorders. Cogn Behav Ther. 2015;44(4):240-51. Epub 20150319. PubMed PMID: 25789738. [CrossRef]
- Ma WF, Wu PL, Su CH, Yang TC. The Effects of an Exercise Program on Anxiety Levels and Metabolic Functions in Patients With Anxiety Disorders. Biol Res Nurs. 2017;19(3):258-68. Epub 20161011. PubMed PMID: 27729394. [CrossRef]
- Gordon BR, McDowell CP, Lyons M, Herring MP. Resistance exercise training among young adults with analogue generalized anxiety disorder. J Affect Disord. 2021;281:153-9. Epub 20201208. PubMed PMID: 33321380. [CrossRef]
- Plag J, Schmidt-Hellinger P, Klippstein T, Mumm JLM, Wolfarth B, Petzold MB, et al. Working out the worries: A randomized controlled trial of high intensity interval training in generalized anxiety disorder. J Anxiety Disord. 2020;76:102311. Epub 20200924. PubMed PMID: 33007710. [CrossRef]
- Herring MP, Jacob ML, Suveg C, Dishman RK, O'Connor PJ. Feasibility of exercise training for the short-term treatment of generalized anxiety disorder: a randomized controlled trial. Psychother Psychosom. 2012;81(1):21-8. Epub 20111122. PubMed PMID: 22116310. [CrossRef]
- O'Sullivan D, Gordon BR, Lyons M, Meyer JD, Herring MP. Effects of resistance exercise training on depressive symptoms among young adults: A randomized controlled trial. Psychiatry Res. 2023;326:115322. Epub 20230628. PubMed PMID: 37429171. [CrossRef]
- Tully PJ, Selkow T, Bengel J, Rafanelli C. A dynamic view of comorbid depression and generalized anxiety disorder symptom change in chronic heart failure: the discrete effects of cognitive behavioral therapy, exercise, and psychotropic medication. Disabil Rehabil. 2015;37(7):585-92. Epub 20140701. PubMed PMID: 24981015. [CrossRef]
- Herring M, Jacob M, Suveg C, Connor P. Effects of short-term exercise training on signs and symptoms of generalized anxiety disorder. Mental Health and Physical Activity. 2011;4:71-7. Effects of Exercise on Sleep Among Young Women With Generalized Anxiety Disorder. [CrossRef]
- Herring MP, Kline CE, O'Connor PJ. Ment Health Phys Act. 2015;9:59-66. PubMed PMID: 26566400; PubMed Central PMCID: PMC4637973. [CrossRef]
- Szuhany KL, Adhikari S, Chen A, Lubin RE, Jennings E, Rassaby M, et al. Impact of preference for yoga or cognitive behavioral therapy in patients with generalized anxiety disorder on treatment outcomes and engagement. J Psychiatr Res. 2022;153:109-15. Epub 20220705. PubMed PMID: 35810600; PubMed Central PMCID: PMC9969964. [CrossRef]
- Simon NM, Hofmann SG, Rosenfield D, Hoeppner SS, Hoge EA, Bui E, et al. Efficacy of Yoga vs Cognitive Behavioral Therapy vs Stress Education for the Treatment of Generalized Anxiety Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78(1):13-20. PubMed PMID: 32805013; PubMed Central PMCID: PMC7788465. [CrossRef]
- Doria S, de Vuono A, Sanlorenzo R, Irtelli F, Mencacci C. Anti-anxiety efficacy of Sudarshan Kriya Yoga in general anxiety disorder: A multicomponent, yoga based, breath intervention program for patients suffering from generalized anxiety disorder with or without comorbidities. J Affect Disord. 2015;184:310-7. Epub 20150624. PubMed PMID: 26142611. [CrossRef]
- Jazaieri H, Goldin PR, Werner K, Ziv M, Gross JJ. A randomized trial of MBSR versus aerobic exercise for social anxiety disorder. J Clin Psychol. 2012;68(7):715-31. Epub 20120523. PubMed PMID: 22623316; PubMed Central PMCID: PMC4136448. [CrossRef]
- Goldin P, Ziv M, Jazaieri H, Hahn K, Gross JJ. MBSR vs aerobic exercise in social anxiety: fMRI of emotion regulation of negative self-beliefs. Soc Cogn Affect Neurosci. 2013;8(1):65-72. Epub 20120513. PubMed PMID: 22586252; PubMed Central PMCID: PMC3541489. [CrossRef]
- Jazaieri H, Lee IA, Goldin PR, Gross JJ. Pre-treatment social anxiety severity moderates the impact of mindfulness-based stress reduction and aerobic exercise. Psychol Psychother. 2016;89(2):229-34. Epub 20150214. PubMed PMID: 25684277; PubMed Central PMCID: PMC4537407. [CrossRef]
- Javed D, Mishra S. Yoga practices in Social Anxiety Disorder (SAnD): A case report WSR to paruresis. J Ayurveda Integr Med. 2022;13(3):100622. Epub 20220907. PubMed PMID: 36087392; PubMed Central PMCID: PMC9468380. [CrossRef]
- Vollbehr NK, Bartels-Velthuis AA, Nauta MH, Castelein S, Steenhuis LA, Hoenders HJR, et al. Hatha yoga for acute, chronic and/or treatment-resistant mood and anxiety disorders: A systematic review and meta-analysis. PLoS One. 2018;13(10):e0204925. Epub 20181001. PubMed PMID: 30273409; PubMed Central PMCID: PMC6166972. [CrossRef]
- Whitworth JW, Nosrat S, SantaBarbara NJ, Ciccolo JT. Feasibility of Resistance Exercise for Posttraumatic Stress and Anxiety Symptoms: A Randomized Controlled Pilot Study. J Trauma Stress. 2019;32(6):977-84. Epub 20191119. PubMed PMID: 31743507. [CrossRef]
- Fetzner MG, Asmundson GJ. Aerobic Exercise Reduces Symptoms of Posttraumatic Stress Disorder: A Randomized Controlled Trial. Cogn Behav Ther. 2015;44(4):301-13. Epub 20140609. PubMed PMID: 24911173. [CrossRef]
- Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand. 2015;131(5):350-9. Epub 20141201. PubMed PMID: 25443996. [CrossRef]
- Yi L, Lian Y, Ma N, Duan N. A randomized controlled trial of the influence of yoga for women with symptoms of post-traumatic stress disorder. J Transl Med. 2022;20(1):162. Epub 20220405. PubMed PMID: 35382845; PubMed Central PMCID: PMC8985332. [CrossRef]
- J.Carter J, Gerbarg P, Brown R, Ware R, ambrosio C, Anand L, et al. Multi-Component Yoga Breath Program for Vietnam Veteran Post Traumatic Stress Disorder: Randomized Controlled Trial. Journal of Traumatic Stress disorders & Treatment. 2013;2:1-10. [CrossRef]
- McCarthy L, Fuller J, Davidson G, Crump A, Positano S, Alderman C. Assessment of yoga as an adjuvant treatment for combat-related posttraumatic stress disorder. Australas Psychiatry. 2017;25(4):354-7. Epub 20170301. PubMed PMID: 28747121. [CrossRef]
- van der Kolk BA, Stone L, West J, Rhodes A, Emerson D, Suvak M, et al. Yoga as an adjunctive treatment for posttraumatic stress disorder: a randomized controlled trial. J Clin Psychiatry. 2014;75(6):e559-65. PubMed PMID: 25004196. [CrossRef]
- Davis LW, Schmid AA, Daggy JK, Yang Z, O'Connor CE, Schalk N, et al. Symptoms improve after a yoga program designed for PTSD in a randomized controlled trial with veterans and civilians. Psychol Trauma. 2020;12(8):904-12. Epub 20200420. PubMed PMID: 32309986. [CrossRef]
- Martin EC, Dick AM, Scioli-Salter ER, Mitchell KS. Impact of a Yoga Intervention on Physical Activity, Self-Efficacy, and Motivation in Women with PTSD Symptoms. J Altern Complement Med. 2015;21(6):327-32. Epub 20150514. PubMed PMID: 25973554; PubMed Central PMCID: PMC4486144. [CrossRef]
- Huberty J, Sullivan M, Green J, Kurka J, Leiferman J, Gold K, et al. Online yoga to reduce post traumatic stress in women who have experienced stillbirth: a randomized control feasibility trial. BMC Complement Med Ther. 2020;20(1):173. Epub 20200605. PubMed PMID: 32503517; PubMed Central PMCID: PMC7275350. [CrossRef]
- Ströhle A, Graetz B, Scheel M, Wittmann A, Feller C, Heinz A, et al. The acute antipanic and anxiolytic activity of aerobic exercise in patients with panic disorder and healthy control subjects. J Psychiatr Res. 2009;43(12):1013-7. Epub 20090316. PubMed PMID: 19289240. [CrossRef]
- Gaudlitz K, Plag J, Dimeo F, Ströhle A. Aerobic exercise training facilitates the effectiveness of cognitive behavioral therapy in panic disorder. Depress Anxiety. 2015;32(3):221-8. Epub 20141217. PubMed PMID: 25515221. [CrossRef]
- Broocks A, Bandelow B, Pekrun G, George A, Meyer T, Bartmann U, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. Am J Psychiatry. 1998;155(5):603-9. PubMed PMID: 9585709. [CrossRef]
- Ensari I, Petruzzello SJ, Motl RW. The effects of acute yoga on anxiety symptoms in response to a carbon dioxide inhalation task in women. Complement Ther Med. 2019;47:102230. Epub 20191103. PubMed PMID: 31780009. [CrossRef]
- Vorkapic CF, Rangé B. Reducing the symptomatology of panic disorder: the effects of a yoga program alone and in combination with cognitive-behavioral therapy. Front Psychiatry. 2014;5:177. Epub 20141208. PubMed PMID: 25538634; PubMed Central PMCID: PMC4259001. [CrossRef]
- Yadla VS, Nj P, Kamarthy P, Matti MR. Effect of Integrated Yoga as an Adjuvant to Standard Care for Panic Disorder: A Randomized Control Trial Study. Cureus. 2024;16(1):e53286. Epub 20240131. PubMed PMID: 38435873; PubMed Central PMCID: PMC10905419. [CrossRef]
- Meyer T, Broocks A. Therapeutic impact of exercise on psychiatric diseases: guidelines for exercise testing and prescription. Sports Med. 2000;30(4):269-79. PubMed PMID: 11048774. [CrossRef]
- Li L, Yu F, Shi D, Shi J, Tian Z, Yang J, et al. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017;9(9):3867-80. Epub 20170915. PubMed PMID: 28979666; PubMed Central PMCID: PMC5622235.
- Schultheis MT, Rizzo AA. The application of virtual reality technology in rehabilitation. Rehabilitation Psychology. 2001;46(3):296-311. PubMed PMID: WOS:000170969400009. [CrossRef]
- Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The Use of Virtual Reality Technology in the Treatment of Anxiety and Other Psychiatric Disorders. Harv Rev Psychiatry. 2017;25(3):103-13. PubMed PMID: 28475502; PubMed Central PMCID: PMC5421394. [CrossRef]
- Veling W, Lestestuiver B, Jongma M, Hoenders HJR, van Driel C. Virtual Reality Relaxation for Patients With a Psychiatric Disorder: Crossover Randomized Controlled Trial. J Med Internet Res. 2021;23(1):e17233. Epub 20210115. PubMed PMID: 33448933; PubMed Central PMCID: PMC7846446. [CrossRef]
- McLay R, Ram V, Murphy J, Spira J, Wood DP, Wiederhold MD, et al. Effect of virtual reality PTSD treatment on mood and neurocognitive outcomes. Cyberpsychol Behav Soc Netw. 2014;17(7):439-46. Epub 20140317. PubMed PMID: 24635120. [CrossRef]
- Beidel DC, Frueh BC, Neer SM, Bowers CA, Trachik B, Uhde TW, et al. Trauma management therapy with virtual-reality augmented exposure therapy for combat-related PTSD: A randomized controlled trial. J Anxiety Disord. 2019;61:64-74. Epub 20170823. PubMed PMID: 28865911. [CrossRef]
- Katz AC, Norr AM, Buck B, Fantelli E, Edwards-Stewart A, Koenen-Woods P, et al. Changes in physiological reactivity in response to the trauma memory during prolonged exposure and virtual reality exposure therapy for posttraumatic stress disorder. Psychol Trauma. 2020;12(7):756-64. Epub 20200427. PubMed PMID: 32338946. [CrossRef]
- Anderson PL, Price M, Edwards SM, Obasaju MA, Schmertz SK, Zimand E, et al. Virtual reality exposure therapy for social anxiety disorder: a randomized controlled trial. J Consult Clin Psychol. 2013;81(5):751-60. Epub 20130624. PubMed PMID: 23796315. [CrossRef]
- Anderson PL, Zimand E, Hodges LF, Rothbaum BO. Cognitive behavioral therapy for public-speaking anxiety using virtual reality for exposure. Depress Anxiety. 2005;22(3):156-8. PubMed PMID: 16231290. [CrossRef]
- Kim MK, Eom H, Kwon JH, Kyeong S, Kim JJ. Neural effects of a short-term virtual reality self-training program to reduce social anxiety. Psychol Med. 2022;52(7):1296-305. Epub 20200903. PubMed PMID: 32880252. [CrossRef]
- Lee S, Ahmed T, Kim H, Choi S, Kim DS, Kim SJ, et al. Bidirectional modulation of fear extinction by mediodorsal thalamic firing in mice. Nat Neurosci. 2011;15(2):308-14. Epub 20111225. PubMed PMID: 22197828. [CrossRef]
- Rubin M, Muller K, Hayhoe MM, Telch MJ. Attention guidance augmentation of virtual reality exposure therapy for social anxiety disorder: a pilot randomized controlled trial. Cogn Behav Ther. 2022;51(5):371-87. Epub 20220406. PubMed PMID: 35383544; PubMed Central PMCID: PMC9458616. [CrossRef]
- Zainal NH, Chan WW, Saxena AP, Taylor CB, Newman MG. Pilot randomized trial of self-guided virtual reality exposure therapy for social anxiety disorder. Behav Res Ther. 2021;147:103984. Epub 20211006. PubMed PMID: 34740099; PubMed Central PMCID: PMC8759454. [CrossRef]
- Bouchard S, Dumoulin S, Robillard G, Guitard T, Klinger É, Forget H, et al. Virtual reality compared with. Br J Psychiatry. 2017;210(4):276-83. Epub 20161215. PubMed PMID: 27979818. [CrossRef]
- Kampmann IL, Emmelkamp PM, Hartanto D, Brinkman WP, Zijlstra BJ, Morina N. Exposure to virtual social interactions in the treatment of social anxiety disorder: A randomized controlled trial. Behav Res Ther. 2016;77:147-56. Epub 20151229. PubMed PMID: 26752328. [CrossRef]
- Wang TC, Sit CH, Tang TW, Tsai CL. Psychological and Physiological Responses in Patients with Generalized Anxiety Disorder: The Use of Acute Exercise and Virtual Reality Environment. Int J Environ Res Public Health. 2020;17(13). Epub 20200706. PubMed PMID: 32640554; PubMed Central PMCID: PMC7370051. [CrossRef]
- Gorini A, Pallavicini F, Algeri D, Repetto C, Gaggioli A, Riva G. Virtual reality in the treatment of generalized anxiety disorders. Stud Health Technol Inform. 2010;154:39-43. PubMed PMID: 20543266.
- Pitti CT, Peñate W, de la Fuente J, Bethencourt JM, Roca-Sánchez MJ, Acosta L, et al. The combined use of virtual reality exposure in the treatment of agoraphobia. Actas Esp Psiquiatr. 2015;43(4):133-41. Epub 20150701. PubMed PMID: 26150057.
- Malbos E, Rapee RM, Kavakli M. A controlled study of agoraphobia and the independent effect of virtual reality exposure therapy. Aust N Z J Psychiatry. 2013;47(2):160-8. Epub 20120711. PubMed PMID: 22790176. [CrossRef]
- Wald J, Taylor S. Preliminary research on the efficacy of virtual reality exposure therapy to treat driving phobia. Cyberpsychol Behav. 2003;6(5):459-65. PubMed PMID: 14583121. [CrossRef]
- Powers MB, Briceno NF, Gresham R, Jouriles EN, Emmelkamp PM, Smits JA. Do conversations with virtual avatars increase feelings of social anxiety? J Anxiety Disord. 2013;27(4):398-403. Epub 20130326. PubMed PMID: 23746490. [CrossRef]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33-47. PubMed PMID: 7042457. [CrossRef]
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615-23. PubMed PMID: 10965637. [CrossRef]
- Depression in adults: treatment and management. 2022.
- Spinhoven P, Hoogerwerf E, van Giezen A, Greeven A. Mindfulness-based cognitive group therapy for treatment-refractory anxiety disorder: A pragmatic randomized controlled trial. J Anxiety Disord. 2022;90:102599. Epub 20220623. PubMed PMID: 35777128. [CrossRef]
- Sado M, Park S, Ninomiya A, Sato Y, Fujisawa D, Shirahase J, et al. Feasibility study of mindfulness-based cognitive therapy for anxiety disorders in a Japanese setting. BMC Res Notes. 2018;11(1):653. Epub 20180906. PubMed PMID: 30189900; PubMed Central PMCID: PMC6127937. [CrossRef]
- Li J, Cai Z, Li X, Du R, Shi Z, Hua Q, et al. Mindfulness-based therapy versus cognitive behavioral therapy for people with anxiety symptoms: a systematic review and meta-analysis of random controlled trials. Ann Palliat Med. 2021;10(7):7596-612. PubMed PMID: 34353047. [CrossRef]
- Haller H, Breilmann P, Schröter M, Dobos G, Cramer H. A systematic review and meta-analysis of acceptance- and mindfulness-based interventions for DSM-5 anxiety disorders. Sci Rep. 2021;11(1):20385. Epub 20211014. PubMed PMID: 34650179; PubMed Central PMCID: PMC8516851. [CrossRef]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther. 2007;45(10):2518-26. Epub 20070503. PubMed PMID: 17572382. [CrossRef]
- Goldin PR, Morrison A, Jazaieri H, Brozovich F, Heimberg R, Gross JJ. Group CBT versus MBSR for social anxiety disorder: A randomized controlled trial. J Consult Clin Psychol. 2016;84(5):427-37. Epub 20160307. PubMed PMID: 26950097; PubMed Central PMCID: PMC4837056. [CrossRef]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10(1):83-91. PubMed PMID: 20141305; PubMed Central PMCID: PMC4203918. [CrossRef]
- Shikatani B, Antony MM, Kuo JR, Cassin SE. The impact of cognitive restructuring and mindfulness strategies on postevent processing and affect in social anxiety disorder. J Anxiety Disord. 2014;28(6):570-9. Epub 20140620. PubMed PMID: 24983798. [CrossRef]
- Koszycki D, Thake J, Mavounza C, Daoust JP, Taljaard M, Bradwejn J. Preliminary Investigation of a Mindfulness-Based Intervention for Social Anxiety Disorder That Integrates Compassion Meditation and Mindful Exposure. J Altern Complement Med. 2016;22(5):363-74. Epub 20160412. PubMed PMID: 27070853. [CrossRef]
- Koszycki D, Guérin E, DiMillo J, Bradwejn J. Randomized trial of cognitive behaviour group therapy and a mindfulness-based intervention for social anxiety disorder: Preliminary findings. Clin Psychol Psychother. 2021;28(1):200-18. Epub 20200825. PubMed PMID: 32818325. [CrossRef]
- Hoge EA, Bui E, Palitz SA, Schwarz NR, Owens ME, Johnston JM, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-32. Epub 20170126. PubMed PMID: 28131433; PubMed Central PMCID: PMC5526744. [CrossRef]
- Jiang SS, Liu XH, Han N, Zhang HJ, Xie WX, Xie ZJ, et al. Effects of group mindfulness-based cognitive therapy and group cognitive behavioural therapy on symptomatic generalized anxiety disorder: a randomized controlled noninferiority trial. BMC Psychiatry. 2022;22(1):481. Epub 20220719. PubMed PMID: 35854250; PubMed Central PMCID: PMC9295460. [CrossRef]
- Hoge EA, Guidos BM, Mete M, Bui E, Pollack MH, Simon NM, et al. Effects of mindfulness meditation on occupational functioning and health care utilization in individuals with anxiety. J Psychosom Res. 2017;95:7-11. Epub 20170123. PubMed PMID: 28314552. [CrossRef]
- Wong SY, Yip BH, Mak WW, Mercer S, Cheung EY, Ling CY, et al. Mindfulness-based cognitive therapy v. group psychoeducation for people with generalised anxiety disorder: randomised controlled trial. Br J Psychiatry. 2016;209(1):68-75. Epub 20160204. PubMed PMID: 26846612. [CrossRef]
- Kim B, Lee SH, Kim YW, Choi TK, Yook K, Suh SY, et al. Effectiveness of a mindfulness-based cognitive therapy program as an adjunct to pharmacotherapy in patients with panic disorder. J Anxiety Disord. 2010;24(6):590-5. Epub 20100403. PubMed PMID: 20427148. [CrossRef]
- Liu X, Yi P, Ma L, Liu W, Deng W, Yang X, et al. Mindfulness-based interventions for social anxiety disorder: A systematic review and meta-analysis. Psychiatry Res. 2021;300:113935. Epub 20210420. PubMed PMID: 33895444. [CrossRef]
- Cocchi L, Zalesky A, Nott Z, Whybird G, Fitzgerald PB, Breakspear M. Transcranial magnetic stimulation in obsessive-compulsive disorder: A focus on network mechanisms and state dependence. Neuroimage Clin. 2018;19:661-74. Epub 20180523. PubMed PMID: 30023172; PubMed Central PMCID: PMC6047114. [CrossRef]
- Hyde J, Carr H, Kelley N, Seneviratne R, Reed C, Parlatini V, et al. Efficacy of neurostimulation across mental disorders: systematic review and meta-analysis of 208 randomized controlled trials. Mol Psychiatry. 2022;27(6):2709-19. Epub 20220401. PubMed PMID: 35365806; PubMed Central PMCID: PMC8973679. [CrossRef]
- Camprodon JA, Pascual-Leone A. Multimodal Applications of Transcranial Magnetic Stimulation for Circuit-Based Psychiatry. JAMA Psychiatry. 2016;73(4):407-8. PubMed PMID: 26981644. [CrossRef]
- Cirillo P, Gold AK, Nardi AE, Ornelas AC, Nierenberg AA, Camprodon J, et al. Transcranial magnetic stimulation in anxiety and trauma-related disorders: A systematic review and meta-analysis. Brain Behav. 2019;9(6):e01284. Epub 20190507. PubMed PMID: 31066227; PubMed Central PMCID: PMC6576151. [CrossRef]
- Klomjai W, Katz R, Lackmy-Vallée A. Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS). Ann Phys Rehabil Med. 2015;58(4):208-13. Epub 20150828. PubMed PMID: 26319963. [CrossRef]
- Petrides M. Impairments on nonspatial self-ordered and externally ordered working memory tasks after lesions of the mid-dorsal part of the lateral frontal cortex in the monkey. J Neurosci. 1995;15(1 Pt 1):359-75. PubMed PMID: 7823141; PubMed Central PMCID: PMC6578311. [CrossRef]
- Sturm VE, Haase CM, Levenson RW. Chapter 22 - Emotional Dysfunction in Psychopathology and Neuropathology: Neural and Genetic Pathways. In: Lehner T, Miller BL, State MW, editors. Genomics, Circuits, and Pathways in Clinical Neuropsychiatry. San Diego: Academic Press; 2016. p. 345-64.
- Qin S, Hermans EJ, van Marle HJ, Luo J, Fernández G. Acute psychological stress reduces working memory-related activity in the dorsolateral prefrontal cortex. Biol Psychiatry. 2009;66(1):25-32. Epub 20090428. PubMed PMID: 19403118. [CrossRef]
- Balderston NL, Beydler EM, Roberts C, Deng ZD, Radman T, Lago T, et al. Mechanistic link between right prefrontal cortical activity and anxious arousal revealed using transcranial magnetic stimulation in healthy subjects. Neuropsychopharmacology. 2020;45(4):694-702. Epub 20191202. PubMed PMID: 31791039; PubMed Central PMCID: PMC7021903. [CrossRef]
- Gibson BC, Vakhtin A, Clark VP, Abbott CC, Quinn DK. Revisiting Hemispheric Asymmetry in Mood Regulation: Implications for rTMS for Major Depressive Disorder. Brain Sci. 2022;12(1). Epub 20220114. PubMed PMID: 35053856; PubMed Central PMCID: PMC8774216. [CrossRef]
- Balconi M, Ferrari C. Left DLPFC rTMS stimulation reduced the anxiety bias effect or how to restore the positive memory processing in high-anxiety subjects. Psychiatry Res. 2013;209(3):554-9. Epub 20130417. PubMed PMID: 23601793. [CrossRef]
- Diefenbach GJ, Bragdon LB, Zertuche L, Hyatt CJ, Hallion LS, Tolin DF, et al. Repetitive transcranial magnetic stimulation for generalised anxiety disorder: a pilot randomised, double-blind, sham-controlled trial. Br J Psychiatry. 2016;209(3):222-8. Epub 20160519. PubMed PMID: 27198484. [CrossRef]
- Mochcovitch MD, da Rocha Freire RC, Garcia RF, Nardi AE. A systematic review of fMRI studies in generalized anxiety disorder: evaluating its neural and cognitive basis. J Affect Disord. 2014;167:336-42. Epub 20140702. PubMed PMID: 25020268. [CrossRef]
- Assaf M, Rabany L, Zertuche L, Bragdon L, Tolin D, Goethe J, et al. Neural functional architecture and modulation during decision making under uncertainty in individuals with generalized anxiety disorder. Brain Behav. 2018;8(8):e01015. Epub 20180621. PubMed PMID: 29931835; PubMed Central PMCID: PMC6085921. [CrossRef]
- Bystritsky A, Kaplan JT, Feusner JD, Kerwin LE, Wadekar M, Burock M, et al. A preliminary study of fMRI-guided rTMS in the treatment of generalized anxiety disorder. J Clin Psychiatry. 2008;69(7):1092-8. PubMed PMID: 18572984. [CrossRef]
- Diefenbach GJ, Assaf M, Goethe JW, Gueorguieva R, Tolin DF. Improvements in emotion regulation following repetitive transcranial magnetic stimulation for generalized anxiety disorder. J Anxiety Disord. 2016;43:1-7. Epub 20160709. PubMed PMID: 27467027. [CrossRef]
- Huang Z, Li Y, Bianchi MT, Zhan S, Jiang F, Li N, et al. Repetitive transcranial magnetic stimulation of the right parietal cortex for comorbid generalized anxiety disorder and insomnia: A randomized, double-blind, sham-controlled pilot study. Brain Stimul. 2018;11(5):1103-9. Epub 20180529. PubMed PMID: 29871798. [CrossRef]
- Wang L, Zhou QH, Wang K, Wang HC, Hu SM, Yang YX, et al. Frontoparietal paired associative stimulation versus single-site stimulation for generalized anxiety disorder: a pilot rTMS study. J Psychiatry Neurosci. 2022;47(2):E153-E61. Epub 20220427. PubMed PMID: 35477683; PubMed Central PMCID: PMC9259432. [CrossRef]
- Dilkov D, Hawken ER, Kaludiev E, Milev R. Repetitive transcranial magnetic stimulation of the right dorsal lateral prefrontal cortex in the treatment of generalized anxiety disorder: A randomized, double-blind sham controlled clinical trial. Prog Neuropsychopharmacol Biol Psychiatry. 2017;78:61-5. Epub 20170519. PubMed PMID: 28533148. [CrossRef]
- d'Andrea G, Mancusi G, Santovito MC, Marrangone C, Martino F, Santorelli M, et al. Investigating the Role of Maintenance TMS Protocols for Major Depression: Systematic Review and Future Perspectives for Personalized Interventions. J Pers Med. 2023;13(4). Epub 20230421. PubMed PMID: 37109083; PubMed Central PMCID: PMC10141590. [CrossRef]
- Paes F, Baczynski T, Novaes F, Marinho T, Arias-Carrión O, Budde H, et al. Repetitive Transcranial Magnetic Stimulation (rTMS) to Treat Social Anxiety Disorder: Case Reports and a Review of the Literature. Clin Pract Epidemiol Ment Health. 2013;9:180-8. Epub 20131031. PubMed PMID: 24278088; PubMed Central PMCID: PMC3837365. [CrossRef]
- Minervini A, LaVarco A, Zorns S, Propper R, Suriano C, Keenan JP. Excitatory Dorsal Lateral Prefrontal Cortex Transcranial Magnetic Stimulation Increases Social Anxiety. Brain Sci. 2023;13(7). Epub 20230624. PubMed PMID: 37508921; PubMed Central PMCID: PMC10377502. [CrossRef]
- Tomita N, Katayama H, Kurihara Y, Takahashi T, Shibata S, Mima T, et al. Tackling social anxiety with targeted brain stimulation: investigating the effects of transcranial static magnetic field stimulation on self-focused attention. Front Behav Neurosci. 2024;18:1373564. Epub 20240313. PubMed PMID: 38545414; PubMed Central PMCID: PMC10965766. [CrossRef]
- Leuchter MK, Rosenberg BM, Schapira G, Wong NR, Leuchter AF, McGlade AL, et al. Treatment of Spider Phobia Using Repeated Exposures and Adjunctive Repetitive Transcranial Magnetic Stimulation: A Proof-of-Concept Study. Front Psychiatry. 2022;13:823158. Epub 20220315. PubMed PMID: 35370840; PubMed Central PMCID: PMC8965447. [CrossRef]
- Cohen H, Kaplan Z, Kotler M, Kouperman I, Moisa R, Grisaru N. Repetitive transcranial magnetic stimulation of the right dorsolateral prefrontal cortex in posttraumatic stress disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2004;161(3):515-24. PubMed PMID: 14992978. [CrossRef]
- Boggio PS, Rocha M, Oliveira MO, Fecteau S, Cohen RB, Campanhã C, et al. Noninvasive brain stimulation with high-frequency and low-intensity repetitive transcranial magnetic stimulation treatment for posttraumatic stress disorder. J Clin Psychiatry. 2010;71(8):992-9. Epub 20091229. PubMed PMID: 20051219; PubMed Central PMCID: PMC3260527. [CrossRef]
- Watts BV, Landon B, Groft A, Young-Xu Y. A sham controlled study of repetitive transcranial magnetic stimulation for posttraumatic stress disorder. Brain Stimul. 2012;5(1):38-43. Epub 20110303. PubMed PMID: 22264669. [CrossRef]
- Isserles M, Shalev AY, Roth Y, Peri T, Kutz I, Zlotnick E, et al. Effectiveness of deep transcranial magnetic stimulation combined with a brief exposure procedure in post-traumatic stress disorder--a pilot study. Brain Stimul. 2013;6(3):377-83. Epub 20120818. PubMed PMID: 22921765. [CrossRef]
- Grisaru N, Amir M, Cohen H, Kaplan Z. Effect of transcranial magnetic stimulation in posttraumatic stress disorder: a preliminary study. Biol Psychiatry. 1998;44(1):52-5. PubMed PMID: 9646883. [CrossRef]
- Salehpour F, Mahmoudi J, Kamari F, Sadigh-Eteghad S, Rasta SH, Hamblin MR. Brain Photobiomodulation Therapy: a Narrative Review. Mol Neurobiol. 2018;55(8):6601-36. Epub 20180111. PubMed PMID: 29327206; PubMed Central PMCID: PMC6041198. [CrossRef]
- Schiffer F, Johnston AL, Ravichandran C, Polcari A, Teicher MH, Webb RH, et al. Psychological benefits 2 and 4 weeks after a single treatment with near infrared light to the forehead: a pilot study of 10 patients with major depression and anxiety. Behav Brain Funct. 2009;5:46. Epub 20091208. PubMed PMID: 19995444; PubMed Central PMCID: PMC2796659. [CrossRef]
- Wang H, Song P, Hou Y, Liu J, Hao W, Hu S, et al. 820-nm Transcranial near-infrared stimulation on the left DLPFC relieved anxiety: A randomized, double-blind, sham-controlled study. Brain Res Bull. 2023;200:110682. Epub 20230608. PubMed PMID: 37301483. [CrossRef]
- Huang CJ, Lin CH, Wu JI, Yang WC. The Relationship Between Depression Symptoms and Anxiety Symptoms During Acute ECT for Patients With Major Depressive Disorder. Int J Neuropsychopharmacol. 2019;22(10):609-15. PubMed PMID: 31282929; PubMed Central PMCID: PMC6822139. [CrossRef]
- Watts BV. Electroconvulsive therapy for comorbid major depressive disorder and posttraumatic stress disorder. J ECT. 2007;23(2):93-5. PubMed PMID: 17548978. [CrossRef]
- Andrade C, McCall WV, Youssef NA. Electroconvulsive therapy for post-traumatic stress disorder: efficacy, mechanisms and a hypothesis for new directions. Expert Rev Neurother. 2016;16(7):749-53. Epub 20160503. PubMed PMID: 27095363. [CrossRef]
- Tang VM, Trought K, Gicas KM, Kozak M, Josselyn SA, Daskalakis ZJ, et al. Electroconvulsive therapy with a memory reactivation intervention for post-traumatic stress disorder: A randomized controlled trial. Brain Stimul. 2021;14(3):635-42. Epub 20210327. PubMed PMID: 33785406. [CrossRef]
- Youssef NA, Dhanani S, Rosenquist PB, McCloud L, McCall WV. Treating Posttraumatic Stress Disorder Symptoms With Low Amplitude Seizure Therapy (LAP-ST) Compared With Standard Right Unilateral Electroconvulsive Therapy: A Pilot Double-Blinded Randomized Clinical Trial. J ECT. 2020;36(4):291-5. PubMed PMID: 33215889. [CrossRef]
- Youssef NA, McCall WV, Andrade C. The role of ECT in posttraumatic stress disorder: A systematic review. Ann Clin Psychiatry. 2017;29(1):62-70. PubMed PMID: 28207917.
- Zhong M, Liu Q, Li L, Tang VM, Wong AHC, Liu Y. Evaluating the effect of electroconvulsive therapy (ECT) on post-traumatic stress disorder (PTSD): A systematic review and meta-analysis of five studies. J Psychiatr Res. 2023;164:37-45. Epub 20230601. PubMed PMID: 37311402. [CrossRef]
- Browne TG. Biofeedback and Neurofeedback. In: Friedman HS, editor. Encyclopedia of Mental Health (Second Edition). Oxford: Academic Press; 2016. p. 170-7.
- Fernández-Alvarez J, Grassi M, Colombo D, Botella C, Cipresso P, Perna G, et al. Efficacy of bio- and neurofeedback for depression: a meta-analysis. Psychol Med. 2022;52(2):201-16. Epub 20211115. PubMed PMID: 34776024; PubMed Central PMCID: PMC8842225. [CrossRef]
- Hou Y, Zhang S, Li N, Huang Z, Wang L, Wang Y. Neurofeedback training improves anxiety trait and depressive symptom in GAD. Brain Behav. 2021;11(3):e02024. Epub 20210127. PubMed PMID: 33503332; PubMed Central PMCID: PMC7994677. [CrossRef]
- Clancy K, Ding M, Bernat E, Schmidt NB, Li W. Restless 'rest': intrinsic sensory hyperactivity and disinhibition in post-traumatic stress disorder. Brain. 2017;140(7):2041-50. PubMed PMID: 28582479; PubMed Central PMCID: PMC6059177. [CrossRef]
- Elsadek M, Liu B, Lian Z. Green façades: Their contribution to stress recovery and well-being in high-density cities. Urban Forestry & Urban Greening. 2019;46:126446. Pathological fear, anxiety and negative affect exhibit distinct neurostructural signatures: evidence from psychiatric neuroimaging meta-analysis. [CrossRef]
- Liu X, Klugah-Brown B, Zhang R, Chen H, Zhang J, Becker B. Transl Psychiatry. 2022;12(1):405. Epub 20220923. PubMed PMID: 36151073; PubMed Central PMCID: PMC9508096. [CrossRef]
- Egner T, Gruzelier JH. Ecological validity of neurofeedback: modulation of slow wave EEG enhances musical performance. Neuroreport. 2003;14(9):1221-4. PubMed PMID: 12824763. [CrossRef]
- Raymond J, Sajid I, Parkinson LA, Gruzelier JH. Biofeedback and dance performance: a preliminary investigation. Appl Psychophysiol Biofeedback. 2005;30(1):64-73. PubMed PMID: 15889586. [CrossRef]
- Mathews A, Mackintosh B. Induced emotional interpretation bias and anxiety. J Abnorm Psychol. 2000;109(4):602-15. PubMed PMID: 11195984.
- Mogg K, Bradley BP. Attentional bias in generalized anxiety disorder versus depressive disorder. Cognitive Therapy and Research. 2005;29(1):29-45. PubMed PMID: WOS:000227362300003. [CrossRef]
- Dadashi M, Birashk B, Taremian F, Asgarnejad AA, Momtazi S. Effects of Increase in Amplitude of Occipital Alpha & Theta Brain Waves on Global Functioning Level of Patients with GAD. Basic Clin Neurosci. 2015;6(1):14-20. PubMed PMID: 27504152; PubMed Central PMCID: PMC4741268.
- Rice KM, Blanchard EB, Purcell M. Biofeedback treatments of generalized anxiety disorder: preliminary results. Biofeedback Self Regul. 1993;18(2):93-105. PubMed PMID: 8324040. [CrossRef]
- Tolin DF, Davies CD, Moskow DM, Hofmann SG. Biofeedback and Neurofeedback for Anxiety Disorders: A Quantitative and Qualitative Systematic Review. Adv Exp Med Biol. 2020;1191:265-89. PubMed PMID: 32002934. [CrossRef]
- Schoneveld EA, Lichtwarck-Aschoff A, Granic I. Preventing Childhood Anxiety Disorders: Is an Applied Game as Effective as a Cognitive Behavioral Therapy-Based Program? Prev Sci. 2018;19(2):220-32. PubMed PMID: 28956222; PubMed Central PMCID: PMC5801383. [CrossRef]
- Scheinost D, Stoica T, Saksa J, Papademetris X, Constable RT, Pittenger C, et al. Orbitofrontal cortex neurofeedback produces lasting changes in contamination anxiety and resting-state connectivity. Transl Psychiatry. 2013;3(4):e250. Epub 20130430. PubMed PMID: 23632454; PubMed Central PMCID: PMC3641411. [CrossRef]
- Wang S, Zhao Y, Chen S, Lin G, Sun P, Wang T. EEG biofeedback improves attentional bias in high trait anxiety individuals. BMC Neurosci. 2013;14:115. Epub 20131007. PubMed PMID: 24099141; PubMed Central PMCID: PMC4124890. [CrossRef]
- Park SJ, Roth M. Heart Rate Variability Biofeedback as Adjunctive Treatment of Generalized Anxiety Disorder: A Case Report. Integr Med (Encinitas). 2023;22(4):42-7. PubMed PMID: 37752932; PubMed Central PMCID: PMC10519238.
- Jaspal Singh S, Maman P, Hitanshu A. Biofeedback Approach in The Treatment of Generalized Anxiety Disorder. Iranian Journal of Psychiatry. 1970;2(3).
- Reiner R. Integrating a portable biofeedback device into clinical practice for patients with anxiety disorders: results of a pilot study. Appl Psychophysiol Biofeedback. 2008;33(1):55-61. Epub 20080220. PubMed PMID: 18286369. [CrossRef]
- Gerlach AL, Mourlane D, Rist F. Public and private heart rate feedback in social phobia: a manipulation of anxiety visibility. Cogn Behav Ther. 2004;33(1):36-45. PubMed PMID: 15224627. [CrossRef]
- Nilsson JE, Lundh LG, Faghihi S, Roth-Andersson G. The enhancement of beneficial effects following audio feedback by cognitive preparation in the treatment of social anxiety: a single-session experiment. J Behav Ther Exp Psychiatry. 2011;42(4):497-503. Epub 20110531. PubMed PMID: 21683053. [CrossRef]
- Nilsson JE, Lundh LG. Audio Feedback with Reduced Self-focus as an Intervention for Social Anxiety: An Experimental Study. Cogn Behav Ther. 2016;45(2):150-62. Epub 20160111. PubMed PMID: 26935474. [CrossRef]
- Nicholson AA, Ros T, Frewen PA, Densmore M, Théberge J, Kluetsch RC, et al. Alpha oscillation neurofeedback modulates amygdala complex connectivity and arousal in posttraumatic stress disorder. Neuroimage Clin. 2016;12:506-16. Epub 20160714. PubMed PMID: 27672554; PubMed Central PMCID: PMC5030332. [CrossRef]
- Rosaura Polak A, Witteveen AB, Denys D, Olff M. Breathing biofeedback as an adjunct to exposure in cognitive behavioral therapy hastens the reduction of PTSD symptoms: a pilot study. Appl Psychophysiol Biofeedback. 2015;40(1):25-31. PubMed PMID: 25750106; PubMed Central PMCID: PMC4375291. [CrossRef]
- Lande RG, Williams LB, Francis JL, Gragnani C, Morin ML. Efficacy of biofeedback for post-traumatic stress disorder. Complement Ther Med. 2010;18(6):256-9. Epub 20100915. PubMed PMID: 21130362. [CrossRef]
- Shapiro F. The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Perm J. 2014;18(1):71-7. PubMed PMID: 24626074; PubMed Central PMCID: PMC3951033. [CrossRef]
- Auren TJB, Klæth JR, Jensen AG, Solem S. Intensive outpatient treatment for PTSD: an open trial combining prolonged exposure therapy, EMDR, and physical activity. Eur J Psychotraumatol. 2022;13(2):2128048. Epub 20221007. PubMed PMID: 36237826; PubMed Central PMCID: PMC9553174. [CrossRef]
- Klaeth JR, Jensen AG, Auren TJB, Solem S. 12-month follow-up of intensive outpatient treatment for PTSD combining prolonged exposure therapy, EMDR and physical activity. BMC Psychiatry. 2024;24(1):225. Epub 20240326. PubMed PMID: 38532374; PubMed Central PMCID: PMC10964674. [CrossRef]
- Hudays A, Gallagher R, Hazazi A, Arishi A, Bahari G. Eye Movement Desensitization and Reprocessing versus Cognitive Behavior Therapy for Treating Post-Traumatic Stress Disorder: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2022;19(24). Epub 20221215. PubMed PMID: 36554717; PubMed Central PMCID: PMC9778888. [CrossRef]
- Guidelines for the Management of Conditions Specifically Related to Stress. 2013.
- Rasines-Laudes P, Serrano-Pintado I. Efficacy of EMDR in Post-Traumatic Stress Disorder: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Psicothema. 2023;35(4):385-96. PubMed PMID: 37882423. [CrossRef]
- Cuijpers P, Veen SCV, Sijbrandij M, Yoder W, Cristea IA. Eye movement desensitization and reprocessing for mental health problems: a systematic review and meta-analysis. Cogn Behav Ther. 2020;49(3):165-80. Epub 20200211. PubMed PMID: 32043428. [CrossRef]
- Wright SL, Karyotaki E, Cuijpers P, Bisson J, Papola D, Witteveen A, et al. EMDR. Psychol Med. 2024;54(8):1580-8. Epub 20240104. PubMed PMID: 38173121. [CrossRef]
- Torres-Giménez A, Garcia-Gibert C, Gelabert E, Mallorquí A, Segu X, Roca-Lecumberri A, et al. Efficacy of EMDR for early intervention after a traumatic event: A systematic review and meta-analysis. J Psychiatr Res. 2024;174:73-83. Epub 20240411. PubMed PMID: 38626564. [CrossRef]
- Shiozawa P, Silva ME, Carvalho TC, Cordeiro Q, Brunoni AR, Fregni F. Transcutaneous vagus and trigeminal nerve stimulation for neuropsychiatric disorders: a systematic review. Arq Neuropsiquiatr. 2014;72(7):542-7. PubMed PMID: 25054988. [CrossRef]
- Wu C, Liu P, Fu H, Chen W, Cui S, Lu L, et al. Transcutaneous auricular vagus nerve stimulation in treating major depressive disorder: A systematic review and meta-analysis. Medicine (Baltimore). 2018;97(52):e13845. PubMed PMID: 30593183; PubMed Central PMCID: PMC6314717. [CrossRef]
- Garcia RG, Cohen JE, Stanford AD, Gabriel A, Stowell J, Aizley H, et al. Respiratory-gated auricular vagal afferent nerve stimulation (RAVANS) modulates brain response to stress in major depression. J Psychiatr Res. 2021;142:188-97. Epub 20210802. PubMed PMID: 34365067; PubMed Central PMCID: PMC8429271. [CrossRef]
- Sartory G, Olajide D. Vagal innervation techniques in the treatment of panic disorder. Behav Res Ther. 1988;26(5):431-4. PubMed PMID: 3056393. [CrossRef]
- Burger AM, Verkuil B, Van Diest I, Van der Does W, Thayer JF, Brosschot JF. The effects of transcutaneous vagus nerve stimulation on conditioned fear extinction in humans. Neurobiol Learn Mem. 2016;132:49-56. Epub 20160521. PubMed PMID: 27222436. [CrossRef]
- Verkuil B, Burger AM. Transcutaneous vagus nerve stimulation does not affect attention to fearful faces in high worriers. Behav Res Ther. 2019;113:25-31. Epub 20181219. PubMed PMID: 30583233. [CrossRef]
- Burger AM, Van der Does W, Thayer JF, Brosschot JF, Verkuil B. Transcutaneous vagus nerve stimulation reduces spontaneous but not induced negative thought intrusions in high worriers. Biol Psychol. 2019;142:80-9. Epub 20190130. PubMed PMID: 30710565. [CrossRef]
- Walpola IC, Nest T, Roseman L, Erritzoe D, Feilding A, Nutt DJ, et al. Altered Insula Connectivity under MDMA. Neuropsychopharmacology. 2017;42(11):2152-62. Epub 20170214. PubMed PMID: 28195139; PubMed Central PMCID: PMC5603811. [CrossRef]
- Danforth AL, Struble CM, Yazar-Klosinski B, Grob CS. MDMA-assisted therapy: A new treatment model for social anxiety in autistic adults. Prog Neuropsychopharmacol Biol Psychiatry. 2016;64:237-49. Epub 20150325. PubMed PMID: 25818246. [CrossRef]
- Mithoefer MC, Feduccia AA, Jerome L, Mithoefer A, Wagner M, Walsh Z, et al. MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology (Berl). 2019;236(9):2735-45. Epub 20190507. PubMed PMID: 31065731; PubMed Central PMCID: PMC6695343. [CrossRef]
- Danforth AL, Grob CS, Struble C, Feduccia AA, Walker N, Jerome L, et al. Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: a randomized, double-blind, placebo-controlled pilot study. Psychopharmacology (Berl). 2018;235(11):3137-48. Epub 20180908. PubMed PMID: 30196397; PubMed Central PMCID: PMC6208958. [CrossRef]
- Keramidas ME, Kölegård R, Eiken O. Hypoxia gradually augments metabolic and thermoperceptual responsiveness to repeated whole-body cold stress in humans. Exp Physiol. 2020;105(12):2123-40. Epub 20201116. PubMed PMID: 33140429; PubMed Central PMCID: PMC7756580. [CrossRef]
- Rymaszewska J, Biały D, Zagrobelny Z, Kiejna A. [The influence of whole body cryotherapy on mental health]. Psychiatr Pol. 2000;34(4):649-53. PubMed PMID: 11059263.
- Rymaszewska J, Tulczynski A, Zagrobelny Z, Kiejna A, Hadrys T. Influence of whole body cryotherapy on depressive symptoms - preliminary report. Acta Neuropsychiatr. 2003;15(3):122-8. PubMed PMID: 26983354. [CrossRef]
- Rymaszewska J, Ramsey D, Chładzińska-Kiejna S, Kiejna A. [Can short-term exposure to extremely low temperatures be used as an adjuvant therapy in the treatment of affective and anxiety disorders?]. Psychiatr Pol. 2007;41(5):625-36. PubMed PMID: 18421919.
- Rymaszewska J, Ramsey D, Chładzińska-Kiejna S. Whole-body cryotherapy as adjunct treatment of depressive and anxiety disorders. Arch Immunol Ther Exp (Warsz). 2008;56(1):63-8. Epub 20080205. PubMed PMID: 18250970; PubMed Central PMCID: PMC2734249. [CrossRef]
- Szczepańska-Gieracha J, Borsuk P, Pawik M, Rymaszewska J. Mental state and quality of life after 10 session whole-body cryotherapy. Psychol Health Med. 2014;19(1):40-6. Epub 20130327. PubMed PMID: 23535078. [CrossRef]
- Lee EJ, Frazier SK. The efficacy of acupressure for symptom management: a systematic review. J Pain Symptom Manage. 2011;42(4):589-603. Epub 20110430. PubMed PMID: 21531533; PubMed Central PMCID: PMC3154967. [CrossRef]
- Kao CL, Chen CH, Lin WY, Chiao YC, Hsieh CL. Effect of auricular acupressure on peri- and early postmenopausal women with anxiety: a double-blinded, randomized, and controlled pilot study. Evid Based Complement Alternat Med. 2012;2012:567639. Epub 20120510. PubMed PMID: 22649475; PubMed Central PMCID: PMC3358095. [CrossRef]
- Mirzaee F, Hasaroeih FE, Mirzaee M, Ghazanfarpour M. Comparing the effect of acupressure with or without ice in LI-4 point on labour pain and anxiety levels during labour: a randomised controlled trial. J Obstet Gynaecol. 2021;41(3):395-400. Epub 20200612. PubMed PMID: 32530373. [CrossRef]
- Redfern RE, Chen JT, Sibrel S. Effects of Thermomechanical Stimulation during Vaccination on Anxiety, Pain, and Satisfaction in Pediatric Patients: A Randomized Controlled Trial. J Pediatr Nurs. 2018;38:1-7. Epub 20170928. PubMed PMID: 29167074. [CrossRef]
- Aktaş YY, Karabulut N. The use of cold therapy, music therapy and lidocaine spray for reducing pain and anxiety following chest tube removal. Complement Ther Clin Pract. 2019;34:179-84. Epub 20181205. PubMed PMID: 30712725. [CrossRef]
- Hur MH, Choi HS. Effects of a Thermoelectric Element Band on Venipuncture-associated Pain and Anxiety: A Randomized Controlled Trial. Asian Nurs Res (Korean Soc Nurs Sci). 2021;15(5):337-44. Epub 20211216. PubMed PMID: 34923170. [CrossRef]
- Simsek K, Ozler M, Yildirim AO, Sadir S, Demirbas S, Oztosun M, et al. Evaluation of the oxidative effect of long-term repetitive hyperbaric oxygen exposures on different brain regions of rats. ScientificWorldJournal. 2012;2012:849183. Epub 20120202. PubMed PMID: 22454610; PubMed Central PMCID: PMC3289899. [CrossRef]
- Hajhosseini B, Kuehlmann BA, Bonham CA, Kamperman KJ, Gurtner GC. Hyperbaric Oxygen Therapy: Descriptive Review of the Technology and Current Application in Chronic Wounds. Plast Reconstr Surg Glob Open. 2020;8(9):e3136. Epub 20200925. PubMed PMID: 33133975; PubMed Central PMCID: PMC7544320. [CrossRef]
- Cozene B, Sadanandan N, Gonzales-Portillo B, Saft M, Cho J, Park YJ, et al. An Extra Breath of Fresh Air: Hyperbaric Oxygenation as a Stroke Therapeutic. Biomolecules. 2020;10(9). Epub 20200904. PubMed PMID: 32899709; PubMed Central PMCID: PMC7563917. [CrossRef]
- Harch PG, Andrews SR, Fogarty EF, Amen D, Pezzullo JC, Lucarini J, et al. A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder. J Neurotrauma. 2012;29(1):168-85. Epub 20111122. PubMed PMID: 22026588. [CrossRef]
- Feng JJ, Li YH. Effects of hyperbaric oxygen therapy on depression and anxiety in the patients with incomplete spinal cord injury (a STROBE-compliant article). Medicine (Baltimore). 2017;96(29):e7334. PubMed PMID: 28723746; PubMed Central PMCID: PMC5521886. [CrossRef]
- Müller WE, Sillani G, Schuwald A, Friedland K. Pharmacological basis of the anxiolytic and antidepressant properties of Silexan®, an essential oil from the flowers of lavender. Neurochem Int. 2021;143:104899. Epub 20201109. PubMed PMID: 33181239. [CrossRef]
- Woelk H, Schläfke S. A multi-center, double-blind, randomised study of the Lavender oil preparation Silexan in comparison to Lorazepam for generalized anxiety disorder. Phytomedicine. 2010;17(2):94-9. Epub 20091203. PubMed PMID: 19962288. [CrossRef]
- Kasper S, Gastpar M, Müller WE, Volz HP, Möller HJ, Schläfke S, et al. Lavender oil preparation Silexan is effective in generalized anxiety disorder--a randomized, double-blind comparison to placebo and paroxetine. Int J Neuropsychopharmacol. 2014;17(6):859-69. Epub 20140123. PubMed PMID: 24456909. [CrossRef]
- Kasper S, Möller HJ, Volz HP, Schläfke S, Dienel A. Silexan in generalized anxiety disorder: investigation of the therapeutic dosage range in a pooled data set. Int Clin Psychopharmacol. 2017;32(4):195-204. PubMed PMID: 28379882. [CrossRef]
- Gastpar M, Müller WE, Volz HP, Möller HJ, Schläfke S, Dienel A, et al. Silexan does not cause withdrawal symptoms even when abruptly discontinued. Int J Psychiatry Clin Pract. 2017;21(3):177-80. Epub 20170320. PubMed PMID: 28319423. [CrossRef]
- Dold M, Bartova L, Volz HP, Seifritz E, Möller HJ, Schläfke S, et al. Efficacy of Silexan in patients with anxiety disorders: a meta-analysis of randomized, placebo-controlled trials. Eur Arch Psychiatry Clin Neurosci. 2023;273(7):1615-28. Epub 20230130. PubMed PMID: 36717399; PubMed Central PMCID: PMC10465640. [CrossRef]
- Crippa JA, Derenusson GN, Ferrari TB, Wichert-Ana L, Duran FL, Martin-Santos R, et al. Neural basis of anxiolytic effects of cannabidiol (CBD) in generalized social anxiety disorder: a preliminary report. J Psychopharmacol. 2011;25(1):121-30. Epub 20100909. PubMed PMID: 20829306. [CrossRef]
- Bergamaschi MM, Queiroz RH, Chagas MH, de Oliveira DC, De Martinis BS, Kapczinski F, et al. Cannabidiol reduces the anxiety induced by simulated public speaking in treatment-naïve social phobia patients. Neuropsychopharmacology. 2011;36(6):1219-26. Epub 20110209. PubMed PMID: 21307846; PubMed Central PMCID: PMC3079847. [CrossRef]
- Stanley TB, Ferretti ML, Bonn-Miller MO, Irons JG. A Double-Blind, Randomized, Placebo-Controlled Test of the Effects of Cannabidiol on Experiences of Test Anxiety Among College Students. Cannabis Cannabinoid Res. 2023;8(6):1090-9. Epub 20220720. PubMed PMID: 35861792. [CrossRef]
- Hindley G, Beck K, Borgan F, Ginestet CE, McCutcheon R, Kleinloog D, et al. Psychiatric symptoms caused by cannabis constituents: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(4):344-53. Epub 20200317. PubMed PMID: 32197092; PubMed Central PMCID: PMC7738353. [CrossRef]
- Sarris J, Stough C, Bousman CA, Wahid ZT, Murray G, Teschke R, et al. Kava in the treatment of generalized anxiety disorder: a double-blind, randomized, placebo-controlled study. J Clin Psychopharmacol. 2013;33(5):643-8. PubMed PMID: 23635869. [CrossRef]
- Savage K, Sarris J, Hughes M, Bousman CA, Rossell S, Scholey A, et al. Neuroimaging Insights: Kava's (Nutrients. 2023;15(21). Epub 20231028. PubMed PMID: 37960239; PubMed Central PMCID: PMC10649338. [CrossRef]
- Abraham KC, Connor KM, Davidson JR. Explanatory attributions of anxiety and recovery in a study of kava. J Altern Complement Med. 2004;10(3):556-9. PubMed PMID: 15253862. [CrossRef]
- Sarris J, Byrne GJ, Bousman CA, Cribb L, Savage KM, Holmes O, et al. Kava for generalised anxiety disorder: A 16-week double-blind, randomised, placebo-controlled study. Aust N Z J Psychiatry. 2020;54(3):288-97. Epub 20191208. PubMed PMID: 31813230. [CrossRef]
- Andreatini R, Sartori VA, Seabra ML, Leite JR. Effect of valepotriates (valerian extract) in generalized anxiety disorder: a randomized placebo-controlled pilot study. Phytother Res. 2002;16(7):650-4. PubMed PMID: 12410546. [CrossRef]
- Müller D, Pfeil T, von den Driesch V. Treating depression comorbid with anxiety--results of an open, practice-oriented study with St John's wort WS 5572 and valerian extract in high doses. Phytomedicine. 2003;10 Suppl 4:25-30. PubMed PMID: 12807339. [CrossRef]
- Roh D, Jung JH, Yoon KH, Lee CH, Kang LY, Lee SK, et al. Valerian extract alters functional brain connectivity: A randomized double-blind placebo-controlled trial. Phytother Res. 2019;33(4):939-48. Epub 20190110. PubMed PMID: 30632220. [CrossRef]
- Mineo L, Concerto C, Patel D, Mayorga T, Paula M, Chusid E, et al. Valeriana officinalis Root Extract Modulates Cortical Excitatory Circuits in Humans. Neuropsychobiology. 2017;75(1):46-51. Epub 20171017. PubMed PMID: 29035887. [CrossRef]
- Hieu TH, Dibas M, Surya Dila KA, Sherif NA, Hashmi MU, Mahmoud M, et al. Therapeutic efficacy and safety of chamomile for state anxiety, generalized anxiety disorder, insomnia, and sleep quality: A systematic review and meta-analysis of randomized trials and quasi-randomized trials. Phytother Res. 2019;33(6):1604-15. Epub 20190421. PubMed PMID: 31006899. [CrossRef]
- Mao JJ, Xie SX, Keefe JR, Soeller I, Li QS, Amsterdam JD. Long-term chamomile (Matricaria chamomilla L.) treatment for generalized anxiety disorder: A randomized clinical trial. Phytomedicine. 2016;23(14):1735-42. Epub 20161024. PubMed PMID: 27912875; PubMed Central PMCID: PMC5646235. [CrossRef]
- Keefe JR, Guo W, Li QS, Amsterdam JD, Mao JJ. An exploratory study of salivary cortisol changes during chamomile extract therapy of moderate to severe generalized anxiety disorder. J Psychiatr Res. 2018;96:189-95. Epub 20171016. PubMed PMID: 29080520; PubMed Central PMCID: PMC5710842. [CrossRef]
- Keefe JR, Amsterdam J, Li QS, Soeller I, DeRubeis R, Mao JJ. Specific expectancies are associated with symptomatic outcomes and side effect burden in a trial of chamomile extract for generalized anxiety disorder. J Psychiatr Res. 2017;84:90-7. Epub 20160930. PubMed PMID: 27716513; PubMed Central PMCID: PMC5589134. [CrossRef]
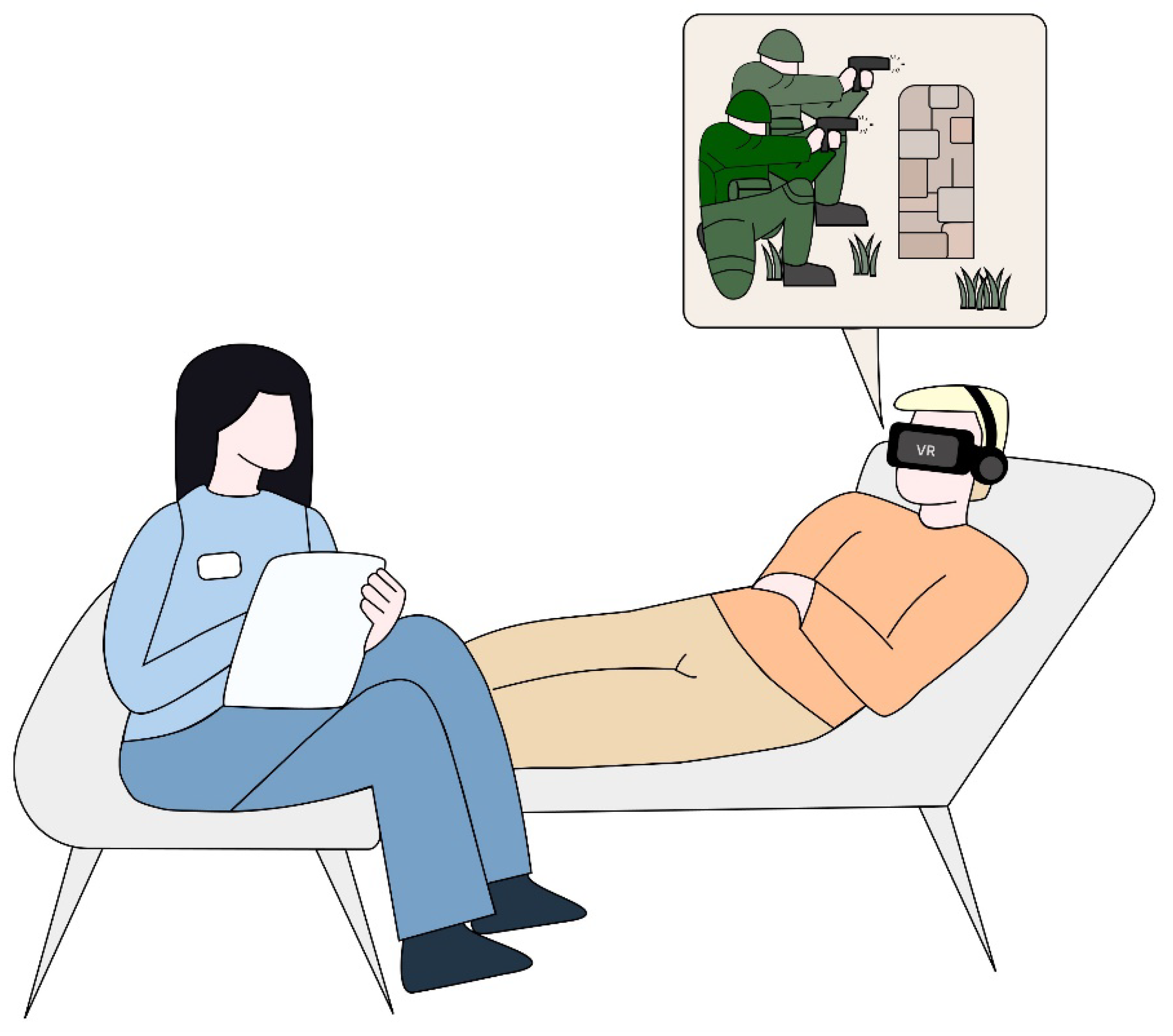
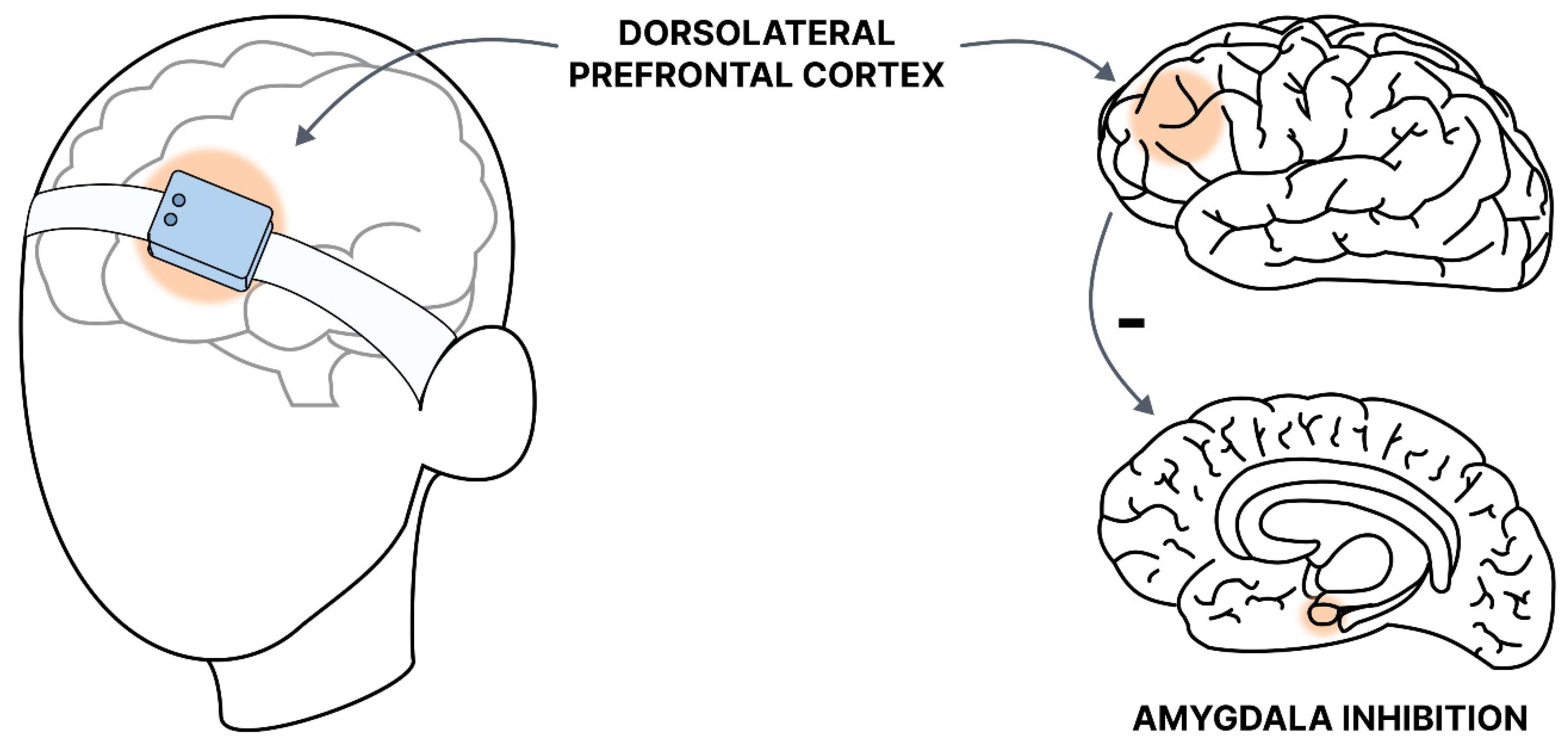
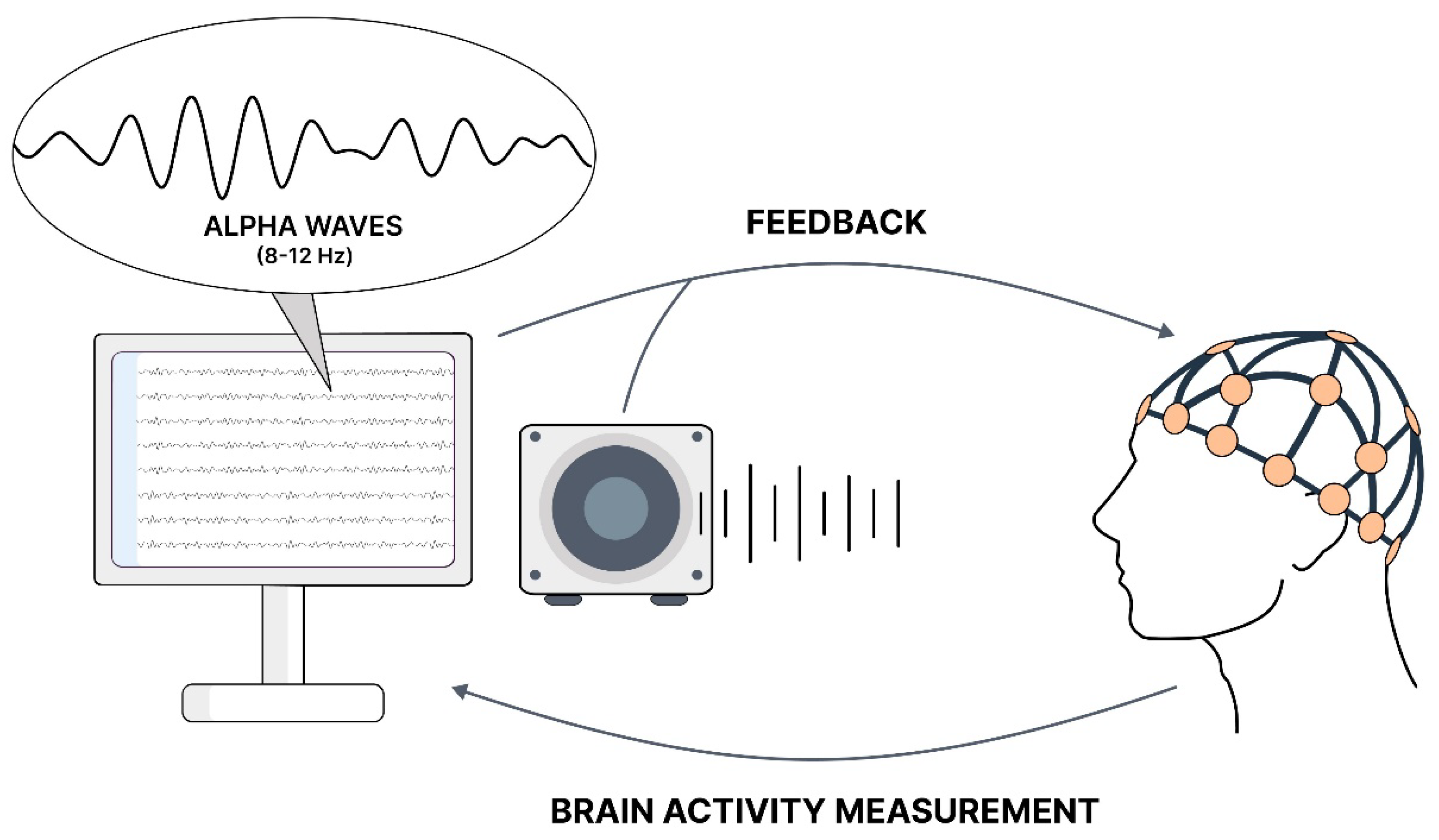
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





