Submitted:
17 June 2024
Posted:
18 June 2024
You are already at the latest version
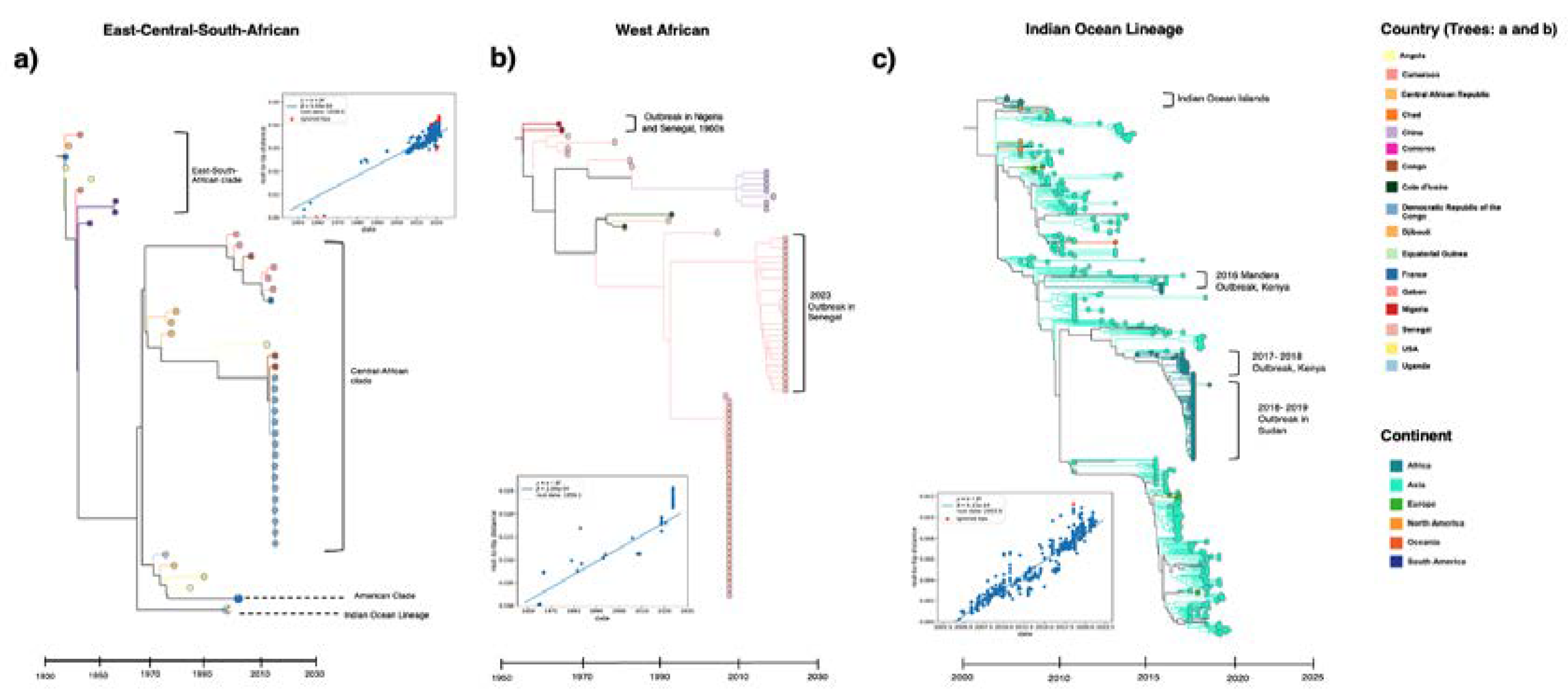
Abstract
Keywords:
1. Introduction
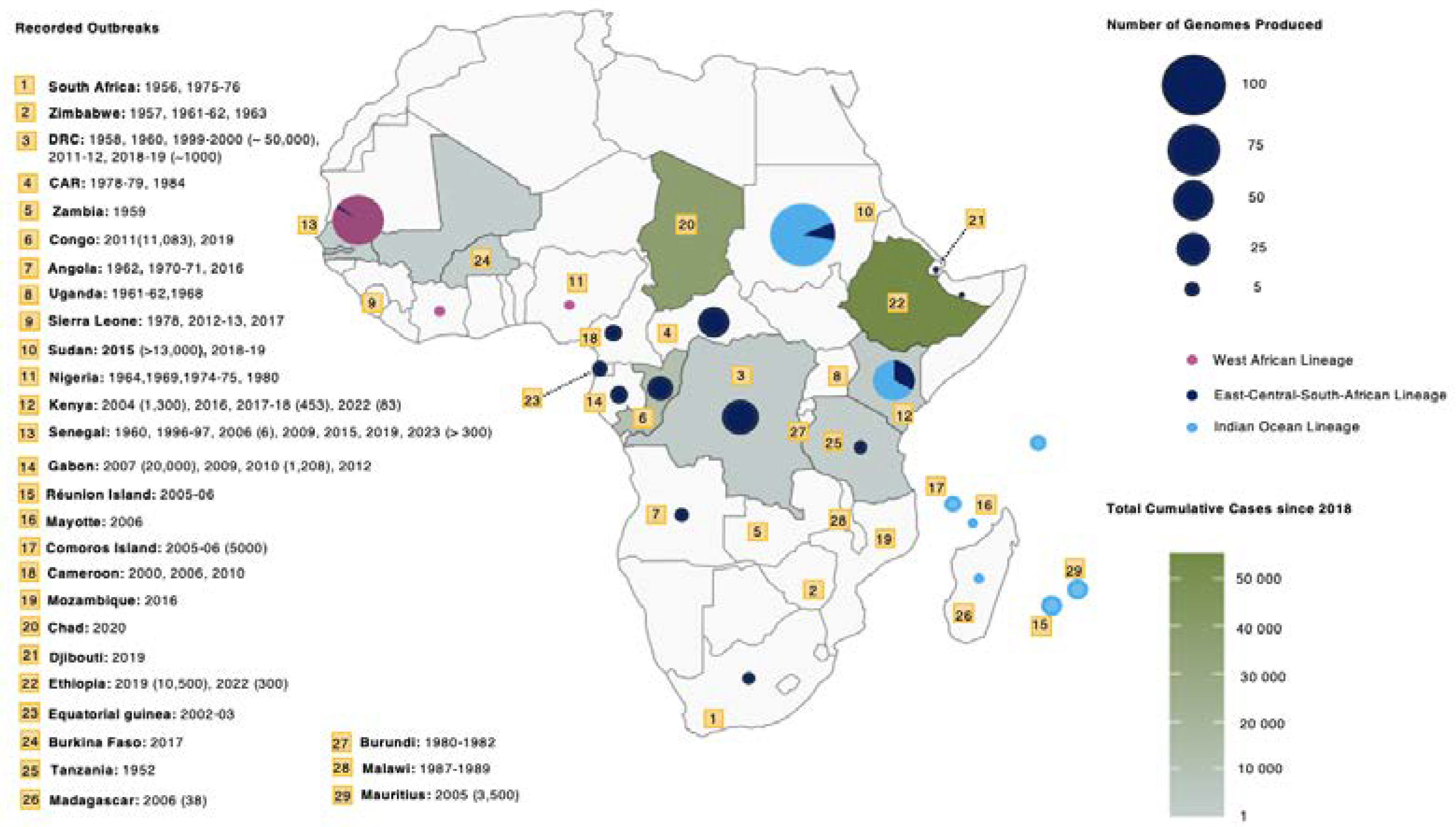
2. Cases, Outbreaks, and Current Burden in Africa
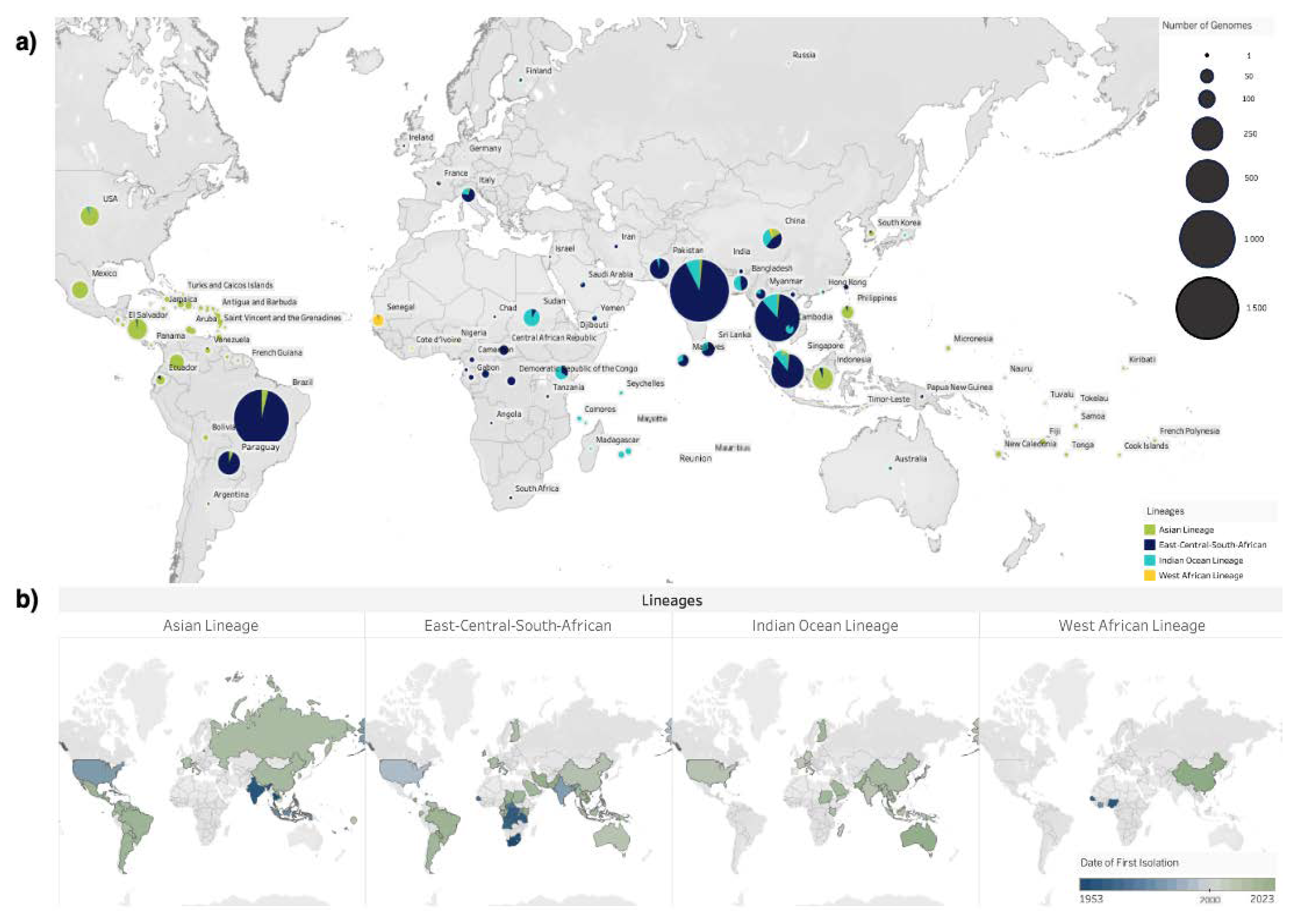
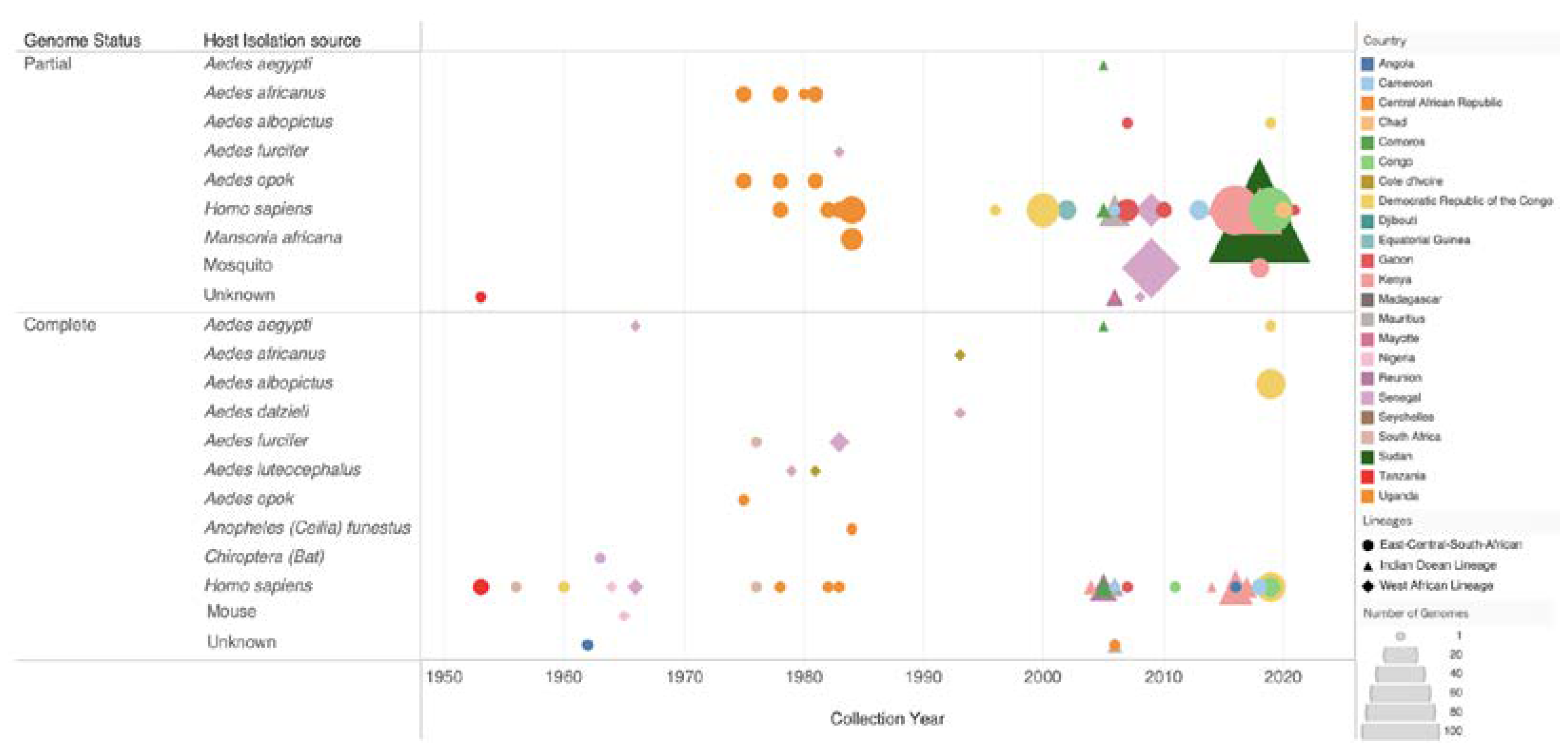
3. Genotype Distribution
4. Importance of Genomic and Epidemiological Surveillance
5. Genetic Diversity and Transmission Dynamics in Africa
6. Vectors and Transmission
7. Challenges and Gaps in CHIKV Surveillance in Africa
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Phadungsombat, J.; Imad, H.; Rahman, M.; Nakayama, E.E.; Kludkleeb, S.; Ponam, T.; Rahim, R.; Hasan, A.; Poltep, K.; Yamanaka, A.; et al. A Novel Sub-Lineage of Chikungunya Virus East/Central/South African Genotype Indian Ocean Lineage Caused Sequential Outbreaks in Bangladesh and Thailand. Viruses 2020, 12. [Google Scholar] [CrossRef]
- Deeba, F.; Haider, M.S.H.; Ahmed, A.; Tazeen, A.; Faizan, M.I.; Salam, N.; Hussain, T.; Alamery, S.F.; Parveen, S. Global Transmission and Evolutionary Dynamics of the Chikungunya Virus. Epidemiol Infect 2020. [Google Scholar] [CrossRef] [PubMed]
- Schuffenecker, I.; Iteman, I.; Michault, A.; Murri, S.; Frangeul, L.; Vaney, M.-C.; Lavenir, R.; Pardigon, N.; Reynes, J.-M.; Pettinelli, F.; et al. Genome Microevolution of Chikungunya Viruses Causing the Indian Ocean Outbreak. PLoS Med 2006, 3, 1058–1070. [Google Scholar] [CrossRef]
- Silva, J.V.J.; Ludwig-Begall, L.F.; de Oliveira-Filho, E.F.; Oliveira, R.A.S.; Durães-Carvalho, R.; Lopes, T.R.R.; Silva, D.E.A.; Gil, L.H.V.G. A Scoping Review of Chikungunya Virus Infection: Epidemiology, Clinical Characteristics, Viral Co-Circulation Complications, and Control. Acta Trop 2018, 188, 213–224. [Google Scholar]
- Bartholomeeusen, K.; Daniel, M.; LaBeaud, D.A.; Gasque, P.; Peeling, R.W.; Stephenson, K.E.; Ng, L.F.P.; Ariën, K.K. Chikungunya Fever. Nat Rev Dis Primers 2023, 9, 1–21. [Google Scholar] [CrossRef]
- Russo, G.; Subissi, L.; Rezza, G. Chikungunya Fever in Africa: A Systematic Review. Pathog Glob Health 2020, 114, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Mcintosh, B.M.; Harwin, R.M.; Paterson, H.E.; Westwatert, M.L. An Epidemic of Chikungunya in South-Eastern Southern Rhodesia. Cent Afr J Med 1963, 9, 351–359. [Google Scholar]
- Lumsden, W.H.R. An Epidemic of Virus Disease in Southern Province, Tanganyika Territory, in 1952–1953 II. General Description and Epidemiology. Trans R Soc Trop Med Hyg 1955, 49, 33–57. [Google Scholar] [CrossRef] [PubMed]
- Halstead, S.B. Reappearance of Chikungunya, Formerly Called Dengue, in the Americas. Emerg Infect Dis 2015, 21, 557–561. [Google Scholar] [CrossRef]
- Carey, D.E. Chikungunya and Dengue: A Case of Mistaken Identity? J Hist Med Allied Sci 1971, XXVI, 243–262. [Google Scholar] [CrossRef]
- de Lima Cavalcanti, T.Y.V.; Pereira, M.R.; de Paula, S.O.; Franca, R.F.d.O. A Review on Chikungunya Virus Epidemiology, Pathogenesis and Current Vaccine Development. Viruses 2022, 14. [Google Scholar] [CrossRef]
- Leroy, E.M.; Nkoghe, D.; Ollomo, B.; Nze-Nkogue, C.; Becquart, P.; Grard, G.; Pourrut, X.; Charrel, R.; Moureau, G.; Ndjoyi-Mbiguino, A.; et al. Concurrent Chikungunya and Dengue Virus Infections during Simultaneous Outbreaks, Gabon, 2007. Emerg Infect Dis 2009, 15, 591–593. [Google Scholar] [CrossRef] [PubMed]
- Thiberville, S.D.; Boisson, V.; Gaudart, J.; Simon, F.; Flahault, A.; de Lamballerie, X. Chikungunya Fever: A Clinical and Virological Investigation of Outpatients on Reunion Island, South-West Indian Ocean. PLoS Negl Trop Dis 2013, 7. [Google Scholar] [CrossRef]
- Costa, L.B.; Barreto, F.K.d.A.; Barreto, M.C.A.; dos Santos, T.H.P.; de Andrade, M.d.M.O.; Farias, L.A.B.G.; de Freitas, A.R.R.; Martinez, M.J.; Cavalcanti, L.P.d.G. Epidemiology and Economic Burden of Chikungunya: A Systematic Literature Review. Trop Med Infect Dis 2023, 8. [Google Scholar] [CrossRef]
- Soumahoro, M.K.; Boelle, P.Y.; Gaüzere, B.A.; Atsou, K.; Pelat, C.; Lambert, B.; La Ruche, G.; Gastellu-Etchegorry, M.; Renault, P.; Sarazin, M.; et al. The Chikungunya Epidemic on La Réunion Island in 2005-2006: A Cost-of-Illness Study. PLoS Negl Trop Dis 2011, 5. [Google Scholar] [CrossRef]
- Tam, P.Y.I.; Obaro, S.K.; Storch, G. Challenges in the Etiology and Diagnosis of Acute Febrile Illness in Children in Low- and Middle- Income Countries. J Pediatric Infect Dis Soc 2016, 5, 190–205. [Google Scholar] [CrossRef]
- Fenollar, F.; Mediannikov, O. Emerging Infectious Diseases in Africa in the 21st Century. New Microbes New Infect 2018, 26, S10–S18. [Google Scholar] [CrossRef] [PubMed]
- Maze, M.J.; Bassat, Q.; Feasey, N.A.; Mandomando, I.; Musicha, P.; Crump, J.A. The Epidemiology of Febrile Illness in Sub-Saharan Africa: Implications for Diagnosis and Management. Clinical Microbiology and Infection 2018, 24, 808–814. [Google Scholar] [CrossRef]
- Nooh, F.; Chernet, A.; Reither, K.; Okuma, J.; Brattig, N.W.; Utzinger, J.; Probst-Hensch, N.; Paris, D.H.; Dreyfus, A. Prevalence of Fever of Unidentified Aetiology in East African Adolescents and Adults: A Systematic Review and Meta-Analysis. Infect Dis Poverty 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- CLIMADE. Available online: https://climade.health/africa (accessed on 5 June 2024).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst Rev 2016, 5. [Google Scholar] [CrossRef]
- Padane, A.; Tegally, H.; Ramphal, Y.; Seyni, N.; Sarr, M.; Diop, M.M.; Diedhiou, C.K.; Mboup, A.; Diouf, N.D.; Souaré, A.; et al. An Emerging Clade of Chikungunya West African Genotype Discovered in Real-Time during 2023 Outbreak in Senegal. medRxiv 2023. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, E.; Giovanetti, M.; Tegally, H.; San, J.E.; Lessells, R.; Cuadros, D.; Martin, D.P.; Rasmussen, D.A.; Zekri, A.-R.N.; Sangare, A.K.; et al. A Year of Genomic Surveillance Reveals How the SARS-CoV-2 Pandemic Unfolded in Africa. Science 2021, 374, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Egid, B.R.; Coulibaly, M.; Dadzie, S.K.; Kamgang, B.; McCall, P.J.; Sedda, L.; Toe, K.H.; Wilson, A.L. Review of the Ecology and Behaviour of Aedes Aegypti and Aedes Albopictus in Western Africa and Implications for Vector Control. Current Research in Parasitology and Vector-Borne Diseases 2022, 2. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization, Technical Guidelines for Integrated Disease Surveillance and Response in the African Region: Third edition. Available online: https://www.afro.who.int/publications/technical-guidelines-integrated-disease-surveillance-and-response-african-region-third (accessed on 15 May 2024).
- Mascarenhas, M.; Garasia, S.; Berthiaume, P.; Corrin, T.; Greig, J.; Ng, V.; Young, I.; Waddell, L. A Scoping Review of Published Literature on Chikungunya Virus. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation African Region Outbreaks and Emergencies Bulletin. Available online: https://www.afro.who.int/health-topics/disease-outbreaks/outbreaks-and-other-emergencies-updates (accessed on 28 April 2024).
- Edwards, C.J.; Welch, S.R.; Chamberlain, J.; Hewson, R.; Tolley, H.; Cane, P.A.; Lloyd, G. Molecular Diagnosis and Analysis of Chikungunya Virus. J Clin Virol 2007, 39, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Fourié, T.; Dia, A.; Savreux, Q.; Pommier de Santi, V.; de Lamballerie, X.; Leparc-Goffart, I.; Simon, F. Emergence of Indian Lineage of ECSA Chikungunya Virus in Djibouti, 2019. Int J Infect Dis 2021, 108, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Agbodzi, B.; Yousseu, F.B.S.; Simo, F.B.N.; Kumordjie, S.; Yeboah, C.; Mosore, M.T.; Bentil, R.E.; Prieto, K.; Colston, S.M.; Attram, N.; et al. Chikungunya Viruses Containing the A226V Mutation Detected Retrospectively in Cameroon Form a New Geographical Subclade. Int J Infect Dis 2021, 113, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Lo Presti, A.; Ciccozzi, M.; Cella, E.; Lai, A.; Simonetti, F.R.; Galli, M.; Zehender, G.; Rezza, G. Origin, Evolution, and Phylogeography of Recent Epidemic CHIKV Strains. Infect Gene Evol 2012, 12, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Mudurangaplar, B. Molecular Characterisation of Clinical Isolates of Chikungunya Virus: A Study from Tertiary Care Hospitals in Southern India. J Clin Diagn Res 2016. [Google Scholar] [CrossRef] [PubMed]
- Thiberville, S.-D.; Boisson, V.; Gaudart, J.; Simon, F.; Flahault, A.; de Lamballerie, X. Chikungunya Fever: A Clinical and Virological Investigation of Outpatients on Reunion Island, South-West Indian Ocean. PLoS Negl Trop Dis 2013, 7, e2004. [Google Scholar] [CrossRef]
- Pastorino, B.; Muyembe-Tamfum, J.J.; Bessaud, M.; Tock, F.; Tolou, H.; Durand, J.P.; Peyrefitte, C.N. Epidemic Resurgence of Chikungunya Virus in Democratic Republic of the Congo: Identification of a New Central African Strain. J Med Virol 2004, 74, 277–282. [Google Scholar] [CrossRef]
- Peyrefitte, C.N.; Rousset, D.; Pastorino, B.A.M.; Pouillot, R.; Bessaud, M.; Tock, F.; Mansaray, H.; Merle, O.L.; Pascual, A.M.; Paupy, C.; et al. Chikungunya Virus, Cameroon, 2006. Emerg Infect Dis 2007, 13, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Takaya, S.; Kutsuna, S.; Nakayama, E.; Taniguchi, S.; Tajima, S.; Katanami, Y.; Yamamoto, K.; Takeshita, N.; Hayakawa, K.; Kato, Y.; et al. Chikungunya Fever in Traveler from Angola to Japan, 2016. Emerg Infect Dis 2017, 23, 156–158. [Google Scholar] [CrossRef] [PubMed]
- Maljkovic Berry, I.; Eyase, F.; Pollett, S.; Konongoi, S.L.; Joyce, M.G.; Figueroa, K.; Ofula, V.; Koka, H.; Koskei, E.; Nyunja, A.; et al. Global Outbreaks and Origins of a Chikungunya Virus Variant Carrying Mutations Which May Increase Fitness for Aedes Aegypti: Revelations from the 2016 Mandera, Kenya Outbreak. Am J Trop Med Hyg 2019, 100, 1249–1257. [Google Scholar] [CrossRef]
- Bower, H.; el Karsany, M.; Adam, A.A.A.H.; Idriss, M.I.; Alzain, M.A.; Alfakiyousif, M.E.A.; Mohamed, R.; Mahmoud, I.; Albadri, O.; Mahmoud, S.A.A.; et al. “Kankasha” in Kassala: A Prospective Observational Cohort Study of the Clinical Characteristics, Epidemiology, Genetic Origin, and Chronic Impact of the 2018 Epidemic of Chikungunya Virus Infection in Kassala, Sudan. PLoS Negl Trop Dis 2021, 15, e0009387. [Google Scholar] [CrossRef] [PubMed]
- Eyase, F.; Langat, S.; Berry, I.M.; Mulwa, F.; Nyunja, A.; Mutisya, J.; Owaka, S.; Limbaso, S.; Ofula, V.; Koka, H.; et al. Emergence of a Novel Chikungunya Virus Strain Bearing the E1:V80A Substitution, out of the Mombasa, Kenya 2017-2018 Outbreak. PLoS ONE 2020, 15, e0241754. [Google Scholar] [CrossRef]
- Schuffenecker, I.; Iteman, I.; Michault, A.; Murri, S.; Frangeul, L.; Vaney, M.-C.; Lavenir, R.; Pardigon, N.; Reynes, J.-M.; Pettinelli, F.; et al. Genome Microevolution of Chikungunya Viruses Causing the Indian Ocean Outbreak. PLoS Med 2006, 3, e263. [Google Scholar] [CrossRef]
- Moyen, N.; Thiberville, S.-D.; Pastorino, B.; Nougairede, A.; Thirion, L.; Mombouli, J.-V.; Dimi, Y.; Leparc-Goffart, I.; Capobianchi, M.R.; Lepfoundzou, A.D.; et al. First Reported Chikungunya Fever Outbreak in the Republic of Congo, 2011. PLoS ONE 2014, 9, e115938. [Google Scholar] [CrossRef]
- Selhorst, P.; Makiala-Mandanda, S.; De Smet, B.; Mariën, J.; Anthony, C.; Binene-Mbuka, G.; De Weggheleire, A.; Ilombe, G.; Kinganda-Lusamaki, E.; Pukuta-Simbu, E.; et al. Molecular Characterization of Chikungunya Virus during the 2019 Outbreak in the Democratic Republic of the Congo. Emerg Microbes Infect 2020, 9, 1912–1918. [Google Scholar] [CrossRef]
- Moyen, N.; Thiberville, S.-D.; Pastorino, B.; Nougairede, A.; Thirion, L.; Mombouli, J.-V.; Dimi, Y.; Leparc-Goffart, I.; Capobianchi, M.R.; Lepfoundzou, A.D.; et al. First Reported Chikungunya Fever Outbreak in the Republic of Congo, 2011. PLoS ONE 2014, 9, e115938. [Google Scholar] [CrossRef]
- Konongoi, S.L.; Nyunja, A.; Ofula, V.; Owaka, S.; Koka, H.; Koskei, E.; Eyase, F.; Langat, D.; Mancuso, J.; Lutomiah, J.; et al. Human and Entomologic Investigations of Chikungunya Outbreak in Mandera, Northeastern Kenya, 2016. PLoS ONE 2018, 13, e0205058. [Google Scholar] [CrossRef]
- Parola, P.; de Lamballerie, X.; Jourdan, J.; Rovery, C.; Vaillant, V.; Minodier, P.; Brouqui, P.; Flahault, A.; Raoult, D.; Charrel, R. Novel Chikungunya Virus Variant in Travelers Returning from Indian Ocean Islands. Emerg Infect Dis 2006, 12, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Masia, M.; Sánchez-Seco, M.-P.; de Ory, F.; Benito, A.; Cano, J.; Tenorio, A.; Collao, X.; Negredo, A.I. Different Lineages of Chikungunya Virus in Equatorial Guinea in 2002 and 2006. Am J Trop Med Hyg 2010, 82, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Caron, M.; Paupy, C.; Grard, G.; Becquart, P.; Mombo, I.; Nso, B.B.B.; Kassa Kassa, F.; Nkoghe, D.; Leroy, E.M. Recent Introduction and Rapid Dissemination of Chikungunya Virus and Dengue Virus Serotype 2 Associated With Human and Mosquito Coinfections in Gabon, Central Africa. Clinical Infectious Diseases 2012, 55, e45–e53. [Google Scholar] [CrossRef] [PubMed]
- Leroy, E.M.; Nkoghe, D.; Ollomo, B.; Nze-Nkogue, C.; Becquart, P.; Grard, G.; Pourrut, X.; Charrel, R.; Moureau, G.; Ndjoyi-Mbiguino, A.; et al. Concurrent Chikungunya and Dengue Virus Infections during Simultaneous Outbreaks, Gabon, 2007. Emerg Infect Dis 2009, 15, 591–593. [Google Scholar] [CrossRef] [PubMed]
- Phadungsombat, J.; Imad, H.A.; Nakayama, E.E.; Leaungwutiwong, P.; Ramasoota, P.; Nguitragool, W.; Matsee, W.; Piyaphanee, W.; Shioda, T. Spread of a Novel Indian Ocean Lineage Carrying E1-K211E/E2-V264A of Chikungunya Virus East/Central/South African Genotype across the Indian Subcontinent, Southeast Asia, and Eastern Africa. Microorganisms 2022, 10, 354. [Google Scholar] [CrossRef]
- Simo Tchetgna, H.; Sem Ouilibona, R.; Nkili-Meyong, A.A.; Caron, M.; Labouba, I.; Selekon, B.; Njouom, R.; Leroy, E.M.; Nakoune, E.; Berthet, N. Viral Exploration of Negative Acute Febrile Cases Observed during Chikungunya Outbreaks in Gabon. Intervirology 2018, 61, 174–184. [Google Scholar] [CrossRef]
- Vairo, F.; Aimè Coussoud-Mavoungou, M.; Ntoumi, F.; Castilletti, C.; Kitembo, L.; Haider, N.; Carletti, F.; Colavita, F.; Gruber, C.; Iannetta, M.; et al. Chikungunya Outbreak in the Republic of the Congo, 2019—Epidemiological, Virological and Entomological Findings of a South-North Multidisciplinary Taskforce Investigation. Viruses 2020, 12, 1020. [Google Scholar] [CrossRef]
- Onoja, A.B.; Omatola, A.C.; Maiga, M.; Gadzama, I.S. Recurrent Episodes of Some Mosquito-Borne Viral Diseases in Nigeria: A Systematic Review and Meta-Analysis. Pathogens 2022, 11, 1162. [Google Scholar] [CrossRef]
- Delisle, E.; Rousseau, C.; Broche, B.; Leparc-Goffart, I.; L’Ambert, G.; Cochet, A.; Prat, C.; Foulongne, V.; Ferré, J.B.; Catelinois, O.; et al. Chikungunya Outbreak in Montpellier, France, September to October 2014. Eurosurveillance 2015, 20. [Google Scholar] [CrossRef]
- Chinedu Eneh, S.; Uwishema, O.; Nazir, A.; El Jurdi, E.; Faith Olanrewaju, O.; Abbass, Z.; Mustapha Jolayemi, M.; Mina, N.; kseiry, l.; Onyeaka, H. Chikungunya Outbreak in Africa: A Review of the Literature. Annals of Medicine & Surgery 2023, 85, 3545–3552. [Google Scholar] [CrossRef] [PubMed]
- Wahid, B.; Ali, A.; Rafique, S.; Idrees, M. Global Expansion of Chikungunya Virus: Mapping the 64-Year History. Intl J Infect Dis 2017, 58, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Collao, X.; Negredo, A.I.; Cano, J.; Tenorio, A.; De Ory, F.; Benito, A.; Masia, M.; Sánchez-Seco, M.P. Short Report: Different Lineages of Chikungunya Virus in Equatorial Guinea in 2002 and 2006. Am J Trop Med Hyg 2010, 82, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Bettis, A.A.; L’Azou Jackson, M.; Yoon, I.K.; Breugelmans, J.G.; Goios, A.; Gubler, D.J.; Powers, A.M. The Global Epidemiology of Chikungunya from 1999 to 2020: A Systematic Literature Review to Inform the Development and Introduction of Vaccines. PLoS Negl Trop Dis 2022, 16. [Google Scholar] [CrossRef] [PubMed]
- Desdouits, M.; Kamgang, B.; Berthet, N.; Tricou, V.; Ngoagouni, C.; Gessain, A.; Manuguerra, J.C.; Nakouné, E.; Kazanji, M. Genetic Characterization of Chikungunya Virus in the Central African Republic. Infect Gene Evol 2015, 33, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Ratsitorahina, M.; Harisoa, J.; Ratovonjato, J.; Biacabe, S.; Reynes, J.M.; Zeller, H.; Raoelina, Y.; Talarmin, A.; Richard, V.; Soares, J.L. Outbreak of Dengue and Chikungunya Fevers, Toamasina, Madagascar, 2006. Emerg Infect Dis 2008, 14, 1135–1137. [Google Scholar] [CrossRef] [PubMed]
- Beesoon, S.; Funkhouser, E.; Kotea, N.; Spielman, A.; Robich, R.M. Chikungunya Fever, Mauritius, 2006. Emerg Infect Dis 2008, 14, 337–338. [Google Scholar] [CrossRef] [PubMed]
- Sergon, K.; Njuguna, C.; Kalani, R.; Ofula, V.; Onyango, C.; Konongoi, L.S.; Bedno, S.; Burke, H.; Dumilla, A.M.; Konde, J.; et al. Seroprevalence of Chikungunya Virus (CHIKV) Infection on Lamu Island, Kenya, October 2004. Am J Trop Med Hyg 2008, 78, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Nkoghe, D.; Kassa, R.F.; Caron, M.; Grard, G.; Mombo, I.; Bikié, B.; Paupy, C.; Becquart, P.; Bisvigou, U.; Leroy, E.M. Clinical Forms of Chikungunya in Gabon, 2010. PLoS Negl Trop Dis 2012, 6. [Google Scholar] [CrossRef] [PubMed]
- Suhana, O.; Nazni, W.A.; Apandi, Y.; Farah, H.; Lee, H.L.; Sofian-Azirun, M. Insight into the Origin of Chikungunya Virus in Malaysian Non-Human Primates via Sequence Analysis. Heliyon 2019, 5, e02682. [Google Scholar] [CrossRef]
- Nyamwaya, D.K.; Otiende, M.; Omuoyo, D.O.; Githinji, G.; Karanja, H.K.; Gitonga, J.N.; R. de Laurent, Z.; Otieno, J.R.; Sang, R.; Kamau, E.; et al. Endemic Chikungunya Fever in Kenyan Children: A Prospective Cohort Study. BMC Infect Dis 2021, 21, 186. [Google Scholar] [CrossRef] [PubMed]
- Ushijima, Y.; Abe, H.; Mbadinga, M.J.V.M.; Ondo, G.N.; Bikangui, R.; Agnandji, S.T.; Lell, B.; Yasuda, J. Re-Emergence of Dengue, Chikungunya, and Zika Viruses in 2021 after a 10-Year Gap in Gabon. IJID Regions 2022, 5, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Bacterial and Viral Bioinformatics Resource Center (BV-BRC). Available online: https://www.bv-brc.org/ (accessed on 12 January 2024).
- De Weggheleire, A.; Nkuba-Ndaye, A.; Mbala-Kingebeni, P.; Mariën, J.; Kindombe-Luzolo, E.; Ilombe, G.; Mangala-Sonzi, D.; Binene-Mbuka, G.; De Smet, B.; Vogt, F.; et al. A Multidisciplinary Investigation of the First Chikungunya Virus Outbreak in Matadi in the Democratic Republic of the Congo. Viruses 2021, 13, 1988. [Google Scholar] [CrossRef] [PubMed]
- Demanou, M.; Antonio-Nkondjio, C.; Ngapana, E.; Rousset, D.; Paupy, C.; Manuguerra, J.-C.; Zeller, H. Chikungunya Outbreak in a Rural Area of Western Cameroon in 2006: A Retrospective Serological and Entomological Survey. BMC Res Notes 2010, 3, 128. [Google Scholar] [CrossRef]
- Buchwald, A.G.; Hayden, M.H.; Dadzie, S.K.; Paull, S.H.; Carlton, E.J. Aedes-Borne Disease Outbreaks in West Africa: A Call for Enhanced Surveillance. Acta Trop 2020, 209, 105468. [Google Scholar] [CrossRef]
- Ansumana, R.; Jacobsen, K.H.; Leski, T.A.; Covington, A.L.; Bangura, U.; Hodges, M.H.; Lin, B.; Bockarie, A.S.; Lamin, J.M.; Bockarie, M.J.; et al. Reemergence of Chikungunya Virus in Bo, Sierra Leone. Emerg Infect Dis 2013, 19, 1108–1110. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.T.; Tytheridge, S.J.; Smith, S.J.; Levine, R.S.; Hodges, M.H.; Ansumana, R.; Wulff, S.; Whitworth, J.; Logan, J.G. The Threat of Vector-Borne Diseases in Sierra Leone. Am J Trop Med Hyg 2023, 109, 10–21. [Google Scholar] [CrossRef]
- Moore, D.L.; Reddy, S.; Akinkugbe, F.M.; Lee, V.H.; David-West, T.S.; Causey, O.R.; Carey, D.E. An Epidemic of Chikungunya Fever at Ibadan, Nigeria, 1969. Ann Trop Med Parasitol 1974, 68, 59–68. [Google Scholar] [CrossRef]
- Powers, A.M.; Logue, C.H. Changing Patterns of Chikungunya Virus: Re-Emergence of a Zoonotic Arbovirus. Journal of General Virology 2007, 88, 2363–2377. [Google Scholar] [CrossRef]
- Sow, A.; Faye, O.; Diallo, M.; Diallo, D.; Chen, R.; Faye, O.; Diagne, C.T.; Guerbois, M.; Weidmann, M.; Ndiaye, Y.; et al. Chikungunya Outbreak in Kedougou, Southeastern Senegal in 2009-2010. Open Forum Infect Dis 2018, 5. [Google Scholar] [CrossRef]
- Njenga, M.K.; Nderitu, L.; Ledermann, J.P.; Ndirangu, A.; Logue, C.H.; Kelly, C.H.L.; Sang, R.; Sergon, K.; Breiman, R.; Powers, A.M. Tracking Epidemic Chikungunya Virus into the Indian Ocean from East Africa. J Gen Virol 2008, 89, 2754–2760. [Google Scholar] [CrossRef] [PubMed]
- Gérardin, P.; Guernier, V.; Perrau, J.; Fianu, A.; Le Roux, K.; Grivard, P.; Michault, A.; de Lamballerie, X.; Flahault, A.; Favier, F. Estimating Chikungunya Prevalence in La Réunion Island Outbreak by Serosurveys: Two Methods for Two Critical Times of the Epidemic. BMC Infect Dis 2008, 8, 99. [Google Scholar] [CrossRef]
- Kang, H.; Auzenbergs, M.; Clapham, H.; Maure, C.; Kim, J.-H.; Salje, H.; Taylor, C.G.; Lim, A.; Clark, A.; Edmunds, W.J.; et al. Chikungunya Seroprevalence, Force of Infection, and Prevalence of Chronic Disability after Infection in Endemic and Epidemic Settings: A Systematic Review, Meta-Analysis, and Modelling Study. Lancet Infect Dis 2024, 24, 488–503. [Google Scholar] [CrossRef]
- Cottis, S.; Blisnick, A.A.; Failloux, A.-B.; Vernick, K.D. Determinants of Chikungunya and O’nyong-Nyong Virus Specificity for Infection of Aedes and Anopheles Mosquito Vectors Determinants of Chikungunya and O’nyong-Nyong Virus Specificity for Infection of Aedes and Anopheles Mosquito. Viruses 2023, 15, 589. [Google Scholar] [CrossRef] [PubMed]
- Volk, S.M.; Chen, R.; Tsetsarkin, K.A.; Adams, A.P.; Garcia, T.I.; Sall, A.A.; Nasar, F.; Schuh, A.J.; Holmes, E.C.; Higgs, S.; et al. Genome-Scale Phylogenetic Analyses of Chikungunya Virus Reveal Independent Emergences of Recent Epidemics and Various Evolutionary Rates. J Virol 2010, 84, 6497–6504. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Puri, V.; Fedorova, N.; Lin, D.; Hari, K.L.; Jain, R.; Rodas, J.D.; Das, S.R.; Shabman, R.S.; Weaver, S.C. Comprehensive Genome Scale Phylogenetic Study Provides New Insights on the Global Expansion of Chikungunya Virus. J Virol 2016, 90, 10600–10611. [Google Scholar] [CrossRef]
- Galán-Huerta, K.A.; Rivas-Estilla, A.M.; Fernández-Salas, I.; Farfan-Ale, J.A.; Ramos-Jiménez, J. Chikungunya Virus: A General Overview. Medicina Universitaria 2015, 17, 175–183. [Google Scholar] [CrossRef]
- de Souza, W.M.; Ribeiro, G.S.; de Lima, S.T.S.; de Jesus, R.; Moreira, F.R.R.; Whittaker, C.; Anice Sallum, M.M.; Carrington, C.V.F.; Sabino, E.C.; Kitron, U.; et al. Chikungunya: A Decade of Burden in the Americas. Lancet Reg Health -Am 2024, 30, 100673. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Chen, R.; Sherman, M.B.; Weaver, S.C. Chikungunya Virus: Evolution and Genetic Determinants of Emergence. Curr Opin Virol 2011, 1, 310–317. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Chen, R.; Weaver, S.C. Interspecies Transmission and Chikungunya Virus Emergence. Curr Opin Virol 2016, 16, 143–150. [Google Scholar] [CrossRef]
- De Almeida Di Maio Ferreira, F.C.P.; Da Silva, A.S.V.; Recht, J.; Guaraldo, L.; Moreira, M.E.L.; De Siqueira, A.M.; Gerardin, P.; Brasil, P. Vertical Transmission of Chikungunya Virus: A Systematic Review. PLoS ONE 2021, 16. [Google Scholar]
- Faria, N.R.; Lourenço, J.; Marques de Cerqueira, E.; Maia de Lima, M.; Carlos Junior Alcantara, L. Epidemiology of Chikungunya Virus in Bahia, Brazil, 2014-2015. PLoS Curr 2016. [Google Scholar] [CrossRef]
- Grubaugh, N.D.; Ladner, J.T.; Lemey, P.; Pybus, O.G.; Rambaut, A.; Holmes, E.C.; Andersen, K.G. Tracking Virus Outbreaks in the Twenty-First Century. Nat Microbiol 2019, 4, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Wallau, G.L.; Abanda, N.N.; Abbud, A.; Abdella, S.; Abera, A.; Ahuka-Mundeke, S.; Falconi-Agapito, F.; Alagarasu, K.; Ariën, K.K.; Ayres, C.F.J.; et al. Arbovirus Researchers Unite: Expanding Genomic Surveillance for an Urgent Global Need. Lancet Glob Health 2023, 11, e1501–e1502. [Google Scholar] [CrossRef]
- Zeghbib, S.; Kemenesi, G.; Jakab, F. The Importance of Equally Accessible Genomic Surveillance in the Age of Pandemics. Biol Futur 2023, 74, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Naveca, F.G.; Claro, I.; Giovanetti, M.; de Jesus, J.G.; Xavier, J.; Iani, F.C.d.M.; do Nascimento, V.A.; de Souza, V.C.; Silveira, P.P.; Lourenço, J.; et al. Genomic, Epidemiological and Digital Surveillance of Chikungunya Virus in the Brazilian Amazon. PLoS Negl Trop Dis 2018, 13. [Google Scholar] [CrossRef] [PubMed]
- Burgueño, A.; Giovanetti, M.; Fonseca, V.; Morel, N.; Lima, M.; Castro, E.; Guimarães, N.R.; Iani, F.C.M.; Bormida, V.; Cortinas, M.N.; et al. Genomic and Eco-Epidemiological Investigations in Uruguay Reveal Local Chikungunya Virus Transmission Dynamics during Its Expansion across the Americas in 2023. Emerg Microbes Infect 2024, 13. [Google Scholar] [CrossRef]
- Giovanetti, M.; Vazquez, C.; Lima, M.; Castro, E.; Rojas, A.; Gomez de la Fuente, A.; Aquino, C.; Cantero, C.; Fleitas, F.; Torales, J.; et al. Rapid Epidemic Expansion of Chikungunya Virus East/Central/South African Lineage, Paraguay. Emerg Infect Dis 2023, 9, 1859–1863. [Google Scholar] [CrossRef]
- Huber, J.H.; Childs, M.L.; Caldwell, J.M.; Mordecai, E.A. Seasonal Temperature Variation Influences Climate Suitability for Dengue, Chikungunya, and Zika Transmission. PLoS Negl Trop Dis 2018, 12. [Google Scholar] [CrossRef]
- Vazeille, M.; Moutailler, S.; Coudrier, D.; Rousseaux, C.; Khun, H.; Huerre, M.; Thiria, J.; Dehecq, J.S.; Fontenille, D.; Schuffenecker, I.; et al. Two Chikungunya Isolates from the Outbreak of La Reunion (Indian Ocean) Exhibit Different Patterns of Infection in the Mosquito, Aedes Albopictus. PLoS ONE 2007, 2. [Google Scholar] [CrossRef]
- Yonga, M.G.; Yandai, F.H.; Sadeuh-Mba, S.; Abdallah, A.H.; Ouapi, D.; Gamougam, K.; Abanda, N.N.; Endengue-Zanga, M.C.; Demanou, M.; Njouom, R. Molecular Characterization of Chikungunya Virus from the First Cluster of Patients during the 2020 Outbreak in Chad. Arch Virol 2022, 167, 1301–1305. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Ghani, R.; Fouque, F.; Mahdy, M.A.K.; Zhong, Q.; Al-Eryani, S.M.A.; Alkwri, A.; Beier, J.C. Multisectoral Approach to Address Chikungunya Outbreaks Driven by Human Mobility: A Systematic Review and Meta-Analysis. Journal of Infectious Diseases 2020, 222, S709–S716. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.R.T.; Faria, N.R.; de Vasconcelos, J.M.; Golding, N.; Kraemer, M.U.G.; de Oliveira, L.F.; da Silva Azevedo, R.d.S.; da Silva, D.E.A.; da Silva, E.V.P.; da Silva, S.P.; et al. Emergence and Potential for Spread of Chikungunya Virus in Brazil. BMC Med 2015, 13. [Google Scholar] [CrossRef] [PubMed]
- Lanciotti, R.S.; Kosoy, O.L.; Laven, J.J.; Panella, A.J.; Velez, J.O.; Lambert, A.J.; Campbell, G.L. Chikungunya Virus in US Travelers Returning from India, 2006. Emerg Infect Dis 2007, 13, 764–767. [Google Scholar] [CrossRef]
- Tsetsarkin, K.A.; Vanlandingham, D.L.; McGee, C.E.; Higgs, S. A Single Mutation in Chikungunya Virus Affects Vector Specificity and Epidemic Potential. PLoS Pathog 2007, 3, 1895–1906. [Google Scholar] [CrossRef] [PubMed]
- Mourad, O.; Makhani, L.; Chen, L.H. Chikungunya: An Emerging Public Health Concern. Curr Infect Dis Rep 2022, 24, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Yergolkar, P.; Tandale, B.; Arankalle, V.; Sathe, P.; Gandhe, S.; Gokhle, M.; Jacob, G.; Hundekar, S.; Mishra, A. Chikungunya Outbreaks Caused by African Genotype, India. Emerg Infect Dis 2006, 12, 1580–1583. [Google Scholar] [CrossRef]
- Powers, A.M.; Brault, A.C.; Tesh, R.B.; Weaver, S.C. Re-Emergence of Chikungunya and o’nyong-Nyong Viruses: Evidence for Distinct Geographical Lineages and Distant Evolutionary Relationships. Microbiology (N Y) 2000, 81, 471–479. [Google Scholar] [CrossRef]
- Weaver, S.C.; Chen, R.; Diallo, M. Chikungunya Virus: Role of Vectors in Emergence from Enzootic Cycles. Annu Rev Entomol 2020, 65, 313–332. [Google Scholar] [CrossRef]
- Valentine, M.J.; Murdock, C.C.; Kelly, P.J. Sylvatic Cycles of Arboviruses in Non-Human Primates. Parasit Vectors 2019, 12, 463. [Google Scholar] [CrossRef]
- Diallo, M.; Thonnon, J.; ~aore-Lamizana, M. Vectors of Chikungunya Virus in Senegal: Current Data and Transmission Cycles. Am J Trop Med Hyg 1999, 60, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Diallo, D.; Sall, A.A.; Buenemann, M.; Chen, R.; Faye, O.; Diagne, C.T.; Faye, O.; Ba, Y.; Dia, I.; Watts, D.; et al. Landscape Ecology of Sylvatic Chikungunya Virus and Mosquito Vectors in Southeastern Senegal. PLoS Negl Trop Dis 2012, 6. [Google Scholar] [CrossRef]
- Pialoux, G.; Gaüzère, B.-A.; Jauréguiberry, S.; Strobel, M. Chikungunya, an Epidemic Arbovirosis. Lancet Infect Dis 2007, 7, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Richman, R.; Diallo, D.; Diallo, M.; Sall, A.A.; Faye, O.; Diagne, C.T.; Dia, I.; Weaver, S.C.; Hanley, K.A.; Buenemann, M. Ecological Niche Modeling of Aedes Mosquito Vectors of Chikungunya Virus in Southeastern Senegal. Parasit Vectors 2018, 11, 255. [Google Scholar] [CrossRef]
- Weaver, S.C.; Lecuit, M. Chikungunya Virus and the Global Spread of a Mosquito-Borne Disease. New England Journal of Medicine 2015, 372, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Mcintosh, B.M.; Jupp, P.G.; Dos Santos, I. Rural Epidemic of Chikungunya in South Africa with Involvement of Aedes (Diceromyia) Furcifer (Edwards) and Baboons. S Afr J Sci 1977, 73. [Google Scholar]
- Powell, J.R.; Tabachnick, W.J. History of Domestication and Spread of Aedes Aegypti - A Review. Mem Inst Oswaldo Cruz 2013, 108, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Laporta, G.Z.; Potter, A.M.; Oliveira, J.F.A.; Bourke, B.P.; Pecor, D.B.; Linton, Y.M. Global Distribution of Aedes Aegypti and Aedes Albopictus in a Climate Change Scenario of Regional Rivalry. Insects 2023, 14. [Google Scholar] [CrossRef]
- Pfeffer, M.; Zöller, G.; Essbauer, S.; Tomaso, H.; Behrens-Riha, N.; Löscher, T.; Dobler, G. Clinical and Virological Characterization of Imported Cases of Chikungunya Fever. Wien Klin Wochenschr 2008, 120, 95–100. [Google Scholar] [CrossRef]
- Longbottom, J.; Walekhwa, A.W.; Mwingira, V.; Kijanga, O.; Mramba, F.; Lord, J.S. Aedes Albopictus Invasion across Africa: The Time Is Now for Cross-Country Collaboration and Control. Lancet Glob Health 2023, 11, e623–e628. [Google Scholar] [CrossRef] [PubMed]
- Cornel, A.J.; Hunt, R.H. Aedes Albopictus in Africa? First Records of Live Specimens in Imported Tires in Capetown. J Am Mosq Control Assoc 1991, 7, 107–108. [Google Scholar]
- Bonizzoni, M.; Gasperi, G.; Chen, X.; James, A.A. The Invasive Mosquito Species Aedes Albopictus: Current Knowledge and Future Perspectives. Trends Parasitol 2013, 29, 460–468. [Google Scholar] [CrossRef]
- Weetman, D.; Kamgang, B.; Badolo, A.; Moyes, C.L.; Shearer, F.M.; Coulibaly, M.; Pinto, J.; Lambrechts, L.; McCall, P.J. Aedes Mosquitoes and Aedes-Borne Arboviruses in Africa: Current and Future Threats. Int J Environ Res Public Health 2018, 15. [Google Scholar] [CrossRef]
- Tajudeen, Y.A.; Oladunjoye, I.O.; Bajinka, O.; Oladipo, H.J. Zoonotic Spillover in an Era of Rapid Deforestation of Tropical Areas and Unprecedented Wildlife Trafficking: Into the Wild. Challenges 2022, 13, 41. [Google Scholar] [CrossRef]
- Tajudeen, Y.A.; Oladipo, H.J.; Oladunjoye, I.O.; Mustapha, M.O.; Mustapha, S.T.; Abdullahi, A.A.; Yusuf, R.O.; Abimbola, S.O.; Adebayo, A.O.; Ikebuaso, J.G.; et al. Preventing the Next Pandemic through a Planetary Health Approach: A Focus on Key Drivers of Zoonosis. Challenges 2022, 13, 50. [Google Scholar] [CrossRef]
- Kraemer, M.U.G.; Sinka, M.E.; Duda, K.A.; Mylne, A.; Shearer, F.M.; Brady, O.J.; Messina, J.P.; Barker, C.M.; Moore, C.G.; Carvalho, R.G.; et al. The Global Compendium of Aedes Aegypti and Ae. Albopictus Occurrence. Sci Data 2015, 2. [Google Scholar] [CrossRef] [PubMed]
- Giovanetti, M.; Alcantara, L.C.J.; Dorea, A.S.; Ferreira, Q.R.; Marques, W.d.A.; Franca de Barros, J.; Adelino, T.E.R.; Tosta, S.; Fritsch, H.; Iani, F.C. de M.; et al. Promoting Responsible Research and Innovation (RRI) During Brazilian Activities of Genomic and Epidemiological Surveillance of Arboviruses. Front Public Health 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Althouse, B.M.; Guerbois, M.; Cummings, D.A.T.; Diop, O.M.; Faye, O.; Faye, A.; Diallo, D.; Sadio, B.D.; Sow, A.; Faye, O.; et al. Role of Monkeys in the Sylvatic Cycle of Chikungunya Virus in Senegal. Nat Commun 2018, 9. [Google Scholar] [CrossRef]
- Braack, L.; Wulandhari, S.A.; Chanda, E.; Fouque, F.; Merle, C.S.; Nwangwu, U.; Velayudhan, R.; Venter, M.; Yahouedo, A.G.; Lines, J.; et al. Developing African Arbovirus Networks and Capacity Strengthening in Arbovirus Surveillance and Response: Findings from a Virtual Workshop. Parasit Vectors 2023, 16, 129. [Google Scholar] [CrossRef] [PubMed]
- Giovanetti, M.; Salgado, A.; De Souza Fonseca, V.; Tosta, F.D.O.; Xavier, J.; De Jesus, J.G.; Iani, F.C.M.; Adelino, T.E.R.; Barreto, F.K.; Faria, N.R.; et al. Pan-Genomics of Virus and Its Applications. Pan-genomics: Applications, Challenges, and Future Prospects 2020, 237–250. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




