Submitted:
20 June 2024
Posted:
21 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
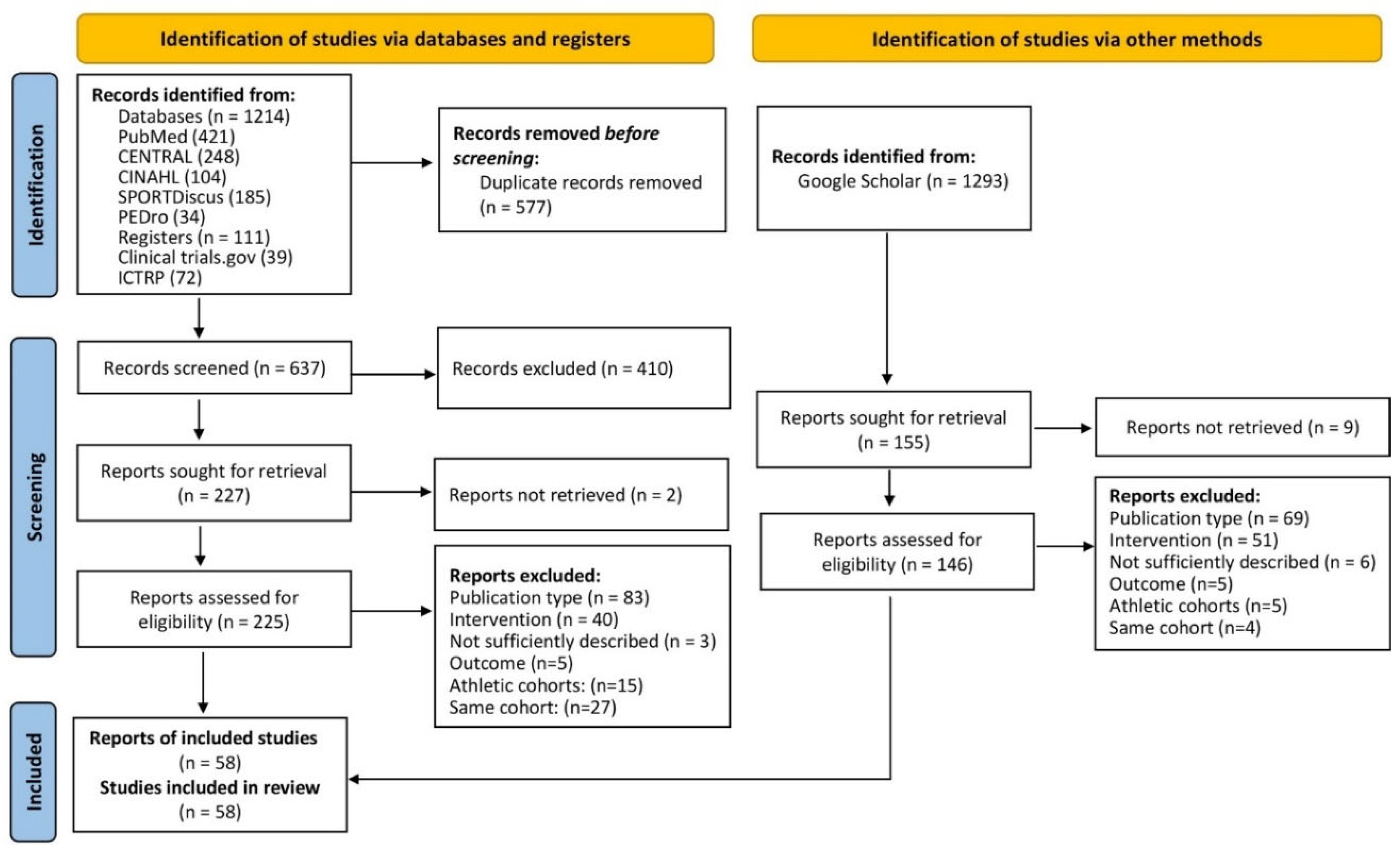
2. Materials and Methods
2.1. Selection Process
2.2. Eligibility Criteria
2.2.1. Population
2.2.2. Intervention
2.2.3. Comparators
2.2.4. Outcomes
2.2.5. Study Design
2.3. Data management
2.4. Data Items
2.5. Quality Assessment
2.6. Data Synthesis
3. Results
3.1. Study and Participant Characteristics
3.2. Intervention Characteristics
3.3. Study Outcomes
3.3.1. Loss to Follow-Up, Withdrawals
| Author | Exercise Type active CG |
Loss to FU WB-EMS (%)3 |
Loss to FU CG (%) |
Loss to FU active CG (%) |
Withdrawal WB-EMS (%) | Withdrawal CG (%) |
Withdrawal active CG (%) |
|---|---|---|---|---|---|---|---|
| Akcay et al [11] | WB-EMS with or without diet | 0 | n.a. | n.a. | 0 | n.a. | n.a. |
| Almada et al [22] | Functional training | 0 | ----- | 0 | 0 | ----- | 0 |
| Amaro-Gahete et al. [23] | Running | 14 | ------ | 14 | 14 | ------ | 14 |
| FIT-Aging, Amaro-Gahete et al [5] | HIT AET + DRT | 17 | 36 | HIT: 30 | 8 | 9 | HIT: 22 |
| WHO PAR | PAR: 24 | PAR: 19 | |||||
| Andre et al [24] | Inactive CG | 15 | 5 | ------ | 10 | 5 | ------ |
| Bellia et al [25] | Inactive CG | 23 | 8 | ------ | n.g. | n.g.. | ------ |
| Berger et al [13] | Inactive CG | 12 | 13 | ------ | 5% | 0 | ------ |
| Blöckl et al [12] | All groups: WB-EMS | 12 | n.a. | n.a. | 8% | n.a. | n.a. |
| Bostan et al [26] | DRT | n.a. | ------ | n.a. | n.g. | ------ | n.a. |
| DiCagno et al [14] | Inactive CG | 0 | 0 | ------ | 0 | 0 | ------ |
| Dyaksa et al [27] | No CG | n.g. | ------ | ------ | n.g. | ------ | ------ |
| Ethem et al [28] | Inactive CG | 0 | 0 | ------ | 0 | 0 | ------ |
| Evangelista et al [30] | DRT | 16 | 0 | 16 | 16 | 0 | 15 |
| Evangelista et al [29] | Funktional Training | 33 | ------ | 33 | 20 | ------ | 33 |
| Fritzsche et al [31] | No CG | 0 | ------ | ------ | 0 | ------ | ----- |
| Ghannadi et al [32] | Aerobic exercise | 15 | ------ | 30 | 5 | ------ | 20 |
| Houdjijk et al [33] | No CG | 0 | ------ | ------ | 0 | ------ | ------ |
| Jee et al [15] | Inactive CG | 5 | 0 | ------ | 5 | 0 | ------ |
| Junger et al [16] | WB-EMS with or without diet | 0 | n.a. | n.a. | 0 | n.a. | n.a. |
| TEST I, Kemmler et al [35] | DRT | 0 | ------ | 0 | 0 | ------- | 0 |
| TEST II Kemmler et al [34] | WBV | 7 | ------ | 29 | 0 | ------ | 0 |
| HIT vs EMS, Kemmler et al [36] | DRT | 9 | ------ | 13 | 4 | ------ | 9 |
| FORMOSA; Kemmler et al [7] | Inactive CG | 10 | 12 | ----- | 4 | 4 | ----- |
| FRANSO, Kemmler et al [8] | Inactive CG/Protein CG | 9 | 7 | ------ | 5 | 4 | ------ |
| Kim et al [37] | Dance, RT, Stretching | 13 | ------ | 20 | 7 | ------ | 13 |
| Kim et al [17] | Isometric RT | 7 | ------ | 7 | 7 | ------ | 0 |
| Kiriscioglu et al [38] | Inactive CG | 0 | 0 | ------ | 0 | 0 | ------ |
| Konrad et al 1 [39] | Multimodal therapy | 6 | ---- | 5 | 0 | ----- | 0 |
| Ludwig et al [18] | Inaktive CG | 10 | 6 | ------ | 2 | 0 | ------ |
| Micke et al [40] | Whole Body Vibration | 9 | ------ | 13 | 3 | ------ | 5 |
| DRT | 13 | 8 | |||||
| Müllerova et al [41] | DRT | 18 | ------ | 20 | 18 | ------ | 20 |
| Öktem et al. [42] | DRT | 0 | ------ | 0 | 0 | ------ | 0 |
| Özdal et al [19] | WB-EMS with or without exercises | 0 | n.a. | n.a. | 0 | n.a. | n.a. |
| Pano-Rodriguez et al [81] | DRT | 6 | ------ | 6 | 6 | ------ | 6 |
| Park et al [46] | Aerobic dance | 6 | ------- | 6 | 6 | ------ | 6 |
| Park et al [45] | Isometric RT | 7 | 7 | 7 | 0 | 0 | 0 |
| Park et al [44] | Low intensity RT | 8 | --- | 0 | 8 | ------ | 0 |
| Park et al [47] | Step Aerobic | 7 | 7 | 0 | 7 | 0 | 0 |
| Qin et al [48] | DRT | 15 | ------ | 25 | 15 | ------ | 8 |
| Reljic et al [49] | HIT-DRT, 1 set protocol | 26 | 26 | 1 set: 18 | 13 | 23 | 1 set: 11 |
| HIT-DRT, 3 set protocol | 3 set: 21 | 3 set 13 | |||||
| Ricci et al [50] | Widely inactive CG | 0 | 0 | ------ | 0 | 0 | ------ |
| Sadeghipour et al [52] | DRT | 0 | 0 | 0 | 0 | 0 | 0 |
| Sadeghipour et al [51] | AE+DRT | 0 | 0 | 0 | 0 | 0 | 0 |
| Sanchez-Infante [53] | AE+DRT | 0 | ------ | 0 | 0 | ------ | 0 |
| Schink et al [54] | Inactive CG, diet | 40 | 31 | ------- | 14 | 17 | ------ |
| Schink et al [55] | Inactive CG, diet | 59 | 33 | ------ | 14 | 11 | ------ |
| Silvestri et al [20] | WB-EMS with or without stretching | 23 | n.a. | n.a | 21 | n.a. | n.a |
| Stephan et al [21] | WB-EMS with or without exercises | 7 | n.a. | n.a. | 7 | n.a. | n.a. |
| Teschler et al [57] | No CG | 0 | ------ | ------ | 0 | ------ | ------ |
| Teschler et al [56] | Local EMS (lower extremities) | 4 | 12 | 16 | 0 | 0 | 0 |
| Vacoulikova et al [58] | DRT | 18 | 0 | 20 | 18 | 0 | 20 |
| Vacoulikova et al [59] | DRT | 0 | 0 | 0 | 0 | 0 | 0 |
| van Buuren et al [61] | Local EMS (lower extremities) | 0 | 0 | 0 | 0 | 0 | 0 |
| van Buuren et al [60] | No CG | 0 | ------ | ------ | 0 | ------ | ------ |
| TEST III, von Stengel et al [6] | Low intensity gymnastics | 16 | ------ | 26 | 5 | ------- | 11 |
| Weissenfels et al [62] | Inactive CG | 7 | 7 | ------ | 0 | 7 | ------ |
| Willert et al [63] | Physical Activity | 3 | 17 | 10 | 0 | 13 | 7 |
| Zink et al [64] | Inactive CG | 33 | 33 | ------ | n.a | n.a. |
3.3.2. Attendance Rate
3.3.3. Adverse Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search date | Search terms | Number of hits |
|---|---|---|---|
| Medline (PubMed) | 6th March 2023 | (WB-EMS[TIAB] OR “whole-body electromyostimulation”[TIAB] OR “whole body electromyostimulation”[TIAB] OR “whole-body electrostimulation”[TIAB] OR “whole body electrostimulation”[TIAB] OR electromyostimulation[TIAB] OR “EMS training”[TIAB] OR “EMS intervention”[TIAB] OR “EMS suit*”[TIAB] OR “EMS belt*”[TIAB] OR “B-SES”[TIAB] OR “belt electrode”[TIAB]) | 421 |
| CENTRAL | 6th March 2023 | (WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body electrostimulation” OR electromyostimulation OR “EMS training” OR “EMS intervention” OR “EMS suit*” OR “EMS belt*” OR “B-SES” OR “belt electrode”):ti,ab,kw | 248 |
| CINAHL | 6th March 2023 | 1. TI (WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body) electrostimulation” OR electromyostimulation OR “EMS training” OR “EMS intervention” OR “EMS suit*” OR “EMS belt*” OR “B-SES” OR “belt electrode” 2. AB (WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body) electrostimulation” OR electromyostimulation OR “EMS training” OR “EMS intervention” OR “EMS suit*” OR “EMS belt*” OR “B-SES” OR “belt electrode” 3. S1 OR S2 |
104 |
| SPORTDiscus | 6th March 2023 | 1. TI (WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body) electrostimulation” OR electromyostimulation OR “EMS training” OR “EMS intervention” OR “EMS suit*” OR “EMS belt*” OR “B-SES” OR “belt electrode” 2. AB (WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body) electrostimulation” OR electromyostimulation OR “EMS training” OR “EMS intervention” OR “EMS suit*” OR “EMS belt*” OR “B-SES” OR “belt electrode” 3. S1 OR S2 |
185 |
| PEDro | 6th March 2023 | Abstract & Title: “whole-body electromyostimulation” Method: clinical trial |
34 |
| Clinicaltrials.gov | 6th March 2023 | other terms: WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body electrostimulation” OR electromyostimulation OR “EMS suit*” OR “EMS belt*” OR “belt electrode*” | 39 |
| ICTRP | 6th March 2023 | Search: WB-EMS OR “whole-body electromyostimulation” OR “whole body electromyostimulation” OR “whole-body electrostimulation” OR “whole body electrostimulation” OR electromyostimulation OR “EMS suit*” OR “EMS belt*” OR “belt electrode*” | 72 |
| Google Scholar | 6th March 2023 | Advanced search: “whole body electromyostimulation” OR “WB EMS” OR “EMS suit” OR “belt electrode” with at least one of the words, anywhere in the article | 1293 |
References
- Kemmler, W.; Kleinoder, H.; Fröhlich, M. Editorial: Whole-Body Electromyostimulation: A Training Technology to Improve Health and Performance in Humans? Front Physiol. 2020, 11, 523. [Google Scholar] [CrossRef] [PubMed]
- Beier, M.; Schoene, D.; Kohl, M.; von Stengel, S.; Uder, M.; Kemmler, W. Non-athletic cohorts enrolled in longitudinal whole-body electromyostimulation trials - An evidence map. Sensors (Basel). 2024, 24, 972. [Google Scholar] [CrossRef] [PubMed]
- Le, Y.E.; Schoene, D.; Kohl, M.; von Stengel, S.; Uder, M.; Kemmler, W. Outcomes addressed by longitudinal whole-body electromyostimulation trials in middle aged-older adults - An evidence map. Japanese Journal of Medical Science. In print. 2023. [Google Scholar]
- Bramer, W.M.; Giustini, D.; de Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016, 104, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Gahete, F.J.; De-la, O.A.; Jurado-Fasoli, L.; et al. Changes in Physical Fitness After 12 Weeks of Structured Concurrent Exercise Training, High Intensity Interval Training, or Whole-Body Electromyostimulation Training in Sedentary Middle-Aged Adults: A Randomized Controlled Trial. Front Physiol. 2019, 10, 451. [Google Scholar] [CrossRef] [PubMed]
- von Stengel, S.; Bebenek, M.; Engelke, K.; Kemmler, W. Whole-Body Electromyostimulation to Fight Osteopenia in Elderly Females: The Randomized Controlled Training and Electrostimulation Trial (TEST-III). J Osteoporos. 2015, 2015, 643520. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Teschler, M.; Weissenfels, A.; et al. Whole-body electromyostimulation to fight sarcopenic obesity in community-dwelling older women at risk. Resultsof the randomized controlled FORMOsA-sarcopenic obesity study. Osteoporos Int. 2016, 27, 3261–3270. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Weissenfels, A.; Teschler, M.; et al. Whole-body Electromyostimulation and protein supplementation favorably affect Sarcopenic Obesity in community-dwelling older men at risk. The Randomized Controlled FranSO Study. Clin Interv Aging. 2017, 12, 1503–1513. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Ribeiro de Avila, V.; Bento, T.; Gomes, W.; Leitao, J.; Fortuna de Sousa, N. Functional Outcomes and Quality of Life After Ankle Fracture Surgically Treated: A Systematic Review. J Sport Rehabil. 2018, 27, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Akçay, N.; Güney, H.; Kaplan, S.; Akgül, M. Electromyostimulation Exercise with Diet Program is More Effective on Body Composition than its Exercise without Diet. Mediterranean Journal of Sport Science. 2022, 4, 814–822. [Google Scholar]
- Bloeckl, J.; Raps, S.; Weineck, M.; et al. Feasibility and Safety of Whole-Body Electromyostimulation in Frail Older People-A Pilot Trial. Front Physiol. 2022, 13, 856681. [Google Scholar] [CrossRef]
- Berger, J.; Ludwig, O.; Becker, S.; Backfisch, M.; Kemmler, W.; Frohlich, M. Effects of an Impulse Frequency Dependent 10-Week Whole-body Electromyostimulation Training Program on Specific Sport Performance Parameters. J Sports Sci Med. 2020, 19, 271–281. [Google Scholar]
- di Cagno, A.; Buonsenso, A.; Centorbi, M.; et al. Whole body-electromyostimulation effects on serum biomarkers, physical performances and fatigue in Parkinson's patients: A randomized controlled trial. Front Aging Neurosci. 2023, 15, 1086487. [Google Scholar] [CrossRef]
- Jee, Y.-S. The effect of high-impulse-electromyostimulation on adipokine profiles, body composition and strength: A pilot study. J Isokinetics. 2019, 27, 163–176. [Google Scholar] [CrossRef]
- Junger, J.; Junger, A.; Ostrowski, P. Body composition of trainees undergoing EMS training with respect to their nutrition. Journal of Physical Education and Sport. 2020, 20, 97–101. [Google Scholar]
- Kim, K.; Eun, D.; Jee, Y.S. Higher Impulse Electromyostimulation Contributes to Psychological Satisfaction and Physical Development in Healthy Men. Medicina (Kaunas). 2021, 57, 197. [Google Scholar] [CrossRef]
- Ludwig, O.; Berger, J.; Becker, S.; Kemmler, W.; Frohlich, M. The Impact of Whole-Body Electromyostimulation on Body Posture and Trunk Muscle Strength in Untrained Persons. Front Physiol. 2019, 10, 1020. [Google Scholar] [CrossRef]
- Özdal, M.; Bostanci, Ö. Effects of whole-body electromyostimulation with and without voluntary muscular contractions on total and regional fat mass of women. Archives of Applied Science Research. 2016, 8, 75–79. [Google Scholar]
- Silvestri, A.; Ruscello, B.; Rosazza, C.; et al. Acute Effects of Whole-Body Electrostimulation Combined with Stretching on Lower Back Pain. Int J Sports Med. 2023, 44, 820–829. [Google Scholar] [CrossRef]
- Stephan, H.; Wehmeier, U.F.; Forster, T.; Tomschi, F.; Hilberg, T. Additional Active Movements Are Not Required for Strength Gains in the Untrained during Short-Term Whole-Body Electromyostimulation Training. Healthcare 2023, 11, 741. [Google Scholar] [CrossRef]
- Almada, R.; Molina Martín, J.J.; Tregón, P.S.; García, J.L. Comparación Entre los Efectos de un Programa de Entrenamiento de Fuerza Explosiva Mediante Bandas Elásticas y un Programa de Entrenamiento con Electro-Estimulación de Cuerpo Completo. Revista Kronos. 2016, 15. [Google Scholar]
- Amaro-Gahete, F.J.; De-la, O.A.; Sanchez-Delgado, G.; et al. Functional Exercise Training and Undulating Periodization Enhances the Effect of Whole-Body Electromyostimulation Training on Running Performance. Front Physiol. 2018, 9, 720. [Google Scholar] [CrossRef]
- Andre, L.D.; Basso-Vanelli, R.P.; Ricci, P.A.; et al. Whole-body electrical stimulation as a strategy to improve functional capacity and preserver lean mass after bariatric surgery: a randomized triple-blind controlled trial. Int J Obes (Lond). 2021, 45, 1476–1487. [Google Scholar] [CrossRef]
- Bellia, A.; Ruscello, B.; Bolognino, R.; et al. Whole-body Electromyostimulation plus Caloric Restriction in Metabolic Syndrome. Int J Sports Med. 2020, 41, 751–758. [Google Scholar] [CrossRef]
- Bostan, G.; Gümüş, M. Effects of fitness and electromyostimulation (EMS) training techniques on body composition [Antrenman Tekniklerinin Vücut Kompozisyonu Üzerine Etkileri]. Turkish Journal of Diabetes and Obesity. 2022, 6, 149–158. [Google Scholar] [CrossRef]
- Dyaksa, R.S.; Susilo, E.A.; Virdianto, A.W. The Effect of EMS Exercise on Body Circumstances in Sedentary Women [PENGARUH LATIHAN EMS TERHADAP LINGKAR TUBUH PADA WANITA SEDENTARY]. Journal of Physical Education, Sports and Health. 2022, 5, 264–270. [Google Scholar]
- Ethem, H.; Orhan, İ.; ÇAnakci, G. Investigation of the Effect of 6 Weeks Whole-Body Electromyostimulation and with Body Weight Strength Training on some Motoric Properties in Sedantery Women [Sedanter Kadınlarda Tüm Beden Elektromyostimülasyonla Kombine Dinamik Kuvvet Alıştırmalarının Bazı Motorik Özellikler Üzerine Etkisinin İncelenmesi]. Eurasian Research in Sport Science. 2019, 2, 83–96. [Google Scholar]
- Evangelista, A.L.; Alonso, A.C.; Ritti-Dias, R.M.; et al. Effects of Whole Body Electrostimulation Associated With Body Weight Training on Functional Capacity and Body Composition in Inactive Older People. Front Physiol. 2021, 12, 638936. [Google Scholar] [CrossRef]
- Evangelista, A.L.; Teixeira CV, S.; Barros, B.M.; et al. Does whole-body electrical muscle stimulation combined with strength training promote morphofunctional alterations? Clinics (Sao Paulo). 2019, 74, e1334. [Google Scholar] [CrossRef]
- Fritzsche, D.; Fruend, A.; Schenk, S.; et al. Elektromyostimulation (EMS) bei kardiologischen Patienten. Wird das EMS-Training bedeutsam für die Sekundärprävention? Herz. 2010, 35, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Ghannadi, S.; Halabchi, F.; Maleklou, F.; et al. The effect of 6 weeks electrical muscle stimulation training and aerobic exercise on body composition of overweight women: a randomized controlled study. Sport Sciences for Health. 2022, 18, 1387–1395. [Google Scholar] [CrossRef]
- Houdijk AP, J.; Bos, N.; Verduin, W.M.; Zwartkruis MA, L. Visceral fat loss by whole-body electromyostimulation is attenuated in male and absent in female older Non-Insulin-Dependent diabetes patients. Endocrinol Diabetes Metab. 2022, 5, e377. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Birlauf, A.; von Stengel, S. Einfluss von Ganzkörper-Elektromyostimulation auf das Metabolische Syndrom bei älteren Männern mit metabolischem Syndrom. Dtsch Z Sportmed. 2010, 61, 117–123. [Google Scholar]
- Kemmler, W.; Schliffka, R.; Mayhew, J.L.; von Stengel, S. Effects of Whole-Body-Electromyostimulation on Resting Metabolic Rate, Anthropometric and Neuromuscular Parameters in the Elderly. The Training and ElectroStimulation Trial (TEST). J Strength Cond Res. 2010, 24, 1880–1886. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Teschler, M.; Weissenfels, A.; et al. Effects of Whole-Body Electromyostimulation versus High-Intensity Resistance Exercise on Body Composition and Strength: A Randomized Controlled Study. Evid Based Complement Alternat Med. 2016, 2016, 9236809. [Google Scholar] [CrossRef]
- Kim, J.; Jee, Y. EMS-effect of Exercises with Music on Fatness and Biomarkers of Obese Elderly Women. Medicina 2020, 56, 156. [Google Scholar] [CrossRef]
- Kirişcioğlu, M.; Bicer, M.; Pancar, Z.; Doğan, İ. Effects of electromyostımulatıon traınıng on body composıtıon. Turkish Journal of Sport and Exercise. 2019, 21, 34–37. [Google Scholar]
- Konrad, K.L.; Baeyens, J.-P.; Birkenmaier, C.; et al. The effects of whole-body electromyostimulation (WB-EMS) in comparison to a multimodal treatment concept in patients with non-specific chronic back pain—A prospective clinical intervention study. PloS one 2020, 15, e0236780. [Google Scholar] [CrossRef]
- Micke, F.; Weissenfels, A.; Wirtz, N.; et al. Similar Pain Intensity Reductions and Trunk Strength Improvements following Whole-Body Electromyostimulation vs. Whole-Body Vibration vs. Conventional Back-Strengthening Training in Chronic Non-specific Low Back Pain Patients: A 3-armed randomized controlled trial. Front Physiol. 2021, 13, 664991. [Google Scholar]
- Müllerová, M.; Vaculíková, P.; Potúčková, A.; Struhár, I.; Balousová, D.N. Impact of Whole-Body Electromyostimulation and Resistance Training Programme on Strength Parameters and Body Composition in Group of Elderly Women at Risk of Sarcopenia. Studia sportiva. 2022, 16, 292–304. [Google Scholar] [CrossRef]
- Öktem, U.; Akin, M. Investigation of the Effects of Electrical Muscle Stimulation (EMS) and Traditional Training on Strength Gain and Anthropometric Properties in Sedentary Women [Sedanter Kadınlarda Elektriksel Kas Uyarımı (EMS) ve Geleneksel Antrenmanın Kuvvet Kazanımı ve Antropometrik Özellikler Üzerine Etkisinin İncelenmesi]. CBU Journal of Physical Education and Sport Science. 2022, 17, 70–79. [Google Scholar]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernandez-Gonzalez, V.; Reverter-Masia, J. Effects of Whole-Body Electromyostimulation on Physical Fitness in Postmenopausal Women: A Randomized Controlled Trial. Sensors (Basel). 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Park, H.K.; Na, S.M.; Choi, S.L.; Seon, J.K.; Do, W.H. Physiological Effect of Exercise Training with Whole Body Electric Muscle Stimulation Suit on Strength and Balance in Young Women: A Randomized Controlled Trial. Chonnam Med J. 2021, 57, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Min, S.; Park, S.H.; Yoo, J.; Jee, Y.S. Influence of Isometric Exercise Combined With Electromyostimulation on Inflammatory Cytokine Levels, Muscle Strength, and Knee Joint Function in Elderly Women With Early Knee Osteoarthritis. Front Physiol. 2021, 12, 688260. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Park, J.; Ham, J.A.; Jee, Y. Effects of aerobic dance with electrical stimulant on body composition and radiological circumference of obese elderly women. Gazzetta Medica Italiana Archivio per le Scienze Mediche. 2021, 180. [Google Scholar] [CrossRef]
- Park, W.; Lee, J.; Hong, K.; et al. Protein-Added Healthy Lunch-Boxes Combined with Exercise for Improving Physical Fitness and Vascular Function in Pre-Frail Older Women: A Community-Based Randomized Controlled Trial. Clin Interv Aging. 2023, 18, 13–27. [Google Scholar] [PubMed]
- Qin, Y.; Chen, H.; Liu, X.; Wu, J.; Zhang, Y. Effects of whole-body electromyostimulation training on upper limb muscles strength and body composition in moderately trained males: A randomized controlled study. Front Public Health. 2022, 10, 982062. [Google Scholar] [CrossRef] [PubMed]
- Reljic, D.; Herrmann, H.J.; Neurath, M.F.; Zopf, Y. Iron Beats Electricity: Resistance Training but Not Whole-Body Electromyostimulation Improves Cardiometabolic Health in Obese Metabolic Syndrome Patients during Caloric Restriction-A Randomized-Controlled Study. Nutrients. 2021, 13, 1640. [Google Scholar] [CrossRef]
- Ricci, P.A.; Di Thommazo-Luporini, L.; Jurgensen, S.P.; et al. Effects of Whole-Body Electromyostimulation Associated with Dynamic Exercise on Functional Capacity and Heart Rate Variability After Bariatric Surgery: a Randomized, Double-Blind, and Sham-Controlled Trial. Obes Surg. 2020, 30, 3862–3871. [Google Scholar] [CrossRef]
- Sadeghipour, S.; Mirzaei, B. Effects of whole-body electromyostimulation with two different frequencies and combined training on lipid profile and body composition in overweight women. Physiotherapy Quarterly. 2022, 30, 79–85. [Google Scholar] [CrossRef]
- Sadeghipour, S.; Mirzaei, B.; Korobeynikov, G.; Tropin, Y. Effects of Whole-Body Electromyostimulation and Resistance Training on Body Composition and Maximal Strength in Trained Women. Health, Sport, Rehabilitation. 2021, 7, 18–28. [Google Scholar] [CrossRef]
- Sánchez-Infante, J.; Bravo-Sáncheza, A.; Abiánb, P.; Estebana, P.; Jimeneza, J.; Abián-Vicén, J. The influence of whole-body electromyostimulation training in middle-aged women. Isokinet Exerc Sci 2020, 1, 1–9. [Google Scholar] [CrossRef]
- Schink, K.; Herrmann, H.J.; Schwappacher, R.; et al. Effects of whole-body electromyostimulation combined with individualized nutritional support on body composition in patients with advanced cancer: a controlled pilot trial. BMC Cancer. 2018, 18, 886. [Google Scholar] [CrossRef]
- Schink, K.; Reljic, D.; Herrmann, H.J.; et al. Whole-Body Electromyostimulation Combined With Individualized Nutritional Support Improves Body Composition in Patients With Hematological Malignancies - A Pilot Study. Front Physiol. 2018, 9, 1808. [Google Scholar] [CrossRef]
- Teschler, M.; Heimer, M.; Schmitz, B.; Kemmler, W.; Mooren, F.C. Four weeks of electromyostimulation improves muscle function and strength in sarcopenic patients: a three-arm parallel randomized trial. J Cachexia Sarcopenia Muscle. 2021, 12, 843–854. [Google Scholar] [CrossRef]
- Teschler, M.; Weissenfels, A.; Bebenek, M.; et al. Very high creatine kinase CK levels after WB_EMS. Are there implications for health. Int J Clin Exp Med 2016, 9, 22841–22850. [Google Scholar]
- Vaculikova, P.; Paclíková, A.; Kotkova, M.; Struhar, I.; Balousova, D.N. Impact of Whole-Body Electromyostimulation and Resistance Training on Bone Mineral Density in women at risk for Osteopororosis. IJPESS. 2022, 69–79. [Google Scholar] [CrossRef]
- Vaculikova, P.; Paclíková, A.; Kotkova, M.; Struhar, I.; Balousova, D.; Rozsypal, R. Impact of Whole-Body Electromyostimulation and Resistance Training on the Level of Functional Fitness in Elderly Women. Studia Sportiva. 2023, 16, 115–126. [Google Scholar] [CrossRef]
- van Buuren, F.; Horstkotte, D.; Mellwig, K.; et al. Electrical Myostimulation (EMS) Improves Glucose Metabolism and Oxygen Uptake in Type 2 Diabetes Mellitus Patients—Results from the EMS Study. Diabetes Technol Ther. 2015, 17, 413–419. [Google Scholar] [CrossRef]
- van Buuren, F.; Mellwig K., P.; Prinz, C. , et al. Electrical myostimulation improves left ventricular function and peak oxygen consumption in patients with chronic heart failure: results from the exEMS study comparing different stimulation strategies. Clin Res Cardiol. 2013, 102, 523–534. [Google Scholar] [CrossRef] [PubMed]
- Weissenfels, A.; Teschler, M.; Willert, S.; et al. Effects of whole-body electromyostimulation on chronic nonspecific low back pain in adults: a randomized controlled study. J Pain Res. 2018, 11, 1949–1957. [Google Scholar] [CrossRef] [PubMed]
- Willert, S.; Weissenfels, A.; Kohl, M.; et al. Effects of Whole-Body Electromyostimulation (WB-EMS) on the energy-restriction-induced reduction of muscle mass during intended weight loss. Frontiers of Physiology. 2019, 1012. [Google Scholar] [CrossRef]
- Zink-Rückel, C.; Kohl, M.; von Stengel, S.; Kemmler, W. Once weekly whole-body electromyostimulation increase strength, stability and body composition in amateur golfers. A randomized controlled study. Int. J. Environ. Res. Public Health. 2021, 18, 5628. [Google Scholar] [CrossRef]
- Kemmler, W.; Bebenek, M.; Engelke, K.; von Stengel, S. Impact of whole-body electromyostimulation on body composition in elderly women at risk for sarcopenia: the Training and ElectroStimulation Trial (TEST-III). Age 2014, 36, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Fröhlich, M.; Eifler, C. Whole-Body Electromyostimulation. Effects, Limitations, Perspectives of an Innovative Training Method; Springer, 2024.
- Kemmler, W.; von Stengel, S.; Kohl, M.; et al. Safety of a Combined WB-EMS and High-Protein Diet Intervention in Sarcopenic Obese Elderly Men. Clin Interv Aging. 2020, 15, 953–967. [Google Scholar] [CrossRef] [PubMed]
- Linssen, G.C.; Bakker, S.J.; Voors, A.A.; et al. N-terminal pro-B-type natriuretic peptide is an independent predictor of cardiovascular morbidity and mortality in the general population. Eur Heart J. 2010, 31, 120–127. [Google Scholar] [CrossRef]
- Kemmler, W.; Fröhlich, M.; Ludwig, O.; et al. Position statement and updated international guideline for safe and effective whole-body electromyostimulation training-the need for common sense in WB-EMS application. Front Physiol. 2023, 14, 1174103. [Google Scholar] [CrossRef]
- de Oliveira TM, D.; Felicio, D.C.; Filho, J.E.; Fonseca, D.S.; Durigan JL, Q.; Malaguti, C. Effects of whole-body electromyostimulation on health indicators of older people: Systematic review and meta-analysis of randomized trials. J Bodyw Mov Ther. 2022, 31, 134–145. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010, 340, c869. [Google Scholar] [CrossRef]
- Phillips, E.M.; Katula, J.; Miller, M.E.; et al. Interruption of physical activity because of illness in the Lifestyle Interventions and Independence for Elders Pilot trial. J Aging Phys Act. 2010, 18, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Oldridge, N.B.; Donner, A.P.; Buck, C.W.; et al. Predictors of dropout from cardiac exercise rehabilitation. Ontario Exercise-Heart Collaborative Study. Am J Cardiol. 1983, 51, 70–74. [Google Scholar] [CrossRef]
- Pahmeier, I. Drop-out und Bindung im Breiten und Gesundheitssport. Sportwissenschaften. 1994, 24, 117–150. [Google Scholar]
- Pahmeier, I. Partizipation, bindung und dropout im freizeit-, breiten-und gesundheitssport. Anwendungen der Sportpsychologie. 2008, 2, 425–497. [Google Scholar]
- Vancampfort, D.; Sanchez CP, R.; Hallgren, M.; et al. Dropout from exercise randomized controlled trials among people with anxiety and stress-related disorders: A meta-analysis and meta-regression. J Affect Disord. 2021, 282, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Van Damme, T.; Brunner, E.; et al. Dropout From Exercise Interventions in Adults With Fibromyalgia: A Systematic Review and Meta-analysis. Arch Phys Med Rehabil. 2024, 105, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Steele, J.; Wolf, M.; Androulakis-Korakakis, P.; Smith, D.; Giessing, J.; Wescott, W.L. The role of supervision in resistance training; an exploratory systematic review and meta-analysis. Sportrxiv. 2021. [Google Scholar] [CrossRef]
- von Stengel, S.; Frohlich, M.; Ludwig, O.; et al. Revised contraindications for the use of non-medical WB-electromyostimulation. Evidence-based German consensus recommendations. Front Sports Act Living. 2024, 6, 1371723. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Pano-Rodriguez, A.; Beltran-Garrido, J.V.; Hernandez-Gonzalez, V.; Nasarre-Nacenta, N.; Reverter-Masia, J. Impact of Whole Body Electromyostimulation on Velocity, Power and Body Composition in Postmenopausal Women: A Randomized Controlled Trial. Int J Environ Res Public Health. 2020, 17, 4982. [Google Scholar] [CrossRef]
| Author | Publication year | Study design | Study groups [n] | Total sample size [n] | Gender | Age [years] |
Body Mass Index (BMI) (kg/m2)1 | Health status | Training status2 | methodological quality (PEDro) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Akcay et al [11] | 2022 | RCT | 2 | 104 | m+w | 33 ± 1 | 27.2 | healthy | untrained | 5 |
| 2 | Almada et al [22] | 2016 | RCT | 2 | 10 | m | 23 ± 3 | 23.7 | healthy | moderate | 4 |
| 3 | Amaro-Gahete et al [23] | 2018 | RCT | 2 | 12 | m | 27 ± 7 | 23.8 | healthy | well-trained | 6 |
| 4 | FitAging, Amaro-Gahete et al [5] | 2019 | RCT | 4 | 89 | m+w | 53 ± 5 | 26.8 | healthy | untrained | 6 |
| 5 | Andre et al [24] | 2021 | RCT | 2 | 39 | m+w | 39 ± 2 | 40.5 | Obese | untrained | 8 |
| 6 | Bellia et al [25] | 2020 | RCT | 2 | 25 | m+w | 49 ± 7 | 40.1 | Obese | moderate | 3 |
| 7 | Berger et al [13] | 2020 | RCT | 3 | 51 | m+w | 26 ± 3 | 23.8 | healthy | moderate | 6 |
| 8 | Blöckl et al [12] | 2022 | NRCT | 2 | 18 | m+w | 80 ± 4 | 26.2 | Frailty | untrained | 4 |
| 9 | Bostan et al [26] | 2022 | RCT | 2 | 128 | m+w | >18 | n.g. | healthy | untrained | 4 |
| 10 | DiCagno et al [14] | 2023 | RCT | 2 | 24 | m+w | 72 ± 6 | n.g. | Parkinson | untrained | 8 |
| 11 | Dyaksa et al [27] | 2022 | Intervention, single group | 1 | 10 | w | n.g. | n.g. | healthy | n.g. | 2 |
| 12 | Ethem et al [28] | 2019 | RCT | 2 | 18 | w | 38 ± 5 | 23.7 | healthy | untrained | 4 |
| 13 | Evangelista et al [30] | 2019 | RCT | 3 | 58 | m+w | 26 ± 4 | 25.2 | healthy | moderate | 4 |
| 14 | Evangelista et al [29] | 2021 | RCT | 2 | 30 | m | 75 ± 7 | n.g. | healthy | untrained | 5 |
| 15 | Fritzsche et al [31] | 2010 | Intervention, single group | 1 | 15 | m+w | 27 - 73 | 26.8 | CHD | untrained | 2 |
| 16 | Ghannadi et al [32] | 2022 | RCT | 2 | 40 | w | 33 ± 6 | 27.3 | healthy | untrained | 4 |
| 17 | Houdjijk et al [33] | 2022 | NRCT | 4 | 75 | m+w | 45-75 | 31.8 | NIDDP | untrained | 3 |
| 18 | Jee et al [15] | 2019 | RCT | 4 | 54 | m | 25 ± 2 | 22.0 | healthy | untrained | 5 |
| 19 | Junger et al [16] | 2020 | NRCT | 2 | 86 | m+w | 18-62 | 23.0 | healthy | moderate | 3 |
| 20 | TEST I, Kemmler et al [35] | 2010 | RCT | 2 | 30 | w | 65 ± 6 | 26.0 | Osteopenia | well-trained | 6 |
| 21 | TEST II, Kemmler et al [34] | 2010 | RCT | 2 | 28 | m | 69 ± 3 | 28.1 | MetS | untrained | 5 |
| 22 | HIT vs EMS, Kemmler et al [36] | 2016 | RCT | 2 | 46 | m | 30-50 | 28.5 | healthy | moderate | 7 |
| 23 | FORMOSA, Kemmler et al [7] | 2016 | RCT | 3 | 75 | w | 77 ± 4 | 25.1 | Sarcopenic Obesity | untrained | 8 |
| 24 | FRANSO, Kemmler et al [8] | 2017 | RCT | 3 | 100 | m | 77 ± 5 | 26.1 | Sarcopenic Obesity | untrained | 8 |
| 25 | Kim et al [37] | 2020 | RCT | 2 | 25 | w | 71 ± 3 | 30.9 | Obesity | untrained | 6 |
| 26 | Kim et al [17] | 2021 | RCT | 4 | 54 | m | 24 ± 2 | 25.1 | healthy | moderate | 7 |
| 27 | Kiriscioglu et al [38] | 2019 | NRCT | 2 | 41 | w | 34 ± 9 | 25.3 | healthy | well-trained | 3 |
| 28 | Konrad et al [39] | 2020 | NRCT | 2 | 128 | m+w | 56 ± 14 | n.g. | LBP | untrained | 2 |
| 29 | Ludwig et al [18] | 2019 | RCT | 3 | 58 | m+w | 25 ± 4 | 23.9 | healthy | moderate | 4 |
| 30 | Micke et al [40] | 2021 | RCT | 4 | 240 | m+w | 40-70 | 26.3 | LBP | moderate | 8 |
| 31 | Müllerova et al [41] | 2022 | RCT | 2 | 21 | w | 63 ± 2 | 26.6 | healthy | untrained | 4 |
| 32 | Özdal et al [19] | 2016 | RCT | 2 | 40 | w | 32 ± 8 | 24.5 | healthy | untrained | 3 |
| 33 | Öktem et al. [42] | 2022 | RCT | 2 | 20 | W | 22-27 | 23.6 | healthy | untrained | 4 |
| 34 | Pano-Rodriguez et al [43] | 2020 | RCT | 2 | 34 | w | 61 ± 4 | 26.5 | healthy | untrained | 7 |
| 35 | Park et al [46] | 2021 | RCT | 2 | 34 | w | 70 ± 4 | 27.5 | Obese | untrained | 7 |
| 36 | Park et al [45] | 2021 | RCT | 3 | 81 | w | 61-79 | 24.4 | Knee OA | untrained | 7 |
| 37 | Park et al [44] | 2021 | RCT | 2 | 24 | w | 20-40 | 25.0 | healthy | n.g. | 8 |
| 38 | Park et al [47] | 2023 | RCT | 4 | 60 | w | ≥65 | 25.4 | Pre-Frailty | untrained | 7 |
| 39 | Qin et al [48] | 2022 | RCT | 2 | 25 | m | 25 ± 4 | 24.0 | healthy | well-trained | 6 |
| 40 | Reljic et al [49] | 2022 | RCT | 4 | 103 | m+w | ≥18 | 37.2 | Obese, MetS |
untrained | 6 |
| 41 | Ricci et al [50] | 2020 | RCT | 2 | 20 | m+w | 32-45 | 38.2 | Obese | untrained | 9 |
| 42 | Sadeghipour et al [52] | 2021 | RCT | 3 | 30 | w | 26 ± 2 | 21.7 | healthy | well-trained | 5 |
| 43 | Sadeghipour et al [51] | 2022 | RCT | 3 | 45 | w | 32 ± 5 | 27.8 | healthy | moderate | 4 |
| 44 | Sanchez-Infante et al [53] | 2020 | RCT | 2 | 28 | w | 40-60 | 25.5 | healthy | moderate | 6 |
| 45 | Schink et al [54] | 2018 | NRCT | 2 | 131 | m+w | ≥18 | 25.2 | Advanced Cancer | untrained | 3 |
| 46 | Schink et al [55] | 2018 | NRCT | 2 | 31 | m+w | ≥18 | 25.4 | Advanced Cancer | untrained | 3 |
| 47 | Silvestri et al [20] | 2023 | NRCT | 2 | 52 | m+w | 43-81 | 24.3 | LBP | untrained | 3 |
| 48 | Stephan et al [21] | 2023 | RCT | 2 | 60 | m+w | 25-36 | 25.3 | healthy | untrained | 5 |
| 49 | Teschler et al [57] | 2016 | Intervention, single group | 2 | 11 | m | 20-50 | 24.9 | healthy | well-trained | 3 |
| 50 | Teschler et al [56] | 2021 | RCT | 3 | 134 | m+w | 56 ± 7 | 35.7 | Sarcopenia | untrained | 7 |
| 51 | Vacoulikova et al [58] | 2021 | RCT | 3 | 32 | w | 60-65 | 27.1 | healthy | untrained | 4 |
| 52 | Vacoulikova et al [59] | 2021 | RCT | 3 | 63 | w | 60-65 | 27.0 | Osteopenia | untrained | 4 |
| 53 | van Buuren et al [61] | 2014 | NRCT | 3 | 60 | m+w | 61 ± 13 | 29.7 | CHD | n.g. | 4 |
| 54 | van Buuren et al [60] | 2015 | Intervention, single group | 1 | 15 | m+w | 62 ± 3 | 34.6 | NIDDM | n.g. | 4 |
| 55 | TEST III, von Stengel et al [6] | 2015 | RCT | 2 | 76 | w | >70 | 22.2 | Osteopenia | untrained | 7 |
| 56 | Weissenfels et al [62] | 2018 | RCT | 2 | 30 | m+w | 57 ± 7 | 27.9 | LBP | moderate | 8 |
| 57 | Willert et al [63] | 2019 | RCT | 3 | 90 | w | 25-50 | 31.3 | Obese | moderate | 6 |
| 58 | Zink et al [64] | 2021 | RCT | 2 | 54 | m | 18-70 | 27.4 | healthy | moderate | 7 |
| Author | Sample size | Age (years) |
Active CG Type of exercise |
Attendance WB-EMS (%) |
Attendance active CG (%) | Adverse effects WB-EMS |
Adverse effects Active CG |
|
|---|---|---|---|---|---|---|---|---|
| 1 | Akcay et al [11] | 104 | 33 ± 1 | WB-EMS with or without diet | 90 | n.a. | No | n.a. |
| 2 | Almada et al [22] | 10 | 23 ± 3 | Funktional training | n.g. | n.g. | n.g. | n.g |
| 3 | Amaro-Gahete et al [23] | 12 | 27 ± 7 | Running | 96 | n.g. | no | n.g. |
| 4 | FitAging, Amaro-Gahete et al. [5] | 89 | 53 ± 5 | HIT Aerobic and DRT | 99 | 98 | no | no |
| WHO-Physical Activity | 99 | no | ||||||
| 5 | Andre et al [24] | 39 | 39 ± 2 | Inactive CG | 91 | ----- | no | ----- |
| 6 | Bellia et al [25] | 25 | 49 ± 7 | Inactive CG (diet) | 90 | ----- | no | ----- |
| 7 | Berger et al [13] | 51 | 26 ± 3 | Inactive CG | 100 | ----- | no | ----- |
| 8 | Blöckl et al [12] | 18 | 80 ± 4 | All groups: WB-EMS | 90 | n.a. | no | ----- |
| 9 | Bostan et al [26] | 128 | >18 | DRT | n.g. | n.g. | no | no |
| 10 | DiCagno et al [14] | 24 | 72 ± 6 | Inactive CG | 100 | ----- | no | ----- |
| 11 | Dyaksa et al [27] | 10 | n.g. | No CG | n.g. | ----- | n.g. | ----- |
| 12 | Ethem et al [28] | 18 | 38 ± 5 | Inactive CG | n.g. | ----- | no | ----- |
| 13 | Evangelista et al [30] | 58 | 26 ± 4 | DRT | n.a. | n.a. | no | no |
| 14 | Evangelista et al [29] | 30 | 75 ± 7 | Functional training | 100 | 100 | no | no |
| 15 | Fritzsche et al [31] | 15 | 27 - 73 | No CG | n.g. | ----- | ALF | ----- |
| 16 | Ghannadi et al [32] | 40 | 33 ± 6 | Aerobic exercise | 80 | 75 | no | no |
| 17 | Houdjijk et al [33] | 75 | 45-75 | No CG | 95 | ----- | no1 | ----- |
| 18 | Jee et al [15] | 54 | 25 ± 2 | Inactive CG | 100 | ----- | no | ----- |
| 19 | Junger et al [16] | 86 | 18-62 | WB-EMS with or without diet | 100 | n.a. | no | n.a. |
| 20 | TEST I, Kemmler et al [35] | 30 | 65 ± 6 | DRT | 98 | 80 | no | no |
| 21 | TEST II, Kemmler et al [34] | 28 | 69 ± 3 | Whole body Vibration | 78 | 74 | no | no |
| 22 | Kemmler et al [36] | 46 | 30-50 | DRT | 90 | 93 | no | no |
| 23 | FORMOSA; Kemmler et al [7] | 75 | 77 ± 4 | Inaktive CG | 89 | ----- | no | ----- |
| 24 | FRANSO, Kemmler et al [8] | 100 | 77 ± 5 | Inaktive CG | 91 | ----- | ALF | ----- |
| 25 | Kim et al [37] | 25 | 71 ± 3 | Dance, RT, Stretching | n.g. | n.g. | no | no |
| 26 | Kim et al [17] | 54 | 24 ± 2 | Isometric RT | n.g. | n.g | no | no |
| 27 | Kiriscioglu et al [38] | 41 | 34 ± 9 | Inactive CG | 95 | ------ | no | ----- |
| 28 | Konrad et al [39] | 128 | 56 ± 14 | Multimodal therapy | 85 | n.g. | no | n.g. |
| 29 | Ludwig et al [18] | 58 | 25 ± 4 | Inactive CG | 100 | ----- | no | ----- |
| 30 | Micke et al [40] | 240 | 40-70 | Whole Body Vibration | 92 | 91 | no | no |
| DRT | 88 | no | ||||||
| 31 | Müllerova et al [41] | 21 | 63 ± 2 | DRT | n.a. | n.a. | n.g. | n.g. |
| 33 | Öktem et al. [42] | 20 | 22-27 | DRT | n.g. | n.g. | n.g. | no |
| 32 | Özdal et al [19] | 40 | 32 ± 8 | WB-EMS with or without exercise | n.g. | n.a. | no | n.a. |
| 34 | Pano-Rodriguez et al [81]} | 34 | 61 ± 4 | DRT | 93 | 89 | no | no |
| 35 | Park et al [46] | 34 | 70 ± 4 | Aerobic dance | 100 | 100 | no | no |
| 36 | Park et al [45] | 81 | 61-79 | Isometric RT | 92 | n.g. | no | no |
| 37 | Park et al [44] | 24 | 20-40 | Low intensity RT | n.g. | n.g. | no | no |
| 38 | Park et al [47] | 60 | ≥65 | Step Aerobic | 91 | 97 | no | no |
| 39 | Qin et al [48] | 25 | 25 ± 4 | DRT | 100 | 100 | no | no |
| 40 | Reljic et al [49] | 103 | ≥18 | HIT-DRT single set | 93 | 94 | no | no |
| HIT-DRT multiple set (3 sets) | 95 | no | ||||||
| 41 | Ricci et al [50] | 20 | 32-45 | (Widely) inactive CG | 100 | ----- | no | ---- |
| 42 | Sadeghipour et al [52] | 30 | 26 ± 2 | DRT | n.g. | n.g. | n.g. | n.g. |
| 43 | Sadeghipour et al [51] | 45 | 32 ± 5 | Aerobic and DRT | 100 | 100 | no | no |
| 44 | Sanchez-Infante et al [53] | 28 | 40-60 | HIIT aerobic and DRT | 100 | n.g. | no | no |
| 45 | Schink et al [54] | 131 | ≥18 | Inactive CG (diet) | 87 | ----- | no | ----- |
| 46 | Schink et al [55] | 31 | ≥18 | Inactive CG (diet) | 77 | ---- | ALF | ----- |
| 47 | Silvestri et al [20] | 52 | 43-81 | WB-EMS with or without stretching | 91 | n.a. | no | n.a. |
| 48 | Stephan et al [21] | 30 | 20-36 | WB-EMS with or without exercise | n.g. | n.a. | no | n.a. |
| 49 | Teschler et al [57] | 11 | 20-50 | No CG | 100 | ------ | ALF2 | ----- |
| 50 | Teschler et al [56] | 134 | 56 ± 7 | Local EMS (lower extremities) | 98 | 98 | no | no |
| 51 | Vacoulikova et al [58] | 32 | 60-65 | DRT | n.a. | n.a. | no | no |
| 52 | Vacoulikova et al [59] | 63 | 60-65 | DRT | n.a. | n.a. | no | no |
| 53 | van Buuren et al [61] | 60 | 61±13 | Local EMS (lower extremities) | 100 | 100 | no | no |
| 54 | van Buuren et al [60] | 15 | 62 ± 3 | No CG | 100 | ------- | no | ----- |
| 55 | TEST III, von Stengel et al [6] | 76 | >70 | Low intensity gymnastics | 79 | 74 | no | no |
| 56 | Weissenfels et al [62] | 30 | 57 ± 7 | Inactive CG | 93 | ----- | no | ----- |
| 57 | Willert et al [63] | 90 | 25-50 | Physical activity (walking) | 100 | 72 | no | no |
| 58 | Zink et al [64] | 54 | 18-70 | Inactive CG | 95 | ----- | no | ----- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




