1. Introduction
Alzheimer’s disease (AD) is an irreversible, progressive brain disorder that affects more than millions of individuals worldwide, slowly destroying memory and thinking skills and eventually the ability to carry out simple tasks. Although the specific pathogenesis of AD is not fully understood, it is characterized by changes in the brain, including amyloid beta (Aβ) plaques, neurofibrillary tangles (NFTs), neuroinflammation and synaptic loss. Among these, Aβ accumulation is thought to play a central role in the AD pathology, and appears to be an upstream trigger for the downstream alterations, including the NFTs, inflammation and synaptic loss [
1]. Aβ is generated from amyloid precursor protein (APP) through two subsequent proteolytic cleavages by β-secretase and γ-secretase, which is known as the amyloidogenic pathway [
2]. Conversely, the majority of APP undergo non-amyloidogenic pathway cleavage by α-secretase, resulting in the production of sAPPα, which plays numerous neuroprotective roles in the maintenance of normal physiological function in neurons [
3]. Normally, Aβ is degraded by proteasomes and Aβ-degrading enzymes (ADE) in order to maintain equilibrium between Aβ generation and clearance. However, in the pathological cases of AD, the level of APP expression is higher in the entorhinal cortex neurons of AD patients than in normal individuals [
3]. Furthermore, the substrate affinity of β- and γ-secretase with APP is increased, while the level of Aβ degradation is decreased, which leads to Aβ dyshomeostasis and the development of AD pathology [
3]. Consequently, the adequate reduction of Aβ is considered to be the pivotal therapeutic objective of AD.
The strategies targeting the reduction of Aβ mainly include: the inhibition of amyloidogenic pathway, the promotion of non-amyloidogenic pathway, the promotion of Aβ clearance and the reduction of APP production [
4]. In recent decades, the majority of pharmaceutical research into anti-amyloid therapy has focused on the development of secretase inhibitors and enhancers, as well as Aβ clearance agents, including BACE1 inhibitor elenbecestat, α-secretase enzyme enhancers APH1105, Aβ aggregation inhibitor PBT1 and Aβ monoclonal antibody lecanemab [
5]. Lecanemab is the second FDA-approved immunotherapies for AD, this represents a significant advance in the ongoing effort to develop effective treatments for AD. Apart from Aβ monoclonal antibody, the autophagy is one of the important pathways involved in cellular response for the removal of protein aggregates, including Aβ [6, 7]. A substantial body of evidence indicates that autophagy enhancers protect against cognitive decline and inhibit Aβ aggregates in AD mouse models, such as rapamycin, lithium, carbamazepine and latrepirdine [
6]. Nevertheless, the efficacy of autophagy stimulators for the treatment of AD patients requires further investigation through comprehensive clinical trials [6, 8].Therefore, it is important for researchers to explore additional strategies to combat Aβ.
In recent years, some researchers have attempted to identify a solution by inhibiting Aβ production from the perspective of APP gene expression levels [
9]. It has been demonstrated that the number of copies of the APP gene, the level of APP mRNA and the level of APP protein in single neuronal cells of sporadic AD are increased [10, 11]. The process of APP gene transcription to APP mRNA was complicated, involving transcriptional and post-transcriptional regulation. Some of the APP translational modulators include 4-(5-methyl-1H-benzimidazol-2-yl) aniline (JTR-009), 2-[(pyridine-2-ylmethyl)-amino]-phenol (2-PMAP), and posiphen, which have been developed for the treatment of AD [
12]. Posiphen, an inhibitor of the transcription of APP mRNA by targeting the iron-response element (IRE), has been demonstrated to reduce APP mRNA at the transcriptional level, having completed the phase III clinical trials with mild to moderate AD [
13]. Although the clinical data for posiphen have not yet been published, the inhibition of APP mRNA represents a promising avenue for the treatment of AD [
4]. Recent advances in molecular biology have revealed that several microRNAs (miRNAs), mall non-coding RNAs that regulate gene expression post-transcriptionally by binding mRNA targets and inhibiting translation or mRNA degradation [
14], are identified to regulate the expression of the APP gene, which is thought to be a causal factor in Aβ formation [
9]. The miR-106a, miR-135a, miR-153 and miR-147 have been demonstrated to bind directly to the 3´-UTR of APP mRNA, which has been shown to downregulate APP expression at the post-transcriptional level. Conversely, miR-346 has been demonstrated to target the APP mRNA 5´-UTR, promoting APP translation and Aβ production [
15]. Nevertheless, growing numbers of miRNAs have been investigated for their potential role as the inhibitors of mRNA expression related to Aβ clearance pathways. While there are some obstacles to overcome for clinical application, the potential of miRNAs as therapeutic agents for AD is an area of active research [16, 17]. In light of these considerations, it seems unlikely that a single pathway will prove effective in inhibiting Aβ generation or deposition. A promising strategy for reducing Aβ plaque generation may therefore be to combine multiple pathways, such as inhibition of amyloidogenic secretases, promotion of Aβ clearance, and inhibition of APP production.
Tetramethylpyrazine nitrone
TBN (2-[[(1,1-dimethylethyl)oxidoimino]-methyl]-3,5,6-trimethylpyrazine) is a novel tetramethylpyrazine derivative armed with a potent free radical scavenging nitrone moiety[
18]. The therapeutic effects of TBN have been demonstrated in various animal models, including those of ischemic stroke, Parkinson’s disease, amyotrophic lateral sclerosis and Alzheimer’s disease[18-21]. Phase 2 clinical trials of TBN for treatment of ischemic stroke, diabetic kidney disease and ALS have been completed and have demonstrated promising results (CTR20190094, CTR20202126, CTR20210206, ChiCTR1900022848, ChiCTR2000039689 and ChiCTR2100043019). The results of the previous study in the 3 × Tg-AD mouse model showed that TBN markedly improved cognitive function by reduction in Aβ levels and plaque deposition, tau hyperphosphorylation, and the restoration of synaptic function, which was likely associated with the inhibition of APP, BACE1, and PS1 protein expression [
18]. Furthermore, TBN significantly inhibited the amyloidogenic processing pathway by inhibiting APP, BACE1 and PS1 expression and promoted the non-amyloidogenic processing pathway by increasing ADAM10 expression in the N2a/APP695swe cells [
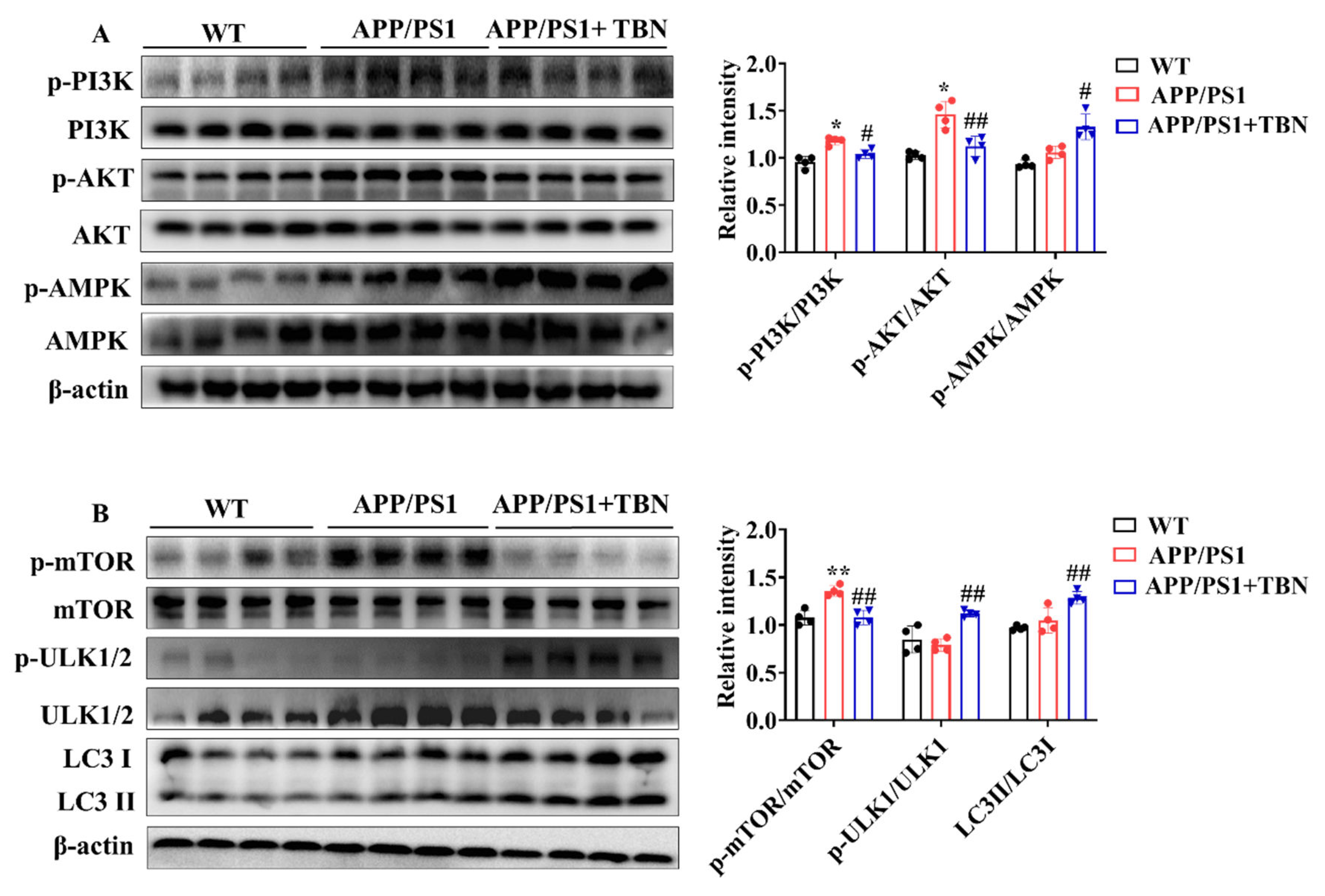
18]. Additionally, the proteomic analysis of hippocampal neurons showed that TBN modulated the MAPK and mTOR pathways, both of which are involved in the regulation of autophagy. In order to provide further evidence for the efficacy of TBN for treatment of AD, we conducted further evaluations of the anti-AD effects and the potential mechanisms of action in Aβ reduction of TBN in APP/PS1 mice
in vivo and N2a/APP695swe cells
in vitro.
3. Discussion
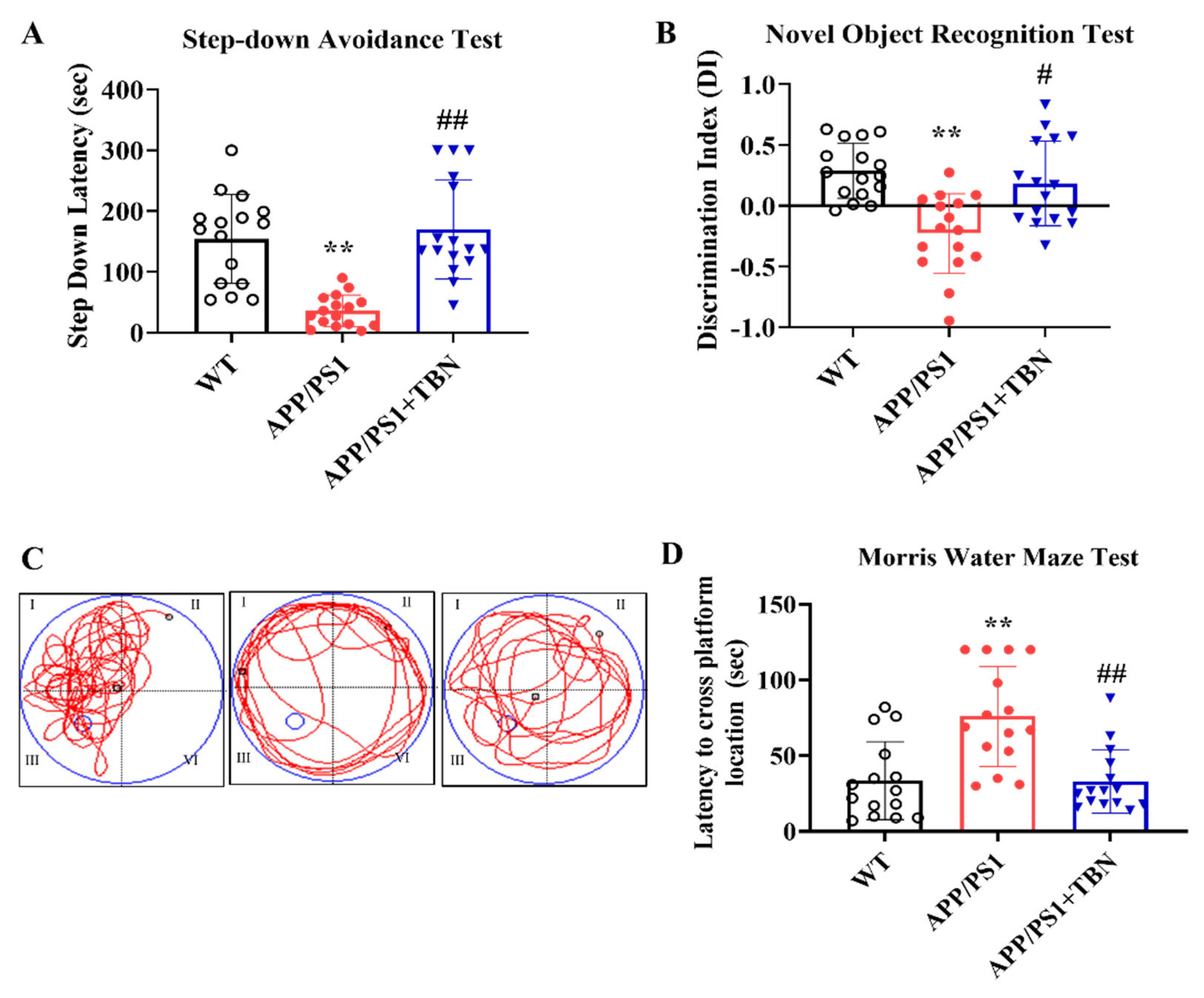
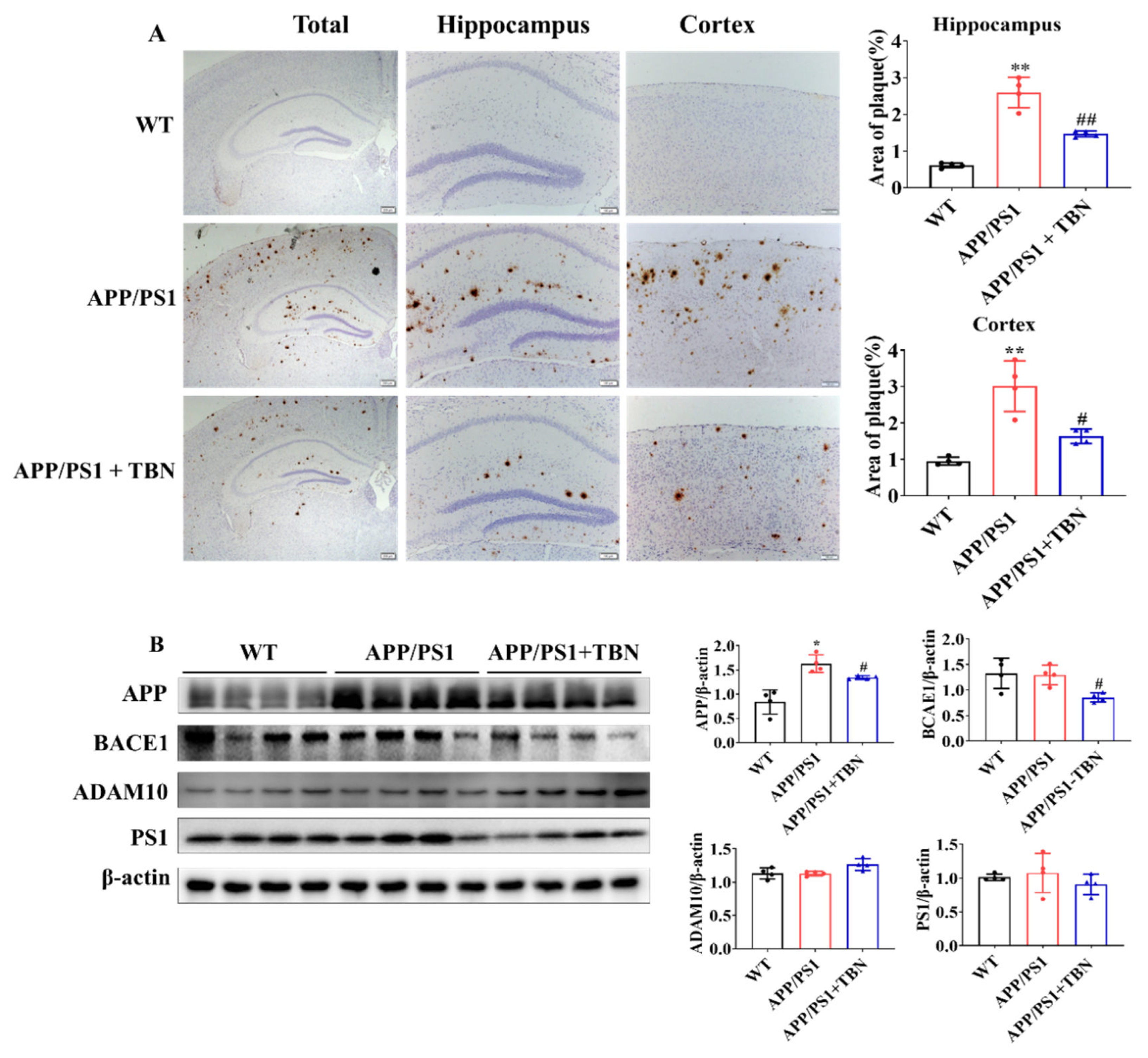
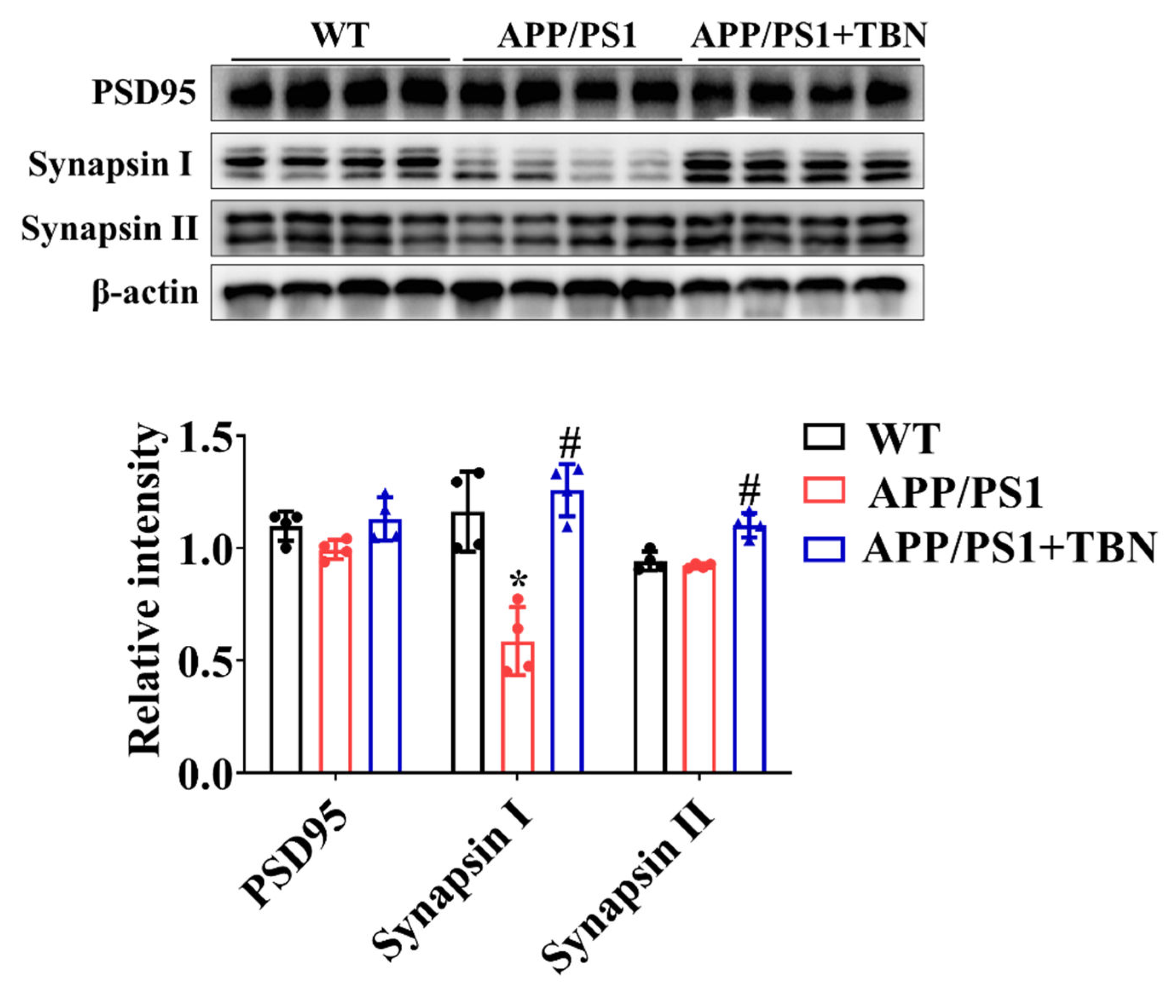
In our previous study, we have demonstrated that TBN significantly reduced Aβ production and deposition in 3×Tg-AD mice [
18]. In the present study, we aimed to further evaluate the therapeutic effects of TBN in the APP/PS1 mice model. Our findings demonstrated that TBN also significantly reduced Aβ production and deposition in APP/PS1 mice. The mechanism by which TBN reduces Aβ levels is likely to be through the inhibition of APP expression via the modulation of APP gene transcriptional factors and miRNAs, the inhibition of BACE 1 expression, and the promotion of autophagy activities.
APP is a type I single-pass transmembrane protein that is the direct source of Aβ generation. As Aβ production can be effectively suppressed by lowering the steady state level of its precursor protein, there has been growing evidence that targeting APP mRNA with a small molecule compound could be a way to treat AD[
12]. The regulation of APP gene expression is a complex process involving a number of different factors. These include the gene promoter, which contains a high GC region with five GGGCGC boxes, as well as transcription factors such as SP-1, AP-1, CTCF, TGF-β, HSF-1 and NF-κB, growth factors such as nerve growth factor, cytokines such as interleukin-1 and post-transcriptional regulators such as miRNA. SP-1, AP-1, CTCF, TGF-β, HSF-1 and NF-κB facilitate the transcription in promotor of APP gene [
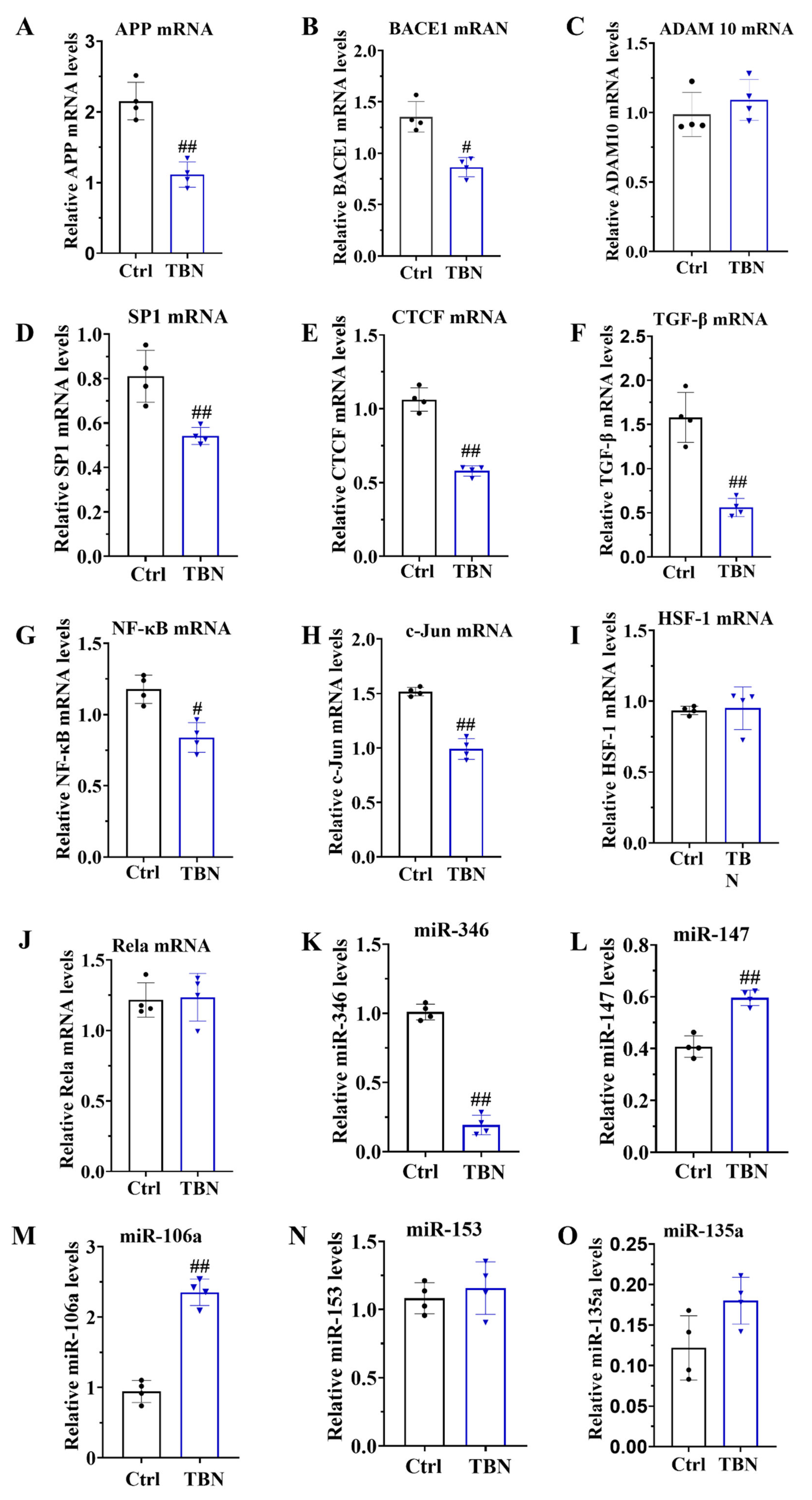
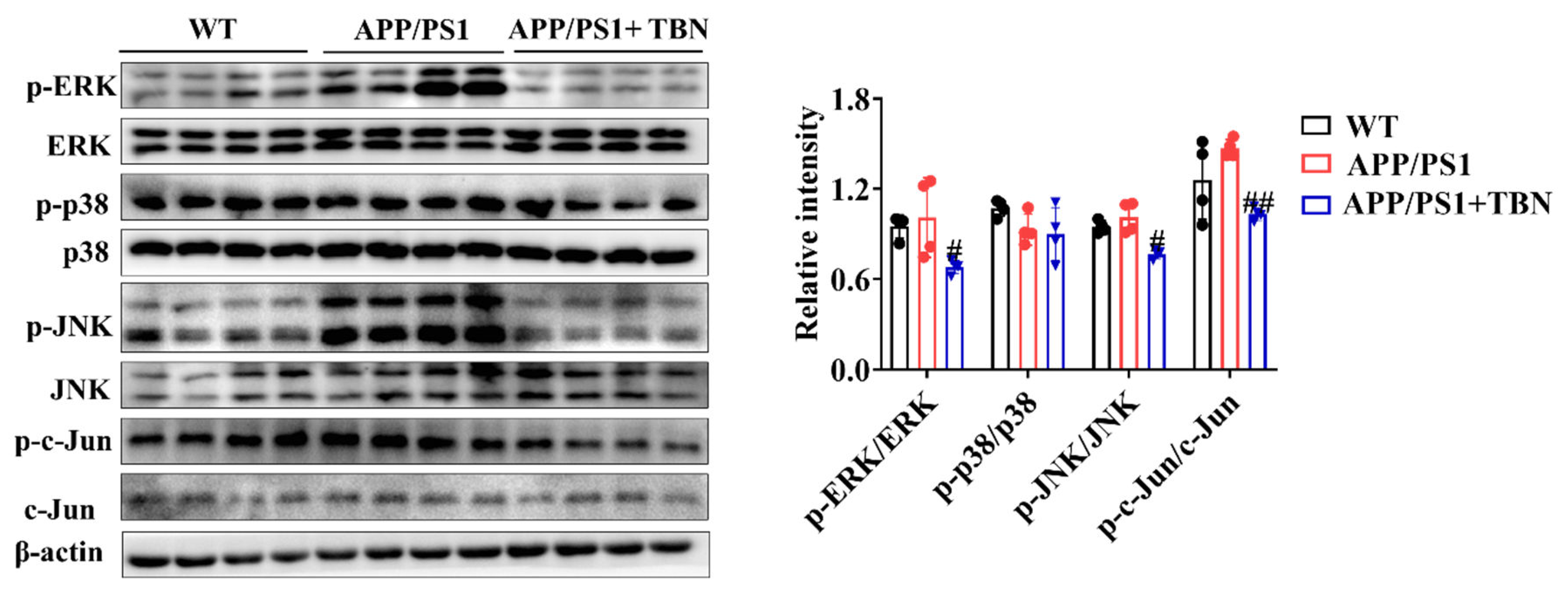
9]. Our studies have demonstrated that TBN significantly decreases the levels of SP-1 mRNA, c-Jun mRNA, TGF-β mRNA and NF-κB mRNA in N2a/APP695swe cells. This suggests that TBN reduces APP mRNA by modulating the levels of related transcription factors. Of note, TBN also decreases p-c-Jun expression in the hippocampus of APP/PS1 mice. C-JUN is the subunit of AP-1. AP-1 is a dimeric protein composed of c-Fos, c-Jun, and related proteins, which effectively promote APP gene transcription to mRNA. This process is stimulated by phosphorylation of MAPKs, which are known to regulate key cellular processes such as gene expression, proliferation, apoptosis, and inflammation, which are involved in the pathophysiology and pathogenesis of AD [
22]. Three main distinct subgroups of MAPKs have been identified in mammalian cells, including extracellular-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38. These three pathways are activated in vulnerable neurons in patients with AD [22, 23]. ERK regulates the expression of c-Fos, JNK tightly regulates the levels of c-Jun, and p38 modulates the activity of p53 and ATF2 [
24]. A substantial body of research has demonstrated that inhibition of ERK, p38 or JNK restores spatial memory and short-term and long-term memory, and reduces the amount of Aβ deposits [22, 25-27]. Furthermore, MAPKs not only regulate APP mRNA transcription, but also regulate tau phosphorylation [
22]. These viewpoints are consistent with the results of our study, which can explain the mechanism of TBN on APP mRNA reduction. It can be postulated that TBN inhibits the phosphorylation levels of JNK and ERK, thereby reducing the level of p-c-jun, which in turn leads to a reduction in AP-1, and finally to a reduction in APP mRNA. Furthermore, our previous study indicated that TBN can reduce tau hyperphosphorylation in 3×Tg-AD mice. This may be related to the inhibition of the MAPKs signaling pathway by TBN.
Another significant finding is that TBN can reduce the level of miR-346, and increase the levels of miR-147 and miR-106a in N2a/APP695swe cells. miRNAs are small, non-coding RNA molecules that play a crucial role in regulating gene expression or mRNA degradation at the post-transcriptional level. They influence various processes associated with AD, including Aβ aggregation, tau pathology, mitochondrial dysfunction, neuroinflammation and synaptic dysfunction [
28]. Recently, miRNAs have emerged as promising, cost-effective and non-invasive biomarkers for AD [
29]. Several miRNAs have been identified as regulators of Aβ metabolism by targeting the expression of APP and the secretases involved in its processing. For example, miR-106a, miR-135, miR-147, miR-101, miR-16 and miR-520c bind to their predicted target sequences in the APP 3´-UTR and negatively regulate reporter gene expression. Over-expression of these miRNAs results in translational repression of APP mRNA and significantly reduces APP protein levels [
14]. Liang et al. have demonstrated that miR-153 suppresses the expression of APP by specifically target site within the APP 3´-UTR [
30]. In contrast, miR-346 targets the APP mRNA 5´-UTR to upregulate APP translation and Aβ production [
31]. miRNAs can also affect AD pathology in other ways. It has been demonstrated that the expression of the BACE 1 can be increased by miR-29a/b-1, miR-107, miR-298, miR-124, miR-135b, miR-188 and miR-338 [
29]. Both miR-34a and miR-26b have been demonstrated to inhibit tau expression and affect NFTs formation [
32]. Furthermore, miR-499 and miR-30 have been implicated in the regulation of mitochondrial dynamics, targeting proteins that influence both fission and fusion processes [
28]. Additionally, miR-26b, miR-132, and miR-206 have been shown to target neurotrophic factors to regulate synaptic function [
32]. Moreover, recent studies have demonstrated that miRNAs modulate autophagic activity. For instance, the gene of mTOR was regulated by several miRNAs, including miR-100, miR-96, miR-338-3p, miR-7 and miR-128. Additionally, ULK 1 expression can be suppressed by miR-290/295 [
33]. Our finding also indicated that TBN significantly reduced the BACE 1 mRNA levels, and activated autophagy by decreasing mTOR and increasing ULK expression. These effects may be related to the regulation of miRNAs by TBN, which requires further investigation.
In conclusion, this study represents a preliminary investigation into the potential mechanism of TBN in reducing APP levels. It has been demonstrated that TBN exerts a novel regulatory effect on miRNAs. However, there is still a significant amount of work to be done before these findings can be validated. These includes the verification of the impact of TBN on miRNAs in the hippocampus of APP/PS1 mice, as well as the investigation of whether TBN affects other miRNAs, such as BACE 1, autophagy and synaptic function. Although two antibody-based drugs, aducanumab and lecanemab, have been approved by the FDA, there is still a need for safe and effective pharmacological treatments capable of stopping or at least delaying the course of AD. TBN treatment has been shown to reverse the learning and memory deficits in AD mice, and therefore TBN is a promising drug candidate for AD treatment.
4. Materials and Methods
4.1. Chemicals and Reagents
TBN was provided by Guangzhou Magpie Pharmaceuticals CO., LTD (Guangzhou, China). DMEM, FBS, G418, and Penicillin-Streptomycin solution (100 ×) were purchased from GibcoTM. RIPA buffer and protease/phosphatase inhibitor cocktail were purchased from ThermoFisher Scientific. Antibody APP, BACE1, PS1, ADAM10, synapsin I, synapsin II, PSD 95 and Goat anti-mouse IgG H + L (Alexa Fluor® 488) were purchased from Abcam. Antibody D3D2N, p-PI3K, PI3K, p-AKT, AKT, p-AMPK, AMPK, p-mTOR, mTOR, p-ULK1/2, ULK1/2, LC3, p-ERK, ERK, p-p38, p38, p-JNK, JNK, p-c-Jun, c-Jun, β-actin, anti-rabbit IgG, HRP-linked antibody and anti-mouse IgG antibody were bought from Cell Signaling Technology. Pure Nitrocellulose Blotting Membrane (66485) was obtained from PALL Corporation. TRleasyTM LS Total RNA Extraction Reagent (19201ES60), Hieff qPCR SYBR Green Master Mix (no ROX) (11201ES08) and Hifair III 1st Strand cDNA Synthesis SuperMix for qPCR (11141ES10) were purchased from YEASEN Biotechnology. Step-down avoidance (SDA), novel object recognition (NOR) and mirror water maze (MWM) devices and software were bought from Huaibei Zhenghua Biological instrument equipment Co., LTD.
4.2. Cell Culture
N2a/APP695swe cells were kindly donated by Professor Xifei Yang’ lab (Key Laboratory of Modern Toxicology of Shenzhen, Shenzhen Center for Disease Control and Prevention, Shenzhen, China). N2a/APP695swe cells were cultured in DMDM with 10% FBS, penicillin-streptomycin (1×), and with 200 μg/mL G418 at 37 ℃ with 95% air and 5% CO2 in a humidified incubator. The cells were inoculated in 25 cm2 culture flasks at a specified density for 24 hours, after which they were treated with 300 μM TBN. After a further 24 hours, the cells were collected for RT-PCR, which was measured according to the instructions of the kits.
4.3. Animal Care and Treatment
All experiments were approved by the Animal Ethics Committee of the Shenzhen Center for Disease Control and Prevention (Shenzhen CDC, China) in accordance with the requirements of the Guide for the Care and Use of Laboratory Animals. The APP/PS1 mice were purchased from the Jackson Laboratory and subsequently inbred in the laboratory animal central of the Shenzhen CDC. The mice were housed under controlled conditions, with a temperature range of 20 ℃~26℃, humidity of 40% ~ 70%, and 12-h light/12-h dark cycles. APP/PS1 mice are hemizygous mice expressing human APP and a mutant human PS1-dE9, and their genotype was confirmed by the polymerase chain reaction on a sample of the tail. The littermates of wild-type mice served as the negative control group (WT). Two-month-old APP/PS1 mice were randomly allocated into the vehicle group (APP/PS1) and TBN group (n=16, respectively). The mice in the TBN group were treated with TBN at a dose of 60 mg/kg via intragastric administration twice daily. WT and APP/PS1 group mice were received with parallel volume of saline. Following a six-month period of TBN or saline administration, all mice underwent a behavioural assessment, after which they were sacrificed via the injection of anaesthetics (Zoletil 50/xylazine).
4.3. Behavioral Tests
Behavioral tests commenced at eight months of age and continued for approximately four weeks, throughout which the treatment was maintained. The SDA test, NOR test and MWM test were performed in accordance with the methodology as previously described [18, 34, 35]. In brief, the SDA test was performed by placing the mouse in a separate compartment with a grid floor underneath and an insulated wooden platform. During the training period, the mouse was placed on the grid floor and the electrical shock was delivered for a period of 5 min. In the testing period, the mouse was placed on the wooden platform while the electricity was applied. The time taken for the mouse to touch the grid floor for the first time was recorded as the step-down latency, and the number of times the grid floor was touched was recorded as the error number. The NOR test was conducted on the fourth day following the SDA test. For the NOR test, the mouse was placed in an open field with two identical objects, and allowed to explore freely for 5 min once daily for 3 days during the training phase. On the fourth day, the mouse was placed in the open field with an old object was replaced by a new object, and its exploration trajectory was recorded by the video-tracking software. The discrimination index (DI), which represents the ability to recognize new objects, was calculated using the following equation: (Time exploring new object - Time exploring old object) / (Time exploring new object + Time exploring old object) × 100. Similarly, MWM was performed on the fourth day following the NOR test. The NOR test was carried out in a circular tank with a platform in the third quadrant and filled with opaque water. During the training phase, the mouse was trained to find the platform four times a day for 5 days. A probe trial was conducted on the sixth day following the training session, during which the platform was removed and the mice were placed in the tank to explore the platform site. The mouse’s swimming trajectory was recorded by a movement-tracking system (Super Maze+ software). The latency to cross platform location was defined as the time taken for the mouse to cross the platform site for the first time.
4.4. Immunohistochemistry
The Aβ plaques in the hippocampus and cerebral cortex were quantified using the D3D2N antibody by immunohistochemical staining, in accordance with the methodology as previously described [18, 34]. In brief, the brain tissues were subjected to a series of processes, including fixation in 4% paraformaldehyde, embedding in paraffin, sectioning, dewaxing with xylene, gradual rehydration with ethanol, antigen retrieval, peroxidase removal by 3% hydrogen peroxide, blocking with 10% FBS, primary antibody and secondary antibody incubation, diaminobenzidine colour development, and polyvinylpyrrolidone mounting. To obtain digital images of the sections, an Olympus BX41 microscope was employed.
4.5. Western Blotting
The western blotting procedure was conducted in accordance with the methodology as previously described in [18, 34]. Briefly, hippocampus tissues were homogenized in RIPA lysis buffer containing 1 mM PMSF, and then centrifuged at 12,000 rpm for 20 min at 4 ℃ to obtain the supernatant liquid. Subsequently, the protein concentration was determined, after which the proteins were subjected to sodium dodecyl sulphate-polyacrylamide gel electrophoresis (SDS-PAGE) using either 4% or 12% gels. Following electrophoresis, the proteins were transferred to a nitrocellulose (NC) blotting membrane. The NC membrane was then washed for 5 min with Tris-buffered saline with Tween 20 (TBST) and blocked with TBST buffer containing 5% non-fat dry milk for 1 hour at room temperature. The membrane was washed with TBST for 3 times and incubated with the primary antibody overnight at 4 ℃. Following the incubation with the primary antibody, the membrane was incubated with the secondary antibody for 1 hour at room temperature. Finally, the blot was scanned by a chemiluminescent imaging system (Tanon 5200 Multi), and the bands were quantified by densitometry using Image J.
4.6. qRT-PCR
The total RNA was extracted from N2a/APP695swe cells using the TRleasyTM LS Total RNA Extraction Reagent, in according to the manufacturer’s instructions. Quantitative PCR was conducted by Real-Time system (KUBO TECH, q225) using Hifair III 1st Strand cDNA Synthesis SuperMix for qPCR kit and Hieff qPCR SYBR Green Master Mix kit (no ROX) in accordance with the manufacturer’s instructions. The results of the qPCR were normalised using GAPDH for mRNA and U6 for miRNA. The primers used for qRT-PCR are listed below: APP: Forward 5´- CCAGAACTGGTGCAAGCG -3´, reverse 5´- TTTGGCGACGGTGTGCCA -3´. BACE1: forward 5´- TGTGGAGATGGTGGACAACC -3´, reverse 5´- GGACAGCTGCCTCTGGTAG -3´. ADAM 10: forward 5´- AGTAGAGGAAGGAGCCCGG -3´, reverse 5´- GCAATCACAGCTTCTCGTGT -3´. SP1: forward 5´-ATGCTGCTCAACTCTCCTCCATG-3´, reverse 5´-CCTTCTCCACCTGCTGTCTCATC-3´; CTCF: forward 5´- TTGAGGAAGAACAGCAGGAAGGAC-3´, reverse 5´- TGGCTTCGGAGGCTTCATATTACC -3´; TGF-β: forward 5´-GGGCATCGCTCATCTCCACAG-3´, reverse 5´-GCAACAGGTCAAGTCGTTCTTCAC -3´; NF-κB: forward 5´- ATGGGAAACCGTATGAGCCTGTG -3´, reverse 5´- AGTTGTAGCCTCGTGTCTTCTGTC -3´; c-Jun: forward 5′-GTTGCGGCCGCGAAACTT-3′, reverse 5′-CATTGCCCTCGAGCCCTG-3′; HSF-1: forward 5´- CCAAGGAGGTGCTGCCCAAG -3´, reverse 5′- ATGCTGGAACTCGGTGTCATCTC -3′; Rela: forward 5′- AGAGAAGCACAGATACCACCAAGAC -3′, reverse 5′- GGTCAGCCTCATAGTAGCCATCC -3′; GAPDH: forward 5´- TCCACTCACGGCAAATTCAAC -3´, reverse 5´- GTAGACTCCACGACATACTCAGC -3´; miR-346: forward 5´- ACACTCCAGCTGGGTGTCTGCCCGAGTGC -3´, forward 5´-CTCAACTGGTGTCGTGGA-3´; miR-147: forward 5´-ACACTCCAGCTGGGTGGAAACTTTCTGCA-3´, forward 5´-CTCAACTGGTGTCGTGGA -3´; miR-106a: forward 5´-ACACTCCAGCTGGGCAAAGTGCTAACAGT -3´, forward 5´-CTCAACTGGTGTCGTGGA-3´; miR-153: forward 5´-ACACTCCAGCTGGGTTGCATAGTCACAA -3´, forward 5´-CTCAACTGGTGTCGTGGA -3´; miR-135a: forward 5´-ACACTCCAGCTGGGTATAGGGATTGGAGCC-3´, forward 5´-CTCAACTGGTGTCGTGGA-3´.