Submitted:
24 June 2024
Posted:
26 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Questionnaire
2.3. Interview
2.4. Statistics
3. Results
3.1. Quantitative Data
3.2. Qualitative Data
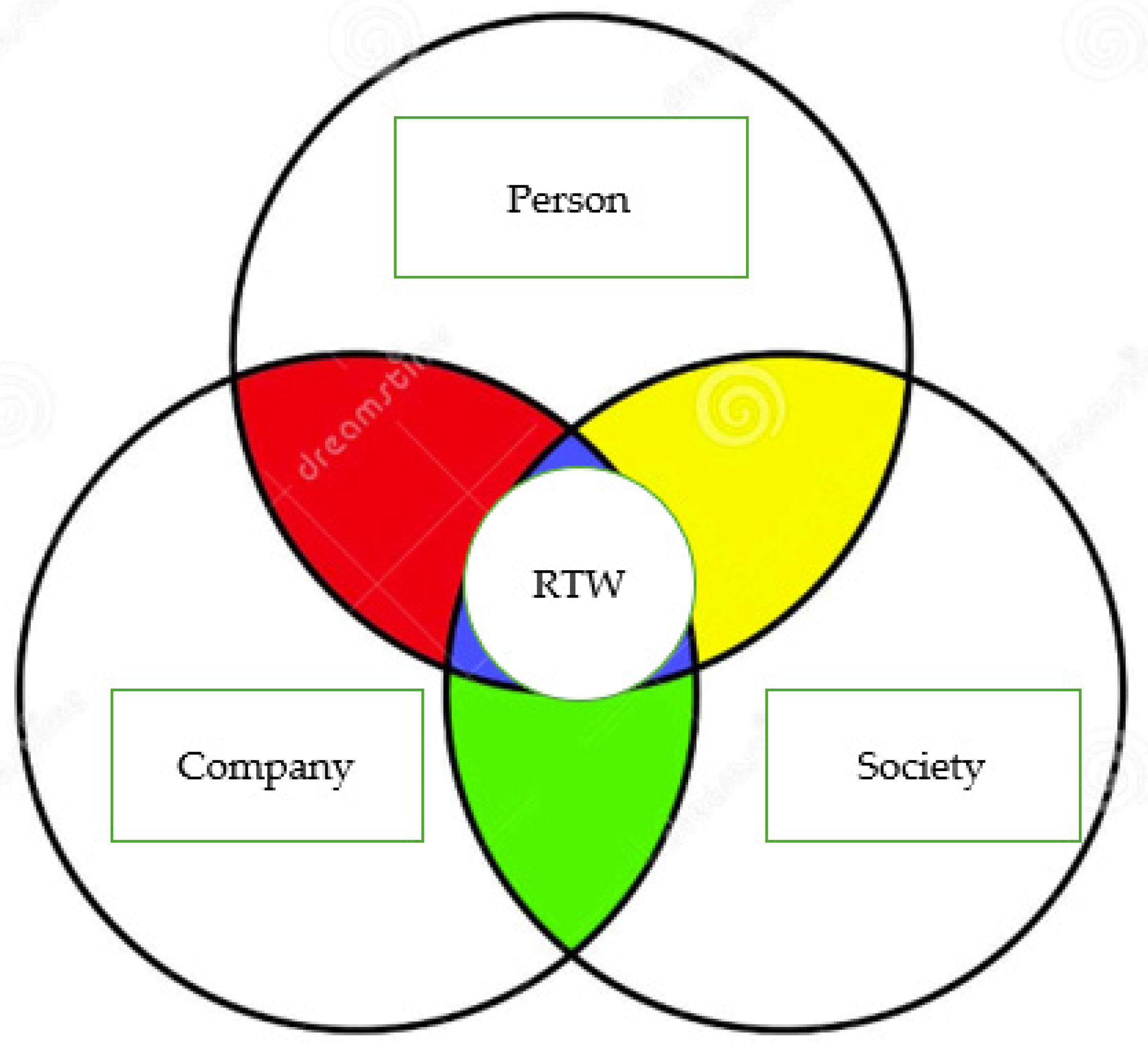
3.2.1. Person-Related Factors
“The lymphoedema and the pain in my hand have made it very difficult for me to move objects and put them up on shelves. I work with the constant fear that my fingers will get stuck, and tools will fall out of my hand.”
“I currently have a lot of difficulty doing normal, common daily activities; there are days when I feel a complete refusal to do anything.”
“I have severe depression, and serious sleep and memory problems. I am undergoing psychotherapeutic treatment,”
“I haven’t gone back to work because the very idea gives me an anxiety attack. I’m afraid I’m having a nervous breakdown.”
“The results of the treatment were excellent. I resumed work sooner than expected.”
“Work helped me a lot to recover my independence.”
3.2.2. Company-Related Factors
“My colleagues were very attentive when I returned to work also because we have known each other for many years, and the office workers are like a family for me.”
“My boss and colleagues were very friendly and helpful; I have not had, and currently do not have any problems at work.”
“When I returned to work, my colleagues welcomed me warmly because they understood and were interested in my difficulties.”
“Both my colleagues and my direct superior helped me with everything possible. “
“My colleagues supported me. They were very nice and were also interested in learning about the path I had followed.
“I had a bit of trouble. I was not allowed to return to my previous job and was given a lower-level task. In my absence, my colleagues had taken my place. After many years of service, I was no longer taken into consideration. Others did not accept my illness and its concomitant disabilities. There are colleagues who complain that there are too many sick employees in the same work environment. It’s demoralizing that they no longer allow you to do what you’ve done all your life because of an illness.”
“The scheduled shift is too tiring for me; at the end of the day, I am exhausted, and I don’t have enough time to rest between shifts. The excessive tiredness is frustrating because I would like to be able to start and finish a task independently; it is annoying to have to ask colleagues to do things for me. To have more time to rest, I asked to be able to alternate morning and afternoon shifts, but this was not possible. The director suggested I work in a different department, but that’s not what I want.”
“When I returned to the company, the human resources manager asked me why I had gone to the hospital to be examined by the occupational doctors, stating that the doctors defend themselves by requesting an excessive number of precautions, and therefore, if I had presented their indications, I would have been fired”.
“I was afraid of returning to work because I knew that a highly responsible job absorbs you completely, marginalizing everything else. I had to avoid it because otherwise the work would overwhelm me. When I returned, I was treated normally, as if I had nothing wrong with me.”
“I was allowed to do my work from home. However, because I didn’t go into the office for months, I felt a bit left out. Before I was diagnosed with breast cancer, I thought I would have a career, which has now ended. I am cut off from progress projects, initiatives, and training projects as well as trips and missions. They don’t take me into consideration. I’m not sure if I would have had a career without breast cancer, but the company didn’t help me prove my reliability!
“I had a somewhat traumatic return because I had on-going problems. When I got your letter, I turned to the corporate “ethics officer” who took charge of my situation,”
“The manager asks for a home visit to ascertain illness every time I take sickness leave to do my check-ups, even if I inform the company of the need to carry out a check-up on a certain day.”
“They placed me on the company toll-free number, I was practically demoted, but on the other hand I can’t do everything I did before at full speed.”
3.2.3. Society-Related Factors
“My mother now has cancer and I have to be close by to help her.”
“My real problems are family ones. My husband took my children away from me and hasn’t let me see them for 3 months”.
“I would like to go back to the office. I am the head of an operational structure of 50 people, so I have many responsibilities on my shoulders. I don’t know if anything will happen to my job when I return. If I had to drive to go to work in-person, it would take me an hour plus an indefinite amount of time looking for a parking space, all time I save by staying at home. Staying at home enables me to manage my family and my fatigue. Even if I work from home a lot and arrive exhausted at the end of the day, I can organize my breaks better. During my lunch break, I can rest for 20 minutes in a much more comfortable environment than in the office, where it wouldn’t be possible to just lie down on the sofa. “
“I am responsible for a complex structure. I have never really stopped working and now I’m teleworking. Unfortunately, my bosses want to see people in the workplace, “they have to see you”. I will try to defend my two days of teleworking because I have two young children and getting to work and looking for a parking space is a difficult and tiring undertaking.”
3.3. Occupational Health Consultancy
“I came to you for consultancy to obtain information regarding legal protection for BCSs. It helped me not only from a personal point of view but also from a corporate point of view because I showed the letter you sent me to my company doctor and, thanks to your advice, was able to telework. I must say that having someone to shield you in some way was a very positive experience since you feel that you are not alone.”
“Occupational health consultancy was very helpful since it persuaded my company to open up job opportunities that had previously not been available for me.”
“The consultancy helped me because I wanted to be aware of the benefits I could take advantage of and the dangers I had to guard against.”
“Your advice helped me a lot because it humanized the problem; the company still helped me by allowing me to stay at home. The company protected me; the work was important to distract me.”
“The occupational health consultancy that you offered me was very useful to me from a personal point of view because of the information it provided. I did not need to show your letter because the company doctor had adopted all the indications it contained.”
“The occupational health consultancy that you gave me was of great help from a personal point of view due to the indications I received; I felt that someone had listened to the symptoms that I never imagined I would have in my life. I can’t say the same from a business perspective as the company was deaf to my needs.”
“I took advantage of your consultancy because I was very angry but, in the end, I went no further. I didn’t let anyone read it because I couldn’t risk losing my job.”
“I didn’t use your occupational health advice because in my company the proposal to “restructure the work task” would have involved demotion, so I only brought it up when I decided to abandon my job to go on leave and then retire.”
“A lot is done in prevention and treatment, but in my chronic condition I feel rather isolated.”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021, 71, 209–249. [CrossRef]
- Giaquinto, A.N.; Sung, H.; Miller, K.D.; Kramer, J.L.; Newman, L.A.; Minihan, A.; Jemal, A.; Siegel, R.L. Breast Cancer Statistics. CA Cancer J Clin 2022, 72(6), 524-541. [CrossRef]
- Ferrier, C.; Thebaut, C.; Levy, P.; Baffert, S.; Asselain, B.; Rouzier, R.; Hequet, D. Absenteeism and indirect costs during the year following the diagnosis of an operable breast cancer: A prospective multicentric cohort study. J Gynecol Obstet Hum Reprod 2021, 50(6), 101871. [CrossRef]
- Chiu, K.; MacEwan, J.P.; May, S.G.; Bognar, K.; Peneva, D.; Zhao, L.M.; Yong, C.; Amin, S.; Bolinder, B.; Batt, K.; Baumgardner, J.R. Estimating Productivity Loss from Breast and Non-Small-Cell Lung Cancer among Working-Age Patients and Unpaid Caregivers: A Survey Study Using the Multiplier Method. MDM Policy Pract 2022, 7(2), 23814683221113846. [CrossRef]
- Su, T.T.; Azzani, M.; Tan, F.L.; Loh, S.Y. Breast cancer survivors: Return to work and wage loss in selected hospitals in Malaysia. Support Care Cancer 2018, 26(5), 1617-1624. [CrossRef]
- Ruiz de Azua, G.; Kousignian, I.; Vaz-Luis, I.; Di Meglio, A.; Caumette, E.; Havas, J.; Martin, E.; Martin, A.L.; Querel, O.; Vanlemmens, L.; Pistilli, B.; Coutant, C.; Cottu, P.H.; Merimeche, A.D.; Lerebours, F.; Tredan, O.; Jouannaud, C.; Levy, C.; Dumas, A.; Menvielle, G. Sustainable return to work among breast cancer survivors. Cancer Med 2023, 12(18), 19091-19101. [CrossRef]
- Trapani, D.; Ginsburg, O.; Fadelu, T.; Lin, N.U.; Hassett, M.; Ilbawi, A.M.; Anderson, B.O.; Curigliano, G. Global Challenges and Policy Solutions in Breast Cancer Control. Cancer Treat Rev 2022, 104, 102339. [CrossRef]
- Park, J.H.; Lee, S.K.; Lee, J.E.; Kim, S.W.; Nam, S.J.; Kim, J.-Y.; Ahn, J.-S.; Park, W.; Yu, J.; Park, Y.H. Breast Cancer Epidemiology of the Working-Age Female Population Reveals Significant Implications for the South Korean Economy. J Breast Cancer 2018, 21, 91–95. [CrossRef]
- Yang, Z.Y.; Chen, W.L.; Wu, W.T.; Lai, C.H.; Ho, C.L.; Wang, C.C. Return to Work and Mortality in Breast Cancer Survivors: A 11-Year Longitudinal Study. Int J Environ Res Public Health 2022, 19(21), 14418. [CrossRef]
- Emerson, M.A.; Reeve, B.B.; Gilkey, M.B.; Elmore, S.N.C.; Hayes, S.; Bradley, C.J.; Troester, M.A. Job loss, return to work, and multidimensional well-being after breast cancer treatment in working-age Black and White women. J Cancer Surviv 2023, 17(3), 805-814. [CrossRef]
- Ng, D.W.L.; So, S.C.Y.; Fielding, R.; Mehnert-Theuerkauf, A.; Kwong, A.; Suen, D.; Wong, L.; Fung, S.W.W.; Chun, O.K.; Fong, D.Y.T.; Chan, S.; Molasiotis, A.; So, W.K.W.; Lam, W.W.T. Return to work, work productivity loss and activity impairment in Chinese breast cancer survivors 12-month post-surgery: A longitudinal study. Front Public Health 2024, 12, 1340920. [CrossRef]
- Ke, Y.; Tan, Y.Y.; Neo, P.S.H.; Yang, G.M.; Loh, K.W.; Ho, S.; Tan, Y.P.; Ramalingam, M.B.; Quah, D.S.C.; Chew, L.; Si, P.E.H.; Tay, B.C.; Chan, A. Implementing an Inclusive, Multidisciplinary Supportive Care Model to Provide Integrated Care to Breast and Gynaecological Cancer Survivors: A Case Study at an Asian Ambulatory Cancer Centre. Int J Integr Care 2023, 23(1), 14. [CrossRef]
- Paolucci, T.; Bernetti, A.; Bai, A.V.; Segatori, L.; Monti, M.; Maggi, G.; Ippolitoni, G.; Tinelli, L.; Santilli, V.; Paoloni, M.; Agostini, F.; Mangone, M. The sequelae of mastectomy and quadrantectomy with respect to the reaching movement in breast cancer survivors: Evidence for an integrated rehabilitation protocol during oncological care. Support Care Cancer 2021, 29(2), 899-908. [CrossRef]
- Vayr, F.; Montastruc, M.; Savall, F.; Despas, F.; Judic, E.; Basso, M.; Dunet, C.; Dalenc, F.; Laurent, G.; Soulat, J.M.; Herin, F. Work adjustments and employment among breast cancer survivors: A French prospective study. Support Care Cancer 2020 28(1), 185-192. [CrossRef]
- Franco, G. Occupation and breast cancer: Fitness for work is an aspect that needs to be addressed. Med Lav 2013, 104(2), 87-92.
- Campagna, M.; Loscerbo, R.; Pilia, I.; Meloni, F. Return to Work of Breast Cancer Survivors: Perspectives and Challenges for Occupational Physicians. Cancers (Basel) 2020, 12(2), 355. [CrossRef]
- Magnavita, N.; Di Prinzio, R.R.; Meraglia, I.; Vacca, M.E.; Arnesano, G.; Merella, M.; Mauro, I.; Iuliano, A.; Terribile, D.A. Supporting Return to Work after Breast Cancer: A Mixed Method Study. Healthcare (Basel) 2023, 11(16), 2343. [CrossRef]
- Converso, D.; Sottimano, I.; Garzaro, G.; Guidetti, G.; Pira, E.; Viotti, S. Contribution to validation of the Italian version of work ability personal radar. Med Lav 2022, 113(6), e2022051. [CrossRef]
- Tuomi, K.; Ilmarinen, J.; Jahkola, A.; Katajarinne, L.; Tulkki, A. Work Ability Index, 2nd revised edn.; Helsinki: Finnish Institute of Occupational Health, 1998.
- El Fassi, M.; Bocquet, V.; Majery, N.; Lair, M.L.; Couffignal, S.; Mairiaux, P. Work ability assessment in a worker population: Comparison and determinants of Work Ability Index and Work Ability score. BMC Public Health 2013, 13, 305. [CrossRef]
- Magnavita, N.; Meraglia, I.; Viti, G., Borghese, L. The Work Ability Index (WAI) in the Healthcare Sector: A Cross-Sectional/Retrospective Assessment of the Questionnaire. Int J Environ Res Public Health 2024, 21(3), 349. [CrossRef]
- Gould, R.; Ilmarinen, J.; Järvisalo, J. Dimensions of Work Ability. Results from the Health 2000 Survey; Finnish Centre for Pensions: Helsinki, Finland, 2008; pp. 25–34.
- Elovainio, M.; Heponiemi, T.; Sinervo, T.; Magnavita, N. Organizational justice and health; review of evidence. G Ital Med Lav Ergon 2010, 32(3), B5-B9.
- Magnavita, N.; Bergamaschi, A. Justice at the workplace. Validation of the Italian version of Colquitt’s justice measurement questionnaire (JM20). Lo studio della giustizia sul lavoro. Validazione della versione italiana del JM20 di Colquitt. G Ital Med Lav Ergon 2008, 30(3), 2 Suppl: 449-450.
- Colquitt, J.A. On the dimensionality of organizational justice: A construct validation of a measure. J Appl Psychol 2001, 86, 386–400.
- Curcio, G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurol Sci 2013, 34(4), 511-9. [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index (PSQI): A new instrument for psychiatric research and practice. Psychiatry Res 1989, 28(2), 193-213.
- Grandner, M.A.; Kripke, D.F.; Yoon, I.Y.; Youngstedt, S.D. Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non-clinical sample. Sleep Biol Rhythms 2006, 4(2), 129-139. [CrossRef]
- Michielsen, H.J.; De Vries, J.; Van Heck, G.L. Psychometric qualities of a brief self-rated fatigue measure: The Fatigue Assessment Scale. J Psychosom Res 2003, 54(4), 345-52.
- Cumming, T.B.; Mead, G. Classifying post-stroke fatigue: Optimal cut-off on the Fatigue Assessment Scale. J Psychosom Res 2017, 103, 147-149. [CrossRef]
- Magnavita, N. Ansia e depressione nei luoghi di lavoro. Il questionario A/D di Goldberg. Anxiety and depression at work. the A/D Goldberg Questionnaire. G Ital Med Lav Ergon 2007, 29(3), 670-671.
- Goldberg, D.; Bridges, K.; Duncan-Jones, P.; Grayson, D. Detecting anxiety and depression in general medical settings. BMJ 1988, 297(6653), 897-9.
- Abdel-Khalek, A.M. Measuring happiness with a single-item scale. Social Behavior and Personality: An international journal; Scientific Journal Publishers 2006; pp. 139-150. [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qualitative Research in Psychology 2006, 3, 77–101. [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated Criteria for Reporting Qualitative Research (COREQ): A 32-Item Checklist for Interviews and Focus Groups. Int J Qual Health Care 2007, 19, 349–357. [CrossRef]
- Petersen, K.S.; Hedeager Momsen, A.M.; Vinther-Nielsen, C. Return-to-work intervention while undergoing cancer treatment: Female cancer survivors’ experiences. Work 2023, 75(2), 495-506. [CrossRef]
- Sheppard, D.M.; O’Connor, M.; Jefford, M.; Lamb, G.; Frost, D.; Ellis, N.; Halkett, G.K.B. ‘Beyond Cancer’ Rehabilitation Program to Support Breast Cancer Survivors to Return to Health, Wellness and Work: Feasibility Study Outcomes. Curr Oncol 2023, 30(2), 2249-2270. [CrossRef]
- de Boer, A.G.; Tamminga, S.J.; Boschman, J.S.; Hoving, J.L. Non-medical interventions to enhance return to work for people with cancer. Cochrane Database Syst Rev 2024, 3(3), CD007569. [CrossRef]
- Tan, F.L.; Loh, S.Y.; Su, T.T.; Veloo, V.W.; Ng, L.L. Return to Work in Multi-Ethnic Breast Cancer Survivors--a Qualitative Inquiry. Asian Pac J Cancer Prev 2012, 13, 5791–5797. [CrossRef]
- Marinas-Sanz, R.; Iguacel, I.; Maqueda, J.; Mínguez, L.; Alquézar, P.; Andrés, R.; Pérez, E.; Sousa, R.; Moreno-Atahonero, E.; Solé, D.; et al. Facilitating Factors and Barriers in the Return to Work of Working Women Survivors of Breast Cancer: A Qualitative Study. Cancers (Basel) 2023, 15, 874. [CrossRef]
- Luo, S.-X.; Liu, J.-E.; Cheng, A.S.K.; Xiao, S.-Q.; Su, Y.-L.; Feuerstein, M. Breast Cancer Survivors Report Similar Concerns Related to Return to Work in Developed and Developing Nations. J Occup Rehabil 2019, 29, 42–51. [CrossRef]
- Zomkowski, K.; Cruz de Souza, B.; Moreira, G.M.; Volkmer, C.; Da Silva Honório, G.J.; Moraes Santos, G.; Flores Sperandio, F. Qualitative Study of Return to Work Following Breast Cancer Treatment. Occup Med (Lond) 2019, 69, 189–194. [CrossRef]
- Slaghmuylder, Y.; Lauwerier, E.; Pype, P. Survivors’ Perceptions Regarding the Follow-up of Pain Complaints after Breast Cancer Treatment: Distinct Coping Patterns. Front Psychol 2022, 13, 1063705. [CrossRef]
- Wang, K.; Yee, C.; Tam, S.; Drost, L.; Chan, S.; Zaki, P.; Rico, V.; Ariello, K.; Dasios, M.; Lam, H.; et al. Prevalence of Pain in Patients with Breast Cancer Post-Treatment: A Systematic Review. Breast 2018, 42, 113–127. [CrossRef]
- Giacalone, G.; Yamamoto, T. Supermicrosurgical Lymphaticovenous Anastomosis for a Patient with Breast Lymphedema Secondary to Breast Cancer Treatment. Microsurgery 2017, 37, 680–683. [CrossRef]
- Cho, Y.; Do, J.; Jung, S.; Kwon, O.; Jeon, J.Y. Effects of a Physical Therapy Program Combined with Manual Lymphatic Drainage on Shoulder Function, Quality of Life, Lymphedema Incidence, and Pain in Breast Cancer Patients with Axillary Web Syndrome Following Axillary Dissection. Support Care Cancer 2016, 24, 2047–2057. [CrossRef]
- Ezzo, J.; Manheimer, E.; McNeely, M.L.; Howell, D.M.; Weiss, R.; Johansson, K.I.; Bao, T.; Bily, L.; Tuppo, C.M.; Williams, A.F.; et al. Manual Lymphatic Drainage for Lymphedema Following Breast Cancer Treatment. Cochrane Database Syst Rev 2015, CD003475. [CrossRef]
- Algeo, N.; Bennett, K.; Connolly, D. Rehabilitation Interventions to Support Return to Work for Women with Breast Cancer: A Systematic Review and Meta-Analysis. BMC Cancer 2021, 21, 895. [CrossRef]
- Nissim, M.; Rottenberg, Y.; Karniel, N.; Ratzon, N.Z. Effects of aquatic exercise program versus on-land exercise program on cancer-related fatigue, neuropathy, activity and participation, quality of life, and return to work for cancer patients: Study protocol for a randomized controlled trial. BMC Complement Med Ther 2024, 24(1), 74. [CrossRef]
- Langer, D.; Tendler, S.; Bar-Haim Erez, A. A broad perspective on breast cancer: Participation, quality of life and return to work throughout the recovery process. Work 2023, 75(1), 325-337. [CrossRef]
- Sun, Y.; Shigaki, C.L.; Armer, J.M. Return to Work among Breast Cancer Survivors: A Literature Review. Support Care Cancer 2017, 25, 709–718. [CrossRef]
- Ruiz-Casado, A.; Álvarez-Bustos, A.; de Pedro, C.G.; Méndez-Otero, M.; Romero-Elías, M. Cancer-Related Fatigue in Breast Cancer Survivors: A Review. Clin Breast Cancer 2021, 21, 10–25. [CrossRef]
- Černíková, K.A.; Klůzová Kráčmarová, L.; Pešoutová, M.; Tavel, P. How Fatigue Affects Return to Work in Breast Cancer Patients. Klin Onkol 2022, 35, 290–296. [CrossRef]
- Rai, R.; Malik, M.; Valiyaveettil, D.; Ahmed, S.F.; Basalatullah, M. Assessment of late treatment-related symptoms using patient-reported outcomes and various factors affecting return to work in survivors of breast cancer. Ecancermedicalscience 2023, 17, 1533. [CrossRef]
- Tay, M.R.J.; Wong, C.J.; Aw, H.Z. Return to Work in Breast Cancer Patients following an Interdisciplinary Rehabilitation Program in a Community-Based Cancer Rehabilitation Center: A Pilot Study. Healthcare (Basel) 2024, 12(7), 805. [CrossRef]
- Servaes, P.; Gielissen, M.F.M.; Verhagen, S.; Bleijenberg, G. The Course of Severe Fatigue in Disease-Free Breast Cancer Patients: A Longitudinal Study. Psychooncology 2007, 16, 787–795. [CrossRef]
- Bower, J.E. Cancer-Related Fatigue--Mechanisms, Risk Factors, and Treatments. Nat Rev Clin Oncol 2014, 11, 597–609. [CrossRef]
- de Jong, N.; Courtens, A.M.; Abu-Saad, H.H.; Schouten, H.C. Fatigue in Patients with Breast Cancer Receiving Adjuvant Chemotherapy: A Review of the Literature. Cancer Nurs 2002, 25, 283–297; quiz 298–299. [CrossRef]
- Bower, J.E.; Ganz, P.A.; Desmond, K.A.; Rowland, J.H.; Meyerowitz, B.E.; Belin, T.R. Fatigue in Breast Cancer Survivors: Occurrence, Correlates, and Impact on Quality of Life. J Clin Oncol 2000, 18, 743–753. [CrossRef]
- Chartogne, M.; Rahmani, A.; Landry, S.; Bourgeois, H.; Peyrot, N.; Morel, B. Neuromuscular, Psychological, and Sleep Predictors of Cancer-Related Fatigue in Cancer Patients. Clin Breast Cancer 2021, 21, 425–432. [CrossRef]
- Fortner, B.V.; Stepanski, E.J.; Wang, S.C.; Kasprowicz, S.; Durrence, H.H. Sleep and Quality of Life in Breast Cancer Patients. J Pain Symptom Manage 2002, 24, 471–480. [CrossRef]
- Davidson, J.R.; MacLean, A.W.; Brundage, M.D.; Schulze, K. Sleep Disturbance in Cancer Patients. Soc Sci Med 2002, 54, 1309–1321. [CrossRef]
- Bean, H.R.; Diggens, J.; Ftanou, M.; Weihs, K.L.; Stanton, A.L.; Wiley, J.F. Insomnia and Fatigue Symptom Trajectories in Breast Cancer: A Longitudinal Cohort Study. Behav Sleep Med 2021, 19, 814–827. [CrossRef]
- Chang, W.-P.; Chang, Y.-P. Meta-Analysis of Changes in Sleep Quality of Women with Breast Cancer before and after Therapy. Breast Care (Basel) 2020, 15, 227–235. [CrossRef]
- Nakamura, Y.; Lipschitz, D.L.; Kuhn, R.; Kinney, A.Y.; Donaldson, G.W. Investigating Efficacy of Two Brief Mind-Body Intervention Programs for Managing Sleep Disturbance in Cancer Survivors: A Pilot Randomized Controlled Trial. J Cancer Surviv 2013, 7, 165–182. [CrossRef]
- Hwang, Y.; Conley, S.; Redeker, N.S.; Sanft, T.; Knobf, M.T. A Qualitative Study of Sleep in Young Breast Cancer Survivors: “No Longer Able to Sleep through the Night.” J Cancer Surviv 2023. [CrossRef]
- Gonzalez, B.D.; Grandner, M.A.; Caminiti, C.B.; Hui, S.-K.A. Cancer Survivors in the Workplace: Sleep Disturbance Mediates the Impact of Cancer on Healthcare Expenditures and Work Absenteeism. Support Care Cancer 2018, 26, 4049–4055. [CrossRef]
- Desai, K.; Mao, J.J.; Su, I.; Demichele, A.; Li, Q.; Xie, S.X.; Gehrman, P.R. Prevalence and Risk Factors for Insomnia among Breast Cancer Patients on Aromatase Inhibitors. Support Care Cancer 2013, 21, 43–51. [CrossRef]
- Van Onselen, C.; Aouizerat, B.E.; Dunn, L.B.; Paul, S.M.; West, C.; Hamolsky, D.; Lee, K.; Melisko, M.; Neuhaus, J.; Miaskowski, C. Differences in Sleep Disturbance, Fatigue and Energy Levels between Women with and without Breast Pain Prior to Breast Cancer Surgery. Breast 2013, 22, 273–276. [CrossRef]
- Costa, A.R.; Fontes, F.; Pereira, S.; Gonçalves, M.; Azevedo, A.; Lunet, N. Impact of Breast Cancer Treatments on Sleep Disturbances—A Systematic Review. Breast 2014, 23, 697–709. [CrossRef]
- Özer Güçlüel, Y.; Can, G. Evaluation of job stress and quality of life in individuals returning to work after cancer treatment. Eur J Oncol Nurs 2023, 66, 102381. [CrossRef]
- Hass, H.G.; Seywald, M.; Wöckel, A.; Muco, B.; Tanriverdi, M.; Stepien, J. Psychological distress in breast cancer patients during oncological inpatient rehabilitation: Incidence, triggering factors and correlation with treatment-induced side effects. Arch Gynecol Obstet 2023, 307(3), 919-925. [CrossRef]
- Hall, D.L.; Jimenez, R.B.; Perez, G.K.; Rabin, J.; Quain, K.; Yeh, G.Y.; Park, E.R.; Peppercorn, J.M. Fear of Cancer Recurrence: A Model Examination of Physical Symptoms, Emotional Distress, and Health Behavior Change. J Oncol Pract 2019, 15, e787–e797. [CrossRef]
- Walker, W.H.; Borniger, J.C. Molecular Mechanisms of Cancer-Induced Sleep Disruption. Int J Mol Sci 2019, 20, 2780. [CrossRef]
- Magnavita, N; Meraglia, I; Di Prinzio, R.R.; Terribile, D.A. Perceived justice in the workplace influences return to work after breast cancer. ICOH 2024 Congress, Marrakesh, Morocco (28/04/2024 to 03/05/2024).
- Mohan, A.; Huybrechts, I.; Michels, N. Psychosocial stress and cancer risk: A narrative review. Eur J Cancer Prev 2022, 31(6), 585-599. [CrossRef]
- Guseva Canu, I.; Bovio, N.; Arveux, P.; Bulliard, J.L.; Fournier, E.; Germann, S.; Konzelmann, I.; Maspoli, M.; Rapiti, E.; Grzebyk, M. Breast cancer and occupation: Non-parametric and parametric net survival analyses among Swiss women (1990-2014). Front Public Health 2023, 11, 1129708. [CrossRef]
- Yang, T.; Qiao, Y.; Xiang, S.; Li, W.; Gan, Y.; Chen, Y. Work stress and the risk of cancer: A meta-analysis of observational studies. Int J Cancer 2019, 144(10), 2390-2400. [CrossRef]
- Brintzenhofe-Szoc, K.M.; Levin, T.T.; Li, Y.; Kissane, D.W.; Zabora, J.R. Mixed Anxiety/Depression Symptoms in a Large Cancer Cohort: Prevalence by Cancer Type. Psychosomatics 2009, 50, 383–391. [CrossRef]
- Hequet, D.; Hamy, A.-S.; Girard, N.; Laas, E.; Coussy, F.; Rouzier, R.; Preau, M.; Delrieu, L.; Dumas, A.; Reyal, F. Variation over Time of the Factors Influencing Return to Work and Work Capacities after a Diagnosis of Breast Cancer: A Study on the Behalf of the Seintinelles Research Network. Support Care Cancer 2022, 30, 5991–5999. [CrossRef]
- Schmidt, M.E.; Scherer, S.; Wiskemann, J.; Steindorf, K. Return to Work after Breast Cancer: The Role of Treatment-Related Side Effects and Potential Impact on Quality of Life. European Journal of Cancer Care 2019, 28, e13051. [CrossRef]
- Hou, W.; Li, Q.; Liu, X.; Zeng, Y.; Cheng, A.S. Exploring the Employment Readiness and Return to Work Status of Breast Cancer Patients and Related Factors. Int J Nurs Sci 2021, 8, 426–431. [CrossRef]
- Rolland, A.-L.; Porro, B.; Kab, S.; Ribet, C.; Roquelaure, Y.; Bertin, M. Impact of Breast Cancer Care Pathways and Related Symptoms on the Return-to-Work Process: Results from a Population-Based French Cohort Study (CONSTANCES). Breast Cancer Res 2023, 25, 30. [CrossRef]
- Caumette, E.; Di Meglio, A.; Vaz-Luis, I.; Charles, C.; Havas, J.; de Azua, G.R.; Martin, E.; Vanlemmens, L.; Delaloge, S.; Everhard, S.; et. al. Change in the value of work after breast cancer: Evidence from a prospective cohort. J Cancer Surviv 2023, 17(3), 694-705. [CrossRef]
- Fu, A.Z.; Chen, L.; Sullivan, S.D.; Christiansen, N.P. Absenteeism and short-term disability associated with breast cancer. Breast Cancer Res Treat 2011, 130(1), 235-42. [CrossRef]
- Yin, W.; Horblyuk, R.; Perkins, J.J.; Sison, S.; Smith, G.; Snider, J.T.; Wu, Y.; Philipson, T.J. Association Between Breast Cancer Disease Progression and Workplace Productivity in the United States. J Occup Environ Med 2017, 59(2), 198-204. [CrossRef]
- Tachi, T.; Teramachi, H.; Tanaka, K.; Asano, S.; Osawa, T.; Kawashima, A.; Hori, A.; Yasuda, M.; Mizui, T.; Nakada, T.; Noguchi, Y.; Tsuchiya, T.; Goto, C. The impact of side effects from outpatient chemotherapy on presenteeism in breast cancer patients: A prospective analysis. Springerplus 2016, 5, 327. [CrossRef]
- Gonzalez, B.D.; Grandner, M.A.; Caminiti, C.B.; Hui, S.A. Cancer survivors in the workplace: Sleep disturbance mediates the impact of cancer on healthcare expenditures and work absenteeism. Support Care Cancer 2018, 26(12), 4049-4055. [CrossRef]
- Kim, S.Y.; Kissane, D.W.; Richardson, G.; Senior, J.; Morgan, J.; Gregory, P.; Birks, S.; Ooi, C.; Lipton, L.; Antill, Y.; Vereker, M.; Michael, N.; Bobevski, I. The role of depression and other psychological factors in work ability among breast cancer survivors in Australia. Psychooncology 2022, 31(2), 167-175. [CrossRef]
- Lindsay, S.; Fuentes, K.; Tomas, V.; Hsu, S. Ableism and Workplace Discrimination Among Youth and Young Adults with Disabilities: A Systematic Review. J Occup Rehabil 2023, 33(1), 20-36. [CrossRef]
- Derbyshire, D.W.; Jeanes, E.; Khedmati Morasae, E.; Reh, S.; Rogers, M. Employer-focused interventions targeting disability employment: A systematic review. Soc Sci Med 2024, 347, 116742. [CrossRef]
- Smith, D.L.; Atmatzidis, K.; Capogreco, M.; Lloyd-Randolfi, D.; Seman, V. Evidence-Based Interventions for Increasing Work Participation for Persons With Various Disabilities. OTJR (Thorofare N J) 2017, 37(2_suppl), 3S-13S. [CrossRef]
- Magnavita, N.; Meraglia, I. Poor work ability is associated with workplace violence in nurses. A longitudinal study. https://www.preprints.org/manuscript/202404.1864.
- Ekwueme, D.U.; Trogdon, J.G.; Khavjou, O.A.; Guy, G.P. Jr. Productivity Costs Associated With Breast Cancer Among Survivors Aged 18-44 Years. Am J Prev Med 2016, 50(2), 286-94. [CrossRef]
- Hastert, T.A.; Kirchhoff, A.C.; Banegas, M.P.; Morales, J.F.; Nair, M.; Beebe-Dimmer, J.L.; Pandolfi, S.S.; Baird, T.E.; Schwartz, A.G. Work changes and individual, cancer-related, and work-related predictors of decreased work participation among African American cancer survivors. Cancer Med 2020, 9(23), 9168-9177. [CrossRef]
- Su, T.T.; Azzani, M.; Tan, F.L.; Loh, S.Y. Breast cancer survivors: Return to work and wage loss in selected hospitals in Malaysia. Support Care Cancer 2018, 26(5), 1617-1624. [CrossRef]
- Khan, I.; Sawhney, R.; McClellan, S.; Chua, K.; Alfaraj, A.; Shevock, J.; Chun, D. Economic Impact of Cancer Diagnosis on Employment, Wages and Intent to Return to Work. Dela J Public Health 2023, 9(4), 54-56. [CrossRef]
- Zomkowski, K.; Bergmann, A.; Sacomori, C.; Dias, M.; Sperandio, F.F. Functionality and factors associated with work behaviour among Brazilian breast cancer survivors: A cross-sectional study. Work 2020, 67(4), 917-925. [CrossRef]
- AIRC Associazione Italiana Ricerca sul Cancro. Le statistiche del cancro. Available on: https://www.airc.it/cancro/informazioni-tumori/cose-il-cancro/numeri-del-cancro (accessed on 20 June 2024).
- Lungarella, R. Redditi delle donne, un gap di 7.700 euro. Il Sole 24 ore, 17 agosto 2022. Available at: https://www.ilsole24ore.com/art/redditi-donne-gap-7700-euro-AE8QQJsB (accessed on 20 June 2024).
- Giangrande N. Occupazione e salari delle donne in Italia. Un’analisi quantitativa. Fondazione Di Vittorio. Available on: https://www.fondazionedivittorio.it/sites/default/files/content-attachment/Occupazione%20e%20salari%20delle%20donne%20in%20Italia.%20Un%27analisi%20quantitativa.pdf (accessed on 20 June 2024).
- Rubion, E.; Bourdon, M.; Sébille, V.; Blanchin, M.; Bertin, M. Return to work and psychosocial trajectories after breast cancer: A longitudinal and sequential approach. Support Care Cancer 2024, 32(5), 307. [CrossRef]
- Bilodeau, K.; Gouin, M.M.; Fadhlaoui, A.; Porro, B. Supporting the return to work of breast cancer survivors: Perspectives from Canadian employer representatives. J Cancer Surviv 2023, 1, 9. [CrossRef]
- Söderman, M.; Friberg, E.; Alexanderson, K.; Wennman-Larsen, A. Women’s experiences of encounters with healthcare professionals’ regarding work after breast-cancer surgery and associations with sickness absence: A 2-year follow-up cohort study. Support Care Cancer 2019, 27(4), 1197-1206. [CrossRef]
- Månsson, T.; Lynøe, N.; Alexanderson, K.; Hinas, E.; Helgesson, G.; Friberg, E. Respectful encounters from healthcare professionals and return to work among 9032 long-term sick-listed due to cancer or due to other diagnoses: Results from a Swedish population-based survey. Support Care Cancer 2019, 27(9), 3555-3561. [CrossRef]
- King, R.; Stafford, L.; Butow, P.; Giunta, S; Laidsaar-Powell, R. Psychosocial experiences of breast cancer survivors: A meta-review. J Cancer Surviv 2024, 18(1), 84-123. [CrossRef]
- Heidkamp, P.; Hiltrop, K.; Breidenbach, C.; Kowalski, C.; Pfaff, H.; Geiser, F.; Ernstmann, N. Coping with breast cancer during medical and occupational rehabilitation: A qualitative study of strategies and contextual factors. BMC Womens Health 2024, 24(1), 183. [CrossRef]
| Age | Justice | Anxiety | Depression | PSQI | Fatigue | ||
| Age | Spearman’s rho | 1.000 | 0.063 | -0.072 | 0.062 | 0.095 | 0.342 |
| Sig. (2-tailed) | . | 0.736 | 0.695 | 0.735 | 0.605 | 0.060 | |
| Justice | Spearman’s rho | 0.063 | 1.000 | -0.549** | -0.605** | -0.445* | -0.287 |
| Sig. (2-tailed) | 0.736 | . | 0.001 | 0.000 | 0.012 | 0.118 | |
| Anxiety | Spearman’s rho | -0.072 | -0.549** | 1.000 | 0.583** | 0.723** | 0.420* |
| Sig. (2-tailed) | 0.695 | 0.001 | . | 0.000 | 0.000 | 0.019 | |
| Depression | Spearman’s rho | 0.062 | -0.605** | 0.583** | 1.000 | 0.595** | 0.579** |
| Sig. (2-tailed) | 0.735 | 0.000 | 0.000 | . | 0.000 | 0.001 | |
| PSQI | Spearman’s rho | 0.095 | -0.445* | 0.723** | 0.595** | 1.000 | 0.521** |
| Sig. (2-tailed) | 0.605 | 0.012 | 0.000 | 0.000 | . | 0.003 | |
| Fatigue | Spearman’s rho | 0.342 | -0.287 | 0.420* | 0.579** | 0.521** | 1.000 |
| Sig. (2-tailed) | 0.060 | 0.118 | 0.019 | 0.001 | 0.003 | . |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





