Submitted:
24 June 2024
Posted:
26 June 2024
You are already at the latest version
Abstract

Keywords:
Introduction
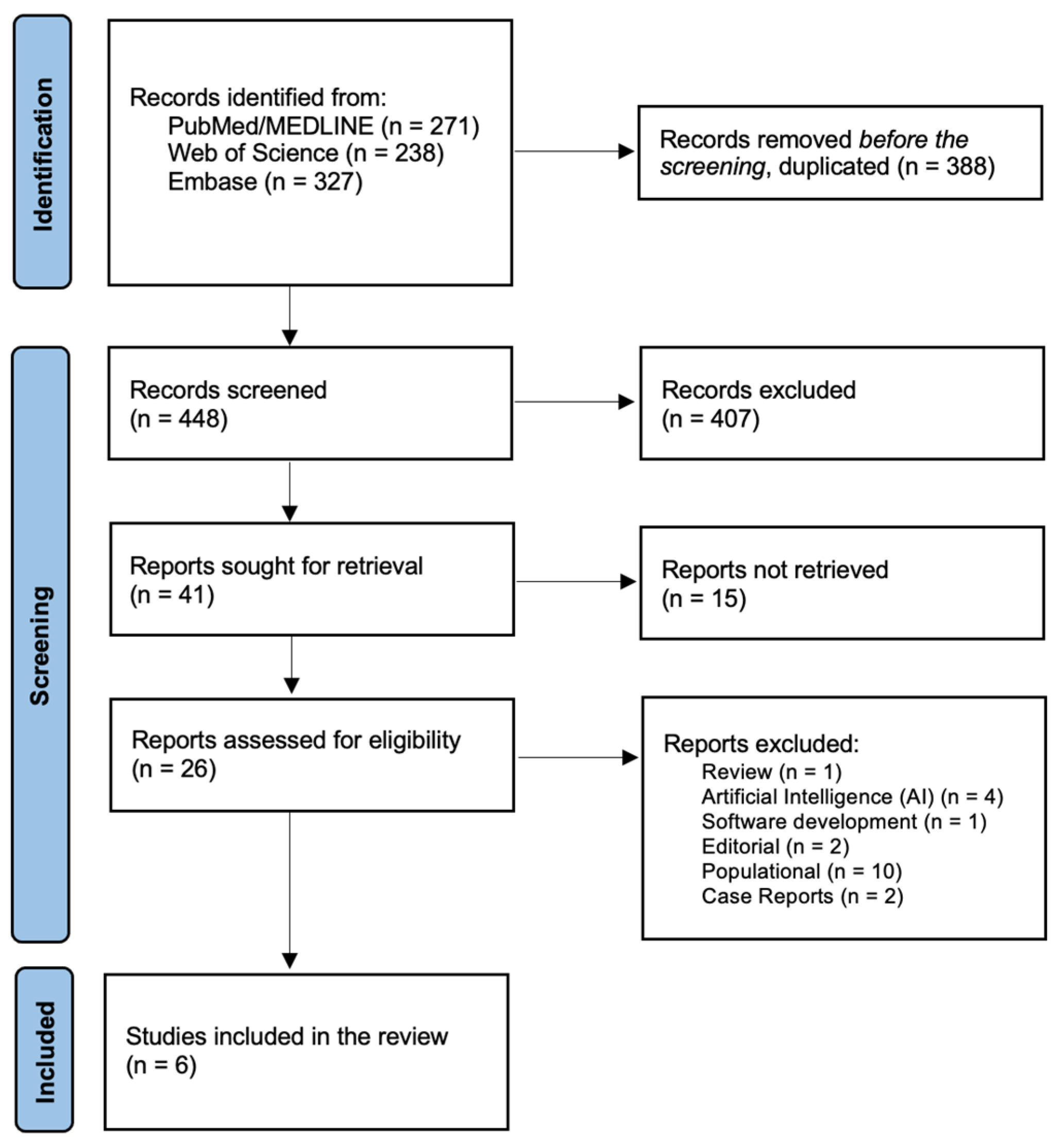
Materials and Methods
Eligibility Criteria
Study Selection
Data Retrieved
Results
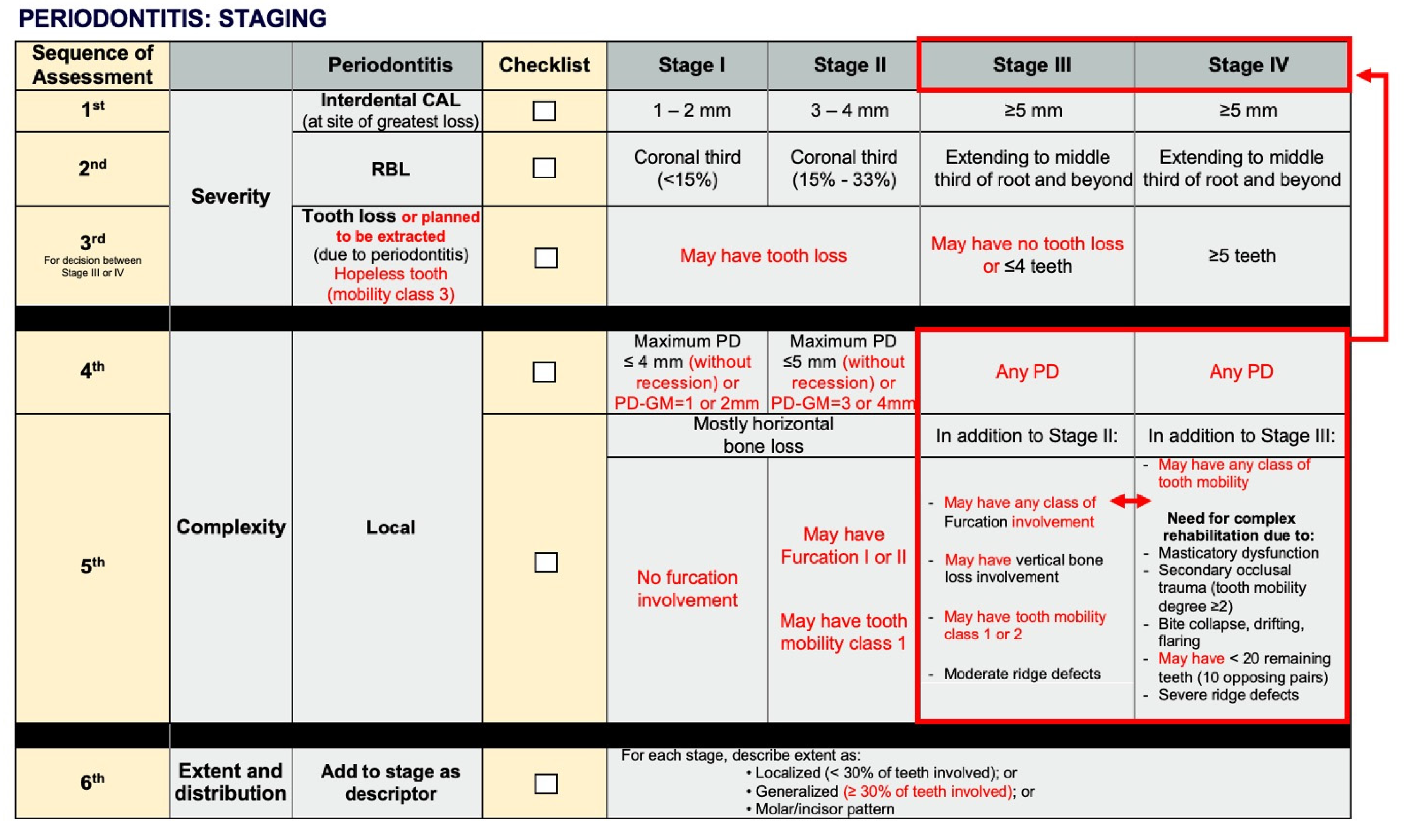
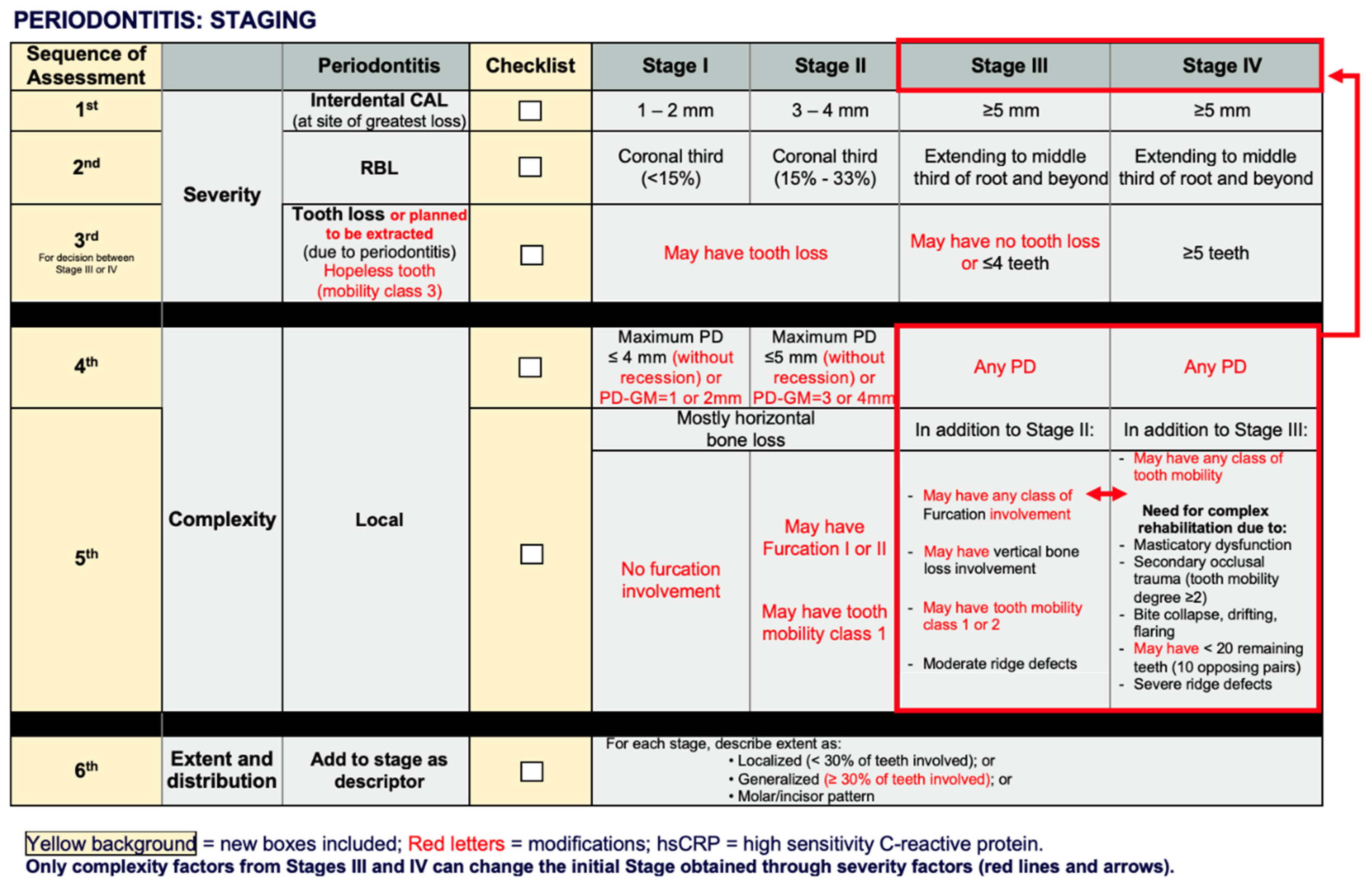
Current General Findings for Staging Periodontitis Based on the New Classification System
Discussion (Critical Understanding and Suggestions for Modifications)
Final Considerations
Conclusion
- -
- For severity:
- -
- For complexity:
References
- Anand, P.S.; Kamath, K.P.; Nair, B. Trends in extraction of permanent teeth in private dental practices in Kerala state, India. J Contemp Dent Pract. 2010, 11, 041–8. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Jepsen, S.; Jin, L.; Otomo-Corgel, J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017, 44, 456–462. [Google Scholar] [CrossRef]
- Reynolds, I.; Duane, B. Periodontal disease has an impact on patients’ quality of life. Ev Based Dent. 2018, 19, 14–15. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- FDI World Dental Federation. White paper on prevention and management of periodontal diseases for oral health and general health. 2018. (https://www.fdiworlddental.org/resource/white-paper-prevention-and-management-periodontal-diseases-oral-health-and-general-health).
- Jin, L.J.; Lamster, I.B.; Greenspan, J.S.; Pitts, N.B.; Scully, C.B.; Warnakulasuriya, S. Global burden of oral diseases: Emerging concepts, management and interplay with systemic health. Oral Dis. 2016, 22, 609–619. [Google Scholar] [CrossRef] [PubMed]
- Tavares, L.T.R.; Saavedra-Silva, M.; López-Marcos, J.F.; Veiga, N.J.; Castilho, R.d.M.; Fernandes, G.V.d.O. Blood and Salivary Inflammatory Biomarkers Profile in Patients with Chronic Kidney Disease and Periodontal Disease: A Systematic Review. Diseases. 2022, 10, 12. [Google Scholar] [CrossRef]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nature Rev. Dis Primers. 2017, 3, 1–14. [Google Scholar] [CrossRef]
- Becker, W.; Becker, B.E.; Berg, L.E. Periodontal treatment without maintenance. A retrospective study in 44 patients. J Periodontol. 1984, 55, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Salvi, G.E.; Lawrence, H.P.; Offenbacher, S.; Beck, J.D. Influence of risk factors on the pathogenesis of periodontitis. Periodontol 2000 1997, 14, 173–201. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Sanz, M.; Buduneli, N.; Dietrich, T.; Feres, M.; Fine, D.H.; Flemmig, T.F.; Garcia, R.; Giannobile, W.V.; Graziani, F.; Greenwell, H.; Herrera, D.; Kao, R.T.; Kebschull, M.; Kinane, D.F.; Kirkwood, K.L.; Kocher, T.; Kornman, K.S.; Kumar, P.S.; Loos, B.G.; Machtei, E.; Meng, H.; Mombelli, A.; Needleman, I.; Offenbacher, S.; Seymour, G.J.; Teles, R.; Tonetti, M.S. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018, 89 (Suppl. 1S), S173–S182. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions – Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018, 45 (Suppl. 20), S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol. 2018, 89 (Suppl. 1), S159–S172. [Google Scholar] [CrossRef] [PubMed]
- Kornman, K.S.; Papapanou, P.N. Clinical application of the new classification of periodontal diseases: ground rules, clarifications and “gray zones. ” J Periodontol. 2020, 91, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Tonetti, M.; Sanz, M. Implementation of the new classification of periodontal diseases: Decision-making algorithms for clinical practice and education. J Clin Periodontol. 2019, 46, S398–S405. [Google Scholar] [CrossRef] [PubMed]
- Sutthiboonyapan, P.; Wang, H.L.; Charatkulangkun, O. Flowcharts for easy periodontal diagnosis based on the 2018 new periodontal classification. Clin Adv Periodontics. 2020, 10, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, T.; Ower, P.; Tank, M.; West, N.X.; Walter, C.; Needleman, I.; Hughes, F.J.; Wadia, R.; Milward, M.R.; Hodge, P.J.; Chapple, I.L.C. Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions – implementation in clinical practice. Br Dental J. 2019, 226, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Sanz, M.; Tonetti, M. Clinical decision tree for staging and grading. J Clin Periodontol. 2019, 46, S398–S405. [Google Scholar]
- Pakdeesettakul, S.; Charatkulangkun, O.; Lertpimonchai, A.; Wang, H.-L.; Sutthiboonyapan, P. Simple flowcharts for periodontal diagnosis based on the 2018 new periodontal classification increased accuracy and clinician confidence in making a periodontal diagnosis: a randomized crossover trial. Clin Oral Inv. 2022, 26, 7021–7031. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, M.; Borgnakke, W.S.; Ogawa, H.; Yamaga, T.; Sato, M.; Minagawa, K.; Ansai, T.; Yoshihara, A.; Miyazaki, H. Effect of lifestyle on 6-year periodontitis incidence or progression and tooth loss in older adults. J Clin Periodontol. 2018, 45, 896–908. [Google Scholar] [CrossRef] [PubMed]
- Takedachi, M.; Shimabukuro, Y.; Sawada, K.; Koshimizu, M.; Shinada, K.; Asai, H.; Mizoguchi, A.; Hayashi, Y.; Tsukamoto, A.; Miyago, M.; Nishihara, F.; Nishihata, T.; Shimabukuro, M.; Kurakami, H.; Sato, T.; Hamazaki, Y.; Iwayama, T.; Fujihara, C.; Murakami, S. Evaluation of periodontitis-related tooth loss according to the new 2018 classification of periodontitis. Sci Rep. 2022, 12, 11893. [Google Scholar] [CrossRef]
- Sanz, M.; Papapanou, P.N.; Tonetti, M.S.; Greenwell, H.; Kornman, K. Guest Editorial: Clarifications on the use of the new classification of periodontitis. J Clin Periodontol. 2020, 47, 658–659. [Google Scholar] [CrossRef] [PubMed]
- Al-Rasheed, A.S. Assessing peculiarity of molar root trunk dimensions in a sample of Saudi population – A radiographic analysis. Saudi Dent J. 2019, 31, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Claffey, N.; Egelberg, J. Clinical indicators of probing attachment loss following initial periodontal treatment in advanced periodontitis patients. J Clin Periodontol. 1995, 22, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G. Contemporary interpretation of probing depth assessments: diagnostic and therapeutic implications. A Literature Review. J Periodontol. 1997, 68, 1194–1205. [Google Scholar] [CrossRef]
- Ravidà, A.; Travan, S.; Saleh, M.; Greenwell, H.; Papapanou, P.N.; Sanz, M.; Tonetti, M.; Wang, H.-L.; Kornman, K. Agreement among international periodontal experts using the 2017 World Workshop classification of periodontitis. J Periodontol. 2021, 92, 1675–1686. [Google Scholar] [CrossRef]
- Abrahamian, L.; Pascual-LaRocca, A.; Barallat, L.; Valles, C.; Herrera, D.; Sanz, M.; Nart, J.; Figuero, E. Intra- and inter-examiner reliability in classifying periodontitis according to the 2018 classification of periodontal diseases. J Clin Periodontol. 2022, 49, 732–739. [Google Scholar] [CrossRef]
- Gandhi, K.K.; Katwal, D.; Chang, J.; Blanchard, S.; Shin, D.; Maupome, G.; Eckert, G.J.; John, V. Diagnosis and treatment planning using the 2017 classification of periodontal diseases among three dental schools. J Dent Educ. 2022, 86, 1521–1528. [Google Scholar] [CrossRef]
- Sirinirund, B.; Di Gianfilippo, R.; Yu, S.-H.; Wang, H.-L.; Kornman, K.S. Diagnosis of Stage III Periodontitis and Ambiguities of the “Gray Zones” in Between Stage III and Stage IV. Clin Adv Periodontics. 2021, 11, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, R.; Andrade, N.; Yu, S.-H.; Kornman, K.S.; Wang, H.-L. Challenges and Decision Making for the Classification of Two Complex Periodontal Cases. Clin Adv Periodontics. 2021, 11, 103–110. [Google Scholar] [CrossRef]
- Steigmann, L.; Sommer, C.; Kornman, K.S.; Wang, H.-L. Staging and Grading Discussion of Borderline Cases in Gray Zones. Clin Adv Periodontics. 2021, 11, 98–102. [Google Scholar] [CrossRef]
- Marini, L.; Tonetti, M.S.; Nibali, L.; Rojas, M.A.; Aimetti, M.; Cairo, F.; Cavalcanti, R.; Crea, A.; Ferrarotti, F.; Graziani, F.; Landi, L.; Sforza, N.M.; Tomasi, C.; Pilloni, A. The staging and grading system in defining periodontitis cases: consistency and accuracy amongst periodontal experts, general dentists and undergraduate students. J Clin Periodontol. 2021, 48, 205–215. [Google Scholar] [CrossRef] [PubMed]
| PubMed/MEDLINE |
| ((“Periodontitis”) AND (“Periodontal” OR “Periodontal disease”) AND (“Classification”) AND (“Diagnosis”) NOT (“Treatment”)) |
| EMBASE |
| #1. (‘periodontitis’/exp OR ‘periodontitis’ OR ‘periodontal disease’/exp OR ‘periodontal disease’) #2. ‘classification’ #3. ‘diagnosis’ NOT ‘Treatment’ #4. #1 AND #2 AND #3 AND [2017-2024]/py |
| Web of Science |
| #1. ALL=(“Periodontitis” OR “Periodontal Disease”) #2. ALL=(“Classification”) #3. ALL=(“Diagnosis” NOT “Treatment”) #4. #1 AND #2 AND #3 and 2017 or 2018 or 2019 or 2020 or 2021 or 2022 or 2023 or 2024 (Publication Years) |
| Authors/ Year |
Title/Journal/IF | Objective | Periodontitis Assessment | Steps for Staging periodontitis | Critics & Comments |
|---|---|---|---|---|---|
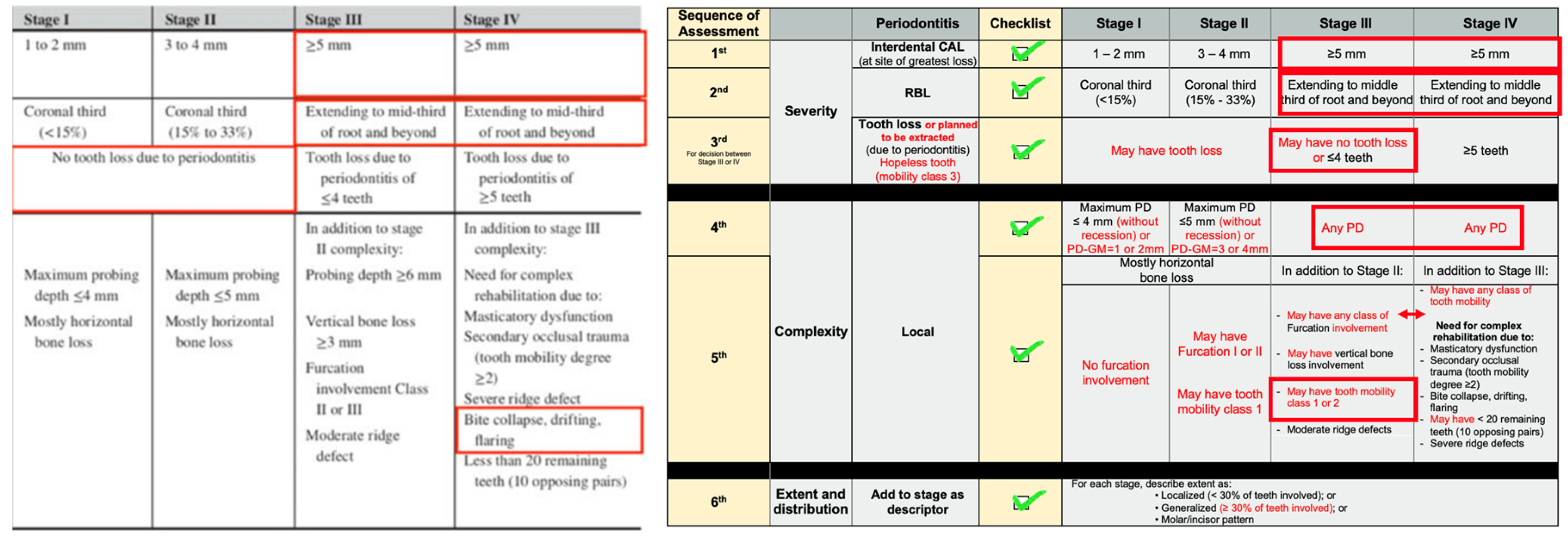
| Maurizio S. Tonetti, Mariano Sanz, 2019 [15] | Implementation of the new classification of periodontal diseases: Decision-making algorithms for clinical practice and education Journal of Clinical Periodontology 8.728 |
The authors developed empiric decision-making algorithms based on the new classification | - The authors created an extremely interesting flowchart, trying to help clinicians with a faster way to evaluate patients - CAL is the primary criterion for definition of periodontitis (when marginal alveolar bone loss is apparent on diagnostic quality radiographs, it may be an adequate proxy measure of CAL) - PPDs does not allow discrimination of periodontal health, gingivitis, periodontitis, reduced but healthy periodontium, gingival inflammation in a periodontitis patient. Clinicians must recognize the signs of CAL and discriminate them from other clinical conditions also associated with CAL (gingival recession, vertical root fractures, endo-periodontal lesions, loss on the distal of the lower second molars associated with impacted wisdom teeth, or attachment loss secondary to cervical decay or restorations) - Inter-dental CAL in the presence of periodontitis is easier recognized than usually appreciated and requires establishing whether or not the inter-dental CEJ is visible, or the tip of the periodontal probe reaches the root surface in the inter-dental space. - Better explore the reasons for tooth loss with the patient (if it was loose/with mobility or with cavities [caries]) to recognize tooth loss due to periodontitis. Lack of implication of this parameter in case definition and diagnosis leads to the paradox that periodontitis severity may improve as the most compromised teeth are lost. |
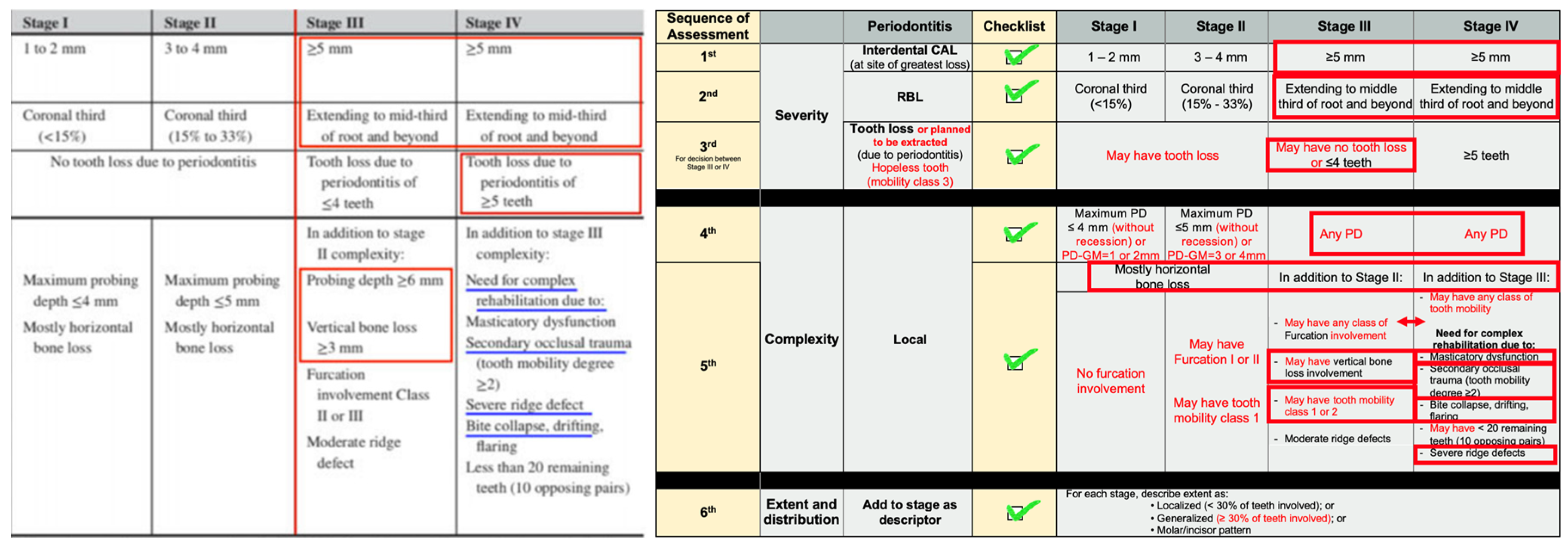
Step 1 a. full-mouth radiographs. Detect marginal bone in any area of the dentition (if available). If bone loss is detectable, the clinician should suspect the presence of periodontitis and move forward to step 2. b. If no radiographs are available or if no bone loss was detectable, it is imperative that the clinician assesses the whole dentition for the presence of signs of inter-dental CAL (presence of visible CEJ or the stopping of the tip of the periodontal probe on the root surface). If inter-dental CAL is detectable, the clinician should suspect the presence of periodontitis. c. If inter-dental CAL is not detected, to evaluate the presence of buccal (oral) recessions with PPDs higher than 3 mm (suspect the presence of periodontitis). d. To ascertain whether CAL is due to local factors only (endo-periodontal lesions, vertical root fractures, presence of caries or restorations or impacted third molars). e. To ascertain whether inter-dental CAL is present in >1 non-adjacent tooth (CAL involves ≥2 non-adjacent teeth, periodontitis) f. If the periodontal charting does not reveal PPD ≥4 mm, then the clinician needs to evaluate the full-mouth BOP (≥10% - gingival Inflammation in a periodontitis patient; <10% - reduced but healthy periodontium). If the periodontal charting shows PPD of 4 mm or more, the diagnosis is a periodontitis case that needs to be further assessed by staging and grading Step 2 a. Patient is a periodontitis case that needs to be staged: needed full-mouth radiographs, a periodontal chart and a periodontal history of tooth loss (PTL). b. Assess the extent of the disease, by determining whether CAL/BL affects <30% of the teeth (localized) of 30% or more (generalized) c. Define the stage of the disease by assessing severity through CAL, BL, and PTL, and complexity by assessing PPD, furcation and intrabony lesions, tooth hypermobility, secondary occlusal trauma, bite collapse, drifting, flaring or having <10 occluding pairs. Staging III and IV versus I and II a. CAL is ≥5mm or BL affects the middle third of the root or beyond, the diagnosis is either stage III or IV periodontitis b. CAL is <5mm, the clinician should look for the presence of class II or III furcation involvement. If present, the diagnosis is either stage III or IV. If no furcation involvement is present, the clinician should check PPD. If PPD is >5 mm, then the diagnosis is either stage III or IV. Clinical judgement should be applied to use PPD to upgrade from Stages I & II to Stage III. Diagnosis of stage I, II, III or IV a. Staging for I and II will be based upon the level of CAL and BL. When BL is <15% and CAL is between 1 and 2 mm, the diagnosis is stage I. When BL is between 15% and 33% and CAL is between 3 and 4 mm, the diagnosis is stage II. When BL affects the middle third of the root or beyond and CAL is 5 mm or more, if PTL is 4 teeth or less and in the presence of 10 or more occluding pairs, in the absence of bite collapse, drifting, flaring or a severe ridge defect, then the diagnosis is stage III. When BL affects the middle third of the root or beyond and CAL is 5 mm or more, if PTL is more than 4 teeth and in the absence of 10 occluding pairs, or when existing bite collapse, drifting, flaring or a severe ridge defect, then the diagnosis is stage IV. b. Once the correct periodontitis stage has been determined, the clinician should proceed to determine the grade. |
General - The flowchart presented was not validated (questions about the diagnostic accuracy and effectiveness) - The article did not clarify or report the best x-ray to check bone loss. Although it is known of all professionals and students, we highlight that is recommend bitewings for measurements and periapical radiographs to evaluate the periodontal ligaments and bone around the root(s). - “Lack of implication of this parameter (PTL) in case definition and diagnosis leads to the paradox that periodontitis severity may improve as the most compromised teeth are lost.” - This phrase must be carefully interpreted and cannot be applied for all cases. Periodontitis is a tooth/teeth-dependent condition and if the compromised tooth was extracted and the remaining teeth do not have CAL, cannot justify any treatment for the patient using SRPs (common treatment for periodontitis) For Step 1 - it seems that the authors want to create a clinical shortcut (due to the high complexity of this classification system) to avoid the complete periodontal evaluation in the beginning (not necessary to do the complete periodontal chart and to have radiographs). The complete periodontal chart and x-rays are mandatory, even though is time consuming, for the adequate evaluation of any periodontal case - evaluation only of the x-ray (if available) without to obtain the periodontal parameters measurements (clinical assessment only if the radiographs are not available). Radiographs are a complementary exam, and the clinical assessment is a mandatory criterion - No evaluation of tooth loss For Step 2 - full mouth radiographs, periodontal chart, and PTL only if the patient was considered periodontitis case. It could be requested/performed in the beginning for all patients, in order to evaluate all scenario Staging III and IV versus I and II - the item b, presented an affirmative condition that cannot be applied for all cases, but most of them. If there is no CAL >5mm (primary criterion of assessment), the complexity factors could not overcome the severity and change the stage, as suggested. The suggestion is to keep the Stage according to CAL, RBL, and PTL, including aggravators (complexity factors) to the Stage found. Diagnosis of stage I, II, III or IV - a shortcoming can be observed here for PTL. Stage I and II can present PTL in some cases, e.g., where the extent and distribution are localized molar-incisor pattern. A patient that lost one lower 1st molar and one lower incisor only and have only one 2nd lower adjacent per-molar with CAL = 2mm (mesial and distal); no other teeth with CAL. Again, the suggestion is to keep the Stage based on the severity (CAL and RBL) and present aggravators found in the PTL and complexity |
| Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MSrrr 2018 [11] |
Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions Journal of Periodontology 4.3 |
This article reviewed, debated and agreed by consensus on the overall conclusions of the five position papers | - Common patterns of CAL were identified across different ages - There is contribution of recession and pocket depth to CAL - Necrotizing periodontal diseases are characterized by three typical clinical features: papilla necrosis, bleeding, and pain; and are associated with host immune response impairments - Endodontic-periodontal lesions are defined by a pathological communication between the pulpal and periodontal tissues at a given tooth, occur in either an acute or a chronic form, and should be classified according to signs and symptoms that have direct impact on their prognosis and treatment; Periodontal abscesses most frequently occur in pre- existing periodontal pockets and should be classified according to their etiology. They are characterized by localized accumulation of pus - Neither age nor sex had any discernible effects on CAL change |
- Loss of periodontal tissue support due to inflammation is the primary feature of periodontitis - A threshold of interproximal, CAL of ≥2 mm or ≥3 mm at ≥2 non-adjacent teeth, is a commonly used parameter - Clinicians typically confirm presence of interproximal tissue loss through radiographic assessments of bone loss - Clinically meaningful descriptions of periodontitis should include the proportion of sites that BOP, and the number and proportion of teeth with probing depth over certain thresholds (commonly ≥4 mm and ≥6mm) and of teeth with CAL of ≥ 3mm and ≥5mm. In the context of clinical care, a patient is a “periodontitis case” if: 1. Interdental CAL is detectable at ≥ 2 non-adjacent teeth, or 2. Buccal or oral CAL ≥3 mm with pocketing ≥3 mm is detectable at ≥2 teeth but the observed CAL cannot be ascribed to non-periodontitis-related causes such as: 1) gingival recession of traumatic origin; 2) dental caries extending in the cervical area of the tooth; 3) the presence of CAL on the distal aspect of a second molar and associated with malposition or extraction of a third molar; 4) an endodontic lesion draining through the marginal periodontium; and 5) the occurrence of a vertical root fracture |
“Clinically meaningful descriptions of periodontitis should include the proportion of sites that BOP, and the number and proportion of teeth with probing depth over certain thresholds (commonly ≥4 mm and ≥6mm) and of teeth with CAL of ≥ 3mm and ≥5mm” (a) BOP can be considered in the Periodontal chart but it is not possible to take in consideration to classify periodontitis; this factor may depend on many variables (b) PD and CAL proportions Although these suggestions are excellent, they cannot represent accuracy and will create one more point of debate in the classification. It is suggested more studies on this topic 1. PD is already considered in the complexity of the periodontal classification (periodontitis), and as suggested above, it cannot change the stage found when observed the severity factors (CAL, RBL, PTL) |
| Maurizio S. Tonetti, Henry Greenwell, Kenneth S. Kornman 2018 [13] |
Staging and grading of periodontitis: Framework and proposal of a new classification and case definition Journal of Periodontology 4.3 |
To review evidence and rationale for a revision of the current classification, to provide a framework for case definition that fully implicates state-of-the-art knowledge and can be adapted as new evidence emerges, and to suggest a case definition system that can be implemented in clinical practice, research and epidemiologic surveillance | A patient is a periodontitis case in the context of clinical care if: 1. Interdental CAL is detectable at ≥ 2 non-adjacent teeth, or 2. Buccal or oral CAL ≥3 mm with pocketing >3 mm is detectable at ≥2 teeth and the observed CAL cannot be ascribed to non-periodontal causes such as: 1) gingival recession of traumatic origin; 2) dental caries extending in the cervical area of the tooth; 3) the presence of CAL on the distal aspect of a second molar and associated with malposition or extraction of a third molar, 4) an endodontic lesion draining through the marginal periodontium; and 5) the occurrence of a vertical root fracture. - BOP itself, or as a secondary parameter with CAL, does not change the initial case definition as defined by CAL or change the classification of periodontitis severity - The severity score is primarily based on interdental CAL in recognition of low specificity of both pocketing and marginal bone loss, although marginal bone loss is also included as an additional descriptor (based on the worst affected tooth in the dentition). Only attachment loss attributable to periodontitis is used for the score - The complexity score is based on the local treatment complexity assuming the wish/need to eliminate local factors and takes into account factors (vertical defects, furcation involvement, tooth hypermobility, drifting and/or flaring of teeth, tooth loss, ridge deficiency and loss of masticatory function) - Besides the local complexity, it is recognized that individual case management may be complicated by medical factors or comorbidities - CAL to determine the initial stage in the severity dimension. Some clinicians may prefer to use diagnostic quality radiographic imaging as an indirect and somehow less sensitive assessment of periodontal breakdown. This may be all that is necessary to establish the stage. |
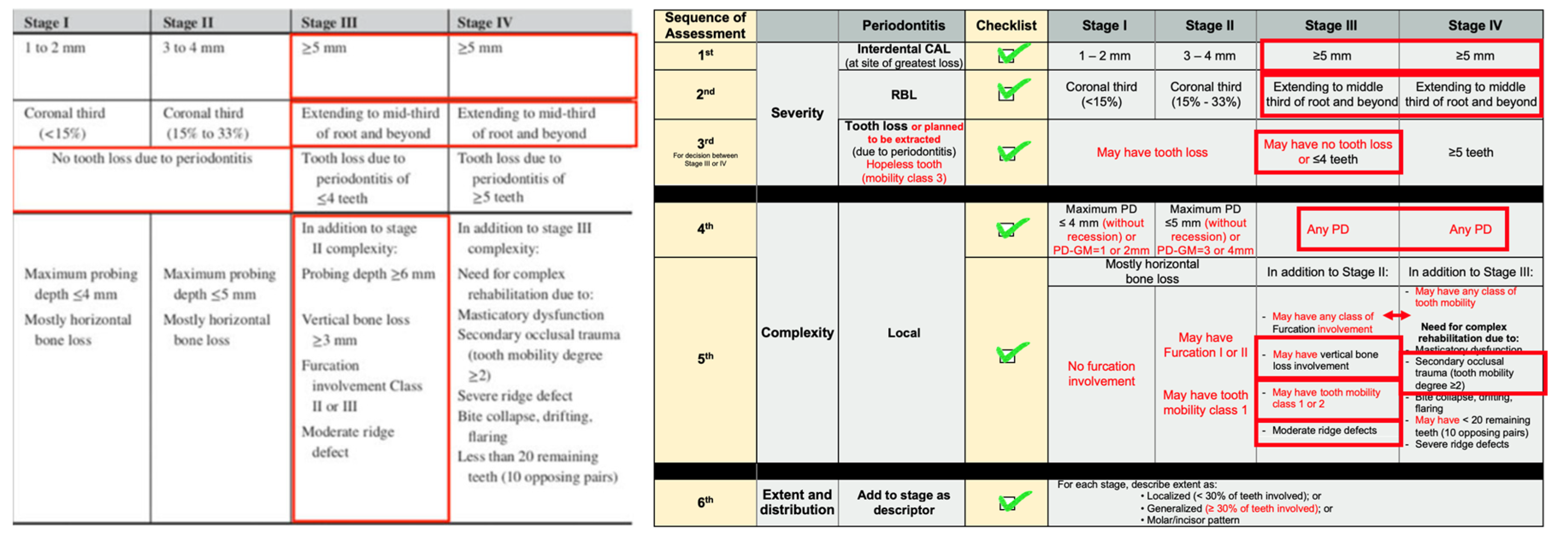
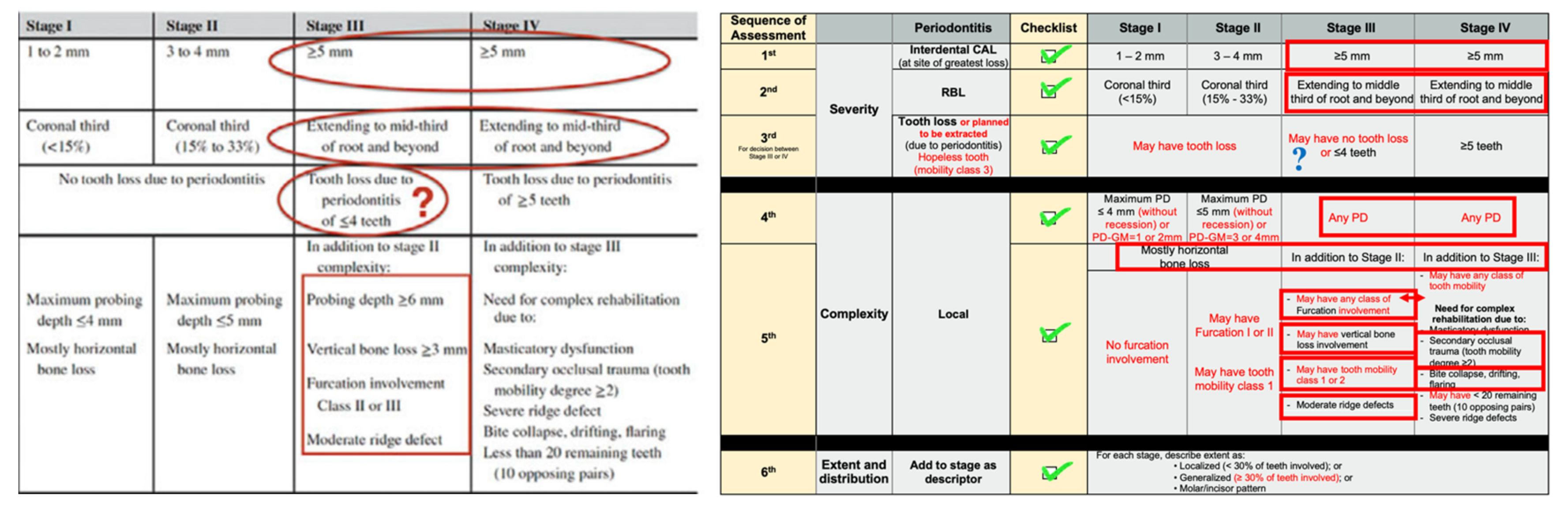
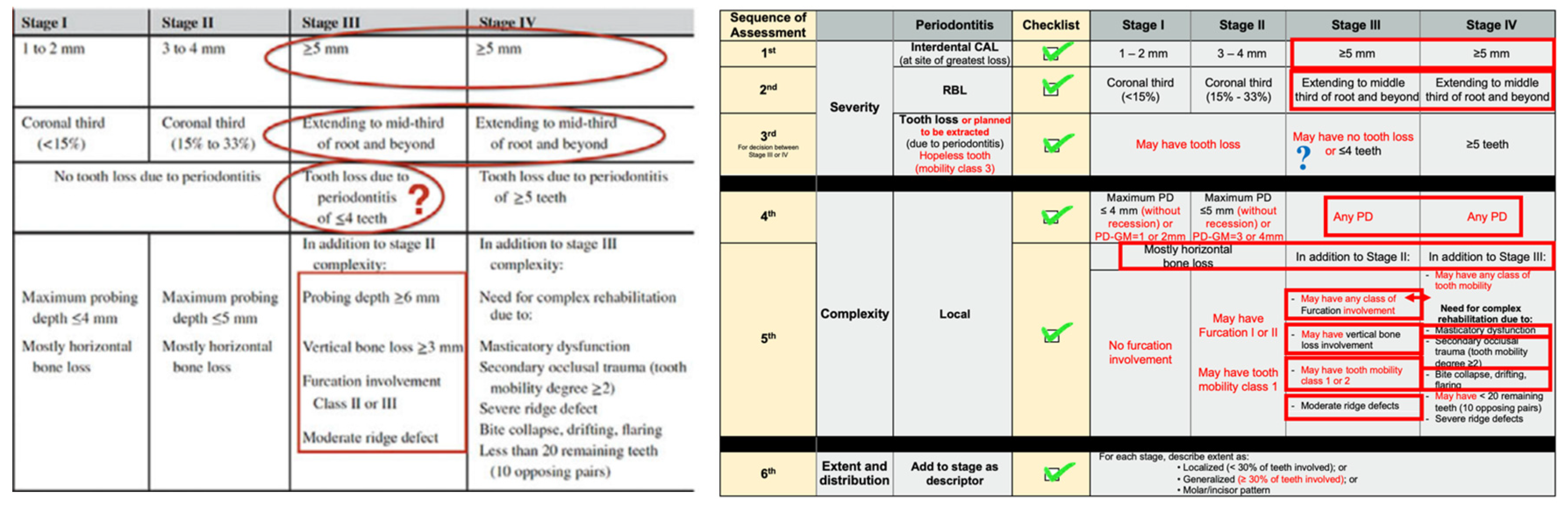
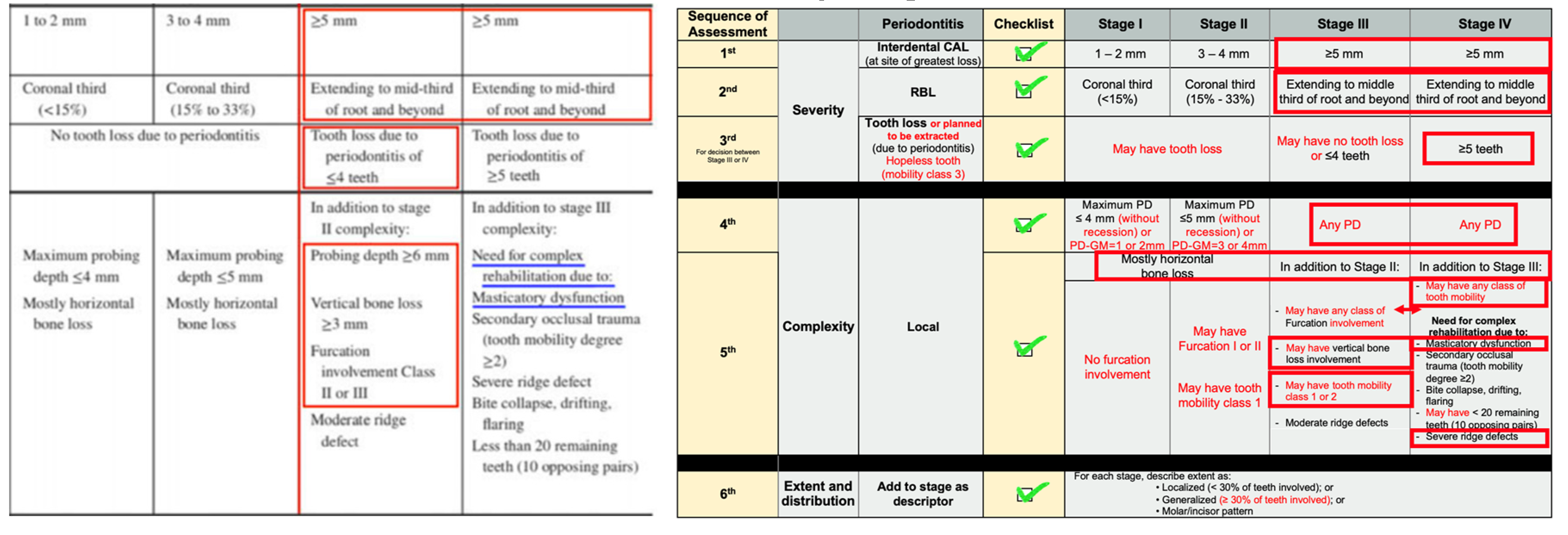
Severity - Stage I = Initial periodontitis; Stage II = Moderate periodontitis; Stage III = Severe periodontitis with potential for additional tooth loss; Stage IV = Advanced periodontitis with extensive tooth loss and potential for loss of dentition - CAL and RBL will be the primary stage determinants - If a stage shifting complexity factor(s) were eliminated by treatment, the stage should not retrogress to a lower stage since the original stage complexity factor should always be considered in maintenance phase management. A notable exception is successful periodontal regeneration that may, through improvement of tooth support, effectively improve CAL and RBL of the specific tooth - Conventional definitions of severe periodontitis need to be revised to better discriminate the more severe forms of periodontitis - Another important limitation of current definitions of severe periodontitis is a paradox: whenever the worst affected teeth in the dentition are lost, severity may actually decrease. Tooth loss attributable to periodontitis was incorporated in the definition of severity Complexity of management - Factors (PD, type of bone loss (vertical and/or horizontal), furcation status, tooth mobility, missing teeth, bite collapse, and residual ridge defect size) increase treatment complexity and need to be considered and should ultimately influence diagnostic classification. Explicit designation of case complexity factors helps to define levels of competence and experience that a case is likely to require for optimal outcomes |
Severity - “whenever the worst affected teeth in the dentition are lost, severity may actually decrease. Tooth loss attributable to periodontitis was incorporated in the definition of severity.” A shortcoming can be observed for the phrase above; Stage I and II, that suggested no tooth loss, can present PTL in some cases, e.g., where the extent and distribution are localized molar-incisor pattern. A patient that lost one lower 1st molar and one lower incisor only and have only one 2nd lower adjacent per-molar with CAL = 2mm (mesial and distal); no other teeth with CAL. The suggestion is to keep the Stage based on the severity (CAL and RBL) and present aggravators found in the PTL and complexity. Complexity of management - Even with all factors that can be present in the complexity of a case, it is suggested that all of them cannot modify the initial diagnosis of periodontitis found with the evaluation of CAL and RBL. Using PTL and the complexity factors, it is possible to change between Stage III and IV only Examples described in the article (1) “in case of very short common root trunk with a CAL of 4 mm, which may have resulted in class II furcation involvement; the classification recommended was Stage II; hence shifting the diagnosis from stage II to stage III periodontitis” (2) In the same case above, “if posterior bite collapse is present then the stage IV would be the appropriate stage diagnosis since the complexity is on the stage IV level” Once again, it is suggested to initially determine stage of periodontitis, must be used CAL and RBL; the other parameters should be considered and registered but they cannot change the diagnosis (Stage). The cases above were presented without a good contextualization of them |
| Kenneth S. Kornman, Panos N. Papapanou 2020 [14] |
Clinical application of the new classification of periodontal diseases: Ground rules, clarifications and “gray zones” Journal of Periodontology 4.3 |
Reiterate some basic principles, emphasize important “ground rules,” identify potential gray zones, and provide practical tips that will help clinicians to seamlessly navigate the new system in their everyday clinical practice | - Stage reflects the severity of the disease (expressed through CAL and RBL), but also tooth loss that has occurred as a result of periodontitis, at least as well as can be determined. it reflects anticipated complexity of treatment required to eradicate/reduce the current level of infection and inflammation - Grade describes additional biological dimensions of the disease including the observed or inferred progression rate, the risk for further deterioration due to environmental exposures (smoking) and co-morbidities (diabetes), and the risk that the disease or its treatment may adversely affect the patient’s general health status - BOP is a valuable clinical parameter to help assess current levels of inflammation and residual risk post-treatment, but BOP does not influence the classification |
1st step – Periodontitis a. CAL: if (1) interproximal CAL is present at least at two different, non-adjacent teeth, and (2) the observed CAL cannot be attributed to traumatic factors or non-periodontitis related etiologies (e.g., root fracture, endodontic infection, surgical trauma) b. In the absence of interproximal CAL, but if CAL that cannot be ascribed to non-periodontitis-related causes is present at buccal or lingual surfaces, a diagnosis of periodontitis requires concomitant presence of CAL of ≥3 mm and PD of ≥3 mm at ≥2 teeth c. Confirm the presence of CAL by corresponding interproximal RBL. Do not use of RBL as the primary criterion (under-detection of incipient periodontitis and an increase in “false negatives”) 2nd step - Stage (severity) - Stages I and II in adult patients (incipient or moderate severity, no loss of any teeth) are likely very different from Stages III and IV (one or several intrinsic or environmental risk factors, more complex cases) - Staging: medical history, radiographs, and probing chart to distinguish between Stage I or II versus Stage III or IV periodontitis (severity of tissue damage and the presence of periodontitis-associated tooth loss) – to study in detail the available full-mouth periodontal charting and full-mouth series of intra-oral radiographs - RBL: bone loss of up to 15%; extending between 15% and 33% of the root length (not necessary a high level of precision) and extending to middle third of root and beyond. The intention is to distinguish between an incipient stage from more substantial bone loss - If in the assessment the patient was classified as Stage III (severe periodontitis) or Stage IV (very severe periodontitis) periodontitis, PTL can be attributed to periodontitis (one to four teeth versus five or more teeth lost); or then, on the presence of the various complexity factors. It must be realized that either Stage III or Stage IV Step 3 - Complexity: e.g., Stage IV - periodontitis threatens the entire dentition and, consequently, treatment requires extensive oral rehabilitation Step 4 - Extent and Distribution: “localized” or “generalized” describe the extent of the dentition that is affected by the Stage-defining severity - Can a patient’s Stage change over time? (a) If a patient that has been staged at a given time point experiences significant disease progression or disease recurrence after therapy that results in increased severity and/or more complex treatment needs, then stage must be shifted upwards at the time of the subsequent examination, as appropriate (b) However, although the severity of CAL and/or RBL can be reduced substantially from beyond the coronal third to within the coronal third in cases of successful regeneration therapy, it is advised that the patient retains the Stage originally assigned prior to the treatment |
1st step – Periodontitis - It is suggested that PTL can be present in Stage I and II; but primarily, it is necessary to obtain the CAL and RBL for the correct diagnosis - “BOP is a valuable clinical parameter to help assess current levels of inflammation and residual risk post-treatment, but BOP does not influence the classification” – BOP cannot have any influence on the diagnosis of periodontitis - “Confirm the presence of CAL by corresponding interproximal RBL. Do not use of RBL as the primary criterion (under-detection of incipient periodontitis and an increase in “false negatives”)” – always to use CAL as 1st criterion of diagnosis 2nd step - Stage (severity) - It is suggested to consider, even though cannot be so common, the existence of tooth loss in Stages I and II Step 4 - “In cases of successful periodontal regeneration therapy, it is advised that the patient retains the Stage originally assigned prior to the treatment” – It is suggested to keep the previous diagnosis for at least 12 months; if the values (numbers) are kept improved/stable, a new assessment and diagnosis must be performed |
| Pimchanok Sutthiboonyapan, Hom-Lay Wang, Orawan Charatkulangkun 2020 [16] |
Flowcharts for Easy Periodontal Diagnosis Based on the 2018 New Periodontal Classification Clinical Advances in Periodontics 0.7 |
Flowchart designed for quick initial screening to make proper diagnosis for three most commonly found periodontal conditions (health, gingivitis, and periodontitis) to differentiate the types of periodontitis diagnosis by using staging and grading system |
- The authors developed an interesting flowchart. It can be extremely useful in order to accelerate the periodontal assessment - Otherwise, there is an inconsistence in the severity of periodontitis analysis: 1st parameter used was “tooth loss” due periodontitis instead of CAL and RBL - Grade |
Severity of periodontitis 1. tooth loss from periodontitis, including teeth planned for extraction due to periodontitis. If tooth loss existed, then the case is either stage III or IV 2. The differentiation of stage III or IV is based on the number of teeth lost and masticatory dysfunction (a) ≥5 teeth and/or <20 remaining teeth and/or need a rehabilitation because of masticatory dysfunction, periodontitis stage IV (b) ≤4 teeth lost due to periodontitis and no other masticatory dysfunction, then stage III (c) no tooth loss or has tooth loss from reasons other than periodontitis or unknown cause, a combination of CAL, PD, and RBL will be used to classify the patient 3. Then, (a)CAL ≥5 mm and/or PD ≥6 mm and/or vertical bone loss ≥3 mm and/or furcation involvement grade 2 or 3, the case is either stage III or IV (masticatory dysfunction and/or number of the remaining teeth will then be used to determine the stage) (b) CAL is <5 mm and/or PD <6 mm, stage I or II is assigned Grade of periodontitis 4. Grade B is usually the default for most periodontitis cases and a clinician will consider if it should be adjusted to grade A or grade C (a) Primary criteria for grade: disease progression - direct evidence from longitudinal data (>5 years) of RBL or CAL, or the indirect evidence from a calculation of percentage of bone loss per age (b) Pattern of periodontal destruction. If there is evidence of rapid progression or inconsistency of biofilm and periodontal destruction - grade C. However, if there is no evidence of periodontal disease progression or percentage of bone loss per age <0.25, grade A is assigned. The presence or control of risk factors can also modify the grade assignments. For example, if the patient is a heavy smoker or has uncontrolled diabetes, periodontitis grade B can be modified to grade C |
Severity of periodontitis - The first point of analysis for staging periodontitis in this flowchart was tooth lost or planned to be extracted. This fact is going against the original classification and many mistakes can be found in this stage. It is highly recommended avoiding to use tooth loss as the first parameter; moreover, it is suggested CAL and RBL to be analyzed before tooth loss - CAL and RBL were used as secondary parameters; this fact is contrary of the proposal of the new classification and can invalidate the correct use of the flowchart related to the new classification - although this flowchart seems extremely useful, it is making mistake to find the Stage of periodontitis. In a clinical trial developed by the authors to validate this flowchart,[19] they recognized that “Modifications of the proposed flowcharts could enhance the accuracy of the periodontal diagnosis. Most errors in the full diagnosis were in the details of each diagnosis rather than disease identification, especially in periodontitis cases”. - The authors affirmed: (a) “This implied that the flowcharts for periodontitis stage and grade provide accuracy for identifying periodontitis extent and grade comparable to the consensus reports (75.93 vs. 72.39%, respectively), and provide better accuracy of the assigned periodontitis stage” (b) “For identifying periodontitis cases, the group using flowcharts obtained higher median scores than the group using consensus reports (p=0.004)” - Therefore, the authors are trying to cause a confusion on the consensus performed, deciding by themselves that evaluate tooth loss before CAL and RBL will lead the clinicians to a better result than the decision obtained of all experts in the consensus. Again, the idea of evaluating first tooth loss is not the original commandment of the new classification, which must be taken in consideration |
| T. Dietrich, P. Ower, M. Tank, N. X. West, C. Walter, I. Needleman, F. J. Hughes, R. Wadia, M. R. Milward, P. J. Hodge, I. L. C. Chapple 2019 [17] |
Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions – implementation in clinical practice British Dental Journal 1.626 |
Periodontal diagnosis in the context of the 2017 classification system of periodontal diseases and conditions – implementation in clinical practice |
- To create an algorithm for clinical periodontal assessment of plaque-induced periodontal disease - The authors proposed a flowchart mixing BPE with the new classification system |
The article posed a lot of true questions for staging: (a) “The BSP implementation group recognized several challenges with the proposed periodontitis staging grid for implementation in general dental practice, specifically: • The lack of an unambiguous decision rule that describes how the various parameters in the staging grid should be combined to determine a patient’s disease stage • The fact that clinical attachment loss is not routinely measured in clinical practice • The inclusion of complexity measures such as tooth loss due to periodontitis and alveolar ridge defects, which may be difficult to ascertain and/or may not be well defined.” Although all these points are correctly posted, the clinician must include in the daily routine not only the use of PD, BOP, and tooth loss, but also CAl and GM position, in order to work adequately (even it increases the time of the appointment) - BPE is divided in 4 codes: ‘0’ indicates that no treatment is required ‘1’ and ‘2’ mean that a basic clean is needed ‘3’ and ‘4’ means gum disease is advancing and subsequently requires advanced therapy - if PPD is at least 4 mm (BPE code 3); if the PPD is at least 6 mm (BPE code 4) - staging and grading from the new classification were summarized/adapted for periodontitis cases: (a) interproximal bone loss (Staging): <15% or RBL <2 mm (Stage I); Coronal third of root (Stage II); Mid third of root (Stage III), and Apical third of root (Stage IV) (b) % bone loss / age (Grade): < 0.5 (Grade A); 0.5-1.0 (Grade B); > 1.0 (Grade C) - Extent and distribution were equal of the new classification |
- The flowchart proposed a mix of the Performing a BPE entails ‘walking’ the probe around each tooth and recording only the worst score (code 0–4) in each sextant for efficiency - The authors explained that BPE and its equivalent systems have been well established in the clinical community across Europe due to its relative simplicity and efficiency. Then, they modified the BPE original version, mixing with part of the new classification, but adapted - the initial evaluation using BPE is based on the recession in the interdental area, BOP and PPD; then, it is unable to identify patients with historical periodontitis; this system does not use CAL or RBL - The use of BPE on a periodontal patient (with periodontitis) and no BPE scores greater than 2, would wrongly result in a provisional classification of periodontal health (<10% sites with BOP), localized gingivitis (10–30% sites with BOP) or generalized gingivitis (>30% sites with BOP), rather than capture the fact that the patient is a periodontitis patient with a current status of health or gingival inflammation “As per current BSP guidance a maximum BPE code of 3 would trigger a panoramic radiograph and/or selective periapical radiographs, which will allow determination of percentage bone loss relative to the root length.” They suggested the use of radiographs that are not the best to evaluate measures. Therefore, in the Stage section, they suggested bitewings for the posterior areas Summarizing, the article introduced a new methodology/adaptation for periodontal evaluation which abandoned/unsettin part of the new classification. Moreover, this algorithm must be validated |
| CONDITION | FORMULA (CA level = PD – GM) |
|
a. Tooth without recession: Without recession means that it is considering the GM in the “normal” position (+1mm above CEJ) - It is suggested GM (+)1mm coronally to CEJ to facilitate the calculation; therefore, normally, this number can be greater (check clinically this measure from GM to CEJ for greater accuracy) - It is necessary to remember and consider +2mm of the supracrestal tissue attachment (former biological width) |
PD = 4mm; GM = +1mm CA level = 4-1 = 3mm; (remember that 2mm belongs to the biological width); there is no CAL or, then, 1mm of CAL (needs a deeper assessment of the case) PD = 5mm; GM = +1mm CA level = 5-1 = 4mm (-2mm biological width) = 2mm of CAL PD = 6mm; GM = +1mm CA level = 6-1 = 5mm (-2mm biological width) = 3mm of CAL |
|
b. Tooth with recession: (GM at the same level CEJ [CEJ = GM] or apically positioned) |
PD = 2mm; GM = 0 (buccal recession) CA level = 2mm - 0 = 2mm (No CAL) – it is not Periodontitis (needs of a deeper assessment of the case) PD = 3mm; GM = 0 (buccal recession) CA level = 3mm - 0 = 3mm (CAL = 3mm) PD = 4mm; GM = 0 (interdental recession) CA level = 4-0 = 4mm of CAL PD = 2mm; GM = -1 (interdental recession) CA level = 2-(-1) = 3mm CAL PD = 2mm; GM = -2 (interdental recession) CA level = 2-(-2) = 4mm CAL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





