Submitted:
26 June 2024
Posted:
26 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Experimental Design
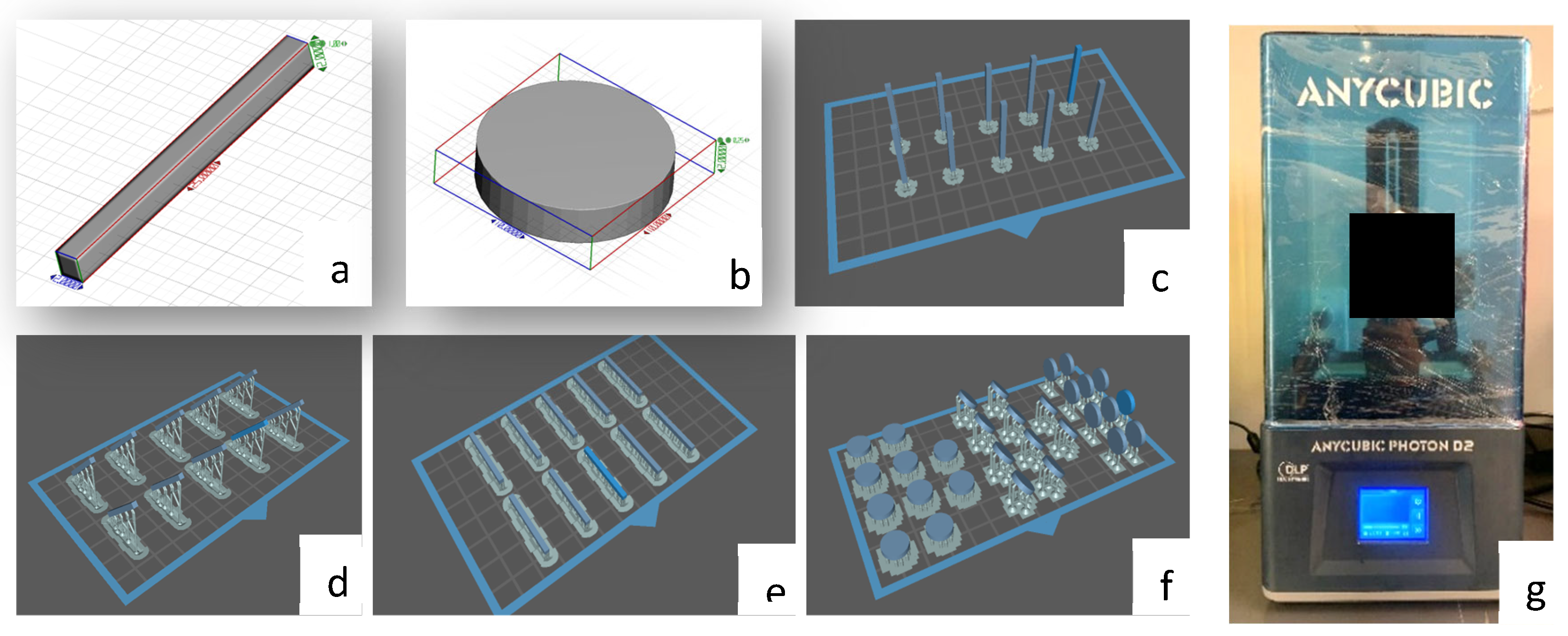
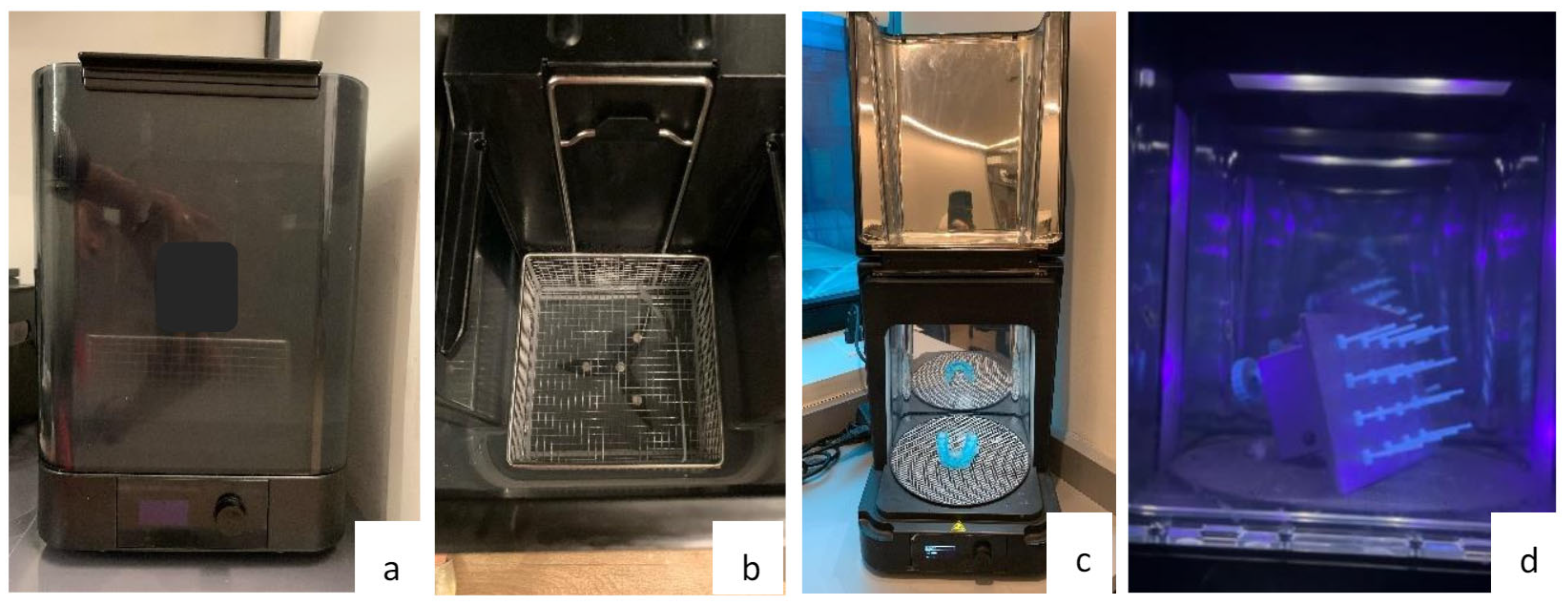
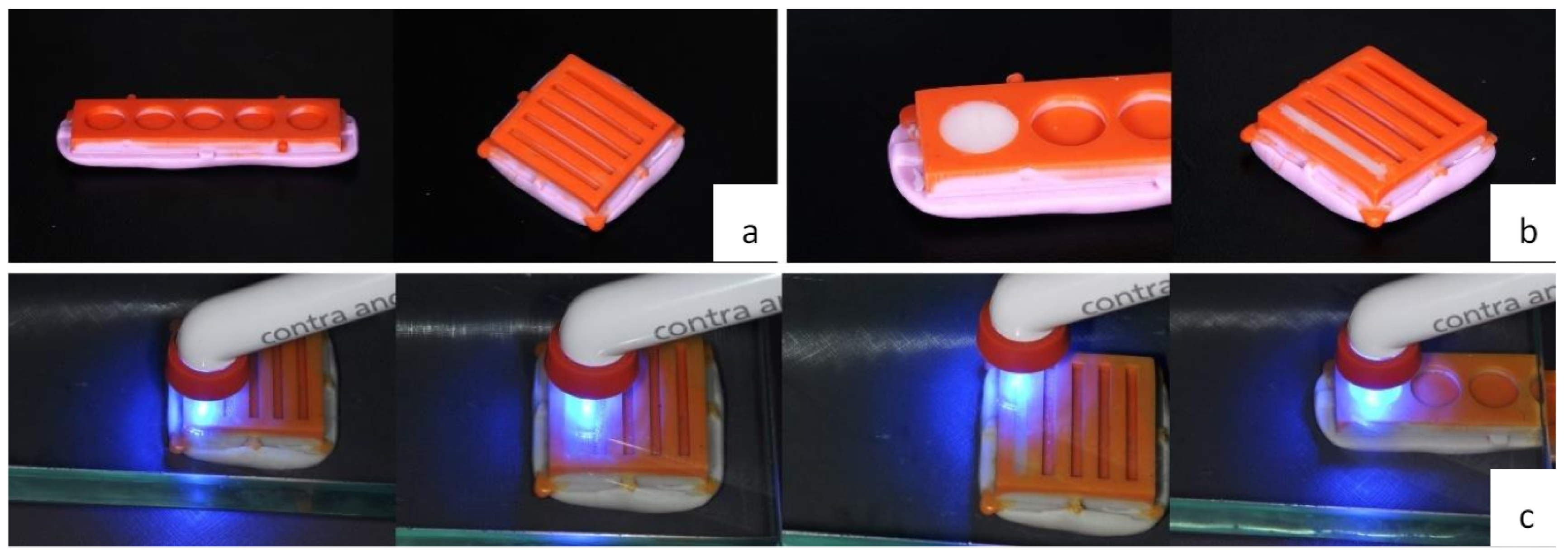
2.2. Preparation of Test Specimens
2.3. Flexural Strength Test (σ)
- σ = flexural strength
- = Load (force) at the fracture point
- = length of support span
- = Width of the sample
- = Sample thickness
2.4. Surface Roughness Test (Ra)
2.5. Microhardness Test
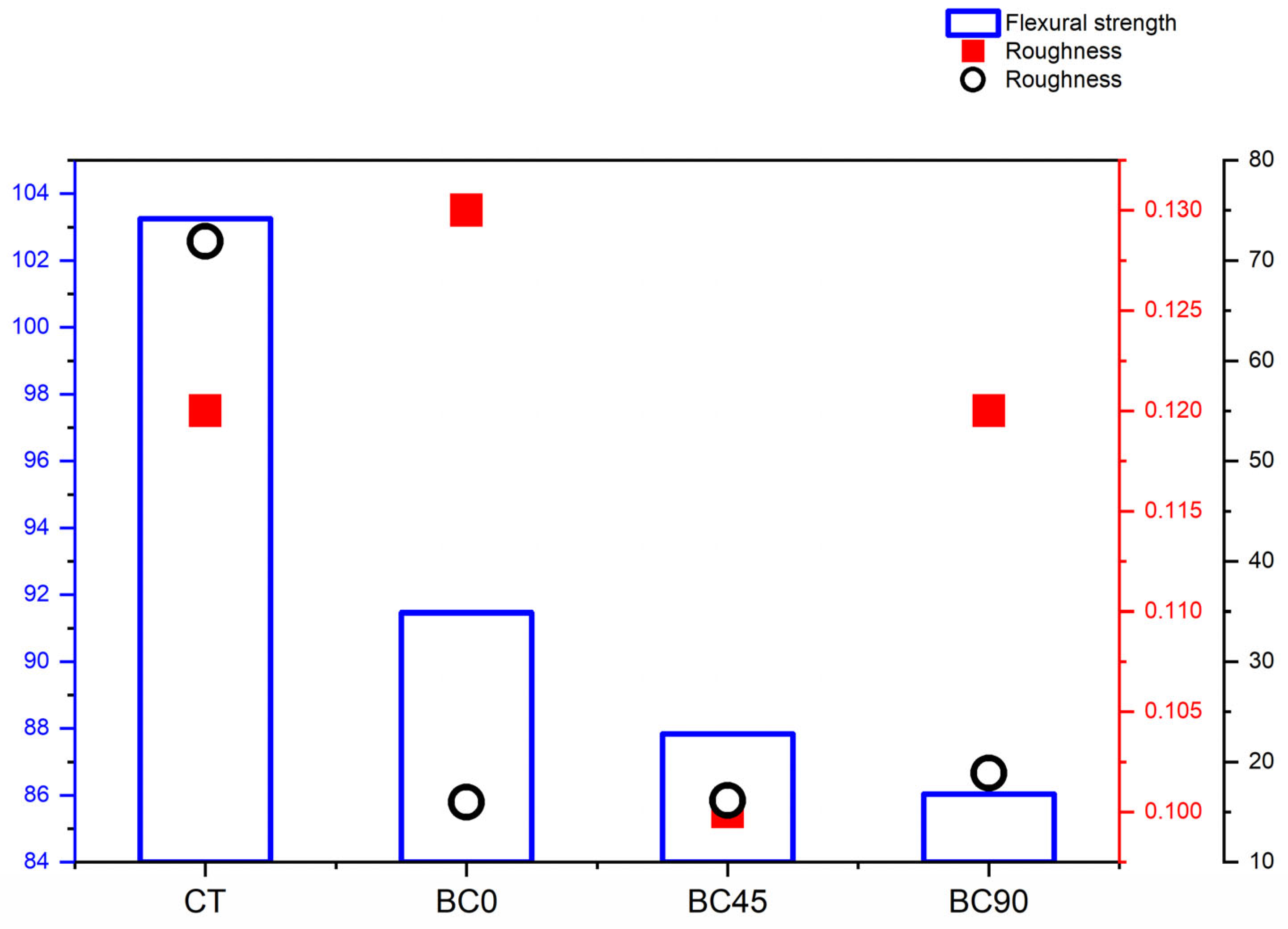
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Duret F, Blouin JL, Duret B. CAD-CAM in dentistry. J Am Dent Assoc. 1988 Nov;117(6):715-20. [CrossRef] [PubMed]
- van Noort, R. The future of dental devices is digital. Dent Mater. 2012 Jan;28(1):3-12. Epub 2011 Nov 26. [CrossRef] [PubMed]
- Myagmar G, Lee JH, Ahn JS, Yeo IL, Yoon HI, Han JS. Wear of 3D printed and CAD/CAM milled interim resin materials after chewing simulation. J Adv Prosthodont. 2021 Jun;13(3):144-151. Epub 2021 Jun 25. [CrossRef] [PubMed]
- Valenti C, Isabella Federici M, Masciotti F, Marinucci L, Xhimitiku I, Cianetti S, Pagano S. Mechanical properties of 3D-printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J Prosthet Dent. 2022 Aug 5:S0022-3913(22)00415-2 Epub ahead of print. [CrossRef] [PubMed]
- Kessler A, Hickel R, Reymus M. 3D Printing in Dentistry-State of the Art. Oper Dent. 2020 Jan/Feb;45(1):30-40. Epub 2019 Jun 7. [CrossRef] [PubMed]
- Nowacki B, Kowol P, Kozioł M, Olesik P, Wieczorek J, Wacławiak K. Effect of Post-Process Curing and Washing Time on Mechanical Properties of mSLA Printouts. Materials (Basel). 2021 Aug 26;14(17):4856. [CrossRef] [PubMed]
- Jockusch J, Özcan M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent Mater J. 2020 Jun 5;39(3):345-354. Epub 2020 Feb 7. [CrossRef] [PubMed]
- Tack P, Victor J, Gemmel P, Annemans L. 3D-printing techniques in a medical setting: a systematic literature review. Biomed Eng Online. 2016 Oct 21;15(1):115. [CrossRef] [PubMed]
- Revilla-León M, Özcan M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J Prosthodont. 2019 Feb;28(2):146-158. Epub 2018 Apr 22. [CrossRef] [PubMed]
- Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018 Feb;34(2):192-200. Epub 2017 Oct 27. [CrossRef] [PubMed]
- Zimmermann M, Ender A, Egli G, Özcan M, Mehl A. Fracture load of CAD/CAM-fabricated and 3D-printed composite crowns as a function of material thickness. Clin Oral Investig. 2019 Jun;23(6):2777-2784. Epub 2018 Oct 27. [CrossRef] [PubMed]
- Lu Y, Wang L, Dal Piva AMO, Tribst JPM, Čokić SM, Zhang F, Werner A, Kleverlaan CJ, Feilzer AJ. Effect of printing layer orientation and polishing on the fatigue strength of 3D-printed dental zirconia. Dent Mater. 2024 Feb;40(2):190-197. Epub 2023 Nov 17. [CrossRef] [PubMed]
- Bora PV, Sayed Ahmed A, Alford A, Pitttman K, Thomas V, Lawson NC. Characterization of materials used for 3D printing dental crowns and hybrid prostheses. J Esthet Restor Dent. 2024 Jan;36(1):220-230. Epub 2023 Nov 26. [CrossRef] [PubMed]
- International Organization for Standarization. ISO 4049:2009 Dentistry Polymer based restorative materials. 2009;2000.
- Shim JS, Kim JE, Jeong SH, Choi YJ, Ryu JJ. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J Prosthet Dent. 2020 Oct;124(4):468-475. Epub 2019 Dec 4. [CrossRef] [PubMed]
- Ribeiro AKC, de Freitas RFCP, de Carvalho IHG, de Miranda LM, da Silva NR, de Fátima Dantas de Almeida L, Zhang Y, da Fonte Porto Carreiro A, de Assunção E Souza RO. Flexural strength, surface roughness, micro-CT analysis, and microbiological adhesion of a 3D-printed temporary crown material. Clin Oral Investig. 2023 May;27(5):2207-2220. Epub 2023 Mar 18. [CrossRef] [PubMed]
- Scotti CK, Velo MMAC, Rizzante FAP, Nascimento TRL, Mondelli RFL, Bombonatti JFS. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J Prosthet Dent. 2020 Nov;124(5):614.e1-614.e5. Epub 2020 Jul 4. [CrossRef] [PubMed]
- Al-Dulaijan YA, Alsulaimi L, Alotaibi R, Alboainain A, Alalawi H, Alshehri S, Khan SQ, Alsaloum M, AlRumaih HS, Alhumaidan AA, Gad MM. Comparative Evaluation of Surface Roughness and Hardness of 3D Printed Resins. Materials (Basel). 2022 Oct 1;15(19):6822. [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences Second Edition.
- Digholkar S, Madhav VN, Palaskar J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J Indian Prosthodont Soc. 2016 Oct-Dec;16(4):328-334. [CrossRef] [PubMed]
- Chen H, Cheng DH, Huang SC, Lin YM. Comparison of flexural properties and cytotoxicity of interim materials printed from mono-LCD and DLP 3D printers. J Prosthet Dent. 2021 Nov;126(5):703-708. [CrossRef]
- KEßLER A, Hickel R, Ilie N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent Mater J. 2021 May 29;40(3):641-649. Epub 2021 Jan 15. [CrossRef] [PubMed]
- Soto-Montero J, de Castro EF, Romano BC, Nima G, Shimokawa CAK, Giannini M. Color alterations, flexural strength, and microhardness of 3D printed resins for fixed provisional restoration using different post-curing times. Dent Mater. 2022 Aug;38(8):1271-1282. Epub 2022 Jun 16. [CrossRef] [PubMed]
- Baytur S, Diken Turksayar AA. Effects of post-polymerization conditions on color properties, surface roughness, and flexural strength of 3D-printed permanent resin material after thermal aging. J Prosthodont. 2023 Dec 15. Epub ahead of print. [CrossRef] [PubMed]
- Miura D, Miyasaka T, Aoki H, Aoyagi Y, Ishida Y. Correlations among bending test methods for dental hard resins. Dent Mater J. 2017 Jul 26;36(4):491-496. Epub 2017 Apr 18. [CrossRef] [PubMed]
- Al-Qahtani AS, Tulbah HI, Binhasan M, Abbasi MS, Ahmed N, Shabib S, Farooq I, Aldahian N, Nisar SS, Tanveer SA, Vohra F, Abduljabbar T. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers (Basel). 2021 Nov 24;13(23):4077. [CrossRef] [PubMed]
- Pereira LDE, Couto Neto MP, Pereira RG, Schneider LFJ. Influence of resin matrix on the rheology, translucency, and curing potential of experimental flowable composites for bulk-fill applications. Dent Mater. 2021 Jun;37(6):1046-1053. Epub 2021 Apr 14. [CrossRef] [PubMed]
- Lin CH, Lin YM, Lai YL, Lee SY. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J Prosthet Dent. 2020 Feb;123(2):349-354. Epub 2019 Jun 12. [CrossRef] [PubMed]
- Wang L, Ni X. The effect of the inorganic nanomaterials on the UV-absorption, rheological and mechanical properties of the rapid prototyping epoxy-based composites. Polymer Bulletin. 2017 Jun 1;74(6):2063–79.
- Devlukia S, Hammond L, Malik K. Is surface roughness of direct resin composite restorations material and polisher-dependent? A systematic review. J Esthet Restor Dent. 2023 Sep;35(6):947-967. Epub 2023 Jul 17. [CrossRef] [PubMed]
- Alharbi N, Osman R, Wismeijer D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J Prosthet Dent. 2016 Jun;115(6):760-7. Epub 2016 Jan 21. [CrossRef] [PubMed]
- Unkovskiy A, Bui PH, Schille C, Geis-Gerstorfer J, Huettig F, Spintzyk S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent Mater. 2018 Dec;34(12):e324-e333. Epub 2018 Oct 4. [CrossRef] [PubMed]
- Väyrynen VO, Tanner J, Vallittu PK. The anisotropicity of the flexural properties of an occlusal device material processed by stereolithography. J Prosthet Dent. 2016 Nov;116(5):811-817. Epub 2016 Jun 14. [CrossRef] [PubMed]
- Alharethi, NA. Evaluation of the Influence of Build Orientation on the Surface Roughness and Flexural Strength of 3D-Printed Denture Base Resin and Its Comparison with CAD-CAM Milled Denture Base Resin. Eur J Dent. 2024 Feb;18(1):321-328. Epub 2023 Jun 9. [CrossRef] [PubMed]
- Daher R, Ardu S, di Bella E, Krejci I, Duc O. Efficiency of 3D printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J Prosthet Dent. 2024 May;131(5):943-950. Epub 2022 Nov 1. [CrossRef] [PubMed]
- Della Bona A, Cantelli V, Britto VT, Collares KF, Stansbury JW. 3D printing restorative materials using a stereolithographic technique: a systematic review. Dent Mater. 2021 Feb;37(2):336-350. Epub 2021 Jan 19. [CrossRef] [PubMed]
- Tsolakis IA, Gizani S, Panayi N, Antonopoulos G, Tsolakis AI. Three-Dimensional Printing Technology in Orthodontics for Dental Models: A Systematic Review. Children (Basel). 2022 Jul 23;9(8):1106. [CrossRef] [PubMed]
- van Dijken, JW. Direct resin composite inlays/onlays: an 11 year follow-up. J Dent. 2000 Jul;28(5):299-306. [CrossRef] [PubMed]
- Pallesen U, Qvist V. Composite resin fillings and inlays. An 11-year evaluation. Clin Oral Investig. 2003 Jun;7(2):71-9. Epub 2003 May 10. [CrossRef] [PubMed]
- Cetin AR, Unlu N, Cobanoglu N. A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth. Oper Dent. 2013 Mar-Apr;38(2):E1-11. Epub 2012 Dec 5. [CrossRef] [PubMed]
| Material | Composition | Lote |
| Forma Resin (Ultradent from Brazil) | Bis-GMA; Bis-EMA; TEGDMA; B HT; PEGDMA; UDMA; Ytterbium trifluoride; fillers based on silane-treated ceramics, silanized silica, silanized silica-zirconium oxide and barium glass. | D0IEU |
| Prizma 3D Biocrown (Makertech Labs) |
UDMA > 40%; other methacrylated monomers > 20%; TPO <3%; Mixed Silanized Zirconia Oxide <10%; other filler particles (silanized silicas, nano, and micro barium glass) <25%; Pigments <2%; Blockers, stabilizers, and coactivators <2%. | 209623 |
| Mean (Standard deviation) | IC95% | ||||
| Lower Bound | Upper Bound | ƞ2 parcial | |||
| Flexural Strength (Mpa) | CT | 103.26 (13.84)A | 93.35 | 113.16 | 0.386 |
| BC0 | 91.46 (7.83)B | 85.86 | 97.06 | ||
| BC45 | 87.83 (5,56)B | 83.85 | 91.81 | ||
| BC90 | 86.03 (5.89)B | 81.81 | 90.24 | ||
| Surface roughness (µm) | CT | 0.12 (0.02)A | 0.10 | 0.13 | |
| BC0 | 0.13 (0.04)A | 0.10 | 0.17 | ||
| BC45 | 0.10 (0.02)A | 0.09 | 0.12 | ||
| BC90 | 0.12 (0.05)A | 0.08 | 0.16 | ||
| Microhardness (VHN) | CT | 71.93 (2.51)A | 70.13 | 73.73 | |
| BC0 | 15.97 (1.68)B | 14.77 | 17.18 | 0.995 | |
| BC45 | 16.15 (1.55)B | 15.04 | 17.26 | ||
| BC90 | 18.89 (1.51)C | 17.80 | 19.98 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





