Submitted:
26 June 2024
Posted:
27 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
2.1. Isolation of B. cereus Group Strains
2.2. MALDI-TOF Mass Spectrometry (MS) Analysis
2.3. WGS Analysis
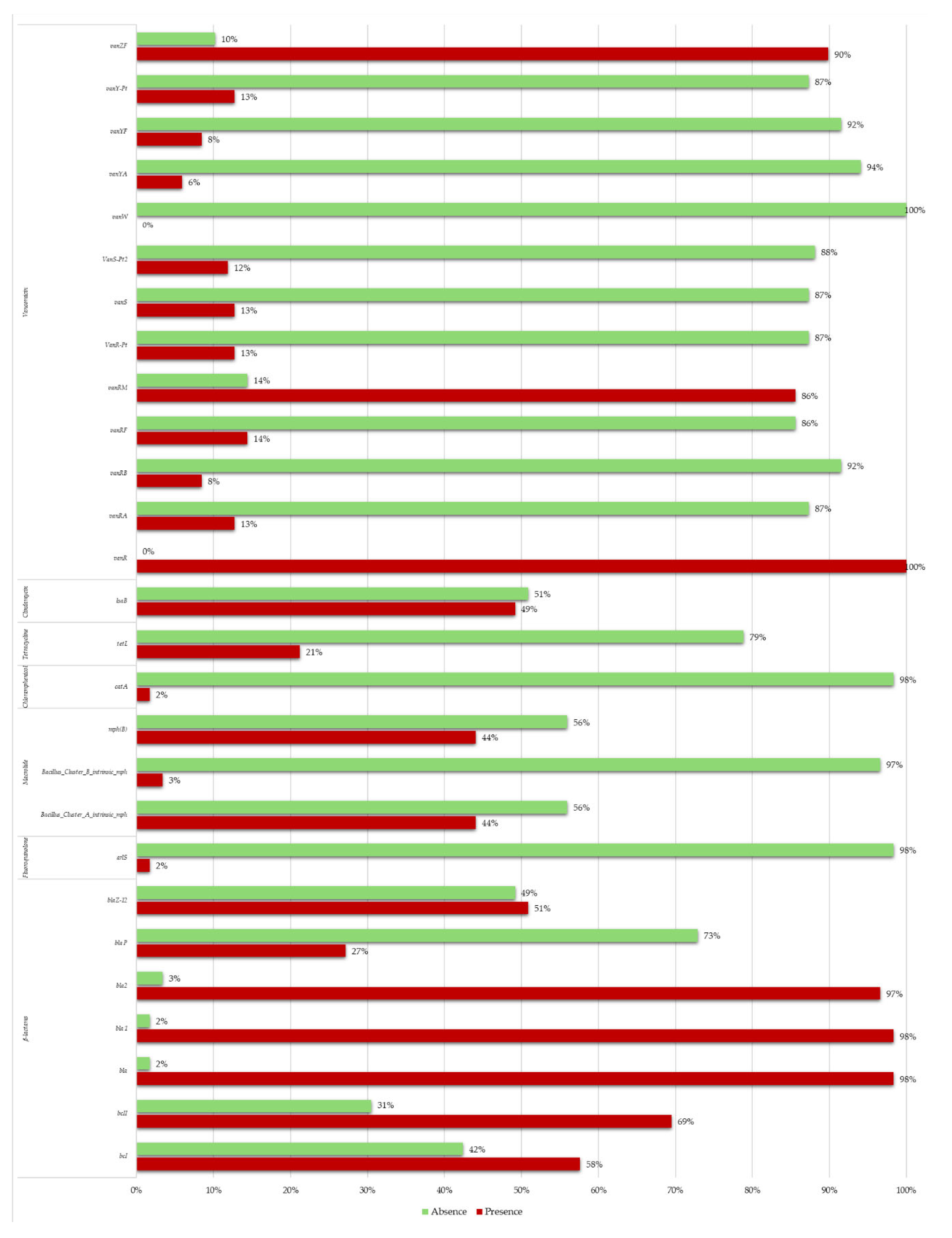
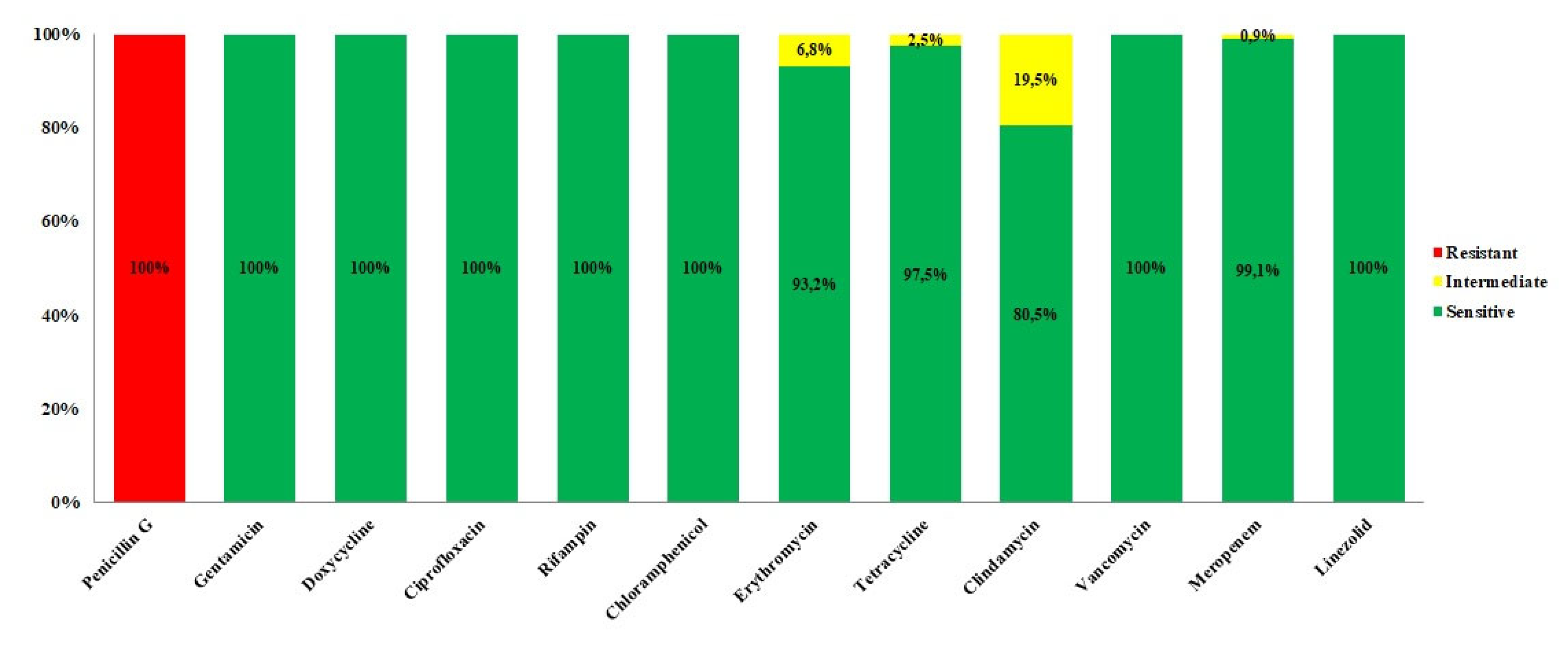
2.4. Antibiotic Susceptibility Analysis
3. Discussion
4. Materials and Methods
4.1. B. cereus Group Isolated Strains
4.2. MALDI-TOF Mass Spectrometry Analysis
4.3. WGS Sequencing and Bioinformatic Analyses
4.4. Antimicrobial Susceptibility Tests
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Drobniewski, F.A. Bacillus cereus and related species. Clin Microbiol Rev. 1993 Oct;6:324-38. [CrossRef]
- Ehling-Schulz, M.; Koehler, T.M.; Lereclus, D. The Bacillus cereus Group: Bacillus species with Pathogenic Potential. Microbiol Spectr 2019, 7. [CrossRef]
- El-Arabi, T.F.; Griffiths, M.W. Bacillus cereus. In: Morris JG, Potter ME. Foodborne infections and intoxications, 4th ed. Academic Press – Elsevier, 2013, pp: 401-407.
- Tirloni, E.; Stella, S.; Celandroni, F.; Mazzantini, D.; Bernardi, C.; Ghelardi, E. Bacillus Cereus in Dairy Products and Production Plants. Foods 2022, 11 (17), 2572. [CrossRef]
- Abee, T.; Groot, M. N.; Tempelaars, M.; Zwietering, M.; Moezelaar, R.; Voort, M. van der. Germination and Outgrowth of Spores of Bacillus Cereus Group Members: Diversity and Role of Germinant Receptors. Food Microbiology 2011, 28 (2), 199–208. [CrossRef]
- Logan, N.A. Bacillus and relatives in foodborne illness. Journal of Applied Microbiology, 2012, 112: 417-429. [CrossRef]
- Majed, R.; Faille, C.; Kallassy, M.; Gohar, M. Bacillus cereus Biofilms — Same, Only Different. Front. Microbiol. 2016, 7, 1054. [CrossRef]
- Ceuppens, S., Boon, N., Uyttendaele, M. Diversity of Bacillus cereus group strains is reflected in their broad range of pathogenicity and diverse ecological lifestyles. FEMS microbiology ecology, 2013, 84, 433–450. [CrossRef]
- Ikeda, M.; Yagihara, Y.; Tatsuno, K.; Okazaki, M.; Okugawa, S.; Moriya, K. Clinical characteristics and antimicrobial susceptibility of Bacillus cereus blood stream infections. Ann. Clin. Microbiol. Antimicrob., 2015, 14:43. [CrossRef]
- Rasko, D.A.; Altherr, M.R.; Han, S.C.; Ravel, J. Genomics of the Bacillus cereus group of organisms. FEMS Microbiology Reviews. 2005, 29 303–329. [CrossRef]
- Senesi, S; Ghelardi, E. Production, Secretion and Biological Activity of Bacillus cereus Enterotoxins. Toxins 2010,2, 1690-1703; [CrossRef]
- Bottone, E.J. Bacillus cereus, a Volatile Human Pathogen. Clinical Microbiology Reviews, 2010, 382–398 Vol. 23, No. 2 0893-8512/10/$12.00. [CrossRef]
- Dietrich, R.; Jessberger, N.; Ehling-Schulz, M.; Märtlbauer, E.; Granum, P.E. The Food Poisoning Toxins of Bacillus cereus. Toxins 2021, 13, 98. [CrossRef]
- Celandroni, F.; Salvetti, S.; Senesi, S.; Ghelardi, E. Bacillus Thuringiensis Membrane-Damaging Toxins Acting on Mammalian Cells. FEMS Microbiol Lett 2014, 361 (2), 95–103. [CrossRef]
- Guérin, A.; Rønning, H. T.; Dargaignaratz, C.; Clavel, T.; Broussolle, V.; Mahillon, J.; Granum, P. E.; Nguyen-The, C. Cereulide Production by Bacillus Weihenstephanensis Strains during Growth at Different PH Values and Temperatures. Food Microbiology 2017, 65, 130–135. [CrossRef]
- Miller, R.A.; Beno, S.M.; Kent, D.J.; Carroll, L.M.; Martin, N.H.; Boor, K.J.; Kovac, J. Bacillus Wiedmannii Sp. Nov., a Psychrotolerant and Cytotoxic Bacillus Cereus Group Species Isolated from Dairy Foods and Dairy Environments. Int J Syst Evol Microbiol 2016, 66 (11),4744–4753. [CrossRef]
- Yuan, J.; Li, Y.-Y.; Xu, Y.; Sun, B.-J.; Shao, J.; Zhang, D.; Li, K.; Fan, D.-D.; Xue, Z.-B.; Chen, W.-H.; Pak, C.; Lou, Y.-L.; Su, J.-Z.; Zheng, M.-Q. Molecular Signatures Related to the Virulence of Bacillus Cereus Sensu Lato, a Leading Cause of Devastating Endophthalmitis. mSystems 2019, 4 (6), e00745-19. [CrossRef]
- EFSA BIOHAZ Panel (EFSA Panel on Biological Hazards). Scientific opinion on the risks for public health related to the presence of Bacillus cereus and other Bacillus spp. including Bacillus thuringiensis in foodstuffs. EFSA Journal 2016; 14:4524, 93 pp. [CrossRef]
- Shawish, R.; Tarabees, R. Prevalence and antimicrobial resistance of Bacillus cereus isolated from beef products in Egypt. Open Vet J. 2017;7:337-341. [CrossRef]
- Granum, P.E.; Lund, T. Bacillus cereus and its food poisoning toxins, FEMS Microbiology Letters. 1997, Volume 157, Issue 2, Pages 223–228. [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: part 1: causes and threats. P & T: a peer-reviewed journal for formulary management 2015, 40(4), 277–283.
- Salam, M.A.; Al-Amin, M.Y.; Salam, M.T.; Pawar, J.S.; Akhter, N.; Rabaan, A.A.; Alqumber, M.A.A. Antimicrobial Resistance: A Growing Serious Threat for Global Public Health. Healthcare (Basel). 2023;11(13):1946. [CrossRef]
- Turnbull, P.C.; Sirianni, N.M.; LeBron, C.I.; Samaan, M.N.; Sutton, F.N.; Reyes, A.E.; Peruski, L.F.Jr. MICs of selected antibiotics for Bacillus anthracis, Bacillus cereus, Bacillus thuringiensis, and Bacillus mycoides from a range of clinical and environmental sources as determined by the Etest. J Clin Microbiol. 2004 Aug;42(8):3626-34. [CrossRef]
- Ghelardi, E.; Celandroni, F.; Salvetti, S.; Fiscarelli, E.; Senesi, S. Bacillus thuringiensis pulmonary infection: critical role for bacterial membrane-damaging toxins and host neutrophils. Microbes Infect. 2007;9(5):591-8. [CrossRef]
- Roca, A.; Cabeo, M.; Enguidanos, C.; Martínez-Checa, F.; Sampedro, I.; Llamas, I. Potential of the quorum-quenching and plant-growth promoting halotolerant Bacillus toyonensis AA1EC1 as biocontrol agent. Microb Biotechnol. 2024;17(3):e14420. [CrossRef]
- Andriūnaitė, E.; Tamošiūnė. I; Aleksandravičiūtė, M.; Gelvonauskienė, D.; Vinskienė, J.; Rugienius, R.; Baniulis, D. Stimulation of Nicotiana tabacum L. In Vitro Shoot Growth by Endophytic Bacillus cereus Group Bacteria. Microorganisms. 2021;9(9):1893. [CrossRef]
- Hollensteiner, J.; Wemheuer, F.; Harting, R.; Kolarzyk, A.M.; Diaz, Valerio S.M.; Poehlein, A.; Brzuszkiewicz, E.B.; Nesemann, K.; Braus-Stromeyer, S.A.; Braus, G.H.; Daniel, R.; Liesegang, H. Bacillus thuringiensis and Bacillus weihenstephanensis Inhibit the Growth of Phytopathogenic Verticillium Species. Front Microbiol. 2017 Jan 18;7:2171. [CrossRef]
- Hinnekens, P.; Fayad, N.; Gillis, A.; Mahillon, J. Conjugation across Bacillus cereus and kin: A review. Front Microbiol. 2022 Nov 4;13:1034440. [CrossRef]
- Jian, Z.; Zeng, L.; Xu, T.; Sun, S.; Yan, S.; Yang, L.; Huang, Y.; Jia, J.; Dou, T. Antibiotic Resistance Genes in Bacteria: Occurrence, Spread, and Control. J Basic Microbiol 2021, 61 (12), 1049–1070. [CrossRef]
- Bianco, A.; Capozzi, L.; Monno, M.R.; Del Sambro, L.; Manzulli, V.; Pesole, G.; Loconsole, D.; Parisi, A. Characterization of Bacillus cereus Group Isolates from Human Bacteremia by Whole-Genome Sequencing. Front Microbiol. 2021 Jan 12;11:599524. [CrossRef]
- Zhai, Z.; Cui, C.; Li ,X.; Yan, J.; Sun, E.; Wang, C.; Guo, H.; Hao, Y. Prevalence, antimicrobial susceptibility, and antibiotic resistance gene transfer of Bacillus strains isolated from pasteurized milk. J Dairy Sci. 2023;106(1):75-83. [CrossRef]
- Bartoszewicz, M. and Czyżewska, U. Comparison of the antibiotic resistance between genetically diverse and toxigenic Bacillus cereus sensu lato from milk, pepper and natural habitats. J Appl Microbiol. 2021;130(2):370-381. [CrossRef]
- Mills, E.; Sullivan, E.; Kovac, J. Comparative Analysis of Bacillus cereus Group Isolates' Resistance Using Disk Diffusion and Broth Microdilution and the Correlation between Antimicrobial Resistance Phenotypes and Genotypes. Appl Environ Microbiol. 2022;88(6):e0230221. [CrossRef]
- Fiedler, G.; Schneider, C.; Igbinosa, E. O.; Kabisch, J.; Brinks, E.; Becker, B.; Stoll, D. A.; Cho, G.-S.; Huch, M.; Franz, C. M. A. P. Antibiotics Resistance and Toxin Profiles of Bacillus Cereus-Group Isolates from Fresh Vegetables from German Retail Markets. BMC Microbiol. 2019;19(1):250. [CrossRef]
- Yim, J.-H.; Kim, K.-Y.; Chon, J.-W.; Kim, D.-H.; Kim, H.-S.; Choi, D.-S.; Choi, I.-S.; Seo, K.-H. Incidence, Antibiotic Susceptibility, and Toxin Profiles of Bacillus Cereus Sensu Lato Isolated from Korean Fermented Soybean Products. Journal of food science 2015, 80. [CrossRef]
- Nicoletti, G.; Russo, G.; Bonfiglio, G. Recent Developments in Carbapenems. Expert Opinion on Investigational Drugs 2002, 11 (4), 529–544. [CrossRef]
- Materon, I.C.; Queenan, A.M.; Koehler, T.M.; Bush, K.; Palzkill, T. Biochemical characterization of beta-lactamases Bla1 and Bla2 from Bacillus anthracis. Antimicrob Agents Chemother. 2003;47(6):2040-2. [CrossRef]
- Wagner, T.M.; Howden, B.P.; Sundsfjord, A.; Hegstad, K. Transiently silent acquired antimicrobial resistance: an emerging challenge in susceptibility testing. J Antimicrob Chemother. 2023;78(3):586-598. [CrossRef]
- Deekshit, V.K.; Srikumar, S. 'To be, or not to be'-The dilemma of 'silent' antimicrobial resistance genes in bacteria. J Appl Microbiol. 2022;133(5):2902-2914. [CrossRef]
- Stasiak, M.; Maćkiw, E.; Kowalska, J.; Kucharek, K.; Postupolski, J. Silent Genes: Antimicrobial Resistance and Antibiotic Production. Pol J Microbiol. 2021;70(4):421-429. [CrossRef]
- Bravo, A.; Moreno-Blanco, A.; Espinosa, M. One Earth: The Equilibrium between the Human and the Bacterial Worlds. Int J Mol Sci. 2023;24(20):15047. [CrossRef]
- Manzulli, V.; Rondinone, V.; Buchicchio, A.; Serrecchia, L.; Cipolletta, D.; Fasanella, A.; Parisi, A.; Difato, L.; Iatarola, M.; Aceti, A.; Poppa, E.; Tolve, F.; Pace, L.; Petruzzi, F.; Rovere, I.D.; Raele, D.A.; Del Sambro, L.; Giangrossi, L.; Galante, D. Discrimination of Bacillus cereus Group Members by MALDI-TOF Mass Spectrometry. Microorganisms. 2021 Jun 2;9(6):1202. [CrossRef]
- Bolger, A.M., Lohse, M., Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 2014,30, 2114–2120. [CrossRef]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol. 2012 ;19(5):455-77. [CrossRef]
- Carroll, L.M.; Kovac, J.; Miller, R.A.; Wiedmann, M. Rapid, High-throughput identification of anthrax-causing and emetic Bacillus cereus group genome assemblies via BTyper, a computational tool for virulence-based classification of Bacillus cereus group isolates by using nucleotide sequencing data. Appl. Environ. Microbiol. 2017, 83:e1096-17. [CrossRef]
- Gupta, S.K.; Padmanabhan, B.R.; Diene, S.M.; Lopez-Rojas, R.; Kempf, M.; Landraud, L.; et al. ARG-ANNOT, a new bioinformatic tool to discover antibiotic resistance genes in bacterial genomes. Antimicrob. Agents Chemother. 2014, 58, 212–220. [CrossRef]
- Feldgarden, M.; Brover, V.; Haft, D.H.; Prasad, A.B.; Slotta, D.J.; Tolstoy, I., et al. Validating the AMRFinder tool and resistance gene database by using antimicrobial resistance genotype-phenotype correlations in a collection of isolates. Antimicrob. Agents Chemother. 2019,63:e483-19. [CrossRef]
- Jia, B.; Raphenya, A.R.; Alcock, B.; Waglechner, N.; Guo, P.; Tsang, K.K., et al. CARD 2017: expansion and model-centric curation of the comprehensive antibiotic resistance database. Nucleic Acids Res. 2017,45,D566–D573. [CrossRef]
- Zankari, E.; Hasman, H.; Cosentino, S.; Vestergaard, M.; Rasmussen, S.; Lund, O.; et al. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 2012, 67, 2640–2644. [CrossRef]
- Carattoli, A.; Zankari, E.; García-Fernández, A.; Larsen, M.V.; Lund, O.; Villa, L.; et al. In silico detection and typing of plasmids using plasmidfinder and plasmid multilocus sequence typing. Antimicrob. Agents Chemother. 2014, 58, 3895–3903. [CrossRef]
- Clinical and Laboratory Standards Institute. Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria. CLSI Guideline M45. 2016, 3rd ed. Wayne: CLSI.
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. CLSI Supplement M100. 2017, 27th ed. Wayne: CLSI.
- Glasset, B.; Herbin, S.; Guillier, L.; Cadel-Six, S.; Vignaud, M.L.; Grout, J.; Pairaud, S.; Michel, V.; Hennekinne, J.A.; Ramarao, N.; Brisabois, A. Bacillus cereus-induced food-borne outbreaks in France; 2007 to 2014: epidemiology and genetic characterisation. Euro Surveill. 2016;21(48):30413. [CrossRef]
- Kotiranta, A.; Lounatmaa, K.; Haapasalo, M. Epidemiology and pathogenesis of Bacillus cereus infections. Microbes Infect. 2000;2(2):189-98. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




