Submitted:
26 June 2024
Posted:
27 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
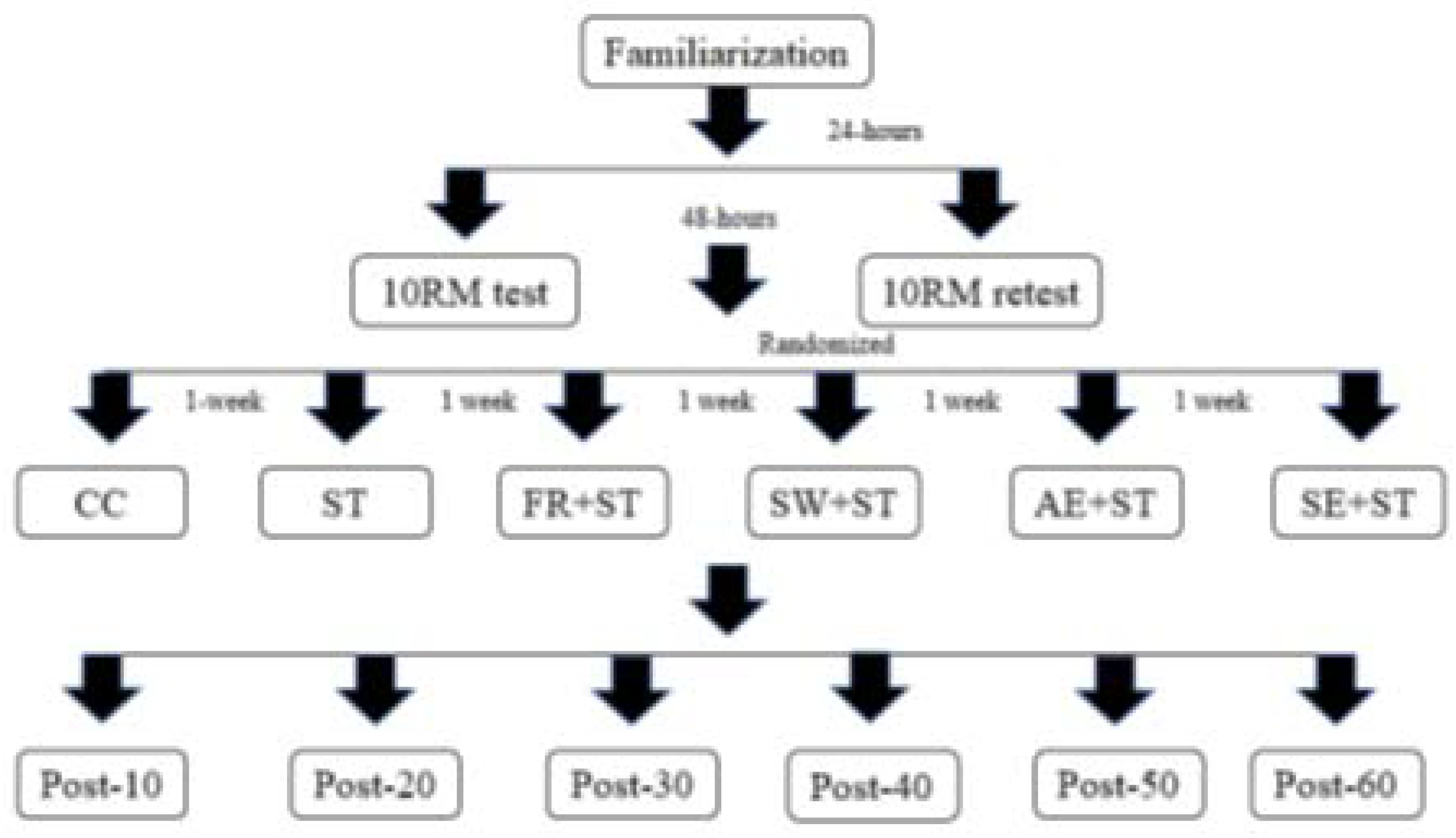
2. Materials and Methods
2.1. Ethical Considerations
2.2. Participants
2.3. Procedure
2.4. Load Test
2.5. Instruments
2.6. Measures
2.7. Statistical Analyses
3. Results
3.1. Muscle Performance
3.1.1. Total Training Volume
3.2. Maximum Repetition Performance
3.3. Fatigue Index
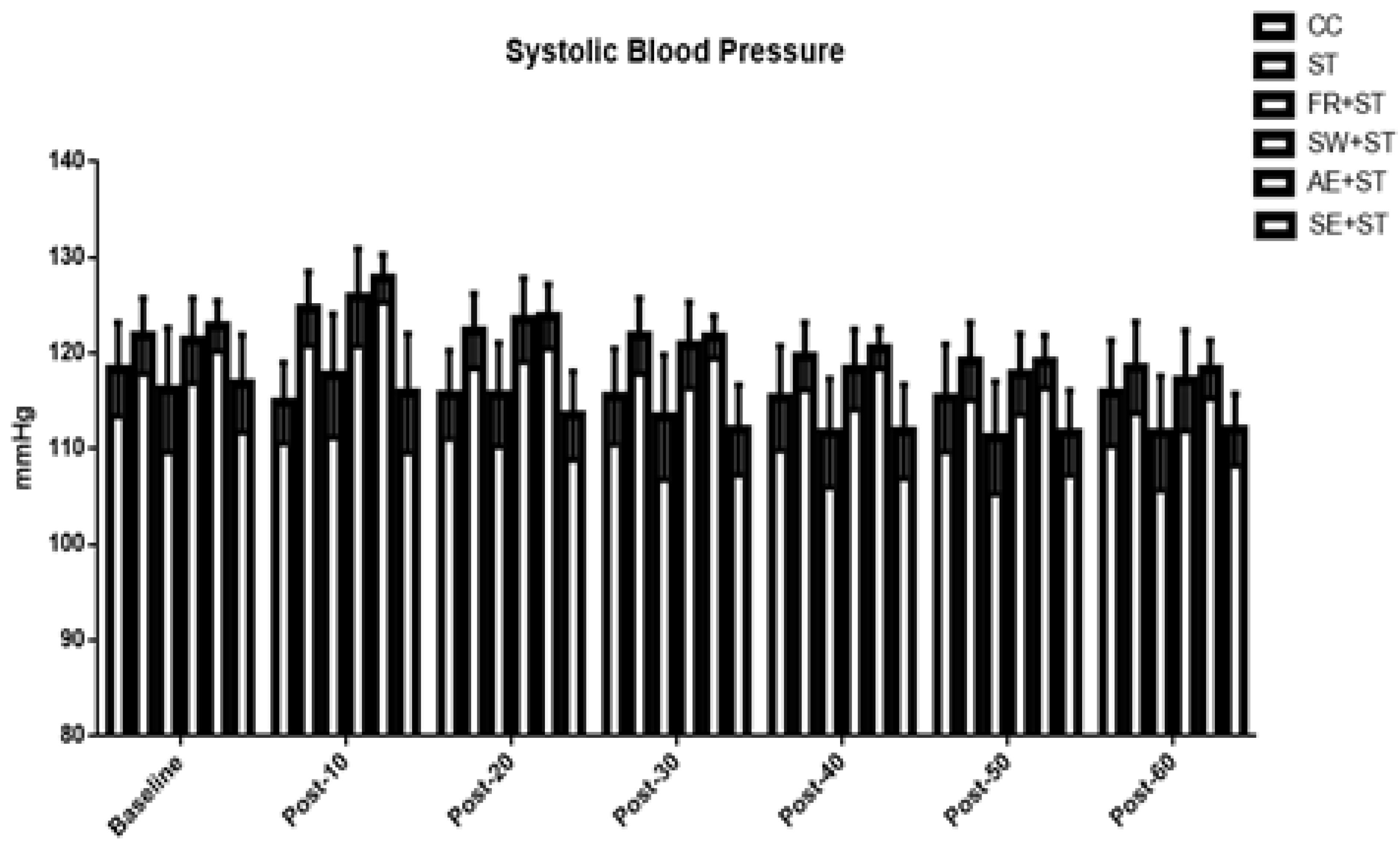
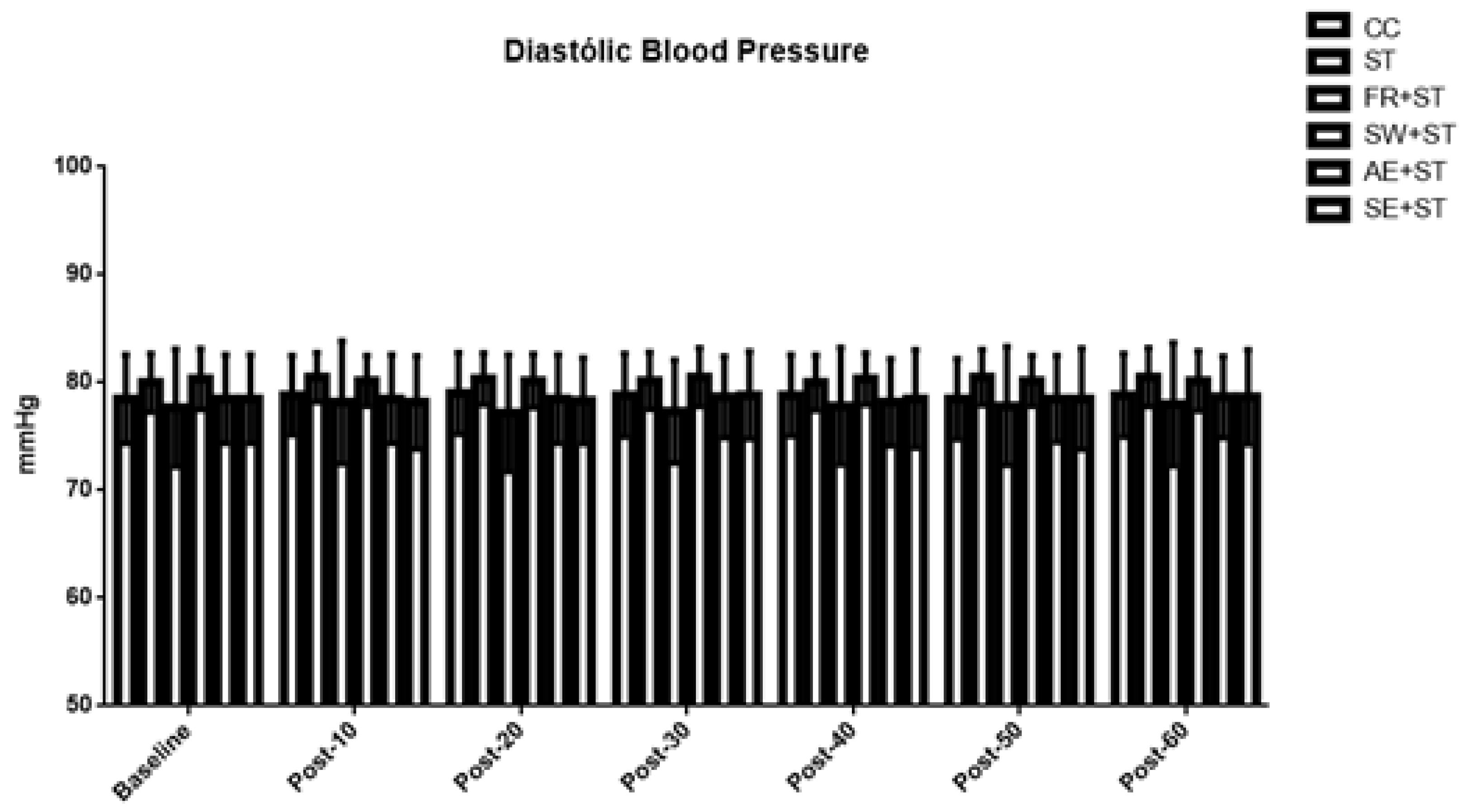
3.4. Blood Pressure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- American College of Sports Medicine Position Stand. Quantity and quality of exercise for developing and maintain cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sport Exerc 2011, 43, 1334-1359.
- Thompson, W. R. Worldwide survey of fitness trends for 2023. ACM’s. Health & Fitness Journal 2023, 26, 11-20.
- Da Silva Telles, L. G. , Carelli, L. C., Bráz, I. D., Junqueira, C. J., Monteiro, E. R., Reis, V. M., et al. Effects of ischemic preprotocoling as a warm-up on leg press and bench press performance. J Hum Kinet 2020, 75, 267-277.
- Mills, K. T. , Stefanescu, He. J. The global epidemiology of hypertension. Nat Rev Nephrol 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Schiffrin, E. L. Immune mechanisms in hypertension and vascular injury. Clin Sci (Lond) 2014, 126, 267–274. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, H. V., Johnson, B. T, Huedo-Medina, T. B., Livingston, J., Forsyth, K. C., Kraemer, W. J, et al. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: a meta-analysis. J Am Heart Assoc 2016, 5, e003231.
- Pescatello, L. S., Buchner, D. M., Jakicic, J. M., Powell, K. E., Kraus, W. E., Bloodgood, B., et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc 2019, 51, 1314-1323.
- Okamoto, T., Masuhara, M., Ikuta, K. Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res 2014, 28, 69-73.
- Hotfiel, T. , Swoboda, B., Krinner, S., Grim, C., Engelhardt, M., Uder, M., et al. Acute effects of lateral thigh foam rolling on arterial tissue perfusion determined by spectral doppler and power doppler ultrasound. J Strength Cond Res 2017, 31, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Araújo, G. , Behm, D. G., Monteiro, E. R., Fiuza, A. G. F. deM., Gomes, T. M., Vianna, J. M., et al. Order effects of resistance and stretching exercises on heart rate variability and blood pressure in healthy adults. J Strength Cond Res 2018, 33, 2684–2693. [Google Scholar] [CrossRef] [PubMed]
- Spranger, M. D., Krishnan, A. C., Levi, P. D., O’leary, D. S., Smith, S. A. Blood flow restriction training and the exercise pressor reflex: a call for concern. Am J Physiol Heart Circ Physiol 2015, 309, H1440–H1452.
- Sidhu, S. K. , Weavil, J. C., Rossman, M. J., Jessop, J. E., Bledsoe, A. D., Buys, M. J., et al. Exercise Pressor Reflex Contributes to the Cardiovascular Abnormalities Characterizing Hypertensive Humans During Exercise. Hypertension 2019, 74, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Brasileiro-Santos, M. S., Santos, A. C. Neural mechanisms and post-exercise hypotension: The importance of experimental studies. Motriz 2017, 23, e101622.
- Halliwill, J. R. Mechanisms and Clinical Implications of Post-exercise Hypotension in Humans. Exerc Sport Sci Rev 2001, 29, 65–70. [Google Scholar] [PubMed]
- Beck, T. W. The importance of a priori sample size estimation in strength and conditioning research. J Strength Cond Res 2013, 27, 2323–2337. [Google Scholar] [CrossRef] [PubMed]
- Faul, F. , Erdfelder, E., Lang, A. G., Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Zahiri, A. , Alizadeh, S., Daneshjoo, A., Pike, N., Konrad, A., Behm, D. G. Core muscle activation with foam rolling and static planks. Frontiers in Physiology 2022, 13, 852094. [Google Scholar] [CrossRef]
- Fermino, R. C. , Winiarski, Z. H., Da Rosa, R. J., Lorenci, L. G., Buso, S., Simão, R. Influence of the specific warm-up and stretching in the performance of the muscular force in 10 maximum repetitions. Rev Bras Cie e Mov, 2005, 13, 25-32.
- Parameswarppa, S. B. , Narayana, J. Impact of noise hearing and hypertension among works in steel industry. Int J Curr Microbiol App Sci 2015, 4, 124–133. [Google Scholar]
- Becker, B. Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology 1988, 41, 257–278. [Google Scholar] [CrossRef]
- Morris, S. B. Estimating effect sizes from pretest-posttest-control group designs. Organizational Research Methods 2007, 11, 364–386. [Google Scholar] [CrossRef]
- Smith Lindsey, J. Wolff and Beretvas, S. Natasha (2009) “Estimation of the standardized mean difference for repeated measures designs,” Journal of Modern Applied Statistical Methods: Vol.8: Iss. 2, Article 27.
- Monteiro, E. R. , Costa, P. B., Corrêa Neto, V. G., Hoogenboom, B. J., Steele, J., Silva Novaes, J. D. Posterior Thigh Foam Rolling Increases Knee Extension Fatigue and Passive Shoulder Range-of-Motion. J Strength Cond Res, 2019, 33, 987-994.
- Halperin, I. , Copithorne, D., Behm, D. G. Unilateral isometric muscle fatigue decreases force production and activation of contralateral knee extensors but not elbow flexors. Appl Physiol Nutr Metab 2014, 39, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Halperin, I. , Chapman, D. W., Behm, D. G. Non-local muscle fatigue: effects and possible mechanisms. Eur J Appl Physiol 2015, 115, 2031–2048. [Google Scholar] [CrossRef] [PubMed]
- Behm, D. G. , Alizadeh, S., Hadjizedah Anvar, S., Hanlon, C., Ramsay, E., Mahmoud, M. M. I., et al. Non-local muscle fatigue effects on muscle strength, power, and endurance in healthy individuals: A systematic review with meta-analysis. Sports Med, 2021, 51, 1893-1907. [CrossRef]
- Aboodarda, S. J. , Copithorne, D. B., Power, K. E., Drinkwater, E., Behm, G. Excitability of the knee extensors. Appl Physiol Nutr Metab, 2015, 40, 924-930.
- Šambaher, N. , Aboodarda, S. J., Behm, D. G. Bilateral knee extensor fatigue modulates force and responsiveness of the corticospinal path-way in the non-fatigued, dominant elbow flexors. Front Hum Neurosci, 2016, 10, 18-24.
- Aboodarda, S. J. , Šambaher, N., Millet, Gy., Behm, D. G. Knee extensors neuromuscular fatigue changes the corticospinal pathway excitability in biceps brachii muscle. Neuroscience 2017, 340, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Behm, D. G. , Button, D. C., Barbour, G., Butt, J. C., Young, W. B. Conflicting effects of fatigue and potentiation on voluntary force. J Strength Cond Res 2004, 18, 365–372. [Google Scholar] [PubMed]
- Santana, H. G. , Lara, B., da Silva, F. C. A., Eiras, P. M., Paz, G. A., Willardson, J. M., et al. Total training volume and muscle soreness parameters performing agonist or antagonist foam rolling between sets. Sports, 2021, 9, 57.
- Rubini, E. C. , Costa, A. L., Gomes, P. S. The Effects of Stretching on Strength Performance. Sports Med 2007, 37, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Atherton, P. J. , Babraj, J., Smith, K., Singh, J., Rennie, M. J., Wackerhage, H. Selective activation of AMPK-PGC-1alpha or PKB-TSC2-mTOR signaling can explain specific adaptive responses to endurance or resistance training-like electrical muscle stimulation. FASEB J, 2005, 19, 786-778.
- Ramadoss, R. , Stanzione, J. R., Volpe, S. L. A Comparison of Substrate Utilization Profiles During Maximal and Submaximal Exercise Tests in Athletes. Front Psychol 2022, 13, 854451. [Google Scholar] [CrossRef] [PubMed]
- Anthi, X. , Dimitrios, P., Christos, K. On the mechanisms of post-activation potentiation: the contribution of neural factors. Journal of Physical Education and Sport, 2014, 14, 134-137.
- Figueiredo, T. , Rhea, M. R., Peterson, M., Miranda, H., Bentes, C. M., Reis, V. M. R., et al. Influence of number of sets on blood pressure and heart rate variability after a strength training session. J Strength Cond Res 2015, 29, 1556–1563. [Google Scholar] [CrossRef]
- MacDougall, J. D. , Tuxen, D., Sale, D. G., Moroz, J. R., Sutton, J. R. Arterial blood pressure response to heavy resistance exercise. J Appl Physiol 1985, 58, 785–790. [Google Scholar] [CrossRef]
- Monteiro, E. R. , Vingren, J. L., Pescatello, L. S., Corrêa Neto, V. G., Brown, A. F., Kingsley, J. D, et al. Effects of foam rolling and strength training on post exercise hypotension in normotensive women: A cross-over study. J Bodyw Mov Ther, 2023, 34, 81-86.
- Liao, I. C. , Chen, S. L., Wang, M. Y., Tsai, P. S. Effects of massage on blood pressure in patients with hypertension and prehypertension: a meta-analysis of randomized controlled trials. J Cardiovasc Nurs, 2016, 31, 73-83.
- White, D. W. , Raven, P. B. Autonomic neural control of heart rate during dynamic exercise: Revisited. J Physiol, 2014, 592, 2491-2500.
- Farinatti, P. , Polito, M. D., Massaferri, R., Monteiro, W. D., Vasconcelos, D., Johson, B. T., et al. Postexercise hypotension due to resistance exercise is not mediated by autonomic control: a systematic review an meta-analysis. Autonomic Neuroscience, 2021, 234, 102825.
- Forjaz, C. L. deM., Santaella, D. F., Rezende, L. O., Barretto, A. C. P., Negrão, C. E. Exercise duration determines the magnitude and duration of post-exercise hypotension. Arquivos Brasileiros de Cardiologia, 1998, 70, 99-104.
- Inami, T. , Bara, R., Nakagari, A., Shimizu, T. Acute changes in peripheral vascular tonus and systemic circulation during static stretching. Res Sports Med 2015, 23, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Kruse, N. T. , Scheuermann, B. W. Cardiovascular responses to skeletal muscle stretching: “stretching” the truth or a new exercise paradigm for cardiovascular medicine? Sports Med 2017, 47, 2507–2520. [Google Scholar] [CrossRef] [PubMed]
- Esformes, J. L. , Norman, F., Sigley, J., Birch, K. M. The influence of menstrual cycle phase upon postexercise hypotension. Med Sci Sports Exerc 2006, 38, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, A. C. C. , Rezk, C. C., Teixeira, L., Tinucci, T., Mion, D., Forjaz, C. L. M. Gender influence on post-resistance exercise hypotension and hemodynamics. Int J Sports Med, 2013, 34, 939-944.
| Variable | Mean ± SD |
|---|---|
| Bench Press 10RM Test (kg) | 36.33 ± 3.98 |
| Bench Press 10RM Retest (kg) | 36.17 ± 3.46 |
| Bench Press 10RM ICC | 0.824 (CV% = 12.23) |
| Back Squat 10RM Test (kg) | 59.33 ± 10.49 |
| Back Squat 10RM Retest (kg) | 60.50 ± 13.35 |
| Back Squat 10RM ICC | 0.946 (CV% = 21.01) |
| Bench Press 45º 10RM Test (kg) | 34.00 ± 4.18 |
| Bench Press 45º 10RM Retest (kg) | 33.83 ± 3.01 |
| Bench Press 45º 10RM ICC | 0.555 (CV% = 13.68) |
| Front Squat 10RM Test (kg) | 44.83 ± 7.79 |
| Front Squat 10RM Retest (kg) | 43.33 ± 7.69 |
| Front Squat 10RM ICC | 0.861 (CV% = 19.98) |
| Lat Pull-Down 10RM Test (kg) | 42.92 ± 8.38 |
| Lat Pull-Down 10RM Retest (kg) | 41.6 ± 6.85 |
| Lat Pull-Down 10RM ICC | 0.908 (CV% = 8.37) |
| Leg Press 10RM Test (kg) | 233.33 ± 47.67 |
| Leg Press 10RM Retest (kg) | 231.67 ± 36.64 |
| Leg Press 10RM ICC | 0.9230 (CV% = 13.11) |
| Shoulder Press 10RM Test (kg) | 35.42 ± 4.75 |
| Shoulder Press 10RM Retest (kg) | 35.83 ± 5.47 |
| Shoulder Press 10RM ICC | 0.920 (CV% = 13.11) |
| Leg Extension 10RM Test (kg) | 80.83 ± 11.65 |
| Leg Extension 10RM Retest (kg) | 81.25 ± 10.69 |
| Leg Extension 10RM ICC | 0.972 (CV% = 13.17) |
| Protocols | ||||||
|---|---|---|---|---|---|---|
| Exercises | ST | FR+ST | SW+ST | AE+ST | SE+ST | |
| Bench Press | 2550 (2360 - 2895) | 2172 (2017 - 2403)* | 2172 (2080 – 2397.5)* | 2217 (2097.5 – 2719.5) | 2311 (2166 – 2420.5)* | |
| Back Squat | 3080 (2657.5 – 3227.5) | 2465 (2262.5 - 2860)* | 2530 (2257.5 - 3117.5)* | 2860 (2447.5 - 3090) | 2725 (2447.5 - 3142.5) | |
| Bench Press 45º | 2377.5 ± 374.97 | 1955 ± 258.77* | 2056.5 ± 354.9* | 2109.5 ± 2776* | 2165.33 ± 311.47# | |
| Front Squat | 2094 (1981-2447) | 1812 (1528,5 - 1963,5)* | 1902 (1685.5 – 2189.5)* | 1818 (1632 - 2136)* | 1877 (1692 - 2315.5)* | |
| Lat Pull-Down | 2347.5 (2191.25 – 2683.75) | 2017.5 (1780-2197.5)* | 2062.5 (1927.5 - 2307.5)* | 2210 (1940 - 2250)* | 2185 (1807.5 – 2362.5)* | |
| Leg Press | 6810 (5600-7995) | 5740 (4800 - 6945)* | 5720 (5010 - 6500)* | 5880 (5220 - 7210)* | 5740 (4800 - 6665)* | |
| Shoulder Press | 997.5 (976.25 – 1156.87) | 842.5 (743.75 – 1023.75)* | 880 (770 - 1035)* | 918.75 (813.75 – 1059.37)* | 915 (817.5 - 1050) | |
| Leg Extension | 2280 (2115-2485) | 1865 (1697.5 - 2160)* | 2007.5 (1760 – 2197.5)* | 2058.75 (1852.5 - 2295) | 1988.75 (1825-2360) | |
| Set 1 | Set 2 | Set 3 | FI (%) | |
|---|---|---|---|---|
| BENCH PRESS | ||||
| ST | 10 (9.25-10.75) | 10 (9-10.75) | 9 (9-10) | 90 (84.99-100) |
| FR+ST | 9 (8.25-10) | 8 (8-9)@ | 7 (6-8)*@ | 73.86 (63.54-86.66)@ |
| SW+ST | 9.5 (9-10) | 8 (7.25-8.5)#@ | 7.5 (7-8)*@ | 78.89 (70-86.66)@ |
| AE+ST | 9.5 (9-10) | 9 (8-9.75) | 8 (7-9)* | 85.35 (71.94-100) |
| SE+ST | 9 (9-10) | 8 (7.25-9)@ | 8 (7-9)* | 80 (77.78-100) |
| BACK SQUAT | ||||
| ST | 10 (9.25-10.75) | 9.5 (9-10) | 9 (9-10) | 90.45 (90-100) |
| FR+ST | 10 (9-10) | 8 (7-8.75)@ | 7 (5.25-7)*@ | 70 (60-77.78)@& |
| SW+ST | 9 (8-9.75) | 8 (7-9)@ | 7.5 (7-9)* | 87.5 (77.78-97.5) |
| AE+ST | 9 (9-10) | 9 (8-9) | 8 (7-9.75) | 88.19 (80-100) |
| SE+ST | 9.5 (9-10) | 9 (8.25-10) | 8 (7-8.75) | 80 (77.78-97.22) |
| BENCH PRESS 45º | ||||
| ST | 10 (9-10) | 10 (9-10) | 9.5 (9-10) | 95.45 (90-108.33) |
| FR+ST | 9 (8-10) | 8 (7.25-8.75)@ | 7 (6-7.75)*@ | 76.39 (71.25-80)@ |
| SW+ST | 9 (8-9.75) | 8 (8-9) | 7.5 (7-9)*@ | 88.19 (71.25-100) |
| AE+ST | 9 (9-10) | 8 (8-9) | 8 (7.25-9)* | 88.89 (80-100) |
| SE+ST | 9.5 (9-10) | 9 (8-10) | 8 (7-8.75) | 80 (77.78-97.22) |
| FRONT SQUAT | ||||
| ST | 10 (9.25-10.75) | 10 (9.25-10.75) | 9.5 (9-10) | 100 (83.86-107.5) |
| FR+ST | 9 (8.25-10) | 8 (7-9)@ | 7 (6-7)*@ | 72,5 (67.5-79.44)@ |
| SW+ST | 9 (9-10) | 8.5 (8-9) | 8 (7-8.75)*@ | 83.75 (77.78-90) |
| AE+ST | 9.5 (8.25-10) | 8 (7.25-9)@ | 7 (7-8)*@ | 78.89 (70-87.5)@ |
| SE+ST | 10 (9-10) | 95 (8-10.75) | 7.5 (7-8.75)*$@ | 78.89 (70-95)@ |
| LAT PULL-DOWN | ||||
| ST | 10 (9-10.75) | 10 (9-10) | 9 (9-10) | 100 (83.86-100) |
| FR+ST | 9.5 (9-10) | 8 (7.25-9)@ | 6.5 (6-7.75)*@ | 68.33 (56.67-79.44)@ |
| SW+ST | 9.5 (9-10) | 8.5 (8-9) | 7 (7-8)*@ | 78.89 (70-88.89) |
| AE+ST | 9.5 (9-10) | 8 (7.25-9)@ | 8 (7.25-9) | 88.19 (80-100) |
| SE+ST | 10 (9-10) | 8 (8-10) | 8 (7-8)*@ | 80 (77.78-95) |
| LEG PRESS | ||||
| ST | 10 (9-10) | 9.5 (9-10) | 9 (9-10) | 95 (90-111.11) |
| FR+ST | 9 (8.25-10) | 8 (8-8.75)@ | 7 (6.25-8)*@ | 77.78 (67.5-100) |
| SW+ST | 9 (9-10) | 8 (7.25-9) | 7 (7.25-8)*@ | 78.89 (71.25-85.62)@ |
| AE+ST | 9.5 (9-10) | 8 (7.25-9) | 8 (7-8)*@ | 80 (77.78-100) |
| SE+ST | 9 (9-10) | 8 (7-8.75)@ | 7.5 (7-8)*@ | 83.75 (71.94-88.89)@ |
| SHOULDER PRESS | ||||
| ST | 10 (9-10) | 9 (9-10) | 9 (9-10) | 100 (90-100) |
| FR+ST | 9 (8.25-10) | 8 (7-8)@ | 7.5 (6-8)*@ | 80 (66.67-88.54)@ |
| SW+ST | 9 (9-10) | 8 (7-8.75)# | 7 (7-8)*@ | 78.89 (70-89.72) |
| AE+ST | 9.5 (9-10) | 8 (7.25-9) | 7 (7-8.75)*@ | 77.78 (70-100) |
| SE+ST | 9.5 (9-10) | 9 (7.25-10) | 7.5 (7-9.5)* | 78.89 (75.69-100) |
| LEG EXTENSION | ||||
| ST | 10 (9-10) | 10 (9-10) | 9.5 (9-10) | 100 (92.5-100) |
| FR+ST | 9 (8-10) | 8 (7-8)@ | 7 (6-8)*@ | 82.85 (70-97.22)@ |
| SW+ST | 9 (8.25-10) | 8 (7-9)@ | 7 (7-8)*@ | 80 (70-88.54)@ |
| AE+ST | 9 (9-10) | 8.5 (7.25-9) | 8 (7-8)*@ | 80 (77.78-97.22) |
| SE+ST | 9.5 (9-10) | 8 (7.25-10) | 8 (7-8)*@ | 80 (75.69-88.89)@ |
| Protocol | Post-10 | Post-20 | Post-30 | Post-40 | Post-50 | Post-60 |
|---|---|---|---|---|---|---|
| Systolic Blood Pressure | ||||||
| CC | -0.76 (Medium) | -0.56 (Medium) | -0.57 (Medium) | -0.58 (Medium) | -0.57 (Medium) | -0.48 (Small) |
| ST | 0.72 (Medium) | 0.12 (No Effect) | 0.00 (No Effect) | -0.57 (Medium) | -0.66(Medium) | -0.76 (Medium) |
| FR+ST | 0.23 (Small) | -0.08 (No Effect) | -0.43 (Small) | -0.73 (Medium) | -0.80 (Large) | -0.72 (Medium) |
| SW+ST | 0.94 (Large) | 0.49 (Small) | -0.11 (No Effect) | -0.69 (Medium) | -0.80 (Large) | -0.85 (Large) |
| AE+ST | 1.96 (Large) | 0.33 (Small) | -0.47 (Small) | -0.98 (Large) | -1.30 (Large) | -1.42 (Large) |
| SE+ST | -0.17 (No Effect) | -0.68 (Medium) | -0.99 (Large) | -1.00 (Large) | -1.08 (Large) | -1.09 (Large) |
| Diastolic Blood Pressure | ||||||
| CC | 0.08 (No Effect) | 0.12 (No Effect) | 0.08 (No Effect) | 0.08 (No Effect) | 0.00 (No Effect) | 0.08 (No Effect) |
| ST | 0.20 (Small) | 0.12 (No Effect) | 0.06 (No Effect) | 0.00 (No Effect) | 0.18 (No Effect) | 0.18 (No Effect) |
| FR+ST | 0.08 (No Effect) | -0.09 (No Effect) | -0.06 (No Effect) | 0.02 (No Effect) | 0.02 (No Effect) | 0.05 (No Effect) |
| SW+ST | -0.06 (No Effect) | -0.06 (No Effect) | 0.06 (No Effect) | 0.00 (No Effect) | -0.06 (No Effect) | -0.05 (No Effect) |
| AE+ST | 0.00 (No Effect) | 0.00 (No Effect) | 0.04 (No Effect) | -0.08 (No Effect) | 0.00 (No Effect) | 0.04 (No Effect) |
| SE+ST | -0.07 (No Effect) | -0.04 (No Effect) | 0.08 (No Effect) | 0.00 (No Effect) | 0.00 (No Effect) | 0.04 (No Effect) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





