Preprint
Article
Biomarker Profiling by Targeted Metabolomic Analysis of Plasma and Urine Samples in Type 2 Diabetes Mellitus Patients and Early Diabetic Kidney Disease
Altmetrics
Downloads
216
Views
69
Comments
0
A peer-reviewed article of this preprint also exists.
Submitted:
29 June 2024
Posted:
01 July 2024
You are already at the latest version
Alerts
Abstract
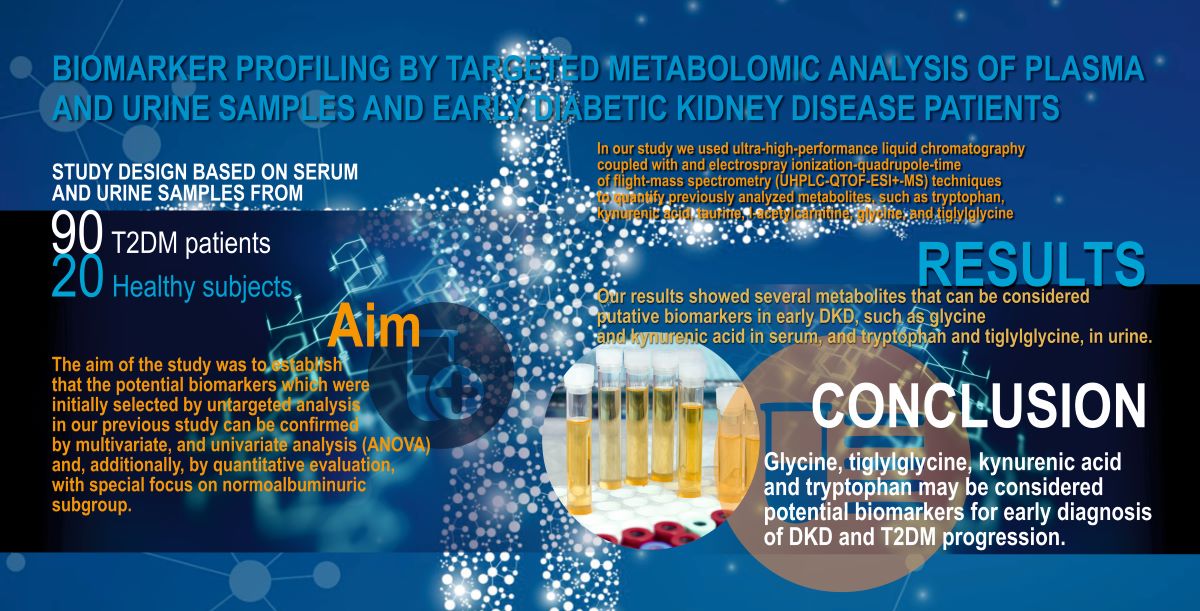
The incidence of diabetes mellitus (DM) continues to rise worldwide and one of the most serious microvascular complications is diabetic kidney disease (DKD), which is the leading cause of end-stage renal disease. Current bi-omarkers such as urinary albumin excretion rate have limitation for early detection of DKD. In our study we used ultra-high-performance liquid chromatography coupled with electrospray ionization-quadrupole-time of flight-mass spectrometry (UHPLC-QTOF-ESI+-MS) techniques to quantify previously analyzed metabolites, such as tryptophan, kynurenic acid, taurine, l-acetylcarnitine, glycine, and tiglylglycine. We performed the targeted analy-sis of metabolites from urine and serum samples, collected from 110 subjects. Of these, 90 patients with type 2 DM (T2DM) were divided according to the urinary albumin/creatinine ratio (UACR) into normoalbuminuria 300 mg/g groups, respectively, while 20 subjects were rep-resented by healthy controls. Through various validation methods, we identified several metabolites as potential biomarkers, such as kynurenic acid, glycine, and l-tryptophan in serum and l-acetylcarnitine, tiglylglycine, and tau-rine in urine.
Keywords:
Subject: Medicine and Pharmacology - Urology and Nephrology
1. Introduction
Diabetes mellitus (DM) represents a considerable medical challenge worldwide due to the high ongoing prevalence of derived complications [1]. One of the long-term complications of DM is represented by diabetic kidney disease (DKD), which has an immense negative impact on patients’ life expectancy by evolving to end-stage renal disease (ESRD) in up to 40% of cases [2]. Although DKD is a frequently encountered condition, the current methods of diagnosis, which include estimated glomerular filtration rate (eGFR) and albuminuria, lack specificity and sensibility for disease onset [3,4].
Albuminuria was the epicenter of DKD identification for a long time. However, recent data indicate that not only the glomerular tuft is affected by long-term hyperglicemia. Emerging evidence points to the proximal tubule as the first affected site in the context of DM. Hence, it is critical to investigate novel biomarkers which may have an effect on these structures [5].
Metabolomics represents a refined and a deeply comprehensive tool, which grants for the investigation of the whole metabolome of a particular person. This technique is based on the untargeted and targeted analysis of metabolites encountered in certain biofluids, such as urine and plasma, offering crucial data regarding mechanisms of disease development, drug toxicity, and possibly gene function [6]. The untargeted analysis may be applied to explore the potential metabolic pathways in which the identified metabolites are implicated.
In a step-way fashion, the targeted analysis allows for the quantification of the metabolites previously discovered by untargeted techniques. Metabolites derived from amino acids (AAs), nucleotides, lipids, and sugars are small molecules which can be analyzed by metabolomic techniques. [7,8,9].
Amino acids are organic compounds constituted of basic amino and carboxy groups playing a fundamental role in the synthesis of proteins, polypeptides, and other biologically active nitrogenous molecules. The human body is able to synthesize only certain types of amino acids and the rest of them, the essential amino acids, such as isoleucine, histidine, lysine, leucine, phenylalanine, tryptophan, methionine, threonine, and valine, are supplied through diet [10]. The dietary derived AAs are metabolized in many tissues, particularly in the liver, intestine, muscle, and kidney. From a renal point of view, AAs are reabsorbed in 99,5% in the proximal tubule, their dynamic being highly reflective of tubular well-function [11].
Tryptophan (TRP) is a fundamental aromatic AA encountered in aliments such as milk, beans, fish, and eggs. [12]. TRP metabolism follows three major metabolic pathways under direct or indirect control of gut microbiota: (1) the serotonin or 5-hydroxytryptamine (5-HT) pathway, which ends up in serotonin derivatives formation, via tryptophan hydroxylase; (2) the indole pathway, in which TRP breaks down to indole derivatives under the action of the intestinal microbial community; and (3) the kynurenine (KYN) pathway, which utilizes indoleamine 2,3-dioxygenase (IDO) to produce kynurenine derivates [13,14,15]. Studies conducted by Chou et al., and Wu et al., revealed low serum concentration of TRP associated with rapid decline of eGFR and a higher KYN/TRP ratio linked to macroalbuminuria. [2,16].
Taurine is an amino-sulfonic acid located in the cerebral, muscular, cardiovascular, and gastrointestinal systems, being endogenously synthesized from cysteine. In the kidney, taurine stands at the basis of multiple actions on cellular functions such as: ion absorption (to efflux from renal cells, requires the presence of Na+ and Cl-) and renal vascular endothelial function (high level of taurine leads to increased serum levels of nitric oxide and NO synthase activity; also, the renin-angiotensin-aldosterone system was affected and it was observed elevation of endothelin levels) [17]. Bergstrom et al., revealed reduced concentration of taurine in plasma patients with chronic kidney disease [18]. Moreover, other studies, pointed out significantly decreased serum taurine levels in patients with DKD [19,20,21,22].
Carnitines are derived from an amino acid and include L-carnitine and its acylated forms, such as acetyl-L-carnitine and propionyl-L-carnitine. Carnitines can be found in foods and also may be secreted endogenously. Belay B et al., stated that carnitines play a critical role in energy production by transporting long-chain fatty acids into the mitochondria so that they can be oxidized to produce energy [23]. In the kidney, Van der Kloet et al., observed that under certain conditions, such as the diabetic state, reabsorption of acylcarnitine is poor, thus they are eliminated through urine [24,25].
Glycine is an amino acid participating in multiple metabolic pathways. Its synthesis is located in the renal and hepatic systems from threonine, choline, and serine via threonine dehydrogenase pathway, the generation of sarcosine and serine hydroxymethyltransferase pathway, respectively [26]. Although the mechanism by which glycine acts in patients with T2DM is not very clear, authors consider that this is related to low levels of serine. Also, the excessive free fatty acids (FFA) and BCAA (branched-chain amino acids) metabolism cand lead to poor levels of glycine [27]. Tiglylglycine is an intermediate product of the catabolism of isoleucine and it is less studied in the literature. Few recent reports describe a high secretory clearance of this metabolite among patients with DKD [28,29].
Renal disease in T2DM is associated with excess morbidity/mortality. Although large studies offer an insight on evolution of DKD, early biomarkers are needed to elaborate algorithms and improve renal disorder stratification [30]. The current study represents an extension of a previous study where we used untargeted multivariate and univariate metabolomic analyses of serum and urine in T2DM patients with DKD [31]. The aim of the study is to assess, through targeted analyses, novel biomarkers that can predict an incipient renal impairment in DKD.
2. Materials and Methods
2.1. Patients and Compliance with Ethical Standards
In our study we enrolled patients with 90 T2DM recruited from the Department of Nephrology and Department of Diabetes and Metabolic Diseases ,,Pius Brinzeu" County Emergency Hospital Timisoara. As an inclusion criterion we selected patients with long-standing T2DM, with a duration of more than 5 years. Patients with T2DM with poor control of diabetes (HbA1c > 10%) were excluded from the study. At the time of screening all patients were undergoing treatment with angiotensin converting enzyme inhibitor or angiotensin receptor blocker, oral antidiabetic agents and/or insulin, and statins. Based on UACR and eGFR we divided the 90 T2DM patients in 3 subgroups (30-normo- <30 mg/g subgroup P1, 30-micro- 30-300 mg/g subgroup P2, and 30 macroalbuminuria >300 mg/g subgroup P3) and 20 healthy controls (group C) [31].
Table 1.
Demographic and clinical data of the groups and subgroups of patients.
| P1 | P2 | P3 | C | |
|---|---|---|---|---|
| Number of participants | 30 | 30 | 30 | 20 |
| Male/female (number) | 17/13 | 16/14 | 20/10 | 12/8 |
| Age (y) | 68.41 ± 4.98 | 68.65 ± 4.91 | 68.84 ± 4.98 | 55.85 ± 7.25 |
| DM duration (y) | 9.6 ± 3.99 | 9.7 ± 3.99 | 12.78 ± 3.35 | 0 |
| Serum creatinine (mg/dL) | 0.82 ± 0.18 | 0.93 ± 0.21 | 1.07 ± 0.32 | 0.73 ± 0.08 |
| eGFR (mL/min/1.73 m2) | 90.42 ± 18.10 | 89.70 ± 18.19 | 77.85 ± 19.38 | 97.93 ± 11.71 |
| UACR (mg/g) | 7.38 ± 3.22 | 45.42 ± 57.08 | 319.86 ± 585.80 | 5 ± 0.23 |
| HbA1c (%) | 5 ± 0.23 | 6.42 ± 1.29 | 7.15 ± 1.60 | 4.98 ± 0.23 |
| Body weight (kg) | 79.06 ±4.90 | 84.86 ±3.9 | 86.06 ±4.46 | 78.05 ±5.47 |
The protocol of the study was authorized by the Ethics Committee for Scientific Research of “Victor Babes” University of Medicine and Pharmacy Timisoara (no. 28/02.09.2020) and the Ethics Committee for Scientific Research of “Pius Brinzeu” County Emergency Hospital Timisoara (no. 296/06.04.2022) including the details about samples and written informed consent prior to entering in study.
2.2. Chemicals and Reagents.
For the targeted analysis of this study, we used the following chemicals and regents: HPLC-grade formic acid was obtained from Sigma-Aldrich (USA), HPLC/MS-grade formic acid and acetonitrile were acquired from Fisher Scientific (USA). The standard biomarkers used are represented by L-Tryptophan >98.5%(T)(HPLC) (T0541 ;TCI Chemicals, US) MW=204, O-Acetyl-L-carnitine hydrochloride (J6153606; Alfa Aesar by Thermo Fisher) MW=203, Kynurenic acid, >98.0%(HPLC) (H0303; TCI Chemicals, US) MW=189, Taurine, 99% (A1240322; Alfa Aesar by Thermo Fisher) MW=125, Tiglylglycine- was not available, Glycine from Amino acid standard H (product #20088, Thermo Scientific) MW=75 and Creatinine>98% product C4255, Sigma-Aldrich Chemie GmbH. MW=113. As internal standard it was used Doxorubicin hydrocholride (MW=580)( injectable, 2 mg/ml Sun Pharmaceutical Industries). Other reagents: LC–MS grade MeOH, MeCN, and formic acid were purchased from Fisher Scientific (Loughborough, UK). Ultra-pure water was purified by a Milli-Q water system (Millipore, Milford, MA, USA). Instruments used in this study included a vortex mixer, Minicentrifuge Eppendorf (Thermo Fisher Scientific, USA), UPLC-Q-TOF/MS (Bruker GmbH, Germany).
2.3. Sample Preparation
For the samples collected from patients, confidential numerical codes were used to preserve their identity. Venipuncture was the method used to collect the blood serum. The blood samples were put in sterile vacutainers without anticoagulant and urine in sterile vials. The samples were held at -80˚˚̊C until analysis. A volume of 0.8 mL mix of pure HPLC-grade Methanol and Acetonitrile (2:1 v/v) was added for each volume of 0.2 mL of blood serum and 0.2mL urine, respectively. In each case the mixture was vortexed to precipitate proteins, ultrasonicated 5 min and kept 24 hrs at -20˚˚̊C for increasing the protein precipitation. The supernatant was collected after centrifugation at 12,500 rpm for 10 min (4°C) and filtered through Nylon filters (0.2 μm). Finally, it was placed in glass micro vials and introduced in the autosampler of the ultra-high-performance liquid chromatograph (UHPLC) before injection. The supernatant was transferred to an autosampler vial for HPLC-MS analysis. Quality control (QC) samples from a mix of 0.1 ml from each serum or urine samples were also obtained and used as representative generic samples which were injected at the beginning and end and as every 10th injection while analyzing the study samples.
2.4. UHPLC-QTOF-ESI+-MS Analysis
The metabolomic profiling was performed by ultra-high-performance liquid chromatography coupled with electrospray ionization-quadrupole-time of flight-mass spectrometry (UHPLC-QTOF-ESI+-MS) using a ThermoFisher Scientific UHPLC Ultimate 3000 instrument equipped with a quaternary pump, Dionex delivery system, and MS detection equipment with MaXis Impact (Bruker Daltonics). Details about this method is described in our previous study [31].
2.5. Data Processing and Statistical Analysis
In our first study we performed untargeted analysis for the same groups (P and C) [31].
Initially, multivariate analysis was performed to indicate the differences between the 2 groups (C group versus P group) using Fold change, PCA, and PLSDA score plots, including VIP values. Volcano plots were generated with the log2 fold change values and Bonferroni-adjusted p- values. The value of p < 0.05 was defined as statistically significant.
In order to evaluate the particularity of each metabolite, we performed receiver operating characteristic (ROC) analysis. Metabolites with AUC values higher than 0.8 meet the criteria to be considered potential biomarkers in future studies, having a high prediction effect on disease.
Subsequent the one-way ANOVA univariate analysis aimed the discrimination between the controls and the subgroups of patients (P1, P2, P3). The PCA and PLSDA score plots including VIP values, cross validation parameters, as well as the mean decrease accuracy scores by Random Forest analysis were performed. For the statistical analysis of targeted metabolites matrices were selected which included the five metabolites mentioned above (m/z values vs. MS peak intensity, as .csv file) [31].
From untargeted metabolomics analysis we selected a number of 7 specific molecules. To compare the various subgroups of patients we used Mass spectrometry (MS) peak intensities. Specific biomarkers selected by the untargeted metabolomics were calculated using mean values of peak intensity (PI) and their standard deviations SD and for the quantitative analysis were used pure standards determined by calibration curves.
2.6. Metabolites Identification
Untargeted metabolomic analysis pointed out 5 significant metabolites which can be considered as putative biomarkers for differentiation between subgroups. For multivariate and univariate analysis, we utilized Metaboanalyst 5.0 platform in order to perform the statistical analysis. ((https://www.metaboanalyst.ca). Moreover, the platform mentioned above was used to identify and describe the major metabolic pathways and the way these metabolites were affected during the onset of a disease.
Platforms such as Human metabolome database HMDB (http://www.hmdb.ca), PubChem (https://pubchem.ncbi.nlm.nih.gov) and Lipidmaps (https://www.lipidmaps.org) offered us chemical information about metabolites considering a deviation of the m/z value of 0.05. By associating the exact number (m/z) with the ionization method and differentiating the primary and secondary mass spectra information metabolites with the theoretical fragments of the HMDB search results demonstrate the identification of metabolites.
2.7. Quantitative Evaluation
Preparation of calibration solution and quality control (QC) samples. The stock solutions of the five potential biomarkers were: L-tryptophan 1 mM, L-Acetylcarnitine 1 mM, Kinurenic acid 1 mM, Taurine 1 mM, Glycine 2 mM, Creatinine 2mM dissolved in Ultra-pure Water. The stock solutions were successively diluted in the mix of methanol: acetonitrile 2:1 to obtain the series of working solutions at different concentration levels for external calibration. In parallel, volumes of 0.3 ml QC deproteinated samples were spiked with different volumes of standard solutions.
The linearity, specificity, precision, accuracy, limit of detection (LOD) and limit of quantification (LOQ) was evaluated by the UHPLC-QTOF-ESI+-MS method. This method was validated according to the “Guidance for Industry-Bioanalytical Method Validation”. Two calibration curves were generated: an external standard calibration curve (1), made by diluting standard solutions in the mobile phase and an internal standard curve (2), whose linearity was determined for QC samples spiked with different volumes of standard solutions. The mean peak area of three replicate measurements at each concentration was calculated.
Limit of Detection (LOD) and Limit of Quantification (LOQ). The LOD was the lowest concentration of analyte in the test sample that can be reliably distinguished from zero to signal/noise ratio ≥ 10. The LOQ was the lowest concentration of analyte that can be determined with an acceptable repeatability and trueness (signal/noise ratio ≥ 10 and SD values ≤ 40%).
3. Results
3.1. Multivariate Analysis for Targeted Metabolites: Fold Change, p-Values and AUC
Considering the separation data accumulated from UHPLC-MS analysis, the matrices representing the retention time (RT), the m/z values and the Peak intensities (PI) corresponding to the targeted metabolites were used for statistical analysis.
Table 2 includes the retention times and AUC values for the metabolites targeted in serum and urine in order to identify the differences between the healthy group (controls) versus pathological DKD group, P. .
According to the data recorded, serum kynurenic acid, glycine, and L-tryptophan had higher AUC values (over 0.610). Tiglylglycine was not found in serum. Similarly, urine Glycine, L-Acetylcarnitine, Taurine, Tiglylglycine, Kynurenic acid, and creatinine had higher AUC values above 0.600. Compared to serum, the urine metabolites seem to be more relevant to discriminate between the groups C and P.
3.2. One Way Analysis of Variance (ANOVA) & Post-Hoc TESTS
To evaluate the effect of albuminuria (from normal to macroalbuminuria) on the differentiation of the biomarkers, One Way ANOVA algorithm was applied, considering the group C vs. subgroups P1, P2, and P3.
The untargeted analysis allowed the discrimination for six metabolites between subgroups P1 versus P2 and P3, based on One Way ANOVA and Fisher’s LSD displayed in Supplementary file S1A, B.
Statistical data obtained by the methods mentioned above point out metabolites considered for the targeted analysis: glycine, creatinine, taurine, kynurenic acid, L-acetyl-carnitine, and L-Tryptophan in serum, and glycine, creatinine, taurine, Tiglylglycine, kynurenic acid, L-Acetyl carnitine, and L-Tryptophan in urine. Their discrimination between subgroups and their differences expressed in MS peak intensities are represented in Supplementary Figures S1 and S2.
3.3. Quantitative Evaluation
3.3.1. Calibrations and Validation Parameters
Determination of linear ranges (calibration curves and equations including R2values), the LODs, and LOQ of each standard are given in Table 3. The correlation coefficients (R2) were higher than 0.898 for all standards in their line range, showing good linear relationship within linear ranges. All the LOD values were in the range 0.3-4 μM, and LOQ values were in range 0.9-5.5 μM.
The validation of the LC-MS method for the quantitative evaluation of metabolites was done using controlled additions of internal standard (DOXO) and each of the five pure standards to QC extracts.
To the same volume of QC extracts (0.3 ml) there were added 0.2 ml from each of the eight standard solutions (50 mM creatinine and glycine, 25 mM taurine and L-tryptophan, 5 mM kynurenic acid, L-Acetylcarnitine) and 3.4 mM of internal standard DOXO.
Table 4 shows the initial concentrations of metabolites after mixing with QC extract and the measured concentrations after the LC-MS analysis. The recovery percentage was calculated, as a measure of the method reproducibility.
3.3.2. Quantitative Evaluation
The quantitative evaluation, based on the curve equations for each biomarker in serum and urine is presented in Table 5 and Table 6.
Normal ranges for the targeted metabolites based on HMDB
| Biomarker | Normal range based on HMDB | Link | |
| Serum (mM) | Urine (mM/mM creatinine) | ||
| L-tryptophan | 40-90 | 3-6 |
https://hmdb.ca/metabolites/HMDB0000929 |
| L-Acetyl carnitine | 5-7 |
1-3 |
https://hmdb.ca/metabolites/HMDB0000201 |
| Kynurenic acid | 0.03 +/- 0.007 <5 |
1-1.6 | https://hmdb.ca/metabolites/HMDB0000715 |
| Taurine | 40-80 |
25-90 | https://hmdb.ca/metabolites/HMDB0000251 |
| Tiglylglycine | Not detected | 0.1-7 | https://hmdb.ca/metabolites/HMDB0000959 |
| Creatinine |
60.0-200 |
Large variation 6970 (3490-10500)- 500-35000 |
https://hmdb.ca/metabolites/HMDB0000562 |
| Glycine | 120-450 | 106-135 | https://hmdb.ca/metabolites/HMDB0000123 |
4. Discussion
In the present study, we performed a comparative targeted metabolomic analysis of blood and urine samples from T2DM patients and healthy subjects, with special focus on the normoalbuminuric subgroup. The aim of the study was to establish that the potential biomarkers which were initially selected by untargeted analysis in our previous study [31] can be confirmed by multivariate, and univariate analysis (ANOVA) and, additionally, by quantitative evaluation.
In the targeted analysis, there were employed calibration and validation curves in order to evaluate the concentration and the way in which each targeted biomarker undergoes changes during the evolution of a disease. From the previous study we selected the following biomarkers with potential role in diagnosis of incipient DKD: tryptophan, kynurenic acid, taurine, l-acetyl carnitine, glycine, and tiglylglycine. We found several metabolites that can be considered putative biomarkers in early DKD such as glycine and kynurenic acid in serum and tryptophan and tiglylglycine in urine.
4.1. TRP Metabolic Pathway and Its Role in DKD
In our study, we detected that TRP had a tendency to decrease progressively in accordance with the evolution of albuminuria. By contrast, in urinary samples we found that in normoalbuminuric patients TRP had low concentrations in group P1 versus group C and subgroups P2, P3 which cand be considered an important early DKD biomarker. These findings are in concordance with previous studies where Chou et al., Faheem et al., and Wu et al., reveal low serum concentrations of TRP associated with rapid decline in eGFR and also with macroalbuminuria [2,16,32]. When compared to HMDB, the concentrations of TRP vary between 40-90 µM in blood and 3-6 µM/mM creatinine in urine samples and kynurenic acid between 0.03 +/- 0.007 <5 µM in serum and 1-1.6 µM/mM creatinine in urine samples. In addition, Chou et al., provide a value of TRP < 44,2 µmol/L and Wu et al., TRP < 46,75 µmol/L at macroalbuminuric patients.
TRP is an essential amino acid that contributes in protein synthesis. TRP has complex biological effects due to extensive metabolites implicated in various metabolic pathways. Tryptophan metabolism follows three major pathways: serotonin pathway in which TRP is catalyzed with TRP hydroxylase1 (TPH1) in the enterochromaffin cell to produce peripheral 5-HT which takes part in regulation of gastrointestinal functions; indole pathway, where TRP is directly metabolized to indole and indole derivates via intestinal flora; the kynurenine pathway in which TRP is metabolized by 3 enzymes IDO1, IDO2, and TRP 2,3-dyoxygenase (TDO) to produce formyl kynurenine (FKYN) which catalyze formilase to generate kynurenine and other bioactive metabolites, such as kynurenic acid, picolinic acid, nicotinamide adenine dinucleotide, and xanthurenic acid [12]. According to data presented by Mohib et al., and Stone TW et al., there is an excessive accumulation of the IDO1 enzyme in the kidney tissues, which can lead to the assumption that the changes in the activity of the enzymes in the kynurenine pathway could contribute to the pathogenesis of DKD. [33,34].
Being a metabolite of TRP, serum kynurenic acid displayed the same behavior as TRP with a decreased trend in serum from C group to P subgroups, but did not achieve significance in urine samples.
4.2. Assesement of Taurine as a Potential Biomarker in DKD
In this article we reported a slightly decrease of Taurine concentrations in serum samples from C group to normoalbuminuric group, and a slightly increase in subgroups P2 and P3, respectively. In contrast, in urine samples, we found out that concentrations of this metabolite are not very different between group C and subgroups P1, P2, and P3, respectively. Some of this information can be related with data from the literature where Bergstrom et al., describe a reduced concentration of taurine in plasma of patients with chronic kidney disease (CKD) [18]. Regarding patients with DKD, Shao et al., Peng et al, Baliou et al, and ITO et al, highlight the same decline in serum levels of taurine [19,20,21,22]. Also, in a recent review there has been observed a significant decrease of serum taurine in diabetic patients when compared to the frank group [35]. Being a metabolite less studied, we could not find data about the urine concentration of taurine. As stated by HMDB, the normal range is 40-80 µM in serum and 25-90 µM/mM creatinine in urine samples.
Taurine is an amino sulfonic acid found in great quantity in almost all tissues and cells of animals and humans [36]. Taurine is a non-essential amino acid produced in the liver from methionine or cysteine. This metabolite is involved in many physiological processes. For example, taurine is involved in glucose homeostasis, by reducing oxidative stress, inflammation, and increasing insulin sensitivity and secretion [37].
The active transport of taurine takes place via a sodium-dependent transporter [38]. Besides sodium, renal epithelia require chloride or bromide to assimilate taurine [39]. The mechanism of sodium and chloride explains that Na+ moves into cells using a gradient, and subsequently is removed from the cell by the Na+K+ dependent ATPase. Taurine transport is inhibited by β amino acids and GABA (gamma-aminobutyric acid) and is membrane surface specific. In the renal tubules, taurine behaves differently depending on the location: in the proximal tubule the maximal uptake is on the apical surfaces, while the uptake of this metabolite is at the level of basolateral surface in distal tubule [40].
The mechanism described above shows that taurine does not contribute to the adaptive renal response but is dependent on specific ions to participate in passive diffusion. Also, taurine interacts with glucose. In the renal system, taurine appears to reduce the glucose via Na+-dependent mechanism, which can potentially determine glucosuria. It was presumed that the presence of taurine in the renal tubules compete for sodium, a fact which leads to a reduction in glucose. As a consequence, taurine may have impact on the intra or transcellular movement of glucose [17].
Moreover, taurine represents a substrate for mitochondrial tRNA. A study elaborated by Fakruddin et al. demonstrated an activation of cellular oxidative stress by mitochondrial disfunction due to deficit of taurine [41]. Also, it can inhibit oxidative stress by reducing excess of calcium, increasing antioxidant glutathione and inhibiting ROS (reactive oxygen species) [21,42,43].
4.3. Association between Acetylcarnitine and the Presence of DKD
Our paper describes high concentrations of L-acetylcarnitine in serum in subgroup P1 versus group C and subgroups P2 and P3, respectively, but in urine samples this metabolite did not achieve significance between subgroups. According to HMDB, the normal range is 5-7 µM in serum and 1-3 µM/mM creatinine in urine samples. L-acetyl carnitine, the acetylated form of amino acid derivate l-carnitine, is a small molecule that fulfills essential roles in intermediate metabolism. It is implicated in cellular energy, which, through β-oxidation, transports long-chain fatty acids from the cytosol into the mitochondria. Also, carnitines regulate the activity of some mitochondrial enzymes involved in tricarboxylic cycle (TCA), urea cycle, and gluconeogenesis [44]. In several studies, it was documented that the level of serum acetyl carnitines has increased with the reduction with renal function in patients with CKD [45,46]. Regarding the significance of this metabolite in patients with T1DM and T2DM, the studies conducted by Van der Kloet et al., and Gunther et al., show the associations between serum and urinary acetyl carnitines and the risk of diabetes development [24,47].
4.4. Glycine and Its Metabolite Tiglylglycine – Involvement in DKD
Regarding the concentration of glycine determined in this research, we have observed a downward trend of glycine levels in blood and urine samples, results which are in keeping with data in the literature where Barrios et al., and Yatzidis et al., found strong association between low levels of glycine and decrease in eGFR [48,49]. Moreover, Floegel et al. and Sekher et al., compared patients without diabetes and those with diabetes and discovered reduced concentrations of glycine [50,51]. Glycine, a non-essential amino acid, is synthesized from serine. Although the mechanism by which glycine acts in patients with T2DM is not very clear, authors consider that this is related to low levels of serine. Also, the excessive free fatty acids (FFA) and BCAA metabolism cand lead to poor levels of glycine [27].
In agreement with HMDB, the normal range for glycine is 120-450 µM in serum and 106-135 µM/mM creatinine in urine samples, whereas for tiglylglycine 0,1-7 µM/mM creatinine in urine samples. Of interest, in blood samples this metabolite was not detected.
Tiglylglycine, a metabolite of glycine, has the same characteristics as glycine. We could not identify this metabolite in plasma, but we detected progressively decreasing levels starting with group C to subgroup P3. After statistically analysis was applied, we found low concentrations in urine in the P3 subgroup as compared to our previous study, where we revealed increased values of this metabolite in the P3 subgroup. Tiglylglycine is an amino acid less studied in the literature, but few recent reports describe differences of this metabolite between DKD and non-diabetic CKD [29,46,52].
4.5. From Metabolic Studies to Clinical Practice
The biomarkers mentioned above may have implication in clinical practice. Studies performed on glycine administration indicate improvements in eGFR and DM [49,51,53]. There are contradictions regarding the supplementation of taurine. For example, Hansen SH et al and Harada H et al., demonstrated that the administration of taurine improves hyperglycemia and insulin resistance in diabetic rats, while Chauncey et al., reported that supplementation of taurine does not have effect on glucose in patients with T2DM. Furthermore, for tryptophan it was stated by Inubushi et al., that L-tryptophan suppressed both serum glucose and insulin levels after oral glucose administration and inhibited glucose absorption from the intestine in diabetic rats [57].
5. Conclusions
In the present study we integrated information regarding serum and urine metabolites using LC-UHPLC techniques in order to reveal the differences between controls and subgroups of patients with DKD, with a special focus on the normoalbuminuric subgroup. Our results showed several metabolites that can be considered putative biomarkers in early DKD, such as glycine and kynurenic acid in serum, and tryptophan and tiglylglycine, in urine.
Our study has its limitations. First, this is a cross-sectional study which does not allow to establish causality between our findings and clinical parameters. Second, the variability of the glycemic control could have introduced a bias in the interpretation of data. Third, lipid metabolism variables were not utilized in correlations.
However, our study has its strength which resides in the documentation of a particular metabolomics profile in serum and urine in patients with T2DM, highly indicative of early renal involvement within the confines of DKD.
The candidate metabolites from this study need to be validated in larger studies and their implication in different mechanisms of DKD requires further research.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, M.M., F.G. and L.P., methodology, M.M., F.G., L.P. and A.V.; software, O.M. and A.S.-S.; validation, C.S., A.I.S., M.G., S.I. and L.B.; formal analysis, C.S. and A.I.S.; investigation, M.M., C.S., L.P., F.G., A.V., M.G. and L.I. resources, C.S. and L.P.; data curation, L.P. and C.S.; writing—original draft preparation, M.M.; writing—review and editing, C.S., L.P., F.G. and C.S.; visualization, M.M., F.G., L.P., F.B., O.M.C. and D.C.J.; supervision, M.M., F.G. and L.P.; project administration, M.M., C.S., F.G. and L.P. S.U., statistical analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania, through doctoral grant GD 2020 to M.M.
Institutional Review Board Statement
The protocol of the study was approved by the Ethics Committee for Scientific Research of “Victor Babes” University of Medicine and Pharmacy Timisoara number 28/02.09.2020 and “Pius Brinzeu” County Emergency Hospital Timisoara number 296/06.04.2022.
Informed Consent Statement
Informed consent was obtained from all subject involved in this study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- K.S. Kim.; J.S. Lee.; J.H. Park.; E.Y. Lee.; J.S. Moon.; S.K. Lee.; J.S. Lee.; J.H. Kim.; H.S. Kim.; Identification of Novel Biomarker for Early Detection of Diabetic Nephropathy. Biomedicines 2021, 9(5), 457. [CrossRef] [PubMed]
- Chou, C.A.; Lin, C.N.; Tsun-Yee Chiu, D.; Chen, I.W.; Chen, S.T. Tryptophan as a surrogate prognostic. [CrossRef] [PubMed]
- marker for diabetic nephropathy. J Diabetes Investig. 2018; 9(2): 366–374. [CrossRef] [PubMed]
- K.C. Norris.; K.E. Smoyer.; C. Rolland.; J. Van der Vaart.; E.B. Grubb.; Albuminuria, serum creatinine, and estimated glomerular filtration rate as predictors of cardio-renal outcomes in patients with type 2 diabetes mellitus and kidney disease: a systematic literature review. BMC Nephrol 19, 36 (2018). [CrossRef] [PubMed]
- N. Tangri.; L.A. Inker.; M.B. Hiebert.; J. Wong.; D. Naimark.; D. Kent.; A.S. Levey.; A Dynamic Predictive Model for Progression of CKD, American Journal of Kidney Diseases, Volume 69, Issue 4. [CrossRef] [PubMed]
- 2017, Pages 514-520, ISSN 0272-6386. [CrossRef] [PubMed]
- C.J. Magri.; S. Fava.; The role of tubular injury in diabetic nephropathy. European Journal of Internal Medicine,Volume 20, Issue 6, 2009, Pages 551-555, ISSN 0953-6205. [CrossRef] [PubMed]
- A.Zhang.; H. Sun.; Z. Wang.; W. Sun.; P. Wang.; X. Wang.; Metabolomics: Towards Understanding Traditional Chinese Medicine. Planta Med 2010; 76(17): 2026-2035. [CrossRef]
- Wu, F., & Liang, P. (2022). Application of Metabolomics in Various Types of Diabetes. Diabetes, Metabolic Syndrome and Obesity, 15, 2051–2059. [CrossRef]
- Roberts, L. D., A. Koulman, and J. L. Griffin. "Towards metabolic biomarkers of insulin resistance and type 2 diabetes: progress from the metabolome. Lancet Diabetes Endocrinol. 2014; 2: 65–75." S2213-8587 (13): 70143-8. [CrossRef]
- Jin, Qiao, and Ronald Ching Wan Ma. "Metabolomics in diabetes and diabetic complications: insights from epidemiological studies." Cells 10.11 (2021): 2832. [CrossRef]
- Wu, Guoyao. Amino acids: biochemistry and nutrition. CRC Press, 2021.
- Makrides, V., Camargo, S. M., & Verrey, F. (2014). Transport of amino acids in the kidney. Compr Physiol, 4(1), 367-403. [PubMed]
- Liu, L.; Xu, J.; Zhang, Z.; Ren, D.; Wu, Y.; Wang, D.; Zhang, Y.; Zhao, S.; Chen, Q.; Wang, T. Metabolic Homeostasis of Amino Acids and Diabetic Kidney Disease. Nutrients 2023, 15, 184. [CrossRef] [PubMed]
- Wyant, Gregory A., and Javid Moslehi. "Expanding the therapeutic world of tryptophan metabolism." Circulation 145.24 (2022): 1799-1802. [CrossRef] [PubMed]
- Pataskar, A et al. "Tryptophan depletion results in tryptophan-to-phenylalanine substitutants." Nature 603.7902 (2022): 721-727. [CrossRef] [PubMed]
- Platten, M., Nollen, E. A., Röhrig, U. F., Fallarino, F., & Opitz, C. A. (2019). Tryptophan metabolism as a common therapeutic target in cancer, neurodegeneration and beyond. Nature reviews Drug discovery, 18(5), 379-401. [CrossRef]
- 16. Wu, M.H.; Lin, C.N.; Chiu, D.T; Chen, S.T; Kynurenine/Tryptophan Ratio Predicts Angiotensin Receptor Blocker Responsiveness in Patients with Diabetic Kidney Disease, Diagnostics 2020, 10, 207.
- Chesney, R.W.; Han, X.; Patters, A.B. Taurine and the renal system. J Biomed Sci 17 (Suppl 1), S4 (2010). [CrossRef]
- Bergström, J., et al. "Sulphur amino acids in plasma and muscle in patients with chronic renal failure: evidence for taurine depletion." Journal of internal medicine 226.3 (1989): 189-194. [CrossRef] [PubMed]
- Shao M, Lu H, Yang M, Liu Y, Yin P, Li G, Wang Y, Chen L, Chen Q, Zhao C, Lu Q, Wu T, Ji G. Serum and urine metabolomics reveal potential biomarkers of T2DM patients with nephropathy. Ann Transl Med. 2020 Mar;8(5):199. [CrossRef] [PubMed]
- 20. Peng, X.; Wang, X.; Shao, X.; Wang, Y.; Feng, S.; Wang, C.; Ye, C.; Chen, J.; Jiang, H. Serum Metabolomics Benefits Discrimination Kidney Disease Development in Type 2 Diabetes Patients. Front Med (Lausanne). 2022; 9: 819311. [CrossRef]
- 21. Baliou S, Adamaki M, Ioannou P, Pappa A, Panayiotidis MI, Christodoulou I, Spandidos DA, Kyriakopoulos AM and Zoumpourlis V.; Ameliorative effect of taurine against diabetes and renal-associated disorders (Review). Med Int 1: 3, 2021. [CrossRef]
- Ito, Takashi, Stephen W. Schaffer, and Junichi Azuma. "The potential usefulness of taurine on diabetes mellitus and its complications." Amino acids 42 (2012): 1529-1539. [CrossRef] [PubMed]
- Belay, Brook, et al. "The use of levo-carnitine in children with renal disease: a review and a call for future studies." Pediatric Nephrology 21 (2006): 308-317. [CrossRef]
- 24. F M van der Kloet, F W A Tempels, N Ismail, R van der Heijden, P T Kasper, M Rojas-Cherto, R van Doorn, G Spijksma, M Koek, J van der Greef, V P Mäkinen, C Forsblom, H Holthöfer, P H Groop, T H Reijmers, T Hankemeier. Discovery of early-stage biomarkers for diabetic kidney disease using ms-based metabolomics (FinnDiane study) Metabolomic. 2012 Feb; 8(1):109-119. [CrossRef]
- Wu, Y. Y., Gou, W., Yan, Y., Liu, C. Y., Yang, Y., Chen, D., ... & Chen, Y. M. (2022). Gut microbiota and acylcarnitine metabolites connect the beneficial association between equol and adiposity in adults: a prospective cohort study. The American Journal of Clinical Nutrition, 116(6), 1831-1841. [CrossRef] [PubMed]
- Adeva-Andany, M. M., Funcasta-Calderón, R., Fernández-Fernández, C., Ameneiros-Rodríguez, E., & Domínguez-Montero, A. (2019). Subclinical vascular disease in patients with diabetes is associated with insulin resistance. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 13(3), 2198-2206. [CrossRef] [PubMed]
- Yan-Do, Richard, and Patrick E. MacDonald. "Impaired “glycine”-mia in type 2 diabetes and potential mechanisms contributing to glucose homeostasis." Endocrinology 158.5 (2017): 1064-1073. [CrossRef] [PubMed]
- Wang, K., Zelnick, L. R., Hoofnagle, A. N., Chen, Y., de Boer, I. H., Himmelfarb, J., & Kestenbaum, B. (2020). Differences in proximal tubular solute clearance across common etiologies of chronic kidney disease. Nephrology Dialysis Transplantation, 35(11), 1916-1923. [CrossRef] [PubMed]
- Sharma, K.; Karl, B.; Mathew, A.V.; Gangoiti, J.A.; Wassel, C.L.; Saito, R.; Pu, M.; Sharma, S.; You, Y.H.; Wang, L.; Diamond-Stanic, M.; Lindenmeyer, M.T.; Forsblom, C.; Wu, W.; Ix, J.H.; Ideker, T.; Kopp, J.B.; Nigam, S.K.; Cohen, C.D.; Groop, P.H.; Barshop, B.A.; Natarajan, L.; Nyhan, W.L.; Naviaux, R.K. Metabolomics reveals signature of mitochondrial dysfunction in diabetic kidney disease. J Am Soc Nephrol, 2013, 24(11):1901-12. [CrossRef] [PubMed]
- Solini, A., Manca, M. L., Penno, G., Pugliese, G., Cobb, J. E., & Ferrannini, E. (2016). Prediction of declining renal function and albuminuria in patients with type 2 diabetes by metabolomics. The Journal of Clinical Endocrinology & Metabolism, 101(2), 696-704. [CrossRef]
- Mogos, M., Socaciu, C., Socaciu, A. I., Vlad, A., Gadalean, F., Bob, F., ... & Petrica, L. (2023). Metabolomic Investigation of Blood and Urinary Amino Acids and Derivatives in Patients with Type 2 Diabetes Mellitus and Early Diabetic Kidney Disease. Biomedicines, 11(6), 1527. [CrossRef]
- Al-Barshomy, Said M. "Tryptophan Level as a Potential Prognostic Marker of Diabetic Nephropathy." Zagazig University Medical Journal 29.2.1 (2023): 222-227. [CrossRef]
- Mohib, K., Wang, S., Guan, Q., Mellor, A. L., Sun, H., Du, C., & Jevnikar, A. M. (2008). Indoleamine 2, 3-dioxygenase expression promotes renal ischemia-reperfusion injury. American Journal of Physiology-Renal Physiology, 295(1), F226-F234. [CrossRef] [PubMed]
- Stone, Trevor W., and L. Gail Darlington. "Endogenous kynurenines as targets for drug discovery and development." Nature reviews Drug discovery 1.8 (2002): 609-620. [CrossRef] [PubMed]
- Mostafa, Asmaa M., et al. "Assesment of serum taurine level as a potential biomarker for early diagnosis of diabetic nephropathy." GSC Biological and Pharmaceutical Sciences 22.1 (2023): 312-320. [CrossRef]
- Jacobsen, J. G., & Smith, L. H. (1968). Biochemistry and physiology of taurine and taurine derivatives. Physiological reviews, 48(2), 424-511. [CrossRef] [PubMed]
- Li, C., Gao, L., Lv, C., Li, Z., Fan, S., Liu, X., ... & Liu, J. Active role of amino acid metabolism in early diagnosis and treatment of diabetic kidney disease. Frontiers in Nutrition, 10. (2023). [CrossRef] [PubMed]
- Smith, K. E., Borden, L. A., Wang, C. H., Hartig, P. R., Branchek, T. A., & Weinshank, R. L. (1992). Cloning and expression of a high affinity taurine transporter from rat brain. Molecular pharmacology, 42(4), 563-569.
- Zelikovic, I., Stejskal-Lorenz, E., Lohstroh, P., Budreau, A., & Chesney, R.W. (1989). Anion dependence of taurine transport by rat renal brush-border membrane vesicles. American Journal of Physiology-Renal Physiology, 256(4), F646-F655. [CrossRef] [PubMed]
- Jones, Deborah P., Leslie A. Miller, and Russell W. Chesney. "Adaptive regulation of taurine transport in two continuous renal epithelial cell lines." Kidney international 38.2 (1990): 219-226. [CrossRef]
- Fakruddin, Md, et al. "Defective mitochondrial tRNA taurine modification activates global proteostress and leads to mitochondrial disease." Cell reports 22.2 (2018): 482-496. [CrossRef]
- Haojun, Zhang, et al. "Effects of NaF on the expression of intracellular Ca2+ fluxes and apoptosis and the antagonism of taurine in murine neuron." Toxicology Mechanisms and Methods 22.4 (2012): 305-308. [CrossRef] [PubMed]
- Jafri, Azliana Jusnida Ahmad, et al. "Taurine protects against NMDA-induced retinal damage by reducing retinal oxidative stress." Amino Acids 51 (2019): 641-646. [CrossRef] [PubMed]
- Bene, Judit, Kinga Hadzsiev, and Bela Melegh. "Role of carnitine and its derivatives in the development and management of type 2 diabetes." Nutrition & diabetes 8.1 (2018): 8. [CrossRef]
- Chen, Dan-Qian, et al. "Identification of serum metabolites associating with chronic kidney disease progression and anti-fibrotic effect of 5-methoxytryptophan." Nature communications 10.1 (2019): 1476. [CrossRef] [PubMed]
- Wang, Feijie, et al. "Associations of plasma amino acid and acylcarnitine profiles with incident reduced glomerular filtration rate." Clinical Journal of the American Society of Nephrology 13.4 (2018): 560-568. [CrossRef] [PubMed]
- Gunther, Samuel H., et al. "Serum acylcarnitines and amino acids and risk of type 2 diabetes in a multiethnic Asian population." BMJ Open Diabetes Research and Care 8.1 (2020): e001315. [CrossRef]
- Barrios, Clara, et al. "Circulating metabolic biomarkers of renal function in diabetic and non-diabetic populations." Scientific Reports 8.1 (2018): 15249. [CrossRef] [PubMed]
- Yatzidis, Hippocrates. "Oral supplement of six selective amino acids arrest progression renal failure in uremic patients." International urology and nephrology 36 (2004): 591-598. [CrossRef] [PubMed]
- Floegel, Anna, et al. "Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach." Diabetes 62.2 (2013): 639-648. [CrossRef]
- Sekhar, Rajagopal V., et al. "Glutathione synthesis is diminished in patients with uncontrolled diabetes and restored by dietary supplementation with cysteine and glycine." Diabetes care 34.1 (2011): 162-167. [CrossRef]
- Darshi M, Van Espen B, Sharma K: Metabolomics in Diabetic Kidney Disease: Unraveling the Biochemistry of a Silent Killer. Am J Nephrol 2016; 44:92-103. [CrossRef]
- Rong, Guangli, et al. "Artemether alleviates diabetic kidney disease by modulating amino acid metabolism." BioMed research international 2022.1 (2022): 7339611. [CrossRef] [PubMed]
- Hansen, Svend Høime. "The role of taurine in diabetes and the development of diabetic complications." Diabetes/metabolism research and reviews 17.5 (2001): 330-346. [CrossRef] [PubMed]
- Harada, Hisashi, et al. "Oral taurine supplementation prevents fructose-induced hypertension in rats." Heart and Vessels 19 (2004): 132-136. [CrossRef]
- Chauncey, Katherine B., et al. "The effect of taurine supplementation on patients with type 2 diabetes mellitus." Taurine 5: Beginning the 21st Century (2003): 91-96. [CrossRef]
- Inubushi, Tomoko, et al. "L-tryptophan suppresses rise in blood glucose and preserves insulin secretion in type-2 diabetes mellitus rats." Journal of nutritional science and vitaminology 58.6 (2012): 415-422. [CrossRef] [PubMed]
Table 2.
Retention times and AUC values for the metabolites targeted in serum and urine in order to identify the differences between the healthy group (controls) and pathological DKD group ( P).
Table 2.
Retention times and AUC values for the metabolites targeted in serum and urine in order to identify the differences between the healthy group (controls) and pathological DKD group ( P).
| m/z | Identification | TR (min) | Plasma AUC | Urine AUC |
|---|---|---|---|---|
| 76.0815 | Glycine | 0.9 | 0.868 | 0.926 |
| 114.0983 | Creatinine | 0.7 | 0.512 | 0.637 |
| 125.1042 | Taurine | 1.6 | 0.602 | 0.525 |
| 190.0625 | Kynurenic acid | 11.4 | 0.787 | 0.591 |
| 204.1369 | L-Acetylcarnitine | 1. | 0.556 | 0.550 |
| 205.1068 | L-tryptophan | 2.8 | 0.618 | 0.788 |
| 158.106 | Tiglylglycine | 10.7 | - | 0.684 |
Table 3.
Validation parameters (linear range, curve equation, the correlation coefficients (R2) limit of detection (LOD) and limit of quantification (LOQ) for each of the five molecules selected as potential biomarkers.
Table 3.
Validation parameters (linear range, curve equation, the correlation coefficients (R2) limit of detection (LOD) and limit of quantification (LOQ) for each of the five molecules selected as potential biomarkers.
| Name | Linear Range μM |
Curve Equation | R2 | LOD | LOQ |
|---|---|---|---|---|---|
| Glycine | 10-200 | y=596.72x-963.05 | 0.993 | 0.2 | 0.8 |
| Creatinine – serum | 5-25 | y=2693.3x-254.5 | 0.994 | 0.5 | 1.0 |
| Creatinine – urine | 200-2000 | y=2765.8x-73120 | 0.993 | 0.5 | 1.0 |
| Taurine | 5-25 | y=1479.6x+543.2 | 0.996 | 0.5 | 1.0 |
| Kynurenic acid | 0.1-2 | y=24309x+355.37 | 0.999 | 0.08 | 0.1 |
| L-Acetyl carnitine | 1-5 | y=36813x-3879.2 | 0.994 | 0.2 | 0.8 |
| L-tryptophan | 3-50 | y=820.31x-981.3 | 0.998 | 0.8 | 1.00 |
Table 4.
The recovery percentage (%) calculated from the measured concentrations of internal standard (IS) and each metabolite (pure standard) comparative to their Initial concentrations, after addition to QC extract.
Table 4.
The recovery percentage (%) calculated from the measured concentrations of internal standard (IS) and each metabolite (pure standard) comparative to their Initial concentrations, after addition to QC extract.
| Metabolite | Initial Concentration (mM) | Measured Concentration (mM) | Recovery (%) |
|---|---|---|---|
| Glycine | 20 | 17.5 | 87.5 |
| Creatinine | 20 | 18.2 | 91.0 |
| Taurine | 10 | 8.55 | 85.5 |
| Kynurenic acid | 2 | 1.65 | 82.5 |
| L-Acetyl carnitine | 2 | 1.85 | 92.5 |
| L-tryptophan | 10 | 9.15 | 91.5 |
| IS (DOXO) | 1.4 | 1.25 | 89.3 |
Table 5.
The mean values and standard deviations (±SD) of serum concentrations (mM) of the potential biomarkers targeted in this study for groups C and subgroups P1, P2 and P3.
Table 5.
The mean values and standard deviations (±SD) of serum concentrations (mM) of the potential biomarkers targeted in this study for groups C and subgroups P1, P2 and P3.
| Molecule | Control (n=20) | P1 (n=30) | P2 (n=30) | P3 (n=30) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean | ±SD | Mean | ±SD | Mean | ±SD | |
| Glycine | 221.32 | 39.84 | 196.24 | 39.25 | 188.56 | 43.37 | 214.62 | 47.22 |
| L-tryptophan | 56.59 | 10.19 | 51.38 | 10.28 | 49.53 | 11.39 | 54.51 | 11.99 |
| Kynurenic acid | 5.81 | 1.05 | 4.80 | 0.96 | 4.50 | 1.04 | 4.32 | 0.95 |
| Taurine | 86.04 | 15.49 | 85.98 | 17.20 | 75.99 | 17.48 | 80.34 | 17.67 |
| L-Acetyl carnitine | 5.52 | 0.99 | 5.73 | 1.15 | 5.41 | 1.24 | 5.58 | 1.23 |
| Creatinine (S) | 75.26 | 13.55 | 74.20 | 14.84 | 65.67 | 15.10 | 105.06 | 23.11 |
Table 6.
The mean values and standard deviations (±SD) of urine concentrations (mM/mM creatinine) of the potential biomarkers targeted in this study for groups C and subgroups P1, P2 and P3.
Table 6.
The mean values and standard deviations (±SD) of urine concentrations (mM/mM creatinine) of the potential biomarkers targeted in this study for groups C and subgroups P1, P2 and P3.
| Molecule | Control (n=20) | P1 (n=30) | P2 (n=30) | P3 (n=30) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean | ±SD | Mean | ±SD | Mean | ±SD | |
| Glycine | 114.89 | 20.68 | 87.36 | 17.47 | 87.43 | 20.11 | 111.39 | 24.51 |
| Tiglylglycine | 22.08 | 3.97 | 17.45 | 3.49 | 16.69 | 3.84 | 29.77 | 6.55 |
| L-tryptophan | 7.63 | 1.37 | 12.14 | 2.43 | 9.03 | 2.08 | 16.64 | 3.66 |
| Kynurenic acid | 0.34 | 0.06 | 0.42 | 0.08 | 0.35 | 0.08 | 0.59 | 0.13 |
| Taurine | 7.6 | 1.37 | 7.58 | 1.52 | 6.65 | 1.53 | 10.72 | 2.36 |
| L-Acetyl carnitine | 0.78 | 0.14 | 0.65 | 0.13 | 0.63 | 0.14 | 0.56 | 0.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated









