Submitted:
02 July 2024
Posted:
03 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
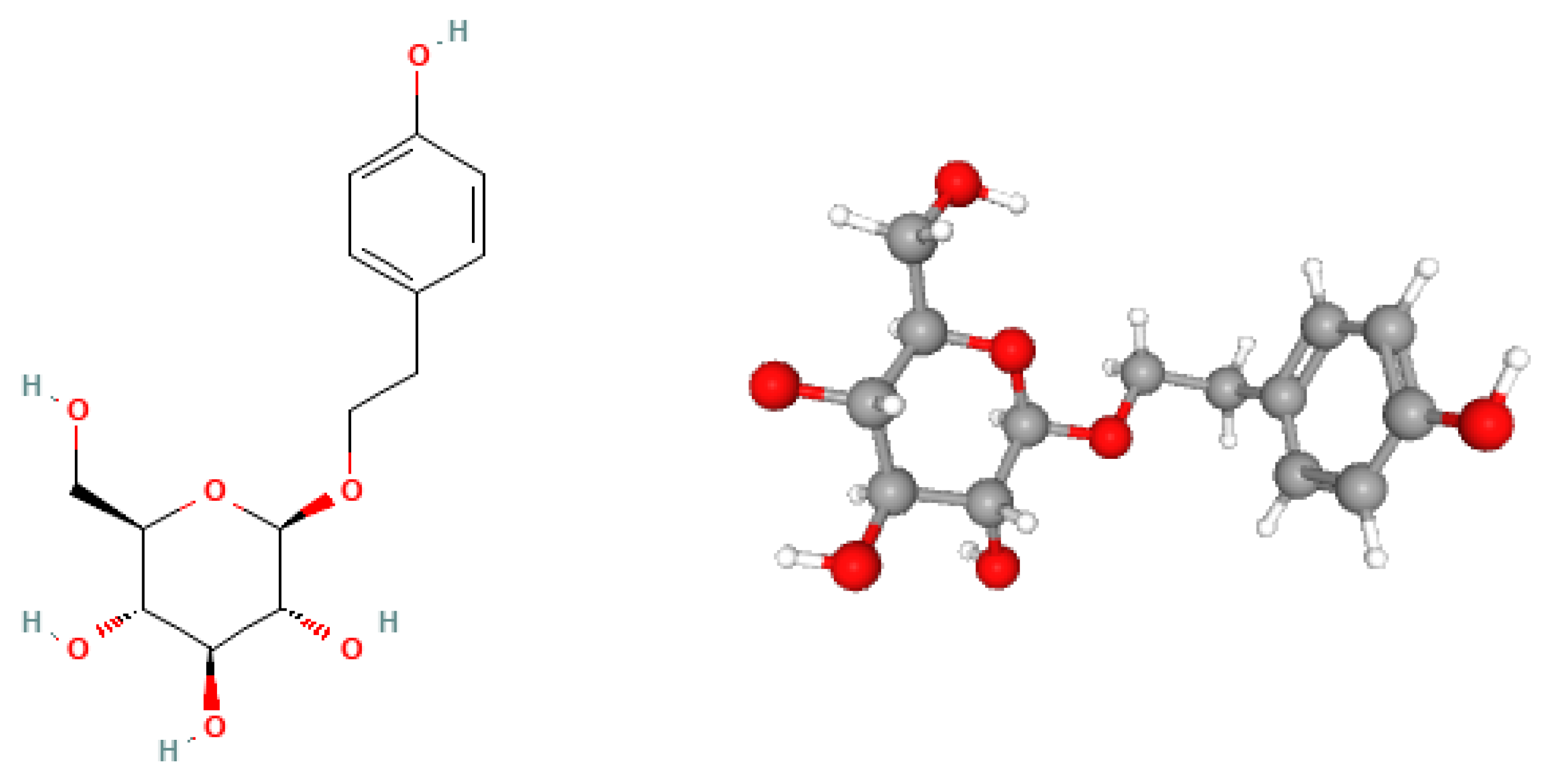
2. Biochemical Structure of Salidroside
3. Influence of Salidroside on Bone Metabolism
3.1. In vitro studies
3.1.1. Proliferation and Differentiation of Osteoblast Precursors
3.1.2. Activation of Bone Morphogenetic Protein 2 Signaling Pathway
3.1.3. Alkaline Phosphatase Activity and Mineralization
3.1.4. Bone Morphogenetic Protein 2, Bone Morphogenetic Protein 6, and Bone Morphogenetic Protein 7 Expression
3.1.5. Adenosine Monophosphate-Activated Protein Kinase Activation
3.1.6. Cellular and Molecular Impact of Salidroside on Endothelial Cells
3.1.7. Proliferation and Viability Assays
3.1.8. Migration and Capillary Tube Formation
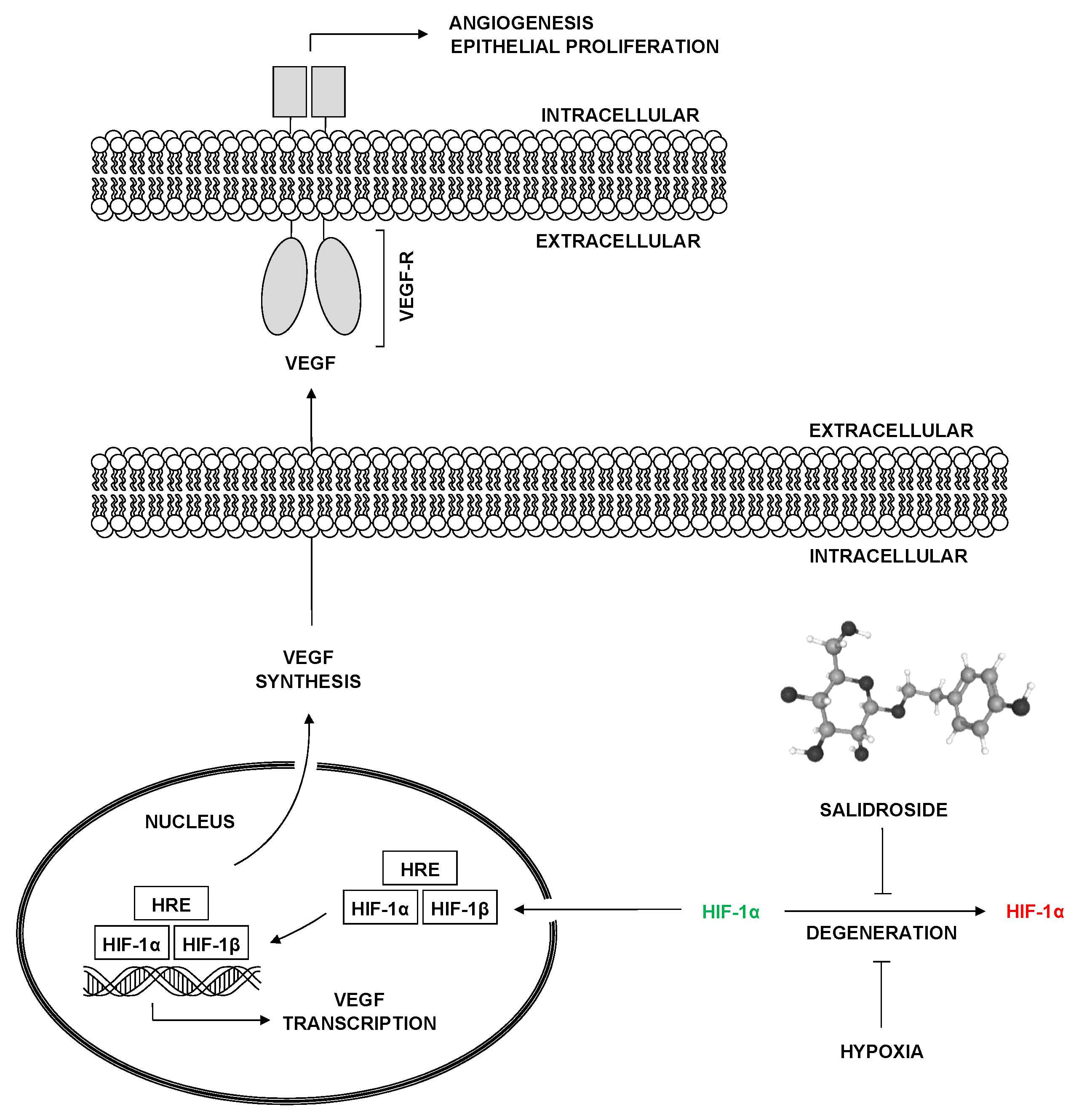
3.1.9. Expression of Hypoxia-Inducible Factor 1-Alpha and Vascular Endothelial Growth Factor
3.1.10. Effects of Salidroside on Glucocorticoid-Induced Osteoporosis
3.1.11. Salidroside's Role in Mitigating Osteoporosis Through Antioxidant Activity
3.2. In Vivo Studies
3.2.1. Protective Effects Against Oxidative Stress
3.2.2. Effects on Knee Osteoarthritis in Mice
3.2.3. Angiogenesis in Mouse Embryonic Metatarsals
3.2.4. Osteogenesis and Bone Healing
3.2.5. Effects on Osteoporosis Model in Rats
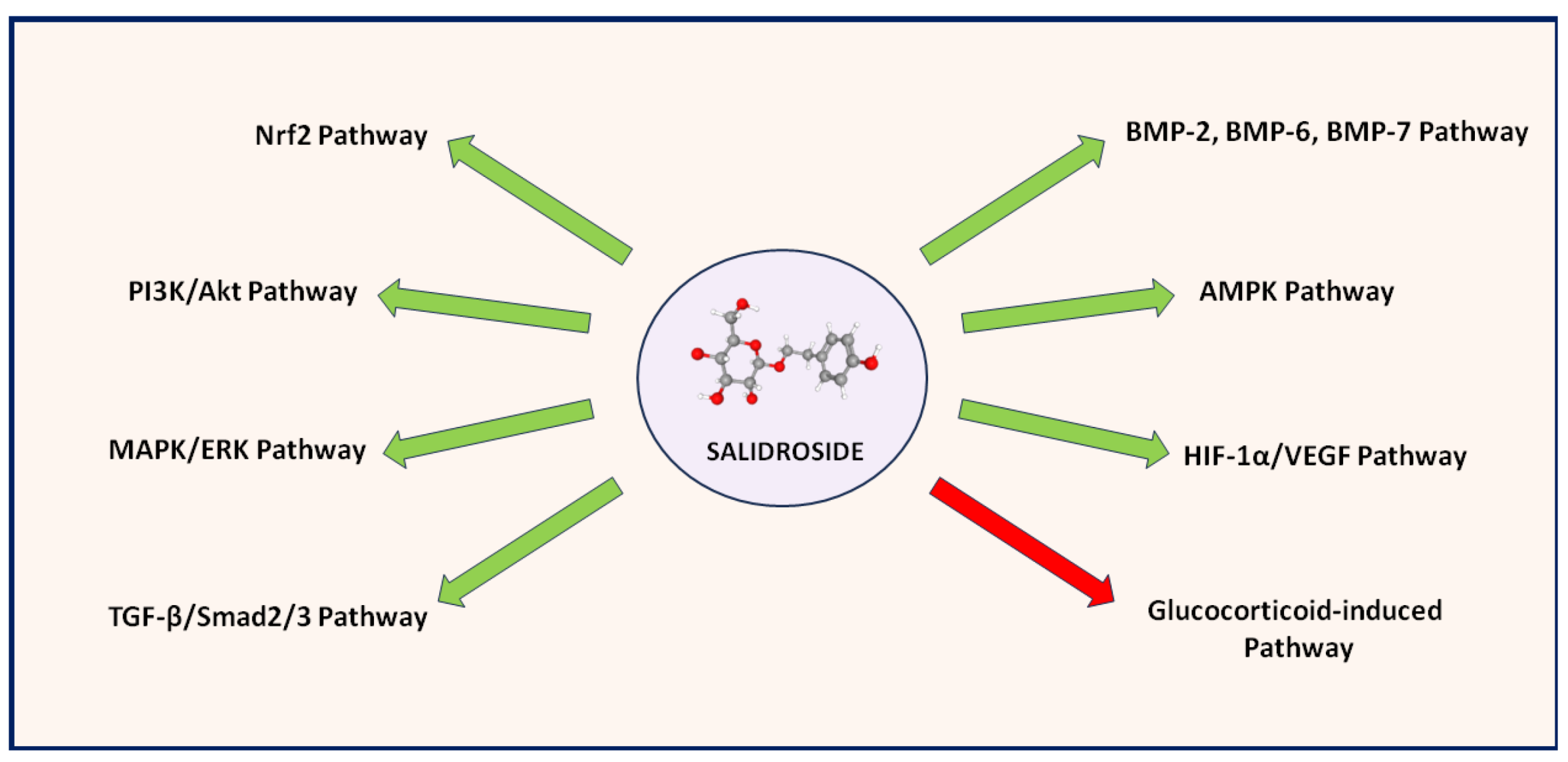
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Panossian, A.; Wikman, G. Effects of Adaptogens on the Central Nervous System and the Molecular Mechanisms Associated with Their Stress-Protective Activity. Pharmaceuticals 2010, 3, 188–224. [Google Scholar] [CrossRef] [PubMed]
- Darbinyan, V.; Aslanyan, G.; Amroyan, E.; Gabrielyan, E.; Malmström, C.; Panossian, A. Clinical trial of Rhodiola rosea L. extract SHR-5 in the treatment of mild to moderate depression. Nordic Journal of Psychiatry 2000, 61, 343–348. [Google Scholar] [CrossRef]
- Olsson, E.M.; von Schéele, B.; Panossian, A.G. A randomised double-blind placebo-controlled parallel-group study of the standardised extract SHR-5 of the roots of Rhodiola rosea in the treatment of subjects with stress-related fatigue. Planta Medica 2009, 75, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Kelly, G.S. Rhodiola rosea: A possible plant adaptogen. Alternative Medicine Review 2001, 6, 293–302. [Google Scholar] [PubMed]
- Brown, R.P.; Gerbarg, P.L.; Ramazanov, Z. Rhodiola rosea: A phytomedicinal overview. HerbalGram 2002, 56, 40–52. [Google Scholar]
- Ishaque, S.; Shamseer, L.; Bukutu, C.; Vohra, S. Rhodiola rosea for physical and mental fatigue: A systematic review. BMC Complementary and Alternative Medicine 2012, 12, 70. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Li, Q.; Yao, L.; Jiang, Z.; Jin, G.; Zhao, X. Salidroside: Advances in pharmacological activities and molecular mechanisms of action. Journal of Ethnopharmacology 2020, 261, 113112. [Google Scholar] [CrossRef]
- Chan, Y.S.; Cheng, L.N.; Wu, J.H.; Chan, E.; Kwan, Y.W.; Lee, S.M.; Leung, G.P.; Yue, P.Y.; Wong, R.N. A review of the pharmacological effects of Rhodiola rosea L. and its bioactive compounds. Phytotherapy Research 2012, 26, 1727–1734. [Google Scholar] [CrossRef]
- Zhang, J.; Zeng, Y.; Li, Y.; Lu, D.; Wang, X.; Ji, X. Salidroside regulates cardiac dysfunction in heart failure by enhancing mitochondrial biogenesis and inhibiting oxidative stress. Biomedicine & Pharmacotherapy 2018, 105, 119–128. [Google Scholar] [CrossRef]
- Li, Y.; Pham, V.; Bui, M.; Song, L.; Wu, C.; Walia, A.; Uchio, E.; Smith-Liu, F.; Zi, X. Rhodiola rosea: An herb with anti-stress, anti-aging, and anti-cancer properties. Cancer Cell International 2019, 19, 202. [Google Scholar]
- Hernlund, E.; Svedbom, A.; Ivergård, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jönsson, B.; Kanis, J.A. Osteoporosis in the European Union: medical management, epidemiology, and economic burden. Archives of Osteoporosis 2013, 8, 136. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; Liu, E.; Vandenput, L.; McCloskey, E.V. SCOPE 2021: a new scorecard for osteoporosis in Europe. Archives of Osteoporosis 2022, 17, 104. [Google Scholar] [CrossRef] [PubMed]
- Pisani, P.; Renna, M.D.; Conversano, F.; Casciaro, E.; Di Paola, M.; Quarta, E.; Muratore, M.; Casciaro, S. Major osteoporotic fragility fractures: Risk factor updates and societal impact. World Journal of Orthopedics 2016, 7, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Huang, K.; Xu, H. Protective effects of Rhodiola rosea on oxidative stress and liver injury in rats. Molecular and Cellular Biochemistry 2009, 331, 31–41. [Google Scholar]
- Fan, X.J.; Wang, Y.; Wang, L.; Zhu, M. Salidroside induces apoptosis and autophagy in human colorectal cancer cells through inhibition of PI3K/Akt/mTOR pathway. Oncology Reports 2016, 6, 3559–3567. [Google Scholar] [CrossRef] [PubMed]
- György, Z.; Hohtola, A. Production of cinnamyl glycosides in compact callus aggregate cultures of Rhodiola rosea through biotransformation of cinnamyl alcohol. In Protocols for in vitro cultures and secondary metabolite analysis of aromatic and medicinal plants; Jain, S.M., Saxena, P.K., Eds.; Humana Press: Totowa, NJ, USA, 2009; pp. 305–312. [Google Scholar]
- Panossian, A.; Wikman, G.; Sarris, J. Rosenroot (Rhodiola rosea): Traditional use, chemical composition, pharmacology, and clinical efficacy. Phytomedicine 2010, 17, 481–493. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Wang, Y.; Guo, H.; Li, W.; Yan, S.; Zhao, S. Phytochemical analysis of traditional Chinese medicine using liquid chromatography coupled with mass spectrometry. Journal of Chromatography A 2015, 1428, 155–165. [Google Scholar] [CrossRef]
- Grech-Baran, M.; Sowa-Kasprzak, K. Salidroside as an adaptogen compound. Natural Product Communications 2013, 8, 1435–1440. [Google Scholar] [CrossRef]
- Panossian, A.; Wikman, G. Pharmacology of Schisandra chinensis Bail. : An overview of Russian research and uses in medicine. Journal of Ethnopharmacology 2009, 118, 183–212. [Google Scholar] [CrossRef]
- Chen, J.J.; Zhang, N.F.; Mao, G.X.; He, X.B.; Zhan, Y.C.; Deng, H.B.; Wang, Z. Salidroside stimulates osteoblast differentiation through BMP signaling pathway. Food and Chemical Toxicology 2013, 62, 499–505. [Google Scholar] [CrossRef]
- Pan, X.; Peng, X.; Jiang, C.; Yu, H.; Yang, Y.; Chen, H. Salidroside promotes the osteogenic differentiation of rat bone marrow mesenchymal stem cells through the BMP/Smad pathway. Drug Design Development and Therapy 2019, 13, 2501–2511. [Google Scholar]
- Li, J.; Guo, W. The effects of salidroside on bone marrow mesenchymal stem cells and their application in the treatment of osteoporosis. Life Sciences 2018, 207, 333–340. [Google Scholar] [CrossRef]
- Pan, X.; Liu, H.; Liu, J.; Shu, B.; Sun, L. Salidroside promotes osteogenic differentiation and bone formation in primary rat bone marrow stromal cells. Experimental and Therapeutic Medicine 2013, 5, 1265–1273. [Google Scholar] [CrossRef]
- Fu, S.; Yan, M.; Fan, Q.; Xu, J. Salidroside promotes osteoblast proliferation and differentiation via the activation of AMPK to inhibit bone resorption in knee osteoarthritis mice. Tissue Cell 2022, 79, 101917. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q.; Yang, J.; Chen, Y.; Jin, X.; Li, Z.; Wen, X.; Xia, Q.; Wang, Y. Salidroside improves angiogenesis-osteogenesis coupling by regulating the HIF-1α/VEGF signalling pathway in the bone environment. European Journal of Pharmacology 2020, 884, 173394. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.Q.; Qi, L.; Yang, J.; Wang, Y.; Wang, C.; Li, Z.M.; Li, L.; Qu, Y.; Wang, D.; Han, Z.M. Salidroside accelerates fracture healing through cell-autonomous and non-autonomous effects on osteoblasts. Cell Tissue Research 2017, 367, 197–211. [Google Scholar] [CrossRef]
- Xie, B.; Zhou, H.; Liu, H.; Liao, S.; Zhou, C.; Xu, D. Salidroside alleviates dexamethasone-induced inhibition of bone formation via transforming growth factor-beta/Smad2/3 signaling pathway. Phytotherapy Research 2023, 37, 1938–1950. [Google Scholar] [CrossRef] [PubMed]
- Xue, X.; Feng, Z.; Li, Z.; Pan, X. Salidroside inhibits steroid-induced avascular necrosis of the femoral head via the PI3K/Akt signaling pathway: In vitro and in vivo studies. Molecular Medicine Reports 2018, 17, 3751–3757. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.F.; Chang, Y.Y.; Zhang, X.M.; Gao, M.T.; Zhang, Q.L.; Li, X.; Zhang, L.; Yao, W.F. Salidroside protects against osteoporosis in ovariectomized rats by inhibiting oxidative stress and promoting osteogenesis via Nrf2 activation. Phytomedicine 2022, 99, 154020. [Google Scholar] [CrossRef]
- Zhang, J.K.; Yang, L.; Meng, G.L.; Yuan, Z.; Fan, J.; Li, D.; Liu, J. Protection by salidroside against bone loss via inhibition of oxidative stress and bone-resorbing mediators. PloS One 2013, 8, e57251. [Google Scholar] [CrossRef]
- Li, L.; Qu, Y.; Jin, X.; Guo, X.Q.; Wang, Y.; Qi, L.; Yang, J.; Zhang, P.; Li, L.Z. Protective effect of salidroside against bone loss via hypoxia-inducible factor-1α pathway-induced angiogenesis. Scientific Reports 2016, 6, 32131. [Google Scholar] [CrossRef]
- Zheng, H.; Qi, S.; Chen, C. Salidroside Improves Bone Histomorphology and Prevents Bone Loss in Ovariectomized Diabetic Rats by Upregulating the OPG/RANKL Ratio. Molecules 2018, 23, 2398. [Google Scholar] [CrossRef]
- Wang, S.; Feng, Y.; Zheng, L.; He, P.; Tan, J.; Cai, J.; Wu, M.; Ye, X. Rosavin: Research Advances in Extraction and Synthesis, Pharmacological Activities and Therapeutic Effects on Diseases of the Characteristic Active Ingredients of Rhodiola rosea L. Molecules 2023, 28, 7412. [Google Scholar] [CrossRef] [PubMed]
- Wojdasiewicz, P.; Turczyn, P.; Lach-Gruba, A.; Poniatowski, Ł.A.; Purrahman, D.; Mahmoudian-Sani, M.-R.; Szukiewicz, D. The Role of Rosavin in the Pathophysiology of Bone Metabolism. Int. J. Mol. Sci. 2024, 25, 2117. [Google Scholar] [CrossRef] [PubMed]
- Jamróz, W.; Arafat, B.; Gultekin, H.E. 3D-printed dosage forms for oral administration: a review. Drug Delivery and Translational Research 2023, 13, 210–223. [Google Scholar]
- Pan, X.; Liu, H.; Liu, J.; Shu, B.; Sun, L. Advances in Oral Drug Delivery Systems: Challenges and Opportunities. Pharmaceutics 2023, 15, 484. [Google Scholar] [CrossRef] [PubMed]
| First Author, Year (Reference) | Cell Lines | Biological manifestation |
|---|---|---|
| Pan et al., 2013 [24] | rBMSC | Promotion of osteoblast differentiation and bone formation, upregulation of osteogenic markers ALP and COL1A1. |
| Guo et al., 2017 [27] | MG-63, ROB | Enhanced proliferation and differentiation of osteoblasts, activation of MAPK/ERK and PI3K/Akt pathways, increased Runx2 and OSX expression. |
| Li et al., 2018 [23] | rBMSC | Increased osteogenic differentiation, enhanced ALP activity, and mineralization, promotion of bone formation, increased expression of Runx2 and ALP. |
| Xue et al., 2018 [29] | ROB | Protection against apoptosis, activation of PI3K/Akt pathway, reduction of apoptotic markers such as BAX, CASP3, and CASP9, increased expression of Runx2 and OSX. |
| Chen et al., 2019 [21] | C3H10T1/2, MC3T3-E1, rBMSC | Increased proliferation and differentiation of osteoblasts, enhanced ALP activity, and mineralization via BMP/Smad pathway activation, increased expression of Runx2 and OSX. |
| Guo et al., 2020 [26] | EA.hy926, HUVEC, MG-63, ROB | Increased proliferation, migration, capillary formation, and mineralization through HIF-1α/VEGF pathway activation, increased expression of ALP, Runx2, OSX, and VEGF. |
| Fu et al., 2022 [25] | MC3T3-E1 | Enhanced proliferation and differentiation of osteoblasts, AMPK activation, inhibition of bone resorption, increased expression of ALP, COL1A1, OCN, and Runx2. |
| Wang et al., 2022 [30] | ROB | Protection against oxidative stress, increased Nrf2 activation, decreased Keap1 expression, promotion of osteogenesis, increased expression of ALP and Runx2. |
| Xie et al., 2023 [28] | MC3T3-E1 | Protection against dexamethasone-induced inhibition, increased ALP activity, activation of TGF-β/Smad2/3 pathway, increased expression of OSX and ALP. |
| First Author, Year (Reference) | Animal Model | Biological effect |
|---|---|---|
| Pan et al., 2013 [24] | Sprague Dawley rats (OVX-induced bone loss model) | Reduced oxidative stress, increased bone mass, reduced RANKL, increased OPG. |
| Guo et al., 2017 [27] | BALB/c mice (tibia fracture model) | Accelerated fracture healing, enhanced osteoblast proliferation and differentiation, increased HIF-1α and VEGF. |
| Li et al., 2018 [23] | Sprague Dawley rats (OVX-induced OP model) | Increased bone mass and mineral apposition rates, improved bone microarchitecture, increased HIF-1α and VEGF. |
| Xue et al., 2018 [29] | Sprague Dawley rats (SANFH model) | Reduced osteoblast apoptosis, increased osteogenic differentiation via PI3K/Akt, increased Bcl-2, decreased BAX and CASP3. |
| Zheng et al., 2018 [33] | Sprague Dawley rats (OVX-induced OP model with diabetes) | Improved bone histomorphology, prevention of bone loss, upregulation of the OPG/RANKL ratio |
| Chen et al., 2019 [21] | C57BL/6 mice (oxidative stress model) | Preserved bone microstructure, reduced MDA and ROS, increased osteoblast function and antioxidant enzymes such as SOD and GSH-Px. |
| Guo et al., 2020 [26] | C57BL/6 mice (angiogenesis model using mouse embryonic metatarsals) | Enhanced endothelial sprouting, increased VEGF, increased CD31-positive endothelial cells. |
| Fu et al., 2022 [25] | C57BL/6 mice (KOA model) | Reduced inflammation, increased osteogenic protein expression, enhanced AMPK activation, reduced TNF-α, IL-1β, and IL-6. |
| Wang et al., 2022 [30] | Sprague Dawley rats (OVX-induced OP model) | Reduced oxidative stress, increased osteogenesis via Nrf2, increased Runx2, ALP, and OCN. |
| Xie et al., 2023 [28] | C57BL/6 mice (dexamethasone-induced OP model) | Mitigated inhibitory effects of dexamethasone on osteogenesis, activated TGF-β/Smad2/3, increased ALP and COL1A1. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





