1. Introduction
Anesthesiological procedures are widely used in various fields of dentistry with the aim of reducing patient discomfort when the treatment would be painful [
1].
The type of anesthesia depends on the dental therapy, the duration of the anesthetic block and the anatomical region affected [
2].
Among the most used anesthesia, we have the local infiltration of anesthetic, which is usually injected near the fornix in correspondence with the affected teeth with the possible addition of a further infiltration of anesthetic either palatal or lingual.
In some clinical situations it is also convenient to carry out a more important anesthetic block such as that relating to the inferior alveolar nerve [
3].
In other clinical conditions, can be also performed, intraligamentary anesthesia, carried out directly in the gingival sulcus, or the intrapulpal if the anesthetic is injected directly into the pulp [
4,
5].
All these different anesthetic methods involve different types of needles, even with different lengths, whose diameters can still be traced back to two different sizes: 27G, used mainly for the block of the inferior alveolar nerve and 30G for the remaining conditions [
6,
7].
The dentist may need to infiltrate the anesthetic into multiple places and this is usually done with the same needle which is forced to pass through the soft tissue several times to distribute the anesthetic solution over a larger area.
In Europe, anesthesia needles in dentistry follow Regulation (EU) 2017/745 which places them in class II subclass A which includes medium risk instruments that penetrate the body even only partially, through an orifice or a body surface and whose duration of use can be more than 30 days.
The needles are made of AISI 304 (UNI X5CrNi18-10) medical grade stainless steel that is a nickel-chromium alloy, austenitic, non-hardenable, hardenable by cold deformation, which allows good mechanical workability [
8].
More precisely, 304 stainless steel is a stainless steel from the austenitic steel family, it is non-magnetic and is composed of a chromium content between 18% and 20% and a nickel content between 8% and 11%.
Given the reduced carbon content, AISI 304 is little subject to intercrystalline corrosion and has corrosion resistance towards a large variety of chemical substances used in the medical field. This alloy is resistant to corrosion thanks to the passivation phenomenon as the chemical elements present in the alloy react easily with the surrounding environment and in particular the chromium forms a small protective film which avoids corrosive attacks on the steel [
9,
10].
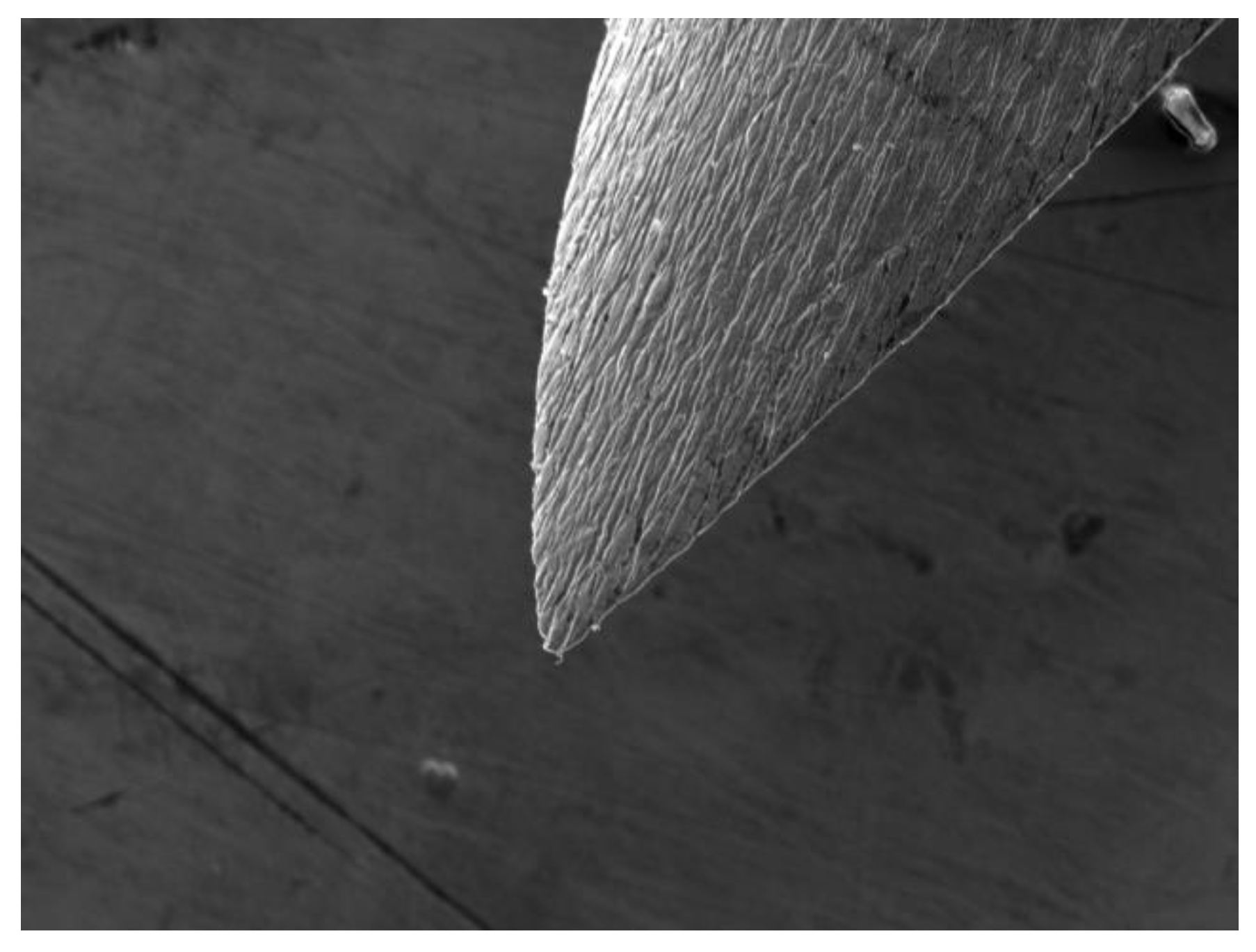
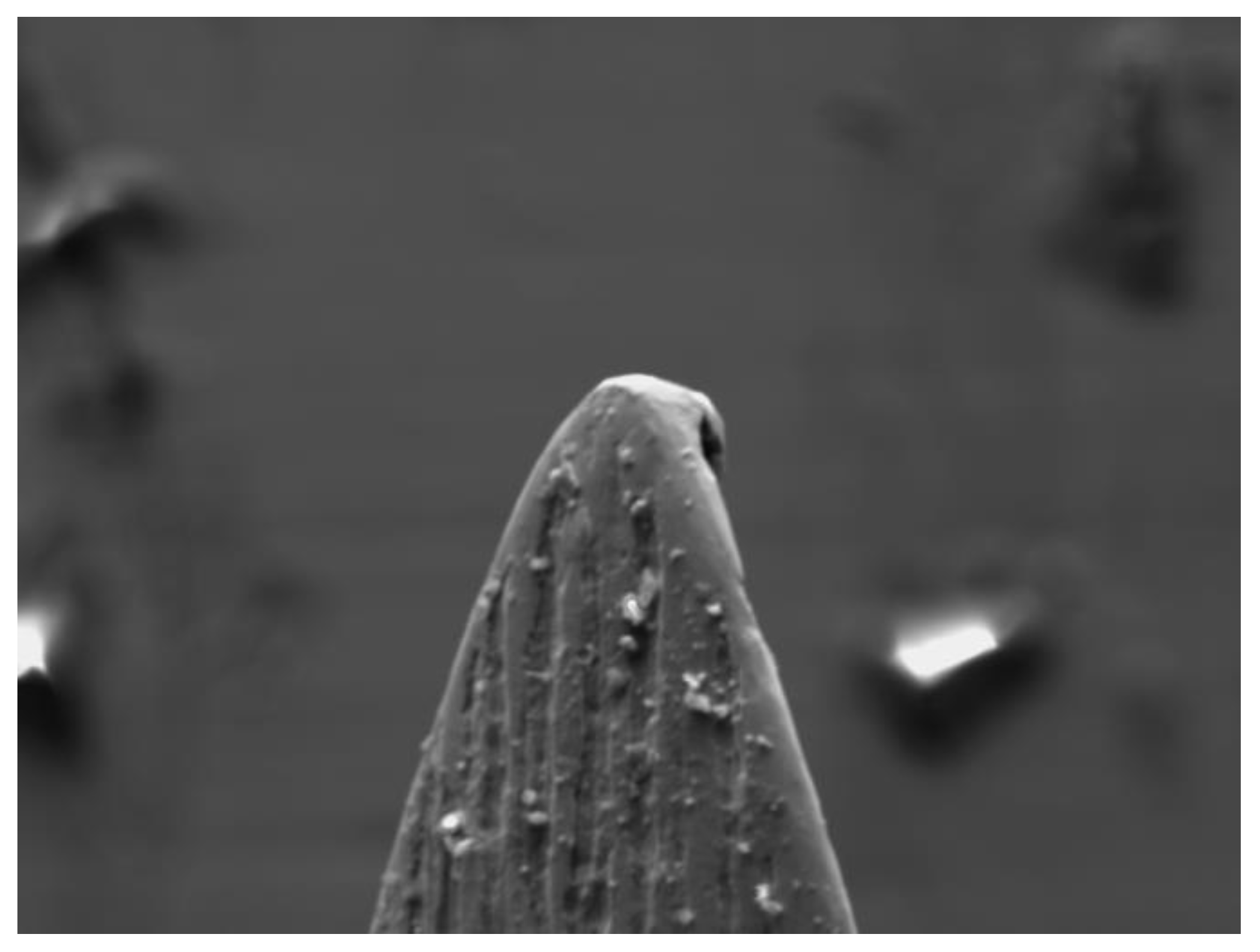
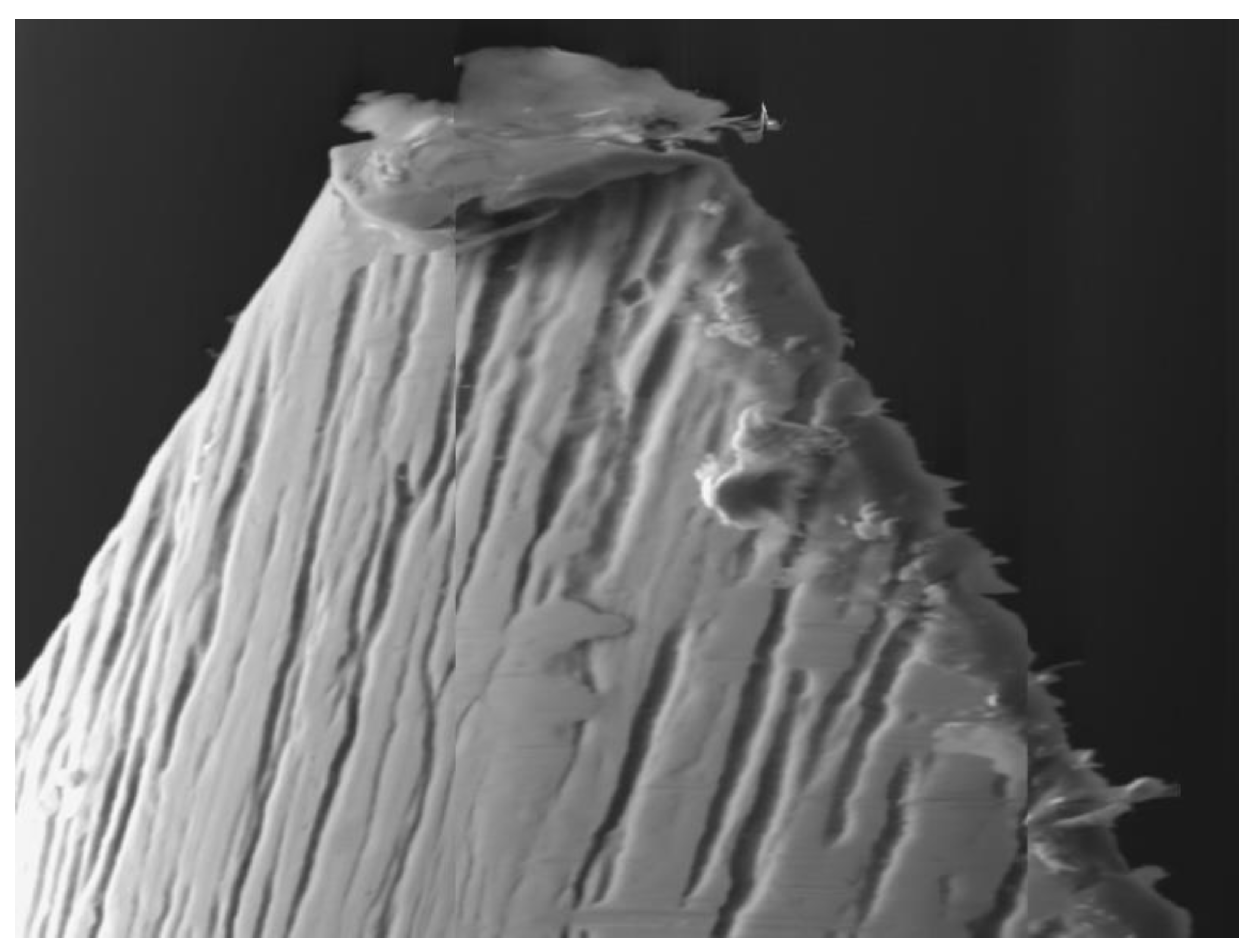
In order to reduce both the painful sensation of the needle pricking the tissues and the trauma induced on them, the end of the needle has a particular bevel shape which, sharp and cutting, easily penetrates both the mucosa and the soft tissues below (
Figure 1).
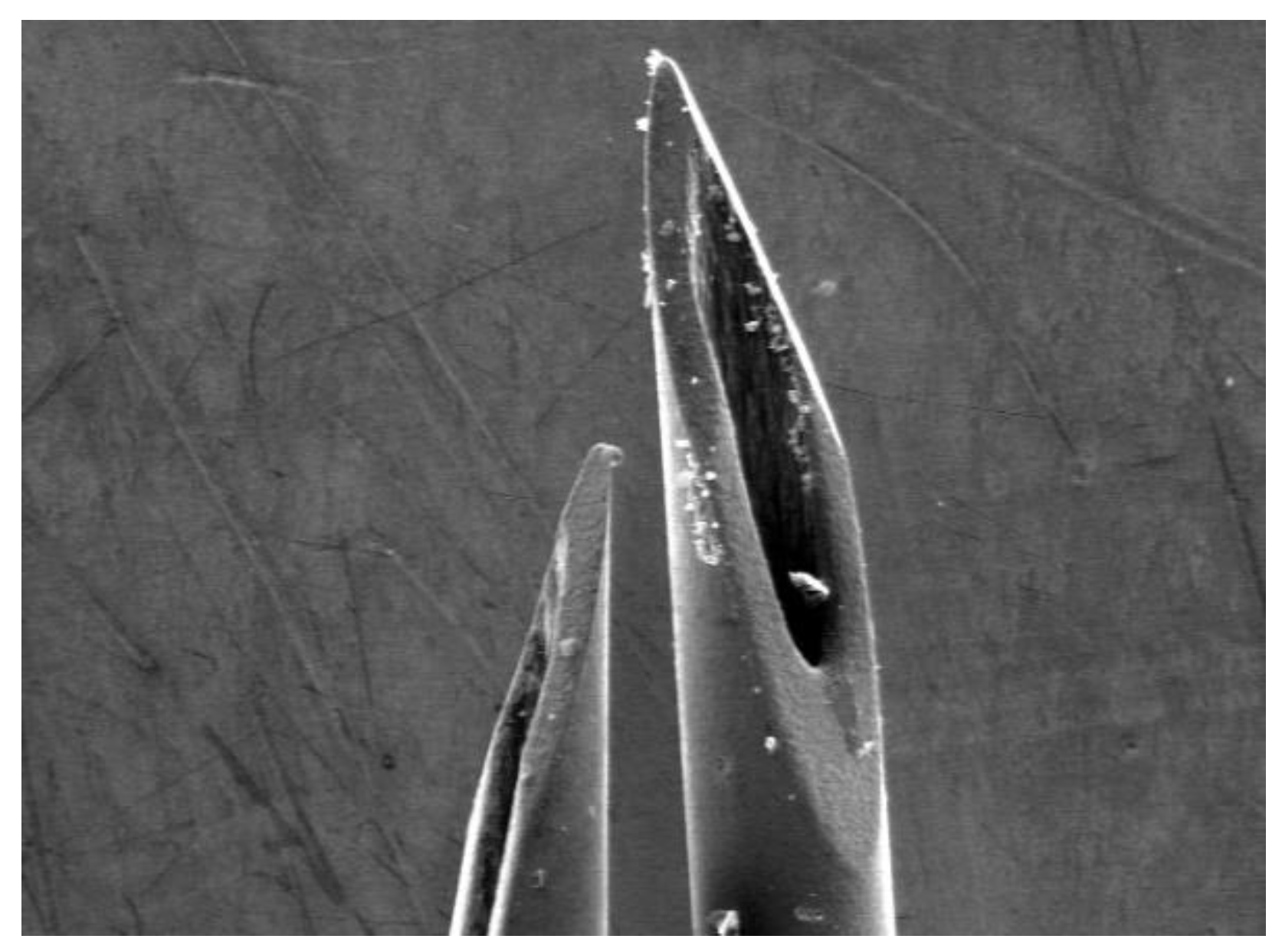
The shape of the chamfer, for 30G diameter dental anesthesia needles, is triple-sharpened: the terminal part of the needle is initially sharpened like a flute, creating a first bevel which is followed by two other sharpenings that create two more lateral bevels on the terminal part of the tip to make it even sharper (
Figure 2).
The bevel design of a dental needle significantly influences the force required for penetration and the pain perceived by patients [
11].
Research indicates that needles with a chisel-designed bevel require less penetration force, thus potentially reducing patient discomfort during the injection [
12].
In contrast, needles with a standard bevel may induce more pain due to increased resistance during tissue penetration.
Sharper and more pointed needle bevel designs may also result in a higher rate of needle deformations by soft tissue and bone contact [
13].
All needles used to introduce medications, including local anesthetics, into the tissue environment must maintain structural integrity to ensure effectiveness and minimize patient discomfort.
This delicate part of the needle, because of its shape and the thin thicknesses, is susceptible to deformation after use, especially if repeated, with the appearance of barbs or irregularities which can both limit its ability to penetrate in soft tissues and induce micro-traumas in the areas where the anesthetic is injected [
14] (
Figure 3).
The present study aims to evaluate, through a morphological analysis under a scanning electron microscope (SEM), how the beveled tip of a 30G needle, used to inject anesthetic several times into different areas of the vestibular mucosa, changes.
SEM provides high-resolution images that allow detailed observation of dental anesthesia needle tip deformation providing information on their structural integrity and clinical performance.
In detail, our study simulates a real clinical condition in which the dentist injects the total dose of anesthetic by distributing it over several points, subjecting the bevel of the same needle to cut the soft tissues several times, progressively losing the original sharpness.
In the literature, anesthesia needles have already been studied, in fact some SEM analyzes reveal that dental needles often undergo deformations after use, compromising their performance. Deformations such as bending or barb formation may occur due to mechanical forces exerted during injection [
15,
16].
Studies have shown that a significant percentage of dental needles exhibit deformations after use, with barbed needles observed in approximately 60% of cases. These deformations can be attributed to the mechanical stress experienced during insertion and manipulation within the tissue [
17].
The clinical implications of needle deformation are multiple; deformed needles can increase the risk of trauma to soft tissue, blood vessels and nerves, potentially causing persistent pain or iatrogenic damage [
18,
19,
20,
21].
Furthermore, impaired flow of anesthetic solutions, through deformed needles, may compromise the effectiveness of anesthesia, resulting in inadequate pain control and the need for additional injections.
The gauge of anesthesia needles used in dentistry also plays a critical role in its susceptibility to deformation. For example, larger diameter needles such as 27G have greater mechanical resistance than 30G needles, which fracture more frequently under mechanical stress. This difference in performance highlights the importance of choosing a needle of appropriate gauge and morphology for each specific clinical condition to ensure both efficacy and safety [
22].
These structural changes not only increase patient discomfort, but can also reduce the effectiveness of anesthetic delivery, making additional injections necessary.
The literature lacks scientific research that investigates how the tip of the needle changes and modifies in the case of multiple injections, a frequent condition in daily practice. Our morphological study fills this gap in the literature.
By understanding the factors that contribute to needle deformation and selecting appropriate needle designs, the dental community can improve clinical outcomes and patient comfort during dental procedures.
Continuous research and adherence to safety standards are essential to optimize needle performance and reduce complications.
2. Materials and Methods
This study, which was conducted in vivo on patients who required dental care to be carried out after local regional anesthesia, had as its aim the morphological SEM analysis of 30G needles, 21mm long with triple sharpening bevel produced by 2 different manufacturers, used to inject local anesthetic (Articaina Cartidont Curasept with adrenaline 1:100,000 Saronno Italy).
The clinical research adhered to the principles outlined in the Declaration of Helsinki and received approval from the Institutional Review Board of the Paolo Giaccone University of Palermo (Protocol Code: #4-19-04-23). All patients participating in the study were provided with a declaration of consent, which they read and signed to express their willingness to participate in the research and to consent to the publication of data.
By conducting the study in accordance with ethical guidelines and obtaining informed consent from participants, we ensured the ethical conduct of the research while also respecting the rights and well-being of the individuals involved.
A total of 192 patients were selected who had to carry out the following therapies: tooth extractions, root planing, endodontic and conservative restorations.
The patients were aged between 18 and 60, 99 males and 91 females, all of Italian nationality.
The needles used (30G x 21mm) to perform anesthesia were divided into two groups based on the manufacturer according to the following scheme:
Group A: 30G x 21 mm needles produced by Biodent Co Ltd, Paju Korea.
Group B: 30G x 21 mm needles produced by Medibase Tecnofar Spa, Delebio Italy.
Ninety-six patients were anesthetized with Group A needles and the remaining 96 with Group B needles; the division of patients was random.
Based on the clinical use on the patient, six subgroups were created according to the following scheme:
Subgroup 1: needles used for a single administration of anesthetic;
Subgroup 2: needles used for two consecutive adjacent anesthetic injections;
Subgroup 3: needles used for three consecutive adjacent anesthetic injections;
Subgroup 4: needles used for four consecutive adjacent anesthetic injections;
Subgroup 5: needles used for five consecutive adjacent anesthetic injections;
Subgroup 6: needles used for six consecutive adjacent anesthetic injections;
By combining groups A and B with the subgroups the research provided 12 different possibilities:
A1, A2, A3, A4, A5, A6, B1, B2, B3, B4, B5, B6. (
Table 1)
For each possible combination, 16 patients were treated for a total of 192 patients.
In order to adapt the tested combination to clinical needs, patients who had to undergo conservative therapies had one or two local infiltrations of anesthetic in vestibular soft tissues in correspondence with the tooth to be treated (combinations A1, A2, B1 and B2).
The patients who had to carry out endodontic treatments had 3 infiltrations of local anesthetic with the same needle, all vestibular and sequential at a distance of about one centimeter from each other (combination A3 or B3).
Patients who needed tooth extractions received four sequential infiltrations of anesthetic with the same needle on the vestibular mucosa at a distance of one centimeter from each other (combination A4 or B4).
Patients who needed root planing on six teeth received 5 or 6 sequential infiltrations of anesthetic with the same needle on the buccal mucosa at a distance of one centimeter from each other (combinations A5, A6, B5 and B6).
Table 1.
Combinations between groups and subgroups.
Table 1.
Combinations between groups and subgroups.
| Group + subgroup |
Descrizione |
No. patients |
Group + subgroup |
Descrizione |
No. patients |
| A + 1 |
Biodent
1 injection
Conservative therapy |
16 |
B + 1 |
Medibase
1 injection
Conservative therapy |
16 |
| A + 2 |
Biodent
2 injections
Conservative therapy |
16 |
B + 2 |
Medibase
2 injections
Conservative therapy |
16 |
| A + 3 |
Biodent
3 injections
Endodontic therapy |
16 |
B + 3 |
Medibase
3 injections
Endodontic therapy |
16 |
| A + 4 |
Biodent
4 injections
Tooth extraction |
16 |
B + 4 |
Medibase
4 injections
Tooth extraction |
16 |
| A + 5 |
Biodent
5 injections
Root planing |
16 |
B + 5 |
Medibase
5 injections
Root planing |
16 |
| A + 6 |
Biodent
6 injections
Root planing |
16 |
B + 6 |
Medibase
6 injections
Root planing |
16 |
All injections were conducted by one dentist to avoid the possible influence of different examiners.
All anesthetic injections were made using a three-ring steel syringe (GNZ Dental), in the mucosa without touching the periosteum in order to evaluate the impact of the sharp bevel only against the soft tissues; all injections were performed following the international guidelines [
23,
24].
If, for clinical purposes, it was necessary to vary or integrate the anesthetic protocol, other needles were used which were outside the context of the research and therefore were not observed under SEM.
After clinical use, each needle was cleaned from the inside of any organic residues by inserting it into syringes with anesthetic cartridges that were first emptied and then filled with distilled water.
When handling each needle, care was taken to prevent the bevel from coming into contact with other surfaces in order not to further alter this delicate area.
For electron microscopy needs, all needles were finally cut 2 cm from the tip, individually wrapped in paper-film and for safety reasons, subjected to a sterilization cycle in autoclave at 132°C for 12 minutes.
The needles were subjected to SEM observation (JEOL Jsm 6390 LV) by positioning them on suitable supports for electronic microscopy; the morphological analysis under the scanning microscope was carried out using the secondary electron detector in order to have maximum detail of the surface morphology of the needles to highlight any deformations due to the impact with the soft tissues.
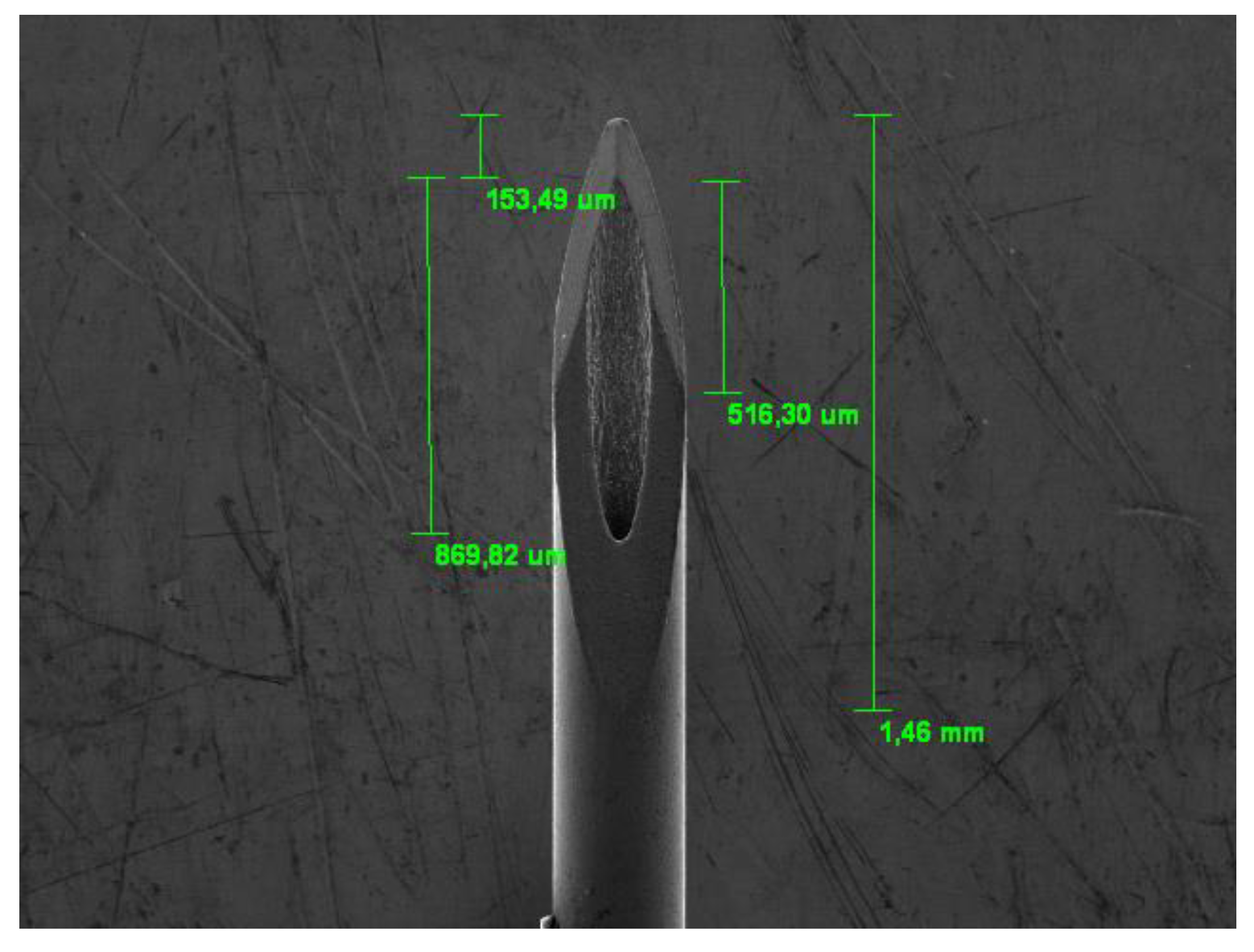
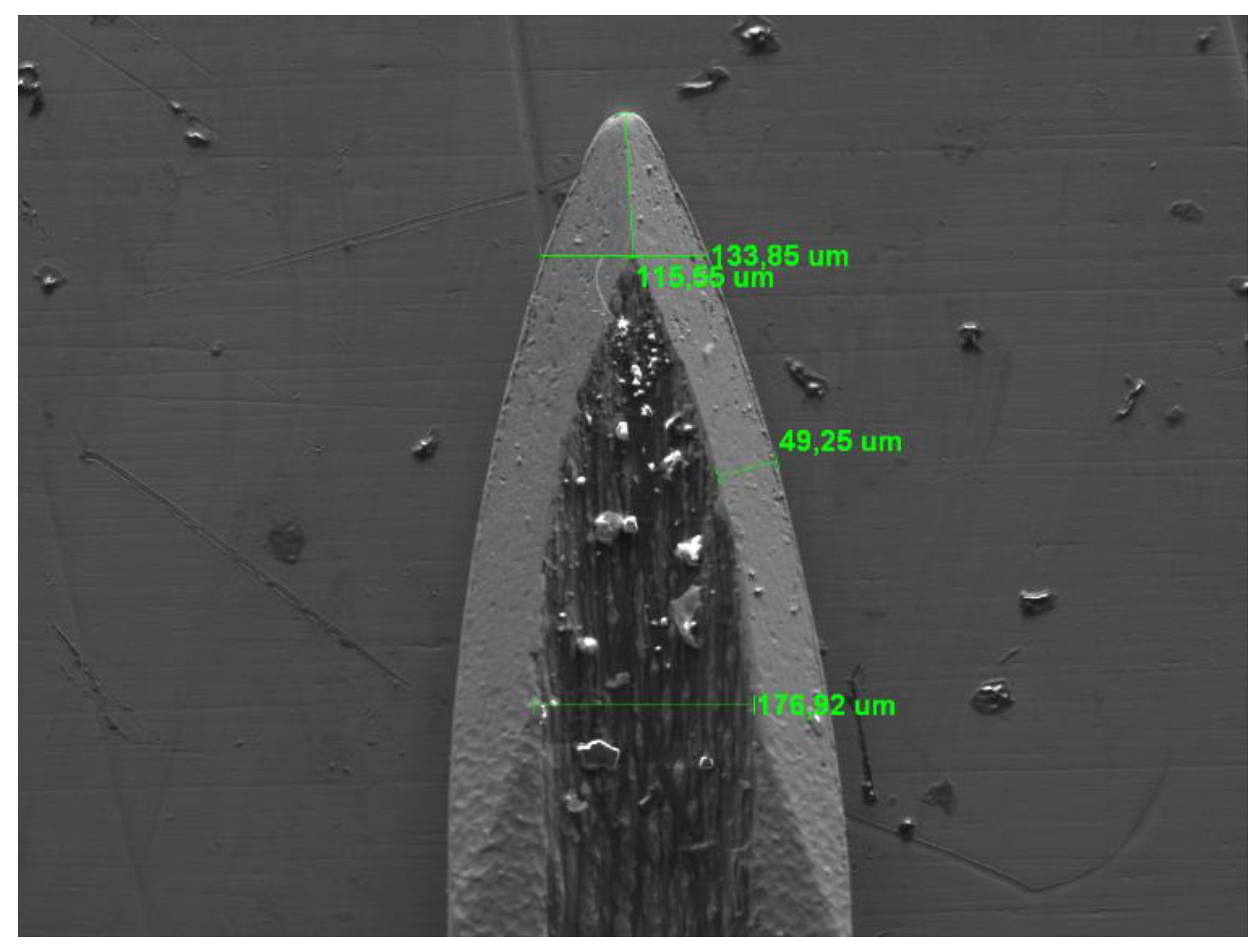
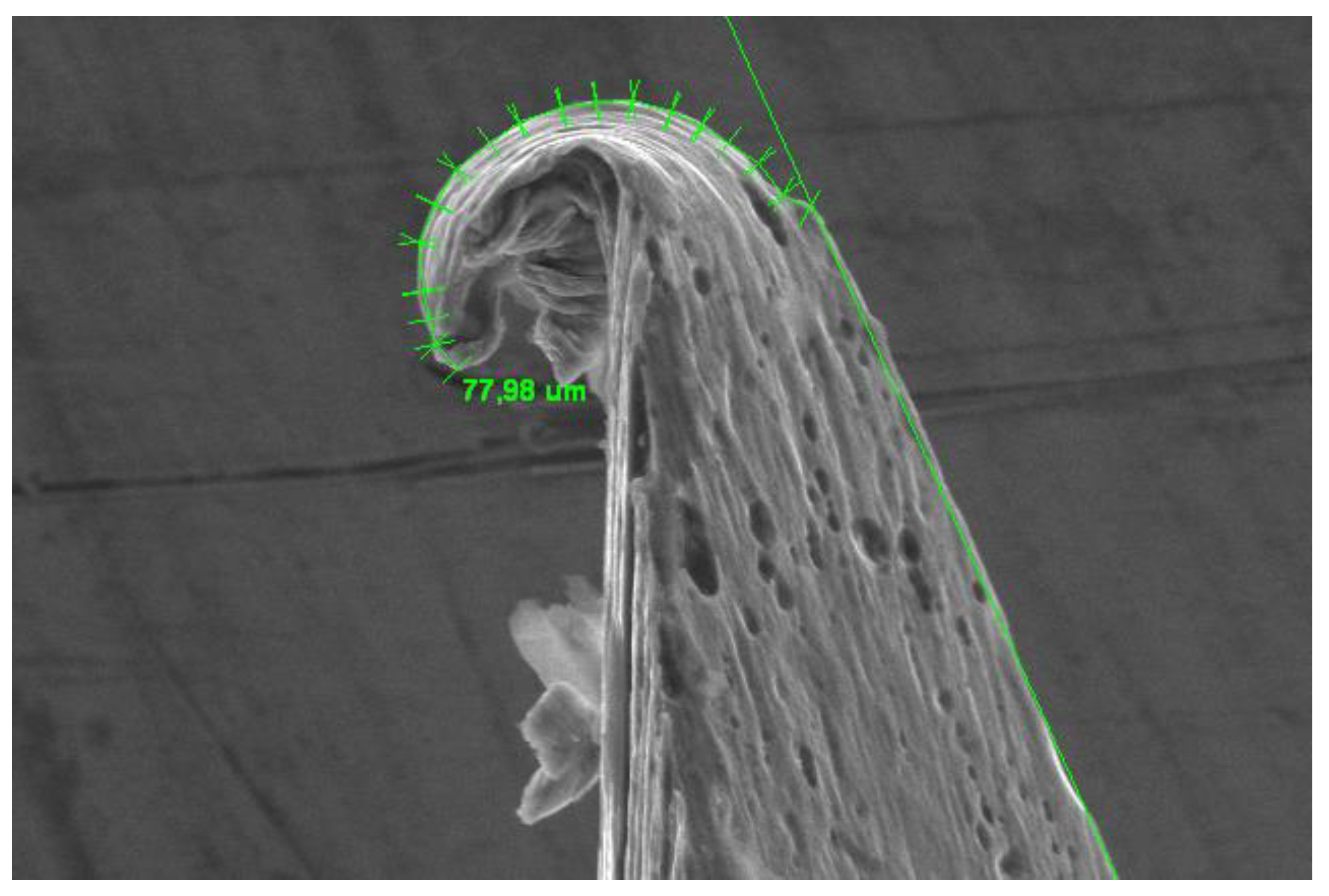
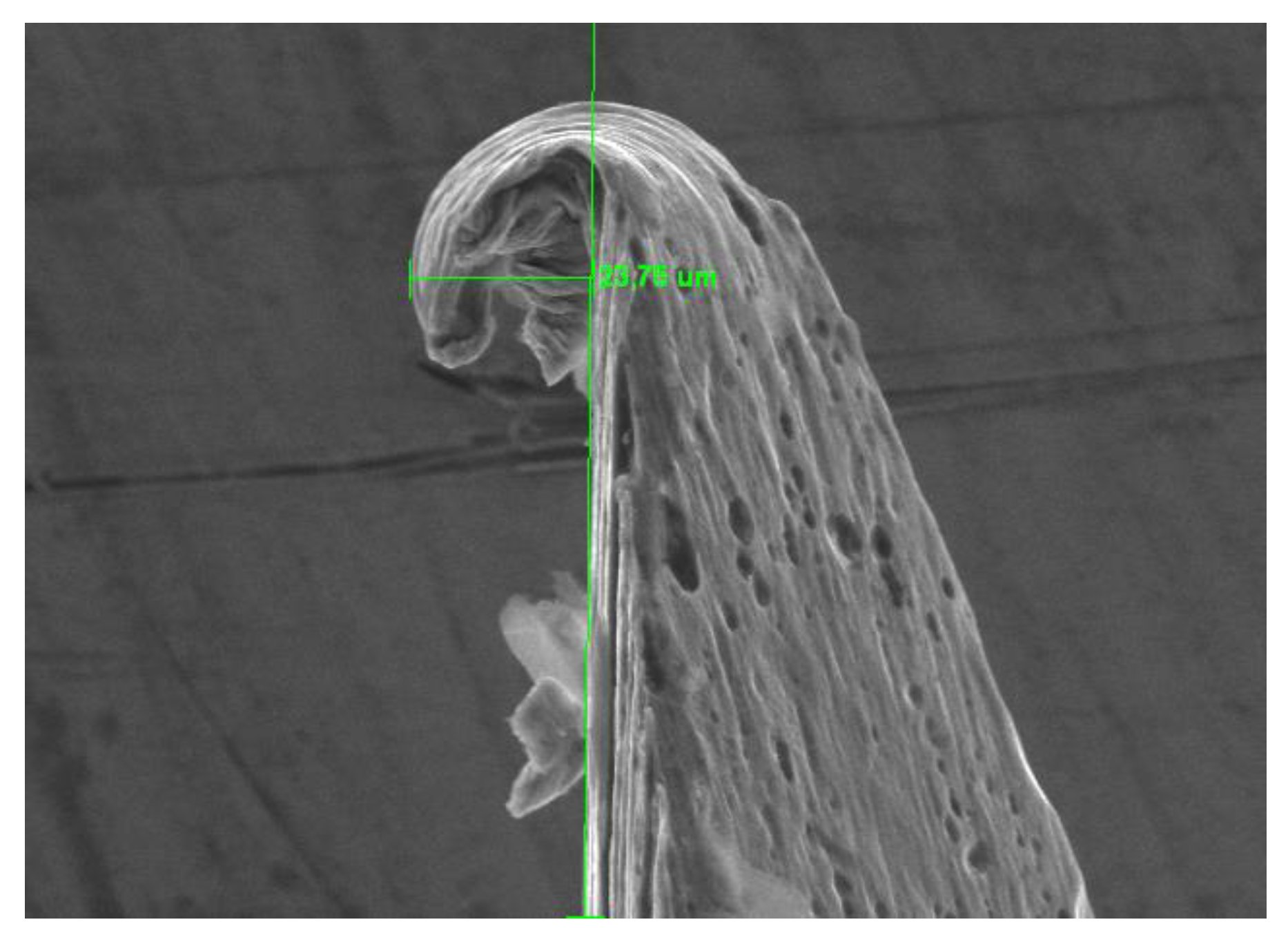
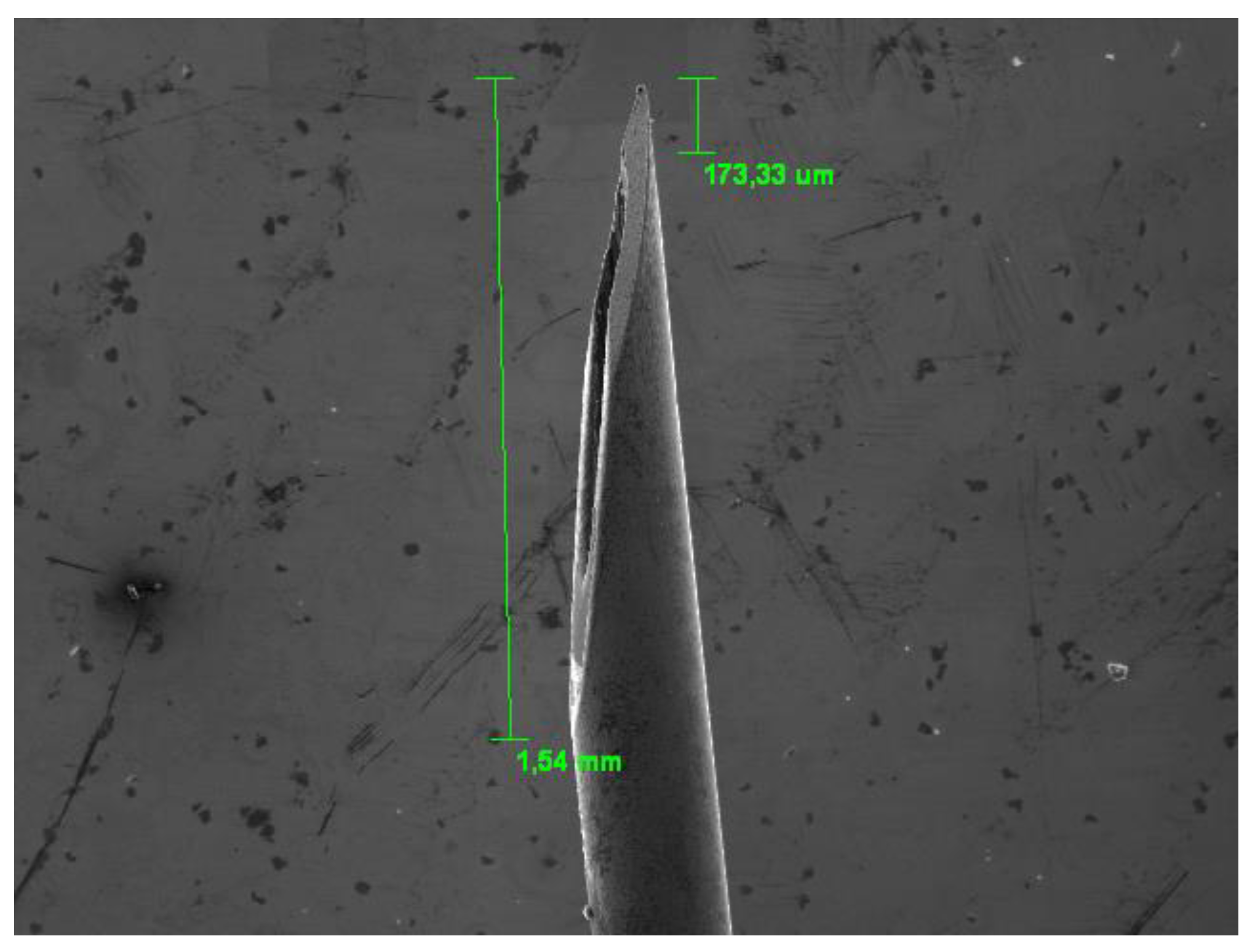
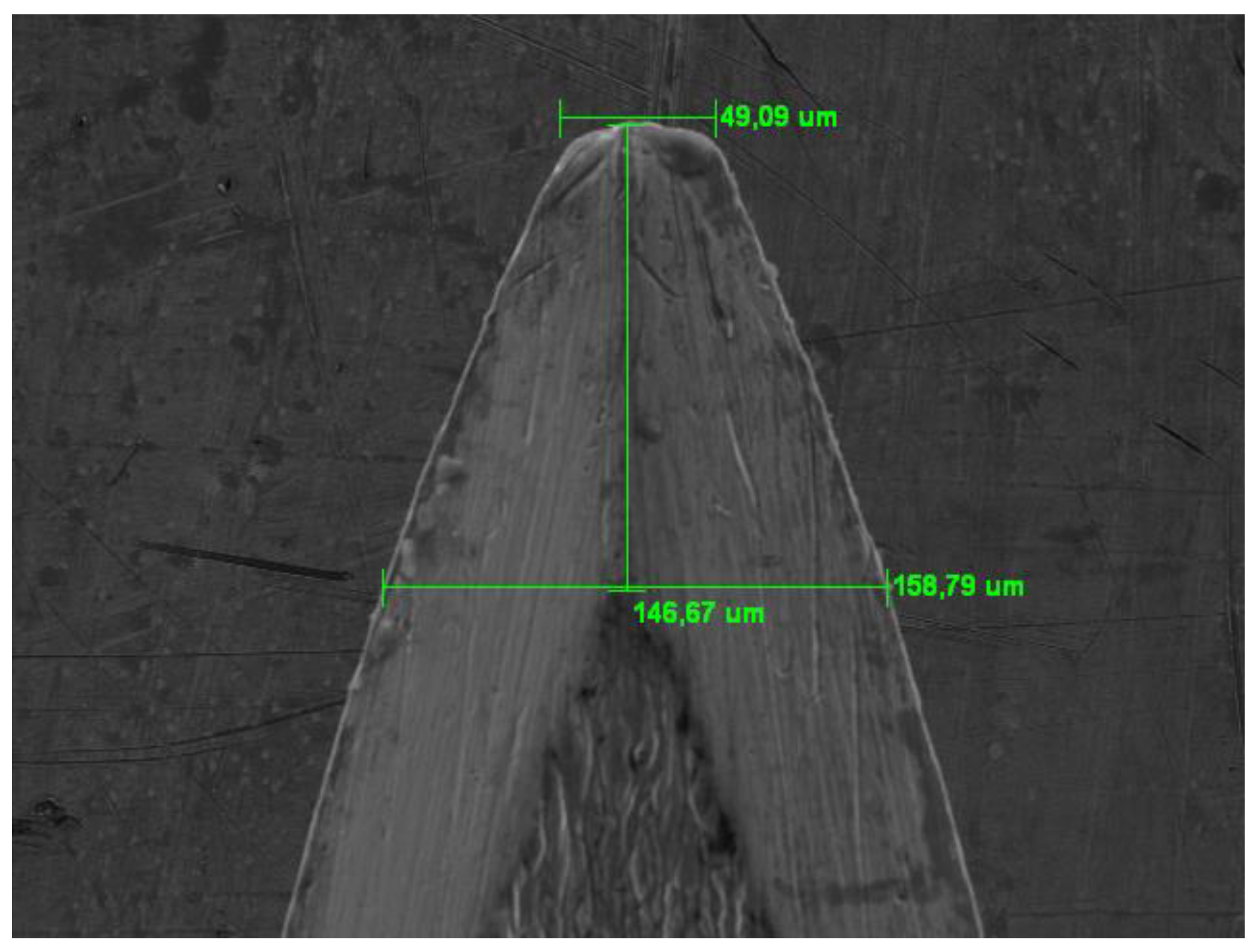
The SEM observation also allowed us to precisely measure some dimensional values of the tested needles to evaluate the homogeneity of the construction dimensional parameters and any differences between groups A and B; in order to carry out this measurement the needles were observed from different observation points. (
Figure 4 and
Figure 5).
The images were obtained and processed with the computer software Photoshop CS5 (Adobe Systems Incorporated, San Jose, CA, USA).
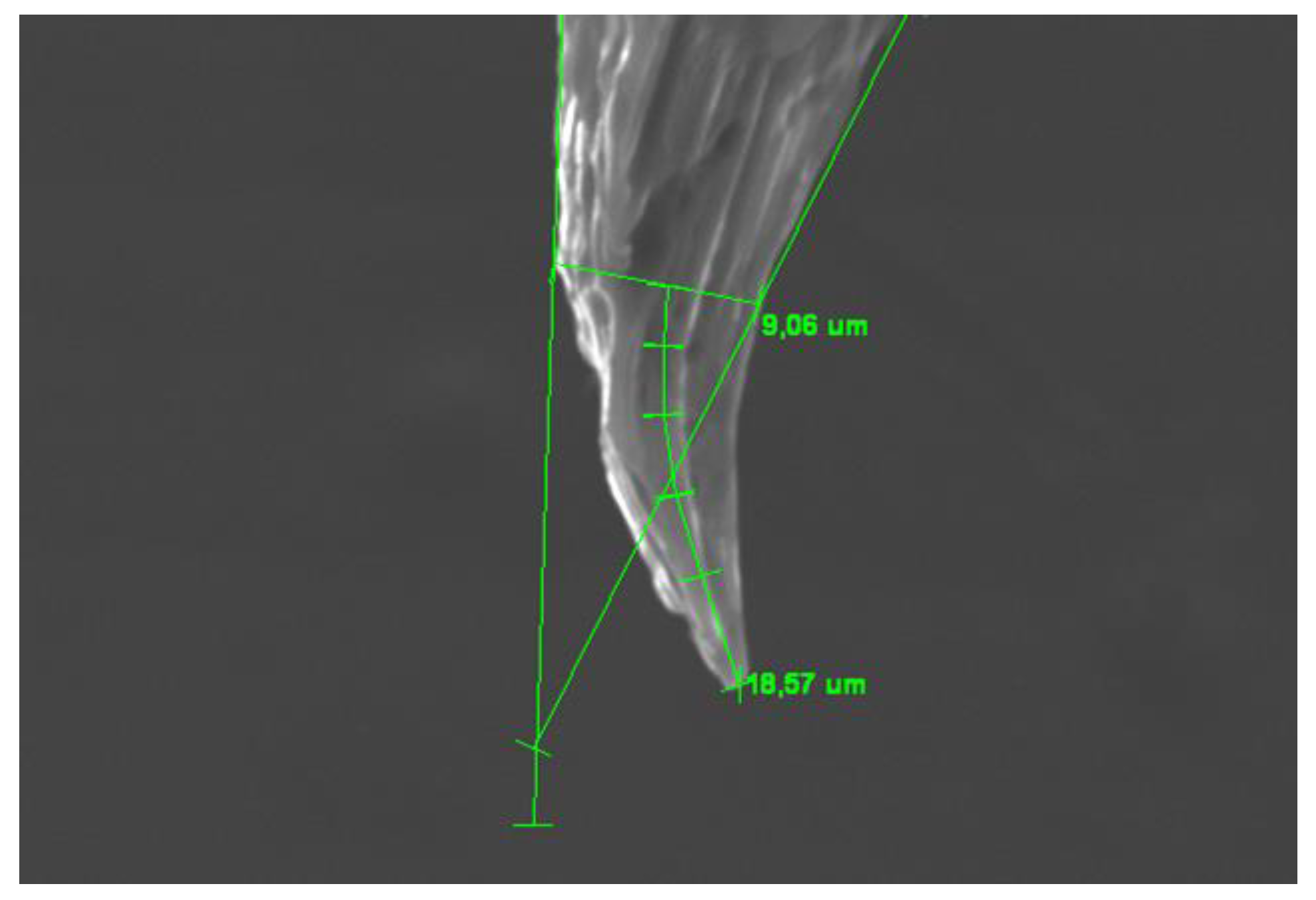
In order to quantify the deformations, two different measurements were carried out on the scanning electron microscopy images. The first measurement refers to the length of the deformed portion of the needle (
Figure 6 and
Figure 7).
The second measurement was carried out to evaluate how much the deformations protruded on the needle profile with the aim of relating this parameter to the danger of the hook created on the bevel (
Figure 8).
For completeness, the direction of the deformation was also noted, which could be towards the bevel or towards the opposite side (
Figure 9 and
Figure 10).
The data resulting from the SEM observations were statistically analyzed with the SPSS Statistics IBM software using the ANOVA test, P-values = 0.05 were seen as significant.
The null hypothesis was that there were differences in deformations found between the two brands of needles and that there were no differences between needles used for a single injection and those that were used for multiple sequential injections.
3. Results
All needles (30G) tested and observed under SEM showed an external diameter of 0.30 mm (+/- 0.03) and an internal diameter of 0.15 mm (+/- 0.04).
The percentage of deformed needles as an absolute figure is equal to 93.75% (180 needles out of 192).
No prevalent, statistically significant deformation was noted towards the bevel or towards the opposite side: out of 180 deformed needles, 98 (54.444%) showed a deformation towards the bevel and 82 (45.55%) towards the opposite side. Result are shown on
Table 2 and
Table 3.
4. Discussion
The results of our research clearly show that the sharp tip of the bevel is mechanically weak and therefore a easily deformable part, precisely at the moment in which it exercises its function which is to counteract the elasticity of the mucosa by cutting it allowing the needle to go into depth into the tissues to be anesthetized [
25].
Even if the consistency of the soft tissues is not high, it seems to be sufficient to bend the thinnest part of the bevel which becomes increasingly deformed as the needle is used for multiple and sequential injections [26].
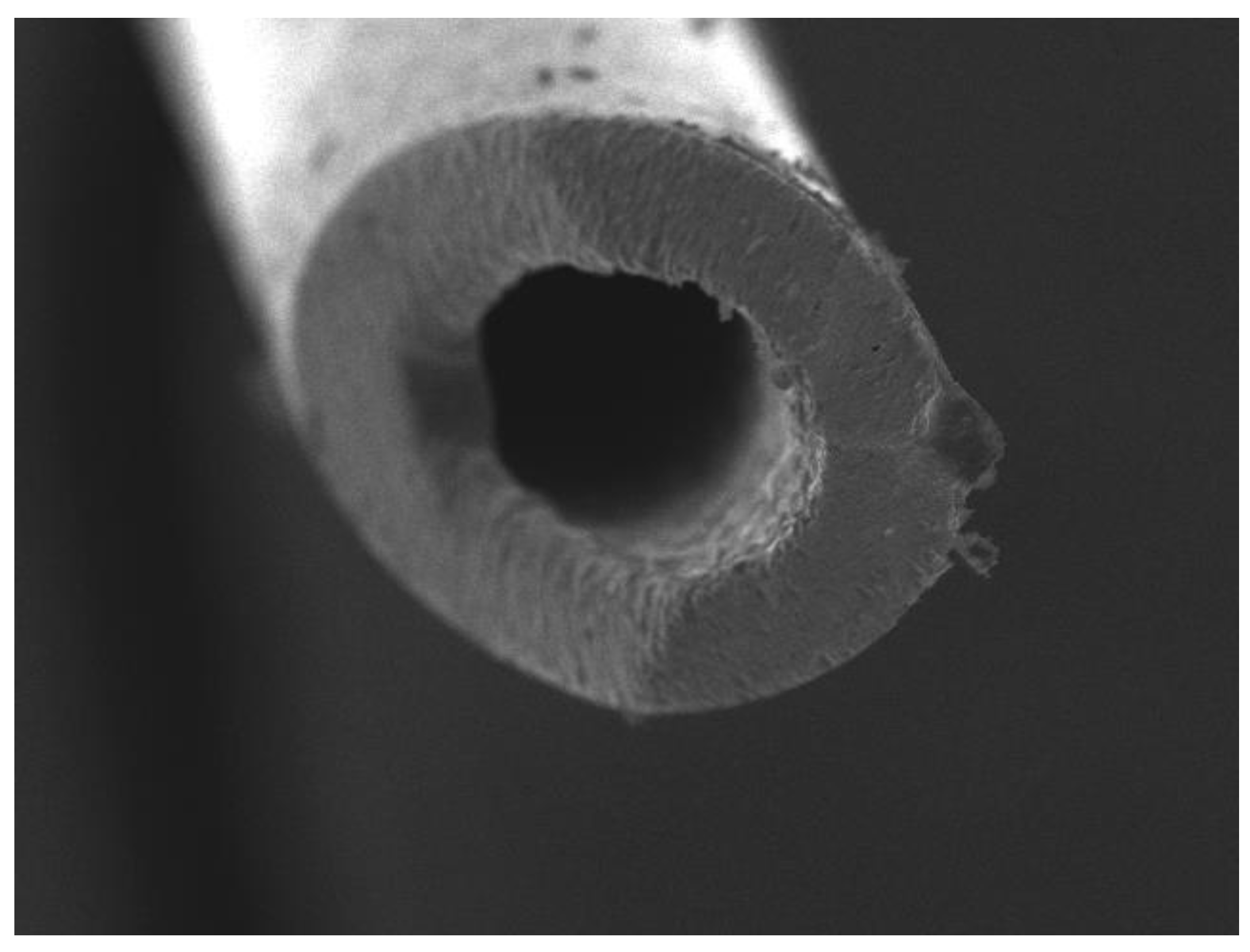
It is important to underline that the deformations were all observed in the tip of the bevel where the wall thicknesses are more reduced and make the tip of the needle most susceptible to deforming (
Figure 11 and
Figure 12).
The null hypothesis, which predicted that there were no differences in the deformation induced on the needle during use depending on how many times the mucosa was punctured, must be rejected.
In fact, the values relating to the deformation measured along the needle increase going from subgroup 1 to subgroup 6 and the differences are statistically significant (P>0.05). This increasing deformation was noted in both group A (Bestdent needles) and group B (Medibase needles).
It is necessary to add that no statistically significant differences were noted between the two groups A and B (P>0.05).
Our research has highlighted that the deformation of the tip of the bevel changes depending on the number of times that the mucosa is pricked and the needle passes through the soft tissues which in any case offer resistance to advancement.
Regarding the deformation measured as protrusion from the needle, it is noted that the highest values occur in correspondence with subgroups 1, 2 and 3 in combination with both group A and group B.
In clinical conditions where the needle punctures the mucosa 4, 5 or 6 times (subgroups 4, 5 and 6), the measurement of the protrusion from the needle profile is paradoxically the lowest.
This paradox could be explained by the fact that the bent part of the needle that creates the small protruding beard is very thin and when the needle is used sequentially several times, it is further pushed to move closer to the external surface of the needle itself.
Another noteworthy fact is that the part of the bevel that bends is that of the tip limited to the terminal section; it was also noted that, in our observations, the deformation rarely involves the part of the bevel furthest from the tip where the internal wall of the needle begins which, due to its characteristic shape of the section (which is C-shaped), offers greater resistance to bending (
Figure 13).
Considering the extent of the deformations measured in length (on the needle axis), there were no statistically significant differences between the two brands tested (P>0.05).
From a clinical point of view, episodes of blood extravasation in the context of the mucosa have been reported in subgroups 3 and 4 and it is worth mentioning even if the clinical phenomenon was not the subject of the research.
Probably, the metal of the needle folded on itself behaves like a sort of hook which is capable of easily injuring the soft tissues especially during the movement of extracting the needle which seems to have a greater lacerating effect.
In the presence of nerves and vessels of particular dimensions, this phenomenon appears particularly important as it facilitates the onset of iatrogenic damage potentially induced by anesthetic procedures.
Our study has the limitation of having tested the needles used only in the context of soft tissues and on the vestibular side of the teeth to be anesthetized without touching mineralized tissues such as bone and tooth. It is appropriate to extend the research to clinical practices of dental anesthesia which involve contact of the needle tip with tissues of greater consistency such as the bone cortex or, as in the case of intraligament anesthesia, with the root surface.
These mineralized tissues, of greater consistency than soft tissues, could induce larger and more complex deformation to the needle tip.
Another limitation of this study is that only one needle diameter was tested, even though 30 G is one of the most used.
Probably the 27 G diameter could, given the different thicknesses, behave differently.
Even if our research aimed to eliminate the operator variable by using a single experimenter, it would be useful to test and compare the results deriving from operators with different clinical experience.
5. Conclusions
We can conclude by hoping that any improvements in the bevel shape and in the alloys used in combination with further improvement treatments of the alloy, during production, will lead to a reduction in the tendency to plastic deformation of the cutting tip.
In any case it seems clear that the tested needles are not produced to withstand multiple injections and that even after the first injection on soft tissues, they undergo a deformation which could increase the risk of injury to the mucosa itself or to nerves and vessels with which they come into contact (
Figure 14 and
Figure 15).
It is better to limit the use of dental anesthesia needles by avoiding consecutive anesthetic injections and if the bevel is close to important and delicate nervous structures it would be better to replace the needle. A new needle without spikes and deformations, which behave like hooks, is much less likely to traumatize a any nerve or blood vessel that it comes into contact with.
Author Contributions
Conceptualization, E.C.; methodology, E.C.; software, E.C., G.A.S.; validation, G.G., P.M., G.A.S.; formal analysis, E.C.; investigation, E.C., G.A.S.; writing—original draft preparation, E.C.; writing—review and editing, G.A.S.; visualization, P.M., G.A.S.; supervision, G.A.S. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The clinical research adhered to the principles outlined in the Declaration of Helsinki and received approval from the Institutional Review Board of the Paolo Giaccone University of Palermo (Protocol Code: #4-19-04-23).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- St George G, Morgan A, Meechan J, Moles DR, Needleman I, Ng YL, Petrie A. Injectable local anaesthetic agents for dental anaesthesia. Cochrane Database of Systematic Reviews. 2018(7). [CrossRef]
- Bahl R. Local anesthesia in dentistry. Anesthesia progress. 2004;51(4):138.
- Blanton PL, Jeske AH. Dental local anesthetics: alternative delivery methods. The Journal of the American Dental Association. 2003 Feb 1;134(2):228-34. [CrossRef]
- Nusstein J, Claffey E, Reader A, Beck M, Weaver J. Anesthetic effectiveness of the supplemental intraligamentary injection, administered with a computer-controlled local anesthetic delivery system, in patients with irreversible pulpitis. Journal of endodontics. 2005 May 1;31(5):354-8. [CrossRef]
- Moore PA, Cuddy MA, Cooke MR, Sokolowski CJ. Periodontal ligament and intraosseous anesthetic injection techniques: alternatives to mandibular nerve blocks. The Journal of the American Dental Association. 2011 Sep 1;142:13S-8S. [CrossRef]
- Hawkins JM, Moore PA. Local anesthesia: advances in agents and techniques. Dental Clinics. 2002 Oct 1;46(4):719-32. [CrossRef]
- Jung R, Rybak M, Milner P, Lewkowicz N. Local anesthetics and advances in their administration-an overview. Journal of Pre-Clinical and Clinical Research. 2017;11(1). [CrossRef]
- Alexa V, Kiss I. Experimental Testson the Plasticity and Deformability Characteristics of Several Stainless Steel Grades used for Hydro–Pneumatic Equipment's Manufacturing. Acta Polytechnica Hungarica. 2018 Jan 1;15(8).
- Tukur SA, Dambatta MS, Ahmed A, Mu’az NM. Effect of heat treatment temperature on mechanical properties of the AISI 304 stainless steel. International Journal of Innovative Research in Science, Engineering and Technology. 2014;3(2):9516-20.
- Asghari-Rad P, Nili-Ahmadabadi M, Shirazi H, Hossein Nedjad S, Koldorf S. A significant improvement in the mechanical properties of AISI 304 stainless steel by a combined RCSR and annealing process. Advanced Engineering Materials. 2017 Mar;19(3):1600663. [CrossRef]
- McPherson JS, Dixon SA, Townsend R, Vandewalle KS. Effect of needle design on pain from dental local anesthetic injections. Anesthesia progress. 2015 Mar 1;62(1):2-7. [CrossRef]
- Steele AC, German MJ, Haas J, Lambert G, Meechan JG. An in vitro investigation of the effect of bevel design on the penetration and withdrawal forces of dental needles. Journal of dentistry. 2013 Feb 1;41(2):164-9. [CrossRef]
- Dau M, Buttchereit I, Ganz C, Frerich B, Anisimova EN, Daubländer M, Kämmerer PW. Influence of needle bevel design on injection pain and needle deformation in dental local infiltration anaesthesia–randomized clinical trial. International Journal of Oral and Maxillofacial Surgery. 2017 Nov 1;46(11):1484-9. [CrossRef]
- Gaitán-Fonseca C, Romo-Castillo D, Cerda-Cristerna B, Masuoka D, Pozos-Guillén A. Bevel tip deformation in new and used dental needles. Microscopy Research. 2015 Jan 14;3(01):1. [CrossRef]
- Hartmann A, Lawall T, Philipp L, Daubländer M. Needle tip deformation in local dental anesthesia–A technical note. Journal of the Mechanical Behavior of Biomedical Materials. 2022 Feb 1;126:105034. [CrossRef]
- Steele AC, German MJ, Haas J, Lambert G, Meechan JG. An in vitro investigation of the effect of bevel design on the penetration and withdrawal forces of dental needles. Journal of dentistry. 2013 Feb 1;41(2):164-9. [CrossRef]
- Rout PG, Saksena A, Fisher SE. An investigation of the effect on 27-gauge needle tips following a single local anaesthetic injection. Dental Update. 2003 Sep 2;30(7):370-4. [CrossRef]
- Ho JP, van Riet TC, Afrian Y, Sem KT, Spijker R, de Lange J, Lindeboom JA. Adverse effects following dental local anesthesia: a literature review. Journal of dental anesthesia and pain medicine. 2021 Dec;21(6):507. [CrossRef]
- Ho JP, van Riet TC, Afrian Y, Sem KT, Spijker R, de Lange J, Lindeboom JA. Adverse effects following dental local anesthesia: a literature review. Journal of dental anesthesia and pain medicine. 2021 Dec;21(6):507. [CrossRef]
- Stacy GC, Hajjar G. Barbed needle and inexplicable paresthesias and trismus after dental regional anesthesia. Oral surgery, oral medicine, oral pathology. 1994 Jun 1;77(6):585-8. [CrossRef]
- Roh S, Song L. Avoidance of Anesthesia Needle Tip Barb Formation to Reduce Risk of Injury during Inferior Alveolar Nerve Block Injection. Journal of Oral and Maxillofacial Surgery. 2019 Sep 1;77(9):e61-3. [CrossRef]
- Kämmerer PW, Staedt H, Wesslau K, Buttchereit I, Stiller HL, Frankenberger T, Dau M. The bevel effect: a prospective, randomized investigation into needle design in dental intraligamentary anesthesia. Clinical Oral Investigations. 2024 Mar;28(3):1-7. [CrossRef]
- Logothetis DD. Local Anesthesia for the Dental Hygienist-E-Book. Elsevier Health Sciences; 2021 Mar 23.
- Ogle OE, Mahjoubi G. Local anesthesia: agents, techniques, and complications. Dental Clinics. 2012 Jan 1;56(1):133-48. [CrossRef]
- de Oliveira Monteiro MA, da Gama Antunes AN, Basting RT. Physical, chemical, mechanical, and micromorphological characterization of dental needles. Journal of dental anesthesia and pain medicine. 2021 Apr;21(2):139. [CrossRef]
Figure 1.
Needle bevel, SEM observation, convex side.
Figure 1.
Needle bevel, SEM observation, convex side.
Figure 2.
Needle evel with triple sharpening, SEM observation.
Figure 2.
Needle evel with triple sharpening, SEM observation.
Figure 3.
Deformation of the needle tip observed under SEM.
Figure 3.
Deformation of the needle tip observed under SEM.
Figure 4.
Initial measurement of new needles.
Figure 4.
Initial measurement of new needles.
Figure 5.
Measurement of wall thicknesses.
Figure 5.
Measurement of wall thicknesses.
Figure 6.
Example of measurement of the length of deformations observed under SEM.
Figure 6.
Example of measurement of the length of deformations observed under SEM.
Figure 7.
Example of strain measurement. (Deformation length=18.57 µ, bevel thickness at the beginning of deformation=9.06 µ,).
Figure 7.
Example of strain measurement. (Deformation length=18.57 µ, bevel thickness at the beginning of deformation=9.06 µ,).
Figure 8.
Measurement of the protrusion of the deformation on the needle profile. (In the observed sample it is 21.34 µ).
Figure 8.
Measurement of the protrusion of the deformation on the needle profile. (In the observed sample it is 21.34 µ).
Figure 9.
Example of deformation towards the concave side of the needle.
Figure 9.
Example of deformation towards the concave side of the needle.
Figure 10.
Example of deformation towards the convex side of the needle.
Figure 10.
Example of deformation towards the convex side of the needle.
Figure 11.
Needle tip where the walls are very thin.
Figure 11.
Needle tip where the walls are very thin.
Figure 12.
Tip bevel detail where most of the deformations occur.
Figure 12.
Tip bevel detail where most of the deformations occur.
Figure 13.
SEM view of the thickness of the needle walls.
Figure 13.
SEM view of the thickness of the needle walls.
Figure 14.
Protruding hook on the needle profile which could cause trauma to the tissues it comes into contact with.
Figure 14.
Protruding hook on the needle profile which could cause trauma to the tissues it comes into contact with.
Figure 15.
Needle deformation capable of tearing soft tissue.
Figure 15.
Needle deformation capable of tearing soft tissue.
Table 2.
Length of deformation measured along the axis of the needle.
Table 2.
Length of deformation measured along the axis of the needle.
| Brand |
Combination |
Deformations |
Mean |
Standard deviation |
| Biodent |
A+1 |
12 |
36.40 |
4.50 |
| A+2 |
14 |
50.42 |
2.57 |
| A+3 |
16 |
62.43 |
1.93 |
| A+4 |
16 |
75.61 |
2.05 |
| A+5 |
16 |
86.84 |
2.72 |
| A+6 |
16 |
99.67 |
4.21 |
| Medibase |
B+1 |
12 |
37.11 |
3.64 |
| B+2 |
14 |
52.99 |
2.24 |
| B+3 |
16 |
66.32 |
1.61 |
| B+4 |
16 |
75.75 |
2.36 |
| B+5 |
16 |
86.25 |
2.44 |
| B+6 |
16 |
103.87 |
2.54 |
Table 3.
Protrusion of the deformation on the external surface of the needle.
Table 3.
Protrusion of the deformation on the external surface of the needle.
| Brand |
Combination |
Deformations |
Mean |
Standard deviation |
| Biodent |
A+1 |
12 |
35.67 |
2.95 |
| A+2 |
14 |
37.79 |
3.39 |
| A+3 |
16 |
38.02 |
3.54 |
| A+4 |
16 |
38.61 |
2.85 |
| A+5 |
16 |
30.32 |
4.06 |
| A+6 |
16 |
28.53 |
3.14 |
| Medibase |
B+1 |
12 |
38.59 |
2.70 |
| B+2 |
14 |
39.63 |
2.55 |
| B+3 |
16 |
39.77 |
1.66 |
| B+4 |
16 |
38.74 |
1.97 |
| B+5 |
16 |
29.70 |
3.68 |
| B+6 |
16 |
28.74 |
4.61 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).