Submitted:
02 July 2024
Posted:
03 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
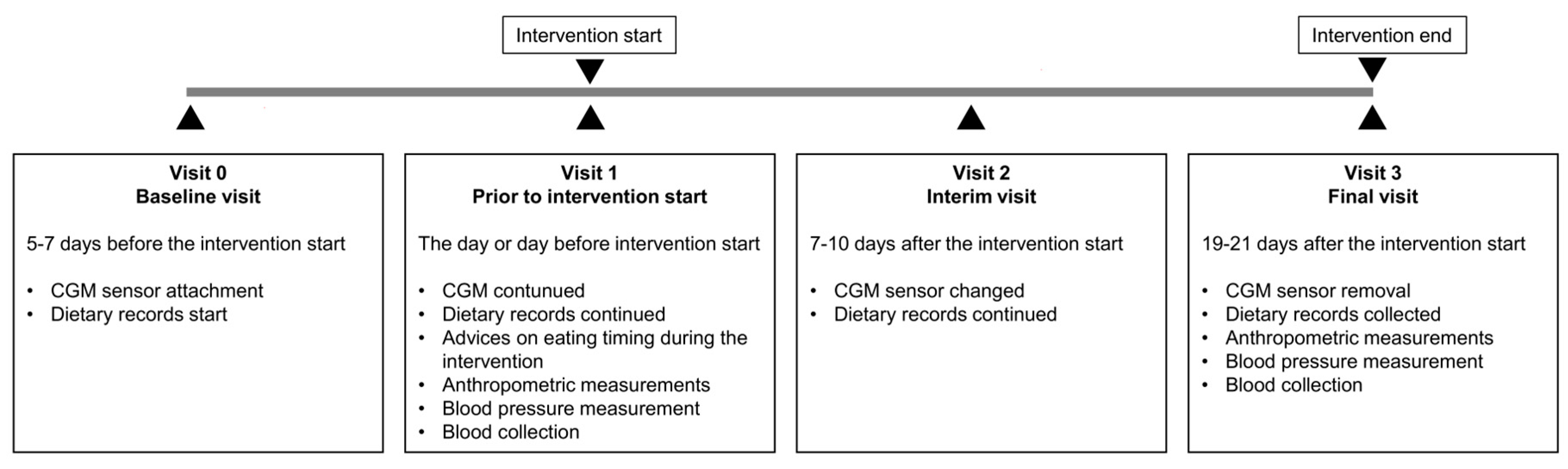
2.1. Study Design
2.2. Study Subjects and Eligibility Criteria
2.3. Fasting Interventions, Dietary Records and Assessment of the Timely Compliance
2.4. Anthropometric Measurements
2.5. Continuous Glucose Monitoring (CGM) and HbA1c Assessment
2.6. Glucotypes
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Study Population
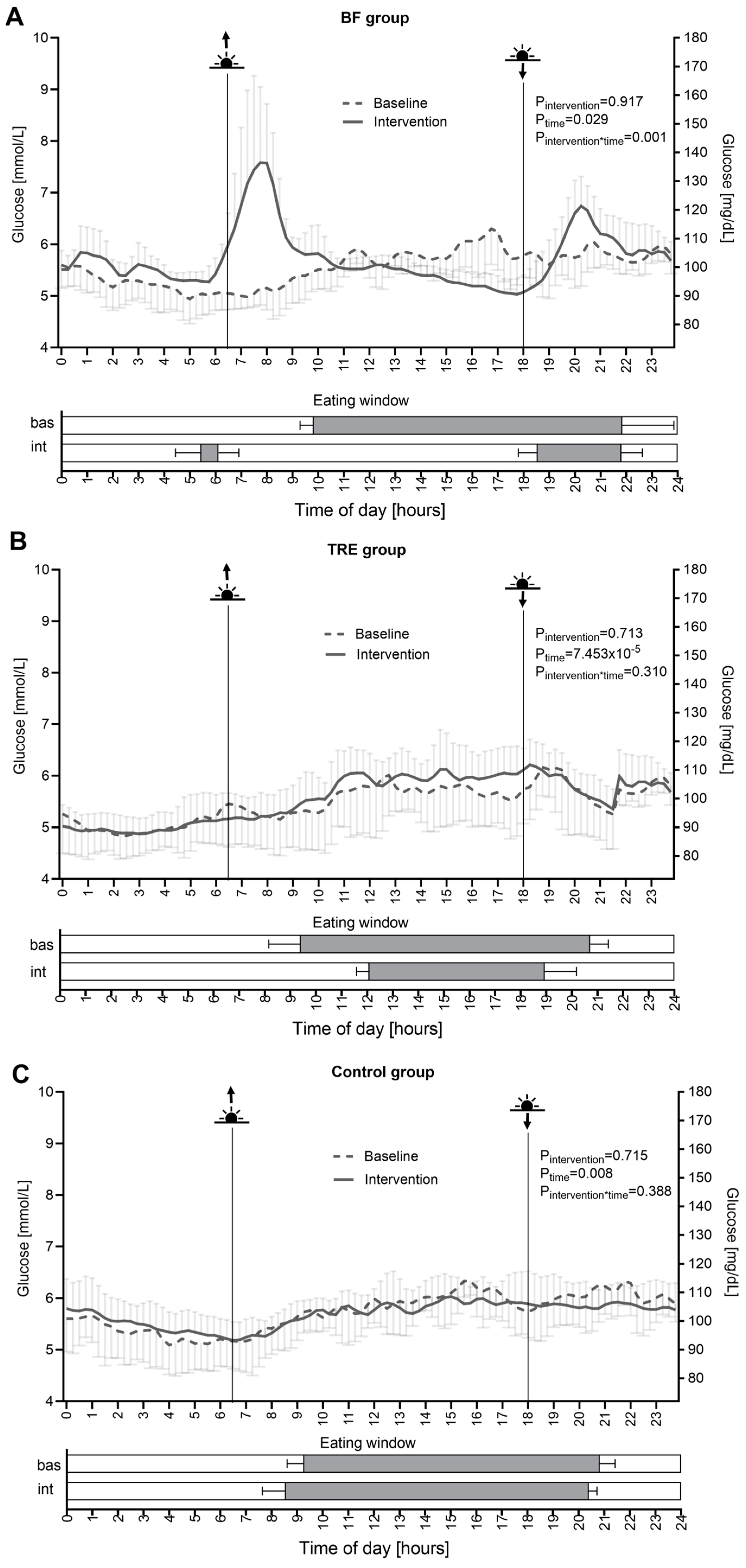
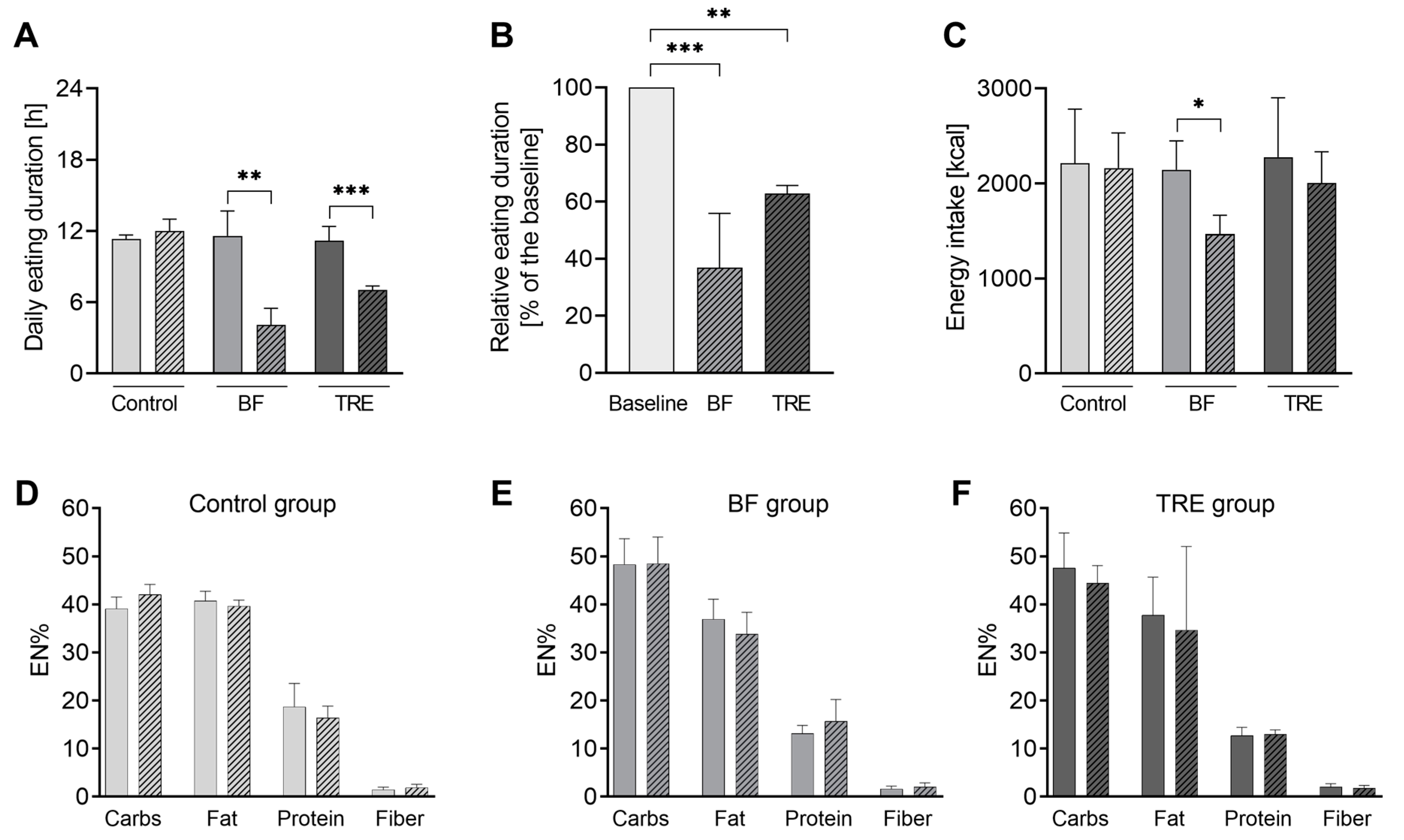
3.2. Timely Compliance
3.3. Energy and Macronutrient Intake
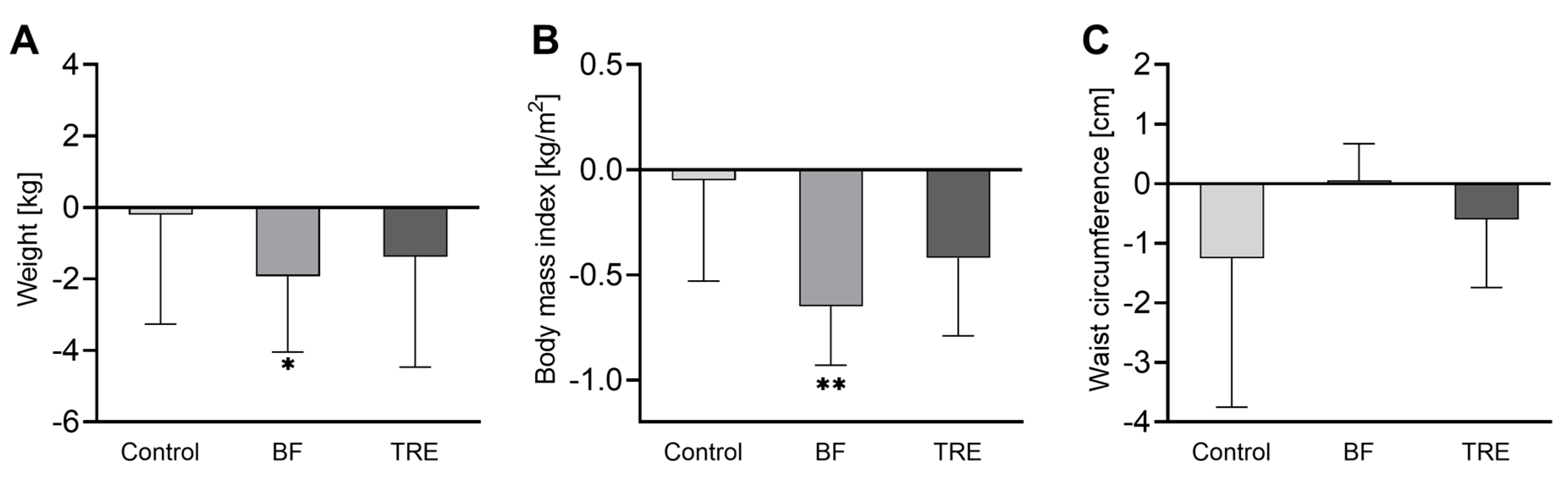
3.4. Anthropometric Measurements and Blood Pressure
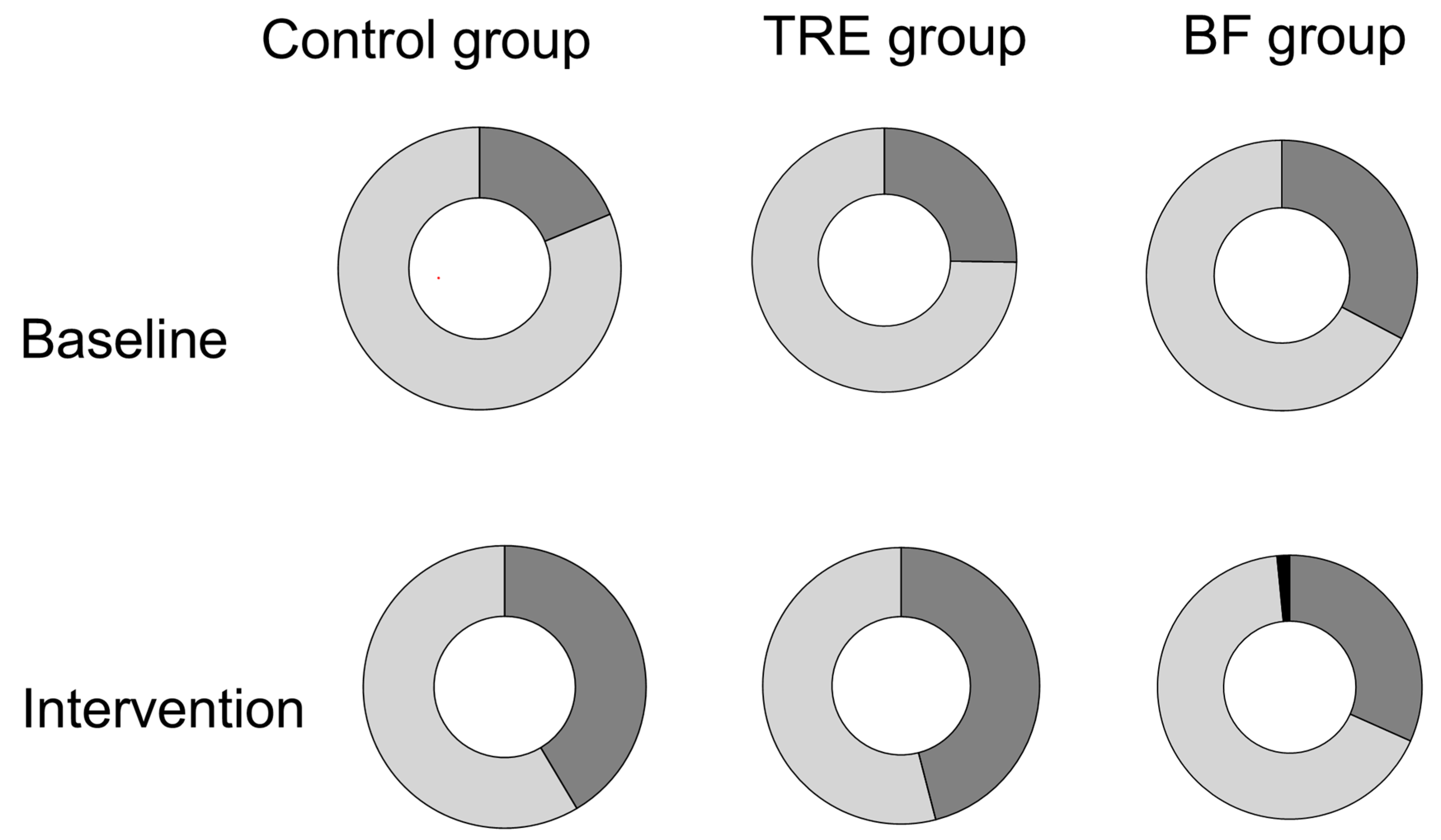
3.6. Glucotypes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Cabo R, Mattson MP. Effects of Intermittent Fasting on Health, Aging, and Disease. The New England journal of medicine. 2019;381(26):2541-51. [CrossRef]
- Rahmatullah, Ahmedani MY, Basit A, Zia S, Hasan I, Masroor Q, et al. Evidence-based risk factors for major complications during Ramadan fasting in people with diabetes grouped under IDF-DAR risk categories. Diabetes research and clinical practice. 2022;185:109234. [CrossRef]
- Ba-Essa EM, Hassanein M, Abdulrhman S, Alkhalifa M, Alsafar Z. Attitude and safety of patients with diabetes observing the Ramadan fast. Diabetes research and clinical practice. 2019;152:177-82. [CrossRef]
- Bahá’u’lláh. The Kitáb-i-Aqdas: The Most Holy Book. 1 ed. ed: London: Baha’i Publishing Trust; 1993. 315 p.
- Mähler A, Jahn C, Klug L, Klatte C, Michalsen A, Koppold-Liebscher D, et al. Metabolic Response to Daytime Dry Fasting in Bahá'í Volunteers-Results of a Preliminary Study. Nutrients. 2021;14(1).
- Hassanein M, Afandi B, Yakoob Ahmedani M, Mohammad Alamoudi R, Alawadi F, Bajaj HS, et al. Diabetes and Ramadan: Practical guidelines 2021. Diabetes Res Clin Pract. 2022;185:109185. [CrossRef]
- Ali T, Lessan N. Chrononutrition in the context of Ramadan: Potential implications. Diabetes/metabolism research and reviews. 2023:e3728. [CrossRef]
- Koppold-Liebscher DA, Klatte C, Demmrich S, Schwarz J, Kandil FI, Steckhan N, et al. Effects of Daytime Dry Fasting on Hydration, Glucose Metabolism and Circadian Phase: A Prospective Exploratory Cohort Study in Baha'i Volunteers. Front Nutr. 2021;8:662310.
- Alawadi F, Rashid F, Bashier A, Abdelgadir E, Al Saeed M, Abuelkheir S, et al. The use of Free Style Libre Continues Glucose Monitoring (FSL-CGM) to monitor the impact of Ramadan fasting on glycemic changes and kidney function in high-risk patients with diabetes and chronic kidney disease stage 3 under optimal diabetes care. Diabetes research and clinical practice. 2019;151:305-12.
- Salti I, Benard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study. Diabetes care. 2004;27(10):2306-11.
- Zouhal H, Bagheri R, Triki R, Saeidi A, Wong A, Hackney AC, et al. Effects of Ramadan Intermittent Fasting on Gut Hormones and Body Composition in Males with Obesity. Int J Environ Res Public Health. 2020;17(15).
- Lum ZK, Khoo ZR, Toh WYS, Kamaldeen SAK, Shakoor A, Tsou KYK, et al. Efficacy and Safety of Use of the Fasting Algorithm for Singaporeans With Type 2 Diabetes (FAST) During Ramadan: A Prospective, Multicenter, Randomized Controlled Trial. Ann Fam Med. 2020;18(2):139-47.
- Tay J, Thompson CH, Brinkworth GD. Glycemic Variability: Assessing Glycemia Differently and the Implications for Dietary Management of Diabetes. Annu Rev Nutr. 2015;35:389-424. [CrossRef]
- Yu JH, Han K, Park S, Lee DY, Nam GE, Seo JA, et al. Effects of long-term glycemic variability on incident cardiovascular disease and mortality in subjects without diabetes: A nationwide population-based study. Medicine (Baltimore). 2019;98(29):e16317.
- Afandi B, Kaplan W, Al Hassani N, Hadi S, Mohamed A. Correlation between pre-ramadan glycemic control and subsequent glucose fluctuation during fasting in adolescents with Type 1 diabetes. Journal of endocrinological investigation. 2017;40(7):741-4. [CrossRef]
- Saadane I, Ali T, El-Laboudi A, Lessan N. Ramadan fasting in insulin-treated patients is associated with potentially unfavourable changes in glucose metrics: A flash glucose monitoring (FGM) study. Diabetes research and clinical practice. 2021;172:108592. [CrossRef]
- Lessan N, Hannoun Z, Hasan H, Barakat MT. Glucose excursions and glycaemic control during Ramadan fasting in diabetic patients: insights from continuous glucose monitoring (CGM). Diabetes Metab. 2015;41(1):28-36. [CrossRef]
- Elmalti A, Mukhtar M, Kenz S, Skaria S, Elgzyri T. Transient increase in glucose variability during Ramadan fasting in patients with insulin-treated type 2 diabetes: A preliminary study. Diabetes Metab Syndr. 2023;17(4):102745. [CrossRef]
- Aldawi N, Darwiche G, Abusnana S, Elbagir M, Elgzyri T. Initial increase in glucose variability during Ramadan fasting in non-insulin-treated patients with diabetes type 2 using continuous glucose monitoring. Libyan J Med. 2019;14(1):1535747. [CrossRef]
- Peters B, Koppold-Liebscher DA, Schuppelius B, Steckhan N, Pfeiffer AFH, Kramer A, et al. Effects of Early vs. Late Time-Restricted Eating on Cardiometabolic Health, Inflammation, and Sleep in Overweight and Obese Women: A Study Protocol for the ChronoFast Trial. Front Nutr. 2021;8:765543. [CrossRef]
- Schuppelius B, Peters B, Ottawa A, Pivovarova-Ramich O. Time Restricted Eating: A Dietary Strategy to Prevent and Treat Metabolic Disturbances. Frontiers in endocrinology. 2021;12:683140. [CrossRef]
- Tsitsou S, Zacharodimos N, Poulia KA, Karatzi K, Dimitriadis G, Papakonstantinou E. Effects of Time-Restricted Feeding and Ramadan Fasting on Body Weight, Body Composition, Glucose Responses, and Insulin Resistance: A Systematic Review of Randomized Controlled Trials. Nutrients. 2022;14(22). [CrossRef]
- Baum Martinez I, Peters B, Schwarz J, Schuppelius B, Steckhan N, Koppold-Liebscher DA, et al. Validation of a Smartphone Application for the Assessment of Dietary Compliance in an Intermittent Fasting Trial. Nutrients. 2022;14(18). [CrossRef]
- Hill NR, Oliver NS, Choudhary P, Levy JC, Hindmarsh P, Matthews DR. Normal reference range for mean tissue glucose and glycemic variability derived from continuous glucose monitoring for subjects without diabetes in different ethnic groups. Diabetes technology & therapeutics. 2011;13(9):921-8. [CrossRef]
- Pappe CL, Peters B, Dommisch H, Woelber JP, Pivovarova-Ramich O. Effects of reducing free sugars on 24-hour glucose profiles and glycemic variability in subjects without diabetes. Front Nutr. 2023;10:1213661. [CrossRef]
- Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, DeVries JH. Glucose variability is associated with intensive care unit mortality*. Critical Care Medicine. 2010;38(3):838-42. [CrossRef]
- Thomsen MN, Skytte MJ, Astrup A, Deacon CF, Holst JJ, Madsbad S, et al. The clinical effects of a carbohydrate-reduced high-protein diet on glycaemic variability in metformin-treated patients with type 2 diabetes mellitus: A randomised controlled study. Clin Nutr ESPEN. 2020;39:46-52. [CrossRef]
- Hall H, Perelman D, Breschi A, Limcaoco P, Kellogg R, McLaughlin T, et al. Glucotypes reveal new patterns of glucose dysregulation. PLoS Biol. 2018;16(7):e2005143. [CrossRef]
- Broll S, Urbanek J, Buchanan D, Chun E, Muschelli J, Punjabi NM, et al. Interpreting blood GLUcose data with R package iglu. PLoS One. 2021;16(4):e0248560.
- Antoni R, Robertson T, Robertson M, Johnston J. A pilot feasibility study exploring the effects of a moderate time-restricted feeding intervention on energy intake, adiposity and metabolic physiology in free-living human subjects. Journal of Nutritional Science. 2018;7:e22. [CrossRef]
- Chow LS, Manoogian ENC, Alvear A, Fleischer JG, Thor H, Dietsche K, et al. Time-Restricted Eating Effects on Body Composition and Metabolic Measures in Humans who are Overweight: A Feasibility Study. Obesity (Silver Spring). 2020;28(5):860-9. [CrossRef]
- Jamshed H, Beyl RA, Della Manna DL, Yang ES, Ravussin E, Peterson CM. Early Time-Restricted Feeding Improves 24-Hour Glucose Levels and Affects Markers of the Circadian Clock, Aging, and Autophagy in Humans. Nutrients. 2019;11(6).
- Moro T, Tinsley G, Bianco A, Marcolin G, Pacelli QF, Battaglia G, et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. Journal of translational medicine. 2016;14(1):290.
- Peeke PM, Greenway FL, Billes SK, Zhang D, Fujioka K. Effect of time restricted eating on body weight and fasting glucose in participants with obesity: results of a randomized, controlled, virtual clinical trial. Nutrition & diabetes. 2021;11(1):6. [CrossRef]
- Hutchison AT, Regmi P, Manoogian ENC, Fleischer JG, Wittert GA, Panda S, et al. Time-Restricted Feeding Improves Glucose Tolerance in Men at Risk for Type 2 Diabetes: A Randomized Crossover Trial. Obesity (Silver Spring). 2019;27(5):724-32.
- Martens CR, Rossman MJ, Mazzo MR, Jankowski LR, Nagy EE, Denman BA, et al. Short-term time-restricted feeding is safe and feasible in non-obese healthy midlife and older adults. Geroscience. 2020;42(2):667-86. [CrossRef]
- Parr EB, Devlin BL, Radford BE, Hawley JA. A Delayed Morning and Earlier Evening Time-Restricted Feeding Protocol for Improving Glycemic Control and Dietary Adherence in Men with Overweight/Obesity: A Randomized Controlled Trial. Nutrients. 2020;12(2). [CrossRef]
- Wilkinson MJ, Manoogian ENC, Zadourian A, Lo H, Fakhouri S, Shoghi A, et al. Ten-Hour Time-Restricted Eating Reduces Weight, Blood Pressure, and Atherogenic Lipids in Patients with Metabolic Syndrome. Cell metabolism. 2020;31(1):92-104 e5.
- Kesztyus D, Cermak P, Gulich M, Kesztyus T. Adherence to Time-Restricted Feeding and Impact on Abdominal Obesity in Primary Care Patients: Results of a Pilot Study in a Pre-Post Design. Nutrients. 2019;11(12). [CrossRef]
- Lowe DA, Wu N, Rohdin-Bibby L, Moore AH, Kelly N, Liu YE, et al. Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial. JAMA Intern Med. 2020;180(11):1491-9.
- Parr EB, Devlin BL, Lim KHC, Moresi LNZ, Geils C, Brennan L, et al. Time-Restricted Eating as a Nutrition Strategy for Individuals with Type 2 Diabetes: A Feasibility Study. Nutrients. 2020;12(11).
- Phillips NE, Mareschal J, Schwab N, Manoogian ENC, Borloz S, Ostinelli G, et al. The Effects of Time-Restricted Eating versus Standard Dietary Advice on Weight, Metabolic Health and the Consumption of Processed Food: A Pragmatic Randomised Controlled Trial in Community-Based Adults. Nutrients. 2021;13(3).
- Yeoh EC, Zainudin SB, Loh WN, Chua CL, Fun S, Subramaniam T, et al. Fasting during Ramadan and Associated Changes in Glycaemia, Caloric Intake and Body Composition with Gender Differences in Singapore. Ann Acad Med Singap. 2015;44(6):202-6.
- Fernando HA, Zibellini J, Harris RA, Seimon RV, Sainsbury A. Effect of Ramadan Fasting on Weight and Body Composition in Healthy Non-Athlete Adults: A Systematic Review and Meta-Analysis. Nutrients. 2019;11(2).
- Sadeghirad B, Motaghipisheh S, Kolahdooz F, Zahedi MJ, Haghdoost AA. Islamic fasting and weight loss: a systematic review and meta-analysis. Public Health Nutr. 2014;17(2):396-406.
- Al-Barha NS, Aljaloud KS. The Effect of Ramadan Fasting on Body Composition and Metabolic Syndrome in Apparently Healthy Men. Am J Mens Health. 2019;13(1):1557988318816925.
- Kessler K, Pivovarova-Ramich O. Meal Timing, Aging, and Metabolic Health. International journal of molecular sciences. 2019;20(8).
- Kohsaka A, Laposky AD, Ramsey KM, Estrada C, Joshu C, Kobayashi Y, et al. High-fat diet disrupts behavioral and molecular circadian rhythms in mice. Cell metabolism. 2007;6(5):414-21.
- Zhao L, Hutchison AT, Liu B, Wittert GA, Thompson CH, Nguyen L, et al. Time restricted eating alters the 24-hour profile of adipose tissue transcriptome in men with obesity. Obesity (Silver Spring). 2022.
| Control group | BF group | TRE group | |
|---|---|---|---|
|
Clinical characteristics N |
4 |
6 |
6 |
| Male | 2 | 3 | 3 |
| Age [years] | 29 (28 – 35) | 31 (22 – 43) | 28 (25 – 32) |
| Weight [kg] | 85.9 ± 24.2 | 80.1 ± 18.1 | 79.5 ± 14.0 |
| BMI [kg/m²] | 27.4 ± 6.2 | 26.8 ± 3.9 | 25.5 ± 3.9 |
| Waist circumference [cm] | 89.5 ± 21.0 | 91.9 ± 17.8 | 85.2 ± 5.8 |
| SBP [mmHg] | 131.0 ± 20.2 | 132.3 ± 10.5 | 126.2 ± 12.6 |
| DBP [mmHg] | 78.0 ± 13.7 | 83.8 ± 6.6 | 85.0 ± 11.1 |
|
Glycemic parameters MSG [mmol/L] |
5.74 ± 0.47 |
5.56 ± 0.30 |
5.44 ± 0.57 |
| Minimum [mmol/L] | 4.96 ± 0.54 | 4.79 ± 0.35 | 4.72 ± 0.51 |
| Maximum [mmol/L] | 6.77 ± 0.44 | 6.68 ± 0.38 | 6.69 ± 0.74 |
| TBR <3.9 mmol/L [%] | 0.20 (0.00 – 4.39) | 0.78 (0.00 – 2.73) | 0.23 (0.00 – 3.83) |
| TAR >10 mmol/L [%] | 0.10 (0.00 – 0.37) | 0.00 (0.00 – 0.81) | 0.00 (0.00 – 0.12) |
| AUCgluc [min x mmol/L] | 8217 ± 673 | 7964 ± 431 | 7789 ± 813 |
| SD [mmol/L] | 0.81 ± 0.29 | 0.83 ± 0.10 | 0.78 ± 0.11 |
| CV [%] | 14.2 ± 5.69 | 14.9 ± 1.55 | 14.4 ± 1.79 |
| MAGE [mmol/L] | 1.03 ± 0.31 | 1.13 ± 0.05 | 1.09 ± 0.12 |
| CONGA [mmol/L] | 5.23 ± 0.44 | 4.96 ± 0.27 | 4.93 ± 0.57 |
| MAG change [mmol/L/h] | 1.12 ± 0.26 | 1.21 ± 0.08 | 1.09 ± 0.09 |
| MODD [mmol/L] | 0.73 ± 0.21 | 0.75 ± 0.08 | 0.66 ± 0.06 |
| LBGI | 1.28 ± 1.09 | 1.44 ± 0.61 | 1.86 ± 1.40 |
| HBGI | 0.78 ± 0.58 | 0.70 ± 0.31 | 0.59 ± 0.21 |
| Glucotype [low:moderate:severe] | 0:4:0 | 0:5:0 | 0:5:0 |
| HbA1c [%] | 5.10 ± 0.29 | 5.13 ± 0.42 | 5.07 ± 0.16 |
| Control group | BF group | TRE group | p-value between groupsc | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Changesa | p-valueb | Changesa | p-valueb | Changesa | p-valueb | BF vs. Control | TRE vs. Control | TRE vs. BF | ||||
| Glycaemic Parameters | ||||||||||||
| MSG [mmol/L] | -0.05 ± 0.24 | 0.710 | 0.17 ± 0.26 | 0.220 | 0.05 ± 0.27 | 0.690 | 0.556 | 0.921 | 0.871 | |||
| Minimum [mmol/L] | 0.20 ± 0.46 | 0.460 | 0.19 ± 0.27 | 0.187 | 0.08 ± 0.25 | 0.520 | 1.000 | 0.941 | 0.939 | |||
| Maximum [mmol/L]f | -0.55 ± 0.19 | 0.011 | 1.41 ± 1.04 | 0.039 | -0.22 ± 0.75 | 0.556 | 0.010 | 0.901 | 0.022 | |||
| TBR <3.9 mmol/L [%] | -0.11 (-2.56 – 0.00) | 0.180 | -0.78 (-2.45 – 0.67) | 0.273 | 0.08 (-2.85 – 0.70) | 0.715 | - | - | - | |||
| TAR >10 mmol/L [%] | -0.07 (-0.31 – 0.00) | 0.180 | 0.38 (0.00 – 2.52) | 0.109 | 0.00 (0.00 – 0.15) | 0.317 | 0.012 | 0.180 | 0.209 | |||
| AUCgluc [min x mmol/L] | -71 ± 343 | 0.705 | 241 ± 367 | 0.216 | 79 ± 388 | 0.673 | 0.548 | 0.912 | 0.876 | |||
| Glycemic Variability | ||||||||||||
| SD [mmol/L] | -0.07 ± 0.14 | 0.423 | 0.13 ± 0.18 | 0.184 | -0.02 ± 0.05 | 0.422 | 0.155 | 0.950 | 0.287 | |||
| CV [%] | -1.19 ± 3.16 | 0.507 | 1.71 ± 2.57 | 0.226 | -0.54 ± 1.34 | 0.422 | 0.270 | 0.971 | 0.422 | |||
| MAGE [mmol/L] | -0.14 ± 0.13 | 0.121 | 0.19 ± 0.34 | 0.251 | -0.12 ± 0.13 | 0.113 | 0.130 | 0.999 | 0.133 | |||
| CONGA [mmol/L] | -0.02 ± 0.22 | 0.893 | 0.18 ± 0.26 | 0.188 | 0.14 ± 0.31 | 0.370 | 0.648 | 0.792 | 0.992 | |||
| MAG change [mmol/L/h] | -0.11 ± 0.06 | 0.036 | -0.10 ± 0.16 | 0.238 | -0.16 ± 0.19 | 0.135 | 1.000 | 0.952 | 0.925 | |||
| MODD [mmol/L] | -0.04 ± 0.09 | 0.473 | -0.12 ± 0.12 | 0.098 | -0.07 ± 0.07 | 0.098 | 0.599 | 0.957 | 0.848 | |||
| LBGI | -0.13 ± 0.72 | 0.738 | -0.28 ± 0.46 | 0.244 | -0.27 ± 0.86 | 0.523 | 0.986 | 0.989 | 1.000 | |||
| HBGI | -0.31 ± 0.40 | 0.220 | 0.60 ± 0.79 | 0.164 | -0.13 ± 0.15 | 0.118 | 0.077 | 0.953 | 0.141 | |||
| HbA1c [%] | -0.08 ± 0.22 | 0.257 | 0.04 ± 0.11 | 0.342 | -0.06 ± 0.11 | 0.547 | 0.628 | 0.998 | 0.683 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





