1. Introduction
Neurofibromas are benign tumors that originate from the peripheral nerve sheath and constitute approximately 5% of all benign soft tissue tumors [
1]. Solitary neurofibromas, which occur without an association with neurofibromatosis, are particularly rare and typically present as painless slow-growing masses[
2]. These tumors pose significant diagnostic challenges, particularly in patients with coexisting conditions.
Diabetic foot ulcers, which frequently result from peripheral neuropathy and vascular insufficiency, are a common and serious complication of diabetes mellitus[
3]. These ulcers usually present with infection, induration, and delayed healing, often necessitating a multidisciplinary approach for effective management[
4]. However, the assumption that all toe tip ulcers in patients with diabetes are related to diabetic foot pathology can lead to misdiagnosis and inappropriate management strategies.
This case report highlights a rare instance of a solitary neurofibroma presenting as a toe tip ulcer in a patient with diabetes initially misdiagnosed with a diabetic foot ulcer. Despite the initial misdiagnosis, the diabetic foot evaluations, including peripheral neuropathy and vascular assessments, are relatively safe and cost-effective, justifying their use as first-line diagnostics[
5]. However, the presence of atypical features necessitates further investigation to exclude other tumors. This case underscores the importance of considering a wide range of differential diagnoses, even in the presence of common diabetic complications. By detailing the clinical presentation, diagnostic workup, and successful management of this patient, we aimed to enhance awareness of this rare entity and its potential for misdiagnosis.
2. Case Presentation
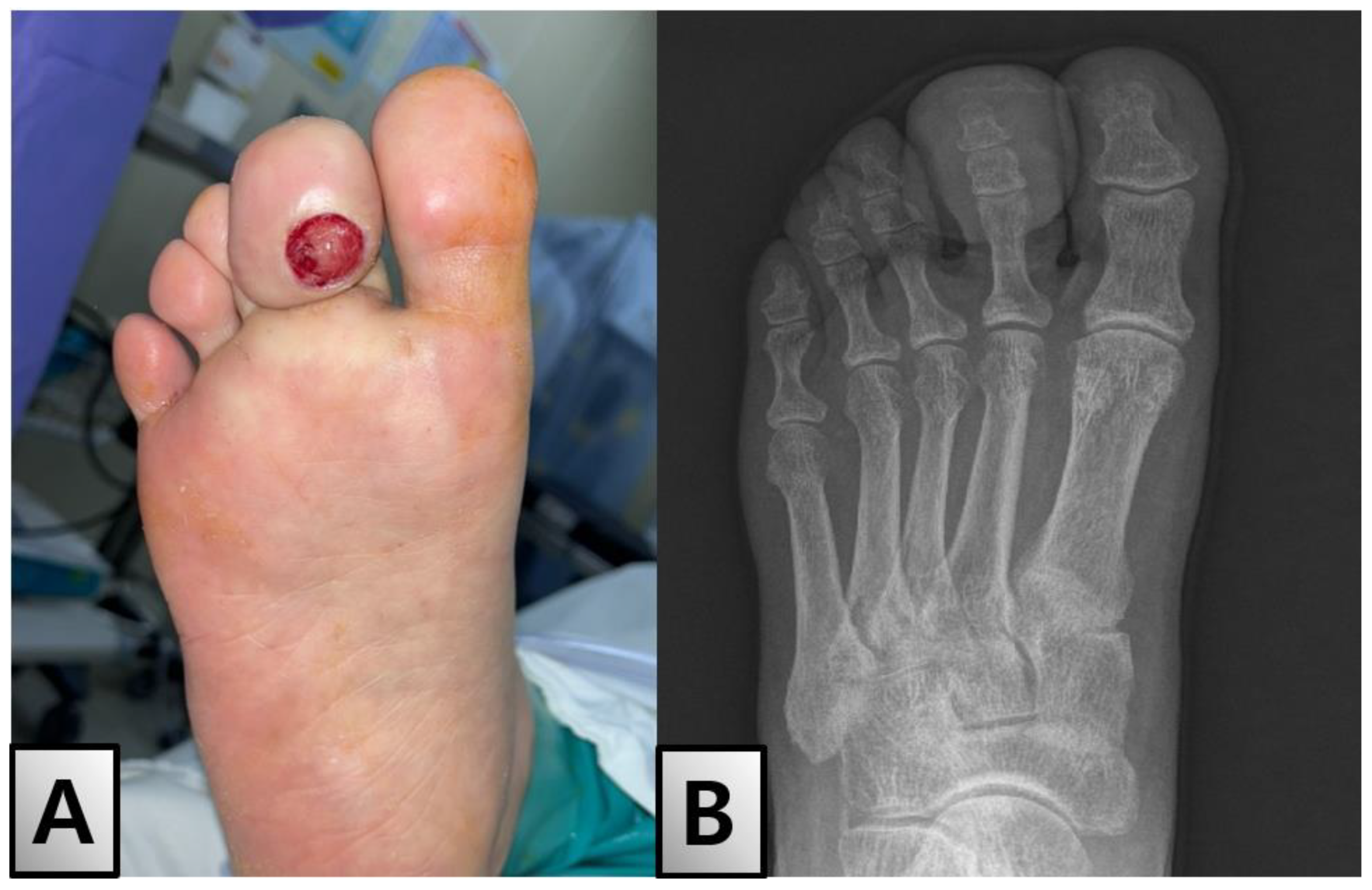
A 55-year-old woman with a history of type 2 diabetes mellitus diagnosed 5 months prior presented with a gradually enlarging ulcer on the right second toe tip over the past 2 months. Physical examination revealed substantial enlargement, induration, and discharge of the toe tips (
Figure 1A). The toe was swollen and showed signs of inflammation; however, there were no signs of systemic infection. Diabetic foot evaluation, including the assessment of peripheral neuropathy and vascular insufficiency, revealed that all test results were within the normal range.
Initial imaging studies included an X-ray, which showed no specific findings in the bony structure (
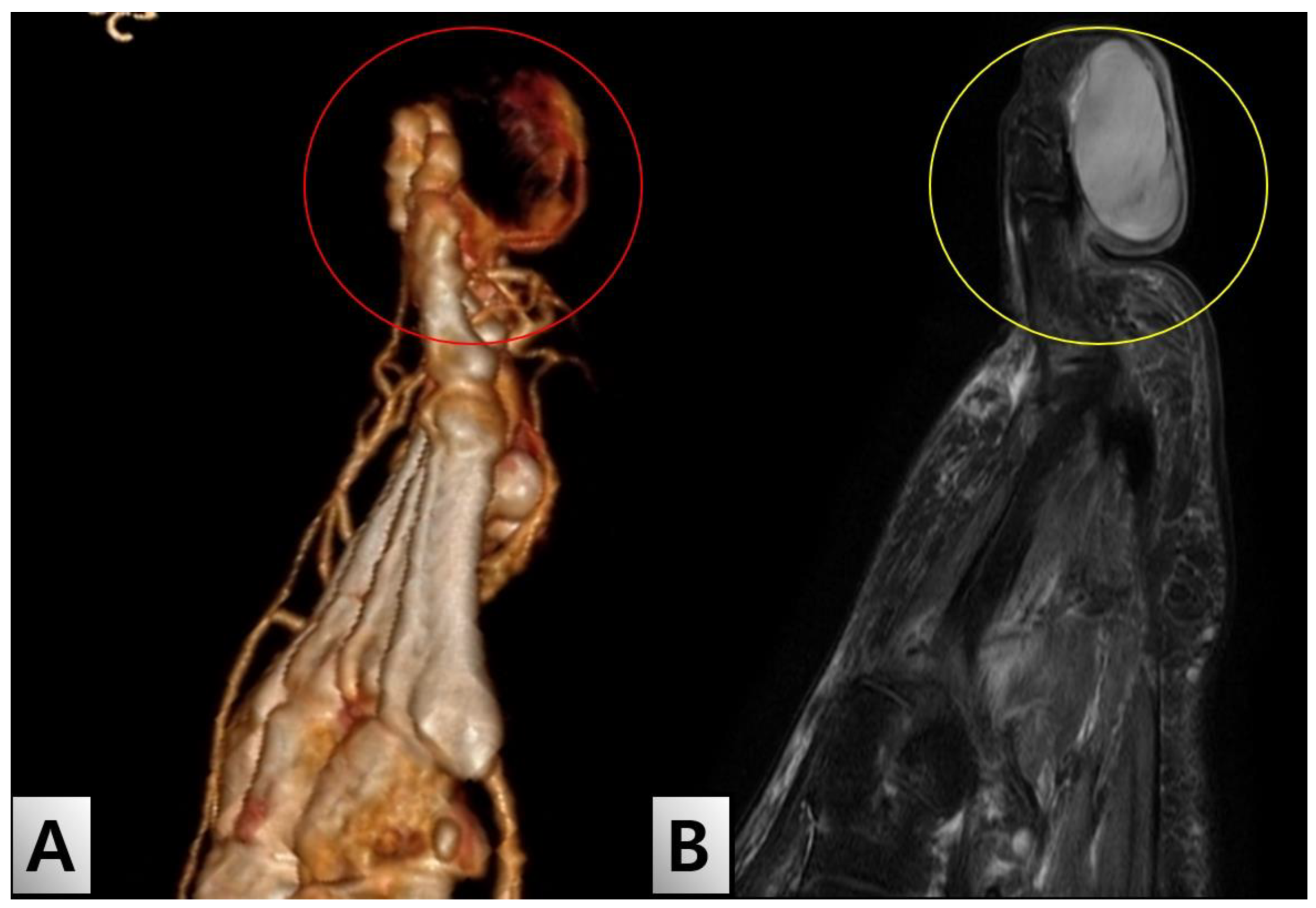
Figure 1B). However, lower extremity angiography-enhanced computed tomography (CT) revealed a mass-like lesion with feeding vessels (
Figure 2A). Magnetic resonance imaging (MRI) depicted a cystic lesion, raising the suspicion of a soft tissue tumor rather than a simple diabetic ulcer (
Figure 2B). Laboratory tests showed that blood parameters were within normal limits, except for slightly elevated levels of inflammatory markers.
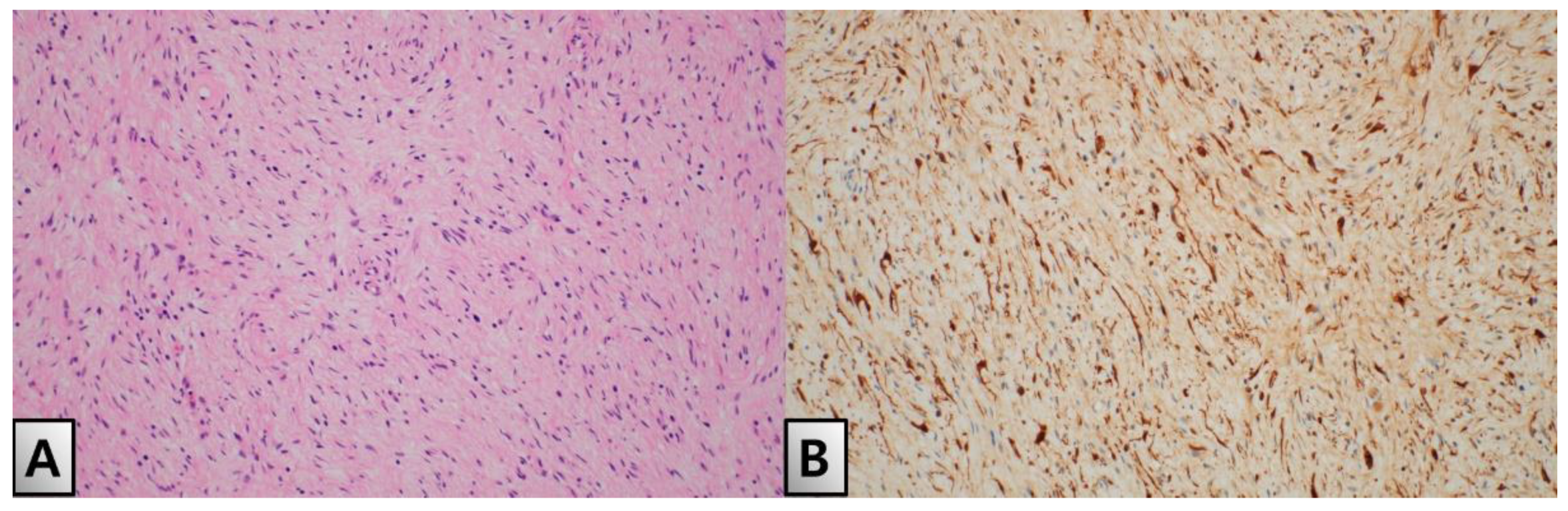
The patient initially underwent a partial excision and biopsy of the lesion. Histopathological examination confirmed the presence of neurofibroma, characterized by interlacing bundles of spindle cells with wavy, darkly stained nuclei, myxoid stroma and collagen fibers. The tumor showed strong positivity in nucleus and cytoplasm for S100 protein (
Figure 4A,B). One month later, the patient was readmitted for the total excision of the mass under general anesthesia. During the surgery, a neurovascular bundle was observed, meticulously skeletonized, and separated before the mass was evacuated (
Figure 3A). The excised mass showed a sheath encasing the neurofibroma (
Figure 3B). Reconstruction of the toe-tip shape was achieved using Z-plasty (
Figure 3C).
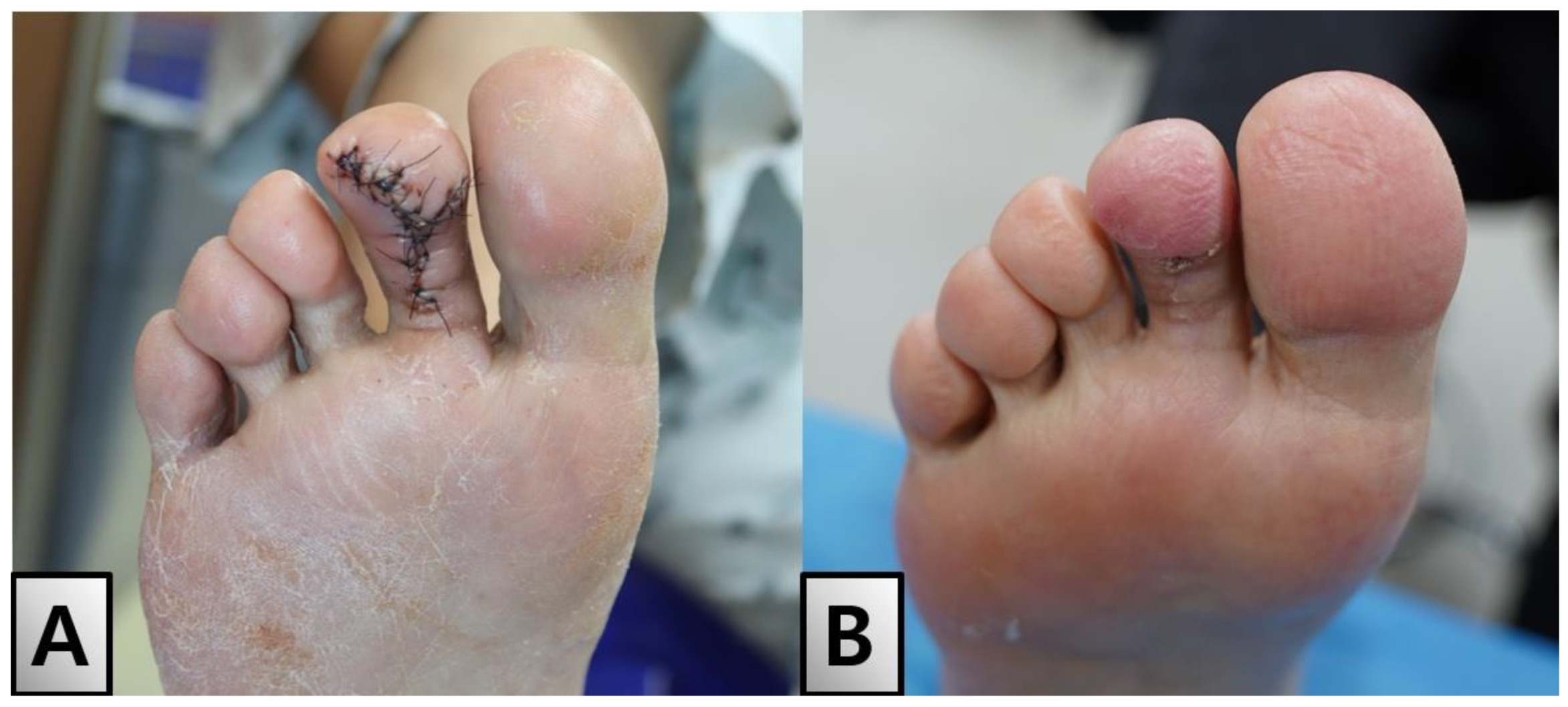
The patient was discharged without wound-related complications one week postoperatively. Follow-ups revealed no scar contractures, functional issues, or sensory abnormalities. The patient reported no symptom recurrence or ulceration at subsequent visits (
Figure 5A). Two months postoperatively, the toe appeared to be well-healed without any signs of infection or other adverse effects (
Figure 5B). This case illustrates the importance of considering neurofibromas in the differential diagnosis of toe tip ulcers, particularly in patients with diabetes, to avoid misdiagnosis and ensure appropriate management.
3. Discussion
Solitary neurofibromas are rare benign tumors originating from the peripheral nerve sheath, with even rarer occurrences in the toe tip region [
6]. These tumors typically present as painless, slow-growing masses, and do not commonly cause ulceration or induration [
2]. Due to their asymptomatic nature and benign appearance, it is challenging to immediately recognize them as neurofibromas when they occur in uncommon locations such as the toe tip. This diagnostic challenge is heightened in patients with diabetes in whom foot lesions are more commonly attributed to diabetic complications [
7].
In this case, the patient’s initial diagnosis of diabetic foot ulcer was reconsidered following advanced imaging studies, which revealed a mass-like lesion with feeding vessels. This finding, combined with the MRI results indicating a cystic lesion, prompted a differential diagnosis that included soft tissue tumors. The initial partial excision and biopsy confirmed the presence of a neurofibroma, leading to subsequent total excision and toe reconstruction.
Despite initial misdiagnosis, diabetic foot evaluation, including peripheral neuropathy and vascular assessment, is relatively safe and cost-effective. These tests are justifiable as first-line diagnostic tests because of their efficiency and low risk [
8]. However, the presence of atypical features in this case highlights the necessity of ruling out other tumors.
The potential for misdiagnosis in patients with diabetes is significant, given that foot ulcers are a common complication of diabetes [
9]. This case underscores the importance of comprehensive diagnostic evaluation, including imaging and biopsy, when typical diabetic foot ulcer treatments fail or when unusual characteristics are present. Early identification and appropriate surgical intervention are crucial to prevent complications and ensure favorable outcomes [
10].
The successful management of this patient underscores the importance of a multidisciplinary approach involving radiologists, pathologists, and surgeons to accurately diagnose and treat solitary neurofibromas. In the present case, a lesion initially suspected to be a routine diabetic foot infection was promptly identified through early histological examination, allowing for a precise pathological diagnosis. This facilitates timely and appropriate surgical excision, resulting in an aesthetically superior toe reconstruction. This case highlights the importance of early histopathological assessment and targeted surgical intervention in achieving optimal functional and cosmetic outcomes in reconstructive surgery. Thorough investigation of lesions, including those initially suspected as straightforward infections, is essential to ensure accurate diagnosis and effective treatment.
One limitation of this case report is the inability to generalize the findings owing to the singular nature of the case. Additionally, the lack of long-term follow-up data limits our understanding of potential recurrence or late-onset complications. However, despite the absence of long-term follow-up, the patient demonstrated an aesthetically pleasing outcome with no adverse effects or complications. The significance of this report lies in its contribution to the differential diagnosis of similar cases. Future studies involving larger cohorts with extended follow-up periods are necessary to validate these findings and establish comprehensive management guidelines.
Although rare, solitary neurofibromas should be considered in the differential diagnosis of atypical toe tip ulcers, particularly in patients with diabetes. This case highlights the critical need for vigilance and thorough evaluation in the management of foot lesions to avoid misdiagnosis and ensure appropriate treatment. Despite the rarity of such cases, this report underscores the importance of considering neurofibromas in the differential diagnosis and provides valuable insights into their management. Further research should aim to elucidate the characteristics and optimal management strategies for neurofibromas in atypical locations to ensure effective diagnosis and treatment in future cases.
Author Contributions
Conceptualization, S.-Y.K.; methodology, S.-Y.K.; formal analysis, H.-J.C.; data curation, M.-H.O.; writing—original draft preparation, H.-J.N.; writing—review and editing, S.-M.L.; visualization, H.-J.C.; supervision, H.-J.C.; project administration, M.-H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
The study was approved for exemption by the Institutional Review Board of Soonchunhyang University Hospital (IRB exemption No. 2024-05-03)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on reasonable request from the corresponding author.
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (grant number 2020R1A2C1100891) and Soonchunhyang Research Fund.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hoda, S.A. Enzinger and Weiss’s S,oft Tissue Tumors. Am J Clin Pathol. 2020, 154, 424. [Google Scholar] [CrossRef]
- Mahmud, S.A.; Shah, N.; Chattaraj, M.; Gayen, S. Solitary Encapsulated Neurofibroma Not Associated with Neurofibromatosis-1 Affecting Tongue in a 73-Year-Old Female. Case Rep Dent. 2016, 2016, 3630153. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, T.V.; Moeini, S.; Skou, S.T.; Madsen, U.R.; Brorson, S. Benefits and Harms of Exercise Therapy for Patients With Diabetic Foot Ulcers: A Systematic Review. Int J Low Extrem Wounds. 2022, 21, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr Diab Rep. 2019, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Pilavaki, M.; Chourmouzi, D.; Kiziridou, A.; Skordalaki, A.; Zarampoukas, T.; Drevelengas, A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol. 2004, 52, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Cheer, K.; Shearman, C.; Jude, E.B. Managing complications of the diabetic foot. BMJ. 2009, 339. [Google Scholar] [CrossRef] [PubMed]
- Hingorai, A.; LaMuraglia, G.M.; Henke, P.; Meissner, M.H.; Loretz, L.; Zinszer, K.M.; Driver, V.R.; Frykberg, R.; Carman, T.L.; Marston, W.; Mills, J.L. Sr.; Murad, M.H. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in Collaboration With the American Podiatric Medical Association and the Society for Vascular Medicine. J Vasc Surg. 2016, 63, 3S–21S. [Google Scholar] [CrossRef] [PubMed]
- Monteiro-Soares, M.; Boyko, E.J.; Ribeiro, J.; Ribeiro, I.; Dinis-Ribeiro, M. Risk stratification systems for diabetic foot ulcers: a systematic review. Diabetologia. 2011, 54, 1190–1199. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lipsky, B.A. Diabetic foot infections: stepwise medical and surgical management. Int Wound J. 2004, 1, 123–132. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).