1. Introduction
Many contact lens wearers experience discomfort either by the end of the day or over the lifespan of their lenses [
1]. This discomfort can stem from various factors, such as deteriorating wettability of the lens over time, deposits accumulating on the lens surface, disruptions in the tear film, and other related issues [
2,
3].
Several studies have investigated changes in vision quality among contact lens wearers during the wearing period [
4,
5,
6]. Visual acuity serves as a primary measure of visual function in clinical settings [
7]. Belda-Salmerón et al. [
5] reported a decrease in visual acuity of approximately 0.02 to 0.04 after 10 hours of daily disposable contact lens wear. Such changes are within the range of repeatability observed in visual acuity measurements (0.04 to 0.06 log units) [
8], suggesting they may not be clinically significant.
Another critical parameter describing vision quality is contrast sensitivity, which is more sensitive to changes than visual acuity [
9]. Belda-Salmerón et al. [
5] observed changes in contrast sensitivity among contact lens wearers throughout the day, although these changes were not statistically significant for some spatial frequencies.
Light scattering in the eye, specifically retinal straylight, also plays a significant role in vision quality. Straylight-related complaints often occur independently of visual acuity or contrast sensitivity issues, necessitating its assessment in clinical practice [
10]. The cornea is a significant source of straylight in young, healthy eyes [
11]. Corneal edema can occur even after a short duration of contact lens wear [
12], potentially increasing retinal straylight. Meulen et al. [
13] found no statistically significant difference in retinal straylight during soft contact lens wear compared to after lens removal; however, rigid lenses significantly increased straylight. Similarly, Cerviño et al. [
4] reported that soft contact lenses do not significantly increase retinal straylight compared to no lenses. There is no published research indicating changes in retinal straylight with the use of new or longer-worn contact lenses. The purpose of this research is to investigate changes in retinal straylight among monthly disposable soft contact lens wearers, comparing new lenses with those worn for a month.
2. Materials and Methods
2.1. Participants
A total of 33 young adults (mean age of 22 ± 1.4 [SD] years) wearing monthly disposable silicone hydrogel contact lenses (SCL) with no ocular diseases participated in this research. Contact lenses were used on daily wear mode and were removed during sleep. All subjects had visual acuity of at least 1.0 (dec. units) and no ocular pathology. The spherical equivalent refraction for participants was between −9.00 and -1.00 D with average refraction -2.75 D. 17 participants wore contact lenses made from comfilcon A material, while 16 participants wore lenses made from lotrafilcon B material. Written consent was obtained from each participant before the study. Ethical approval was given by the Ethical Committee of the Institute of Cardiology and Regenerative Medicine at the University of Latvia.
2.2. Device and Method
Retinal straylight levels were measured by means of a C-Quant straylight metre (Oculus), based on the compensation comparison method. This method involves presenting a flickering (~8 Hz) stimulus with a concentric annulus and a central test field which is divided into two halves. Light scattering in the eye causes some of the flickering light from the annulus to reach the test field and the two halves of the central field will be perceived as flickering. By adding counterphase compensation light, the flickering can be attenuated, resulting in differing modulations between the two halves of the central test field. The subject fixates and identifies which half exhibits stronger flicker. A psychometrical response curve is computed from the responses obtained from the subject [
14]. Values are expressed as the logarithmic value of the straylight parameter, log(s), where higher values indicate greater levels of straylight.
Due to restriction in time the retinal straylight measurements were first made with monthly worn SCL, which were put in no more than 4 hours ago. Then subject removed old lenses and put in new SCL. After 15 min. adaptation time straylight measurements were taken with new SCL. At least three straylight measurements were performed in each condition. Measurements with an estimated standard deviation SD > 0.08 or a quality parameter < 0.5 were rejected and repeated. Among all subjects the questions concerning vision complaints and contact lens material (lotrafilcon B or comfilcon A) was conducted.
All measurements were taken in a dim room (~9 lux, Konica Minolta Illuminance Meter T-10). The dominant eye was used for the measurements, and the other eye was covered with an eyepatch.
2.3. Statistical Analysis
The Kolmogorov-Smirnov test (socscistatistics.com) was employed to assess the normality of data distributions. Average values between data groups were compared using a one-tailed dependent or independent samples t-test. To determine whether the slope of the regression line significantly differs from a hypothetical value, a regression t-test was conducted. A significance level of 0.05 was used for all statistical analyses. The calculations were performed using MS Excel.
When retinal straylight measurements were conducted, the program G*Power 3.1.9.7 [
15] was used to determine if there was an appropriate level of statistical power in this research. A power level of at least 0.8 is recommended for studies involving humans [
16]. Considering the groups' mean values and standard deviations, calculations indicated that a sample size of 33 participants is sufficient to achieve the desired power level.
3. Results
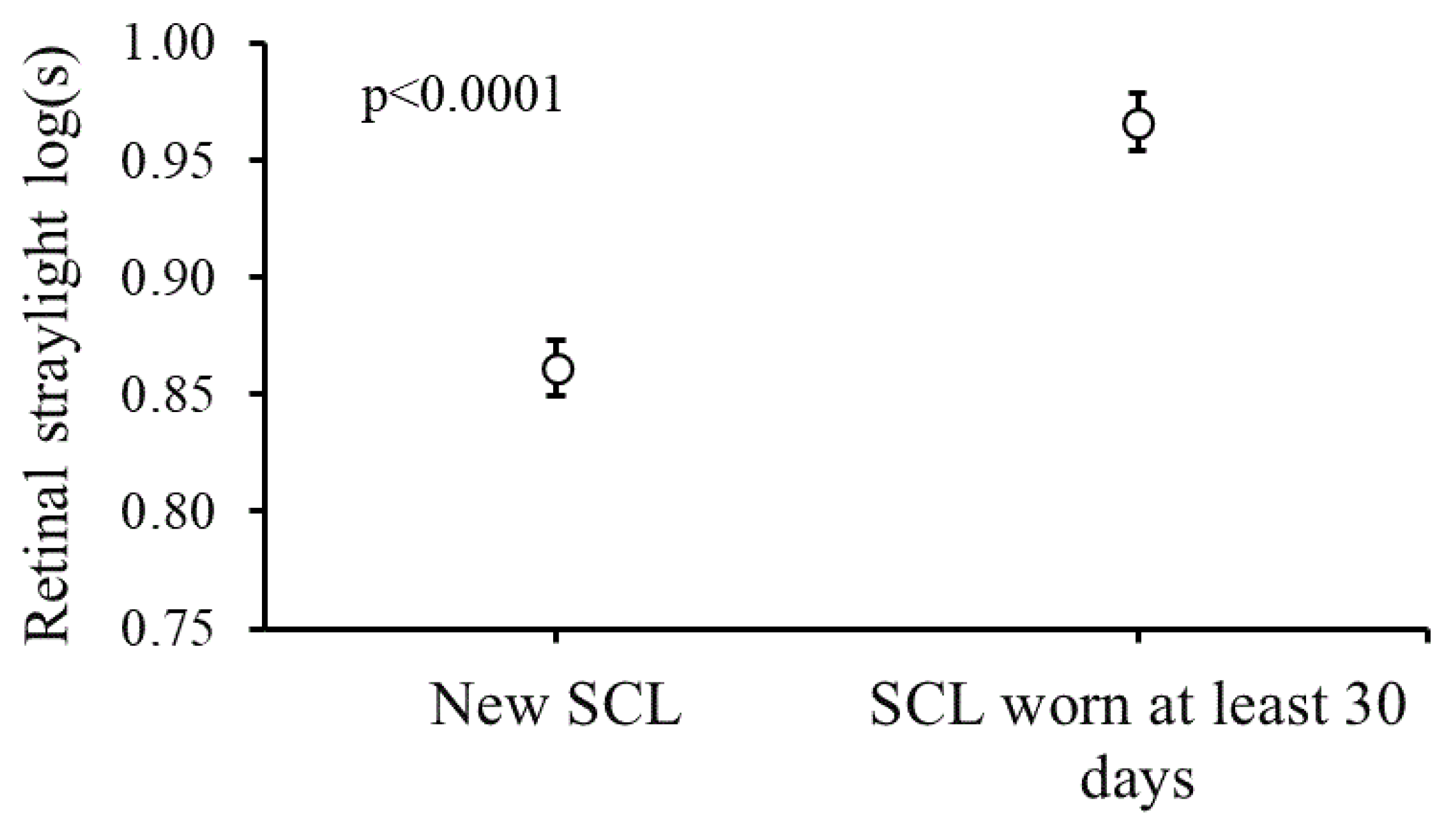
Figure 1 shows the average log(s) values obtained with new and with month-old SCL. A one-tailed paired t-test was used to compare the mean straylight values. There were significant greater retinal straylight with month-old (M = 0.97, SD = 0.17) than with new SCL (M = 0.86, SD = 0.15), t(32) = 7.49, p < 0.0001. Average increase in retinal straylight with old contact lenses was Δlog(s) = 0.11 ± 0.08.
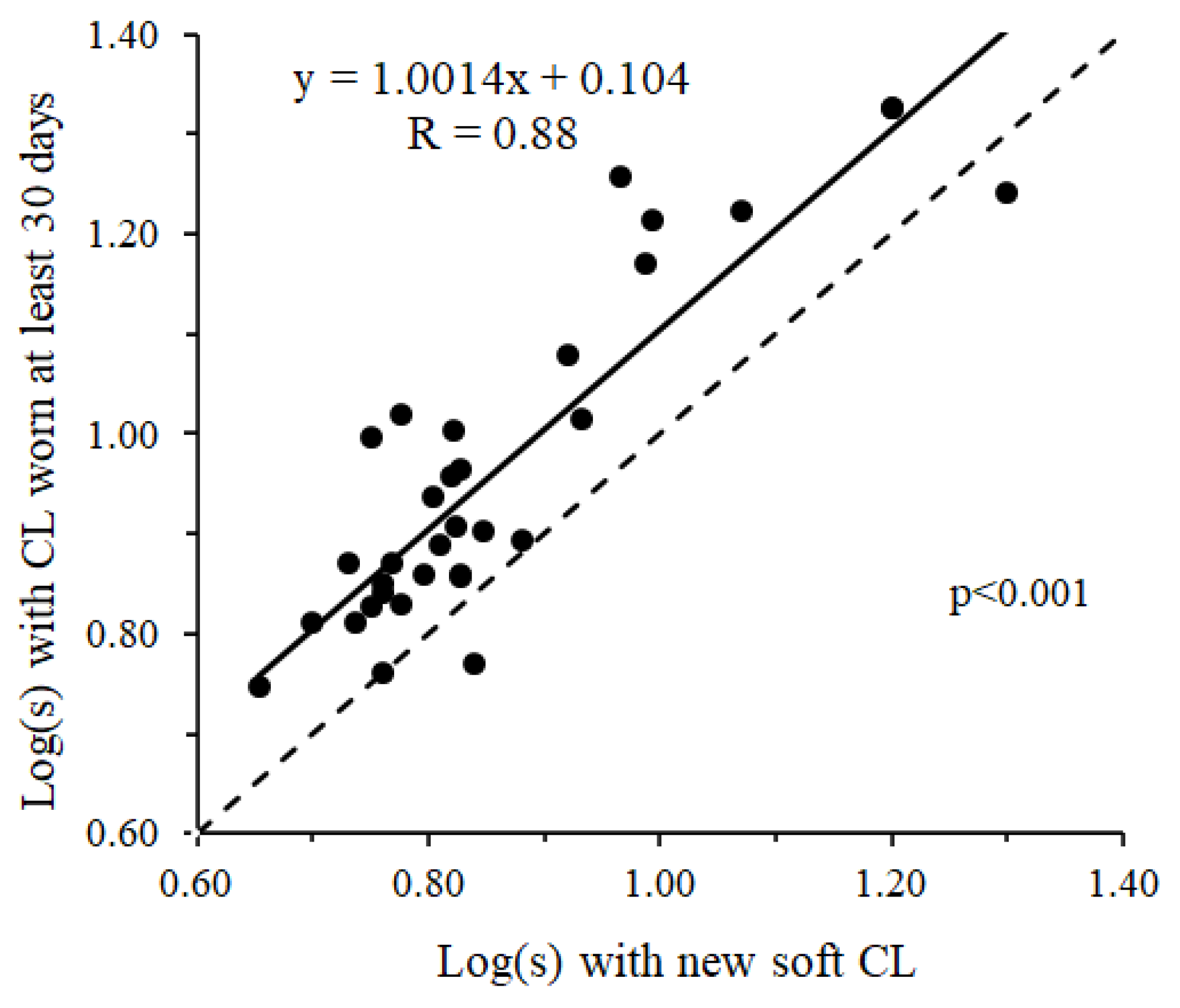
Figure 2 shows the relationship between straylight values with new and monthly worn contact lenses. There is a significant correlation between retinal straylight values obtained under different conditions. Pearson's correlation coefficient was r = 0.88, p < 0.00001. The slope of the regression equation was 1.004, which was not significantly different from 1.0 (p=0.99).
This indicates that the increase in retinal straylight with monthly worn SCLs is consistent regardless of the initial straylight values with new contact lenses.
Figure 2.
Mean log(s) values of all participants measured with new SCl and SCL worn at least 30 days. Standard errors is shown for each data series.
Figure 2.
Mean log(s) values of all participants measured with new SCl and SCL worn at least 30 days. Standard errors is shown for each data series.
There were no significant differences in retinal straylight between the measurements obtained with new lotrafilcon B (M = 0.81, SD = 0.11) and comfilcon A (M = 0.87, SD = 0.18) silicone hydrogel contact lenses contact lenses (p > 0.05).
4. Discussion
Results showed that retinal straylight is significantly greater with monthly worn disposable soft contact lenses (SCLs) compared to new lenses. The average increase in retinal straylight with worn SCLs was Δlog(s) = 0.11 ± 0.08. According to De Wit et al.[
17], an increase of at least log(s) = 0.10 is required for a perceivable difference in vision quality. Therefore, the observed increase with monthly worn disposable SCLs could be clinically relevant.
One of the questions asked to participants was whether they follow instructions for replacing contact lenses and how many days they use monthly contact lenses. Ten participants (~30%) used contact lenses longer than permitted, wearing them for up to 40 days. For this reason, light scatter could have been greater with old contact lenses compared to new ones.
A limitation of this research is that participants wore the worn SCLs for a short period (no longer than 4 hours) before measurements. Corneal edema can occur even after a brief duration of contact lens wear [
12], so it is possible that the increase in retinal straylight with worn SCLs was not solely due to changes in lens material after one month of wear, but also due to corneal edema. However, other research has shown that visual acuity does not significantly change after 4 hours of SCL wear [
5], suggesting that these changes in retinal straylight might be minimal.
We can conclude that monthly soft contact lenses, which were worn at least 30 days, could decrease vision quality, because with used soft contact lenses retinal straylight is significantly larger than with new soft contact lenses.
Author Contributions
Conceptualization, G.I. and I.P.; methodology, G.I.; validation, G.I. and I.P.; formal analysis, G.I.; investigation, G.I.; writing—original draft preparation, G.I. and I.P.; writing—review and editing, G.I. and I.P.; visualization, G.I. supervision, G.I.; project administration: G.I.; funding acquisition, G.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the University of Latvia project No. Y5-AZ77.
Institutional Review Board Statement
The study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethical Committee of the Institute of Cardiology and Regenerative Medicine at the University of Latvia.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Woods, C. A., Bentley, S. A., Fonn, D. (2016). Temporal changes in contact lens comfort over a day of wear. Ophthalmic Physiol. Opt. 2016, 36, 643–648. [CrossRef]
- Guillon, M., Dumbleton, K. A., Theodoratos, P., Wong, S., Patel, K., Banks, G., Patel, T. Association Between Contact Lens Discomfort and Pre-lens Tear Film Kinetics. Optom. Vis. Sci. 2016, 93, 881–891. [CrossRef]
- Sapkota, K., Franco, S., & Lira, M. Daily versus monthly disposable contact lens: Which is better for ocular surface physiology and comfort? Cont. Lens Anterior. Eye 2018, 41, 252–257. [CrossRef]
- Cerviño, A., Gonzalez-Meijome, J.M., Linhares, J.M.M., Hosking, S.L., Montes-Mico, R. Effect of sport-tinted contact lenses for contrast enhancement on retinal straylight measurements. Ophthalmic Physiol. Opt. 2008, 28, 151-156. [CrossRef]
- Belda-Salmerón, L., Ferrer-Blasco, T., Albarrán-Diego, C., Madrid-Costa, D., Montés-Micó, R. Diurnal variations in visual performance for disposable contact lenses. Optom. Vis. Sci., 2013, 90, 682–690. [CrossRef]
- Sapkota, K., Franco, S., Lira, M. Contrast sensitivity function with soft contact lens wear. J. Optom. 2020, 13, 96–101. [CrossRef]
- Williams, M. A., Moutray, T. N., Jackson, A. J. Uniformity of visual acuity measures in published studies. Invest. Ophthalmol. Vis. Sci. 2008, 49, 4321–4327. [CrossRef]
- Raasch, T. W., Bailey, I. L., Bullimore, M. A. Repeatability of visual acuity measurement. Optom. Vis. Sci. 1998, 75, 342–348. [CrossRef]
- Elliott, D. B., Bullimore, M. A., Patla, A. E., Whitaker, D. Effect of a cataract simulation on clinical and real world vision. Br. J. Ophthalmol. 1996, 80, 799–804. [CrossRef]
- Van Den Berg, T. J. T. P., Franssen, L., Coppens, J. E. Straylight in the human eye: Testing objectivity and optical character of the psychophysical measurement. Ophthalmic. Physiol. Opt. 2009, 29, 345–350. [CrossRef]
- Vos, J. J. On the cause of disability glare and its dependence on glare angle, age and ocular pigmentation. Clin. Exp. Ophthalmol. 2003, 86, 363–370. [CrossRef]
- Liesegang, T. J. Physiologic changes of the cornea with contact lens wear. CLAO J. 2002 28, 12–27. https://europepmc.org/article/med/11838985.
- van der Meulen, I. J., Engelbrecht, L. A., van Vliet, J. M., Lapid-Gortzak, R., Nieuwendaal, C. P., Mourits, M. P., Schlingemann, R. O., van den Berg, T. J. Straylight measurements in contact lens wear. Cornea 2010 29, 516–522. [CrossRef]
- Franssen, L., Coppens, J. E., van den Berg, T. J. T. P. Compensation comparison method for assessment of retinal straylight. Investig. Ophthalmol. Vis. Sci. 2006 47, 768–776. [CrossRef]
- Faul, F., Erdfelder, E., Lang, A.-G., Buchner, A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [CrossRef]
- Beck T. W. The importance of a priori sample size estimation in strength and conditioning research. J. Strength. Cond. Res. 2013, 27, 2323–2337. [CrossRef]
- de Wit, G. C., Franssen, L., Coppens, J. E., van den Berg, T. J. Simulating the straylight effects of cataracts. J. Cataract Refract. Surg. 2006, 32, 294–300. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).