Submitted:
09 July 2024
Posted:
09 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Area
2.3. Study Population
2.4. Sample Size
2.5. Survey Instrument
2.6. Recruitment and Data Collection
2.7. Data Analysis
3. Results
3.1. Participant Characteristics
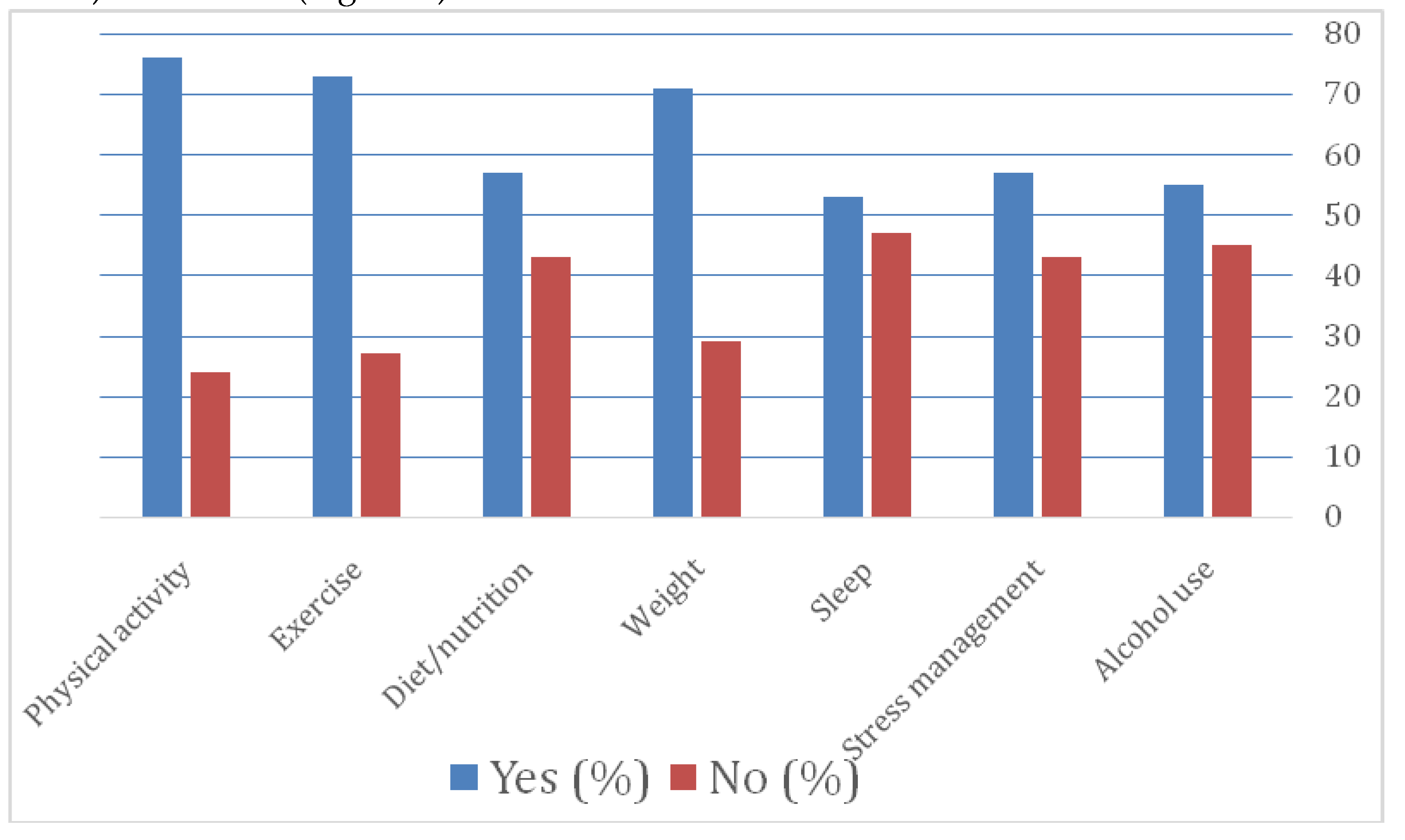
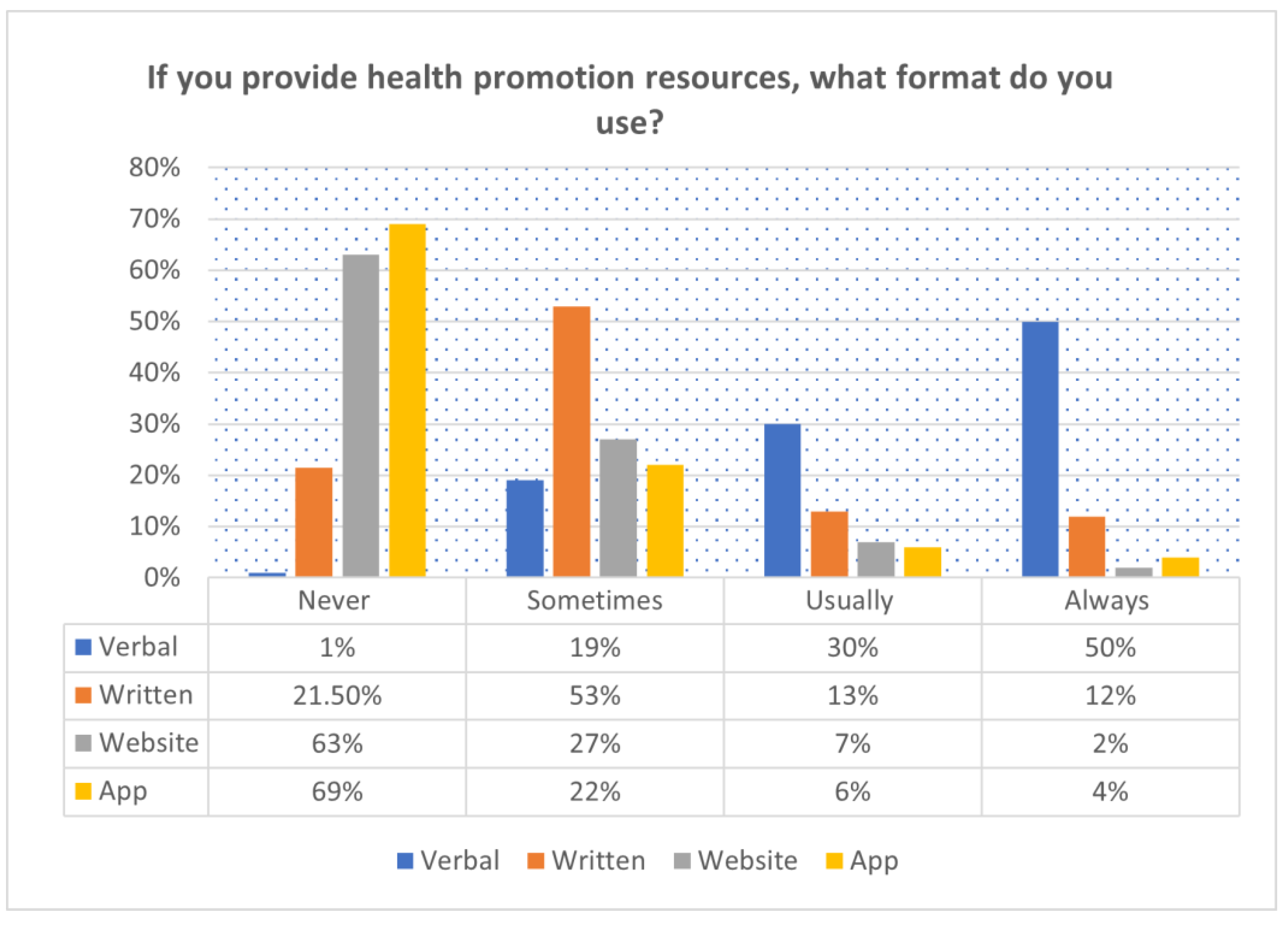
3.2. PT Practice and Levels of Confidence of HP for PwCVDs
3.4. Factors Affecting HP Practice Among PT in Cameroon for pwCVDs
4. Discussion
4.1. PT Practice of HP for PwCVDs by PTs
4.2. PT Levels of Confidence to Deliver HP for PwCVDs by PTs
4.3. Factors Affecting HP Practice for pwCVDs
4.4. Implications for Practice
4.4.1. Clinical
4.4.2. Educational
4.4.3. Policy
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hajat, C.; Stein, E. The Global Burden of Multiple Chronic Conditions: A Narrative Review. Preventive Medicine Reports 2018, 12, 284–293. [Google Scholar] [CrossRef]
- Deaths from Cardiovascular Disease Surged 60% Globally over the Last 30 Years: Report - World Heart Federation Available online:. Available online: https://world-heart-federation.org/news/deaths-from-cardiovascular-disease-surged-60-globally-over-the-last-30-years-report/ (accessed on 10 March 2024).
- Anand, S.; Bradshaw, C.; Prabhakaran, D. Prevention and Management of CVD in LMICs: Why Do Ethnicity, Culture, and Context Matter? BMC Med 2020, 18, 1–5. [Google Scholar] [CrossRef]
- Bowry, A.D.K.; Lewey, J.; Dugani, S.B.; Choudhry, N.K. The Burden of Cardiovascular Disease in Low- and Middle-Income Countries: Epidemiology and Management. Canadian Journal of Cardiology 2015, 31, 1151–1159. [Google Scholar] [CrossRef]
- Peiris, D.; Ghosh, A.; Manne-Goehler, J.; Jaacks, L.M.; Theilmann, M.; Marcus, M.E.; Zhumadilov, Z.; Tsabedze, L.; Supiyev, A.; Silver, B.K.; et al. Cardiovascular Disease Risk Profile and Management Practices in 45 Low-Income and Middle-Income Countries: A Cross-Sectional Study of Nationally Representative Individual-Level Survey Data. PLoS Med 2021, 18, e1003485. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Sun, Y.; Jiang, D.; Wang, C.; Liu, S. Risk-Attributable Burden of Ischemic Heart Disease in 137 Low- and Middle-Income Countries From 2000 to 2019. JAHA 2021, 10, e021024. [Google Scholar] [CrossRef] [PubMed]
- Dzudie, A.; Fourie, J.M.; Scholtz, W.; Scarlatescu, O.; Nel, G.; Kingue, S. PASCAR and WHF Cardiovascular Diseases Scorecard Project. 2020, 31, 8. 31.
- Akono, M.N.; Simo, L.P.; Agbor, V.N.; Njoyo, S.L.; Mbanya, D. The Spectrum of Heart Disease among Adults at the Bamenda Regional Hospital, North West Cameroon: A Semi Urban Setting. BMC Res Notes 2019, 12, 761. [Google Scholar] [CrossRef]
- Nkoke, C.; Jingi, A.M.; Makoge, C.; Teuwafeu, D.; Nkouonlack, C.; Dzudie, A. Epidemiology of Cardiovascular Diseases Related Admissions in a Referral Hospital in the South West Region of Cameroon: A Cross-Sectional Study in Sub-Saharan Africa. PLoS ONE 2019, 14, e0226644. [Google Scholar] [CrossRef] [PubMed]
- About the CVD World Monitor | CVD World Monitor Available online:. Available online: http://cvdworldmonitor.org/about/ (accessed on 22 November 2021).
- World Health Statistics Available online:. Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/world-health-statistics (accessed on 22 November 2021).
- Aminde, L.N.; Takah, N.; Ngwasiri, C.; Noubiap, J.J.; Tindong, M.; Dzudie, A.; Veerman, J.L. Population Awareness of Cardiovascular Disease and Its Risk Factors in Buea, Cameroon. BMC Public Health 2017, 17, 545. [Google Scholar] [CrossRef]
- Tatah, L.; Mapa-Tassou, C.; Shung-King, M.; Oni, T.; Woodcock, J.; Weimann, A.; McCreedy, N.; Muzenda, T.; Govia, I.; Mbanya, J.C.; et al. Analysis of Cameroon’s Sectoral Policies on Physical Activity for Noncommunicable Disease Prevention. IJERPH 2021, 18, 12713. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. European Heart Journal 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Bezner, JR. Promoting Health and Wellness: Implications for Physical Therapist Practice. Phys Ther. 2015;95:1433–1444. Physical Therapy 2016, 96, 123–123. [Google Scholar] [CrossRef]
- Malik, S.H.; Blake, H.; Suggs, L.S. A Systematic Review of Workplace Health Promotion Interventions for Increasing Physical Activity. Br J Health Psychol 2014, 19, 149–180. [Google Scholar] [CrossRef] [PubMed]
- Physiotherapy Practice Start up, Cameroon Available online:. Available online: https://www.indiegogo.com/projects/1307213 (accessed on 8 July 2022).
- Dean, E.; Dornelas de Andrade, A.; O’Donoghue, G.; Skinner, M.; Umereh, G.; Beenen, P.; Cleaver, S.; Afzalzada, D.; Fran Delaune, M.; Footer, C.; et al. The Second Physical Therapy Summit on Global Health: Developing an Action Plan to Promote Health in Daily Practice and Reduce the Burden of Non-Communicable Diseases. Physiotherapy Theory and Practice 2014, 30, 261–275. [Google Scholar] [CrossRef] [PubMed]
- Dean, E.; Umerah, G.; Dornelas de Andrade, A.; Söderlund, A.; Skinner, M. The Third Physical Therapy Summit on Global Health: Health-Based Competencies. Physiotherapy 2015, 101, e13–e14. [Google Scholar] [CrossRef]
- Dean, E. Physical Therapy in the 21st Century (Part I): Toward Practice Informed by Epidemiology and the Crisis of Lifestyle Conditions. Physiotherapy theory and practice 2009, 25, 330–353. [Google Scholar] [CrossRef] [PubMed]
- Frerichs, W.; Kaltenbacher, E.; van de Leur, J.P.; Dean, E. Can Physical Therapists Counsel Patients with Lifestyle-Related Health Conditions Effectively? A Systematic Review and Implications. Physiotherapy Theory and Practice 2012, 28, 571–587. [Google Scholar] [CrossRef] [PubMed]
- Bezner, J.R.; Lloyd, L.; Crixell, S.; Franklin, K. Health Behaviour Change Coaching in Physical Therapy: Improving Physical Fitness and Related Psychological Constructs of Employees in a University Setting. European Journal of Physiotherapy 2017, 19, 1–2. [Google Scholar] [CrossRef]
- Ragupathi, L.; Stribling, J.; Yakunina, Y.; Fuster, V.; McLaughlin, M.A.; Vedanthan, R. Availability, Use, and Barriers to Cardiac Rehabilitation in LMIC. gh 2017, 12, 323. [Google Scholar] [CrossRef]
- Ontario Physiotherapy Leadership Consortium Physiotherapists in Health Promotion: Findings of a Forum. Physiotherapy Canada 2011, 63, 391–392. [CrossRef]
- Higgins, R.; Gray, H. Barriers and Facilitators to Student Physiotherapists’ Use of Psychological Interventions in Physiotherapy Practice. Physiotherapy 2020, 107, e154. [Google Scholar] [CrossRef]
- Rogers, H.L.; Pablo Hernando, S.; Núñez - Fernández, S.; Sanchez, A.; Martos, C.; Moreno, M.; Grandes, G. Barriers and Facilitators in the Implementation of an Evidence-Based Health Promotion Intervention in a Primary Care Setting: A Qualitative Study. JHOM 2021, 35, 349–367. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Valera, M.; Pons-Vigués, M.; Martínez-Andrés, M.; Moreno-Peral, P.; Berenguera, A.; Fernández, A. Barriers and Facilitators for the Implementation of Primary Prevention and Health Promotion Activities in Primary Care: A Synthesis through Meta-Ethnography. PLoS ONE 2014, 9, e89554. [Google Scholar] [CrossRef] [PubMed]
- Cameroon Society of Physiotherapy Available online:. Available online: https://world.physio/membership/cameroon (accessed on 16 March 2022).
- Sharma, K.N. Evidence of Barriers to Evidence-Based Physiotherapy Practice in Central Africa. Int J Health Sci Res 2022, 12, 299–302. [Google Scholar] [CrossRef]
- Kossi, O. Training, Care Delivery, and Research in Physiotherapy in Sub-Saharan French-Speaking Africa. South African Journal of Physiotherapy 2023, 79. [Google Scholar] [CrossRef] [PubMed]
- Abaraogu UO; Edeonuh JC; Frantz J Promoting Physical Activity and Exercise in Daily Practice: Current Practices, Barriers, and Training Needs of Physiotherapists in Eastern Nigeria. Physiother Can 2016, 68, 37–45. [CrossRef]
- Ngeh, E.N.; Lowe, A.; Garcia, C.; McLean, S. Physiotherapy-Led Health Promotion Strategies for People with or at Risk of Cardiovascular Diseases: A Scoping Review. IJERPH 2023, 20, 7073. [Google Scholar] [CrossRef] [PubMed]
- Kelley, K. Good Practice in the Conduct and Reporting of Survey Research. International Journal for Quality in Health Care 2003, 15, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Minh Duc, N.T.; Luu Lam Thang, T.; Nam, N.H.; Ng, S.J.; Abbas, K.S.; Huy, N.T.; Marušić, A.; Paul, C.L.; Kwok, J.; et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J GEN INTERN MED 2021, 36, 3179–3187. [Google Scholar] [CrossRef]
- University of Zambia; Musonda, N. ; Simpamba, M.M.; The University of Zambia A Review of Health Promotion Practices Among Physiotherapists In Africa. JPRM 2021, 3, 14–19. [Google Scholar] [CrossRef]
- Abaraogu, U.O.; Onah, U.; Abaraogu, O.D.; Fawole, H.O.; Kalu, M.E.; Seenan, C.A. Knowledge, Attitudes, and the Practice of Health Promotion among Physiotherapists in Nigeria. Physiotherapy Canada 2019, 71, 92–100. [Google Scholar] [CrossRef]
- Boakye, H.; Quartey, J.; Baidoo, N.A.B.; Ahenkorah, J. Knowledge, Attitude and Practice of Physiotherapists towards Health Promotion in Ghana. South African Journal of Physiotherapy 2018, 74. [Google Scholar] [CrossRef] [PubMed]
- Frantz, J.; Ngambare, R. Physical Activity and Health Promotion Strategies among Physiotherapists in Rwanda. Af Hlth Sci 2013, 13, 17–23. [Google Scholar] [CrossRef]
- Aweto, H.A.; Oligbo, C.N.; Fapojuwo, O.A.; Olawale, O.A. Knowledge, Attitude and Practice of Physiotherapists towards Promotion of Physically Active Lifestyles in Patient Management. BMC Health Serv Res 2013, 13, 21. [Google Scholar] [CrossRef]
- Bodner, M.E.; Rhodes, R.E.; Miller, W.C.; Dean, E. Smoking Cessation and Counseling. American Journal of Preventive Medicine 2012, 43, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Al-Sharman, A.; Aldughmi, M.; Khalil, H.; AlKhawaldeh, H.; Siengsukon, C.F.; El-Salem, K. Knowledge and Attitudes of Physiotherapists toward Sleep: A Survey Study. WOR 2022, 73, 739–746. [Google Scholar] [CrossRef]
- Abaraogu, U.O.; Ogaga, M.O.; Odidika, E.; Frantz, J. Promotion of Healthy Nutrition in Clinical Practice: A Cross-Sectional Survey of Practices and Barriers among Physiotherapists in Southeast Nigeria. Hong Kong Physiotherapy Journal 2016, 35, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Snodgrass, S.J.; Carter, A.E.; Guest, M.; Collins, C.E.; James, C.; Kable, A.K.; Ashby, S.E.; Plotnikoff, R.C. Weight Management Including Dietary and Physical Activity Advice Provided by Australian Physiotherapists: A Pilot Cross-Sectional Survey. Physiotherapy Theory and Practice 2014, 30, 409–420. [Google Scholar] [CrossRef]
- O’Donoghue, G.; Cunningham, C.; Murphy, F.; Woods, C.; Aagaard-Hansen, J. Assessment and Management of Risk Factors for the Prevention of Lifestyle-Related Disease: A Cross-Sectional Survey of Current Activities, Barriers and Perceived Training Needs of Primary Care Physiotherapists in the Republic of Ireland. Physiotherapy 2014, 100, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Abaraogu UO; Ogaga MO; Dean E Practices of Nigerian Physiotherapists with Respect to Lifestyle Risk Factor Assessment and Intervention: A National Cross-Sectional Survey. Physiother Theory Pract 2017, 33, 497–507. [CrossRef]
- Siengsukon, C.F.; Al-dughmi, M.; Sharma, N.K. A Survey of Physical Therapists’ Perception and Attitude About Sleep. J Allied Health 2015, 44, 41–50. [Google Scholar]
- McLean, S.; Charlesworth, L.; May, S.; Pollard, N. Healthcare Students’ Perceptions about Their Role, Confidence and Competence to Deliver Brief Public Health Interventions and Advice. BMC Med Educ 2018, 18, 114. [Google Scholar] [CrossRef] [PubMed]
- Coren, S. Sleep Health and Its Assessment and Management in Physical Therapy Practice: The Evidence. Physiotherapy Theory and Practice 2009, 25, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Fortune, J.; Breckon, J.; Norris, M.; Eva, G.; Frater, T. Motivational Interviewing Training for Physiotherapy and Occupational Therapy Students: Effect on Confidence, Knowledge and Skills. Patient Education and Counseling 2019, 102, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Alodaibi, F.A.; Alotaibi, M.A.; Almohiza, M.; Alhowimel, A.S. Physical Therapists’ Role in Health and Wellness Promotion for People with Musculoskeletal Disorders: A Cross-Sectional Description Study Conducted in Saudi Arabia. JMDH 2022, Volume 15, 567–576. [Google Scholar] [CrossRef]
- Shore, H.; Hebron, C. Musculoskeletal Physiotherapists’ Perceptions of Health Promotion. Musculoskeletal science & practice 2020, 50, 102260. [Google Scholar] [CrossRef]
- Batsis, J.A.; Petersen, C.L.; Clark, M.M.; Cook, S.B.; Kotz, D.; Gooding, T.L.; Roderka, M.N.; Al-Nimr, R.I.; Pidgeon, D.; Haedrich, A.; et al. Feasibility and Acceptability of a Technology-Based, Rural Weight Management Intervention in Older Adults with Obesity. BMC geriatrics 2021, 21, 44. [Google Scholar] [CrossRef]
- Batsis, J.A.; Petersen, C.L.; Clark, M.M.; Cook, S.B.; Lopez-Jimenez, F.; Al-Nimr, R.I.; Pidgeon, D.; Kotz, D.; Mackenzie, T.A.; Bartels, S.J. A Weight Loss Intervention Augmented by a Wearable Device in Rural Older Adults With Obesity: A Feasibility Study. The journals of gerontology. Series A, Biological sciences and medical sciences 2021, 76, 95–100. [Google Scholar] [CrossRef]
- Good and Bad Help: How Purpose and Confidence Transform Lives Available online:. Available online: http://allcatsrgrey.org.uk/wp/wpfb-file/good_and_bad_help_0-pdf/ (accessed on 19 August 2023).
- WHPA Health Improvement Card - Physiopedia Available online:. Available online: https://www.physio-pedia.com/WHPA_Health_Improvement_Card (accessed on 18 April 2024).
- Morrison, C.; Lee, J.P.; Gruenewald, P.J.; Marzell, M. A Critical Assessment of Bias in Survey Studies Using Location-Based Sampling to Recruit Patrons in Bars. Substance Use & Misuse 2015, 50, 1427–1436. [Google Scholar] [CrossRef]
| Variable | n | % | |
|---|---|---|---|
| Sex | Male Female |
96 85 |
53.0 47.0 |
| Mean age (years) | 34.43 ± 9.0 | 181 | 100 |
| Mean working duration | 8.96 ±6.0 | 181 | 100 |
| Mean number of PT per service | 4.31 ± 4.60 | 181 | 100 |
| Educational level | Higher Diploma Bachelor’s Degree Master’s Degree Others |
75 81 22 3 |
41.4 44.4 12.2 1.7 |
| Location of participants | Central East Far North Littoral North North-West South-West West |
68 4 3 51 1 27 21 6 |
37.6 2.2 1.7 28.2 0.6 14.9 11.6 3.3 |
| Location of training | Cameroon Africa Europe United States |
173 4 3 1 |
95.6 2.3 1.7 0.6 |
| Clinical specialism | Musculoskeletal Cardiorespiratory Neurology Paediatric Sports No speciality |
7 3 6 3 11 151 |
3.9 1.7 3.3 1.7 6.1 83.4 |
| Settlement | Rural Urban |
24 157 |
13.3 86.7 |
| Sector of work | Private Public Both private and public Others (NGOs and missionary hospitals) |
73 51 51 6 |
40.3 28.2 28.2 3.3 |
| Current institution of practice | Tertiary Hospital Secondary/regional hospital District Hospital Community Health Centre Clinic Rehabilitation centre Special School Education/university others |
29 29 23 4 54 32 2 13 19 |
16.0 16.0 12.7 2.2 29.8 17.7 1.1 7.2 10.5 |
| Please indicate which of the relevant areas best describes your interventions. | |||
|---|---|---|---|
| Never | Sometimes | Always | |
| Discuss weight management. | 8% (n=14) | 18% (n=30) | 74%(n=123) |
| Dietary advice regarding eating more fruits | 6% (n=11) | 21% (n=35) | 73%(n=127) |
| Increase general physical activity | 2% (n=3) | 30% (n=51) | 69%(n=118) |
| Increase specific exercise uptake | 3% (n=5) | 28% (n=48) | 69%(n=118) |
| Encourage the patient to stop smoking. | 11% (n=18) | 21% (n=35) | 69%(n=116) |
| Dietary advice to decrease excessive salt use | 13%(n=22) | 22% (n=38) | 65%(n=111) |
| Condition-specific education for patients with Known chronic Cardiovascular Conditions | 8% (n=14) | 28% (n=47) | 64%(n=109) |
| Counsel to manage stress | 9% (n=16) | 30% (n=50) | 61%(n=103) |
| Dietary advice regarding eating more vegetables | 9% (n=15) | 32% (n=54) | 60%(n=102) |
| Explain the value of BMI as a measure of health | 13% (n=22) | 29% (n=49) | 58%(n=98) |
| Education around normal sleeping patterns. | 17% (n=29) | 34%(n=57) | 48%(n=83) |
| Are you confident in assessing the lifestyle and behaviour of people at risk or with CVDs? | |||
|---|---|---|---|
| Not confident at all | Slightly confident | confident | |
| Weight | 14% (n=24) | 22% (n=38) | 64%(n=110) |
| Alcohol use | 19% (n=33) | 25%(n=43) | 56%(n=95) |
| Physical activity | 11% (n=18) | 36%(n=61) | 53%(n=92) |
| Stress management | 19% (n=32) | 29%(n=50) | 52%(n=95) |
| Diet | 15% (n=26) | 35%(n=59) | 50%(n=84) |
| Sleep | 24% (n=41) | 36%(n=61) | 39%(n=67) |
| To what extent do you agree with the following statements: | |||
| POTENTIALLY LIMITING HP PRACTICE | |||
| Intrapersonal factors | Disagree | Undecided | Agree |
| I commonly use health promotion for those at high risk of CVD or those with complications only. | 15%(n=26) | 21%(n=36) | 64%(n=110) |
| I believe the professional role of physiotherapist is to primarily treat patients using passive modalities | 42%(n=72) | 27%(n=47) | 30%(n=53) |
| Interpersonal factors | |||
| I lack the skills and economic resources to implement health promotion in my practice. | 51%(n=87) | 21%(n=36) | 28%(n=49) |
| I use my personal lifestyle experiences to facilitate health promotion for patients | 6%(n=11) | 17%(n=30) | 76%(n=131) |
| My patients lack the interest to adhere to health promotion recommendations | 40%(n=68) | 36%(n=61) | 25%(n=42) |
| Institutional factors | |||
| I have regular training (continuous professional development) in health promotion | 35%(n=60) | 25%(n=43) | 40%(n=68) |
| There are no resources on health promotion in my institution | 53%(n=90) | 24%(n=40) | 23%(n=39) |
| We lack an organised practice with referral units like nutrition service and counselling units | 27%(n=47) | 20%(n=35) | 53%(n=90) |
| The lack of role clarification with other healthcare providers hinders health promotion practice in my institution. | 41%(n=70) | 27%(n=46) | 32%(n=55) |
| I lack office space for health promotion | 51%(n=88) | 22%(n=38) | 27%(n=46) |
| Community/Public factors | |||
| There are no existing guidelines for prevention of CVD in our setting | 48% (n= 82) | 24%(n=41) | 28%(n=49) |
| There are no physiotherapy health promotion practices in public hospitals or settings | 48%(n=82) | 30%(n=52) | 22%(n=38) |
| There are no physiotherapy health promotion practices in a private hospital | 42%(n=73) | 40%(n=69) | 17%(n=30) |
| POTENTIALLY ENHANCING HP PRACTICE | |||
| Intrapersonal factors | Disagree | Undecided | Agree |
| Medical management is more important than lifestyle modification for chronic conditions | 63%(n=110) | 22%(n=37) | 15%(n=25) |
| I am confident I have appropriate skills and knowledge on health promotion and disease prevention | 6%(n=11) | 22%(n=38) | 68%(n=123) |
| Because of my personal difficulty dealing with a lifestyle issue like being overweight, smoking, etc, I find it difficult to talk about similar issues with my patients | 67%(n=115) | 19%(n=32) | 14%(n=24) |
| I normally do not waste my time on health promotion for patients as it will not be effective. | 74%(n=127) | 12%(n=21) | 13%(n=22) |
| I believe that there will be no change in patients’ behaviour even if I provide lifestyle recommendations | 71%(n=121) | 13%(n=23) | 16%(n=28) |
| Interpersonal factors | |||
| I have confidence in my team members and colleagues to assist me in implementing health promotion in my practice | 8%(n=14) | 22%(n=38) | 70%(n=119) |
| I do not practice health promotion because it will conflict with the original reason for patient consultation | 75%(n=128) | 13%(n=22) | 12%(n=21) |
| Institutional factors | |||
| I lack the time to implement health promotion in my practice. | 59%(n=100) | 24%(n=40) | 17%(n=30) |
| My working conditions do not permit me to implement health promotion. | 52%(n=89) | 28(n=48) | 20%(n=34) |
| I do not practice health promotion because there are no financial benefits to health promotion | 66%(n=113) | 18%(n=31) | 16%(n=28) |
| Community/Public factors | |||
| Because of the social class or status of some patients, I find it difficult to discuss health promotion recommendations | 56%(n=97) | 25%(n=43) | 19%(n=32) |
| Religious practices make it difficult for me to promote health in my practice. | 61%(n=104) | 20%(n=35) | 19%(n= 33) |
| Because of cultural practices and language, I find it challenging to implement health promotion in my practice. | 59%(n=102) | 23%(n=39) | 18%(n=31) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




