Introduction
The Covid19 pandemic, an unparalleled global health crisis, has profoundly impacted the world, claiming over 6.3 million lives from more than 571 million cases by July 28, 2022. Ghana, experiencing its first cases on March 12, 2020, has not been spared, reflecting the pandemic's extensive reach and its deep-seated effects on societal well-being, including economic, social, and health-related dimensions (Adu et al., 2021). The pandemic has led to enforced quarantines, significant job losses, and a staggering loss of life, highlighting its multifaceted impact on global society.
Research underscores the pandemic's negative effects on workplace environments, with a notable rise in stress, depression, and anxiety among employees (Walton, Murray & Christian, 2020; Yu, Park & Hyun, 2021). Vulnerable populations, such as women, children, those with pre-existing health conditions, and the unemployed, have been particularly hard hit, exacerbating existing inequalities (Greenberg et al., 2020; Zaka et al., 2020). The fear of unemployment has become a significant source of stress, leading to widespread emotional distress and deteriorating mental health (Vizheh et al., 2020; Makridis & Wu, 2021).
In this context, social capital has emerged as a crucial element in mitigating the impacts of crises (Makridis & Wu, 2021; Zheng, Khan & Hussain, 2020). Historical instances, such as the SARS, Ebola, and Zika outbreaks, have shown the vital role of social capital in crisis response and recovery, underscoring its significance in building community resilience and cooperation (Lee et al., 2021; Bartscher et al., 2021). For developing countries like Ghana, where societal challenges often compound health issues, the World Health Organization (WHO) has identified social capital as a key factor in moderating mental health outcomes (Sato et al., 2020; Ehsan & Spini, 2020). Social networks facilitate the exchange of resources, both tangible and intangible, enhancing individual and collective well-being. Theories suggest that social capital can increase resilience, promote adherence to beneficial norms, and improve collective efficacy, thereby bettering health outcomes (Goodman et al., 2022).
Although there is a well-documented relationship between Covid19 and reduced mental health (Usher, Durkin & Bhullar, 2020), specific research focusing on the Ghanaian context remains limited. While the general protective effects of social capital are well-established, there is a need to explore how these dynamics specifically manifest among employees in Ghana. The socio-cultural context of Ghana, characterized by strong communal ties and social networks, may present unique interactions between social capital and mental health. This study suggests that social capital moderates the relationship between the COVID19 pandemic and mental health among employees in Ghana. It argues that robust social networks can alleviate the pandemic's adverse effects on mental health, despite challenges like prolonged lockdowns, food shortages, and limited healthcare access. Thus, the study tend to answer how social capital moderates the relationship between the Covid19 pandemic and mental health among employees in Ghana?
Objectives of the Study
The following are the objectives of the study:
To examine the effect of the Covid19 Pandemic on mental health of employees in Ghana
To examine the effect of Social Capital on the mental health of employees in Ghana
To examine the moderating effect of Social capital on the relationship between Covid19 Pandemic and Mental Health of Employees in Ghana
Literature Review
Covid19 Pandemic and Mental Health
The Covid19 pandemic has significantly exacerbated many occupational risk factors for poor mental health. As the virus spread globally, concerns about community transmission, rising case numbers, and fatalities have heightened worry and anxiety among employees (Liu et al., 2020). Numerous international studies have highlighted that many employees are anxious about contracting and spreading Covid19 at their workplaces (Horsch, Lalor, & Downe, 2020). This persistent fear can negatively impact mental health, leading to increased anxiety, depression, and decreased job performance (Wilson et al., 2020).
In Canada, the economic instability and fear of illness induced by the Covid19 pandemic have been primary contributors to declining mental health among employees (Ruffolo et al., 2021). Notably, these adverse mental health effects have been more pronounced in high-risk, high-visibility workplaces, where the potential for virus transmission is higher (Greenberg, 2020). Furthermore, employees experiencing increased awareness of Covid19 spread report heightened emotional exhaustion, which is influenced by demographic factors and perceived infection risk at the workplace (Song et al., 2020; Greenberg et al., 2021).
In addition, the fear of jeopardizing the health of loved ones adds to the mental burden faced by employees (Tracy et al., 2020). The constant exposure to an infodemic, characterized by overwhelming and rapidly evolving information about Covid19, further exacerbates pandemic fatigue and mental distress (Kontoangelos, Economou, & Papageorgiou, 2020). Isolation measures such as confinement and quarantine, though necessary for controlling virus spread, have also been linked to worsening mental health issues among employees (Huang et al., 2020). The lack of social interaction with coworkers can increase stress levels, and healthcare workers, in particular, may experience stigma and social isolation, leading to emotional distress and depression (Tsamakis et al., 2020).
The pandemic has also resulted in significant job losses, which have further heightened stress and deteriorated health among those affected (Toh et al., 2021). Therefore, understanding the unique impact of the Covid19 pandemic on employees' mental health is crucial for developing effective interventions. Given this context, we hypothesize that social capital may play a moderating role in mitigating these adverse mental health outcomes among employees in Ghana.
Social Capital and Mental Health
The relationship between social capital and mental health has been extensively studied across various populations, including employees. Social capital, defined as the resources available within social networks, has consistently been linked to improved mental health outcomes (McKenzie & Harpham, 2006; De Silva et al., 2005). Higher levels of social capital have been associated with better mental health across different socioeconomic backgrounds, including among working adults (De Silva et al., 2005; Drukker, 2003). For employees, social capital can provide emotional support, information, and tangible resources, which are essential for coping with workplace stress and anxiety (Aldridge et al., 2002; Kawachi & Berkman, 2001). Supportive friendships and a sense of belonging within the workplace can buffer the negative effects of stress, daily challenges, and even illness, thereby enhancing overall mental well-being (Wilkinson, 2002).
Studies have shown that strong social networks among employees can reduce feelings of loneliness, hopelessness, and depression, while promoting happiness and a sense of community (Brown & Harris, 1978). For instance, Aneshensel and Sucoff (1996) found that children and young adults in low-income areas with higher social capital were less likely to experience mental health issues such as depression and anxiety. Similarly, increased social connections among employees can foster a supportive work environment, mitigating mental health challenges.
In the context of the COVID-19 pandemic, social capital has emerged as a critical protective factor for employees' mental health. Research has highlighted that community-based social capital can provide significant support for older adults during the pandemic, particularly as they face increased isolation (Li, Jiang, & Fang, 2020). For employees, maintaining social ties and accessing support through their networks can reduce the social costs of individual activities and encourage collective actions to protect common interests (Anwar et al., 2020). Given the context-specific nature of social capital, our study aimed to explore its moderating role in the relationship between COVID-19 and mental health among employees in Ghana. We hypothesize that higher levels of social capital will buffer the negative mental health impacts of the pandemic on employees, providing essential emotional and practical support
Moderation Effects of Social Capital
The COVID-19 pandemic has significantly impacted the mental health of workers worldwide. Both those with pre-existing mental health conditions and those without prior mental health issues are at increased risk of experiencing psychological distress due to the pandemic (Bufquin et al., 2021). Employment-related factors and organizational structures can either exacerbate or mitigate these mental health impacts. Therefore, examining the social aspects of the pandemic, alongside medical and economic ramifications, is crucial for understanding and addressing the mental health challenges faced by employees.
Social capital, as a modifiable protective factor, can play a pivotal role in supporting employees' mental health during and after the acute phase of the COVID-19 pandemic. Strong social networks can provide emotional support, reduce feelings of isolation, and enhance resilience among employees (Giorgi et al., 2020). The community ties and social cohesion inherent in social capital are particularly valuable for older employees and those required to self-quarantine, as they navigate the challenges posed by the pandemic (Li, Jiang, & Fang, 2020).
In conclusion, our study aims to investigate the moderating role of social capital in the relationship between COVID-19 and mental health among employees in Ghana. By exploring this dynamic, we seek to provide evidence-based recommendations for leveraging social capital to improve mental health outcomes for employees during and beyond the COVID-19 pandemic.
Theoretical Framework
The theoretical foundation of our study is anchored in the Health Belief Model (HBM) and social capital theory.
Health Belief Model (HBM)
Health Belief Model (HBM) is a comprehensive framework that has significantly influenced health behavior research since its inception in the 1950s by social psychologists Hochbaum, Rosenstock, and Kegels in response to the failure of a free tuberculosis health screening program (Rosenstock, 1974). The HBM posits that individuals' decisions regarding health behaviors are influenced by their perceptions of a health threat and the benefits of and barriers to taking action to avoid or mitigate the threat (Janz and Becker, 1984). This model is particularly relevant to our study, which examines the impact of social capital on mental health-related stress among workers in Ghana during the Covid19 pandemic.
Firstly, the HBM's construct of perceived susceptibility, which refers to an individual's assessment of their risk of contracting a condition, directly correlates with our investigation into workers' perceptions of Covid19 risk. Studies have shown that higher perceived susceptibility to Covid19 is associated with increased adherence to preventive measures (Bish and Michie, 2010), underscoring the importance of understanding these perceptions in promoting health-enhancing behaviors.
Moreover, the model's concept of perceived severity, or the belief in the seriousness of contracting an illness, provides a lens through which to view the psychological impact of the pandemic. Research indicates that perceptions of Covid19 as a severe health threat can significantly affect mental health, leading to increased stress and anxiety (Person et al., 2004). This aligns with our focus on mental health distress among Ghanaian workers, suggesting that interventions aimed at managing perceptions of severity could mitigate adverse mental health outcomes.
The interplay between perceived susceptibility and perceived severity is critical in shaping health behaviors and outcomes. According to the HBM, individuals are more likely to take preventive actions when they believe they are susceptible to a serious illness. In our study, this relationship is particularly relevant as it helps explain how employees' perceptions of their risk and the severity of Covid19 influence their mental health and behavior. For instance, an employee who perceives a high susceptibility to Covid19 and believes that contracting the virus would have severe health consequences is likely to experience significant anxiety and stress. This heightened mental distress can be mitigated through social capital, which provides emotional support, information, and practical resources (Kawachi & Berkman, 2001). Thus, understanding these perceptions is crucial for developing effective interventions aimed at reducing anxiety and promoting mental well-being among employees during the pandemic.
The inclusion of perceived susceptibility and perceived severity constructs is not only theoretically significant but also practically relevant for our study. We hypothesize that higher levels of perceived susceptibility and severity are associated with greater anxiety and mental distress among employees. These hypotheses are rooted in the broader health behavior literature, which suggests that individuals who perceive themselves to be at high risk and who believe the consequences of the disease to be severe are more likely to experience heightened anxiety and stress (Bish & Michie, 2010). Furthermore, the role of social capital is examined as a moderating factor in these relationships. Social capital, encompassing elements such as trust, communication, and support within the workplace, can buffer the negative mental health impacts of high perceived susceptibility and severity. This moderating effect is crucial for understanding how social networks and support systems can mitigate stress and anxiety among employees during the pandemic.
The HBM also emphasizes the role of perceived benefits and barriers in health behavior decisions. In the context of our study, this translates to the assessment of social capital as a beneficial resource that can offset the negative outcomes of the pandemic. Social networks and support systems are known to play a crucial role in health behavior, offering emotional support, information, and tangible resources that can reduce stress and promote coping strategies (Kawachi and Berkman, 2001). By leveraging the HBM, we can better understand how the perceived benefits of social capital influence individuals' engagement with health-promoting behaviors and mental health resilience.
Lastly, the model's cue to action component, which involves external or internal stimuli prompting health behavior change, is reflected in our examination of Covid19 awareness and information dissemination within social networks. The rapid spread of the virus and the evolving nature of public health guidelines highlight the importance of timely and accurate health communication in influencing behaviors (Rosenstock et al., 1988).
In essence, the Health Belief Model offers a robust theoretical framework for our study, providing valuable insights into the complex interplay between individual health beliefs, social capital, and health behaviors during the Covid19 pandemic. By applying the HBM, we aim to contribute to the broader discourse on health behavior research, offering evidence-based recommendations for enhancing public health responses in Ghana and beyond. This approach not only enriches our understanding of health behavior dynamics in the face of a global health crisis but also underscores the critical role of social capital in navigating the pandemic's challenges.
Social Capital Theory
Social Capital Theory provides a more fitting theoretical underpinning for our study, focusing on the resources accessible through social networks and their impact on individual and collective well-being (Putnam, 2000). In the context of the Covid-19 pandemic, social capital can be a critical buffer against mental health stressors by providing emotional support, access to information, and practical assistance (Bourdieu, 1986; Coleman, 1988).
The relevance of social capital to mental health is well-documented, with studies showing that robust social networks can mitigate stress and anxiety, enhance coping mechanisms, and improve overall mental well-being (Kawachi & Berkman, 2001). In Ghana, where communal ties and social networks are integral to daily life, understanding the role of social capital in buffering the mental health impact of the pandemic is crucial.
By integrating Social Capital Theory, we aimed to offer a nuanced understanding of how social networks influence mental health outcomes among employees in Ghana during the Covid19 pandemic. This approach allowed us to examine the multifaceted ways in which social capital can serve as a protective factor, thereby enriching our analysis and providing actionable insights for public health interventions.
Methods
Data Collection
The study employed a cross-sectional survey design to collect data from employees across various industries in Ghana. To enhance the reliability and validity of our findings, we adopted a simple random sampling technique. This approach was chosen to minimize selection bias and ensure that every potential participant within the target population had an equal chance of being included in the study.
The sampling process for the study was designed to ensure both transparency and replicability, beginning with the careful identification of the target population. Employees across a variety of sectors in Ghana, such as manufacturing, services, and agriculture, were earmarked for participation, ensuring a broad representation of the workforce. Following this, the selection of worksites was conducted with precision. Utilizing a comprehensive list from the Ghanaian Chamber of Commerce's database, 50 worksites were randomly chosen through a computer-generated sequence of numbers, each linked to a specific worksite, thereby ensuring an unbiased selection process.
Transitioning smoothly into the next phase, simple random sampling was employed within these predetermined worksites. Each employee was assigned a unique identifier, a crucial step that paved the way for the use of a random number generator. This tool selected participants from the pool, guaranteeing that every employee had an equal chance of being included in the study. This methodological rigor not only underscored the study's commitment to fairness but also bolstered the integrity of the sampling process, laying a solid foundation for the subsequent research activities.
Sample Population
The survey was conducted amongst a total of 450 employees initially targeted for the study, out of which 422 fully participated, resulting in a participation rate of approximately 93.8%. The high participation rate suggests a strong representation of the target population. These participants were selected from various industries located in Ghana, providing a diverse and comprehensive sample that represents the broader workforce in the region aiming to reflect the diversity of the workforce.
Measures
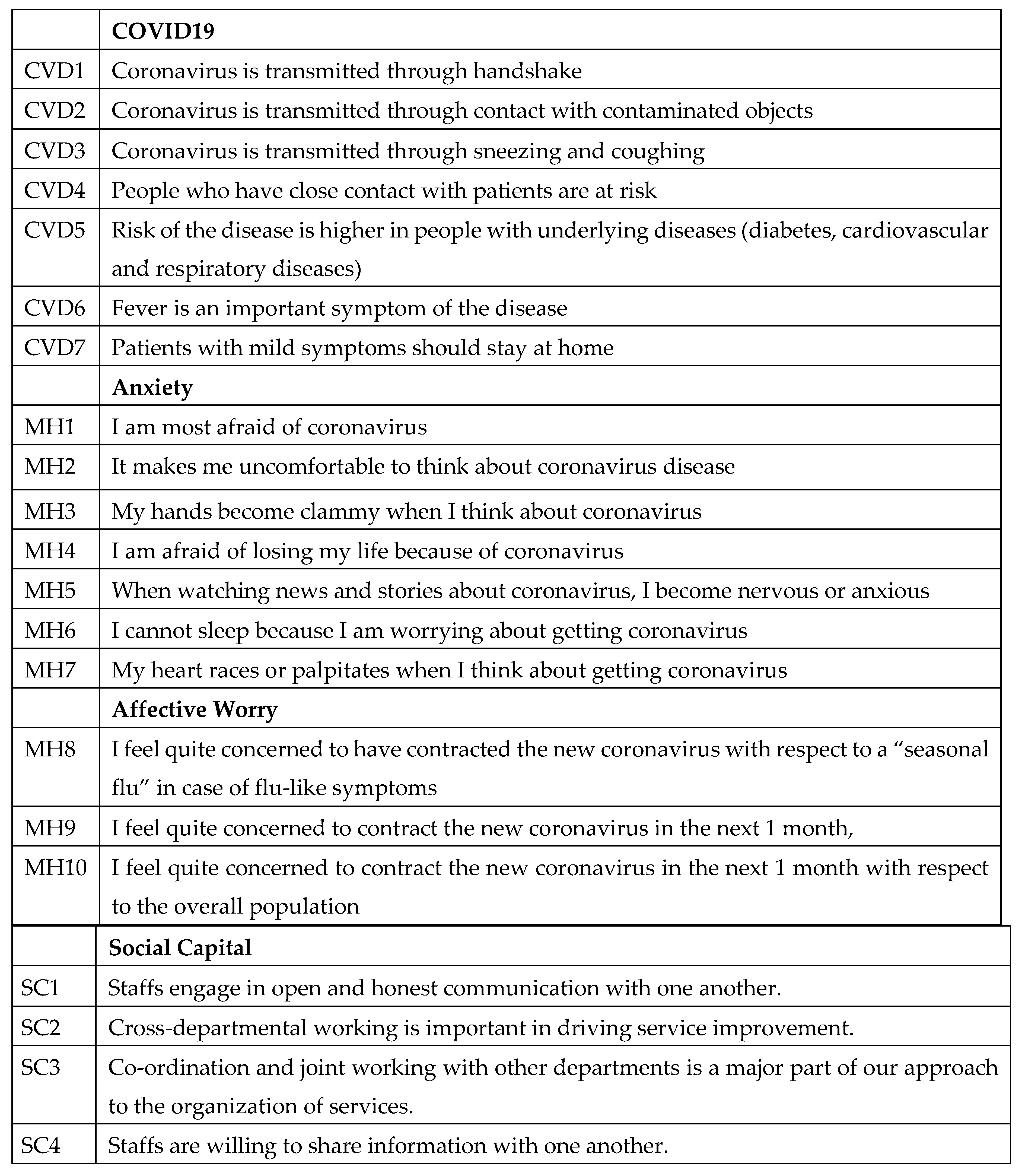
The questionnaire comprised several items designed to assess attitudes towards Covid19, anxiety related to the virus, affective worry, and social capital within the workplace. These items were derived from a combination of published scales and items specifically developed for this study to capture the unique context of the Covid19 pandemic and its impact on employees in Ghana.
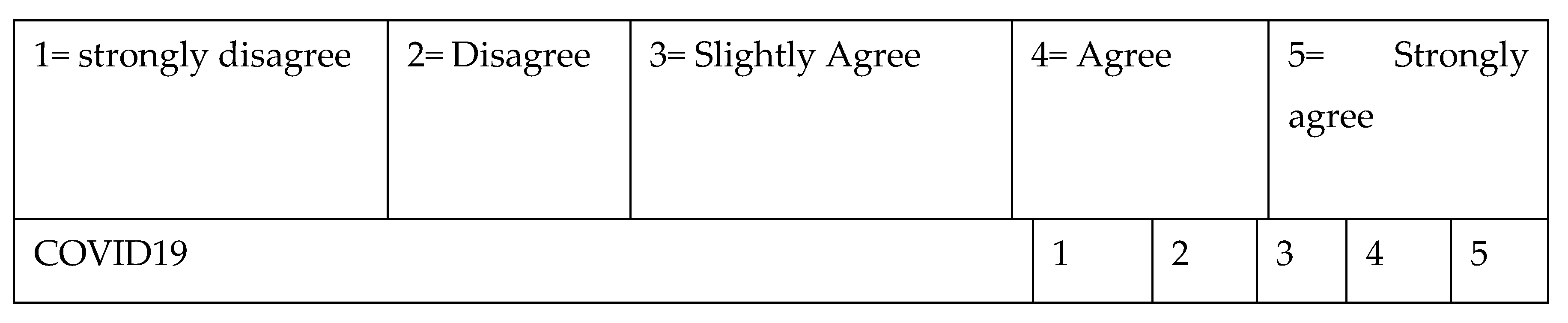
Covid19 Knowledge and Perceptions
Items CVD1 through CVD7 focused on knowledge and perceptions of Covid19 transmission, risk factors, and symptoms. These items were adapted from the World Health Organization (WHO) guidelines on Covid19 (WHO, 2020) to ensure accuracy and relevance. The inclusion of these items aimed to assess participants' understanding of the virus, which is crucial for analyzing the relationship between knowledge levels and anxiety or worry about the disease.
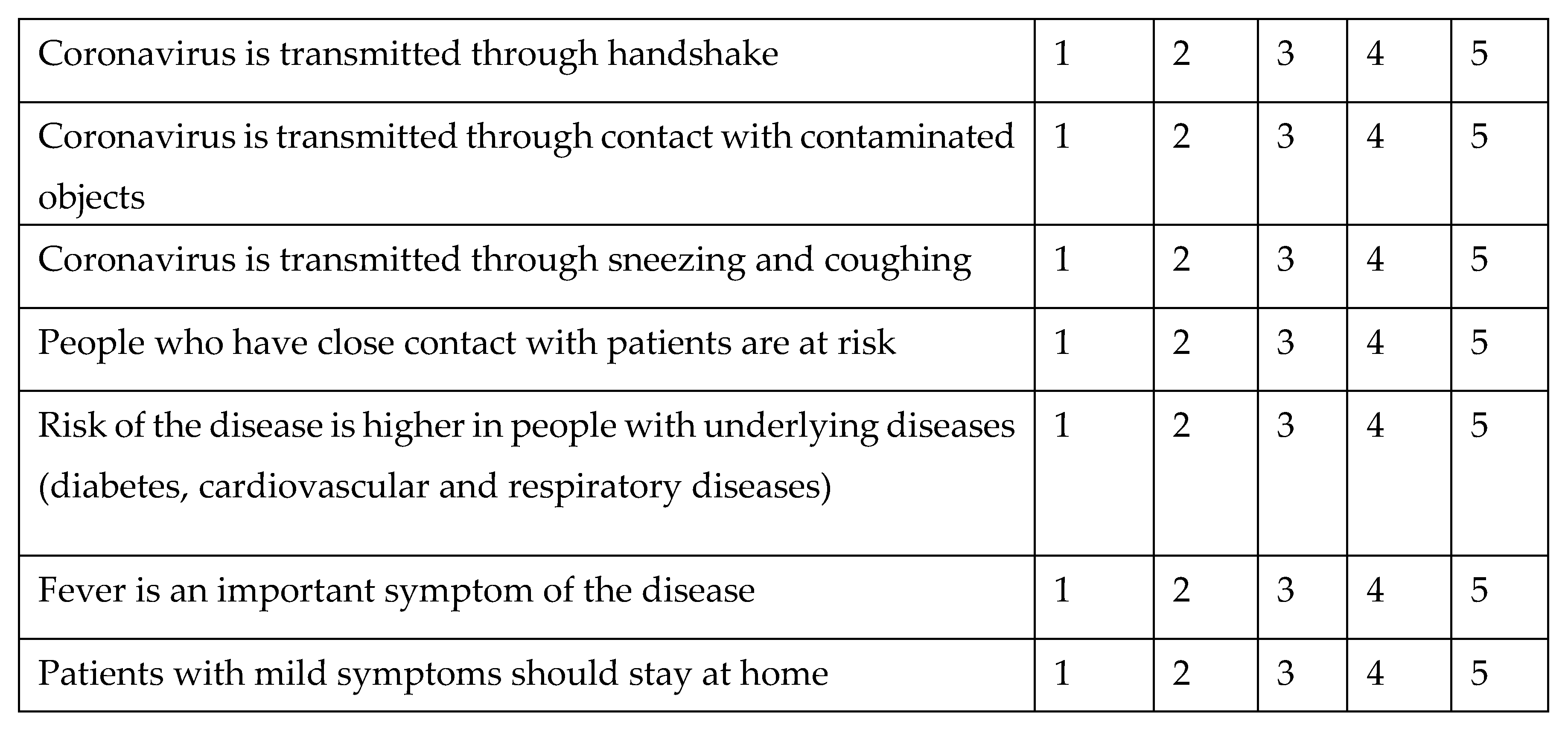
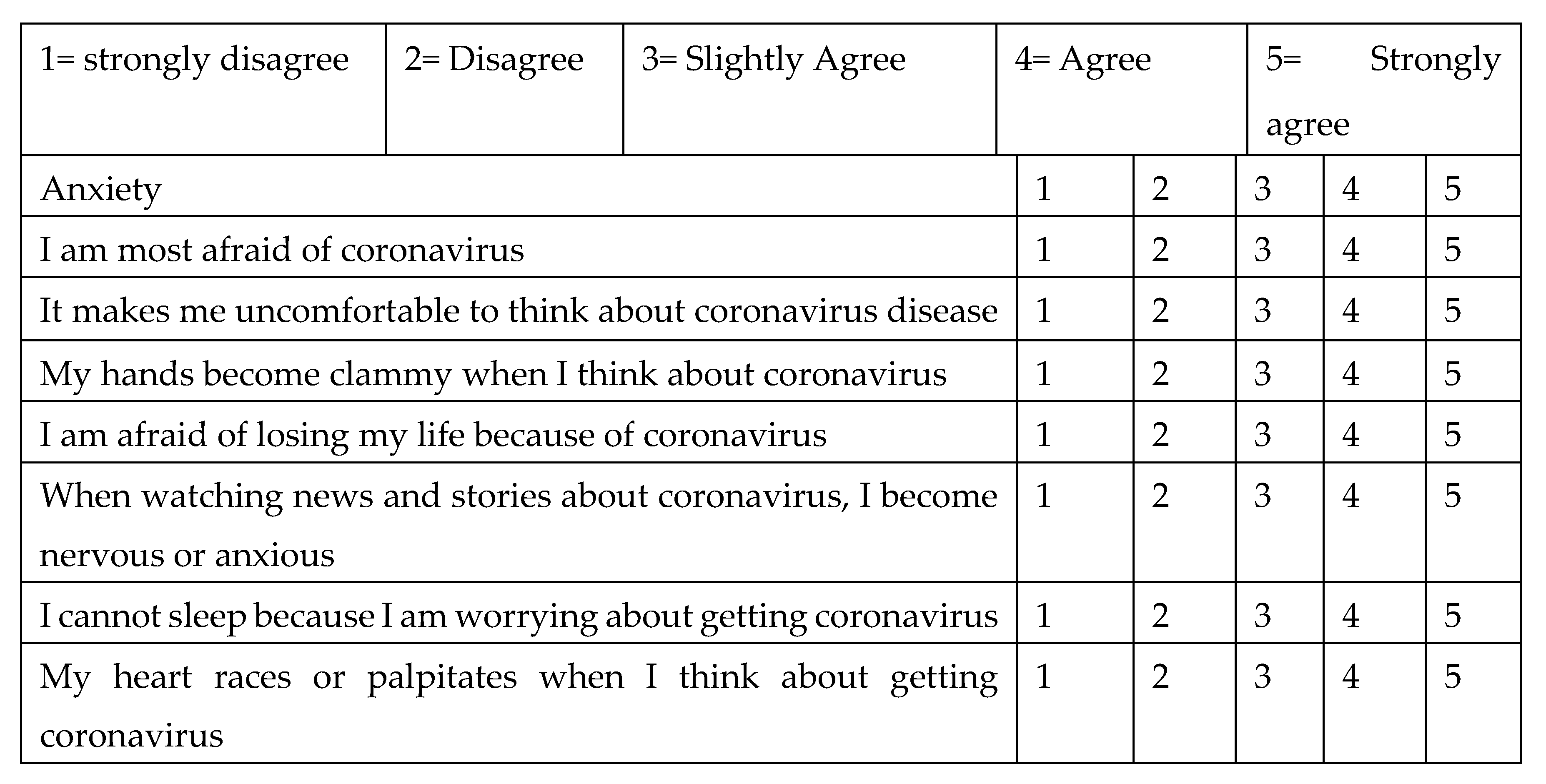
Anxiety
Items MH1 through MH7 were designed to measure anxiety specifically related to Covid19. These items were inspired by the Generalized Anxiety Disorder (GAD-7) scale (Spitzer et al., 2006), a widely used and validated tool for assessing generalized anxiety symptoms. The adaptation focused on tailoring the items to reflect fears and concerns specific to the Covid19 pandemic, thereby capturing the unique psychological impact of the crisis.
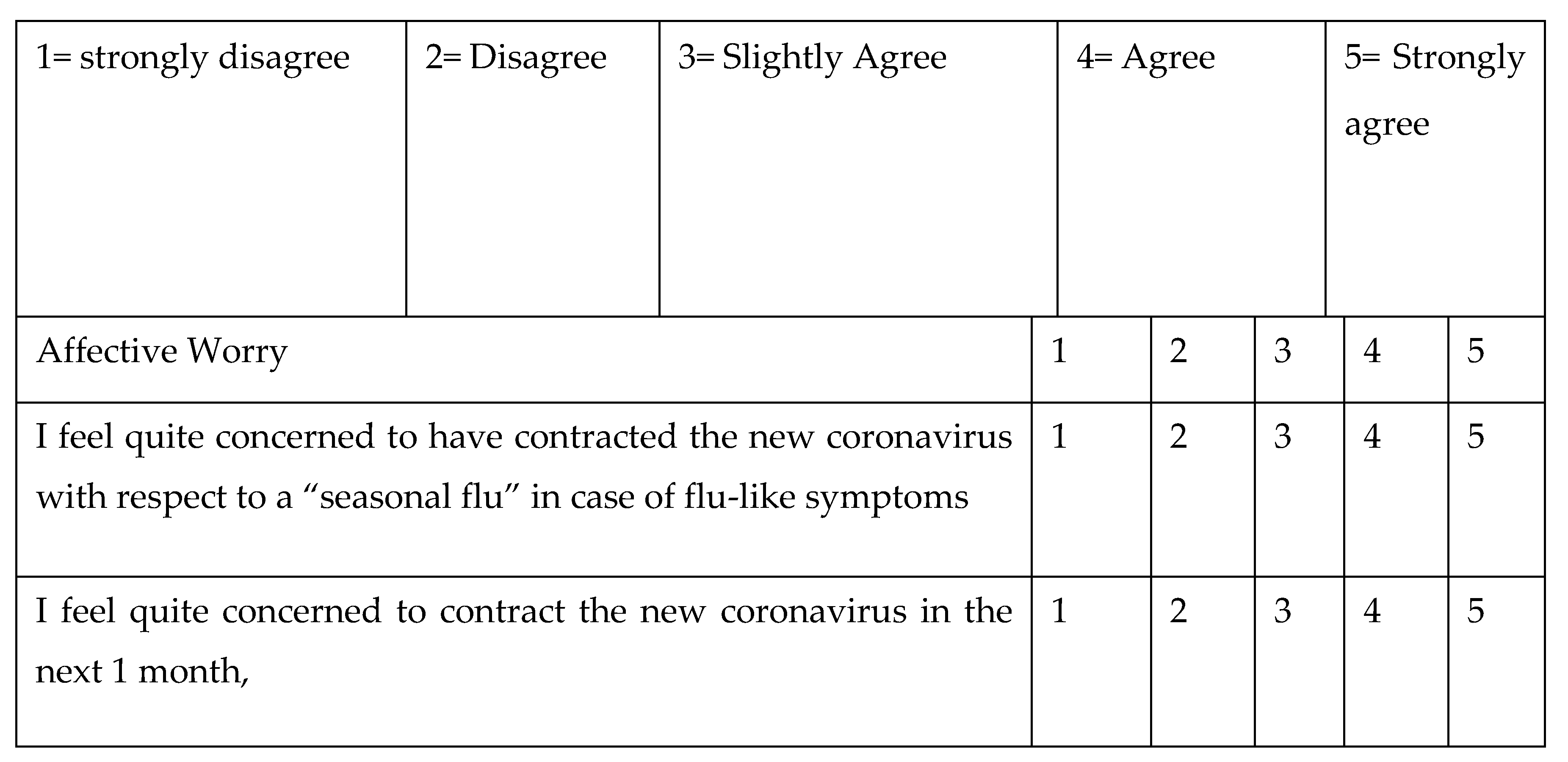
Affective Worry
Items MH8 through MH10 assessed affective worry about contracting Covid19, comparing it to seasonal flu and considering the perceived risk over the next month. These items were developed for this study to specifically address the unique and evolving nature of Covid19-related worry among the population. The aim was to distinguish between general anxiety and the more specific worry related to the pandemic's immediate health implications.
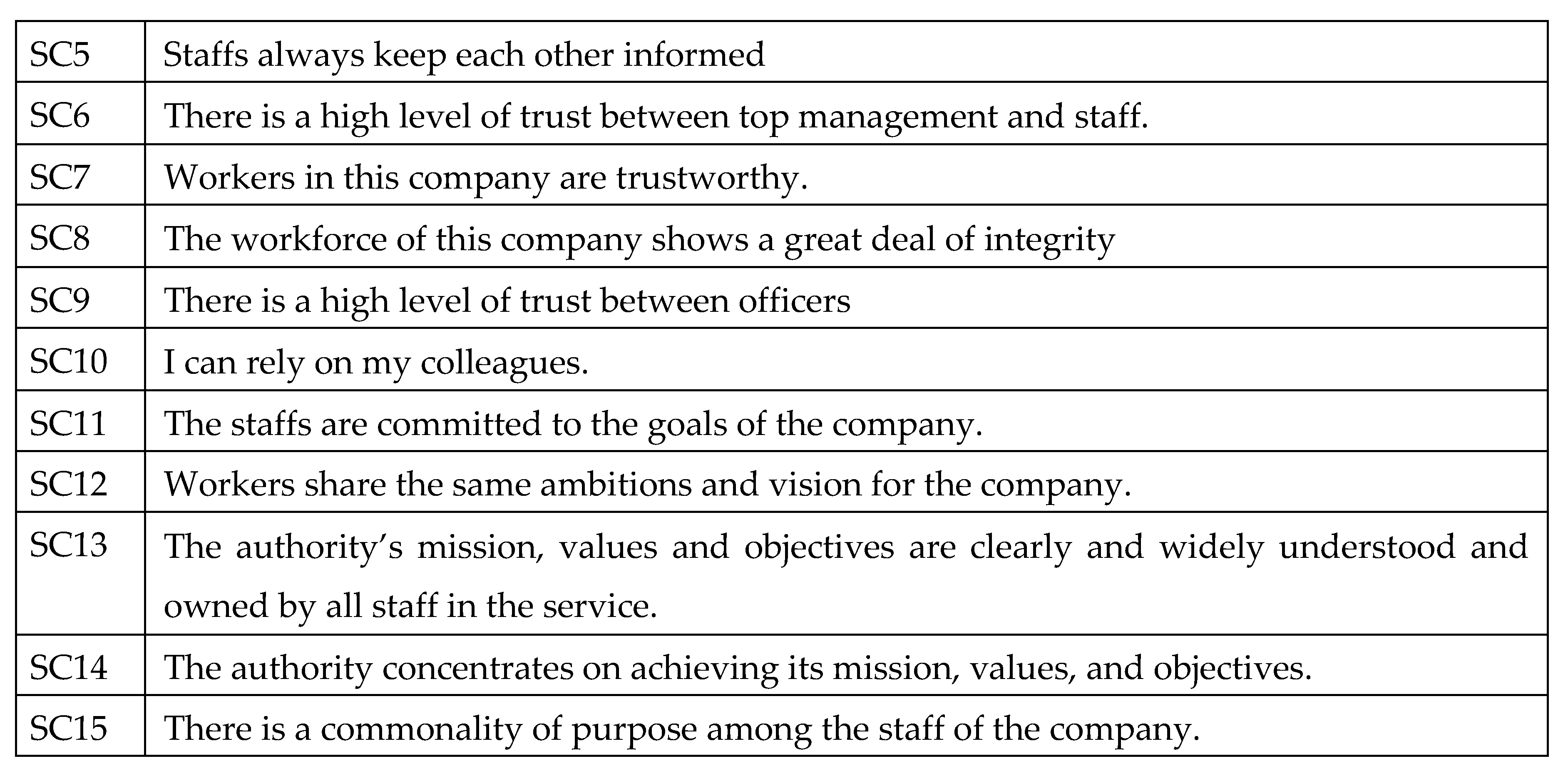
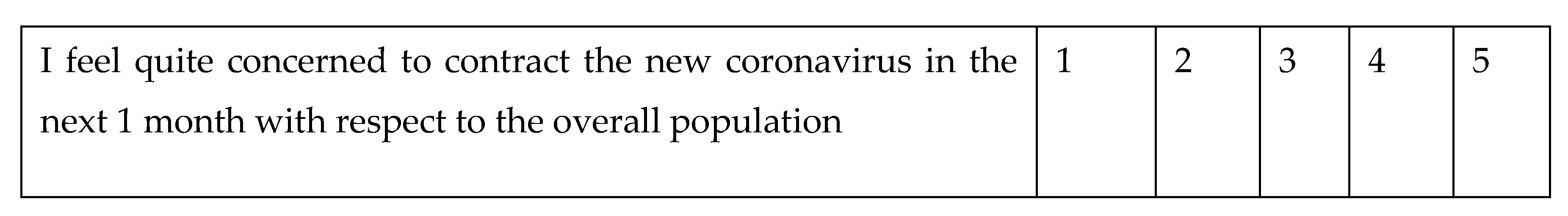
Social Capital
Items SC1 through SC15 measured various dimensions of social capital within the workplace, including communication, trust, and shared goals among staff. These items were adapted from the Social Capital Assessment Tool (SOCAT) developed by the World Bank (Grootaert et al., 2004), which provides a comprehensive framework for evaluating social capital in different contexts. The adaptation process involved tailoring the items to reflect the organizational setting and the specific challenges posed by the Covid19 pandemic.
While some previous studies have measured social capital using a single indicator, we argue that such an approach is insufficient to capture the multifaceted nature of social capital. Single-indicator measures often fail to account for the complex interplay of various dimensions such as trust, reciprocity, and social networks (Bourdieu, 1986; Putnam, 2000). Therefore, our study employed a multi-dimensional scale to ensure a more comprehensive and accurate assessment of social capital.
Analytical Approach
To analyze the collected data, the research employed Partial Least Squares-based Structural Equation Modelling (PLS-SEM). This advanced statistical technique was chosen for its ability to handle complex relationships between multiple variables. Partial Least Squares Structural Equation Modeling (PLS-SEM) was selected as the primary analytical method for several reasons, aligning with the study's objectives and the nature of the data collected. PLS-SEM is particularly suited for exploratory research where the primary goal is theory building and the prediction of key constructs (Hair et al., 2021). This method is advantageous in complex models involving latent variables, such as social capital and mental health, where the relationships are not strictly linear and may involve multiple mediator and moderator variables (Ringle et al., 2020).
One of the critical reasons for choosing PLS-SEM over Social network analysis (SNA) is the study's focus on the impact of perceived social capital on individual outcomes rather than the structural properties of social networks themselves. While SNA provides a powerful tool for analyzing the structure and dynamics of social networks, PLS-SEM allows for a more nuanced understanding of how perceptions of social capital influence mental health and behavior in the context of a public health crisis (Sarstedt et al., 2014).
Data Quality Measures
To ensure the integrity and reliability of the collected data, we implemented several rigorous data quality measures. Firstly, we conducted thorough data cleaning to identify and remove incomplete or inconsistent responses. This process involved checking for missing data, logical inconsistencies, and outlier values that could potentially skew the results.
Additionally, we employed specific techniques to detect and exclude responses generated by bots or other automated systems. To achieve this, we embedded attention-check questions within the survey. These questions were designed to verify that respondents were carefully reading and responding to the survey items. For instance, we included simple verification questions such as “Please select ‘Strongly Agree’ for this item,” which allowed us to flag inattentive respondents who failed to follow these instructions.
As a result of these quality checks, we excluded 28 responses that did not meet our criteria for valid data. This process ensured that our final sample consisted of 422 participants out of the initial 450, all of whom provided reliable and consistent responses, thereby enhancing the overall quality and robustness of our research findings.
Validity and Reliability
Confirmatory Factor Analysis
To assess the validity and reliability of our measurement instruments, we conducted a Confirmatory Factor Analysis (CFA). CFA was employed to test the hypothesized factor structure and to confirm that the observed data fit the theoretical model. The following benchmarks for model fitness and reliability measures were adhered to, based on established guidelines in the literature.
Model Fitness
The overall model fitness was evaluated using several fit indices. The chi-square statistic (X²), degrees of freedom (df), and the ratio of chi-square to degrees of freedom (X²/df) were calculated. A ratio of less than 3 is generally considered indicative of a good fit (Kline, 2015). The Root Mean Square Error of Approximation (RMSEA), Standardized Root Mean Square Residual (RMR), Goodness of Fit Index (GFI), and Comparative Fit Index (CFI) were also reported. Acceptable thresholds for these indices are RMSEA < 0.06, RMR < 0.08, GFI > 0.90, and CFI > 0.95 (Hu & Bentler, 1999).
Reliability
The internal consistency reliability of the scales was assessed using Cronbach's alpha coefficients. A Cronbach’s alpha value of 0.70 or higher is considered acceptable for demonstrating internal consistency (Nunnally & Bernstein, 1994). The reliability analysis for our constructs yielded the following Cronbach's alpha values
Results
Demographic Characteristics of Respondents
The
Table 1 below demonstrates the demographic distribution of these respondents. The results suggest that the age distribution of the respondents varied across different age groups. The majority of the respondents fell within the age range of 21-25 years, accounting for 18.0% of the total. This was closely followed by the 31-35 years age group, which represented 17.8% of the respondents. The 26-30 years and 36-40 years age groups had similar representations, with 12.3% and 16.4% respectively. Respondents aged between 41-45 years made up 15.4% of the sample. The least represented age groups were 46-50 years (7.1%), 51-55 years (4.5%), and those aged 56 and above, which accounted for 8.5% of the total respondents.
The gender distribution showed a significant disparity between male and female respondents. Females made up the majority, representing 70.9% of the total respondents, while males accounted for 29.1%. When it comes to the industry of employment, the health sector had the highest representation with 41.5% of the respondents working in this industry. This was followed by the manufacturing sector at 28.7%. The service industry accounted for 21.1% of the respondents, and the extractive industry had the least representation with 8.8%.
Regarding the history of Covid19 among the respondents, 34.1% indicated that they had contracted the virus at some point, while a majority of 65.9% stated they had not. In terms of marital status, the majority of the respondents (64.0%) identified as single, while 36.0% indicated they were married. When asked about their level of concern regarding Covid19, a significant portion of the respondents (49.8%) stated that they were often concerned about the virus. 42.2% mentioned they were sometimes concerned, while a minority of 8.1% said they hardly ever felt concerned about Covid19.
Descriptive Statistics
The study's descriptive statistics for 422 participants reveal insights into Covid19 knowledge, mental health, and social capital. Participants showed a moderately high understanding of Covid19 (mean=3.7786), suggesting a good grasp of its transmission and prevention, crucial for effective public health responses. Mental health scores indicated moderate distress (mean=2.75), with consistent experiences across the sample, highlighting the pandemic's significant but uniform impact on mental well-being and the need for targeted interventions. Social capital was perceived positively (mean=3.4735), despite some variability, indicating supportive workplace environments with strong networks and trust. This variability in social capital experiences might be influenced by departmental roles or individual social networks. Overall, the findings underscore the importance of addressing mental health concerns and leveraging workplace social capital to mitigate the pandemic's negative effects.
Table 2.
Descriptive Statistics of Variables.
Table 2.
Descriptive Statistics of Variables.
| |
N |
Minimum |
Maximum |
Mean |
Std. Deviation |
| Covid19 |
422 |
1.00 |
5.00 |
3.7786 |
.88946 |
| Mental Health |
422 |
1 |
4 |
2.75 |
.684 |
| Social Capital |
422 |
1.47 |
4.73 |
3.4735 |
.65946 |
Validity and Reliability
Data is analyzed in three steps: Step 1 we performed a preliminary analysis of the scale by Exploratory Factor Analysis using the Maximum likelihood and Varimax rotation through SPSS. Step 2 consisted of further validating the factor structure which was the output of EFA sent to CFA conducted through AMOS. Step 3 was to test the hypotheses by assessing the structural model using AMOS.
Exploratory Factor analysis using the maximum likelihood method with Varimax rotation is used for analyzing the factor structure and correlation between items included in the scale. The KMO values for all the variables are above 0.50 so it indicates that criteria of sampling adequacy is met. The Bartlett test of Sphericity is statistically significant (P<.05) so it shows that our correlation matrix is statistically different from an identity matrix as desired.
The results of the exploratory factor analysis show that the solution is based on 2 factors as expected and all items are loading on their own factors. The results of the exploratory factor analysis show that our factors have good level of validity. For further validation, we used the confirmatory factor analysis (CFA) which is discussed next.
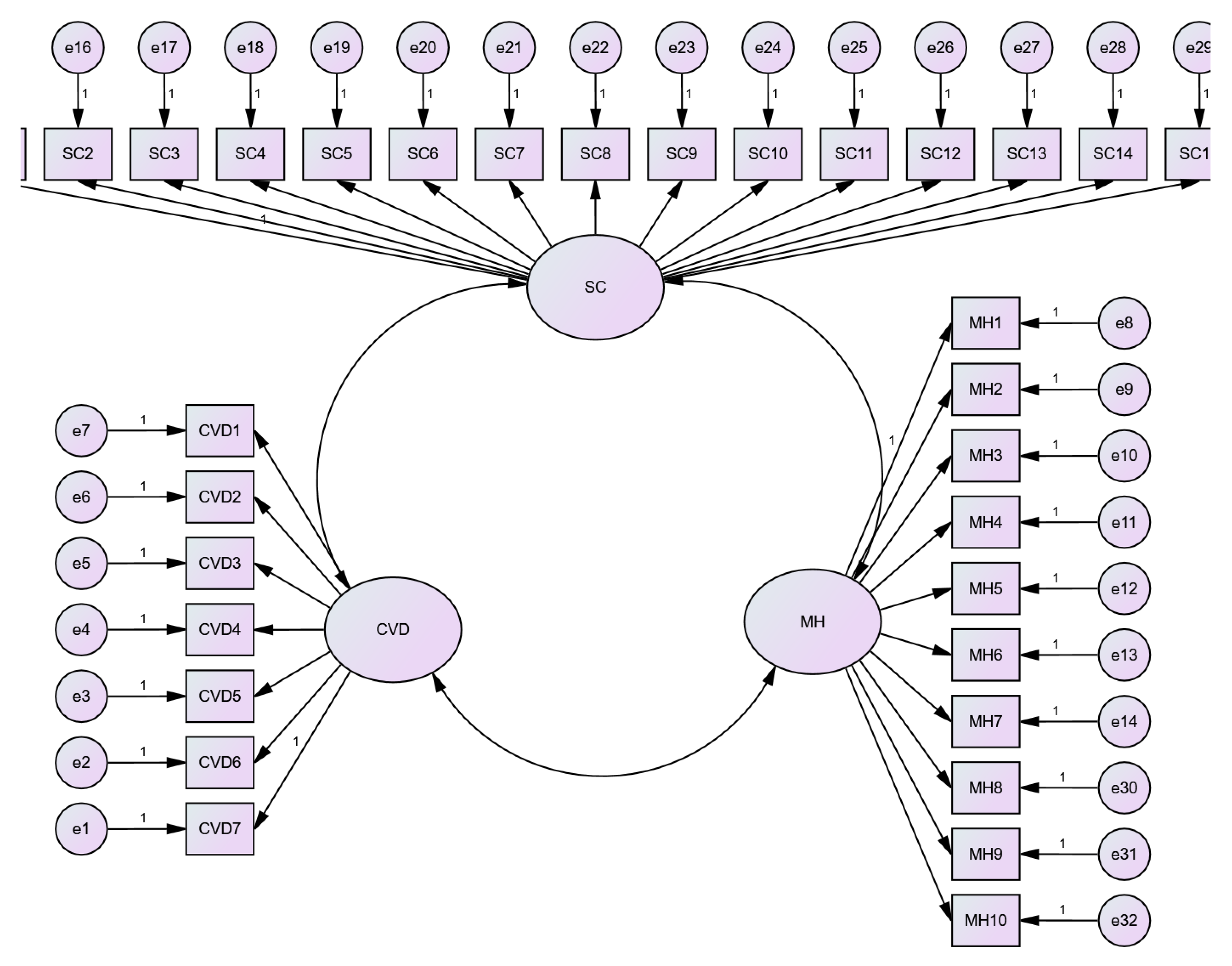
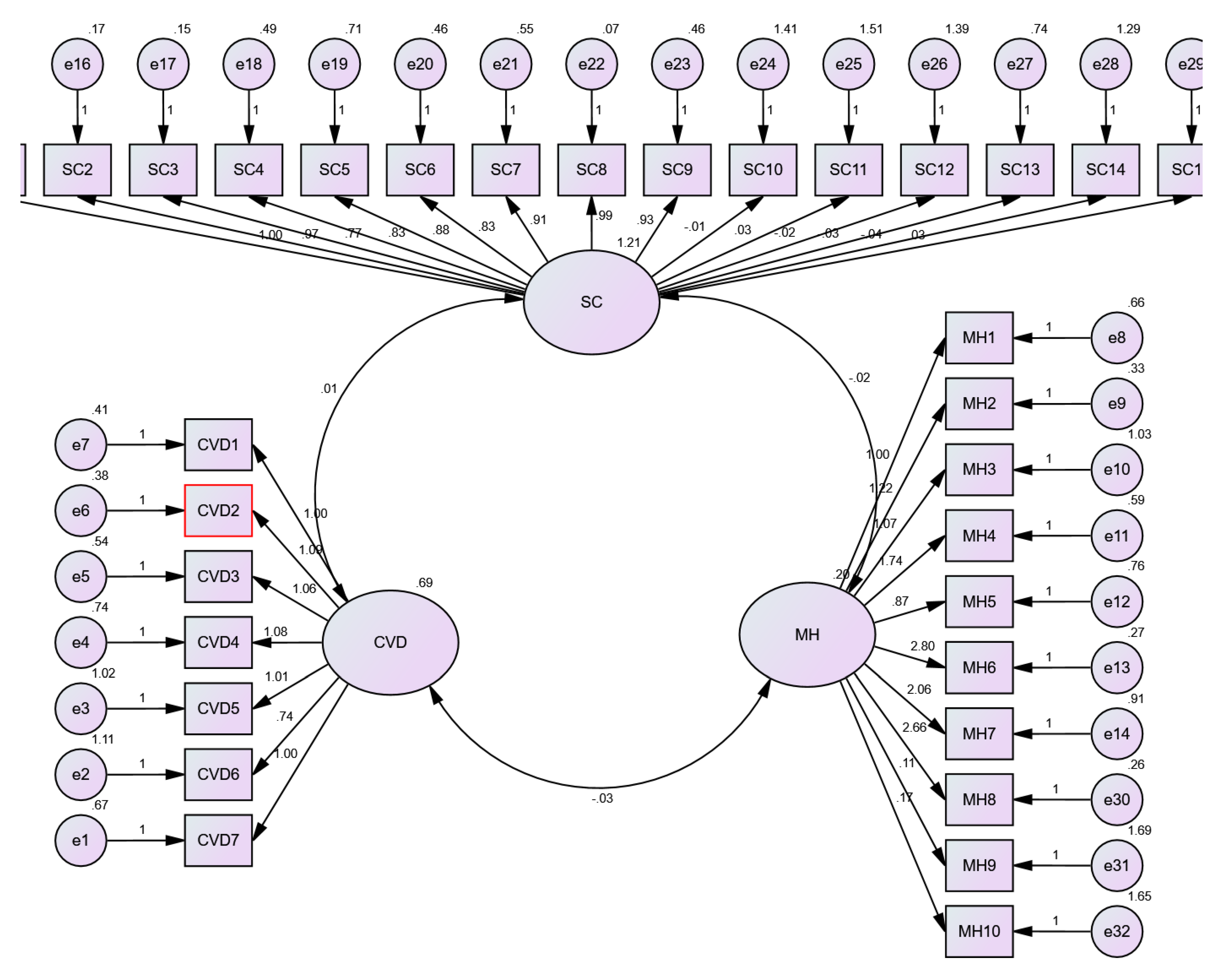
Confirmatory Factor Analysis
The AMOS version 18 is used for performing the Confirmatory Factor Analysis. The model is assessed for testing the reliability, convergent validity, and discriminant validity. The final calculated model followed by results in the
Table 2.
Table 3.
Results of validity and reliability.
Table 3.
Results of validity and reliability.
| Variables |
Measurements |
Factor Loading |
Cronbach’s Alpha |
KMO |
Variance Explained |
| Covid19 |
CVD1 |
.690 |
.872 |
.732 |
72.628 |
| CVD2 |
.712 |
| CVD3 |
.837 |
| CVD4 |
.695 |
| CVD5 |
.674 |
| CVD6 |
.834 |
| CVD7 |
.641 |
| Mental Health |
MH1 |
.340 |
.793 |
.543 |
72.196 |
| MH2 |
.576 |
| MH3 |
.697 |
| MH4 |
.639 |
| MH5 |
.698 |
| MH6 |
.829 |
| MH7 |
.749 |
| MH8 |
.896 |
| MH9 |
.902 |
| MH10 |
.895 |
| Social Capital |
SC1 |
.792 |
.855 |
.843 |
76.464 |
| SC2 |
.860 |
| SC3 |
.864 |
| SC4 |
.693 |
| SC5 |
.607 |
| SC6 |
.727 |
| SC7 |
.689 |
| SC8 |
.917 |
| SC9 |
.719 |
| SC10 |
.739 |
| SC11 |
.801 |
| SC12 |
.834 |
| SC13 |
.792 |
| SC14 |
.671 |
| SC15 |
.766 |
|
Model Fitness: X2=917.384, df=416, X2/df= 2.205, RMSEA=.054, RMR=.034, GFI=.813, CFI=.956 |
The result of CFA shows that model had good fit statistics including x2/df=2.205, RMSEA of 0.054, RMR of 0.034, and CFI of .956. The recommended values are provided in the bracket based on the guidelines of Hu and Bentler (1999) and Browne and Cudeck (1992) (RMSEA<.08, RMR<.05, CFI>.90). All items standardized factor loading was above 0.60 and it is an indication of good convergent validity (Hair, Sarstedt, Ringle, & Gudergan, 2017). Another evidence of convergent validity is that Maximum Shared Variance is less than respective Average Variance Extracted for all variables. The Cronbach alpha and composite reliability for all variables are above 0.70 so it shows that our variables had good reliability.
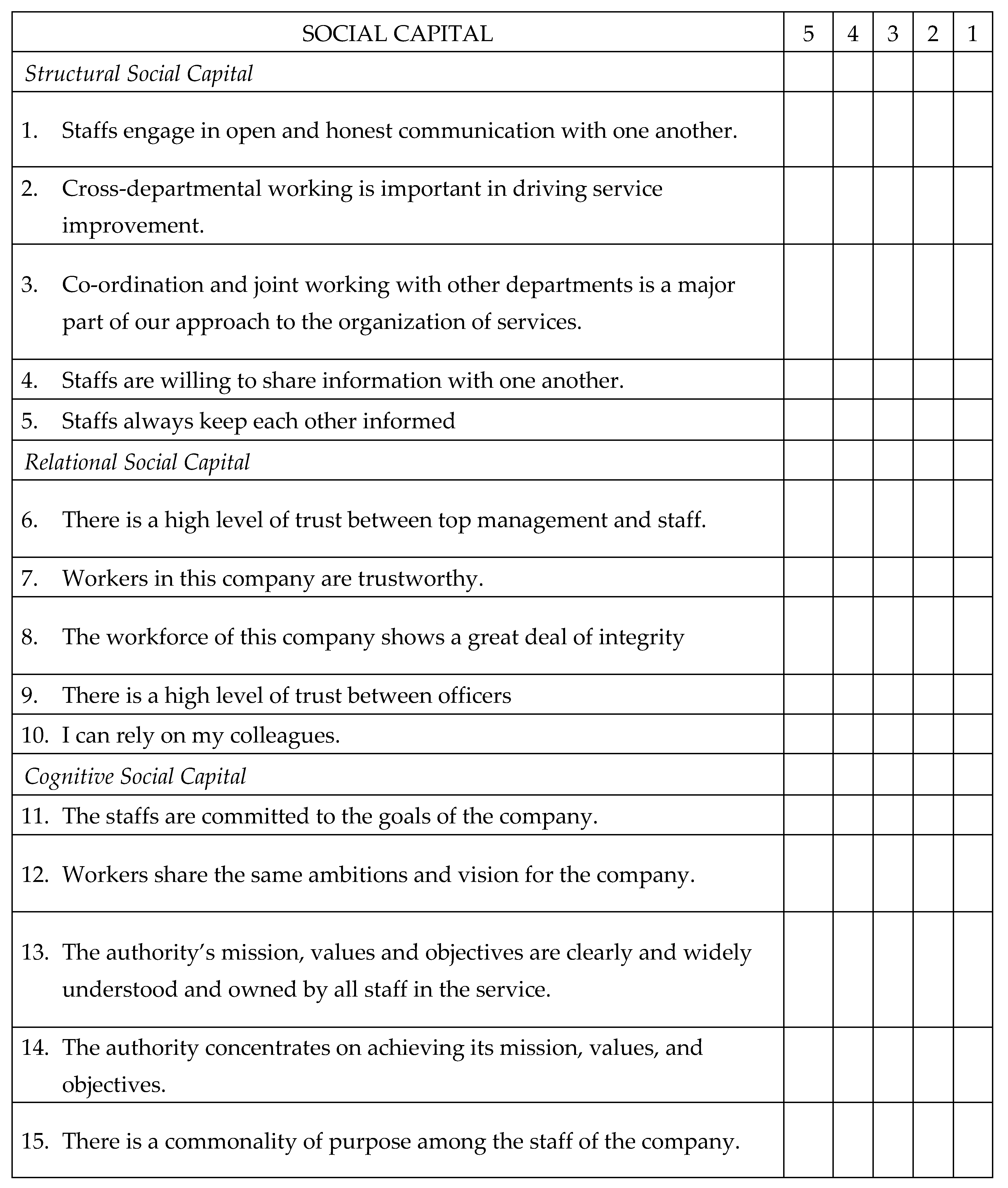
Hypotheses Testing
To examine the relationship between Covid19, social capital and mental health of employees, we used the structural equation modelling using the AMOS path analysis by imputing the Factor Score from CFA using AMOS. As part of hypotheses testing, we tested the social capital as a moderator. The
Table 4 shows that, the hypotheses resulting based on path analysis shows that the Covid19 pandemic is negatively and significantly associated with mental health of employees in Ghana (β=-.066, P<.05). Social capital is positively and significantly associated with mental health of employees in Ghana (β=.079, P<.05). Based on these results, we accept the H1 and H2.
Moderation Effect Results
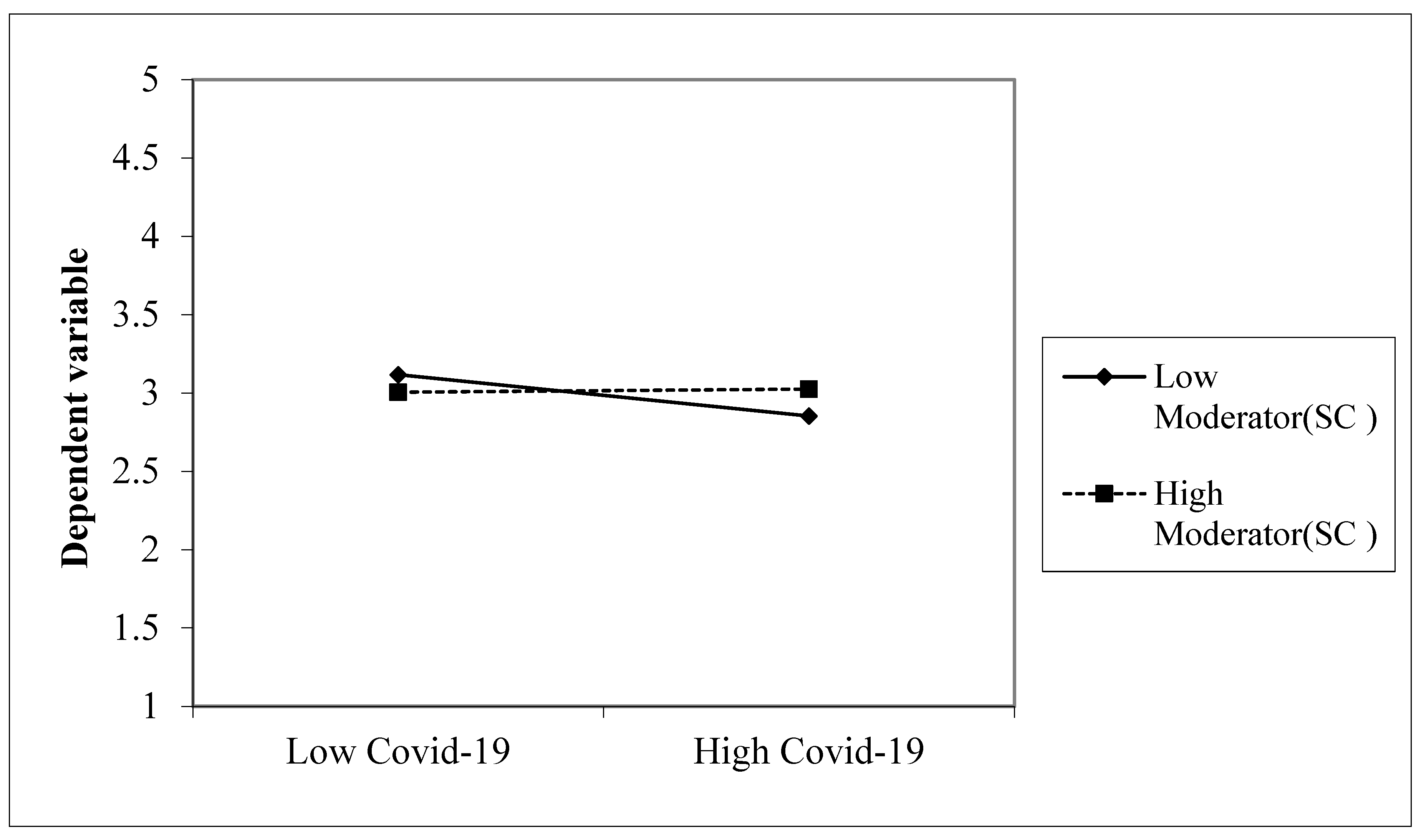
The moderation analysis is conducted by treating Covid19 as independent variable, Mental Health as dependent variable, and Social Capital as moderator variable. The results from
Table 5 demonstrate that the interaction term (CVD∗SC) represents the moderation effect of Social Capital on the relationship between Covid19 and Mental Health. The standardized coefficient for this interaction is 0.015, indicating a positive moderation effect. This suggests that the negative impact of Covid19 on mental health is somewhat mitigated or reduced in the presence of higher social capital. This moderation effect is statistically significant at the 0.05 level (2-tailed), providing evidence that social capital plays a role in influencing the relationship between Covid19 and mental health, therefore, we accept the third hypothesis
Figure 2.
Social Capital as moderator in the relationship between Covid19 and Mental Health.
Figure 2.
Social Capital as moderator in the relationship between Covid19 and Mental Health.
Discussions
The results of the study support the first hypothesis of the study “Covid19 Pandemic negatively predicts mental health of employees”. These findings, align with findings from Del-Aguila-Arcentales et al. (2022) that detail mental health declines, including PTSD, due to the pandemic. Similarly, Şimşir et al. (2021) found a strong association between Covid19 fear and mental health issues like anxiety and traumatic stress, underscoring the pandemic's significant mental health impact. Russell et al. (2020) highlighted how Covid19 affects family dynamics by increasing caregiver burdens and children's stress. Rathakrishnan et al. (2022) added that while fear related to the pandemic worsens mental health, spirituality may offer some protection. This body of research collectively emphasizes the pandemic's detrimental effects on mental health, though factors like spirituality may provide resilience.
The results also support the second hypothesis of the study “Social Capital positively predicts the mental health of employees”. The study's finding that social capital positively impacts mental health is echoed across various studies. Bakhshi et al. (2021) demonstrated significant links between social capital dimensions like trust, social activity, and life value with better mental health among HIV patients, highlighting social capital's role in enhancing mental well-being in vulnerable groups. Similarly, Anwar et al. (2020) found that social networks, cohesion, and trust within social capital significantly improve mental health outcomes in older adults, underscoring its protective effect. Amin et al. (2018) showed that social capital boosts life quality and mental health in Malaysia's lower-income B40 group, suggesting its buffering role against mental health challenges in economically disadvantaged populations. Moeini et al. (2020) hinted at a positive link between social capital and mental health among health workers, although details were limited. Collectively, these studies affirm the beneficial influence of social capital on mental health across diverse groups and settings.
The study further demonstrated that Social capital moderates the relationship between Covid19 Pandemic and Mental Health of Employees which supported the third hypothesis. The current study's observation that social capital moderates the impact of Covid19 on mental health is supported by related research. Gong et al. (2022) explored how resilience and social support mitigate the mental health effects of Covid19 restrictions among college students, emphasizing the role of social capital-like factors in countering pandemic-related stress. Zhuo et al. (2021) found that social support buffers the mental health impacts of Covid19 uncertainties, suggesting that enhanced social support can reduce pandemic-induced mental health issues. Snel et al. (2022) confirmed the protective role of social capital against the mental health effects of the pandemic, directly aligning with the study's findings on social capital's moderation effect. Additionally, Adelinejad et al. (2022) highlighted resilience as a mediator between social capital and mental health during the pandemic, indicating that fostering social capital and resilience can help navigate pandemic-related psychological challenges. Collectively, these studies affirm the crucial role of social capital and associated factors like social support and resilience in alleviating the mental health challenges posed by Covid19.
Conclusions
This study embarked on an exploratory journey to unravel the intricate dynamics between Covid19, social capital, and the mental health of employees in Ghana, employing structural equation modeling (SEM) via AMOS path analysis. The empirical evidence gleaned from this rigorous analytical process has illuminated the significant roles both Covid19 and social capital play in shaping mental health outcomes among the workforce.
The findings demonstrate that the Covid19 pandemic exerts a negative influence on employees' mental health, as indicated by a statistically significant negative association. This result corroborates the intuitive understanding that pandemics, by their very nature, exacerbate stressors, thereby detrimentally impacting mental well-being. The psychological strain attributed to the pandemic could stem from a myriad of factors, including fear of infection, economic uncertainties, and the profound disruptions to daily life and work routines.
Conversely, social capital emerges as a beacon of resilience, showcasing a positive and significant association with mental health. This pivotal finding underscores the protective buffer social capital provides against mental health deterioration. In essence, the networks of relationships, trust, and mutual support that constitute social capital are instrumental in fostering a sense of belonging, reducing feelings of isolation, and enabling access to emotional and informational support during crises. Such resources are invaluable in navigating the tumultuous waters of a pandemic, highlighting the critical importance of nurturing social capital within workplaces.
The moderation analysis further enriches our understanding by revealing that social capital not only directly benefits mental health but also plays a moderating role in the relationship between Covid19 and mental health. The positive moderation effect (β=.015, P<.05) suggests that the adverse impact of Covid19 on mental health is attenuated in the presence of higher levels of social capital. This finding is a testament to the power of social capital in mitigating the psychological fallout from the pandemic, offering a glimmer of hope amidst the prevailing gloom.
In conclusion, this study contributes to the burgeoning body of literature on the psychological impacts of pandemics by highlighting the dual forces of Covid19 and social capital in shaping mental health outcomes. The evidence presented herein not only validates the hypotheses posited but also underscores the nuanced interplay between these variables. As the world grapples with the ramifications of Covid19 and future pandemics, the insights gleaned from this research underscore the imperative of bolstering social capital as a strategic lever to safeguard mental health. Policymakers, employers, and public health practitioners are thus called upon to recognize and harness the potential of social capital in fortifying the mental resilience of populations, particularly in regions with limited resources like Ghana. This study paves the way for further research into the mechanisms through which social capital can be cultivated and mobilized to combat the mental health challenges posed by global health crises.
Practical Implications
The speed with which the Covid19 problem has extended to numerous nations and had an effect on the global economy is unprecedented. In terms of knowledge, tools, and expertise, not every business is prepared to deal with this epidemic. In order to keep operations running smoothly and keep employees safe, managers and HR professionals will need to be creative. This report is useful for its insight into the primary stresses faced by organizations during Covid19 and those that may persist after the event has ended. There's also details on the primary moderators that might soften or harden the blow on workers' psyches from the Covid19. The paper's authors hope that the following suggestions will be useful to managers and human resource practitioners as they devise an intervention strategy for the period during and after Covid19, preserve an effective and swift continuous line of communication with their staff members, including supervisors, and continue their collaboration with health and state officials.
During pandemics, people, groups, and governments should all work to strengthen their social networks. Physical separation and other preventative measures are more likely to be maintained and more effective when supported by high levels of social capital. In light of the protracted nature of this crisis, with no clear end in sight, the long-term viability of response and recovery activities is of utmost importance, and, if history is any guide, this will depend in large part on social capital. Our collective reaction to Covid19 will rely heavily on our relationships with one another, whether they be with members of our personal households, members of our local communities, or with Ghanaians from all walks of life.
At the end of the day, we need to take the lessons we have learned from this crisis and use them to get ourselves ready for the next one. Research on the effects of Covid19 on social capital and the role of social capital in dealing with Covid19 is essential. The lessons obtained during Covid19 must be incorporated into the disaster response cycle, much as the crucial knowledge gleaned from prior epidemic and pandemic scenarios is used today. Future pandemics are not a matter of if, but when they will occur. In times of crisis, it will be helpful to have a deeper knowledge of how to use digital communication technologies to establish and sustain social capital amid social isolation. The moment to prepare is not when the levee breaches, but rather before the water begins to rise, as this catastrophe and many others before it have demonstrated.
Implications for Health Behavior Research
Health behavior research delves into understanding the myriad factors that influence individuals' health-related decisions and actions. These behaviors, ranging from dietary choices to exercise habits, play a pivotal role in determining overall health outcomes. As the global health landscape evolves, with challenges like the Covid19 pandemic emerging, it becomes imperative to examine the broader implications of these behaviors. Factors such as social capital, workplace dynamics, and cultural contexts can significantly moderate health behaviors. By critically analyzing these implications, researchers, policymakers, and health professionals can better design interventions, promote positive health behaviors, and ultimately improve public health outcomes
A key takeaway from this study is the vital importance of comprehending health behaviors within specific socio-cultural and geographical contexts. Ghana, like many other nations faced with the challenges of the Covid19 pandemic, encountered unique obstacles. By specifically focusing on Ghanaian employees, this research provides valuable insights into how local factors influence health behaviors and mental well-being, underscoring the necessity for interventions tailored to the specific context.
One particularly noteworthy finding in this study is the moderating role of social capital in the relationship between the pandemic and mental health. This highlights the significant influence of social networks, relationships, and community ties on health behaviors. Future research can delve even deeper into understanding the various dimensions of social capital and how they can be strategically utilized to promote positive health behaviors.
This study brings to light the workplace as a critical setting for health behavior research. As employees spend a substantial amount of their time at work, it becomes crucial to understand the intricacies of the workplace, including interpersonal relationships and organizational culture, in order to design effective health interventions.
Although this study primarily focuses on Ghana, its findings have far-reaching implications for global health. The protective nature of social capital against adverse mental health outcomes during a crisis can serve as a focal point for health interventions on a worldwide scale. Policymakers and health professionals can derive valuable insights from this research to develop strategies that foster social capital, especially in regions with limited resources.
When conducting research on sensitive subjects such as mental health during a global crisis, it is imperative to approach it with ethical rigor. Future studies can build upon the methodologies utilized in this research, ensuring that the well-being and privacy of participants are prioritized.
In conclusion, this study offers invaluable insights into the intricate relationship between the Covid19 pandemic, mental health, and social capital. Its findings have profound implications for research on health behavior, emphasizing the necessity for context-specific, ethically sound, and holistic approaches to understanding and promoting positive health behaviors
Limitations and Future Work
First of all, the capacity to make causal inferences among the Covid19 Pandemic, Social Capital, and employees' mental health state is limited, as is inherent in any cross-sectional study. We cannot be sure that we have accounted for all confounding factors or establish the direction of the relationship between the Covid19 Pandemic, Social Capital, and the mental health state of employees in Ghana, despite our best efforts. For example, it is reasonable to assume that people with depression will have a more pessimistic outlook on their surroundings, including their social capital, due to their low mood and the cognitive biases that accompany it. Furthermore, the study was cross sectional, therefore future studies can be longitudinal research on the correlation between the Covid19 pandemic, workers' social capital, and their mental health. In addition, we did not evaluate social capital in any context other from the workplace. This is because, the workplace is a primary environment where adults spend a significant portion of their time, and it plays a pivotal role in shaping interpersonal relationships and networks. By focusing on the workplace, we aimed to gain insights into how professional networks and relationships influence mental health, especially during challenging times like the Covid19 pandemic. Secondly, the dynamics of social capital in the workplace are distinct from other contexts, such as family, community, or recreational settings. The professional environment often involves a mix of competitive and collaborative interactions, hierarchical structures, and formalized roles, all of which can uniquely influence the formation and benefits of social capital.
Appendix A
Operationalization of Variables
Mental Health
Mental health in this study was operationalized through a multi-dimensional approach, focusing on symptoms of anxiety, depression, and stress as primary indicators. These dimensions were chosen based on their relevance to the psychological impact of the Covid19 pandemic, as identified in existing literature (e.g., Spitzer et al., 2006; WHO, 2020). Anxiety was measured using adapted items from the Generalized Anxiety Disorder (GAD-7) scale, focusing on fears specifically related to Covid19 (e.g., fear of contracting the virus, impact on sleep). Depression and stress indicators were derived from the Patient Health Questionnaire (PHQ-9) and the Perceived Stress Scale (PSS), respectively, with modifications to contextualize questions around the pandemic's effects. Each item was rated on a Likert scale, allowing for quantitative analysis of mental health status among participants.
Social Capital
Social capital was conceptualized according to its cognitive and structural dimensions within the workplace. Cognitive social capital includes perceived trust and shared values among employees, while structural social capital refers to the extent and intensity of interpersonal networks and collaborative practices within the organization (Grootaert et al., 2004). Indicators for cognitive social capital included items measuring trust in management and colleagues, shared goals, and organizational commitment. Structural social capital was assessed through questions about cross-departmental collaboration, information sharing, and joint problem-solving activities. These measures were adapted from the Social Capital Assessment Tool (SOCAT) to fit the organizational context and the unique challenges posed by the Covid19 pandemic.
COVID19
The operationalization of Covid19 related variables focused on knowledge, perceptions, and preventive behaviors. Knowledge items assessed respondents' understanding of virus transmission modes, symptoms, and high-risk factors, based on WHO guidelines. Perceptions were measured through items evaluating the perceived severity of and susceptibility to Covid19, reflecting constructs from the Health Belief Model. Preventive behaviors were operationalized by assessing the frequency of handwashing, mask-wearing, and social distancing, as recommended by public health authorities. Each of these components was measured using a combination of yes/no questions and Likert scale ratings to quantify participants' responses.
Questionnaire Items
QUESTIONNAIRE
This data collection is part of a postgraduate research project being conducted by Master’s student of KNUST. The research topic is on the effects of COVID19 pandemic on the mental health of the elderly in Italy. Data obtained from this research is for academic purposes only and confidentiality is assured. Please indicate your response to statements by ticking the appropriate box [√]. Thank you for your cooperation and participation
SECTION A: YOUR PERSONAL DATA
Age: 21–25 Years [ ] 26–30 Years [ ] 31–35 Years [ ] 36–40 Years [ ] 41–45 Years [ ] 46–50 Years [ ] 51–55 Years [ ] 56 and Above Years [ ]
Gender: Male [ ] Female [ ]
Industry of Employment: Service [ ] Health [ ] Manufacturing [ ] Extractive [ ]
COVID History: Yes [ ] No [ ]
Marital Status: Married [ ] Single [ ] Divorced/Seprated [ ]
Concerned about COVID19: Hardly [ ] Sometimes [ ] often [ ]
This survey addresses the state of COVID19, anxiety, affective worry and protective behaviours. Please indicate the degree of agreement or disagreement with the following statements on the state of COVID19, anxiety, affective worry and protective behaviours, using the scale provided:
References
- Adu, M. K., Wallace, L. J., Lartey, K. F., Arthur, J., Oteng, K. F., Dwomoh, S., ... & Agyapong, V. I. (2021). Prevalence and correlates of likely major depressive disorder among the adult population in Ghana during the Covid19 pandemic. International journal of environmental research and public health, 18(13), 7106.
- Alshurafat, H., Al Shbail, M. O., Masadeh, W. M., Dahmash, F., & Al-Msiedeen, J. M. (2021). Factors affecting online accounting education during the Covid19 pandemic: An integrated perspective of social capital theory, the theory of reasoned action and the technology acceptance model. Education and Information Technologies, 26(6), 6995-7013.
- Anwar, S., Supriyanto, S., Budiarto, W., & Hargono, R. (2020). Relationship between social capital and mental health among the older adults in Aceh, Indonesia. Indian Journal of Forensic Medicine & Toxicology, 14(3), 2204-2209.
- Bartscher, A. K., Seitz, S., Siegloch, S., Slotwinski, M., & Wehrhöfer, N. (2021). Social capital and the spread of Covid19: Insights from European countries. Journal of Health Economics, 80, 102531.
- Bish, A., & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British journal of health psychology, 15(4), 797-824.
- Bufquin, D., Park, J. Y., Back, R. M., de Souza Meira, J. V., & Hight, S. K. (2021). Employee work status, mental health, substance use, and career turnover intentions: An examination of restaurant employees during Covid19. International Journal of Hospitality Management, 93, 102764.
- Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., ... & Zhang, Z. (2020). Mental health care for medical staff in China during the Covid19 outbreak. The Lancet Psychiatry, 7(4), e15-e16.
- Chung, J. P., & Yeung, W. S. (2020). Staff mental health self-assessment during the Covid19 outbreak. East Asian Archives of Psychiatry, 30(1), 34.
- Ehsan, A., & Spini, D. (2020). Place, social capital, and mental health: A mixed-methods case study of a community-based intervention. Health & place, 64, 102386.
- Giorgi, G., Lecca, L. I., Alessio, F., Finstad, G. L., Bondanini, G., Lulli, L. G., ... & Mucci, N. (2020). Covid19-related mental health effects in the workplace: A narrative review. International journal of environmental research and public health, 17(21), 7857.
- Goodman, M. L., Temple, J. R., Elliott, A. J., Seidel, S. E., Gitari, S., & Raimer-Goodman, L. A. (2022). Child maltreatment, social capital, maternal mental health and duration of program involvement: Assessment from a community-based empowerment program in Kenya. Journal of Family Violence, 1-11.
- Greenberg, N. (2020). Mental health of health-care workers in the Covid19 era. Nature Reviews Nephrology, 16(8), 425-426.
- Greenberg, N., Docherty, M., Gnanapragasam, S., & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during Covid19 pandemic. bmj, 368.
- Greenberg, N., Weston, D., Hall, C., Caulfield, T., Williamson, V., & Fong, K. (2021). Mental health of staff working in intensive care during Covid19. Occupational Medicine, 71(2), 62-67.
- Hair Jr, J., Hair Jr, J. F., Hult, G. T. M., Ringle, C. M., & Sarstedt, M. (2021). A primer on partial least squares structural equation modeling (PLS-SEM). Sage publications.
- Horsch, A., Lalor, J., & Downe, S. (2020). Moral and mental health challenges faced by maternity staff during the Covid19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1), S141.
- Huang, J. Z., Han, M. F., Luo, T. D., Ren, A. K., & Zhou, X. P. (2020). Mental health survey of medical staff in a tertiary infectious disease hospital for Covid19. Zhonghua lao dong wei sheng zhi ye bing za zhi, 192-195.
- Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health education quarterly, 11(1), 1-47.
- Johnson, S., Dalton-Locke, C., Vera San Juan, N., Foye, U., Oram, S., Papamichail, A., ... & Simpson, A. (2021). Impact on mental health care and on mental health service users of the Covid19 pandemic: A mixed methods survey of UK mental health care staff. Social psychiatry and psychiatric epidemiology, 56, 25-37.
- Kawachi, I., & Berkman, L. F. (2001). Social ties and mental health. Journal of Urban health, 78, 458-467.
- Kontoangelos, K., Economou, M., & Papageorgiou, C. (2020). Mental health effects of Covid19 pandemia: A review of clinical and psychological traits. Psychiatry investigation, 17(6), 491.
- Lee, J., Kim, K., Park, G., & Cha, N. (2021). The role of online news and social media in preventive action in times of infodemic from a social capital perspective: The case of the Covid19 pandemic in South Korea. Telematics and Informatics, 64, 101691.
- Li, C., Jiang, S., & Fang, X. (2020). Effects of multi-dimensional social capital on mental health of children in poverty: An empirical study in Mainland China. Journal of health psychology, 25(6), 853-867.
- Liu, Z., Han, B., Jiang, R., Huang, Y., Ma, C., Wen, J., ... & Ma, Y. (2020). Mental health status of doctors and nurses during Covid19 epidemic in China. Available at SSRN 3551329.
- Makridis, C. A., & Wu, C. (2021). How social capital helps communities weather the Covid19 pandemic. PLoS ONE, 16(1), e0245135.
- Makridis, C. A., & Wu, C. (2021). How social capital helps communities weather the Covid19 pandemic. PLoS ONE, 16(1), e0245135.
- Person, B., Sy, F., Holton, K., Govert, B., Liang, A., Team, S. C. O., ... & Zauderer, L. (2004). Fear and stigma: The epidemic within the SARS outbreak. Emerging infectious diseases, 10(2), 358.
- Ringle, C. M., Sarstedt, M., Mitchell, R., & Gudergan, S. P. (2020). Partial least squares structural equation modeling in HRM research. The International Journal of Human Resource Management, 31(12), 1617-1643.
- Rosenstock, I. M. (1974). The health belief model and preventive health behavior. Health education monographs, 2(4), 354-386.
- Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health education quarterly, 15(2), 175-183.
- Ruffolo, M., Price, D., Schoultz, M., Leung, J., Bonsaksen, T., Thygesen, H., & Geirdal, A. Ø. (2021). Employment uncertainty and mental health during the Covid19 pandemic initial social distancing implementation: A cross-national study. Global Social Welfare, 8, 141-150.
- Sarstedt, M., Ringle, C. M., Smith, D., Reams, R., & Hair Jr, J. F. (2014). Partial least squares structural equation modeling (PLS-SEM): A useful tool for family business researchers. Journal of family business strategy, 5(1), 105-115.
- Sato, K., Amemiya, A., Haseda, M., Takagi, D., Kanamori, M., Kondo, K., & Kondo, N. (2020). Postdisaster changes in social capital and mental health: A natural experiment from the 2016 Kumamoto earthquake. American journal of epidemiology, 189(9), 910-921.
- Song, L., Wang, Y., Li, Z., Yang, Y., & Li, H. (2020). Mental health and work attitudes among people resuming work during the Covid19 pandemic: A cross-sectional study in China. International journal of environmental research and public health, 17(14), 5059.
- Sun, Q., & Lu, N. (2020). Social capital and mental health among older adults living in urban China in the context of Covid19 pandemic. International Journal of Environmental Research and Public Health, 17(21), 7947.
- Toh, W. L., Meyer, D., Phillipou, A., Tan, E. J., Van Rheenen, T. E., Neill, E., & Rossell, S. L. (2021). Mental health status of healthcare versus other essential workers in Australia amidst the Covid19 pandemic: Initial results from the collate project. Psychiatry Research, 298, 113822.
- Tracy, D. K., Tarn, M., Eldridge, R., Cooke, J., Calder, J. D., & Greenberg, N. (2020). What should be done to support the mental health of healthcare staff treating Covid19 patients?. The British Journal of Psychiatry, 217(4), 537-539.
- Tsamakis, K., Rizos, E., Manolis, A. J., Chaidou, S., Kympouropoulos, S., Spartalis, E., ... & Triantafyllis, A. S. (2020). [Comment] Covid19 pandemic and its impact on mental health of healthcare professionals. Experimental and therapeutic medicine, 19(6), 3451-3453.
- Usher, K., Durkin, J., & Bhullar, N. (2020). The COVID-19 pandemic and mental health impacts. International journal of mental health nursing, 29(3), 315.
- Vizheh, M., Qorbani, M., Arzaghi, S. M., Muhidin, S., Javanmard, Z., & Esmaeili, M. (2020). The mental health of healthcare workers in the Covid19 pandemic: A systematic review. Journal of Diabetes & Metabolic Disorders, 19, 1967-1978.
- Walton, M., Murray, E., & Christian, M. D. (2020). Mental health care for medical staff and affiliated healthcare workers during the Covid19 pandemic. European Heart Journal: Acute Cardiovascular Care, 9(3), 241-247.
- Wilson, J. M., Lee, J., Fitzgerald, H. N., Oosterhoff, B., Sevi, B., & Shook, N. J. (2020). Job insecurity and financial concern during the Covid19 pandemic are associated with worse mental health. Journal of occupational and environmental medicine, 62(9), 686-691.
- Wong, A. S., & Kohler, J. C. (2020). Social capital and public health: Responding to the Covid19 pandemic. Globalization and Health, 16, 1-4.
- Yu, J., Park, J., & Hyun, S. S. (2021). Impacts of the COVID19 pandemic on employees’ work stress, well-being, mental health, organizational citizenship behavior, and employee-customer identification. Journal of Hospitality Marketing & Management, 30(5), 529-548.
- Zaka, A., Shamloo, S. E., Fiorente, P., & Tafuri, A. (2020). COVID19 pandemic as a watershed moment: A call for systematic psychological health care for frontline medical staff. Journal of Health Psychology, 25(7), 883-887.
- Zheng, F., Khan, N. A., & Hussain, S. (2020). The COVID 19 pandemic and digital higher education: Exploring the impact of proactive personality on social capital through internet self-efficacy and online interaction quality. Children and Youth Services Review, 119, 105694.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).