1. Introduction
Influenza vaccination is a pivotal health intervention for individuals with Diabetes Mellitus (DM), who are disproportionately susceptible to influenza and its complications [
1]. This susceptibility is further compounded by the immunocompromised state often associated with DM, highlighting the importance of seasonal influenza vaccination (SIV) which has shown a valid protection against Influenza in young and old persons with DM (pwDM), reducing risk of hospitalization and mortality [
2,
3,
4]. As recommended by WHO [
5], in Spain, pwDM are classified as high-risk patients for influenza, leading to targeted public health initiatives in Spain to enhance their protection, and specifically include pwDM in their SIV campaigns, offering free immunization [
6].
Propelled by guidelines issued by health authorities globally [
1,
5] and within the EU [
7,
8], and the Spanish Government [
6], uptake rates of SIV among pwDM in Spain have slowly increased from 61.4% in 2003 to 63.8% in 2006 and plateaued at 65.0% in 2010 [
9], missing the minimum coverage of SIV among pwDM of ≥75 % recommended by the ECDC by 10% points [
8], thus remaining below targeted levels and highlighting a significant necessity for public health action [
10].
The influence of socio-demographic factors, such as age and income, and behavioural factors, including healthcare engagement and education, on vaccination uptake has been documented in various studies [
11,
12,
13]. Moreover, the lack of a regular HCP and the absence of a professional recommendation have been identified as barriers to SIV [
4,
14]. Recent publications from South Corea and Hungary investigating factors influencing uptake of SIV found consistently higher uptakes among older pwDM [
15,
16]. Sex and education, however, was only shown Hungary to affect SIV uptake. In France, age and frequent contact to the healthcare system showed an improvement of SIV uptake rates over time [
17].
Given the above-mentioned stall of SIV uptake-rates within pwDM in Spain, our study delves into the EHIS 2020 data to explore the current state of SIV uptake. We aim to dissect the complex interplay of factors contributing to the suboptimal vaccination rates and to pinpoint key determinants that could be leveraged in public health strategies to improve coverage, all while adhering to the rigorous standards set forth by the STROBE criteria for cross-sectional studies [
18]. By doing so, we hope to bolster the defences of this at-risk population against influenza and its potentially life-threatening complications, thus contributing to the overarching goal of enhanced public health [
19].
2. Materials and Methods
Study Design and Data Source
A cross-sectional study was conducted with data from the 2020 European Health Interview Survey (EHIS). A detailed protocol was published earlier elsewhere [
20]. Representative population samples were drawn from sampling frames set up at national level that allowed persons or households to be selected at random, with a known probability of selection. The Eurostat protocol was subsequently complemented by the Spanish National Institute for Statistics (INE) whose detailed protocol as well as the corrections for no response due to the COVID-19 pandemic has been published elsewhere [
21].
Spanish data were acquired by a population register with a stratified multi-stage sampling through INE, using a three-step approach based on data from the last census stratified three-stage sampling, with proportional random selection of primary and secondary sampling units (towns and sections, respectively), with the final units (non-institutionalized individuals) being selected by means of random routes and sex- and age-based quotas. Eligible participants were individuals at the age of 15 years or above. In Spain, the EHIS was conducted in the time-period from July 2019 to July 2020 as a stand-alone study under the name of “Health Interview Study”. The study questionnaire was available in Spanish, Catalan, Valenciano, Euskera, Gallego and English. The data-collection was realized by face-to-face interviews and telephone interviews. Thereby, an effective sample size of 22,072 participants was archived.
Study Population and Variables of Interest
The study population included adults and minors over 15 years old with the diagnosis of DM. The status of DM was fulfilled when participants answered yes to one or more of the following questions: “having a diagnosis of DM”, “having had a former diagnosis of DM” or “medication for diabetes”.
Our outcome of interest was the self-reported non-vaccination during the last SIV, with a binary outcome of ‘Yes’ or ‘No’. In Spain, there is an active recommendation for individuals aged 60 and above to receive the SIV, regardless of the presence of chronic diseases that might further justify vaccination. To account for this potential confounder, we stratified the data by age, dividing the population into those under 60 years and those 60 years and older [
28].
Independent covariables encompassed sociodemographic, healthcare use, healthcare barriers, psychological and behavioural characteristics that were a priori selected and included in the descriptive analysis and considered for the logistic regression model. Sociodemographic variables included Sex [Men-Women], Spanish Nationality [Yes-No], Marital Status [Single, Married, Widowed, Divorced], Cohabitation [Yes-No], Study Level [Incomplete Primary Education, Complete Primary Education, Graduate, Postgraduate], and Social Class [Directors and Managers, Intermediate Occupations and Self-Employed, Skilled and Semi-Skilled Workers in the Primary Sector, Supervisors and Technical Skilled Workers, Unskilled Workers]. Healthcare use variables encompassed Health Perception [Good, Poor], Health Insurance [Public, Private], Time of Last Medical Visit [In the last 4 weeks, Between 4 weeks and 12 months, 12 months or more ago], Nurse or Midwife Consultation [Yes-No], Cold Medications [Yes-No], Use of Emergency Services [Yes-No], and Hospitalization [Yes-No] and Alternative Medicine Visits (homeopath, acupuncturist, naturist or another alternative medicine) [Yes-No]. Healthcare barriers included No Medical Attention for Economic Barriers [No, Yes], No Medical Attention due to Transport Barriers [Yes-No] and No Medical Attention due to Waiting List in the last 12 months [Yes-No]. Psychological and weight status included were Depressive Severity [None, Moderate, Severe] and body mass index (BMI) [underweight, normal, overweight, obesity]. Behavioral factors were Physical activity [Sedentary lifestyle, Occasional activity, Monthly activity, Weekly training], Alcohol Consumption [Never or not in the last 12 months, Once per month or less, More than once per week], Tobacco Use [Yes-No], and Social Support [A lot, Somewhat, Neither much nor little, Little, Nothing].
Statistical Analysis
For the descriptive analyses, each of the categorical variables were presented as the total number and percentage according to the vaccination status. The bivariable association analyses between variables were assessed using chi-square or Fisher’s exact tests as appropriate. Selected participants with no information about any of the covariates were excluded in the bivariable analyses.
The multivariate binary logistic regression analysis identified independent predictors of vaccination in a stepwise manner, by removing of non-significant variables (p>0.2) except for sex and study level as a proxy covariate to socioeconomical status [
12,
15,
22]. For multivariate logistic regression, categories with low numbers were grouped (i.e., social support). Only those significant at p<0.05 were retained in the final model, with reported non-adjusted and adjusted ORs and associated 95% CI. The log-likelihood, Akaike information criterion and Bayesian information criterion was used to compare the fit of different models.
Similarly, to the univariate analyses, the presented multivariable analyse corresponds to a complete case analysis, in which the 3.69% (81/2194) of observations with missing values were excluded. No patterns of missing data were detected for each of the covariates both in univariable and multivariable analyses with skimr and visdat R packages. Nevertheless, substitution analyses with MICE package were performed for the multivariable model, showing similar results (results not shown). Collinearity was evaluated using variance inflation factors with a threshold of < 5 to indicate significant collinearity.
Descriptive and logistic regression analyses were performed with R Version 2023.12.
3. Results
To better understand the factors associated with non-vaccination, we analysed the sociodemographic profile, healthcare access, comorbidities, and substance use among pwDM.
Participants’ Characteristics and Immunization Status
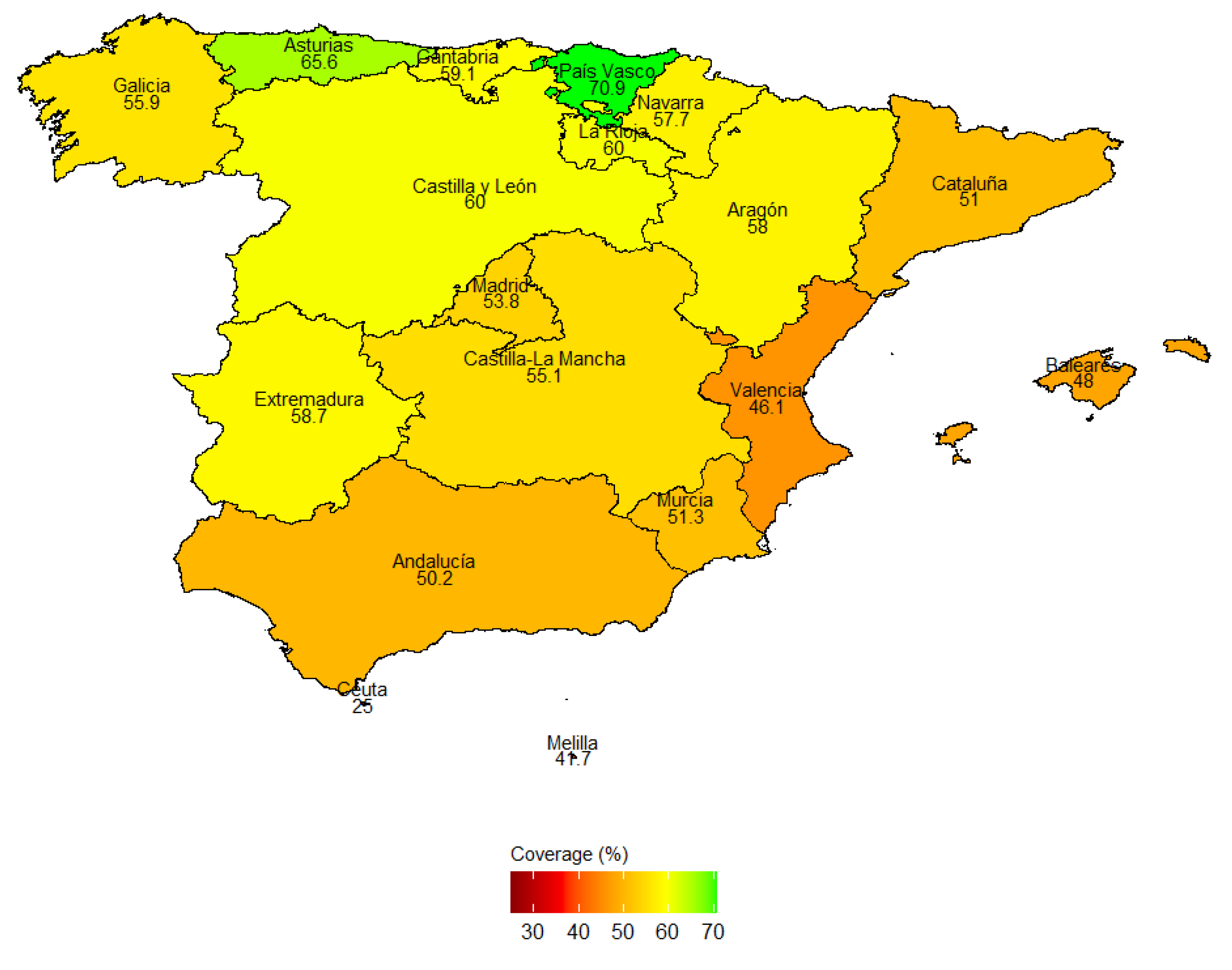
Out of 22,072 participants from the Spanish EHIS 2020, 2,193 fulfilled inclusion criteria to be considered a pwDM, with 1030 (47%) non-vaccinated in the last SIV season. The mean age among pwDM was 70.1 years CI 95% (69.6-70.7), with a minimum of 15 and maximum of 95 years. The geographical analysis reveals notable regional disparities, demonstrating a clear north-south gradient (
Figure 1). Vaccination coverage ranges significantly across the autonomous communities. The País Vasco exhibits the highest vaccination rate at 70.9%, while Ceuta has the lowest at 25%. Northern regions such as Asturias (65.6%) and Galicia (59.9%) show higher vaccination rates compared to southern areas like Andalusia (50.2%) and Melilla (47.7%).
Sociodemographic Profile
Age is significantly associated with vaccination uptake, showing 1,767 participants over 60 years, where 721 (41%) were unvaccinated sharply contrasted by the 309 (73%) under 60 years, who remained unvaccinated (p<0.001).
The gender split was almost even, with 1,109 (50.5%) men and 1,085 (49.5%) women (
Table 1). Amongst men, 545 (49%) were unvaccinated, amongst women 486 (45%) were unvaccinated. However, in the age stratified model the results showed that for women under 60 years, the OR for not-vaccination was 0.73 with a 95%CI of 0.46 to 1.13 and a p-value of 0.2, indicating no significant difference in the likelihood of vaccination compared to men in this age group (
Table 2). For those equal or over 60 years, the OR was 1.02 with a 95% CI of 0.83 to 1.25 and a (p= 0.9), also showing no significant difference in vaccination rates between women and men in this older age group.
Those with complete primary education were 1,110, with 502 (45%) unvaccinated. Graduates numbered 259, with 151 (58%) unvaccinated, and postgraduates were 283, with 167 (59%) unvaccinated, interestingly indicating a significant inverse influence of educational attainment on vaccination rates (p<0.001). This observation was confirmed within the age stratified model showing that, among individuals 60 years or older, compared to those with incomplete primary education, graduates showed again an increased likelihood of non-vaccination (OR 1.79, 95% CI: 1.24, 2.60, p=0.002), while the effect for complete primary education and postgraduates was not significant (OR 0.97, 0.76-1.22, p=0.8 and OR 1.41, 0.98-2.03, p=0.064, respectively). In contrast, in individuals under 60 years, compared to incomplete primary education, those with complete primary education had an OR of 3.53 (95% CI: 1.49, 8.38, p=0.004), graduates had an OR of 3.43 (95% CI: 1.31, 8.61, p=0.012), and postgraduates had an OR of 3.67 (95% CI: 1.45, 9.38, p=0.006) of non-vaccination, indicating that pwDM of higher education had approximately three times higher likelihood of not being vaccinated and thus showing even more pronounced results compared to those over 60 years of age.
Nationality suggested a statistically significant difference, between Spanish and non-Spanish nationals, (46% vs 74% unvaccinated). However, there was no statistically significant difference shown in the model. Similar, marital status showed that married pwDM above 60 years of age were significantly (p<0.011) less often unvaccinated (40%) than single (48%) and divorced (55%), nonetheless, there was no statistically significant association shown in the model.
In terms of social support, the analysis showed that 1,897 participants reported having a lot of support, with 864 (46%) unvaccinated. Those reporting somewhat of support numbered 206, with 113 (55%) unvaccinated. A smaller group felt neither much nor little support, totalling 51, with 31 (61%) unvaccinated. Very few reported little or no support, 11 and 17 respectively, with higher percentages unvaccinated, indicating the important role of social support in vaccination decisions (p=0.004). In the model, this observation could be confirmed within the strata of people ≥ 60 years, showing that compared to pwDM with a lot of social support, those with somewhat were 46% (OR 1.46 CI95% 1.04-2.05, p=0.028) and those with little or no social support even 87% (OR 1.84, CI95% 1.06–3.21, p=0.031) more likely of not being vaccinated.
Healthcare Access
The timing of the last medical visit showed significant variation in non-vaccination rates with pwDM who visited a medical professional in the last 4 weeks showing the lowest (40%) and those who had not visited in more than 12 months showing the highest (70%). In the model, individuals 60 years or older, when compared to a visit within the last 4 weeks, the ORs for non-vaccination were 1.47 (95% CI: 1.20, 1.81, p<0.001) for visits between 4 weeks and 12 months, and 2.18 (95% CI: 1.00, 4.83, p=0.050) for those without a visit in the past year. For pwDM under 60 years, compared to a visit within the last 4 weeks, those who had a visit between 4 weeks and 12 months had an OR of non-vaccination of 2.34 (95% CI: 1.61, 3.43, p<0.001).
Descriptively, pwDM with past nurse or midwife consultations showed significantly higher non-vaccination rates (40%) than those without (50%). In the model, not consulting a nurse or midwife was associated with higher non-vaccination rates across both age groups, but particularly in the older cohort (OR 2.22, 95% CI: 1.56, 3.19, p<0.001) compared to the younger group where it was not significant (OR 0.77, 95% CI: 0.36, 1.60, p=0.5).
Previous use of cold medications was described to be significantly associated with lower non-vaccination rates (52% vs 59%). In the model, although not statistically significant, there was a trend suggesting those who did not took cold medications were more likely not to be vaccinated, especially in the older group (OR 1.34, 95% CI: 0.96, 1.88, p=0.094) compared to the younger cohort (OR 1.69, 95% CI: 0.86, 3.26, p=0.12).
Neither a difference of health insurance (public 47% vs private 59%) nor use of emergency services (45% use vs 52% no use) showed statistically significant difference in non-vaccination rates.
Hospitalization within the last 12 months showed a slight and statistically significant difference in non-vaccination rates (42% hospitalized vs 48% in non-hospitalized), but no association was found in the model.
Concerning economic barriers to medical attention, 2,139 participants reported no barriers, with 995 (47%) unvaccinated. Those facing barriers numbered 55, with 36 (65%) unvaccinated, indicating economic factors’ impact on vaccination (p=0.005). In the model, this could be confirmed in pwDM aged 60 years or older showing a higher likelihood of not-vaccination with an OR of 2.68 (95% CI: 1.34, 5.58, p=0.006), whereas the younger group did not show a significant difference (OR 1.12, 95% CI: 0.41, 3.45, p=0.8), indicating a higher importance of economic barriers among older pwDM.
Comorbidities and Substance Use
Depressive severity was also considered but showed no significant difference in non-vaccination rates between categories (48% in no depression, vs 44% in moderate depression vs 58% in severe depression).
Frequent alcohol consumption showed substantially lower vaccination rates (48%) compared to moderate (50%) and no alcohol consumption (57%). Similar, smokers (49%) showed lower vaccination rates than non-smokers (57%). However, neither alcohol nor tobacco consumption showed statistically significant associations in the model.
4. Discussion
This study provides a comprehensive analysis of factors associated with non-vaccination among pwDM in Spain, employing data from the EHIS 2020. The findings highlight several significant factors associated with vaccination uptake in this population.
The descriptive analysis revealed a proportion of SIV uptake within the last season amongst pwDM in Spain of 53%, while 47% remained unvaccinated. This number deviates strongly from the latest reports on vaccination uptake of 65%, issued by Jimenez-Trujillo and colleagues in 2013 [
9]. The analysis with a multi-variable logistic regression model showed that, against expectations, higher education attainment, specifically graduate education, is associated with an increased likelihood of non-vaccination, indicating a gap of attention towards higher educated. Social support also emerged as a significant factor, with varying levels of support influencing vaccination likelihood, suggesting a dose-response effect, highlighting the importance of community and family in health behaviours. To our knowledge, in the context of pwDM, this was not shown before. Interestingly, the time since the last medical visit emerged as a significant predictor, with those visiting an HCP more than 12 months ago more likely to be unvaccinated, underscoring the need of yearly medical visits for pwDM. Consultations with nurses or midwives and the use of cold medications were associated with higher vaccination rates, pointing to the influence of healthcare accessibility and health-seeking behaviour on vaccination decisions. These results underscore the positive role that HPCs like nurses, midwives, and pharmacists can play in recommending or administering the SIV, suggesting that these healthcare professionals are pivotal in enhancing vaccination coverage through their direct interactions with patients [
23]. Also, economic barriers to medical care were found to negatively affect vaccination uptake. Efforts to mitigate economic barriers to healthcare could enhance vaccination rates as previously described by Schmid et al. (2017).
Recent flu vaccination campaigns have predominantly targeted the demographic aged 60 and above, reflecting a strategic emphasis on this cohort through the concerted development of audiovisual materials, including posters and infographics, across both national and regional health [
25,
26,
27] authorities. Moreover, the standardized vaccination schedule, applicable across various age groups [
28], predominantly references populations over the age of 65 or below 4, inadvertently marginalizing the vaccination imperative for intermediary risk groups, notably pwDM. This gap is ostensibly bridged in the seasonal flu and COVID-19 vaccination recommendations [
29], which establish foundational guidelines subsequently adapted by autonomous communities in their respective health directives [
30,
31].
The age-specific prioritization for vaccination, particularly among those aged 60 and above, is corroborated by findings from the ADVISE study [
32] indicating a perceptual discrepancy among healthcare professionals regarding the uniform importance of vaccination across different age groups. This underscores an exigent need for enhanced vaccination-related training for healthcare providers, with a notable emphasis on addressing the prevalent scepticism and negative perceptions towards vaccination efficacy within the medical and nursing fraternities [
33]. Such educational interventions are necessary for ameliorating the vaccination uptake rates within the country, particularly given that a significant proportion of vaccinations among diabetic patients occur consequent to medical or nursing recommendations [
34] highlighting the pivotal role of healthcare professionals in patient vaccination decisions.
These findings have important implications for public health policy and intervention strategies. Tailored educational programs targeting individuals with higher education levels and strengthening community support systems and enhancing accessibility to HCPs, including nurse-driven vaccination, as well as employing digital reminders through Electronic Health Records (EHR) may also prove beneficial [
35,
36,
37].
Limitations of our study include the reliance on self-reported data and the cross-sectional design, which limits our ability to establish causality. Self-reported data may introduce potential recall and social-desirability bias, and there is a risk of underestimating DM rates. Previous research by Jimenez-Garcia in 2014 suggests that self-reported vaccination rates tend to overestimate actual rates, possibly due to social desirability bias [
12]. Therefore, it is possible that our reported vaccination rates are higher than reality. Additionally, the study does not differentiate between different subtypes of DM, and it does not include non-institutionalized individuals or those under 15 years of age. Further, parts of the EHIS 2020 were conducted during the first year of the COVID-19 pandemic, potentially leading to biases in data acquisition among participants with an unknown direction. Participants might have been influenced by reiterated public Spanish government influenza vaccination recommendations for chronically ill people, possibly leading to an overreporting of influenza vaccination.
On the other hand, the strengths of our study lie in its utilization of the most recent and nationally representative data available for Spain. Our large sample size enhances generalizability, and the robust sampling methodology has minimized missing data. These strengths contribute to the overall reliability and validity of our findings.
5. Conclusions
Overall, this study contributes valuable insights into the factors affecting influenza vaccination among diabetics in Spain, offering a solid foundation for future targeted public health strategies. Based on our insights and to improve SIV rates among pwDM, we recommend that Spanish Public Health Authorities implement tailored interventions such as targeted awareness campaigns specifically aimed at younger, more educated pwDM, infrequent healthcare users, and those facing economic barriers and low social support. It is necessary to educate and engage HCPs about the necessity and benefits of SIV for pwDM of all ages. The utilisation of EHRs and SMS for annual digital reminders for pwDM and HCPs is also recommended. Additionally, it is important to investigate the reasons for non-adherence to vaccination recommendations among HCPs and pwDM. Finally, efforts should be made to fill knowledge gaps concerning institutionalised pwDM and those younger than 15 years of age.
Author Contributions
Conceptualization, E.P.T. and D.H.; Methodology, D.H.; Software, D.H.; Validation, E.P.T., D.H. and J.A.M.R.; Formal Analysis, D.H..; Investigation, E.P.T.; Resources, J.A.M.R.; Data Curation, DH.; Writing – Original Draft Preparation, E.P.T.; Writing – Review & Editing, D.H., J.A.M.R.; Visualization, D.H..; Supervision, J.J.J.M.; Project Administration, J.J.J.M.; Funding Acquisition, J.J.J.M.
Funding
This research received no external funding
Institutional Review Board Statement
Ethical review and approval were waived for this study because it utilised secondary data from the European Health Interview Survey 2020 (EHIS 2020), which underwent its own extensive ethical approval process. Our analysis of this publicly available data adhered to the principles outlined in the Declaration of Helsinki.
Informed Consent Statement
Patient consent was waived for this study because it utilised secondary data from the European Health Interview Survey 2020 (EHIS 2020), which underwent its own extensive ethical approval process including informed consent statements.
Data Availability Statement
Acknowledgments
The authors would like to thank the employees of the Andalusian School of Public Health (EASP) Ricardo Ocaña-Riola and Miguel Rodríguez Barranco for assistance in statistical analysis.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- CDC. Centers for Disease Control and Prevention. CDC’s Vaccine Information for Adults with Diabetes. 2021. Available online: https://www.cdc.gov/vaccines/adults/rec-vac/health-conditions/diabetes/infographic/index.html (accessed on 31 January 2023).
- Dos Santos G, Tahrat H, Bekkat-Berkani R. Immunogenicity, safety, and effectiveness of seasonal influenza vaccination in patients with diabetes mellitus: A systematic review. Hum. Vaccines Immunother. 2018, 14, 1853–1866. [CrossRef]
- Frasca D, Diaz A, Romero M, Mendez NV, Landin AM, Ryan JG, et al. Young and elderly patients with type 2 diabetes have optimal B cell responses to the seasonal influenza vaccine. Vaccine 2013, 31, 3603–3610. [CrossRef] [PubMed]
- Loerbroks A, Stock C, Bosch JA, Litaker DG, Apfelbacher CJ. Influenza vaccination coverage among high-risk groups in 11 European countries. Eur. J. Public. Health. 2012, 22, 562–568. [CrossRef] [PubMed]
- World Health Organization. WHO global strategy on people-centred and integrated health services: interim report. World Health Organization. 2015. https://iris.who.int/handle/10665/155002.
- Ministerio de Sanidad, Política Social e Igualdad. El Ministerio de Sanidad, Política Social e Igualdad recomienda la vacunación frente a la gripe a mayores de 65 años, grupos de riesgo y personal sanitario [Internet]. Available online: https://mpt.gob.es/delegaciones_gobierno/delegaciones/melilla/actualidad/notas_de_prensa/notas/2011/09/30_09_11_sanidad.html (accessed on 21 February 2024).
- Council Recommendation of 22 December 2009 on seasonal influenza vaccination Text with EEA relevance.
- European Centre for Disease Prevention and Control. Seasonal influenza vaccination recommendations and coverage rates in EU/EEA Member States: an overview of vaccination recommendations for 2021−22 and coverage rates for the 2018–19 to 2020–21 influenza seasons. [Internet]. LU: Publications Office; 2023. Available online: https://data.europa.eu/doi/10.2900/335933 (accessed on 26 January 2024).
- Jimenez-Trujillo I, López de Andrés A, Hernández-Barrera V, Carrasco-Garrido P, Santos-Sancho JM, Jiménez-García R. Influenza vaccination coverage rates among diabetes sufferers, predictors of adherence and time trends from 2003 to 2010 in Spain. Hum Vaccines Immunother. 2013, 9, 1326–1332. [CrossRef] [PubMed]
- Soriguer F, Goday A, Bosch-Comas A, Bordiú E, Calle-Pascual A, Carmena R, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia. 2012, 55, 88–93. [CrossRef] [PubMed]
- Heymann AD, Shapiro Y, Chodick G, Shalev V, Kokia E, Kramer E, et al. Reduced Hospitalizations and Death Associated With Influenza Vaccination Among Patients With and Without Diabetes. Diabetes Care 2004, 27, 2581–2584. [CrossRef] [PubMed]
- Jiménez-García R, Hernandez-Barrera V, Rodríguez-Rieiro C, Carrasco Garrido P, López de Andres A, Jimenez-Trujillo I, et al. Comparison of self-report influenza vaccination coverage with data from a population based computerized vaccination registry and factors associated with discordance. Vaccine 2014, 32, 4386–4392. [CrossRef] [PubMed]
- Verger P, Cortaredona S, Pulcini C, Casanova L, Peretti-Watel P, Launay O. Characteristics of patients and physicians correlated with regular influenza vaccination in patients treated for type 2 diabetes: a follow-up study from 2008 to 2011 in southeastern France. Clin Microbiol Infect. 2015, 21, 930.e1–930.e9. [CrossRef]
- Shin HY, Chung JH, Hwang HJ, Kim TH. Factors influencing on influenza vaccination and its trends of coverage in patients with diabetes in Korea: A population-based cross-sectional study. Vaccine 2018, 36, 91–97. [CrossRef]
- Han, A.L. Factors associated with influenza vaccine coverage among patients with diabetes: Korea National Health and Nutrition Examination Survey 2016–2018. Int J Diabetes Dev Ctries. 2022, 42, 297–304. [Google Scholar] [CrossRef]
- Szőllősi GJ, Minh NC, Pataki J, Santoso CM, Nagy AC, Kardos L. Influenza Vaccination Coverage and Its Predictors among Self-Reported Diabetic Patients—Findings from the Hungarian Implementation of the European Health Interview Survey. Int. J. Environ. Res. Public. Health 2022, 19, 16289. [CrossRef] [PubMed]
- Bocquier A, Cortaredona S, Fressard L, Galtier F, Verger P. Seasonal influenza vaccination among people with diabetes: influence of patients’ characteristics and healthcare use on behavioral changes. Hum. Vaccines Immunother. 2020, 16, 2565–2572. [CrossRef] [PubMed]
- Elm E von, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [CrossRef] [PubMed]
- Lewis C, Darnell D, Kerns S, Monroe-DeVita M, Landes SJ, Lyon AR, et al. In Proceedings of the 3rd Biennial Conference of the Society for Implementation Research Collaboration (SIRC) 2015: advancing efficient methodologies through community partnerships and team science, Seattle, WA, USA, 24–26 September 2015. Implement Sci IS. 2016, 11 (Suppl 1), 85.
- European Commission. Statistical Office of the European Union. European Health Interview Survey (EHIS wave 3): methodological manual : 2020 edition (re edition). [Internet]. LU: Publications Office; 2020 [cited 2024 Jan 26]. Available online: https://data.europa.eu/doi/10.2785/135920.
- Instituto Nacional Estadística. Encuesta Europea de Salud en España 2020; EESE-2020, Metodología [Internet]. 2019. Available online: https://www.ine.es/metodologia/t15/t153042020.pdf (accessed on 28 May 2024).
- Bocquier A, Cortaredona S, Fressard L, Loulergue P, Raude J, Sultan A, et al. Trajectories of seasonal influenza vaccine uptake among French people with diabetes: a nationwide retrospective cohort study, 2006–2015. BMC Public Health 2019, 19, 918. [CrossRef]
- Pennant KN, Costa JJ, Fuhlbrigge AL, Sax PE, Szent-Gyorgyi LE, Coblyn J, et al. Improving Influenza and Pneumococcal Vaccination Rates in Ambulatory Specialty Practices. Open Forum Infect. Dis. 2015, 2, ofv119. [CrossRef] [PubMed]
- Schmid P, Rauber D, Betsch C, Lidolt G, Denker ML. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550.
- Comunidad de Madrid. Comunidad de Madrid. 2016. Gripe. Available online: https://www.comunidad.madrid/servicios/salud/gripe (accessed on 21 February 2024).
- Junta de Andalucía C de S y C. Covid [Internet]. Plan de Vacunaciones de Andalucía (Andavac). Available online: https://www.andavac.es/campanas/covid/ (accessed on 21 February 2024).
- Ministero de Sanidad. vacuna a su tiempo. Ministerio de Sanidad - Prensa y comunicación - Cada vacuna a su tiempo. Available online: https://www.sanidad.gob.es/campannas/campanas23/VacunacionEstacional.htm (accessed on 21 February 2024).
- Consejo Interterritorial SN de S. CALENDARIO COMÚN DE VACUNACIONES E INMUNIZACIONES A LO LARGO DE TODA LA VIDA [Internet]. Available online: https://web.mscbs.gob.es/areas/promocionPrevencion/vacunaciones/calendario-y-coberturas/docs/CalendarioVacunacion_Todalavida.pdf (accessed on 21 February 2024).
- Consejo Interterritorial SN de S. Recomendaciones de vacunación frente a gripe y COVID-19 en la temporada 2023-2024 en España. [Internet]. 2023. Available online: https://www.sanidad.gob.es/areas/promocionPrevencion/vacunaciones/gripe_covid19/docs/RecomendacionesVacunacion_Gripe-Covid19.pdf (accessed on 21 February 2024).
- Comunidad de Madrid DG de SP. GRUPOS DE POBLACIÓN DIANA DE VACUNACIÓN ANTIGRIPAL y COVID-19. TEMPORADA 2023-24 [Internet]. Available online: https://www.comunidad.madrid/sites/default/files/doc/sanidad/prev/grupos_de_poblacion_diana_de_vacunacion_antigripal_cm_23-24.pdf (accessed on 21 February 2024).
- Junta de Andalucía C de S y C. VACUNACIÓN FRENTE A GRIPE – COVID-19 EN ANDALUCÍA CAMPAÑA 2023-2024 [Internet]. 2023. Available online: https://www.andavac.es/wp-content/uploads/instrucciones/Instruccion_DGSPyOF-10-2023_Gripe-Covid_Andalucia_2023-2024.pdf (accessed on 21 February 2024).
- Redondo Margüello E, Trilla A, Munguira ILB, López-Herce AJ, Cotarelo Suárez M. Knowledge, attitudes, beliefs and barriers of healthcare professionals and adults ≥ 65 years about vaccine-preventable diseases in Spain: the ADult Vaccination drIverS and barriErs (ADVISE) study. Hum. Vaccines Immunother. 2022, 18, 2025007. [CrossRef] [PubMed]
- Fernández-Villa T, Molina AJ, Torner N, Castilla J, Astray J, García-Gutiérrez S, et al. Factors associated with acceptance of pandemic flu vaccine by healthcare professionals in Spain, 2009-2010. Res Nurs Health 2017, 40, 435–443. [CrossRef]
- Jiménez-Trujillo I, Jiménez-García R, Hernández-Barrera V, López-de Andrés A, del Barrio-Fernández JL, Carrasco-Garrido P, et al. Cobertura y predictores de vacunación contra la gripe en adultos con diabetes en Madrid. Vacunas 2008, 9, 102–107. [CrossRef]
- Chandeying N, Thongseiratch T. Systematic review and meta-analysis comparing educational and reminder digital interventions for promoting HPV vaccination uptake. Npj Digit. Med. 2023, 6, 162. [CrossRef]
- Tuckerman J, Harper K, Sullivan TR, Cuthbert AR, Fereday J, Couper J, et al. Short Message Service Reminder Nudge for Parents and Influenza Vaccination Uptake in Children and Adolescents With Special Risk Medical Conditions: The Flutext-4U Randomized Clinical Trial. JAMA Pediatr. 2023, 177, 337. [CrossRef]
- Wijesundara JG, Ito Fukunaga M, Ogarek J, Barton B, Fisher L, Preusse P, et al. Electronic Health Record Portal Messages and Interactive Voice Response Calls to Improve Rates of Early Season Influenza Vaccination: Randomized Controlled Trial. J. Med. Internet Res. 2020, 22, e16373. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).