1. Introduction
Low back pain (LBP) is the most common health problem resulting in pain and disability [
1,
2], causing substantial economic losses to society [
2,
3]. According to the 2010 Global Burden of Disease Study, LBP is among the top ten diseases and injuries accounting for the highest number of disability-adjusted life years worldwide [
4]. LBP is usually defined as pain, muscle tension, or stiffness localised below the costal margin and above the inferior gluteal folds, with or without leg pain, also known as sciatica [
5]. Altered mechanical muscle properties in the lumbar myofascial region have been identified in individuals with chronic LBP [
6,
7]. A recent study reported higher quantified muscle tone and stiffness of the lumbar extensor myofascia and lower elasticity in older patients with chronic LBP [
8]. These parameters may be related to pain severity, increased exercise load [
9], and underlying pathologies and symptoms [
10].
Because severe LBP usually results in poor treatment outcomes and functional disabilities [
11], timely LBP management is crucial. LBP is difficult to treat solely with medical interventions because of the complex interplay of biological, psychological, and social factors at its onset and progression. There are over 50 potential therapies with the promise to relieve pain [
12,
13], lessen suffering, and offer a cure for LBP. However, reliable evidence exists for only a few of these therapies [
13]. Soft tissue massage is thought to improve physiological and clinical outcomes by providing symptomatic pain relief through physical and mental relaxation and by increasing the pain threshold via the release of endorphins [
12,
14]. The Gate Control Theory predicts that massaging a specific area stimulates large-diameter nerve fibres that have an inhibitory input to T cells. Reduced T cell activity (and conversely, excitatory input from small-diameter nerve [nociceptive] fibres) results in pain relief [
15]. Moreover, massage therapy may promote sympathetic responses in the autonomic nervous system [
16]. Massage is similar or superior in efficacy to other conservative therapies such as exercises, mobilisation, relaxation, physical therapy, acupuncture, and self-care education [
12]. A systematic review found that massage for nonspecific low back pain was more effective than a placebo and some active treatments (e.g., relaxation), especially in the short term [
17]. Another meta-analytic review study found that massage for subacute and chronic LBP was more effective than inactive controls for pain and function in the short term but not in the long term; however, when compared to active controls, massage was a better treatment for pain, both in the short- and long-term follow-up, with no differences in terms of function [
18]. However, manual massage can have inconsistent therapeutic effects depending on the skill of the practitioner and the amount of pressure applied and can be unreliable in terms of reproducibility. Furthermore, most of the effects of massage on LBP have been measured using subjective instruments such as pain and disability questionnaires; therefore, quantitative variables have not been used to elucidate the effects and mechanisms of massage [
17,
18].
Mechanical massage devices are often used to compensate for the limitations of manual massage. A systematic review showed that massage using both hands and a mechanical device was beneficial for patients with subacute and chronic nonspecific LBP, especially when combined with exercise and education [
19]. A technique frequently employed in mechanical massage devices is the rotating roller massage method with thermal therapy (RM-TH), which employs a massage roller that rotates and passes over the body. This massage technique, combined with heat, has been reported to be effective in reducing pain in patients with LBP [
20,
21]. A recent study indicated that both conventional physiotherapy and RM-TH decreased pain, disability, and electromyography levels, and that the RM-TH exhibited a greater increase in maximal voluntary isometric contraction than did the physiotherapy group [
20]. Another study using a rolling chair apparatus revealed that a massage device had a significant effect on pain, satisfaction, and quality of life; however, conventional physiotherapy was more effective in alleviating pain and improving quality of life [
21]. Although RM-TH is a straightforward and prevalent technique employed in massage devices for LBP, manual therapy may be a more precise method for stimulating specific muscles. In addition, it is noteworthy that roller massage devices may cause discomfort and potential injury owing to the physical friction of the rollers. A supplementary methodology was recently developed to address the limitations of RM-TH. The mechanical sequential ascending massage method with thermal therapy (AM-TH) provides localised vertical upward pressure that is adjustable in height. The location of the stimulation can be adjusted to coincide with the location of nerve impulses in the cervical, thoracic, lumbar, and coccygeal spine. Consequently, the AM-TH device incorporates a mechanism designed to reduce pain by applying sequential and selective vertically ascending pressures to specific areas of each spinal region. It is expected that AM-TH will result in a reduction in pain via the application of precise acupressure at a more targeted spinal level; moreover, it is expected to improve the discomfort associated with friction against the body that has been observed in RM-TH.
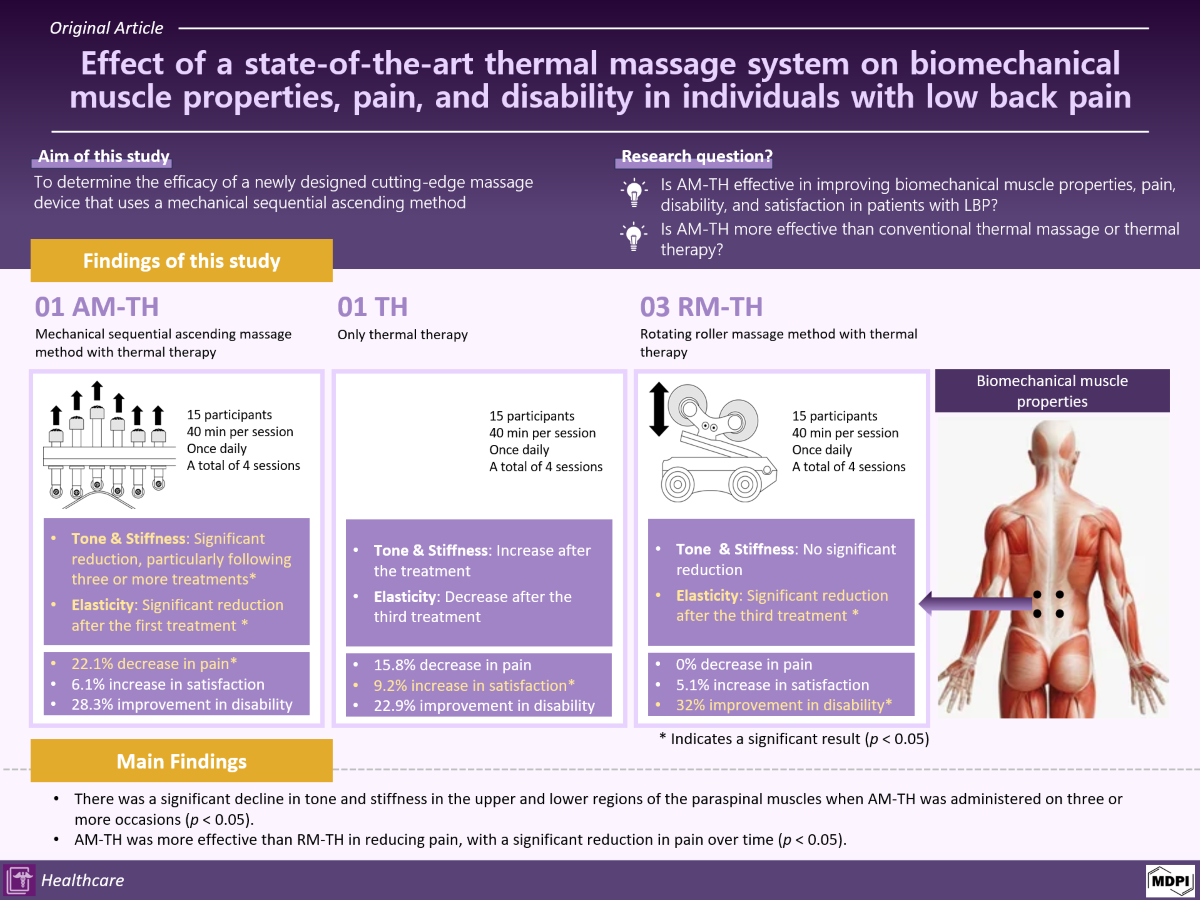
Therefore, this study aimed to investigate the efficacy of AM-TH therapy in alleviating pain in patients with LBP. It is hypothesised that AM-TH will be effective in improving biomechanical muscle properties, pain, disability, and satisfaction in patients with LBP. Besides, it has been postulated that AM-TH is more effective than RM-TH or thermal therapy in improving biomechanical muscle properties, pain, quality of life, and satisfaction.
2. Materials and Methods
2.1. Design
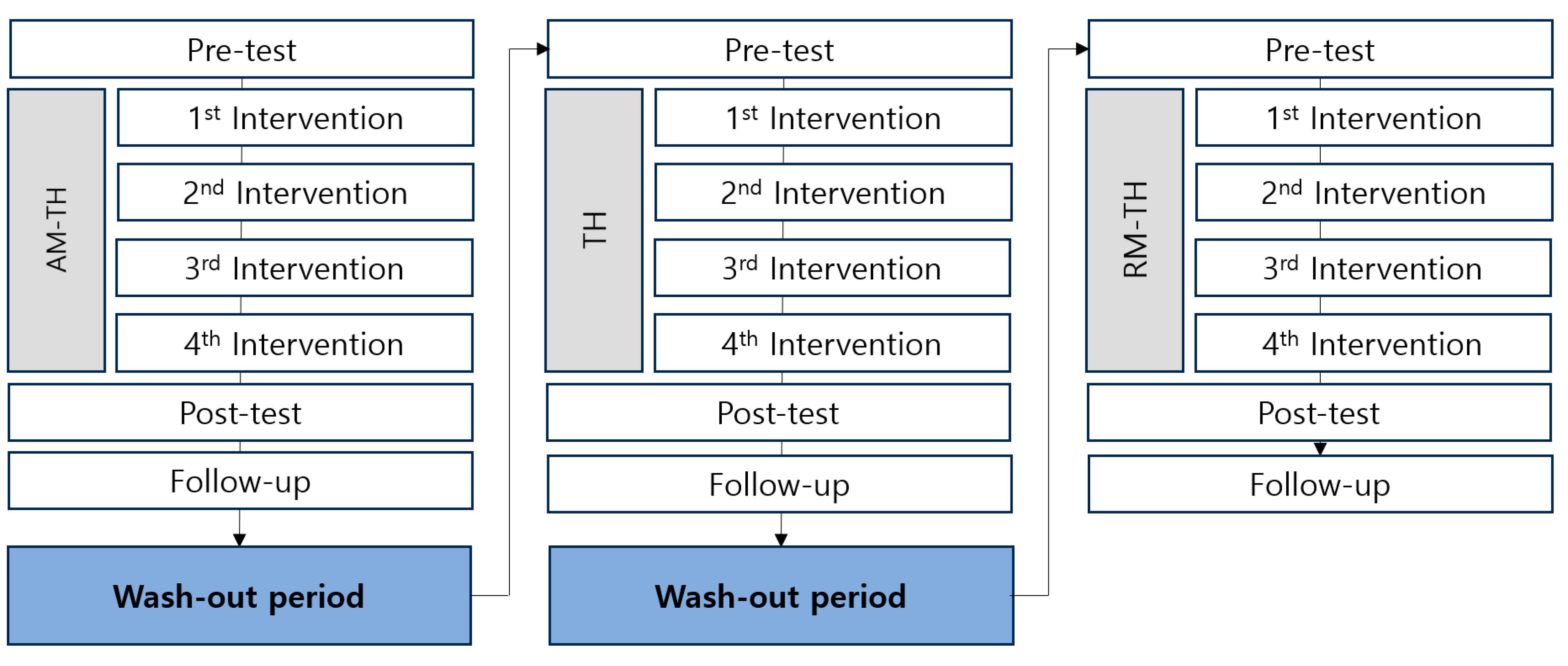
This was a single-centre, double-blind, sequential experimental group versus an active control group study involving 15 participants. All participants underwent three different interventions: AM-TH, thermal therapy (TH), and RM-TH. Each participant had a 2-week washout period before being assigned to the next intervention (
Figure 1). Neither the participants nor the assessors were aware of the distinction between the experimental and control groups.
2.2. Participants
Fifteen individuals with LBP were recruited from the outpatient clinics at Kyungpook National University Hospital to voluntarily participate in the study. All potential participants were provided with an information sheet and were asked questions regarding the study. Afterwards, a member of the research team conducted screening to confirm eligibility. The inclusion criteria were as follows: (1) age over 20 years; (2) persistent pain in the lumbar or lumbosacral region (between the T12 vertebrae and gluteal fold) without radiation to the legs for at least 6 weeks prior to enrolment; (3) ability to express pain and discomfort; and (4) no intervention for at least 4 weeks prior to enrolment. The exclusion criteria were as follows: (1) scoliosis; (2) history of fracture or surgery in the pelvic or spinal regions; (3) history of neurological conditions; (4) pregnancy; (5) presence of medical conditions other than chronic LBP; and (6) presence of a wound in the lumbar spine region at the time of data collection. The experimental protocol was approved by the Ethical Review Board of Kyungpook National University Hospital (Institutional Review Board number: 2022-04-026), and all participants provided written informed consent before participation. The study complied with the principles of the Declaration of Helsinki.
2.3. Biomechanical Properties Measurements of Low Back Muscles
A handheld myotonometer (MyotonPRO®, Estonia) was used to quantify biomechanical properties of the bilateral lumbar paraspinal muscles. Measurements were performed while the participants were lying prone on the assessment couch. Participants were asked to place their hands beside their heads and lie comfortably to achieve full relaxation. The test sites were marked as extensor muscle bulk prominences at the same level as each lumbar spinous process [
7]. The participants were asked to hold their breath for 5 s at the end of inspiration to minimise confounding factors resulting from changes in intra-abdominal pressure during natural respiratory cycles. The myotonometer testing probe was placed vertically on the skin surface on the belly of each tested muscle. First, the probe was loaded by pushing it against the skin surface to the required depth. Once the required depth was reached (indicated by a change in the indicator light from red to green), the device applied three short impulses (1 s apart) to induce damped oscillations within the muscle bulk. The oscillation pattern recorded by the transducer was used to calculate biomechanical muscle properties. The following biomechanical properties including muscle tone, stiffness, and elasticity at the bilateral L1 to L5 levels were recorded: muscle tone in upper left region (TUL), muscle tone in lower left region (TLL), muscle tone in upper right region (TUR), muscle tone in lower right region (TLR), muscle stiffness in upper left region (SUL), muscle stiffness in lower left region (SLL), muscle stiffness in upper right region (SUR), muscle stiffness in lower right region (SLR), muscle elasticity in upper left region (EUL), muscle elasticity in lower left region (ELL), muscle elasticity in upper right region (EUR), and muscle elasticity in lower right region (ELR). Muscle tone is defined as the degree of muscle tone when skeletal muscle is relaxed. Muscle contraction is the most significant and direct factor that affects muscle tone is muscle contraction [
22]. The damped oscillation frequency (Hz) represents the muscle tone at rest; the higher the damped oscillation frequency, the higher the muscle tone [
23,
24,
25]. Stiffness (N/m) refers to the ability of the muscles to resist contraction or external pressure and maintain their original shape [
25]. The higher the dynamic stiffness, the harder the muscle [
23,
25]. Elasticity is an indicator of the ability of muscles to return to their original state after being squeezed or contracted [
26]. The logarithmic decrement of the natural damped oscillation was measured to determine muscle elasticity. It is expressed only in numerical values and has no units [
24,
25]. The lower the logarithmic decrement, the smaller is the dissipation of mechanical energy and the greater is the elasticity. All muscle properties were measured before and after each intervention. The assessor received 3 h of training from a senior research physiotherapist with extensive experience in device operation.
2.4. Clinical Assessments
We measured pain and satisfaction immediately after each of the four treatment sessions for each device for a total of 12 sessions. In addition, we measured disability three times for each device (a total of nine times): before treatment, after four treatment sessions, and at follow-up. The COLDSPA was used to assess the participants' overall pain. The COLDSPA is a comprehensive mnemonic tool used for assessing the character, onset, location, duration, severity, pattern, and associated patterns of pain [
27]. Furthermore, the COLDSPA can be used to better understand how patients experience pain. A satisfaction survey was conducted immediately following each intervention. The survey consisted of the following seven items rated on a five-point scale: (1) overall satisfaction, (2) number of times, (3) time, (4) ease of use, (5) comfort, (6) heat level, and (7) pressure level. Disability was assessed using the Oswestry Disability Index (ODI) to understand how participants’ pain and daily activities were affected. The ODI is one of the most commonly used measures of disability in individuals with LBP [
28]. It is a self-administered questionnaire that requires 5 min to complete and 1 min to score. These scores are associated with the degree of disability, which may range from minimal to bedbound.
2.5. Interventions
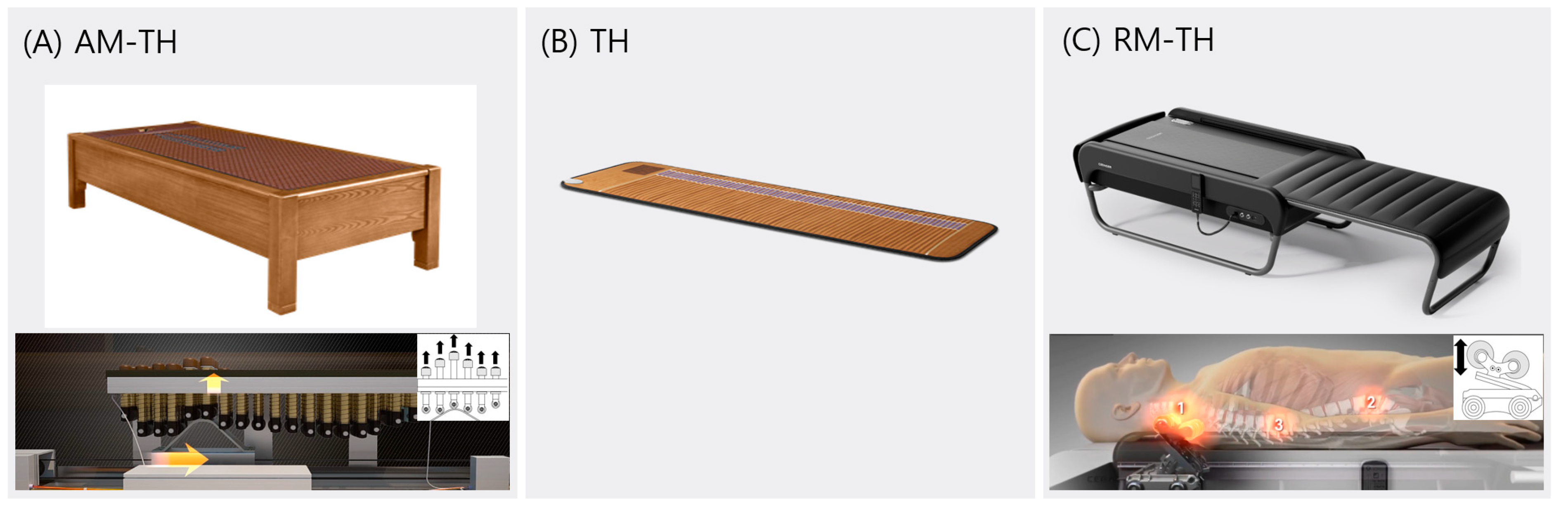
First, the participants received AM-TH with a thermal massage bed (3H-820 HP, 3H, South Korea). The AM-TH device employs a sequential mechanical ascending method that utilises ceramic upward and downward components. (
Figure 2). The bed comprised a heating wire, a heating plate, and individualised acupressure rods. The application of massage pressure from this device in both horizontal and vertical directions can be targeted to specific vertebrae, with each vertebra receiving localised and sequential treatment.
After a 2-week wash-out period, the participants received a second TH treatment using BioMat (BioMat, Richway, USA). BioMat is a natural heating pad that can be placed on a bed or table. It delivers soothing and deep-penetrating heat while stimulating the regeneration of damaged cells in the body. The temperature of the mat was maintained at a comfortable level for each participant, with a range of 45 to 50 °C.
After a 2-week wash-out period, the participants received a third RM-TH using a thermal massage device (CGM MB-1401; Ceragem, Seoul, South Korea). The massage bed was covered with tough synthetic fabric, and a massage roller (projector) moved beneath the fabric. The intervention was performed in the eighth mode (which provides acupressure, moxibustion, and rubbing along the spine). After the participant laid in the supine position on the device, a rolling projector protruded against the posterior aspect of the spinal column to scan its curvature along the sagittal plane from the cervical spine to the sacrum. These rollers applied heat and massage, while automatically adjusting the height of the protrusion, with reference to the curvature of the entire spine.
All interventions were conducted in a quiet environment with lights turned off. The participants received treatment for 40 min per session, once daily, for a total of four sessions per device. A 2-week wash-out period was allowed after the end of the use of one device before a second device was used.
2.6. Sample Size Analysis
The sample size was calculated as described in a previous study that identified immediate effects of massage instrument associated with low back pain [
29]. The calculation was based on the paired t-test value for within-group comparisons of disability assessed by ODI, which was performed using an acceptable level of significance of 0.05 at 95% power. The total sample size was nine for each group (expected effect size: 1.266; actual power: 0.964). Therefore, a total of 15 participants were recruited for the study, considering the power of analysis, variables, and a 40% adjustment for dropout rates during study conduct and missing values during analysis. The G∗ Power 3.1.9.2 program was used in this study.
2.7. Statistical Analysis
All statistical analyses were performed using SPSS software (version 22.0; IBM, Armonk, NY, USA). Descriptive statistics were used to calculate the mean and standard deviation of all the related data. The normal distribution of the baseline data was evaluated using the Kolmogorov–Smirnov and Shapiro–Wilk tests. The Wilcoxon signed-rank test was used to assess differences between time points within groups. The Mann–Whitney U test was employed to compare the pre- and post-difference ratio in muscle properties between treatments across different devices. The impact of time on pain, satisfaction, and disability was analysed using Friedman's one-way repeated-measures analysis of variance (ANOVA), a nonparametric test of repeated measures. Post-hoc analysis was conducted to assess the differences between time points within the groups using the Wilcoxon signed-rank test. The Mann–Whitney U test was used to analyse the differences between treatments for these three variables. All statistical significance levels were set at p < 0.05.
3. Results
3.1. Participants
Fifteen participants with LBP were enrolled in this study. The mean age of the cohort was 36.8 years old (six males and eight females). All the participants completed the experimental protocol. Numerical pain rating scale was 3–9 (mean 7.0 ± 1.6). The mean onset was 4.5 years and 20% of the participants had continuous pain (
Table 1).
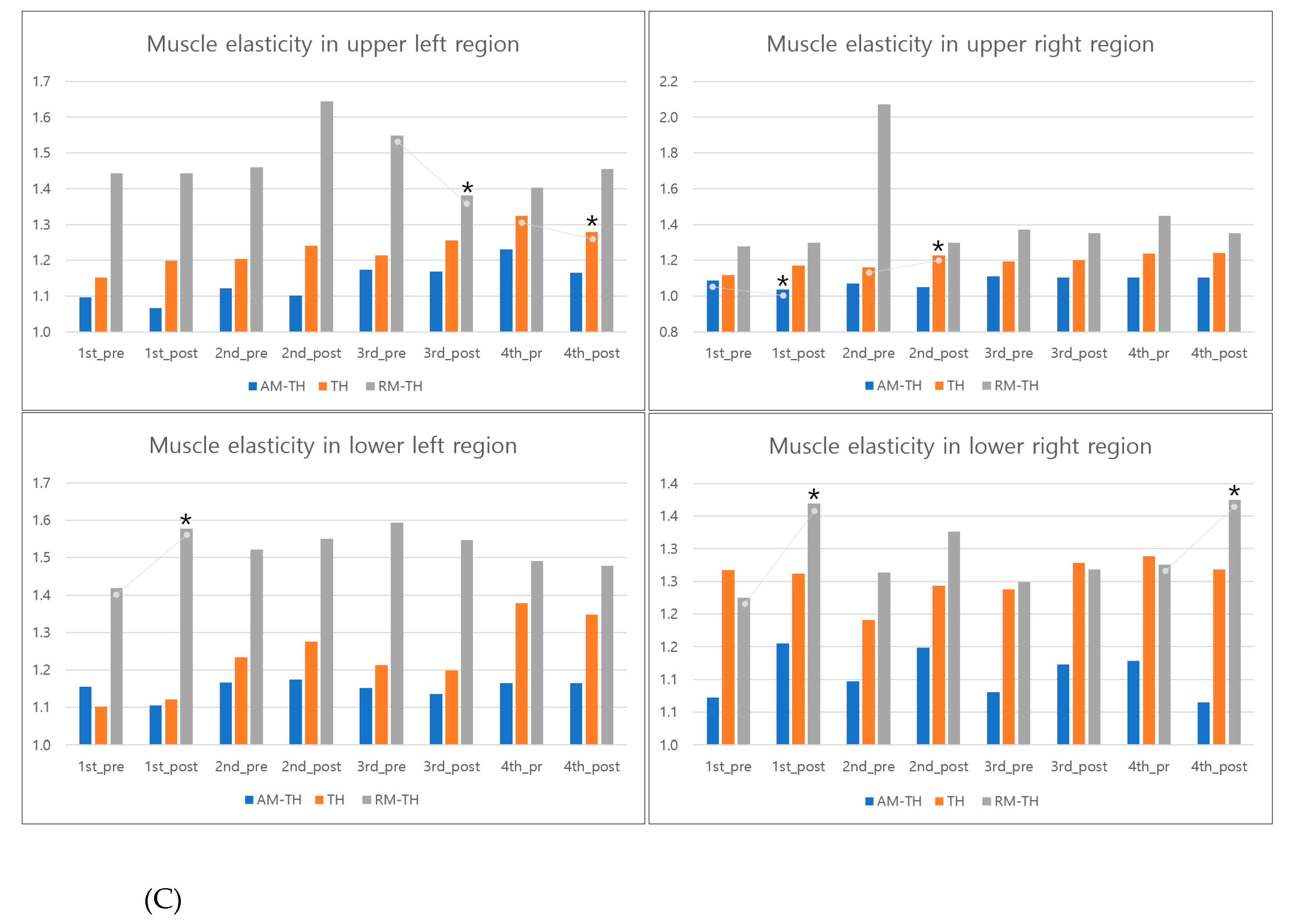
3.2. Comparison of Muscle Properties before and after Treatments
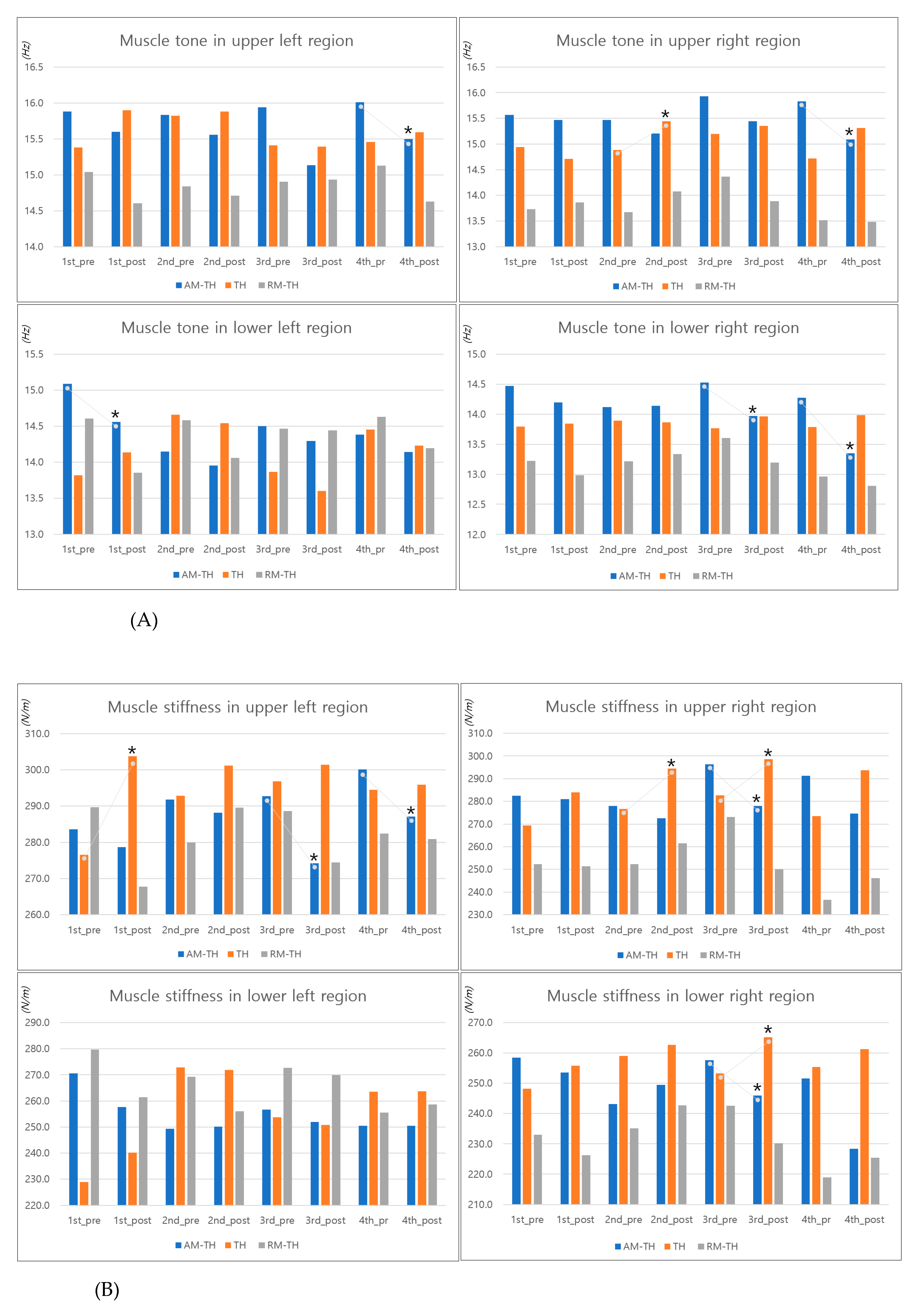
The specific values of the lower back muscle properties before and after treatment are presented in
Table 2 and
Figure 3. Participants who received AM-TH exhibited a consistent decline in muscle tone from the pre- to post-treatment period, accompanied by a significant decrease in TUL in the fourth session, TUR in the fourth session, TLL in the first session, and TLR in the third and fourth sessions (
p < 0.05). Those who received TH indicated that muscle tone appeared to increase or remain stable following treatment, compared with the state before treatment, accompanied by a significant increase in TUR in the second session (
p < 0.05).
Participants who underwent RM-TH exhibited a general trend towards a decrease in muscle tone after treatment, compared with the state before treatment, although the difference was not statistically significant.
Those who underwent AM-TH exhibited a tendency to have decreased muscle stiffness after treatment, compared to the state before treatment, accompanied by a significant decrease in SUL in the third and fourth sessions, SUR in the third session, and SLR in the third session (p < 0.05). Participants who received TH indicated that muscle stiffness appeared to increase following treatment, compared to the state before the session, accompanied by a significant increase in SUL in the first session, SUR in the second and third sessions, and SLR in the third session (p < 0.05). Patients who underwent RM-TH demonstrated a general reduction in muscle stiffness in the pre- and post-session comparisons; however, there were cases of increases.
The interpretation of muscle elasticity was based on the assumption that a smaller logarithmic decrement value presented in the table and graph would indicate greater elasticity [
24,
25]. Participants who underwent AM-TH exhibited a tendency for increased muscle elasticity after treatment, which was accompanied by a significant increase in EUR in the first session (
p < 0.05). Conversely, muscle elasticity tended to decrease in ELR. In the pre- and post-treatment comparisons, participants who received TH demonstrated a tendency for muscle elasticity to remain at similar levels or decrease, accompanied by a significant decrease in the EUR in second session (
p < 0.05). The results indicated that participants who underwent RM-TH exhibited increased muscle elasticity, although there was a tendency for muscle elasticity to decrease. In the RM-TH group, there was a significant increase in EUL in the third session and a significant decrease in ELL in the first session and in the ELR in the first session (
p < 0.05).
3.3. Comparison of Muscle Properties Difference Ratio by Treatment
The comparison of muscle property difference ratios showed that the TLL, SUL, SLL, and EUR in the first session, TUR and SUR in the second session, TUR, TLR, SUR, and SLR in the third session, and TUR and SUR in the fourth session were significantly different between AM-TH and TH. Furthermore, a comparison of AM-TH and RM-TH revealed that the EUR in the first session, EUL in the third session, and ELR of fourth session exhibited statistically significant differences. In addition, a comparison in TH and RM-TH indicated that the SUL in the first session, SUR and EUL in the second session, and the ELR in fourth session exhibited statistically significant differences.
3.4. Comparison of Pain, Satisfaction, and Disability
Table 3 shows the results of the Friedman’s repeated-measures ANOVA. Following four treatment sessions, participants in the AM-TH group exhibited a 22.1% decrease in pain (
p = 0.050). Overall reduction in pain was 15.8% (
p = 0.225) in the TH group and 0% (
p = 0.615) in the RM-TH group, with no significant differences. In addition, patients who underwent RM-TH had significantly less pain in the first session than did patients who underwent AM-TH. Following four treatment sessions, participants who underwent AM-TH exhibited a 6.1% increase in satisfaction (
p = 0.096). Furthermore, TH showed a 9.2% increase (
p = 0.015) and RM-TH showed a 5.1% increase (
p = 0.099) in satisfaction. Patients who underwent RM-TH were significantly more satisfied than were patients who underwent AM-TH in the first (
p = 0.023) and second sessions (
p = 0.037), and patients who underwent RM-TH were significantly more satisfied than were patients who underwent TH in the first (
p = 0.019), second (
p = 0.016) and fourth sessions (
p = 0.041). Participants who underwent AM-TH exhibited a 28.3% improvement in disability (
p = 0.099). In addition, patients who underwent TH exhibited a 22.9% improvement (
p = 0.517) and those who underwent RM-TH showed 32.0% improvement (
p < 0.001) in disability. There was no significant difference in the improvement in disability between the devices.
4. Discussion
The findings of this study revealed a significant decline in muscle tone and stiffness in the upper and lower regions of the paraspinal muscles when AM-TH was administered on three or more occasions (p < 0.05). Furthermore, there was a significant increase in the elasticity of the upper and lower regions of the paraspinal muscles after AM-TH and RM-TH administration (p < 0.05), followed by a decrease after treatment. AM-TH was more effective than RM-TH in reducing pain in our study participants, with a significant reduction in pain over time (p < 0.05). Participants were most satisfied with RM-TH, and over time, RM-TH was effective in improving their disabilities (p < 0.05).
We investigated the effectiveness of three different thermal massage devices in improving lower back muscle properties, pain, and disability in patients with LBP. We specifically aimed to examine the immediate effects of a recently developed massage device that utilises a novel mechanical sequential ascending method on biomechanical muscle properties associated with pain. The findings of the study can be interpreted in three ways. The first is the immediate effects of lower back muscle properties following thermal massage device treatment and their association with pain. The relatively high prevalence of chronic LBP and persistent symptoms (4.2–25.4%) [
30] may be related to changes in structural and neuromuscular properties. A transition from type I to type II muscle fibres of the back muscle has been observed in individuals with LBP [
31]. Given that type II fibres are less fatigue-resistant, it is possible that these muscles may exhibit higher levels of fatigue throughout daily activities. Consequently, type II fibre fatigue in individuals with LBP may result in increased muscle stiffness. A recent meta-analysis review demonstrated that individuals with LBP have higher stiffness of the multifidus and erector spinae at rest than do asymptomatic controls [
32]. In patients with chronic LBP, muscle tone and stiffness were greater than that in healthy people of the same age [
7,
33]. Moreover, the elasticity of the bilateral lumbar extensor myofascia was lower than that of healthy controls [
8]. In the present study, TH did not result in an immediate improvement in muscle properties; however, the massage device with TH was effective. In particular, the AM-TH group demonstrated a significant reduction in immediate muscle tone and stiffness when the intervention was applied three or more times (
p < 0.05). Furthermore, there was a significant increase in the elasticity of the upper regions of the paraspinal muscles after AM-TH administration (
p < 0.05). This indicates that the thermal massage device, which precisely stimulates the appropriate back muscles at different spinal levels, has a significant effect on the structural changes in back muscle properties. Furthermore, AM-TH, which significantly reduced muscle tone and stiffness, significantly reduced pain over time (
p = 0.050). It is unclear whether this reduction in muscle tone and stiffness is the result of an improvement in pain or vice versa. Nevertheless, these results indicate a potential possibility for considering muscle properties in the management of low back pain.
Second, pain relief and functional improvement were achieved over time with the use of a massage device. This study employed a device that integrated thermal therapy and spinal massage with thermal therapy for LBP management. Thermal therapy is usually used to enhance blood circulation and oxygenation of damaged tissues, thereby reducing chronic joint and muscle pain. A review demonstrated that continuous, low-level heat therapy provides pain relief, improves muscular strength, and increases flexibility [
34]. These heat modalities act at different depths with the collective action of reducing muscle tone, increasing blood flow, and relieving pain [
35]. However, TH did not improve muscle properties in this study. Moreover, TH and RM-TH resulted in a gradual, but insignificant, reduction in pain. This may be related to the insufficient number of interventions or the order in which the interventions were administered. Pain levels progressively decreased from the first to the third intervention. In a previous study, 31 participants with LBP were treated with a thermal massage program using the massage rolling technique for 40 min, five times a week for 2 months; this treatment improved pain, disability index, and quality of life [
36]. Although the results of this study cannot definitively elucidate the effect of the intervention on pain relief, AM-TH delivered via a thermospinal massage device may be effective in reducing pain. Patients with Parkinson's disease and chronic pain who received 10 sessions of acupressure thermal bed therapy showed a significant reduction in pain immediately after treatment and at follow-up, as well as significant improvements in balance, gait speed, and walking endurance [
37]. In the present study, the immediate improvements in muscle properties and pain associated with the AM-TH suggest that further interventions over a longer period may lead to improvements in functional outcomes and quality of life in individuals with LBP.
Third, satisfaction and functional improvement of the participants who used the massage device were assessed. The level of acupressure provided by AM-TH was determined to be more intense than that provided by other devices, with participants often reporting that it was painful. The assessment in the first session revealed that the AM-TH group exhibited considerably higher levels of pain and discomfort than did the RM-TH group. Nevertheless, some participants, such as athletic men, were content with the intensity of the AM-TH intervention. Additionally, the intensity of AM-TH may not have been particularly gentle initially; however, after the participants adjusted, it was more effective in reducing pain, and they felt more satisfied. It is well documented that thermal therapy represents a preferred and effective intervention for patients with LBP. This study found a significant increase in satisfaction over time after the use of TH. However, when compared to other devices that combine heat and massage, satisfaction with TH was lower. This indicates that user satisfaction may be contingent on specific treatment options, including the quantity and intensity of stimulation. RM-TH demonstrated the highest levels of posttreatment satisfaction, potentially owing to its user-friendliness. Interestingly, AM-TH was more effective in reducing pain, whereas RM-TH was more effective in reducing disability and improving patient satisfaction. These findings indicate that psychological factors such as satisfaction with the user's familiarity with the machine may influence functional improvement.
4.1. Limitations
This study had some limitations. First, the sample size was relatively small. Second, the four intervention sessions were too short to deliver full benefits of the massage device. Third, the order of application of the massage bed intervention was the same for all participants because of the lack of randomisation. Therefore, although there was a sufficient washout period, the possibility of residual effects of the previous treatment cannot be completely excluded, and a pure comparison of the experimental and control interventions cannot be expected. Therefore, a randomised controlled trial with a larger sample size is required in the future.
5. Conclusions
AM-TH, a newly designed cutting-edge massage device with a mechanical sequential ascending method, has been demonstrated to be effective in individuals with LBP, improving muscle tone and stiffness and reducing pain. Therefore, it may be employed as a treatment modality for LBP. The assessment of back muscle properties may present an opportunity to gain further insights into the changes in trunk mechanical properties associated with LBP and inform the development of more effective rehabilitation strategies. Furthermore, in future LBP management, it is important to consider the heterogeneous nature of LBP and the influence of psychological factors such as satisfaction.
Author Contributions
Conceptualization, D.A., J.L. and J.H.; methodology, H.C; validation, D.A., J.L. and J.H.; formal analysis, J.C.; investigation, H.C.; data curation, H.C.; writing—original draft preparation, J.C.; writing—review and editing, J.C. and D.A.; supervision, J.L. and J.H.; project administration, J.L. and J.H.; funding acquisition, J.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (IRB) of Kyungpook National University Hospital (IRB number: 2022-04-026; date of approval: 2022.05.20.).
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
Data are contained within the article.
Acknowledgments
The authors are grateful to all volunteer participants for their co-operation and participation in this study. This research was supported by the Daegu Metropolitan City and Daegu-Gyeongbuk Medical Innovation Foundation (K-MEDI hub) through the Comparative clinical trial-based regional medical industry capacity building program.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Prince, M.J.; Wu, F.; Guo, Y.; Robledo, L.M.G.; O'Donnell, M.; Sullivan, R.; Yusuf, S. The burden of disease in older people and implications for health policy and practice. Lancet 2015, 385, 549–562. [Google Scholar] [CrossRef]
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum 2012, 64, 2028–2037. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, J.; Jacobs, P.; Bell, N.R.; Klarenbach, S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can 2004, 20, 13–21. [Google Scholar]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef] [PubMed]
- Koes, B.W.; Van Tulder, M.; Thomas, S. Diagnosis and treatment of low back pain. BMJ 2006, 332, 1430–1434. [Google Scholar] [CrossRef]
- Haładaj, R.; Topol, M. Multiple impulse therapy in the assessment of paraspinal muscle tone in patients with low back pain. Ortop Traumatol Rehabil 2016, 18, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Nair, K.; Masi, A.T.; Andonian, B.J.; Barry, A.J.; Coates, B.A.; Dougherty, J.; Schaefer, E.; Henderson, J.; Kelly, J. Stiffness of resting lumbar myofascia in healthy young subjects quantified using a handheld myotonometer and concurrently with surface electromyography monitoring. J Bodyw Mov Ther 2016, 20, 388–396. [Google Scholar] [CrossRef]
- Wu, Z.; Zhu, Y.; Xu, W.; Liang, J.; Guan, Y.; Xu, X. Analysis of biomechanical properties of the lumbar extensor myofascia in elderly patients with chronic low back pain and that in healthy people. Biomed Res Int 2020, 2020, 7649157. [Google Scholar] [CrossRef]
- Kim, D.; Kim, S.; Jung, Y. Measurement of low back muscle characteristic change using MyotonPRO in a long-term driving; pilot study. Ergonomics Soc Korea 2015, 4, 592–598. [Google Scholar] [CrossRef]
- Kawchuk, G.N.; Kaigle, A.M.; Holm, S.H.; Fauvel, O.R.; Ekström, L.; Hansson, T. The diagnostic performance of vertebral displacement measurements derived from ultrasonic indentation in an in vivo model of degenerative disc disease. Spine 2001, 26, 1348–1355. [Google Scholar] [CrossRef]
- Docking, R.E.; Fleming, J.; Brayne, C.; Zhao, J.; Macfarlane, G.J.; Jones, G.T.; Cambridge City over-75s Cohort Study collaboration. Epidemiology of back pain in older adults: prevalence and risk factors for back pain onset. Rheumatology 2011, 50, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Imamura, M.; Dryden, T.; Irvin, E. Massage for low back pain: an updated systematic review within the framework of the Cochrane Back Review Group. Spine 2009, 34, 1669–1684. [Google Scholar] [CrossRef] [PubMed]
- Van Tulder, M.W.; Koes, B.W.; Bouter, LM. Conservative treatment of acute and chronic nonspecific low back pain: a systematic review of randomized controlled trials of the most common interventions. Spine 1997, 22, 2128–2156. [Google Scholar] [CrossRef] [PubMed]
- Ernst, E. Massage therapy for low back pain: a systematic review. J Pain Symptom Manage 1999, 17, 65–69. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P.D. The challenge of pain. Penguin Books: London, United Kingdom, 1988.
- Moyer, C.A.; Rounds, J.; Hannum, J.W. A meta-analysis of massage therapy research. Psychol Bull 2004, 130, 3–18. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Beaton, K.; Hughes, T. The effectiveness of massage therapy for the treatment of nonspecific low back pain: a systematic review of systematic reviews. Int J Gen Med 2013, 6, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Giraldo, M.; Baskwill, A.; Irvin, E.; Imamura, M. Massage for low-back pain. Cochrane Database Syst Rev 2015, 2015, CD001929. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Brosseau, L.; Imamura, M.; Irvin, E. Massage for low-back pain: a systematic review within the framework of the Cochrane Collaboration Back Review Group. Spine 2002, 27, 1896–1910. [Google Scholar] [CrossRef]
- Kim, T.H.; Park, S.K.; Cho, I.Y.; Lee, J.H.; Jang, H.Y.; Yoon, Y.S. Substantiating the therapeutic effects of simultaneous heat massage combined with conventional physical therapy for treatment of lower back pain: a randomized controlled feasibility trial. Healthcare 2023, 11, 991. [Google Scholar] [CrossRef]
- Kim, S.K.; Min, A.; Jeon, C.; Kim, T.; Cho, S.; Lee, S.C.; Lee, C.K. Clinical outcomes and cost-effectiveness of massage chair therapy versus basic physiotherapy in lower back pain patients: A randomized controlled trial. Medicine 2020, 99, e19514. [Google Scholar] [CrossRef]
- Gjelsvik, B.E.B.; Syre, L. The Bobath concept in adult neurology. Thieme: Stuttgart, Germany, 2008.
- Gavronski, G.; Veraksitš, A.; Vasar, E.; Maaroos, J. Evaluation of viscoelastic parameters of the skeletal muscles in junior triathletes. Physiol Meas 2007, 28, 625–637. [Google Scholar] [CrossRef] [PubMed]
- Van Deun, B.; Hobbelen, J.S.; Cagnie, B.; Van Eetvelde, B.; Van Den Noortgate, N.; Cambier, D. Reproducible measurements of muscle characteristics using the MyotonPRO device: comparison between individuals with and without paratonia. J Geriatr Phys Ther 2018, 41, 194–203. [Google Scholar] [CrossRef]
- Schneider, S.; Peipsi, A.; Stokes, M.; Knicker, A.; Abeln, V. Feasibility of monitoring muscle health in microgravity environments using Myoton technology. Med Biol Eng Comput 2015, 53, 57–66. [Google Scholar] [CrossRef]
- Bailey, L.; Samuel, D.; Warner, M.; Stokes, M. Parameters representing muscle tone, elasticity and stiffness of biceps brachii in healthy older males: symmetry and within-session reliability using the MyotonPRO. J Neurol Disord 2013, 1, 1–7. [Google Scholar] [CrossRef]
- Düzel, V.; Aytaç, N.; Öztunç, G. A study on the correlation between the nurses’ and patients’ postoperative pain assessments. Pain Manag Nurs 2013, 14, 126–132. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry disability index. Spine 2000, 25, 2940–2953. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.S.; Yu, K.P.; Lee, K.J.; Kwak, S.H.; Kim, J.Y. Development and application of a newly designed massage instrument for deep cross-friction massage in chronic non-specific low back pain. Ann Rehabil Med 2012, 36, 55. [Google Scholar] [CrossRef] [PubMed]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M.X. Prevalence of chronic low back pain: systematic review. Rev Saude Publica 2015, 49, 1. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Weber, B.R.; Dvorak, J.; Grob, D.; Müntener, M. Fibre type characteristics of the lumbar paraspinal muscles in normal healthy subjects and in patients with low back pain. J Orthop Res 1997, 15, 881–887. [Google Scholar] [CrossRef]
- Vatovec, R.; Voglar, M. Changes of trunk muscle stiffness in individuals with low back pain: a systematic review with meta-analysis. BMC Musculoskelet Disord 2024, 25, 155. [Google Scholar] [CrossRef]
- Lohr, C.; Braumann, K.M.; Reer, R.; Schroeder, J.; Schmidt, T. Reliability of tensiomyography and myotonometry in detecting mechanical and contractile characteristics of the lumbar erector spinae in healthy volunteers. Eur J Appl Physiol 2018, 118, 1349–1359. [Google Scholar] [CrossRef]
- Freiwald, J.; Magni, A.; Fanlo-Mazas, P.; Paulino, E.; Sequeira de Medeiros, L.; Moretti, B.; Schleip, R.; Solarino, G. A role for superficial heat therapy in the management of non-specific, mild-to-moderate low back pain in current clinical practice: A narrative review. Life 2021, 11, 780. [Google Scholar] [CrossRef]
- Malanga, G.A.; Yan, N.; Stark, J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad Med 2015, 127, 57–65. [Google Scholar] [CrossRef]
- Yoon, Y.S.; Park, S.K.; Park, J.S.; Nam, S.Y.; Kim, K.E.; Cho, I.Y. A thermo-spinal massage program changes pain, recurrence rate, and quality of life in patients with low back pain. Int J Pharm Res 2019, 11, 1010–1018. [Google Scholar]
- Lee, S.J.; Lee, J.; Ahn, D.; Hwang, J.M. The effects of lumbar muscle myofascial release technique in Parkinson’s disease with chronic pain: a pilot experimental study. Int J Pain 2023, 14, 48–58. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).