1. Introduction
Robotic-assisted total knee arthroplasty (RA-TKA) has been increasingly adopted in orthopedic surgery, driven by its potential to enhance precision and improve patient outcomes. The use of robotic systems in surgery allows for more accurate implant positioning and alignment, potentially leading to better functional outcomes and longer implant longevity. Studies suggest long-term advantages of RA-TKA, including faster recovery and improved knee mobility [
1,
2,
3,
4]. Despite these benefits, the need for RA-TKA and its full benefits remain under discussion, particularly regarding cost-effectiveness and accessibility.
When evaluating RA-TKA, immediate postoperative benefits such as reduced complications, hospital costs, and shorter hospital stays are crucial. Knee arthroplasty is a common and financially impactful procedure, with 718,000 hospitalizations in the US in 2011 alone [
5,
6]. The economic burden associated with knee arthroplasty is significant, necessitating an evaluation of newer technologies like RA-TKA to determine their value in healthcare systems.
The number of TKAs has been rising and is projected to reach 3.48 million annually in the U.S. by 2030 [
7]. This increase is driven by an aging population, rising obesity rates, and higher patient expectations for mobility and quality of life. Despite advancements in TKA techniques and materials, up to 20% of patients remain dissatisfied postoperatively [
8,
9,
10]. This dissatisfaction is often due to persistent pain, limited function, and complications. Improvements in surgical precision, such as those offered by RA-TKA, may enhance outcomes and reduce these dissatisfaction rates.
The integration of robotic systems in TKA aims to minimize human error, improve reproducibility, and enhance the precision of bone cuts and implant positioning. By facilitating better alignment and balance of the knee joint, RA-TKA may lead to improved functional outcomes and patient satisfaction. However, the adoption of robotic technology in knee arthroplasty is associated with higher initial costs, which include the purchase and maintenance of robotic systems, as well as training for surgical teams [
11,
12,
13].
Research Questions
This study aims to address the following research questions: What are the demographic and clinical characteristics of patients undergoing RA-TKA? How has the adoption of RA-TKA changed from 2016 to 2019? What are the prevalence rates of comorbidities among patients undergoing RA-TKA? What are the trends in total cost and length of stay (LOS) for patients undergoing RA-TKA?
2. Methods
Data Source
This study utilized the Nationwide Inpatient Sample (NIS), the largest publicly available all-payer inpatient care database in the United States. The dataset comprised 88,415 RA-TKA cases from January 1, 2016, to December 31, 2019.
Patient Identification and Exclusions
RA-TKA procedures were identified using specific ICD-10-PCS codes. Clinical outcomes, including in-hospital mortality, length of stay, complications, and hospitalization costs, were analyzed.
Outcome Measures
RA-TKA procedures were identified using specific ICD-10-PCS codes. Clinical outcomes, including in-hospital mortality, length of stay,, and hospitalization costs, were analyzed.
Ethical Considerations
The study was conducted under exempt status granted by the institutional review board, and the requirement for informed consent was waived due to the de-identified nature of the NIS dataset.
3. Results
Demographics of Cohort Population
The demographic analysis of the RA-TKA cohort is summarized in
Table 1. The average age of RA-TKA patients was 66.2 ± 9.46 years. The gender distribution showed that 58.8% of the patients were female. Payer distribution indicated that 54.4% were covered by Medicare, 3.1% by Medicaid, 38.2% by private insurance, and 4.2% by other sources, including self-pay.
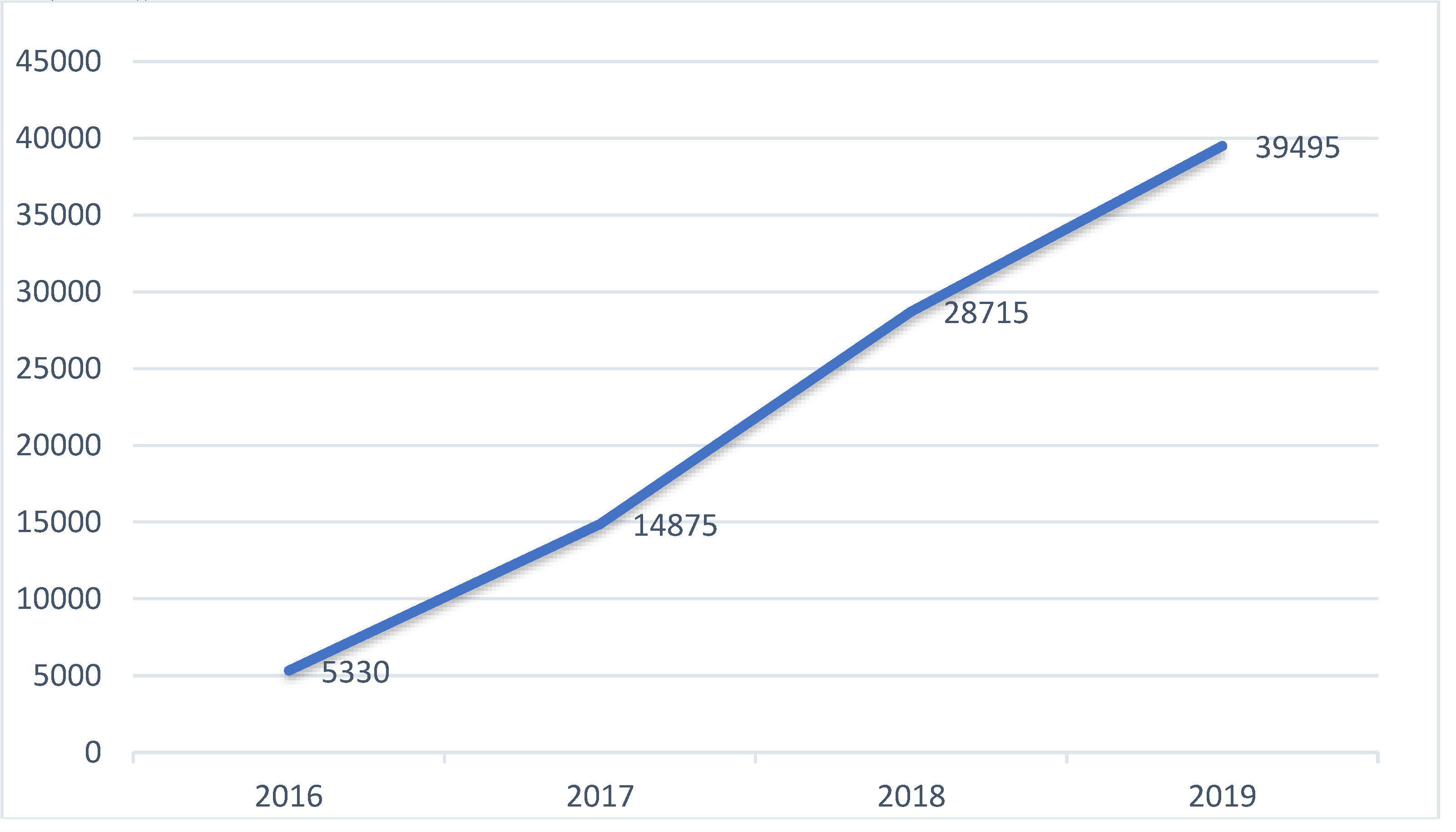
Trend Analysis of RA-TKA Procedures by Year
The trend analysis revealed a significant increase in RA-TKA procedures from 2016 to 2019. In 2016, there were 5,330 RA-TKA procedures, increasing to 39,495 by 2019. This demonstrates a growing adoption
Figure 1.
Trend Analysis of RA-TKA Procedures by Year.
Figure 1.
Trend Analysis of RA-TKA Procedures by Year.
Prevalence of Comorbidities in Patients Who Underwent RA-TKA
The prevalence of various comorbidities in the RA-TKA cohort is shown in
Table 2. The most common comorbidities included hypertension (57.6%), dyslipidemia (44.1%), and Type 2 diabetes (19.2%).
Race Distribution
The race distribution among RA-TKA patients is summarized in
Table 3. The majority of patients were White (83.8%), followed by Black (6.2%), Hispanic (5.3%), and other races.
Median Household Income National Quartile for Patient ZIP Code
The distribution of median household income for RA-TKA patients is shown in
Table 4. Patients were evenly distributed across income quartiles.
Location/Teaching Status of Hospital
The distribution of hospital location and teaching status for RA-TKA procedures is shown in
Table 5. The majority of procedures were performed in urban teaching hospitals (61.0%).
Total Cost and Length of Stay (LOS)
The average length of stay for patients undergoing RA-TKA was 1.89 days, with an average total cost of $65,891.
4. Discussion
The study found that RA-TKA has seen significant growth from 2016 to 2019. The demographic analysis shows that the majority of patients are White, covered by Medicare, and treated in urban teaching hospitals. The prevalence of common comorbidities and the associated costs and length of stay were also detailed.
The trends indicate a shift towards the adoption of robotic technology in knee arthroplasty, likely driven by the potential benefits of enhanced precision and better clinical outcomes [
14,
15]. Despite the higher initial costs, RA-TKA may be cost-effective in the long term due to reduced postoperative complications and shorter hospital stays [
16,
17]. The reduced length of stay can alleviate bed occupancy pressures in hospitals and decrease the risk of hospital-acquired infections [
18].
Furthermore, the study highlights that RA-TKA patients tend to be younger, which may reflect a preference for using advanced technology in patients with potentially longer life expectancy and higher activity demands. The lower prevalence of certain comorbidities in the RA-TKA cohort suggests that this population may be healthier overall, which could contribute to the observed outcomes [
19,
20].
The distribution of RA-TKA procedures across different types of hospitals reveals that urban teaching hospitals are more likely to adopt this technology. This could be due to the higher availability of resources and specialized surgical teams in teaching hospitals [
21]. Additionally, the even distribution of median household income among RA-TKA patients indicates that this technology is accessible to a broad socioeconomic spectrum [
22].
However, several limitations exist in this study. The NIS dataset is limited to in-hospital data and does not capture long-term outcomes [
23,
24,
25,
26], which are crucial for evaluating the full impact of RA-TKA. Additionally, the retrospective nature of the study and reliance on administrative data may introduce coding errors and biases [
27,
28].
Despite these limitations, the study provides valuable insights into the adoption and impact of RA-TKA. As robotic technology continues to evolve, ongoing research and long-term follow-up studies are necessary to fully understand its benefits and cost-effectiveness in knee arthroplasty [
29,
30].
5. Conclusions
RA-TKA usage in the US has increased significantly from 2016 to 2019, with specific demographic and clinical patterns. The adoption of robotic technology in knee arthroplasty shows promising trends, with potential benefits in precision, reduced complications, and shorter hospital stays. Further studies on both short- and long-term outcomes of RA-TKA are needed to fully understand the benefits of this technology.
List of Abbreviations (A-Z)
| HCUP: Healthcare Cost and Utilization Project |
| ICD-10: International Classification of Diseases, 10th Revision |
| LOS: Length of Stay |
| NIS: Nationwide Inpatient Sample |
| SPSS: Statistical Package for the Social Sciences |
| TKA: Total knee Arthroplasty |
Ethical approval
The study was conducted under exempt status granted by the institutional review board, and the requirement for informed consent was waived due to the de-identified nature of the NIS dataset.
Acknowledgements
Irrelevant.
Conflict of interest
None.
References
- Ahmed I, et al. (2016). Total knee arthroplasty with an oxidised zirconium femoral component: ten-year survivorship analysis. Bone & Joint Journal, 98(1), 58-64.
- Hampp EL, et al. (2019). Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg, 32, 239.
- Sultan AA, et al. (2019). Robotic-arm assisted total knee arthroplasty more accurately restored the posterior condylar offset ratio and the insall-salvati index compared to the manual technique.
- Young SW, et al. (2022). A prospective randomised controlled trial of mechanical axis with soft tissue release balancing vs functional alignment with bony resection balancing in total knee replacement. Trials, 23(1), 580.
- Pfuntner A, et al. (2013). Most frequent procedures performed in US hospitals, 2010: Statistical Brief# 149.
- Weiss AJ, Elixhauser A (2014). Trends in operating room procedures in US hospitals, 2001–2011: Statistical Brief# 171.
- Dreyer HC, et al. (2013). Essential amino acid supplementation in patients following total knee arthroplasty. J Clin Invest, 123.
- Scott CEH, et al. (2017). Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone & Joint Journal, 99(8), 1037-1046.
- Luna IE, et al. (2017). Early patient-reported outcomes versus objective function after total hip and knee arthroplasty. Bone & Joint Journal, 99(9), 1167-1175.
- Sousa PL, et al. (2020). Robots in the operating room during hip and knee arthroplasty.
- Barbash GI, Glied SA (2010). New technology and health care costs–the case of robot-assisted surgery. N Engl J Med, 363, 701.
- Rodrigues Martins YM, et al. (2021). Robotic surgery costs: revealing the real villains. Int J Med Robot, 17, e2311.
- Pando A, et al. (2023). Robotic assistance in lumbar fusion surgery: trends and patterns from 2016–2019. Eur Spine J, 32, 1966–1972.
- Cool CL, et al. (2019). A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res, 8(5), 327-336.
- Fontalis A, et al. (2022). Inflammatory Response in Robotic-Arm-Assisted Versus Conventional Jig-Based TKA. J Bone Joint Surg Am, 104(21), 1905-1914.
- Khlopas A, et al. (2017). Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Soft Tissue Protection. Surg Technol Int, 30, 441-446.
- Khorgami Z, et al. (2019). The cost of robotics: an analysis of the added costs of robotic-assisted versus laparoscopic surgery using the National inpatient sample. Surg Endosc, 33, 2217–2221.
- Shen TS, et al. (2023). Reasons and Risk Factors for Failed Same-Day Discharge After Primary Total Knee Arthroplasty. J Arthroplasty, 38(4), 668-672.
- Pass HI (2010). Medical registries: continued attempts for robust quality data. J Thorac Oncol, 5, S198-199.
- Zhang J, et al. (2022). Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient-reported outcomes. Knee Surg Sports Traumatol Arthrosc, 30, 2677-2695.
- Kayani B, et al. (2018). Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty. J Arthroplasty, 33, 2496–2501.
- Thiengwittayaporn S, et al. (2021). Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve. Int Orthop, 45(11), 2851-2858.
- Maman, D. , Mahamid, A., Finkel, B. et al. Comparative evaluation of postoperative outcomes and expenditure between robotic and conventional single-level lumbar fusion surgery: a comprehensive analysis of nationwide inpatient sample data. Eur Spine J (2024). [CrossRef]
- Maman, D. , Laver, L., Becker, R., Mahamid, A. & Berkovich, Y. (2024) Robotic-assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: a national analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 1–7. [CrossRef]
- Maman, D. , Laver, L., Becker, R., Takrori, L., Mahamid, A., Finkel, B., Gan-Or, H.,Yonai, Y. & Berkovich, Y. (2024) Trends and Epidemiology in Robotic-Assisted Total Knee Arthroplasty: Reduced Complications and Shorter Hospital Stays. Knee Surgery, Sports Traumatology, Arthroscopy. [CrossRef]
- Maman, D.; Mahamid, A.; Yonai, Y.; Berkovich, Y. Comparing Complication Rates, Costs, and Length of Stay between Unicompartmental and Total Knee Arthroplasty: Insights from a Big Data Analysis Using the National Inpatient Sample Dataset. J. Clin. Med. 2024, 13, 3888. [Google Scholar] [CrossRef] [PubMed]
- Fontalis A, et al. (2022). Inflammatory Response in Robotic-Arm-Assisted Versus Conventional Jig-Based TKA. J Bone Joint Surg Am, 104(21), 1905-1914.
- Khlopas A, et al. (2017). Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Soft Tissue Protection. Surg Technol Int, 30, 441-446.
- Pando A, et al. (2023). Robotic assistance in lumbar fusion surgery: trends and patterns from 2016–2019. Eur Spine J, 32, 1966–1972.
- Khorgami Z, et al. (2019). The cost of robotics: an analysis of the added costs of robotic-assisted versus laparoscopic surgery using the National inpatient sample. Surg Endosc, 33, 2217–2221.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).