1. Introduction
Temporomandibular disorders (TMD) encompass a variety of clinical issues related to the temporomandibular joint (TMJ), chewing muscles, and surrounding facial structures. These disorders, according to functional magnetic resonance studies, are thought to affect more than
5% of the population [
1].
Patients exhibiting TMD symptoms span a broad age spectrum, but the incidence is particularly high among individuals aged
20 to 40. Recent evidence suggests that TMD prevalence is on the rise, with about
31% of adults and
11% of children and adolescents affected [
1].
The connection between dental occlusion and TMD has been a contentious issue in the field of dentistry. Despite the effectiveness of the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) in diagnosing and categorizing TMD, some researchers have proposed using lateral cephalograms and cephalometric data to determine which morphological profiles and malocclusion types are most likely to trigger TMD.
Lateral cephalometry has been used since 1992 to explore the link between morphological features and TMJ disorders. More recently, the craniofacial morphology of TMD has been thoroughly examined using low-dose cone beam computed tomography (C.B.C.T.) [
2], revealing that TMD patients exhibit distinct craniofacial characteristics compared to those without TMD.
The goal of this study is to identify the morphological profiles and associated skeletal malocclusions that have the greatest impact on the development of TMD. This will be achieved through the analysis of cephalometric data derived from cephalograms and condylar section images of patients from the Orthognathodontics Department of Chieti, who underwent low-dose cbct during their initial visit.
2. Temporo-Mandibular Disorders (TMD)
Temporomandibular disorders (TMD) are a significant health concern, affecting approximately 5% to 12% of the population. TMD is the second most prevalent musculoskeletal condition, trailing only chronic back pain, and can result in pain and disability.
Studies by Lipton and others have demonstrated that while about 6% to 12% of the population exhibit clinical symptoms of TMD, only around 5% display substantial signs and symptoms that necessitate treatment.
TMD related to pain can impact daily activities, psychosocial functioning, and overall quality of life. Patients frequently seek dental advice for their condition, particularly when it is accompanied by pain.
For both clinical and research settings, there is a need for diagnostic criteria for TMD that provide simple, clear, reliable, and valid operational definitions for the clinical history, physical examination, and diagnostic tests. Additionally, it is crucial to evaluate pain-related behavior and psychosocial functioning, which are integral to the diagnostic process. This evaluation provides the minimum information necessary to determine if the patient’s pain disorder, especially if chronic, requires further multidisciplinary assessments. The new
Diagnostic Criteria for TMD (DC/TMD), which are evidence-based, will enable clinicians to assess patients and facilitate communication regarding consultations, referrals, and prognosis [
3].
As far back as 1992, efforts were made to establish a common language to assist clinicians in diagnosing and classifying various temporomandibular joint disorders, with or without pain. Initially, the focus was always on the physical and anatomical aspects of TMD, whether intra-articular or extra-articular (Axis I), without considering the social and psychological aspects of the patient.
Over time, it became apparent that TMD, especially when associated with pain, could also be influenced by the patient’s psychological state or by parafunctions related to stress or other psychological factors such as anxiety and depression. Conversely, pain could exacerbate the patient’s stress and discomfort in daily life.
This led to the introduction of the Axis II protocol, which is divided into sets of self-report screening and comprehensive tools. The screening tools, consisting of 41 questions, assess pain intensity, pain-related disability, psychological distress, functional limitations of the jaw, and parafunctional behaviors. A pain drawing is used to assess the locations of pain.
The comprehensive tools, consisting of 81 questions, provide a more detailed assessment of the functional limitations of the jaw and psychological distress, as well as additional constructs of anxiety and the presence of comorbid pain conditions.
Today, despite the development of various methods with diagnostic reliability and validity for diagnosing TMD, the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) remain the most widely used, accurate, and comprehensive diagnostic criteria globally for evaluating and classifying TMD. These criteria consider both the characterization of the joint and muscle disease (Axis I) and psychosocial disability (Axis II).
2.1. Classification
Temporomandibular disorders (TMD) can be most effectively and educationally categorized as follows: (Dworkin 1992)[
3]
Group 1: Muscular disorders (most prevalent in the population)
Group 2: Disk displacements
Disk displacement with reduction (reduction refers to the recapture of the disk)
Disk displacement without reduction with limited opening
Disk displacement without reduction without limited opening
Group 3: Inflammatory and non-inflammatory diseases
In 1994, A. Modesti proposed a more clinical classification that would guide the practitioner in choosing therapy depending on whether it was of muscular or joint origin.
Type I: Muscular syndrome
Type II: Compressive syndrome with mild initial clicking
Type III: Compressive syndrome with pronounced clicking
Type IV: Blockage
Type V: Dislocation
2.2. Skeletal Malocclusion and TMD
Skeletal Class II and III malocclusions can have varying characteristics and can be multifactorial, resulting from both environmental and genetic factors. Class II skeletal malocclusion can be characterized by a hypomandibular condition or lack of breastfeeding, spoiled habits such as prolonged use of a pacifier, bottle, and finger sucking (these factors could lead to the development of such skeletal malocclusion if the spoiled habit is not corrected), or genetics. Another component can be a repositioned mandible, always influenced by such spoiled habits. Conversely, there can be an excessive advancement of the maxilla.
Studies by McNamara in 1891 revealed that 2/3 of the 277 children analyzed had a normopositioned maxilla, 10% presented a maxillary protrusion, but about 25% even a retrusion. In conclusion, in most cases, the maxilla is normally positioned. About the mandible, 60% showed the mandible in a retruded position, both taking as a reference the cranial base and the distance of the pog point and the line passing through the Nasion perpendicular to FH. In conclusion, the second malocclusion is often caused by a repositioned mandible.
For Class III, the situation is different; the genetic component can be predominant. A study by MC Namara showed that 20% of children had mandibular prognathism, and 25% had maxillary retrusion. This suggests that genetic factors can play a significant role in the development of Class III malocclusions [
4,
5].
Furthermore, a difference has been observed in the more open gonial angle, larger mandibular angle, increased mandibular length, and dentoalveolar compensations compared to Class I subjects.
In conclusion, Class III skeletal malocclusion involves a wide range of variables and dental and skeletal characteristics that need to be well diagnosed and distinguished in order to carry out correct therapy. This highlights the importance of a comprehensive and detailed examination for each individual patient. Few studies have investigated the structural dentofacial and orthodontic relationships related to temporomandibular joint (TMJ) disorders.
One research paper indicates that certain dentofacial and orthodontic traits may be linked with the displacement of the TMJ disc, potentially influencing the risk of developing temporomandibular disorders. This study, [
6] delves into these connections.
Another research, led by Chung-Ju Hwang and team, centers on the lateral cephalometric features in patients with malocclusion who exhibit symptoms related to temporomandibular joint disorders.
Specific facial structures, such as hyperdivergence or skeletal Class II and III malocclusions, could play a role in the emergence of temporomandibular disorders and their associated symptoms.
Moreover, Chung-Ju Hwang and his team suggest a distinct classification system for TMJ disorders, incorporating significant and clinically pertinent characteristics.
Cluster analysis, an unsupervised learning model frequently employed in data mining, aids in identifying subtypes of various diseases based on numerous indicators, including idiopathic inflammatory myositis and Class III malocclusion [
7].
3. Matherials and Methods
3.1. Sample and Study Model
The study was carried out in the orthognathodontics department of Gabriele D’Annunzio University in Chieti. A group of 67 patients (comprising both males and females) who came to the orthognathodontics department at Gabriele D’Annunzio University in Chieti for their initial orthognathic consultation were examined. All these patients showed signs of temporomandibular joint disorders, as diagnosed during their first visit through a comprehensive gnathological history, VAS (visual analogue scale), and finally palpation, by Professor Felice Festa and the specialists of the orthognathodontics department at the University of Chieti.
The criteria for inclusion in the study were as follows: (a) patients being diagnosed with TMD for the first time; (b) patients aged 18 and above; (c) patients with accessible medical records, wide field of view cone beam low dosage, and photographs.
The criteria for exclusion from the study were: (a) presence of a tumor, trauma and/or history of surgical interventions in the jaw and facial area; (b) presence of fractures and other craniofacial anomalies.
3.2. Cone Beam and Low-Dose Protocol
All telecranius were obtained from the 2D lateral section of the wide FOV low-dose cone beam that every patient undergoes before the final evaluation by Professor Felice Festa. This appears to be related to a medical imaging technique used in dentistry123. The low-dose protocol is crucial for reducing the patient’s radiation dose [
2].
The low-dose CBCT protocol with a wide FOV, normal-resolution images, 80 kVp, 5 mA, and a 15-second acquisition time resulted in an effective dose value of 35 microSieverts (μSv). This protocol allows for high-quality imaging of the maxillofacial region with very low radiation exposure. Therefore, it could be proposed in selected cases where a comprehensive evaluation of the dental and maxillofacial region is beneficial for orthodontic treatment planning [
2].
3.3. Extraction Data
For the study, telecranius of 67 patients (44 female and 23 male), who had undergone low-dose cone beam computed tomography (CBCT) in the orthodontics department of Chieti during their initial visit were selected. The patient’s CBCT is performed with the head oriented according to the Natural Head Position (NHP). The patient is seated with their back as perpendicular to the floor as possible. The head is stabilized using ear rods placed in the external auditory meatus. The patient is asked to look into a mirror 1.5 meters in front of them to achieve the NHP and to keep their teeth in contact.
The NHP is a reproducible and physiologically determined position used for morphological analysis, as described in orthodontic and anthropological literature [
8]
After X-ray scanning, the Digital Imaging and Communications in Medicine (DICOM) image files are processed using Dolphin Imaging 3D software (Dolphin Imaging & Management Solutions, Chatsworth, CA) for storage and interpretation. Establishing a predefined orientation of the patient’s head is necessary to obtain predictable and repeatable three-dimensional (3D) analysis [
9].
The cranial image is then oriented according to the NHP in three perpendicular spatial planes:
The transverse plane coincides with the Frankfurt Horizontal Plane (FH), passing through two points: Orbitale (Or) and Porion (Po).
The sagittal plane coincides with the mid-sagittal plane (MSP), perpendicular to the FH plane and passing through two points: Crista Galli (Cg) and Basion (Ba).
The coronal plane coincides with the anteroposterior plane (PO), perpendicular to both the FH and MSP planes, passing through the right and left portions.
Following head orientation, various 2D virtual radiographs are extracted, including the lateral cephalogram, from which we derive the cephalometric data analysis.
4. Analysis of the morphological profile of patients with TMD through data from the telecranium and condylar sections.
For the study, 26 variables were investigated, of which 24 are cephalometric data derived from linear and angular measurements related to verticality and sagittality concerning bone bases, teeth, and soft tissues; the other 2 variables are age and sex. In [
Table 1], the average values of each cephalometric data obtained from the cephalometric study of the telecranius are reported.
Our study also considers gender as a variable, as previous studies have done. Literature suggests that women, due to hormonal fluctuations and menstrual cycles, are more prone to stress, muscle pain, and the onset of non-organic TMD with organic repercussions [
Table 1].
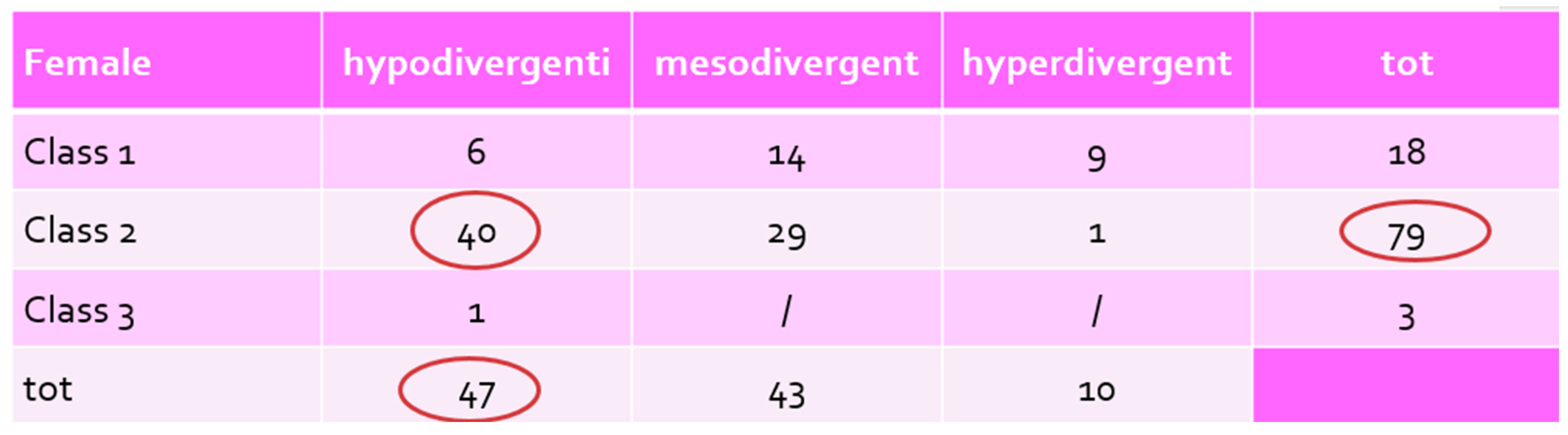
Subsequently, the morphology and position of the condyle of all patients were investigated, taking into account the divergence; thanks to the 3D and 2D sections obtained through the Dolphin software from the low-dose cone beam with a wide FOV; which allows measurements and investigation of anatomical structures at 360°.
Measurements of lengths and volumes in different planes are possible with 3D CBCT images, allowing precise diagnoses and predictability of treatment results [
10].
The position of the condyle was investigated through measurements made on the 2D sections obtained through the Dolphin software. All measurements of the condyle-fossa relationships were performed on the sagittal section passing through the midpoint of the distance between the medial and lateral poles of the condylar head, and perpendicular to the coronal plane. The images were then formatted and oriented according to the coronal and sagittal planes [
11].
The following were calculated: JSA (minimum anterior joint distance), SSP (minimum posterior joint distance), JSS (upper joint space). The concentricity of the condyle in the fossa was calculated using the following equation by Pullinger and Hollinder [
11]
Linear Ratio (LR) = (P-A) / (P+A) x 100 [
Figure 1].
Where: P – The closest posterior measurement; A – The closest anterior measurement
If LR<-12 – posterior position
If -12< LR<12 – concentric position
If LR>12 – anterior position [
12]
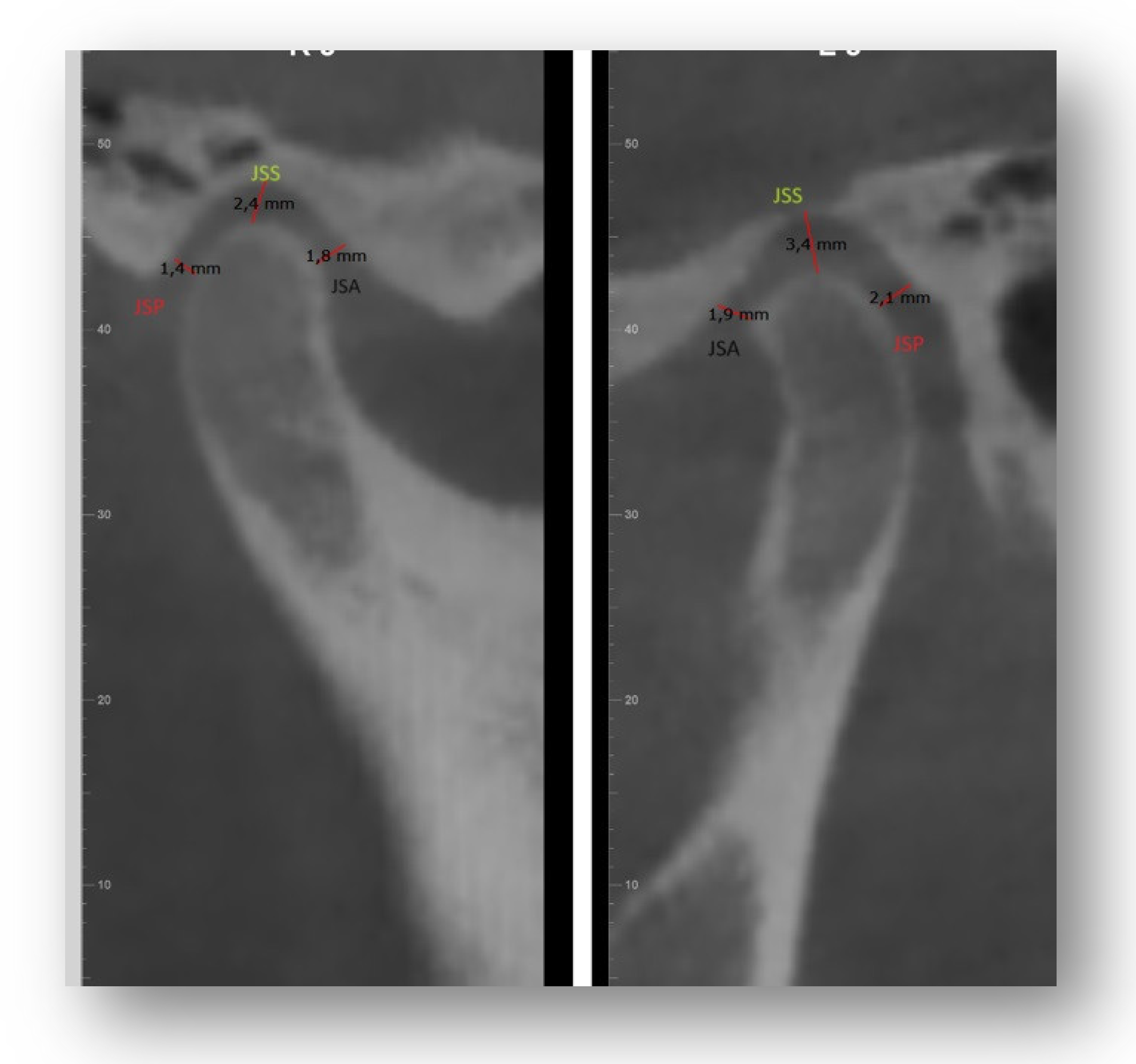
The condylar morphology was studied by observing the 3D sections of the cone beam.
The vertical distance between the deepest point of the fossa and the most prominent upper point of the mandibular condyle was also measured [
Figure 2]
A vertical distance of 1-4 mm was considered normal.
4 mm: condyle positioned inferiorly; <1mm: condyle positioned superiorly A value of 0 mm was indicated as bone contact.
5. Results
After acquiring the cephalometric data of 67 patients, these were divided based on sex (23 males, 44 females) and the averages of their respective cephalometric values were calculated [
Table 1].
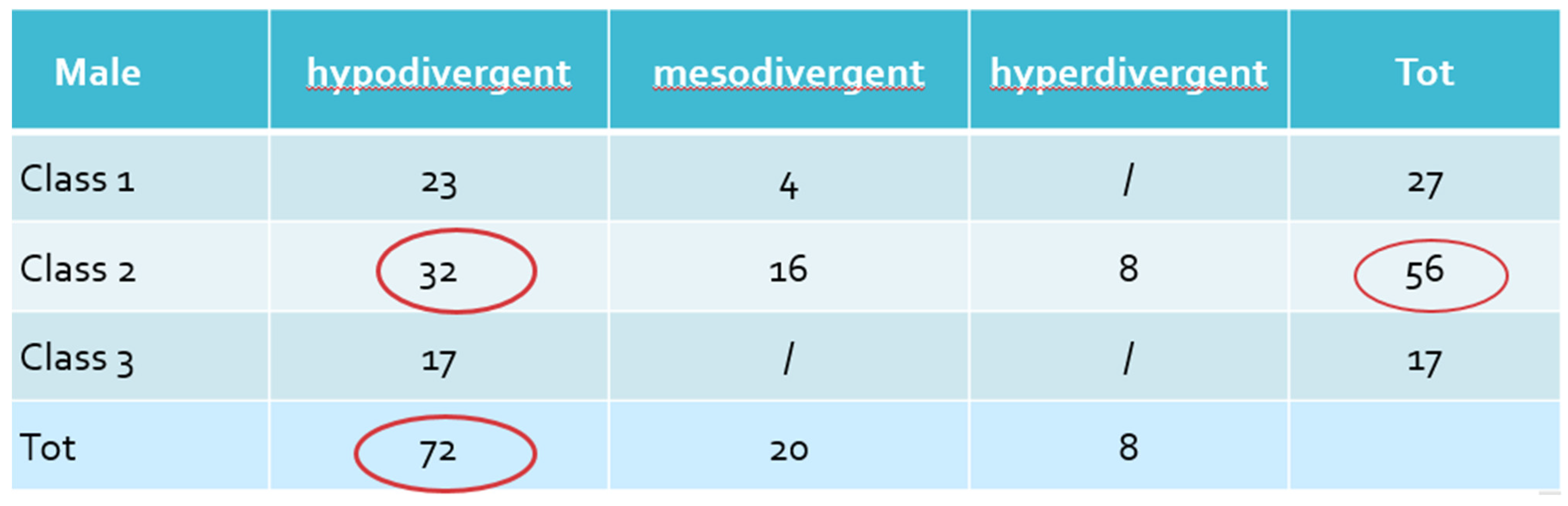
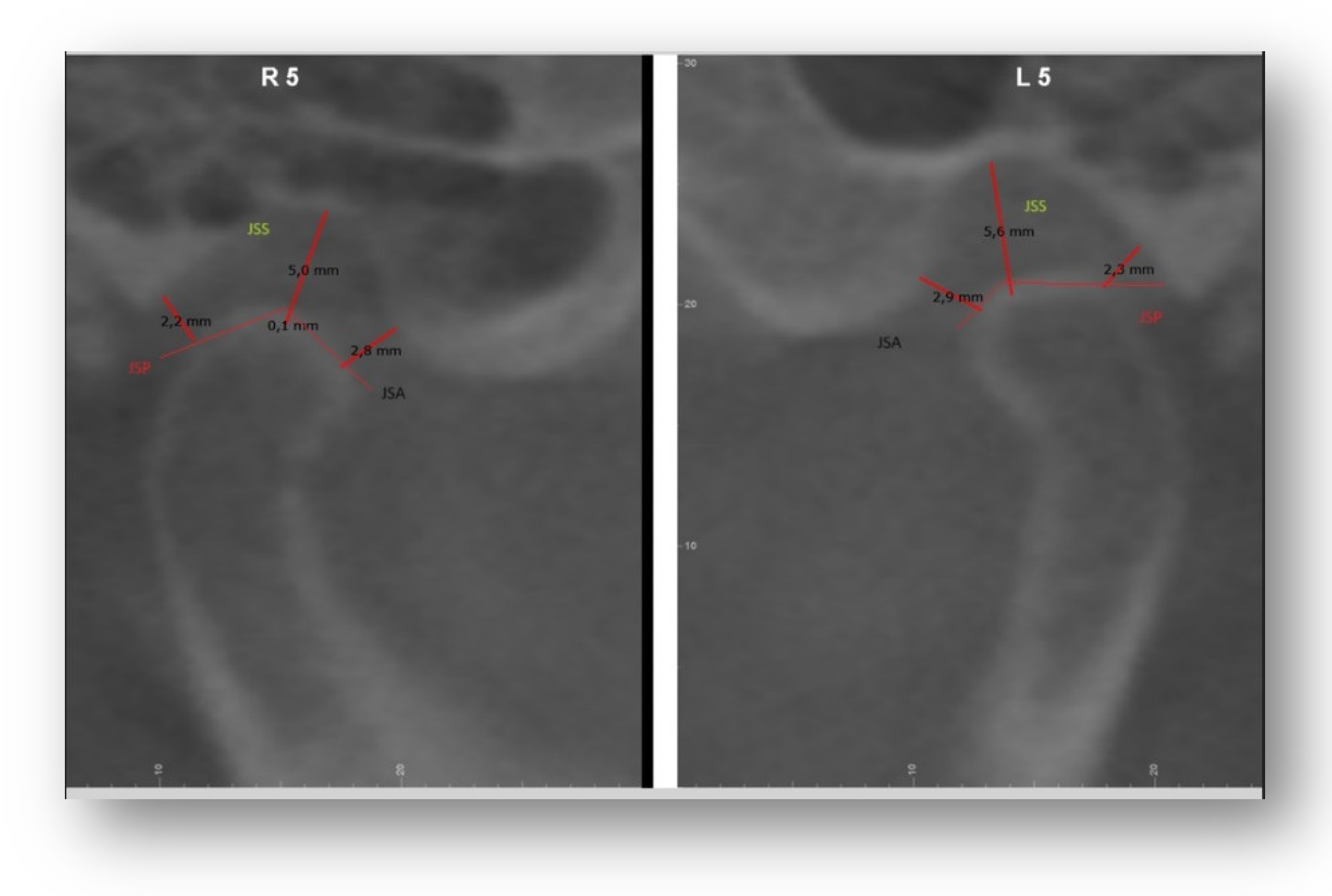
5.1. Male Patients
Regarding sagittality in male patients, there is a tendency towards a skeletal profile of Class II due to hypomandibulia and retrognathia in 56%: [
Table 2a]
The maxilla is in a normal position relative to the cranial base, as indicated by the SNA value (80.08°) which is within the norm.
The mandible is retro-positioned with an SNB value (73.89°) lower than the normal value (80°) and of reduced dimensions, as evidenced by the reduced length of the mandibular body (65.41mm).
The anterior and posterior cranial bases of these patients fall within the minimum limits of the norm.
Only 17% of male patients with TMD present a Class III skeletal profile and 27% a Class I skeletal profile.
In terms of divergence, 73% are brachyfacial and the average of the data tends towards a hypodivergent pattern, as demonstrated by the following values: [
Table 2a]
FMA (19°) is lower than the normal value (25°).
The saddle angle, the articular angle, and the gonial angle are reduced, indicating reduced growth of the mandible with an anticlockwise rotation and a hypodivergent model.
Also, the facial depth and anterior facial height are reduced, due to the reduced anterior vertical dimension.
Dental ratios show a tendency to deep bite with increased overjet and an open interincisal angle compared to the norm.
Of these patients who present a Class II brachyfacial profile, about 23% also have a deep dental bite; 20% of male patients are normodivergent and the remaining 8% are dolichofacial. The profile of the soft tissues is normal, with a tendency towards a flat profile.
5.2. Female Patients
Among female patients, 79% present a Class II skeletal profile: [
Table 2b]
The cephalometric data indicate a tendency towards mandibular retrognathia with an SNA of 81° (within the norm) therefore the maxilla is normally positioned.
SNB of about 74° therefore lower than the norm (80°), mandible retropositioned.
Also for female patients, the mandibular length is shorter compared to the average with a value of about 70 mm compared to the 79 mm that should be normal.
16% instead present a Class I skeletal profile with normally positioned maxilla and mandible; only 8% have a Class III with mandibular protrusion [
Table 1].
Regarding divergence, about 47% of patients are hypodivergent:
The cephalometric data indicate a reduced anterior facial height with an average value of 105° compared to the 130° that designate a normal facial height.
The articular angle and the gonial angle indicate a slight tendency towards a hypodivergent profile with anticlockwise rotation of the mandible; as well as the average angular values of the palatal plane (-1.58°) and the mandibular plane (27.58°) which are acute compared to the norm.
43% have a mesofacial profile, only 10% show a dolichofacial profile.
Dental ratios designate an increase in overbite and overjet and in fact, both among brachyfacial and mesofacial subjects, 17% present deep bite, and instead, 48% of female patients who present a Class II skeletal profile, present an increased overjet.
5.3. Condyle Position
Regarding the difference in condyle position and its relationships with the fossa, it was seen that men with Class II hypodivergent, has a non-concentric condyle position but it is more posterior compared to the center of the fossa, as also stated in the literature [
13].
In mesiodivergent male patients, it respects a position of concentricity and in hyperdivergent patient, as in women, it is positioned slightly more anterior compared to the center of the fossa [
Table 3a].
In skeletal Class I, it has almost a concentric position and only in hyperdivergent is it at the limit with the more anterior positioning.
In skeletal Class III, both hypodivergent and hyperdivergent tend to have an anterior positioning in the fossa.
There are no data regarding the first skeletal hyperdivergent classes and Class III mesiodivergent as there are no male patients in the study sample that present these morphological characteristics.
As for the distance between the highest point of the condyle head and the deepest point of the fossa, it is greater in hypodivergent where the condyle is located lower; it decreases instead in hyperdivergent where the condyle is located higher and forward [
Table 2a].
In women with Class II skeletal hypodivergent and normodivergent, there is not a great difference in positioning, as also stated in the literature [
13] the condyle is in a non-concentric position relative to the fossa and is located, in the analyzed patients in a more posterior position in the fossa both on the right and on the left [
Table 3b].
In agreement with the results of another study [
10], the position of the condyle and its highest point in the fossa is lower in hypodivergent women; in Class II hyperdivergent the condyle has a more anterior position in the fossa and higher [
Table 3°/b].
In Class III both hypodivergent and mesodivergent the condyle is in a more anterior position, as for the superior-inferior ratio there are no particular statistical differences but there is a tendency for hypodivergents to have both on the right and on the left the condyles lower in the fossa and for hyperdivergents the opposite tendency that is to have the condyles higher in the fossa.
6. Discussion
The temporomandibular joint (TMJ) is one of the most sophisticated anatomical elements in the human body, playing a significant role in dental practice.
The mandibular condyle, a fundamental component of the TMJ, directly impacts the stability of therapeutic outcomes in patients undergoing orthodontic, orthopedic, orthognathic surgery, and dental prosthetics treatments.
Consequently, during diagnosis and treatment, physicians should pay particular attention to the position and shape of the mandibular condyle and the patient’s skeletal morphology.
Despite numerous studies observing the specific craniofacial characteristics of patients with TMD through cephalometric analysis, these were unable to represent the entire morphology and were difficult to apply clinically [
7].
In our work, we were inspired by a Chinese study [
7]. This study was the first to classify TMD using an unsupervised analysis based on lateral cephalometric radiographs, identifying only subgroups among patients with TMD and excluding healthy populations without TMD.
With our research, we wanted to delve into which type of malocclusion had a greater impact on the onset of TMD symptoms and, at the same time, on the condyle-fossa relationship.
First of all, the gender distribution in our study reflects the clinical reality where women represent the majority of patients with TMD, as hormonal fluctuations related to menopause and the menstrual cycle often exacerbate and worsen symptoms.
Among the patients who tested positive for TMD symptoms (headache, muscle tension in the head-neck area, dizziness, and cervical pain) on their first visit to the orthognathodontics department in Chieti, out of 67, 44 were women and only 23 were men.
As for age, one of the inclusion criteria was being of legal age; the average age of women was higher, 41.5 years, compared to that of men, 35.8 years; in both cases, it was noted that symptoms tend to manifest more frequently after the age of 35.
It is extremely difficult to predict the appropriate evolution of Temporomandibular Disorder (TMD) based solely on the presence or absence of a malocclusion. From the results of our study but also from those carried out previously [
10] it was possible to infer that Class II malocclusion has a higher incidence in muscular disorders but there is no defined link in the scientific literature with specific joint problems such as clicks, joint block or dislocations. Therefore, Class II malocclusion seems to be associated only with muscular problems.
Understanding the correlation between the condyle and the glenoid fossa in three dimensions can provide experts with the necessary tools to identify the onset of degenerative joint diseases or recognize already existing problems, thus facilitating more effective treatment planning [
14] Consequently, clinical interpretation, together with the accurate identification of these values, can play a crucial role in the diagnosis and treatment planning in various skeletal relationships.
Many studies have highlighted that the correlation between the condyle and the fossa changes based on the shape of the face both in the sagittal and vertical sense. An examination conducted by Saccucci and his team [
15] on the volume of the condyle in individuals with different antero-posterior and vertical skeletal models revealed that subjects with a hypodivergent model have a higher condyle volume compared to those with a normodivergent or hyperdivergent model.
In fact, the morphology of the TMJ varies among individuals. Several variables can influence this morphology, including functional loads; this could be due to the close relationship between form and function, which differs among subjects with different types of malocclusion [
10].
From our study, as already highlighted by a study by Bjork, patients, both women and men regardless of skeletal malocclusion, with a hyperdivergent facial model have a more advanced and higher condyle compared to those with a normal or low FMA angle. These results could have significant implications for understanding the growth and development of the face.
7. Conclusion
In summary, based on the information gathered from the literature and our study, it can be stated that:
Class II malocclusion is more frequently associated with muscular disorders. However, there is no definitive link in the scientific literature with specific joint problems such as clicks, joint blockage or dislocations. Consequently, it appears that Class II malocclusion is only related to muscular problems.
We therefore found that the reduced vertical dimension of the face that hypodivergent patients present, leads to greater compression of the joint tissues and a consequent muscle hypertonia that causes painful symptoms in patients.
Hyperdivergent subjects, on the other hand, have greater ligament laxity, muscle hypotonia that shows fewer symptomatic problems of the TMJ; this does not detract from the fact that hyperdivergent subjects with ligament laxity are more subject to condyle-disc incoordination as also supported by Stringert and Worms in their study [
16].
Women, due to hormonal fluctuations, are more prone to painful symptoms such as headaches and cervical pain compared to men.
The condyle-fossa relationship is closely related to malocclusion, both sagittal of the second and third skeletal classes and vertical of hypo/hyper divergence. In all cases, the condyle is in a non-concentric position in the fossa, causing an articular imbalance and, consequently, muscular, with the onset of DTM symptoms.
Finally, it is important to remember that the studies supporting the link between skeletal malocclusions and temporomandibular disorders are few. Therefore, the available information is still limited and sometimes conflicting. However, research, thanks also to the more detailed images provided by the cone beam CT scan, is progressing and is making progress in this field.
References
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021. [CrossRef]
- Feragalli, B.; Rampado, O.; Abate, C.; Macrì, M.; Festa, F. Cone beam computed tomography for dental and maxillofacial imaging: Technique improvement and low dose protocols. *Radiol. Med. 2017. [CrossRef]
- Schiffman, E.; Ohrbach, R.; Truelove, E. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. *J. Oral Facial Pain Headache 2014. [CrossRef]
- Guyer, A.E.C.; McNamara, J.A., Jr. Components and class III malocclusion in juveniles and adolescents. *Angle Orthod. 1986.
- Saborn, R.T. Difference between the facial patterns of class III malocclusion and normal occlusion. *Angle Orthod.1955.
- Bósio, J.A.; Burch, J.G.; Tallents, R.H.; Wade, D.B.; Beck, F.M. Lateral Cephalometric Analysis of Asymptomatic Volunteers and Symptomatic Patients with and without Bilateral Temporomandibular Joint Disk Displacement. *Am. J. Orthod. Dentofacial Orthop.1998. [CrossRef]
- Zhu, R.; Zheng, Y.-H.; Zhang, Z.-H.; Fan, P.-D.; Wang, J.; Xiong, X. Development of a new category system for the profile morphology of temporomandibular disorders patients based on cephalograms using cluster analysis. *Front. Public Health2022, Nov. [CrossRef]
- Meiyappan, N.; Tamizharasi, S.; Senthilkumar, K.P.; Janardhanan, K. Natural head position: An overview. *J. Pharm. Bioallied Sci.2015, Aug. [CrossRef]
- Festa, F.; Rotelli, C.; Scarano, A.; Navarra, R.; Caulo, M.; Macrì, M. Functional Magnetic Resonance Connectivity in Patients With Temporomandibular Joint Disorders. Front. Neurol.2021.
- Alhadad, S.A.; ALyafrusee, E.S.; Abdulqader, A.A.; Algumaei, W.S.; AL Mohana, R.A.A.M.; Ren, L. Comprehensive three dimensional positional and morphological assessment of the temporomandibular joint in skeletal Class II patients with mandibular retrognathism in different vertical skeletal patterns. BMC Oral Health 2022. [CrossRef]
- Taut, M.; Buduru, S.D.; Talmaceanu, D.; Ban, A.; Roman, R.; Leucuta, D.; Barbur, I.; Ilea, A. Occlusal Splint Therapy Combined with Cranio-Temporomandibular Kinesiotherapy in Patients with Temporomandibular Disorders—A CBCT Study. Life 2022, MDPI. [CrossRef]
- Pullinger, et al. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms. *Oral Surg. Oral Med. Oral Pathol.1987.
- Krisjane, Z.; Urtane, I.; Krumina, G.; Zepa, K. Three-dimensional evaluation of TMJ parameters in Class II and Class III patients. *Stomat., Baltic D. Maxillofac. J.* **2009**.
- Arieta-Miranda, J.M.; Silva-Valencia, M.; Flores-Mir, C.; Paredes-Sampen, N.A.; Arriola-Guillen, L.E. Spatial analysis of condyle position according to sagittal skeletal relationship, assessed by cone beam computed tomography. *Prog. Orthod.* **2013**. [CrossRef]
- Saccucci, M.; Polimeni, A.; Festa, F.; Tecco, S. Do skeletal cephalometric characteristics correlate with condylar volume, surface and shape? A 3D analysis. *Head Face Med.* **2012**. [CrossRef]
- Stringert, H.G.; Worms, F. Variations in skeletal and dental patterns in patients with structural and functional alterations of the temporomandibular joint: A preliminary report. *Am. J. Orthod. Dentofacial Orthop.* **1986**. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).