Introduction
The risk of transfusion-transmitted infections (TTI) in resource-rich countries has been significantly reduced due to the continuous implementation of donor selection policies, enhanced serological testing, the introduction of nucleic acid testing (NAT), and other crucial measures such as precise skin disinfection and the use of diversion bags during blood collection. Current risks vary according to local epidemiology, but are deemed acceptable by most national transfusion systems. According to recent data from the UK and the US, the risks are as follows: HBV 1 in 3 million donations, HIV 1 in 5 million donations, and HCV 1 in 1 million donations [Ainley LI, 2018].
Nevertheless, the possibility of acquiring infections from emerging pathogens (e.g. West Nile virus and Dengue virus), as well as from bacteria and protozoa, remains a concern in transfusion medicine. Bacterial contamination of stored blood products, particularly platelets, is still a threat for the safety of blood supply. PLT bags are kept on agitators at room temperature (20-24°C) to preserve PLT quality and function, but this storage condition can facilitate bacterial growth, leading to transfusion reactions and sepsis. This risk is not negligible; a meta-analysis estimates it to be approximately 1 in 1,900 for buffy coat (BC) PLTs and 1 in 4,348 for apheresis-collected PLTs [White SK]. Furthermore, one-quarter of contaminated PLT bags result in sepsis [Hong H, 2016].
Blood transfusion services may choose to mitigate this risk using bacterial screening approaches. The BacT/ALERT© system, is an efficient tool that promptly detects bacterial growth by measuring CO2 production in samples from PLT bags. Samples are incubated in dedicated culture bottles, and any increase in CO2 triggers an alarm, prompting the operator to remove the implicated unit from the blood product inventory. The unit remains quarantined until further investigation. However, BacT/ALERT© cannot always detect slow-growing bacteria such as Staphylococcus epidermidis, Staphylococcus aureus, and other species [Brailsford, 2018]. Additionally, BacT/ALERT© has a false positivity rate of 0.2-3.2%, leading to unnecessary product discards [Corean J, 2021].
In addition, a further reduction of the possibility of acquiring TTIs is crucial to ensure patient safety and maintain product supply. Globalization and international travel have increased TTI risks, particularly from zoonoses. This was highlighted at the onset of the COVID-19 pandemic, with concerns about potential blood transmission [Stanworth SJ, 2020]. Another challenge for BTS is emerging pathogens. When a new pathogen, such as the Chikungunya or Zika virus, emerges, specific measures like donor deferral, screening, and recall are adopted, significantly impacting donor pools. Implementing these measures requires substantial time, staff, and resources, and their efficacy in reducing TTI risk is only partial [Cicchetti A, 2018]. To prevent TTIs and ensure adequate blood stocks, BTS often import blood products from other regions or countries, leading to service disruptions and high costs.
Evaluating and implementing new pathogen reduction technology (PRT) is thus essential. A recent systematic review by Angel Gimenez-Richarte and colleagues demonstrated that UV-based PRT is particularly effective against arboviruses, significantly reducing the viral load of West Nile virus, Chikungunya virus, Dengue virus, and Zika virus [Angel Gimenez-Richarte, 2023]. The efficacy of UV-based PRT varies with the inactivation method used. Importantly, PRT does not neutralize donor antibodies (e.g., convalescent plasma), allowing recipients of treated blood products to benefit from donor antibodies against new infectious agents.
Recently, the European Directorate for the Quality of Medicines (EDQM) suggested implementing PRT as part of blood processing in its Blood Supply Contingency and Emergency Plan (B-SCEP) [
https://freepub.edqm.eu/publications/PUBSD-174/detail]. Implementing PRT will help harmonize TTI risks across countries. The new PRT types available use UVA, UVB and UVC light and may include special compounds that crosslink or associate with DNA/RNA after UVA irradiation (e.g., INTERCEPT® and MIRASOL®) or UVC light only (THERAFLEX®). This review aims to revisit existing knowledge on the efficacy, practicality, and challenges of using UV light-mediated PRT systems for PLTs.
Understanding Pathogen Reduction Technology (PRT)
-
A.
Explanation and Evolution of PRT (short analysis of the three main methods, better if using a picture)
The need to ensure better blood safety and to prevent TTI became urgent following the blood scandals of the 1980s and early 1990s. In the attempt to reduce the plasma contamination, treatment with solvent detergent (SD) was adopted for blood derived products (not for PLT). This represents very well a first example of pathogen reduction technology (PRT) for blood derived products. SD is very effective against lipid-enveloped viruses (also against protozoa), but not against unenveloped viruses such as HAV. Also, SD affects badly alpha-2 antitrypsin and Protein-S (an important natural occurring anticoagulant) [Klein HG 1998]. Another drug, similarly, used as a PRT agent, is methylene blue (MB). In 2003, to reduce the risk of transmission of variant Jacob Creutzfeldt Disease (vCJD) for the population born post 1996, FFP was outsourced and imported from the USA (lower vCJD geographical risk). At the time plasma was also treated with MB to ensure that the attempt towards the reduction of vCJD risk would have not cause an increase of other blood borne viruses [Seed CR 2018]. MB is associated with allergic reactions and hypotension, currently its use is not more recommended. In Belgium and in some other countries (e.g. Poland and Spain) is still used as an accepted PRT method. Recently, UV based PRT systems became available, and this is the topic of this review.
The existing PRT systems for platelets based on UV light are: i) INTERCEPT®, ii) MIRASOL®, iii) THERAFLEX® [Rebulla & Prati, 2022].
- I.
INTERCEPT® (Cerus Corporation): This PRT system use a synthetic psoralen (amotosalen hydrochloride) and UVA. The amotosalen compound will crosslink to the DNA/RNA chains immediately upon UVA exposure. This system requires an additional step since the compound must be removed before use.
- II.
MIRASOL® (Terumo-BCT): This technology utilizes riboflavin (Vitamin B2) as a photosensitizer that associates with nucleic acids and mediates an oxygen-independent electron transfer process leading to the modification of DNA/RNA upon exposure to UV light. It does not require an additional step to remove the compound.
- III.
THERAFLEX® (Macopharma): This system is based on the use of UVC light.
The exact mechanism of action of these 3 methods are illustrated in
Figure 1.
We will now analyze in depth all 3 methods:
This PRT method uses amotosalen as the inactivation agent. Amotosalen is a synthetized photoactive psoralen compound. Platelets (PLT) are resuspended in approximately 35% plasma and 65% PAS, or in 100% plasma. Amotosalen undergoes photoactivation with UVA light at 320-400 nm. A total dose of 3 joules/cm² is delivered, causing amotosalen to cross-link nucleic acids (DNA or RNA). Over time, this binding becomes permanent, impairing the replication of bacteria and other microorganisms. The residual amotosalen is subsequently removed using a dedicated compound adsorbtion device (CAD), which results in a certain degree of platelet loss (between 7-10%). For these reasons, Gathof BS et al. recommend increasing the lower limit of PLT units to 2.5 x 10¹¹ [Gathof BS et al. 2010]. However, the recent EDQM guidelines have suggested a lower limit of 2.0 x 10¹¹ [Guide to the preparation, use and quality assurance of Blood Components. European Committee EDQM. 21st Edition, 2023].
The efficacy of INTERCEPT® has been evaluated in several randomized clinical trials [CID J 2024]. McCullough reported on a randomized study in bleeding patients (SPRINT trial) with WHO grade 2 degrees (mild blood loss, clinically significant). Patients in the study group were transfused with PLT treated by INTERCEPT®, while patients in the control group received standard PLT [McCullough J 2004]. This study did not show a difference in bleeding events; however, patients transfused with PRT PLT required more products. It also emerged that PRT units had a lower concentration of PLT (<3.0 x 10¹¹). In the same study, post-transfusion CCI at 1 hour and at 24 hours were lower in the arm treated with PRT-PLT. The transfusion interval was shorter, leading overall to a higher prescription of PLT. Nevertheless, no differences in clinical bleeding were seen. Additionally, fewer transfusion reactions were observed when PRT PLT were administered (3.0% PCT versus 4.4% control; p=0.02) [McCullough J 2004].
Another randomized study (PRT treated PLT unit versus standard PLT unit) on INTERCEPT®, carried out in over 100 patients with thrombocytopenia (euroSPRITE), showed no statistically significant difference in CCI at 1 hour and at 24 hours of follow-up. Patients treated with PRT units had slightly lower platelet counts. Hemorrhagic and thrombotic events after transfusion were similar in both groups. However, in 2010, worrisome results were highlighted by the Dutch-Belgian HOVON cooperative group. In a randomized study, Kerkhoffs JLH et al. showed that the use of INTERCEPT® was associated with decreased CCI and with grade ≥2 bleeding. These findings were not confirmed by randomized controlled trials such as the SPRINT trial and the EFFIPAP trial, where the primary endpoint was WHO grade-2 bleeding [Cid Vox Sang 2024]. However, in the EFFIPAP trial, results differed depending on the control arm used (PLT in PAS or PLT in plasma). In the HOVON study, amotosalen was added to platelets suspended in approximately 35% plasma / 65% PASIII (study group) and compared with PLT resuspended in plasma only and PASIII only (control groups) [Ashford] [Kerkhoffs et al. Transfusion 2010]. This may have in part contributed to the overall negative results. Moreover, a recent review of PRT types and their efficacy showed that INTERCEPT® is certainly more efficacious against arboviruses compared to MIRASOL® [Angel Gimenez-Richarte 2023]. This is also confirmed by a better Log Reduction Factor (LRF) of 4 or more (>4 log10) with INTERCEPT®. Similarly, INTERCEPT® inactivates leukocytes, and its implementation could also make irradiation redundant [Castro G 2018]. Moreover, the possibility of a 7 days platelets storage has also been shown with INTERCEPT [Lozano 2011].
-
II.
MIRASOL®
This PRT method utilizes riboflavin (vitamin B2), a photoreactive compound that is non-toxic. Therefore, no further manipulation of the blood components is required after the illumination step, resulting in minimal loss of platelets during the inactivation treatment.
The compound is released in platelets resuspended either in plasma or in plasma with platelet additive solution (PAS). This is followed by photoactivation of riboflavin using UV-B light with a total energy power of 6.2 Joules/cm². A compound adsorption device (CAD) is not required because riboflavin is non-toxic. This method is highly effective against enveloped viruses, such as influenza virus, cytomegalovirus (CMV), HIV, respiratory syncytial virus (RSV), and human coronaviruses.
One of the most notable results achieved by MIRASOL® was demonstrated by Allain JP and colleagues in the AIMS study conducted in Ghana. In this study, whole blood treated with MIRASOL® showed a reduction in the incidence of transfusion-transmitted malaria (p=0.039) [Allain JP]. Furthermore, MIRASOL® has been reported to have moderate inactivation of enveloped viruses such as HEV [Ojea 2022] [Owada T].
Randomized studies have shown a 25% decrease in corrected count increment (CCI) when platelets inactivated with riboflavin-PRT were infused. This finding was confirmed in another study at 1 hour after transfusion. However, no major bleeding or other relevant side effects were observed, although a larger requirement of platelets in some patient categories was reported [Jimenez-Marco T 2018]. A recent study (miPLATE trial) did not show an inferiority of MIRASOL® compared to conventional platelet when the endpoint was calculated in days ≥ Grade 2 bleeding [Koespell S 2024].
Additionally, the platelet shelf life was extended to 7 days without any major side effects, except for a higher rate of lactate increase and glucose depletion starting from day 5. The platelet loss with MIRASOL® was lower than previously reported with INTERCEPT®, although a loss of swirling effect and increased apoptosis (assessed by Annexin) were also reported [Malvaux]. Furthermore, MIRASOL® inactivates leukocytes. This could theoretically suggest that leukoreduction/filtration may not be needed, but Norris P and colleagues have found contradictory results [Norris P 2018].
The main side effect noted with MIRASOL® is ATP consumption, which suggests that glycolytic pathways are activated [Li J 2004]. A randomized study (MERIT trial) from Uganda University is currently underway to clarify the potential benefits of MIRASOL®-PRT for transfusion-transmitted infection (TTI) prevention [Kasirye R]
-
III.
THERAFLEX®
THERAFLEX® is based on the use of UVC (wavelength 200-280 nm) [Escolar 2021] [Seltsam 2011]. This system is highly promising against high concentrations of various bacterial species [Gravemann U]. However, it is not very effective against HIV inactivation. The strongest efficacy (4 or more log steps) was demonstrated against vesicular stomatitis virus, porcine parvovirus (a model virus for parvovirus B19), encephalomyocarditis virus (a model virus for hepatitis A), and Sindbis virus (a model virus for hepatitis C). Other viruses, such as Pseudorabies virus (a model virus for hepatitis B) and West Nile virus, were less effectively inactivated, with reduction factors of approximately 2-3 and 3.5-4 log steps, respectively [Seltsam]. Eickmann M and colleagues conducted an in vitro study demonstrating that THERAFLEX® can effectively reduce the infectivity of severe acute respiratory syndrome coronavirus (SARS-CoV), Crimean-Congo haemorrhagic fever virus (CCHFV), and Nipah virus (NiV) in platelets and plasma [Eickmann M]. THERAFLEX® also induced a mean log reduction greater than 3.5 against Hepatitis E virus [Praditya D].
THERAFLEX® is also effective in reducing transfusion-associated graft-versus-host disease (TA-GvHD) by inactivating leukocytes [Pohler]. It differs from INTERCEPT® and MIRASOL® as it does not require a photosensitizing agent. A German study involving 171 patients reported no significant side effects associated with THERAFLEX® [Brixner V]. However, this study was underpowered to detect side effects, and the primary efficacy outcome was not achieved, as PRT platelets were found to be less effective than standard platelets [Prati D].
THERAFLEX® does carry some quality-related side effects, such as increased annexin V binding, lactate accumulation, and higher expression of CD41/61 [Bashir]. Currently, THERAFLEX® is the only pathogen reduction technology (PRT) that provides time-to-treatment studies, which are crucial for determining the optimal time to start pathogen reduction treatment. THERAFLEX® requires no photosensitizer, eliminating additional processing time for the removal of such chemicals. Consequently, it allows for faster delivery of blood products and enhances safety by eliminating handling and transportation errors [Schulze T].
3. Advantages of PRT for Platelet Transfusions
A- Safety and efficiency benefits.
B- Evidence supporting advantages (extended shelf-life of platelets, decreased transfusion-transmitted infections, reduced risk of GVDH)
Overall Pathogen reduction technology (PRT) has several effects which seems to be mainly positive. We have summarized and commented on most of those here below:
-
i)
PRT extends PLT shelf-life.
-
ii)
PRT and transfusion reactions.
-
iii)
PRT reduces Ta-GvHD.
-
iv)
PRT and TTI.
-
v)
PRT impact on coagulation proteins.
-
vi)
PRT harmonizes TTI risk between countries.
-
vii)
PRT does not affect the presence of pre-existing antibodies.
-
viii)
PRT and sepsis
-
i)
PRT extends PLT shelf-life
The lifespan of platelets (PLT) is currently limited to 5 days. Therefore, any tool that could extend the shelf life of PLT is highly desirable for any Blood Transfusion Service (BTS). The most widely adopted system for monitoring PLT contamination is BacT/ALERT®. This system is particularly prevalent in the UK and Ireland and helps monitor bacterial growth to prevent transfusion-transmitted infections (TTI). BacT/ALERT® can identify contaminated PLT units at a very early stage. Recent studies have shown that BacT/ALERT® can help extend PLT shelf life to 7 days [Ramirez-Arcos]. Additionally, the INTERCEPT® system has demonstrated the ability to preserve PLT quality over 7 days of storage [Ohlsson S]. The potential for extending PLT shelf life should be considered in any cost analysis of pathogen reduction technology (PRT) implementation. A Spanish study indicated that PRT can help reduce the rate of PLT outdates [Gorria C 2020].
-
ii)
PRT reduces transfusion reactions.
PRT has been associated with a reduction of PLT transfusion reactions [Gathof 2010] [Pitman JP 2023]. The exact reason is unknown; however, this may simply be due to the inactivation of white blood cells and the consequent abrogation of cytokine production. Some authors have hypothesized a reduction of reactive stimuli by LPS, anti CD3+ and anti CD28 [Fast LD].
-
iii)
PRT reduces Ta-GvHD
Irradiation of blood products is used to to prevent the development of Transfusion Associated Graft versus Host Disease (TA-GvHD). Indications for irradiated blood components include patients undergoing intrauterine transfusion, neonatal exchange transfusion, those with congenital cell-mediated immunodeficiencies, patients with Hodgkin lymphoma (for all transfusions during their lifetime), hematopoietic stem cell transplant recipients (both autologous and allogeneic), donors of allogeneic hematopoietic stem cells (in the week prior to and during stem cell harvest), CAR-T therapy recipients (7 days prior to collection and 3 months post-infusion), patients receiving purine analog therapy (e.g., fludarabine, cladribine, deoxycoformycin, bendamustine, clofarabine), those undergoing ATG or alemtuzumab therapy for hematologic diseases, recipients of donations from biologic relatives, and recipients of donations selected on the basis of HLA matching. Early reports in large cohorts of patients in France and Switzerland have shown that pathogen reduction technology (PRT) has strong efficacy for the prevention of TA-GvHD [Corash L 2016]. A study by Fast L and colleagues demonstraated that PRT is even more effective than irradiation for the inactivation of T cells [Castro 2018], as irradiation does not fully impair CD69 expression and the potential for lymphocyte proliferation [Fast LD].
Recently, Sim J and colleagues conducted a randomized prospective study to better evaluate the efficacy and safety of PRT. They studied a relatively large allogeneic transplant cohort (n=30) where blood products were treated only with PRT and did not undergo any leukoreduction or irradiation [Sim J 2019]. This study was successful, as none of the patients developed TA-GvHD. This finding is particularly relevant within hematology, highlighting the potential of PRT to make blood product irradiation and leukoreduction redundant. Additionally, from an economic perspective, this could significantly reduce costs [Fast L 2021]. Liebermann and colleagues also commented on the prevention of CMV infection through leukoreduction, noting that PRT can effectively replace leukoreduction for CMV prevention [Liebermann 2014].
-
iv)
PRT reduces TTI
The capacity of reducing the risk of TTI varies according to PRT type. It also differs if PLT are resuspended in plasma or in platelet additive solutions (PAS). The published data on INTERCEPT® showed a high efficacy against: i) Protozoa (Plasmodium falciparum, Trypanosoma Cruzi, Leishmania Mexicana, Leishmania major Jish, Babesia microti); ii) Gram-Negative Bacteria (Escherichia coli, Serratia marcescens, Klebsiella pneumoniae, Pseudomonas aeruginosa, Salmonella choleraesuis, Yersinia enterocolitica, Enterobacter cloacae, Anaplasma phagocytophilum); iii) Gram-Positive Bacteria (Staphylococcus epidermis, Staphylococcus aureus, Streptococcus pyogenes, Listeria monocytogenes, Corynebacterium minutissimum, Bacillus cereus (vegetative), Bifidobacterium adolescentis, Propionibacterium acnes, Lactobacillus species, Clostridium perfringens (vegetative form), Spirochete Bacteria such as Treponema pallidum and Borrelia burgdorferi); iii) Enveloped viruses (HIV-1, HBV (strain MS-2), HCV (strain Hutchinson), HTLV-I , HTLV-II, CMV, Bovine Viral Diarrhea Virus, Duck Hepatitis B Virus, Pseudorabies virus, West Nile Virus, SARS-CoV2 , Chikungunya virus, Influenza A H5N1 virus (Avian Influenza, Zika, Dengue, Yellow Fever); iv) Non-Enveloped Viruses (Bluetongue Virus type 11, Calicivirus, Human Adenovirus-5, Parvovirus B19) [INTERCEPT Platelets, Technical Data Sheet] [Lanteri 2020 MC]. The technical data sheet available on MIRASOL® is not so informative, but clearly states that even this PRT is efficacious against enveloped and non-enveloped viruses, gram negative and gram-positive bacteria and parasites [https://www.terumobct.com/Public/306690232.pdf].
In the case of THERAFLEX activity against the following bacteria is reported (Enterobacter cloacae, Escherichia coli, Klebsiella Pneumoniae, Morganella morganii, Proteus mirabilis, Pseudomonas fluorescens, Serratia marcescens, Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus bovis, Streptococcus dysgalactiae, Streptococcus pyogenes, Listeria monocytogenes, Acinetobacter baumannii, Streptococcus agalactiae, Streptococcus pneumoniae, Bacillus cereus, Bacillus thuringiensis, Propionibacterium acnes)
[https://aob.amegroups.org/article/view/6833/html]. Also, activity against parasites sucha s Babesia divergens
[Castro E 2014] and African mosquito-borne flaviviruses such as
West Nile virus (WNV) and Usutu virus (USUV) have been shown
[Graveman U 2024].
The use of PRT is quite promising. At the present they are several reports on the use of PRT. For example, Pitman reported on 1,221,031 platelet transfusions in France over 2010-2020 [Pitman 2023]. Escolar and colleagues reported that >875,000 transfusion treated with INTERCEPT® and > 700,000 treated with MIRASOL® have been administered so far, and no case of TTI or sepsis was reported [Escolar].
-
v)
PRT impact on plasma coagulation proteins
Plasma products treated with PRT will have reduced levels of key coagulation proteins. Statistically significant reductions in FII, FV, FVIII, FIX, and FXI have been shown [Coene J 2014]. However, this may not necessarily impair the hemostatic function of the plasma product. For example, a thrombin generation (TG) study conducted on plasma treated with INTERCEPT® showed TG levels similar to those of untreated plasmaF, suggesting that hemostatic function is preserved [Ravanat 2018].
Studies have shown that solvent/detergent treated plasma and MB methylene blue) treated can affect Protein-S levels [Flamholz 2000] [Yarranton H] [Hellstern 2011]. This is relevant because Protein-S is a co-factor of Protein-C and is essential for its conversion into activated Protein-C (APC). APC balances the actions of FVa and FVIIIa [Piccin A et al 2022]. MB-treated plasma best preserves FV and FXI levels compared to INTERCEPT® [Backholer L 2016]. This information is particularly relevant because often platelets (PLT) are still resuspended in plasma [Larrea L].
4. Criticisms and Limitations of PRT
Highlight criticisms and limitations (Cost and organizational implications, storage lesion, impact on platelet quality and efficacy, alloimmunization, etc.). Evidence supporting concerns.
The following points were identified as criticism and limitation of PRT:
-
i)
Bleeding risk
-
ii)
PLT increment count
-
iii)
Biochemical changes
-
iv)
Mitochondrial DNA inactivation
-
v)
PRT alters microRNA
-
vi)
Pathogens not impacted by PRT
-
vii)
Costs
-
i)
Bleeding risk and PLT count increment
The possibility that PRT may affect platelet quality and contribute to a higher bleeding risk has been a concern for several investigators and continues to be so for some. An exhaustive Cochrane review on the risk of bleeding associated with PRT was carried out in 2017 [Estcourt LJ]. More recently, systematic review of all published randomized controlled trials was published by the Italian group of Pati I in 2022. In this study, Pati I and colleagues reported no difference in clinically significant bleeding with INTERCEPT® and MIRASOL®. However, a higher number of bleeding events was observed in the PRT groups [Pati I].
Among these studies, the most concerning is the one conducted by the Dutch group of Kerkhoffs JLH and colleagues [Kerkhoffs JLH 2010]. In this study, a reduced 1-hour corrected count increment (CCI) was documented using INTERCEPT®. Moreover, an increased risk of bleeding was also documented. Interestingly, patients with hematological malignancies such as AML, ALL, and LNH were included. This is relevant since these patients have very low PLT counts and are quite prone to bleeding.
Similarly, the Italian Platelet Technology Assessment Study (IPTAS) showed that the absolute risk difference in WHO Grade ≥2 bleeding for INTERCEPT® was 6.1% (with an upper one-sided 97.5% confidence limit of 19.2%), while the absolute risk difference for MIRASOL® was better at 4.1% (with an upper one-sided 97.5% confidence limit of 18.4%) [Rebulla 2017]. However, in neither case was the absolute risk difference statistically significant. In both trials, post-transfusion platelet count increments were significantly lower in treated versus control patients [Rebulla 2017].
A randomized French study (EFFIPAP) did not show that PLTs treated with PRT (INTERCEPT®) and resuspended in PAS were associated with any higher rate of WHO Grade ≥2 bleeding. However, a 12.5% difference margin was considered for this non-inferiority study [Garban F].
Osselaer JC and colleagues studied a large cohort of patients (n = 651) treated with 5106 blood components transfused with PRT INTERCEPT® products. The authors reported no changes in the number of PLT doses administered with and without PRT implementation [Osselaer JC]. Cazenave JP and colleagues also reported similar findings. Interestingly, these authors also found a reduced number of transfusion reactions associated with PRT using INTERCEPT®. More recently, an Austrian study reported a similar consumption of blood products before and after PRT implementation (INTERCEPT®) over 21 months of follow-up. A similar finding was also reported by Infanti L and colleagues, in a study that also showed the possibility of extending PLT shelf life to 7 days [Infanti L].
This suggests that no significant increase in bleeding was seen with PRT implementation [Amato 2017]. The same group of authors also studied a large cohort of patients treated with massive transfusion [Nussbaumer]. Interestingly, no increased bleeding risk was seen after PRT implementation. Additionally, both the SPRINT [McCullough J] and the EFFIPAP [Garban F] studies enrolled patients with severe hematological conditions and low PLT counts, suggesting that these “fragile” patients are not adversely affected when PRT is implemented.
-
ii)
PLT increment count
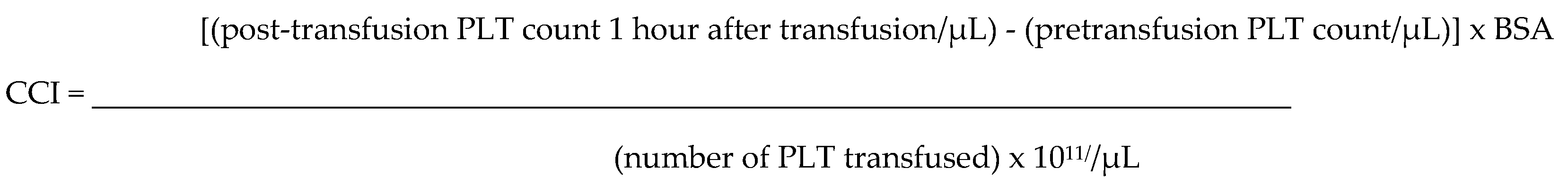
Several reports have suggested that PRT treated PLT lead to an inferior post transfusion PLT count compared to this obtained when PLT without any PRT treatment are transfused [Blake T 2021]. To analyze this aspect, the concept of corrected count increment (CCI) has been introduced. CCI was initially developed with the intent to facilitate physicians dealing with differential diagnosis of idiopathic thrombocytopenic purpura (ITP) and is currently used for analyzing platelet refractoriness. This index directly correlates to the PLT dose transfused. CCI is based on a small calculation on PLT numbers based on a post-transfusion specimen collected 1 hour after transfusion (CCI1hour). This index also considers the patient’s body surface area (BSA). Usually after a transfusion of a standard unit of PLT in a patient with not-active bleeding, the PLT count shows an increment between 5-10.000/µL.
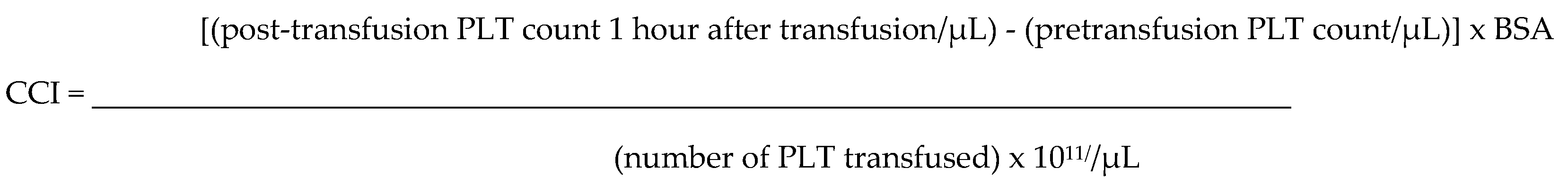
If the CCI does not show an increment, further investigations would be required to identify the cause (e.g., immunization to HLA or HPA antigens, ITP, sepsis, etc). A Canadian simulation study reported on possible risk of wastages and PLT shortages caused by PRT implementation. The authors described a reduced CCI when INTERCEPT® was used. This would have led to prescribing more products, and enhanced patient’s exposure to more blood donors. The authors concluded that this would impact on supply chain and potentially increase the risk of TTI because larger exposure to blood products [Blake T 2021]. Different results were shown by the SPRINT randomized study. In particular, CCI at 1 hour and at 24 hours post transfusion were lower for patients transfused with PRT treated PLT. Also, the transfusion interval was shorter leading overall to a higher prescription of PLT, however, no differences in clinical bleeding were seen [Murphy S et al 2006]. However, other studies have not confirmed this data and have not reported any increased PLT consumption for INTERCEPT® [Cazenave][Osselaer][Amato][Nussbaumer][Infanti].
-
iii)
Biochemical changes
Malvaux N et al. reported on changes in biochemical markers in PLT concentrate treated with either MIRASOL® or INTERCEPT®. A higher production of lactate, along with a greater reduction in glucose, was observed for MIRASOL®. Swirling at day 5 was also worse when PLT were treated with MIRASOL®, suggesting that INTERCEPT® should be preferred [Malvaux 2022]. Conversely, PLT treated with INTERCEPT® preserved swirling until day 7 [Malvaux 2022] [Lotens Transfusion 2018] [Ohlsson Vox Sang 2018]. However, some biochemical studies have shown problems even when INTERCEPT® is used. Specifically, Stivala S and colleagues reported that PLT treated with INTERCEPT® exhibited reduced function in response to activation agonists (i.e., collagen, thrombin, and von Willebrand Factor). The same study showed increased PLT apoptosis through Bak upregulation and a caspase-dependent pathway, enhancing PLT clearance from the circulation, with obvious clinical implications [Stivala S].
-
iv)
Mitochondrial DNA inactivation
Following ultraviolet (UV) light-based pathogen inactivation, mitochondrial DNA (mitDNA) damage can occur. Specific PCR multiplex assays have been developed for testing mitDNA. These assays have demonstrated that pathogen reduction technology is responsible for this damage [Kim S][Bruchmüller]. Furthermore, Bakkour and colleagues showed that mitDNA damage is primarily UV-dependent and not related to the presence of amotosalen [Bakkour].
iv) PRT alters microRNA
Diallo I and his colleagues were the first to report alterations in microRNAs contained in platelet-derived microparticles (PMP) [Diallo I]. The authors suggested that pathogen reduction technology might influence microRNA loading into PMP, which may indirectly affect PMP bioactivity. Alterations of microRNAs (miRNAs) stored within PMP were observed with INTERCEPT®. No such alterations were seen with MIRASOL®. The authors attributed these alterations to the presence of the additive storage solution (amotosalen) used with INTERCEPT®. Arnason and colleagues reported that INTERCEPT® affects only the expression of miRNA-96-5p, showing downregulation of this particular miRNA out of the 25 miRNAs analyzed [Arnason].
-
v)
pathogens not impacted by PRT
PRT can significantly contribute to reducing the pathogen load associated with transfusion, but no type of PRT ensures full sterility of blood products. Additionally, PRT is clearly ineffective against prions, spores, and some viruses without a lipid envelope (e.g., Hepatitis A). However, MIRASOL® and THERAFLEX® have been shown to inhibit HEV [Owada 2017]
-
vi)
PRT high costs
The cost analysis of implementing Pathogen Reduction Technology varies between studies and in different geographical, epidemiological and economical settings. Several factors affect this cost, including the type of PRT procedure, shorter intervals of sustained transfusion, extended shelf-life from 5 to 7 days, the elimination of test procedures ( such as CMV testing and bacterial culture), the elimination of gamma irradiation.
Cicchetti A and colleagues conducted a cost analysis on PRT in Italian patients, considering over 50,000 transfused patients in one year. They predicted an overall cost increase of 30% [Cicchetti A 2018]. Additionally, the same authors suggested that while PRT can significantly reduce the risk of transfusion-transmitted infections (TTI), it does not guarantee protection against all TTIs. Furthermore, they indicated that PRT is not applicable to all blood products (e.g., red cells) and may cause alterations in product quality [Cicchetti A 2018].
In a constructive criticism, Farrugia emphasized that although current PRT is not perfect, previous regulatory authorities, such as the US Blood Product Advisory Committee, investigating blood inquiries related to HIV transmission, have clearly stated that “partial solutions should be welcome and where possible implemented by BTS” [Blood Products Advisory]. We concur with this statement. Our perspective is that ensuring and improving patient safety should always remain a priority for any BTS.
CF Bell and colleagues, in an earlier cost analysis, also noted that introducing PRT would render bacterial testing redundant, leading to indirect cost savings [Bell CF 2003]. The cost saving associated to the prevention of a potentially emerging virus is very significant when considered in economic studies.
Most study on cost analysis have been conducted on INTERCEPT only. In this respect, a study sponsored by INTERCEPT showed that by adopting PRT the incremental cost ratio (ICERs) of PLT is certainly higher, however this may be justified if new emergent pathogens may arise with a 10-fold risk of transmission with transfusion [Davison N et al 2021]. Gregoire Y and colleagues from Québec showed an incremental cost effectiveness ratio (ICER) on quality-adjusted life years (QALY) equal to $8.1 million/QALY [Gregoire Y]. However, in the presence of a new blood-borne pathogen the ICER was reduced to $123,063. Rosskopf K and his colleagues reported on the advantages of not having gamma irradiation and bacterial screening in place. The analysis concluded that implementing PRT added an additional cost of +7.5% [Rosskopf K]. Mc Cullough and colleagues reported on significant cost saving for each PLT unit treated with PRT, if standard microbiological testing would be removed. Furthermore, the same authors stressed that a shelf-life extension to 7 days would contribute significantly to cost reduction [Mc Cullough 2015].
6. Future Perspectives
The prevention of TTI, cannot prescind from implementing PRT or similar systems for RCC and plasma products. Recently a randomized trial called ReCePI on INTERCEPT for RCC has been conducted in patients undergoing cardiovascular surgery. The trial demonstrated non-inferiority for INTERCEPT treated RCC compared to conventional RCC as measured by the incidence of acute kidney injury (AKI).
Similarly study on fibrinogen compound like cryoprecipitate are currently undergoing [Keltner NA Transfusion 2024].
7. Should We Stay or Should We Go?
A critical review of previous RCT studies did not identify relevant clinical complications when PRT was implemented. For example, the worrisome higher bleeding (>WHO grade 2) or lower CCI did not really emerged, even if data have shown that PRT may impact on the post transfusion PLT count. From the perspective of improving blood safety, there is no clear reason why PRT should not be further implemented. The economic cost associated with PRT implementation, may have been an obvious obstacle. However, considering the benefits of PRT (reduced risk of TTI, better TA-GvHD prevention and no need of irradiation), it is not clear to these authors why PRT has not been widely adopted. Perhaps, the large number of RCT designed to prove that PRT does not impact on product quality (reduced CCI count, or increased bleedings), may have contributed to create he perception that PRT is unsafe. Interestingly, those centers that have already adopted PRT have not moved away from this practice. This indirectly validates PRT. However, the wait and watch approach adopted by other BTS indicates that a large resistance towards implementing PRT still exists.
8. Conclusions
A. Summary of Key Points
B. Personal Recommendation and Final Remarks
TTI in Transfusion Medicine have always been a challenge, particularly because new emerging disease will always be present even in the future. The recent COVID-19 pandemic is a good example of this. For this reason, PRT in transfusion Medicine offers the possibility to reduce and control future events caused by unknown pathogens. The relationship between zoonosis and TTI (West Nile Virus, Zika, MERS, SARS, Malaria, Chikungunya virus etc.) is large and well reported in the literature. The possibility to implement blood safety by using UV lights with or without intercalating agents able to block DNA and RNA replication signaling, is likely to become a cornerstone of Transfusion Medicine. Moreover, the introduction of this technology will even potentiate safety of existing PCR screening practice, ensuring that any false negative sample potentially infective, will still undergo inactivation. This transfusion concept has also been recently debated by Farrugia in his description of a “safety tripod” made by 1) appropriate donor selection, 2) blood screening with molecular technology and 3) the adoption of viral inactivation processes [Farrugia A 2023].
Another advantage of introducing PRT, could be the extended shelf life of blood products such as PLTs. This will have an economical and inventory management practical benefit, allowing to have more products available for longer period of time. Implementation of PRT in low-income countries (e.g. sub-Saharan Africa countries), where TTI risk is high, in theory could be beneficial. For example, in Ghana the risk of blood parasitemia by malaria is >50% [Kasirye R].
However this is not practicable and moreover unrealistic due to the high cost [Allain JP 2016]. Paradoxically, PRT implementation seems more difficult to be accepted in Western countries. Part of the difficulty consist in cultural resistance and lack of vision. Several transfusionists and clinician are also reluctant to implement these devices because afraid of side effects or inefficacy of PRT. This is particularly true in UK and Ireland, where any new procedure affecting the blood products is a delicate and sensitive topic or better to say as a “mine field”. This is probably an indirect psychological consequence of the infected blood products (with HIV and hepatitis) scandals and the still ongoing “Blood Inquiry”. Furthermore, cost analysis is often carried out by local BTS, and local services are discouraged to consider PRT because excessive costs. Therefore, we believe that national health regulatory authorities and international societies (above local BTS), should be involved in accurately evaluating scientific data to clarify the role if PRT implementation is really needed or not.
Ethical Consideration
Not applicable.
Acknowledgements
We are grateful to Mr Marco Marzola, Piccin Nuova Libraria, Padova, Italy for designing Figure 1A. We are grateful to Dr Marcia Cardoso, Terumo Blood and Cell Technologies for providing us with Figure 1B.
Conflicts of Interest
DP has received travel and research grants, speaking fees, and teaching fees from Diasorin, Diamed, Diatech Pharmacogenetics, Grifols, Immucor, Macopharma, Ortho Clinical Diagnostics,Terumo, Cerus. All authors have no conflict of interest or any potential conflicts of interest.
References
- Ainley LI, Hewitt PE. Haematology patients and the risk of transfusion transmitted infection. Br J Haematol. 2018 Feb;180(4):473-483. [CrossRef]
- Allain JP, Owusu-Ofori AK, Assennato SM, Marschner S, Goodrich RP, Owusu-Ofori S. Effect of Plasmodium inactivation in whole blood on the incidence of blood transfusion-transmitted malaria in endemic regions: the African Investigation of the Mirasol System (AIMS) randomised controlled trial Lancet. 2016 Apr 23;387(10029):1753-61.
- Amato M, Schennach H, Astl M, Chen CY, Lin JS, Benjamin RJ, Nussbaumer W. Impact of platelet pathogen inactivation on blood component utilization and patient safety in a large Austrian Regional Medical Centre. Vox Sang. 2017 Jan;112(1):47-55. [CrossRef]
- Arnason NA, Johannson F, Landrö R, Hardarsson B, Irsch J, Gudmundsson S, Rolfsson O, Sigurjonsson OE. Pathogen inactivation with amotosalen plus UVA illumination minimally impacts microRNA expression in platelets during storage under standard blood banking conditions. Transfusion. 2019 Dec;59(12):3727-3735. [CrossRef]
- Backholer L, Wiltshire M, Proffitt S, Cookson P, Cardigan R. Paired comparison of methylene blue- and amotosalen-treated plasma and cryoprecipitate. Vox Sang. 2016 May;110(4):352-61. [CrossRef]
- Bagri A, de Assis RR, Tsai CT, Simmons G, Mei ZW, Von Goetz M, Gatmaitan M, Stone M, Di Germanio C, Martinelli R, Darst O, Rioveros J, Robinson PV, Ward D, Ziman A, Seftel D, Khan S, Busch MP, Felgner PL, Corash LM. Antibody profiles in COVID-19 convalescent plasma prepared with amotosalen/UVA pathogen reduction treatment. Transfusion. 2022 Mar;62(3):570-583. [CrossRef]
- Bakkour S, Chafets DM, Wen L, Dupuis K, Castro G, Green JM, Stassinopoulos A, Busch MP, Lee TH. Assessment of nucleic acid modification induced by amotosalen and ultraviolet A light treatment of platelets and plasma using real-time polymerase chain reaction amplification of variable length fragments of mitochondrial DNA. Transfusion. 2016 Feb;56(2):410-20. [CrossRef]
- Bashir S, Cookson P, Wiltshire M, Hawkins L, Sonoda L, Thomas S, Seltsam A, Tolksdorf F, Williamson LM, Cardigan R. Pathogen inactivation of platelets using ultraviolet C light: effect on in vitro function and recovery and survival of platelets. Transfusion 2013; 53(5):990–1000. [CrossRef]
- Bell CE, Botteman MF, Gao X, Weissfeld JL, Postma MJ, Pashos CL, Triulzi D, Staginnus U. Cost-effectiveness of transfusion of platelet components prepared with pathogen inactivation treatment in the United States. Clin Ther. 2003 Sep;25(9):2464-86. [CrossRef]
- Blood Products Advisory Committee, US Food and Drug Administration. Options to further reduce the risk of bacterial contamination in platelets for transfusion [Internet]. Available at: https://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/BloodVaccinesandOtherBiologics/BloodProducts Advisory Committee/UCM587085.pdf. Accessed on 14/10/2018.
- Borrega R, Nelson DKS, Koval AP, Bond NG, Heinrich ML, Rowland MM, Lathigra R, Bush DJ, Aimukanova I, Phinney WN, Koval SA, Hoffmann AR, Smither AR, Bell-Kareem AR, Melnik LI, Genemaras KJ, Chao K, Snarski P, Melton AB, Harrell JE, Smira AA, Elliott DH, Rouelle JA, Sabino-Santos G Jr, Drouin AC, Momoh M, Sandi JD, Goba A, Samuels RJ, Kanneh L, Gbakie M, Branco ZL, Shaffer JG, Schieffelin JS, Robinson JE, Fusco DN, Sabeti PC, Andersen KG, Grant DS, Boisen ML, Branco LM, Garry RF. Cross-Reactive Antibodies to SARS-CoV-2 and MERS-CoV in Pre-COVID-19 Blood Samples from Sierra Leoneans.Viruses. 2021 Nov 21;13(11):2325.
- Brailsford SR, Tossell J, Morrison R, McDonald CP, Pitt TL. Failure of bacterial screening to detect Staphylococcus aureus: the English experience of donor follow-up. Vox Sang. 2018 May 24.
- Brixner V, Bug G, Pohler P, Krämer D, Metzner B, Voss A, Casper J, Ritter U, Klein S, Alakel N, Peceny R, Derigs HG, Stegelmann F, Wolf M, Schrezenmeier H, Thiele T, Seifried E, Kapels H-H, Döscher A, Petershofen EK, Müller TH, Seltsam A. Efficacy of UVC-treated, pathogen-reduced platelets versus untreated platelets: a randomized controlled non-inferiority trial. Haematologica. 2021; 106(4):1086-1096. [CrossRef]
- Bruchmüller I, Lösel R, Bugert P, Corash L, Lin L, Klüter H, Janetzko K. Effect of the psoralen-based photochemical pathogen inactivation on mitochondrial DNA in platelets. Platelets. 2005 Dec;16(8):441-5. [CrossRef]
- Castro E, González LM, Rubio JM, Ramiro R, Gironés N, Montero E. The efficacy of the ultraviolet C pathogen inactivation system in the reduction of Babesia divergens in pooled buffy coat platelets. Transfusion. 2014 Sep;54(9):2207-16.
- Castro G, Merkel PA, Giclas HE, Gibula A, Andersen GE, Corash LM, Lin JS, Green J, Knight V, Stassinopoulos A. Amotosalen/UVA treatment inactivates T cells more effectively than the recommended gamma dose for prevention of transfusion-associated graft-versus-host disease. 2018 Jun;58(6):1506-1515. [CrossRef]
- Cazenave JP, Isola H, Waller C, Mendel I, Kientz D, Laforêt M, Raidot JP, Kandel G, Wiesel ML, Corash L. Use of additive solutions and pathogen inactivation treatment of platelet components in a regional blood center: impact on patient outcomes and component utilization during a 3-year period. Transfusion. 2011 Mar;51(3):622-9. [CrossRef]
- Cicchetti A, Coretti S, Sacco F, Rebulla P, Fiore A, Rumi F, Di Bidino R, Urbina LI, Refolo P, Sacchini D, Spagnolo AG, Midolo E, Marano G, Farina B, Pati I, Veropalumbo E, Pupella S, Liumbruno GM. Budget impact of implementing platelet pathogen reduction into the Italian blood transfusion system. Blood Transfus. 2018 Nov;16(6):483-489. [CrossRef]
- Cicchetti A, Coretti S, Sacco F, Rebulla P, Fiore A, Rumi F, Di Bidino R, Urbina LI, Refolo P, Sacchini D, Spagnolo AG, Midolo E, Marano G, Farina B, Pati I, Veropalumbo E, Pupella S, Liumbruno GM. Budget impact of implementing platelet pathogen reduction into the Italian blood transfusion system. Blood Transfus. 2018 Nov;16(6):483-489. [CrossRef]
- Cid J, Escolar G, Lozano M. Therapeutic efficacy of platelet components treated with amotosalen and ultraviolet A pathogen inactivation method: results of a meta-analysis of randomized controlled trials. Vox Sang. 2012 Nov;103(4):322-30. [CrossRef]
- Cid J, Charry P, Lozano M. Therapeutic efficacy and safety of pathogen-reduced platelet components: Results of a meta-analysis of randomized controlled trials. Vox Sang. 2024 Mar;119(3):203-211. [CrossRef]
- Coene J, Devreese K, Sabot B, Feys HB, Vandekerckhove P, Compernolle V. Paired analysis of plasma proteins and coagulant capacity after treatment with three methods of pathogen reduction. Transfusion. 2014 May;54(5):1321-31. [CrossRef]
- Corash L, Benjamin RJ. The role of hemovigilance and postmarketing studies when introducing innovation into transfusion medicine practice: the amotosalen-ultraviolet A pathogen reduction treatment model. Transfusion. 2016 Mar;56 Suppl 1:S29-38. [CrossRef]
- Corean J, White SK, Schmidt RL, Walker BS, Fisher MA, Metcalf RA. Platelet Component False Positive Detection Rate in Aerobic and Anaerobic Primary Culture: A Systematic Review and Meta-Analysis. Transfus Med Rev. 2021 Jul;35(3):44-52. [CrossRef]
- Davison N, Willis A et al. Vox Sang. 2021;116(Suppl. 1):5–188.
- Diallo I, Benmoussa A, Laugier J, Osman A, Hitzler WE, Provost P. Platelet Pathogen Reduction Technologies Alter the MicroRNA Profile of Platelet-Derived Microparticles. Front Cardiovasc Med. 2020 Mar 19;7:31. [CrossRef]
- Escolar G, Diaz-Ricart M, McCullough J. Impact of different pathogen reduction technologies on the biochemistry, function, and clinical effectiveness of platelet concentrates: An updated view during a pandemic. Transfusion. 2022 Jan;62(1):227-246. [CrossRef]
- Estcourt LJ, Malouf R, Hopewell S, Trivella M, Doree C, Stanworth SJ, Murphy MF. Pathogen-reduced platelets for the prevention of bleeding. Cochrane Database Syst Rev. 2017 Jul 30;7(7). [CrossRef]
- Farrugia, A. Cost of pathogen reduction for platelets: reply to Cicchetti et al. Blood Transfus 2018; 16: 483-9. Blood Transfus. 2019 Jan;17(1):84.
- Farrugia, A. The Evolution of the Safety of Plasma Products from Pathogen Transmission-A Continuing Narrative. Pathogens. 2023 Feb 15;12(2):318. [CrossRef]
- Fast LD, Dileone G, Li J, Goodrich R. Functional inactivation of white blood cells by Mirasol treatment. Transfusion. 2006 Apr;46(4):642-8. [CrossRef]
- Fast LD, DiLeone G, Marschner S. Inactivation of human white blood cells in platelet products after pathogen reduction technology treatment in comparison to gamma irradiation. Transfusion. 2011 Jul;51(7):1397-404. [CrossRef]
- Fast, LD. Developments in the prevention of transfusion-associated graft-versus-host disease. Br J Haematol. 2012 Sep;158(5):563-8.
- Flamholz R, Jeon HR, Baron JM, Baron BW. Study of three patients with thrombotic thrombocytopenic purpura exchanged with solvent/detergent-treated plasma: is its decreased protein S activity clinically related to their development of deep venous thromboses? J Clin Apher. 2000;15(3):169-72.
- Freimanis G, Sedegah M, Owusu-Ofori S, Kumar S, Allain JP. Investigating the prevalence of transfusion transmission of Plasmodium within a hyperendemic blood donation system. Transfusion. 2013 Jul;53(7):1429-41.
- Gathof BS, Tauszig ME, Picker SM. Pathogen inactivation/reduction of platelet concentrates: turning theory into practice. 2010 Jul;5(n1):114-119. [CrossRef]
- Garban F, Guyard A, Labussière H, Bulabois CE, Marchand T, Mounier C, Caillot D, Bay JO, Coiteux V, Schmidt-Tanguy A, Le Niger C, Robin C, Ladaique P, Lapusan S, Deconinck E, Rolland C, Foote AM, François A, Jacquot C, Tardivel R, Tiberghien P, Bosson JL; Evaluation of the Efficacy of Platelets Treated with Pathogen Reduction Process (EFFIPAP) Study Group. Comparison of the Hemostatic Efficacy of Pathogen-Reduced Platelets vs Untreated Platelets in Patients with Thrombocytopenia and Malignant Hematologic Diseases: A Randomized Clinical Trial. JAMA Oncol. 2018 Apr 1;4(4):468-475.
- Giménez-Richarte A, Ortiz de Salazar MI, Giménez-Richarte M, Larrea L, Arbona C, Marco P, Ramos-Rincón JM. Pathogen inactivation methods to prevent transfusion-transmissible arboviruses: A systematic review and meta-analysis. Trop Med Int Health. 2023 Apr;28(4):262-274. [CrossRef]
- Gorria C, Labata G, Lezaun M, López FJ, Pérez Aliaga AI, Pérez Vaquero MÁ. Impact of implementing pathogen reduction technologies for platelets on reducing outdates. Vox Sang. 2020 Feb;115(2):167-173. [CrossRef]
- Gravemann U, Boelke M, Könenkamp L, Söder L, Maurer M, Ziegler U, Schulze TJ, Seltsam A, Becker SC, Steffen I. West Nile and Usutu viruses are efficiently inactivated in platelet concentrates by UVC light using the THERAFLEX UV-Platelets system. Vox Sang. 2024 May 3. [CrossRef]
- Gravemann U, Handke W, Müller TH, Seltsam A. Bacterial inactivation of platelet concentrates with the THERAFLEX UV-Platelets pathogen inactivation system. Transfusion. 2019; 59(4):1324-1332. [CrossRef]
- Grégoire Y, Delage G, Custer B, Rochette S, Renaud C, Lewin A, Germain M. Cost-effectiveness of pathogen reduction technology for plasma and platelets in Quebec: A focus on potential emerging pathogens. Transfusion. 2022 Jun;62(6):1208-1217. [CrossRef]
- Guide to the preparation, use and quality assurance of Blood Components. European Committee EDQM. 21th Edition 2023. https://freepub.edqm.eu/publications/AUTOPUB_48/detail.
- Hechler B, Ohlmann P, Chafey P, Ravanat C, Eckly A, Maurer E, Mangin P, Isola H, Cazenave JP, Gachet C. Preserved functional and biochemical characteristics of platelet components prepared with amotosalen and ultraviolet A for pathogen inactivation. Transfusion. 2013 Jun;53(6):1187-200. [CrossRef]
- Hellstern P, Solheimb BG. The Use of Solvent/Detergent Treatment in Pathogen Reduction of Plasma. Transfus Med Hemother. 2011 Feb; 38(1): 65–70. [CrossRef]
- Hong H, WX, Lazarus HM, Good CE, Maitta RW, Jacobs MR. Detection of septic transfusion reactions to platelet transfusions by active and passive surveillance. Blood. 2016 Jan 28;127(4):496-502.
- Kasirye R, Hume HA, Bloch EM, Lubega I, Kyeyune D, Shrestha R, Ddungu H, Musana HW, Dhabangi A, Ouma J, Eroju P, de LangeT, Tartakovsky M, White JL, Kakura C, Glenn Fowler M, Musoke P, Nolan M, Grabowski MK, Moulton LH, Stramer SL, Whitby D, Zimmerman PA, Wabwire D, Kajja I, McCullough J, Goodrich R, Quinn TC, Cortes R, Ness PM, Tobian AAR. The Mirasol Evaluation of Reduction in Infections Trial (MERIT): study protocol for a randomized controlled clinical trial. 2022 Apr 4;23(1):257. [CrossRef]
- Jimenez-Marco T, Garcia-Recio M, Girona-Llobera E. Our experience in riboflavin and ultraviolet light pathogen reduction technology for platelets: from platelet production to patient care. Transfusion. 2018 Aug;58(8):1881-1889. [CrossRef]
- Keltner NM, Cushing MM, Haas T, Spinella PC. Analyzing and modeling massive transfusion strategies and the role of fibrinogen-How much is the patient actually receiving? Transfusion. 2024 May:64 Suppl 2:S136-S145. [CrossRef]
- Kerkhoffs JLH, van Putten WLJ, Novotny VMJ, Te Boekhorst PAW, Schipperus MR, Zwaginga JJ, van Pampus LCM, de Greef GE, Luten M, Huijgens PC, Brand A, van Rhenen DJ, Dutch - Belgian HOVON cooperative group. Clinical effectiveness of leucoreduced, pooled donor platelet concentrates, stored in plasma or additive solution with and without pathogen reduction. Br J Haematol. 2010 Jul;150(2):209-17. [CrossRef]
- Kim S, Handke W, Gravemann U, Döscher A, Brixner V, Müller TH, Seltsam A. Mitochondrial DNA multiplex real-time polymerase chain reaction inhibition assay for quality control of pathogen inactivation by ultraviolet C light in platelet concentrates. Transfusion. 2018 Mar;58(3):758-765. [CrossRef]
- Klein HG, Dodd RY, Dzik WH, Luban NL, Ness PM, Pisciotto P, Schiff PD, Snyder EL. Current status of solvent/detergent-treated frozen plasma. Transfusion. 1998 Jan;38(1):102-7. [CrossRef]
- Koepsell SA, Stolla M, Sedjo RL, Carson J, Knudson M, Cook R, Fasano R, Ngamsuntikul SG, Cohn C, Gorlin J, Delaney M, Slichter S, Ness P, McCullough J. Results of clinical effectiveness of conventional versus Mirasol-treated Apheresis Platelets in Patients with Hypoproliferative Thrombocytopenia (MiPLATE) trial. Transfusion. 2024 Mar;64(3):457-465. [CrossRef]
- Infanti L, Holbro A, Passweg J, Bolliger D, Tsakiris DA, Merki R, Plattner A, Tappe D, Irsch J, Lin JS, Corash L, Benjamin RJ, Buser A. Clinical impact of amotosalen-ultraviolet A pathogen-inactivated platelets stored for up to 7 days. Transfusion. 2019 Nov;59(11):3350-3361. [CrossRef]
- INTERCEPT Platelets, Technical Data Sheet https://www.interceptbloodsystem.com/sites/default/files/resources/prd-tds_00121_v10.0_reduced_file_size_-_secured.pdf.
- Lanteri MC, Santa-Maria F, Laughhunn A, Girard YA, Picard-Maureau M, Payrat JM, Irsch J, Stassinopoulos A, Bringmann P. Inactivation of a broad spectrum of viruses and parasites by photochemical treatment of plasma and platelets using amotosalen and ultraviolet A light. Transfusion. 2020 Jun;60(6):1319-1331. [CrossRef]
- Larrea L, Ortiz-de-Salazar MI, Martínez P, Roig R. Quantitative analysis of plasma proteins in whole blood-derived fresh frozen plasma prepared with three pathogen reduction technologies. Transfus Apher Sci. 2015 Jun;52(3):305-10. [CrossRef]
- Li J, de Korte D, Woolum MD, Ruane PH, Keil SD, Lockerbie O, McLean R, Goodrich RP. Pathogen reduction of buffy coat platelet concentrates using riboflavin and light: comparisons with pathogen-reduction technology-treated apheresis platelet products. Vox Sang. 2004 Aug;87(2):82-90. [CrossRef]
- Lieberman L, Devine DV, Reesink HW, Panzer S, Wong J, Raison T, Benson S, Pink J, Leitner GC, Horvath M, Compernolle V, Prado Scuracchio PS, Wendel S, Delage G, Nahirniak S, Dongfu X, Krusius T, Juvonen E, Sainio S, Cazenave JP, Guntz P, Kientz D, Andreu G, Morel P, Seifried E, Hourfar K, Lin CK, O'Riordan J, Raspollini E, Villa S, Rebulla P, Flanagan P, Teo D, Lam S, Ang AL, Lozano M, Sauleda S, Cid J, Pereira A, Ekermo B, Niederhauser C, Waldvogel S, Fontana S, Desborough MJ, Pawson R, Li M, Kamel H, Busch M, Qu L, Triulzi D. Prevention of transfusion-transmitted cytomegalovirus (CMV) infection: Standards of care. Vox Sang. 2014 Oct;107(3):276-311. [CrossRef]
- Lozano M, Knutson F, Tardivel R, Cid J, Maymó RM, Löf H, Roddie H, Pelly J, Docherty A, Sherman C, Lin L, Propst M, Corash L, Prowse C. A multi-centre study of therapeutic efficacy and safety of platelet components treated with amotosalen and ultraviolet A pathogen inactivation stored for 6 or 7 d prior to transfusion. Br J Haematol. 2011 May;153(3):393-401. [CrossRef]
- Mathai J, Resmi KR, Sulochana PV, Sathyabhama S, Saritha GB, Krishnan LK. Suitability of measurement of swirling as a marker of platelet shape change in concentrates stored for transfusion. Platelets. 2006 Sep;17(6):393-6. [CrossRef]
- McCullough J, Vesole DH, Benjamin RJ, Slichter SJ, Pineda A, Snyder E, Stadtmauer EA, Lopez-Plaza I, Coutre S, Strauss RG, Goodnough LT, Fridey JL, Raife T, Cable R, Murphy S, Howard F, Davis K, Lin JS, Metzel P, Corash L, Koutsoukos A, Lin L, Buchholz DH, Conlan MG.Therapeutic efficacy and safety of platelets treated with a photochemical process for pathogen inactivation: the SPRINT Trial. Blood. 2004 Sep 1;104(5):1534-41.
- McCullough J, Goldfinger D, Gorlin J, Riley WJ, Sandhu H, Stowell C, Ward D, Clay M, Pulkrabek S, Chrebtow V, Stassinopoulos A. Cost implications of implementation of pathogen-inactivated platelets. Transfusion. 2015 Oct;55(10):2312-20. [CrossRef]
- Murphy S, Snyder E, Cable R, Slichter SJ, Strauss RG, McCullough J, Lin J, Corash L, Conlan MG, SPRINT Study Group. Platelet dose consistency and its effect on the number of platelet transfusions for support of thrombocytopenia: an analysis of the SPRINT trial of platelets photochemically treated with amotosalen HCl and ultraviolet A light. Transfusion. 2006 Jan;46(1):24-33. [CrossRef]
- Norris PJ, Kaidarova Z, Maiorana E, Milani S, Lebedeva M, Busch MP, Custer B, Rebulla P. Ultraviolet light-based pathogen inactivation and alloimmunization after platelet transfusion: results from a randomized trial. Transfusion. 2018 May;58(5):1210-1217. [CrossRef]
- Nussbaumer W, Amato M, Schennach H, Astl M, Chen CY, Lin JS, Corash L, Benjamin RJ. Patient outcomes and amotosalen/UVA-treated platelet utilization in massively transfused patients. Vox Sang. 2017 Apr;112(3):249-256. [CrossRef]
- Ohlsson S, Diedrich B, Uhlin M, Sandgren P. Optimized processing for pathogen inactivation of double-dose buffy-coat platelet concentrates: maintained in vitro quality over 7-day storage. Vox Sang. 2018 Oct;113(7):611-621.
- Ojea AM, Seco C, Mata P, Muñoz MDC, Álvarez Argüelles ME, Rodríguez-Frías F, Quer Sivila J, Rando Segura A, García-Gala JM, Rodriguez M. Transfusion-transmission of hepatitis E virus through red blood cell transfusion but not through platelet concentrates: A case report from Spain. Transfusion. 2023 Sep;63(9):1767-1772. [CrossRef]
- Osman A, Hitzler WE, Meyer CU, Landry P, Corduan A, Laffont B, Boilard E, Hellstern P, Vamvakas EC, Provost P. Effects of pathogen reduction systems on platelet microRNAs, mRNAs, activation, and function. Platelets. 2015;26(2):154-63. [CrossRef]
- Osman A, Hitzler WE, Provost P. Peculiarities of studying the effects of pathogen reduction technologies on platelets Proteomics Clin Appl. 2016 Aug;10(8):805-15.
- Osselaer JC, Doyen C, Defoin L, Debry C, Goffaux M, Messe N, Van Hooydonk M, Bosly A, Lin JS, Lin L, Corash L. Universal adoption of pathogen inactivation of platelet components: impact on platelet and red blood cell component use. Transfusion. 2009 Jul;49(7):1412-22. [CrossRef]
- Owada T, Kaneko M, Matsumoto C, Sobata R, Igarashi M, Suzuki K, Matsubayashi K, Mio K, Uchida S, Satake M, Tadokoro K. Establishment of culture systems for Genotypes 3 and 4 hepatitis E virus (HEV) obtained from human blood and application of HEV inactivation using a pathogen reduction technology system. Transfusion. 2014 Nov;54(11):2820-7. [CrossRef]
- Pati I, Masiello F, Pupella S, Cruciani M, De Angelis V. Efficacy and Safety of Pathogen-Reduced Platelets Compared with Standard Apheresis Platelets: A Systematic Review of RCTs. Pathogens. 2022 Jun 1;11(6):639. [CrossRef]
- Piccin A, O'Connor-Byrne N, Daves M, Lynch K, Farshbaf AD, Martin-Loeches I. Autoimmune disease and sickle cell anaemia: 'Intersecting pathways and differential diagnosis'. Br J Haematol. 2022 Jun;197(5):518-528. [CrossRef]
- Pitman JP, Payrat JM, Park MS, Liu K, Corash L, Benjamin RJ. Longitudinal analysis of annual national hemovigilance data to assess pathogen reduced platelet transfusion trends during conversion to routine universal clinical use and 7-day storage. Transfusion. 2023 Apr;63(4):711-723. [CrossRef]
- Pohler P, Müller M, Winkler C, Schaudien D, Sewald K, Müller T H, & Seltsam A. Pathogen reduction by ultraviolet C light effectively inactivates human white blood cells in platelet products. Transfusion 2015; 55(2):337-347. [CrossRef]
- Praditya D, Friesland M, Gravemann, U, Handke W, Todt D, Behrendt P, Müller TH, Steinmann E and Seltsam A, Hepatitis E virus is effectively inactivated in platelet concentrates by ultraviolet C light. Vox Sang. 2020; 115:555-561. [CrossRef]
- Prati, D. Improving the safety of platelet transfusions by UV-C: Let's go back to the bench. Haematologica 2021;106(4):926-927. [CrossRef]
- Ramirez-Arcos S, Evans S, McIntyre T, Pang C, Yi QL, DiFranco C, Goldman M. Extension of platelet shelf life with an improved bacterial testing algorithm. Transfusion. 2020 Dec;60(12):2918-2928. [CrossRef]
- Rebulla P, Vaglio S, Beccaria F, Bonfichi M, Carella A, Chiurazzi F, Coluzzi S, Cortelezzi A, Gandini G, Girelli G, Graf M, Isernia P, Marano G, Marconi M, Montemezzi R, Olivero B, Rinaldi M, Salvaneschi L, Scarpato N, Strada P, Milani S, Grazzini G. Clinical effectiveness of platelets in additive solution treated with two commercial pathogen-reduction technologies. Transfusion. 2017 May;57(5):1171-1183. [CrossRef]
- Rebulla P, Prati D. Pathogen reduction for platelets-a review of recent implementation strategies. Pathogens 2022;11(2):142. [CrossRef]
- Rosskopf K, Helmberg W, Schlenke P. Pathogen reduction of double-dose platelet concentrates from pools of eight buffy coats: Product quality, safety, and economic aspects. Transfusion. 2020 Sep;60(9):2058-2066. [CrossRef]
- Seed CR, Hewitt PE, Dodd RY, Houston F, Cervenakova L. Creutzfeldt-Jakob disease and blood transfusion safety. Vox Sang. 2018 Apr;113(3):220-231. [CrossRef]
- Seltsam A, Müller TH. UVC Irradiation for Pathogen Reduction of Platelet Concentrates and Plasma. Transfus Med Hemother. 2011;38(1):43-54. [CrossRef]
- Sim J, Tsoi WC, Lee CK, Leung R, Lam CCK, Koontz C, Liu AY, Huang N, Benjamin RJ, Vermeij HJ, Stassinopoulos A, Corash L, Lie AKW. Transfusion of pathogen-reduced platelet components without leukoreduction. Transfusion. 2019 Jun;59(6):1953-1961. [CrossRef]
- Stanworth SJ, New HV, Apelseth TO, Brunskill S, Cardigan R, Doree C, Germain M, Goldman M, Massey E, 86 D, Shehata N, So-Osman C, Thachil J. Effects of the COVID-19 pandemic on supply and use of blood for transfusion. Lancet Haematol. 2020 Oct;7(10):e756-e764. Epub 2020 Jul 3. PMCID: PMC7333996. [CrossRef] [PubMed]
- Stivala S, Gobbato S, Infanti L, Reiner MF, Bonetti N, Meyer SC, Camici GG, Lüscher TF, Buser A, Beer JH. Amotosalen/ultraviolet A pathogen inactivation technology reduces platelet activatability, induces apoptosis and accelerates clearance. Haematologica. 2017 Oct;102(10):1650-1660.
- Schulze TJ, Graveman U, Seltsam A. THERAFLEX ultraviolet C (UVC)-based pathogen reduction technology for bacterial inactivation in blood components: advantages and limitations. Annals of Blood 30 Sept 2002. [CrossRef]
- White SK, Schmidt RL, Walker BS, Metcalf RA. Bacterial contamination rate of platelet components by primary culture: a systematic review and meta-analysis. Transfusion. 2020 May;60(5):986-996. [CrossRef]
- Yarranton H, Lawrie AS, Purdy G, Mackie IJ, Machin SJ. Comparison of von Willebrand factor antigen, von Willebrand factor-cleaving protease and protein S in blood components used for treatment of thrombotic thrombocytopenic purpura. Transfus Med. 2004 Feb;14(1):39-44.
- Yonemura S, Hartson L, Dutt TS, Henao-Tamayo M, Goodrich R, Marschner S. Preservation of neutralizing antibody function in COVID-19 convalescent plasma treated using a riboflavin and ultraviolet light-based pathogen reduction technology. Vox Sang. 2021 Nov;116(10):1076-1083. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).