1. Introduction
The coronavirus SARS-CoV-2 was identified as the etiologic agent of a newly emerging clinical picture named COVID-19 (Coronavirus Disease) [
1]. This syndrome is characterized by respiratory manifestations from mild cough, asthenia, and fever to severe acute distress syndrome and sepsis. Other less common symptoms are neurological (headache, anosmia, dysgeusia), cardiovascular (thromboembolism, myocarditis, shock), digestive (diarrhea, vomiting), and skin [
2]. Despite the limited scientific evidence, an increase in perioperative morbidity and mortality in surgical patients with SARS-CoV-2 infection has been reported [
3].
At present, there are no protocols and guidelines for the administration of drugs and non-pharmacological analgesic measures to treat acute postoperative pain in these patients, so multicenter studies are needed to adopt best practices. This is crucial in the global crisis caused by the SARS-CoV-2 pandemic, where greater efficiency is required in managing limited resources, using the minimum occupancy of operating rooms and hospital beds [
4,
5]. The use of opioids and other analgesic drugs could influence the evolution of the syndrome [
6], and the COVID-19 pandemic worsened the opioid crisis [
7].
PAIN OUT is an international project for quality improvement in postoperative pain management, registered in ClinicalTrials.gov with code NCT02083835, approved and financed by the European Commission; 7th Framework Programme (Grant Agreement no. 223590). This study registered variables of health conditions (cerebrovascular accidents, hypertension, heart disease, diabetes mellitus) and chronic treatments with corticosteroids, NSAIDs, and other medications used in the treatment of pain in surgical patients [
8,
9].
This study aimed to evaluate analgesic practices in perioperative treatment during the SARS- CoV-2 pandemic. The specific objectives were recording parameters collected in the PAIN OUT database in patients with positive serology to SARS-CoV-2, analgesic treatments, pain intensity, and infection severity data. Correlation between pain and analgesic treatment variables recorded in the Pain Out database and compared with surgical non-Covid patients.
2. Materials and Methods
A prospective study approved by the local Ethical Committee on April 30, 2020, with code PI 20-1774 in patients with positive SARS-CoV-2 serology (rapid antibody test or ELISA) or positive naso/oropharyngeal Polymerase Chain Reaction (PCR) swab, undergoing surgery in centers that expressed agreement and signed written informed consent to participation in the study, between June 16 and December 20, 2020, who met the inclusion criteria (more than 18 years aged, scheduled or urgent surgery in the hospitals participating in the study, positive serology for SARS-CoV-2 or positive PCR, with signed consent for entry into the study and do not meet exclusion criteria (no inclusion criteria, no signed study entry consent acceptance, inability to understand the questionnaire: hearing impairment, cognitive dysfunction, not fluent in the language of the questionnaire; and drug addicts.
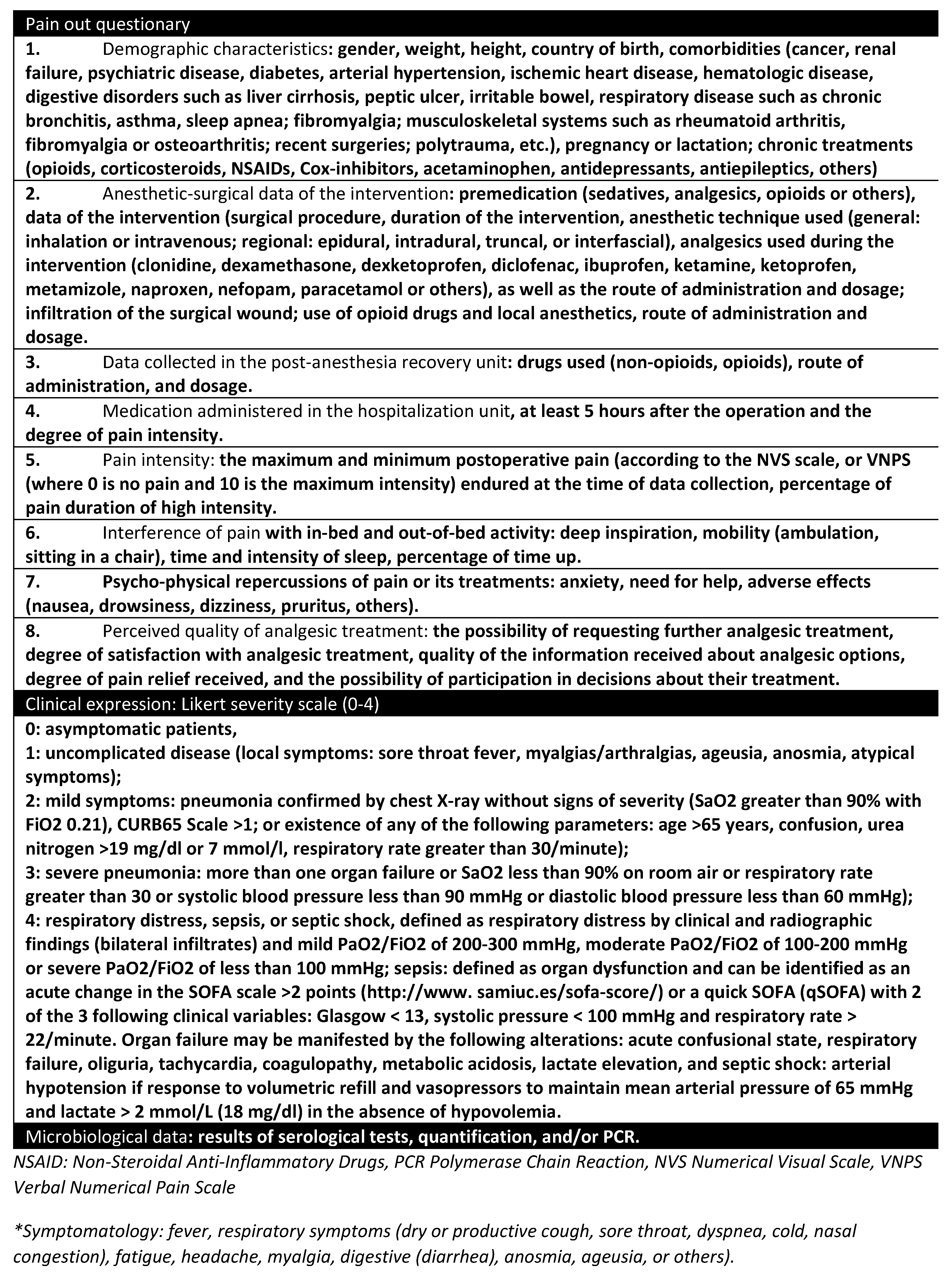
Data were recorded on the comorbidities most frequently associated with expressions of COVID-19 severity and variables collected in the Pain Out database and clinical expression data as it recorded the variables summarized in
Table 1.
In all cases, the delivery of the questionnaires to the patients and the entry of the data in the database designed for the study were carried out by researchers outside the healthcare personnel responsible for the patient´s care. Data were collected at three points in time: in the immediate postoperative period (in the first 24 hours after the end of the operation and at least 6 hours later), one week, and one month after the operation.
Finally, statistical analysis of all the data collected in the study. To define the continuous variables, the mean was used as a measure of central tendency and the standard deviation as a measure of dispersion. The Shapiro-Wilk test was applied to demonstrate the tendency of a normal distribution in the quantitative and qualitative variables according to their frequency distribution.
The sample size was calculated taking into account a population of 1,006 people with laboratory COVID-19 diagnostic and surgical indication, a margin of error of 10%, and a confidence interval of 95%, obtaining a result of 88 patients.
The association of qualitative variables was analyzed using Pearson´s Chi-square test. If the number of cells with expected values less than 5 is greater than 20%, Fisher´s exact test or the likelihood ratio test for variables with more than two categories was used. Significant values were considered in the case of p-values ≤ 0.05.
In case of correlation between postoperative pain intensity, certain drugs recorded, and disease evolution data, Fisher´s exact test was used, after designing the necessary 2×2 contingency tables. The statistical data analysis was performed by applying descriptive statistics using the SPSS vs. 22 statistical packages for Windows.
3. Results
During the study period, 10,702 COVID-19 patients were assisted in hospital centers, and 2,980 (27.84%) of them were scheduled for surgery. Their age was 64.77 +/- 21.10 (0-105) years and the gender distribution was predominantly female (1,934 patients) (54.9%). COVID-19 or a compatible clinic attended the majority (88.63%) of patients (9,485), but only 1,006 cases had a laboratory-confirmed diagnosis (10.61%). A mortality rate of 24.1% (2,575 cases) was recorded.
Data from 2,425 surgical patients were analyzed, who had undergone major surgeries included in the Pain Out database. under thoracic, general, digestive, otorhinolaryngology, urology, vascular, plastic, pediatric, neurosurgery, and cardiac surgeries. (
Table 2).
After crossing the databases of hospitalized patients and the patients undergoing surgeries studied in the PainOut study, only 604 met the study criteria. Among these 604 patients, 41 patients had a laboratory-confirmed diagnosis of COVID-19 disease at the time of the procedure (6.8%), 143 (23.7%) presented compatible symptoms and there was no information in 387 patients (64.1 %). Only 33 patients (5.5%) had laboratory confirmation of being free of SARS-Cov2. (
Table 3).
Data from 277 patients registered in the Pain Out database were analyzed, during the study period; 87 of them with a clinical/radiological or microbiological diagnosis of COVID-19. The sample population was 67.55 +/- 15.714 (27-97) years aged; with predominance of the male gender (47 men and 40 women). The data that could be obtained from the PainOut study questionnaire were studied. (
Table 4)
Postoperative mortality was recorded in 22 patients (25.3%) one month after surgery. The surgeries were as follows: tracheotomy in 11 patients, right colectomy (2), femoral osteosynthesis (2), thoracoscopy (1), surgical wound dehiscence (1), radical hysterectomy (1), femoral-popliteal bypass (1), pectoral hematoma (1), sigmoidectomy (1) and intestinal resection and anastomosis (1). All of them presented confirmed COVID-19.
General anesthesia was more frequently used (67 cases, 77%) versus regional (18 cases, 20.7%) or sedation (2 cases, 2.3%).
Symptoms compatible with Covid appeared in only 21 cases (24.1%). In 54 cases (62.1%), after a negative preoperative PCR test, the laboratory result was positive during postoperative admission.
Of the 87 patients studied, 61 (70.1%) had risk factors included in the Pain out study. There were 4 cases of depression (4.6%), 3 strokes (3.4%), 11 dyslipidemia (12.6%), 13 arterial hypertension (14.9%), 8 alcoholism (9.2%), 2 psychiatric diseases (2.3%), 8 type 2 diabetes (9.2%), 1 asthma (1.1%), 3 irritable bowel syndrome (3.4%), 10 cancer (11.5%), 2 coronary heart disease (2, 3%), 2 patients cirrhosis (2.3%), 2 osteoporosis (2.3%), 7 renal failure (8%), 4 anemia (4.6%), 10 atrial fibrillation (11.5%), 4 pulmonary thromboembolism (PTE) (4.6%), 3 deep vein thrombosis (DVT) (3.4%), 3 obesity (3.4%), 10 smokers (11.5%) and 9 former smokers (10.3%).
Regarding chronic treatments, 2 patients were taking corticosteroids (2.3%), and 38 (43.7%) were taking opioids/IECAs or NSAIDs.
Data from 190 no-COVID-19 surgical patients registered in the Pain Out database were compared with the 87 COVID-19 patients operated on during the study period.
General anesthesia was the most frequently used technique in COVID-19 (77% of cases) versus locoregional anesthesia in no-COVID (56%). The differences were significant with p≤0.01.
There were no significant differences in gender between groups, with a greater predominance of the male sex in COVID (54%) compared to no-COVID (50.2%).
The presence of comorbidities was higher in COVID (69%) than in no-COVID (32.1%), with a statistical significance of p<0.001. Risk factors related to the occurrence of chronic pain appeared significant differences (p<0.05) in alcoholism (higher in COVID), inflammatory bowel disease (higher in COVID); renal failure (higher in COVID), and obesity (higher in no-COVID).
The chronic drug treatments associated with increased incidence or severity of SARS-Cov2 infection, including opioids, angiotensin-converting enzyme inhibitors, and nonsteroidal anti-inflammatory drugs (NSAID) were found in 26 (29.9%) of the patients studied.
The enrollment of patients on chronic opioid therapy was significantly higher (p=0.001) in no-COVID base (20%) versus COVID (4.6%). The most commonly used were transdermal fentanylor oral morphine.
NSAIDs were used in higher proportion (p≤0.001) in no-COVID (57.3%) than in COVID (17.2%).
Angiotensin inhibitors were used in 10.3% of COVID-19 patient cases. (
Table 5)
4. Discussion
Surgical activity had to be interrupted due to the extraordinary demand for medical care caused by the pandemic. In Leon and Castille, in Spain, 22,135 patients were attended, and 10,702 (48.35%) of them required hospital admission. This resulted in an overload of the hospital system. Only 2,980 were operated on. This would be equivalent to less than one-tenth of the usual surgical activity [
10].
In our work, 9,425 (81%) of the hospitalized patients were attended by COVID-19 or a compatible clinic, but only 1,006 of them (13.5%) presented conclusive laboratory tests (PCR tests or serology). This fact is by Arevalo-Rodriguez et al´s article, where they included 34 studies enrolling 12,057 COVID-19 confirmed cases. The findings reinforce the need for repeated testing in patients with suspicion of SARS-Cov-2 infection given that up to 54% of COVID-19 patients may have an initial false-negative RT-PCR [
11].
Despite a negative preoperative PCR test, the laboratory result was positive in 62.1% of the cases after surgery. This may be due to the low negative predictive value of the test used or to the low clinical expressivity of the new SARS-Cov-2 variants. In contrast, retrospective studies such as that of Mavrothalassitis et al concluded that outcomes of patients undergoing surgery and 30-day mortality after surgery were not compromised even in states with the highest severity of COVID-19 in patients undergoing surgery during the first wave of the COVID-19 pandemic in 2020. [
12]
A mortality rate of 24.1% was very high and the most frequent cause of hospital admission was COVID-19. These data are in line with published mortality data for 2020, where 493,776 deaths were recorded and Covid was the leading cause with 60,358 in Spain [
13]; the Kivrak S et al´s study, which found postoperative mortality of 25.3% one month after surgery in COVID-19 patients [
14], and the multicenter study in 2,132 from 25 Spanish hospitals found similar rates of 30-day mortality among surgical patients with and without SARS-CoV-2 infection (12.6% vs. 4.6%) [
15]. However, other studies described that SARS-CoV-2 infection was associated with higher rates of 90-day mortality and 30-day postoperative complications [
16].
General anesthesia was the most frequently used technique in COVID-19 patients (77% of cases) versus locoregional anesthesia (56%), despite recommendations of various scientific societies to avoid aerosol-generating procedures, such as intubation or airway management maneuvers and preservation of respiratory function with regional anesthesia techniques [
17,
18,
19,
20].
In addition, several publications have demonstrated the presence of thrombopenia in COVID-19 patients, and therefore, the possible contraindication to regional blockades [
21,
22,
23].
Of the patients studied, 70.1% had risk factors listed in the Pain Out database, the most frequent being hypertension (14.9%), dyslipidemia (12.6%), atrial fibrillation (11.5%), and smokers (11.5%), and former smokers (10.3%). All of them associated were with high mortality [
24]. This finding could explain the high mortality recorded, in line with Silvapulle´s article that recommended hospitalized or persistent symptoms patients, undergo targeted organ-specific assessment using a combination of echocardiography, lung function tests, and biomarkers to provide quantitative estimation of perioperative risk [
25]. Such information is crucial for the complex surgical decision-making and counseling of patients presenting with positive SARS-CoV-2 infection status. Further studies are required to understand the impact of new variants, large-scale vaccination, and new therapeutics on the postoperative outcomes of COVID-19 patients [
26].
It has been proven significantly higher rates of mortality and postoperative complications, especially thromboembolic events, among patients with perioperative SARS-CoV-2 infection compared with patients without SARS-CoV-2 infection. Moreover, matched SARS-CoV-2–infected patients had a higher risk of mortality even if they were asymptomatic at presentation [
27].
Symptoms compatible with COVID-19 appeared in only 24.1% of patients, but in 62.1% of them, after a negative preoperative PCR test, the laboratory result was positive during postoperative admission. This could be explained by the low negative predictive value of PCR, together with contact with asymptomatic patients not diagnosed with COVID-19. These results are in line with Rose´s article which concluded that nucleic acid amplification confirmation is crucial, however, can make nucleic acid amplification in active COVID-19 infections unnecessary and testing cost-efficient [
28].
The mortality that was registered was high but similar to other registries in critical patients [
29] and the excess mortality rate due to the COVID-19 pandemic. [
30] The difference between excess mortality and reported COVID-19 deaths might be a function of underdiagnosis due to insufficient testing, reporting challenges, or higher-than-expected mortality from other diseases due to pandemic-related changes in behaviors or reduced access to health care or other essential services.
The presence of certain risk factors such as age (younger than 54 years), preoperative pain in the surgical area, female gender, duration of surgery longer than 90 minutes, preoperative opioid administration, anxiety, and the need for help with pain have been associated with a higher frequency and longer time of severe postoperative pain and the need for more analgesic treatment [
31]. Stamenkovic´s study demonstrated that a small set of evidence-based interventions is associated with improved outcomes in perioperative pain. The interventions were a full daily dose of 1 to 2 nonopioid analgesics (eg, paracetamol and/or nonsteroidal anti-inflammatory drugs), at least 1 type of local/regional anesthesia, pain assessment by staff, and offering patients information about pain management [
8].
Clinicians are now equipped with an armamentarium of therapies based on high-quality evidence to manage COVID-19 patients: anti-inflammatory agents, antivirals, antithrombotics, therapies for acute hypoxaemic respiratory failure, anti-SARS-CoV-2 (neutralizing) antibody therapies, modulators of the renin-angiotensin-aldosterone system and vitamins [
32]. In this study only 43.7% of patients were on opioids, angiotensin inhibitors, and non-steroidal anti-inflammatory drugs treatment; and 2.3% were treated with corticosteroids.
The study´s main limitation is that the recent description of Covid disease, together with the urgency of the pandemic situation, makes clinical suspicion and diagnosis of the disease difficult at the moment the study was done. Proof of this is the large number of errata published in the original studies on this topic. Currently, the most sensitive test is PCR of gold or nasopharyngeal exudate, although the false negative rate is high and depends on numerous factors. On the other hand, the study has the limitations inherent to the Pain Out study: numerous factors are involved in the appearance of postoperative pain (included in the study variables) and it is difficult to establish homogeneous groups for comparison; each center collects and analyzes its data using different statistical analysis methods. The high mortality recorded prevents extrapolation of the results to other COVID-19 patients with fewer preoperative risk factors.
In conclusion, despite the high percentage of patients with risk factors for developing severe postoperative pain, no special analgesic measures were applied. A large margin for
improvement is demonstrated in the application of multimodal perioperative analgesic
strategies and patient information. It was found greater intensity and duration of severe
postoperative pain, greater somnolence, pruritus, and dizziness in COVID-19 patients. The limitation of physical activity was lower and the index of perceived quality higher than in non-COVID patients.
The individualized study of the patients and the severity of the disease establishes the probability of postoperative complications in COVID-19 patients. Pain control must also take into account the variability among surgical patients.
Author Contributions
Conceptualization M.P.H. and H.R.; methodology: M.P.H., M.C. and B.V.; validation and formal analysis: M.C.; investigation and data curation: S.C. and C.R.; writing—original draft preparation: S.C., C.R.,M.P.H. and H.R.; writing—review and editing, H.R.; visualization, project administration, B.V. ; funding acquisition, M.P.H. All authors signed the manuscript have read the manuscript, attest to the validity and legitimacy of the data and their interpretation, and agree to submission to Surgeries.
Funding
This work is partially funding received from the Junta de Castilla y Leon, Spain (EXP. GRS 37/A/20).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Easth Health Area Ethical Committee on April 30, 2020, with code PI 20-1774.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Acknowledgments
The authors would like to thank BLINDED for their cooperation during this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Sabbah DA, Hajjo R, Bardaweel SK, et al. An Updated Review on SARS-CoV-2 Main Proteinase (e): Protein Structure and Small-Molecule Inhibitors. Curr Top Med Chem. 2021; 21: 442-460. [CrossRef]
- Hu B, Guo H, Zhou P, et al. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 2021; 19: 141-154.
- Kartsonaki C, Baillie JK, Barrio NG, et al. Characteristics and outcomes of an international cohort of 600,000 hospitalized patients with COVID-19. Int J Epidemiol 2023; 52: 355-376. [CrossRef]
- Gupta AK, Leslie A, Hewitt JN, et al. Cardiac Surgery in Patients with COVID-19: a systematic review and meta-analysis. ANZ J Surg 2022; 92: 1007-1014. [CrossRef]
- Paladini A, Rawal N, Coca Martinez M, et al. Advances in the Management of Acute Postsurgical Pain: A Review. Cureus. 2023 Aug 4; 15: e42974. [CrossRef]
- Farrow L, Gardner WT, Tang CC, et al. Impact of COVID-19 on opioid use in those awaiting hip and knee arthroplasty: a retrospective cohort study. BMJ Qual Saf 2023; 32: 479-484.
- Simha S, Ahmed Y, Brummett CM, et al. Impact of the COVID-19 pandemic on opioid adverse events in the USA and Canada: a systematic review. Reg Anesth Pain Med 2023; 48: 37-43.
- Stamenkovic D, Baumbach P, Radovanovic D, et al. The Perioperative Pain Management Bundle is Feasible: Findings From the PAIN OUT Registry. Clin J Pain. 2023; 39: 537-545. [CrossRef]
- Zaslansky R, Meissner W, Stamer UM. Insights from studying a large cohort of patients. Pain 2023; 164: 919-920.
- Gerencia de Salud Castilla y Leon. https://www.saludcastillayleon.es/institucion/es/biblioteca/materiales-consejeria-sanidad/buscador/memoria-2010-gerencia-regional-salud.ficheros/433826-MEMORIA_GRS_2010.pdf, consulted on 6th November 2023.
- Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al. False-negative results of initial RT-PCR assays for COVID-19: A systematic review. PLoS One 2020; 15: e0242958. [CrossRef]
- Mavrothalassitis O, Pirracchio R, Fong N, et al. Outcome of surgical patients during the first wave of the COVID-19 pandemic in US hospitals. Br J Anaesth 2022; 128: e35-e37. [CrossRef]
- Ministerio de Sanidad y Salud Publica, España. https://www.sanidad.gob.es/ciudadanos/pdf/Estrategia_de_Salud_Publica_2022.pdf, consulted on 6 February 2023.
- Kivrak S, Haller G. Scores for preoperative risk evaluation of postoperative mortality. Best Pract Res Clin Anaesthesiol 2021; 35: 115-134.
- Bozada-Gutiérrez K, Trejo-Ávila M, Moreno-Portillo M. Postoperative complications and predictors of mortality in patients with COVID-19. Cir Cir 2023; 91: 344-353.
- Osorio J, Madrazo Z, Videla S, et al. Analysis of outcomes of emergency general and gastrointestinal surgery during the COVID-19 pandemic. Br J Surg 2021; 108: 1438-1447. [CrossRef]
- Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2023; 401: e21-e33. [CrossRef]
- Kim HJ, Ko JS, Kim TY. Recommendations for anesthesia in patients suspected of COVID-19 Coronavirus infection. Korean J Anesthesiol 2020; 73:89-91.
- Ti LK, Ang LS, Foong TW, et al. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth 2020; 67:756-758.
- Wen X, Li Y. Anesthesia procedure of emergency operation for patients with suspected or confirmed COVID-19. Surg Infect 2020; 21: 299.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506. Erratum in: Lancet. 2020 Jan 30. Erratum in: Lancet 2020; 30 Feb 15;395(10223):496. [CrossRef]
- Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020; 506: 145–8.
- Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8:475-481. Erratum in: Lancet Respir Med 2020; 8: e26. [CrossRef]
- Shan Z, Wang F, Li Y, et al. Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality. JAMA Intern Med 2023; 183: 142-153. Erratum in: JAMA Intern Med 2023; 183:627. [CrossRef]
- Silvapulle E, Johnson D and Darvall JN. Risk stratification of individuals undergoing surgery after COVID-19 recovery. Br J Anaesth 2022; 128: e37-e39.
- Oodit R, Biccard BM, Panieri E, et al. Guidelines for Perioperative Care in Elective Abdominal and Pelvic Surgery at Primary and Secondary Hospitals in Low-Middle-Income Countries (LMIC's): Enhanced Recovery After Surgery (ERAS) Society Recommendation. World J Surg 2022; 46: 1826-1843. [CrossRef]
- Argandykov D, Dorken-Gallastegi A, El Moheb M, et al. Is perioperative COVID-19 associated with worse surgical outcomes? A nationwide COVIDSurg propensity-matched analysis. J Trauma Acute Care Surg 2023; 94: 513-524. [CrossRef]
- Rose O, Obarcanin E, Erzkamp S. Evaluating real-world data in COVID-19 antigen and PCR testing. Int J Clin Pharmacol Ther 2023; 61: 172-177.
- Rogers MP, DeSantis AJ, KUO PC, et al. Predictive modeling of in-hospital mortality following elective surgery. Am J Surg 2022; 223: 544-548.
- COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet 2022; 399: 1513-1536. Erratum in: Lancet 2022; 399:1468.
- Schnabel A, Yahiaoui-Doktor M, Meissner W, et al. They are predicting poor postoperative acute pain outcome in adults: an international, multicentre database analysis of risk factors in 50,005 patients. Pain Rep 2020; 5: e831.
- Murakami N, Hayden R, Hills T, et al. Therapeutic advances in COVID-19. Nat Rev Nephrol 2023; 19: 38-52. Erratum in: Nat Rev Nephrol 2023; 19: 38-52. [CrossRef]
Table 1.
Variables in the study.
Table 1.
Variables in the study.
Table 2.
Distribution of surgical interventions.
Table 2.
Distribution of surgical interventions.
| |
Frequency |
Percentage |
| |
Vascular surgeries |
131 |
.6 |
| Anesthesiology |
83 |
.4 |
| Cardiology |
547 |
2.5 |
| Cardiac surgery |
25 |
.1 |
| General and digestive surgery |
960 |
4.3 |
| Maxillofacial surgery |
12 |
.1 |
| Pediatric Surgery |
23 |
.1 |
| Plastic surgery |
73 |
.3 |
| Thoracic surgery |
59 |
.3 |
| Dermatology |
5 |
.0 |
| Digestive |
603 |
2.7 |
| Endocrinology |
16 |
.1 |
| Gynecology |
176 |
.8 |
| Geriatrics |
143 |
.6 |
| Hematology |
226 |
1.0 |
| Internal Medicine |
12850 |
58.1 |
| Intensive Medicine |
289 |
1.3 |
| Nuclear Medicine |
5 |
.0 |
| Nephrology |
223 |
1.0 |
| Neumology |
1562 |
7.1 |
| Neurosurgery |
162 |
.7 |
| Neurology |
448 |
2.0 |
| Obstetrics |
414 |
1.8 |
| Oftamology |
33 |
.1 |
| Medical Oncology |
461 |
2.1 |
| Radiation Oncology |
11 |
.0 |
| Otolaryngology |
214 |
1.0 |
| Pediatrics |
341 |
1.5 |
| Psychiatry |
273 |
1.2 |
| Radiology |
1 |
.0 |
| Rheumatology |
5 |
.0 |
| Orthopedics |
989 |
4.5 |
| Perinatal Care Unit |
77 |
.3 |
| Pain Unit |
34 |
.2 |
| Emergencies |
118 |
.5 |
| Urology |
527 |
2.4 |
| Renal transplant unit |
6 |
.0 |
| Transplant unit |
10 |
.0 |
| Total |
22,135 |
100.0 |
Table 3.
Preoperative PCR results in surgical Covid-19 patients.
Table 3.
Preoperative PCR results in surgical Covid-19 patients.
| |
Frequency |
Percentage |
Valid Percentage |
Accumulated percentage |
| Válido |
Negative |
33 |
5.5 |
5.5 |
5.5 |
| Positive |
41 |
6.8 |
6.8 |
12.3 |
| Possibility |
143 |
23.7 |
23.7 |
35.9 |
| No information |
387 |
64.1 |
64.1 |
100.0 |
| Total |
604 |
100.0 |
100.0 |
|
Table 4.
Characteristics of patients undergoing surgery with clinical suspicion of COVID-19 disease until June 30, 2020, at the Hospital Clínico Universitario de Valladolid. .
Table 4.
Characteristics of patients undergoing surgery with clinical suspicion of COVID-19 disease until June 30, 2020, at the Hospital Clínico Universitario de Valladolid. .
| |
Mínimum |
Maximum |
Media |
Standard deviation |
| Duration (minutes) |
33 |
600 |
200.7 |
118.6 |
| Age (years) |
27 |
97 |
67.6 |
15.7 |
| Likert Scale (0-4) |
0 |
4 |
1.6 |
1.5 |
| Time in severe pain (hours) |
0 |
15 |
4.6 |
3.2 |
| Minimum pain intensity (EVA scale) |
0 |
6 |
1.1 |
1.6 |
| Maximum pain intensity (EVA Scale) |
0 |
9 |
5.7 |
2.2 |
| Interference of pain with movement in bed (0-10) |
0 |
7 |
2.3 |
2.4 |
| Time to get out of bed (hours) |
0 |
8 |
3.7 |
2.4 |
| Exacerbation of pain with cough (0-10) |
0 |
7 |
3.6 |
1.7 |
| Interference with sleep quality (0-10) |
0 |
8 |
4.4 |
2.9 |
| Out-of-bed activities (0-10) |
0 |
5 |
1.9 |
1.8 |
| Anxiety (0-10) |
0 |
10 |
4.8 |
3.2 |
| Need for help (0-10) |
0 |
10 |
3.8 |
3.1 |
| Nausea (0-10) |
0 |
9 |
1.7 |
2.5 |
| Drowsiness (0-10) |
0 |
9 |
3.7 |
2.7 |
| Itching (0-10) |
0 |
9 |
2.8 |
2.1 |
| Dizziness (0-10) |
0 |
8 |
3.8 |
2.3 |
| Perception of care (10-100) |
10 |
100 |
51.7 |
28.3 |
| Pain relief (0-10) |
2 |
10 |
6.6 |
2.5 |
| Participation (0-10) |
2 |
10 |
7.3 |
2.9 |
| Satisfaction (0-100) |
50 |
100 |
79.8 |
17.5 |
| Information received (0-100) |
50 |
100 |
81.7 |
17.6 |
Table 5.
Correlation in risk factors between COVID and no-COVID patients. Significant differences in bold type letter.
Table 5.
Correlation in risk factors between COVID and no-COVID patients. Significant differences in bold type letter.
| |
COVID-19 |
Non COVID-19 |
p |
| Arterial hypertension |
14.9 % |
11.5 % |
0.4 |
| Alcoholism |
9.2% |
0.9% |
0.01 |
| Psychiatric diseases |
2.8% |
4.6% |
0.4 |
| Diabetes |
9.2% |
7.8% |
0.7 |
| Type 1 diabetes |
0 |
6.9% |
0.07 |
| Type 2 diabetes |
9.2% |
0.9% |
0.01 |
| Asthma |
1 |
0 |
0.3 |
| Inflammatory bowel disease |
3.4% |
0 |
0.02 |
| Oncologic pathology |
11.5% |
12% |
0.99 |
| Chronic bronchitis |
0 |
1.4% |
0.56 |
| Coronary artery disease |
2.3% |
4.6% |
0.52 |
| Chronic corticosteroid therapy |
2.3% |
1.4% |
0.63 |
| Fibromyalgia |
0 |
0.5 % |
0.999 |
| Peptic ulcus |
0 |
0.5% |
0.999 |
| Cirrhosis |
2.3% |
0 |
0.081 |
| Rheumatoid arthritis |
0.5 % |
0.5% |
|
| Osteoporosis |
3.4% |
3.4% |
|
| Renal insufficiency |
8% |
2.8% |
0.057 |
| Renal insufficiency (dialysis) |
1.4% |
1.4% |
|
| Anemia |
4.6% |
2.9% |
0.7 |
| Smokers |
11.5% |
2.9% |
0.045 |
| Non smokers |
10.3% |
10.3% |
|
| Atrial fibrillation |
11.5% |
11.5% |
|
| Pulmonary thromboembolism |
4.6% |
4.6% |
|
| Deep vein thrombosis |
3.4% |
3.4% |
|
| Obesity |
3.4% |
15.1% |
0.005 |
| Chronic drug treatments* |
29.9% |
|
|
| Opioids |
4.6% |
20% |
0.001 |
| NSAIDs |
17.2% |
57.3% |
<0.001 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).