1. Introduction
Chronic low back pain (cLBP) represents a serious public problem and leading cause of disability worldwide that profoundly impacts both the quality of life of patients and healthcare costs (1). Alarming data indicates that LBP affected around 619 million people globally in 2020, with the overall burden of disability and the associated costs related to the disease expected to rise significantly in the coming decades (2). Available treatment modalities include pharmacological approach based on nonsteroidal anti-inflammatory drugs (NSAIDs), and non-pharmacological strategies involving physiotherapy and physical activities. Although therapy for chronic low back pain can be beneficial, it also has serious disadvantages such as incomplete efficacy, limited long-term solution, occurrence of side effects, and lack of impact on psychological aspects. Moreover, cost and accessibility represent barrier for majority of patients since therapy sessions are expensive and not always covered by health insurance [
3,
4,
5].
Balneotherapy (BT), which involves the use of mineral baths or thermal waters for therapeutic purposes, has been suggested as a promising treatment option for cLBP [
6]. It can exert numerous advantages in patients with cLBP such as pain relief, muscle relaxation, and improved physical function with fewer side effects compared to medications or invasive procedures, thus making it a safer solution for this condition [
6,
7]. Previous data suggest that BT also exert positive effects on mental health due to relaxation and sensory experience that result in stress and anxiety alleviation [
8]. However, there is a lack of comprehensive data that fully elucidates the connection between BT and its effects on functional status, quality of life, depression and mental disorders in individuals with cLBP. Available data on benefits of BT in cLBP is lacking and previous studies were mostly focused on elderly people, while assessing only specific impact on either pain reduction and physical functionality or quality of life [
4,
6,
7,
9]. Therefore, addressing multidimensional aspects of both physical and psychological effects of BT is essential for supporting health care providers by updating guidelines that will contribute to enhanced patient outcomes, quality of life and improve overall patient well-being.
Taking abovementioned facts into consideration, our goal was to assess the effects of BT on functional status, quality of life and psychological symptoms in patients with cLBP. These findings will contribute to updating clinical practice guidelines and advancing evidence-based practice in cLBP management.
2. Materials and Methods
This is an analytical cross-sectional study study that included 220 patients aged 18-65 years with cLBP. Examined patients included those admitted to Community Health Center Kragujevac, Serbia, as well as hospitalized patients with the aforementioned syndrome at the Special hospital for treatment and rehabilitation "Merkur" in Vrnjačka Banja, Serbia, who underwent a specific balneophysical treatment. The study was initiated with the approval of the Ethics Committee of Community Health Center Kragujevac (Date: 09.06.2014, Decision Number: 01-2117/1) and Ethics Committee of Special hospital for treatment and rehabilitation "Merkur" in Vrnjačka Banja (Date: 09.06.2014, Decision Number: 01-5617/6). All procedures were carried out in accordance with the ethical rules and the principles of the Declaration of Helsinki.
All the participants were given a written informed consent. Inclusion criteria for all patients were as follows: adults, both sexes, presence of back pain for more than 12 weeks, older than 18 years who voluntarily agree to participate in the study with confirmed non-specific cLBP. Non-specific cLBP syndrome was confirmed by the physician based on the medical history, clinical manifestations, negative laboratory indicators of inflammation (blood sedimentation, C-reactive protein and normal urine findings), the presence of pain for more than 12 weeks and a radiograph of the lumbosacral spine in two directions.
Exclusion factors for both groups were: less than 18 years age, subjects with cancer and metastases, pregnant women, inflammatory processes and conditions after surgical intervention due to wrong perception of pain, subjects with spinal canal stenosis, osteoporosis, osteoporotic fractures of the vertebral bodies, spondylitis, sacroilitis, osteomyelitis, subjects with diseases that lead to a reflex pain syndrome (kidney diseases, diseases of the small pelvis and abdominal organs), as well as people who refuse to participate in the research.
2.1. Assignment
Participants were assigned into groups: conventional therapy (CT) and balneotherapy (BT). Patients belonging to CT group were treated in Community Center Kragujevac and prescribed drug therapy included NSAIDs, analgesics, muscle relaxants, antidepressants. Patients filled out a set of questionnaires at the medical visit after completing the medical therapy. Patients belonging to BT group underwent spa treatment and were examined by a specialist in physical medicine upon admission to the spa. The doctor determined the type and number of sessions of BT based on the medical history, physical examination and review of the medical documentation. In this research, patients whose BT treatment lasted from 10 to 14 days were examined and they were examined after the treatment was completed, i.e. on the day of their discharge.
2.2. Evaluation Parameters
The demographic characteristics of the patients such as age, sex, height (m), weight (kg), body mass index (BMI) (kg/m2), disease duration and number of BT treatments were recorded.
The EQ-5D 3 stage version was used for assessment of health-related quality of life in patients with cLBP and comprises two pages of the EQ-5D descriptive system and the EQ-VAS (Visual Analog Scale). EQ-5D assesses five domains of quality of life (mobility, self-care, daily activities, mood, pain/discomfort) and EQ-VAS were used [
10]. The EQ-VAS included a thermometer-like scale, where the respondent evaluated their own state of health with grades from 0 (worst quality) to 100 (best). The EuroQol group approved the use of this questionnaire for the purposes of this research under number 20561.
VAS scale was used to assess the degree of pain and patients marks their pain severity on the 100 mm line, ranging from 0 to 100 mm. The distance from the lowest VAS value to the patient's mark indicates the numerical severity of their pain [
10].
Work Ability Index Questionnaire (WAI - Work Ability Index Questionnaire) - a standardized questionnaire of the Finnish Institute for Occupational Medicine, is used to examine work ability in relation to the requirements of the job or workplace. The use of this questionnaire is not conditional on obtaining a license [
11].
The Center of Epidemiologic Studies Depression Scale (CES-D) was used for assessing depression and to identify groups at risk for depression. It contains 20 items related to the frequency of symptoms during the last seven days [
12].
The Short Form 36 (SF-36) was used to evaluate quality of life and this scale consists of 36 questions related to health, through 8 domains: physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE) and mental health (MH). Total physical health (PCS -Physical Component Summary) summarizes PF, RP, BP and GH dimensions, while Total psychic health (MCS- Mental Component Summary) is based on the following domains: VT, SF, RE and MH. Scores of questions for each status are scored between 0 (worst health condition) and 100 (best health condition) [
13,
14]. A research license for the use of this standardized questionnaire is filed in the agreement under the number OPTUM#CT193013 OPO68219 OGSR.
2.3. Statistical Analysis
The Kolmogorov-Smirnov test was used to determine whether the distribution of the variables was suitable for normal distribution. Numeric variables were compared based on their distribution using either analysis of variance (ANOVA) for normally distributed variables or the Kruskal-Wallis test for those not following a normal distribution. Post hoc analysis utilized the Mann Whitney U-test and Bonferroni test. The chi-square test was used to compare qualitative data. Statistical significance was set at p < 0.05, as determined by SPSS version 20.
3. Results
3.1. Demographic Characteristic of Participants
A total of 210 patients with chronic non-specific low back pain syndrome were recruited and analyzed in the current study. The baseline characteristics of the study population are shown in
Table 1. The age in CT group was 44.01 ± 11.7 group, while in BT it was 48.95 ± 7.3 years. There was a significant association in age categories between treated groups (p=0.00). In patients belonging to CT group 50.91 % were female and 49.09 male, while in BT group 30.09 were female and 69.09 were male. The statistically significant difference was revealed between the examined groups in terms of gender distribution (p=0.003). Additionally, there was also statistically significant difference in BMI categories and disease duration between CT and BT groups (p=0.00).
3.2. Q-5D-3L Questionnaire and VAS Score
To determine whether there was a statistically significant difference in EQ-5D-3L descriptive system categories in CT and BT groups, Mann-Whitney U test was performed. There were statistically significant difference between patients receiving BT in terms of mobility and usual activities (p<0.05). On the other hand, there were no statistically significant difference in self-care, pain/discomfort and anxiety/depression between CT and BT groups (p>0.05) (
Table 2).
In order to reveal if there is an association between age, gender, BMI categories, disease duration and number of BTs and EQ-5D-3L descriptive system categories, Chi square test was performed. There was no association between gender, BMI groups, disease duration, number of BTs and EQ-5D-3L descriptive system categories (p>0.05), while there was a statistically significant interaction in terms of age categories (≤45 or >45 years) and self-care (p=0.04), usual activities (p=0.03) and anxiety/depression (p=0.038).
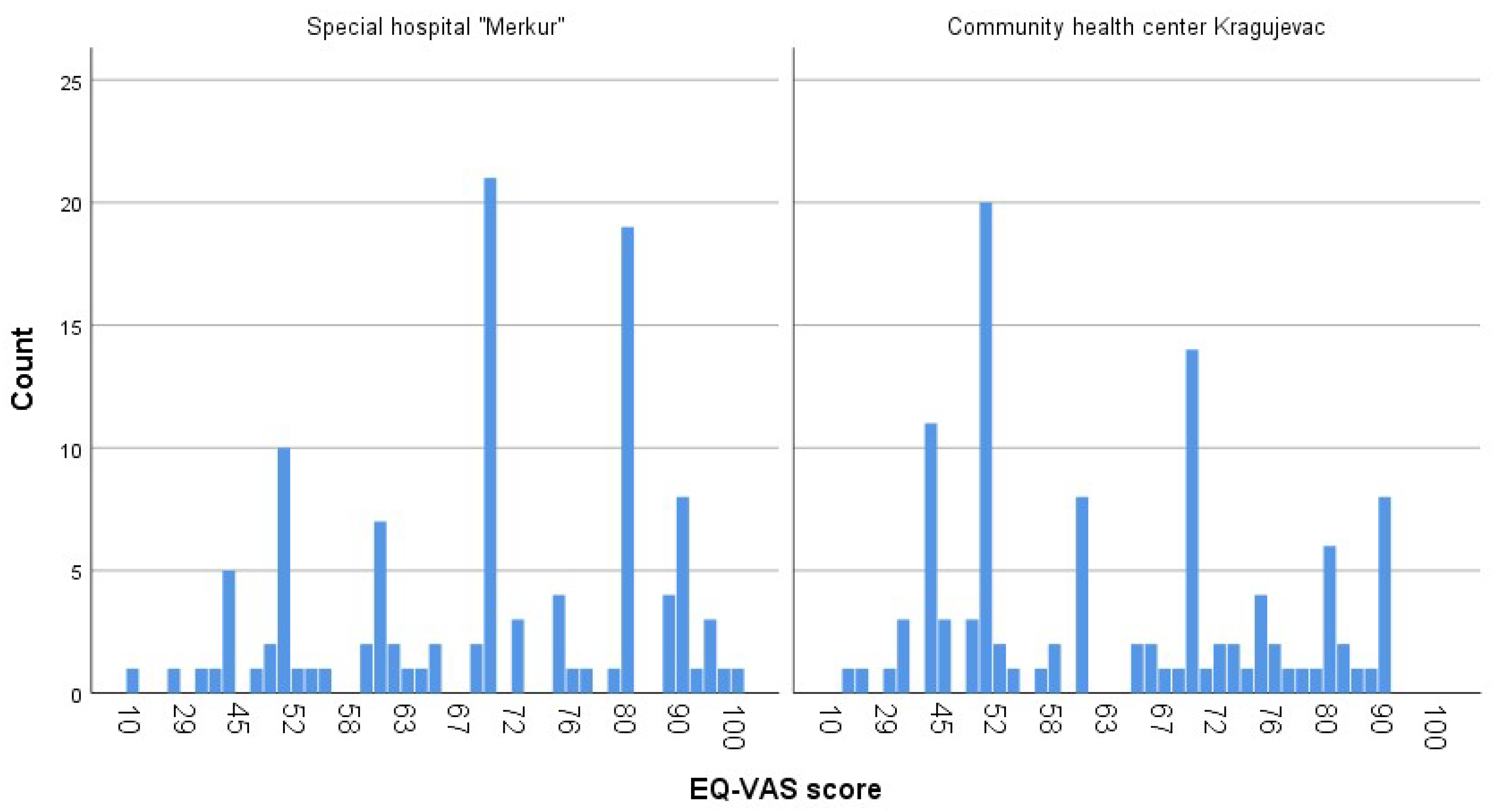
Visual analogue scale (EQ-VAS) overall health score was significantly lower in patients receiving CT (60.96 ± 17.16) compared to BT (68.46 ± 16.93) (p<0.05) (
Table 2).
Results for VAS score among patients are shown in
Table 3. VAS score was significantly higher in CT group of patients (54.7 ± 21.3) compared to BT group (45.7± 23.01).
Associations between sociodemographic, clinical characteristics and EQ VAS and VAS scores are shown in
Table 4.
Assessment of the factors associated with EQ VAS score revealed statistically significant interactions between patients ≤ 45 years and those older than 45. Younger patients had a significantly better EQ-VAS score and improved self-rated health (67.21 ± 16.8 vs 61.88 ± 16.9). Additionally, there was a significant association between disease duration and number of balneotherapies and VAS score (p<0.05) (
Table 4). Patients suffering from low back pain longer than 1 year had higher VAS score (52.44 ± 22.0) compared to those with established diagnosis for less than a year (44.52 ± 23.2). Moreover, patients who received more than one balneotherapies had significantly lower VAS score (46.41 ± 21.72) than those subjected to one therapy (52.02 ± 22.8). Otherwise, there was no statistically significant associations between other parameters and EQ VAS and VAS score (p>0.05) (
Table 4).
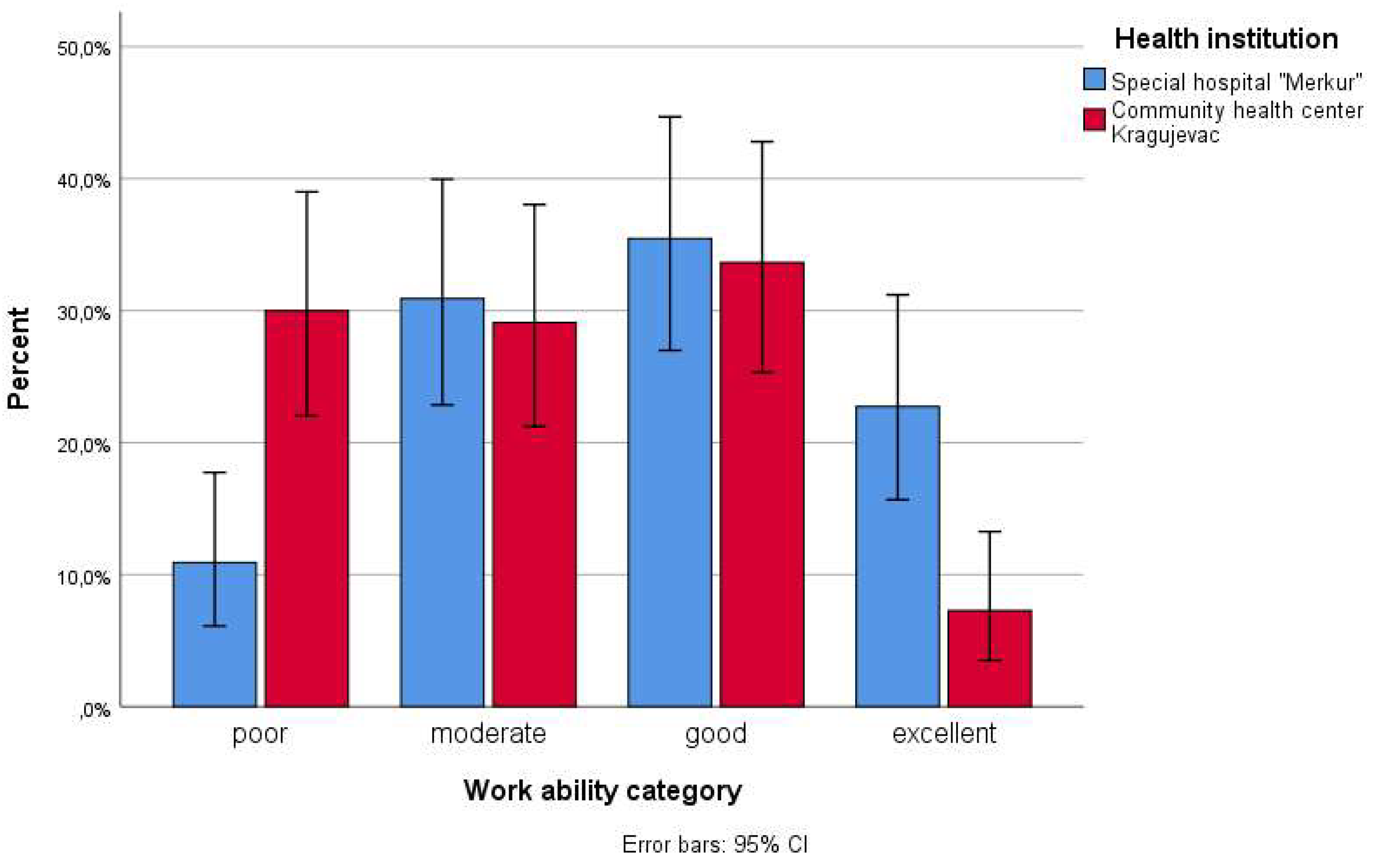
3.3. WAI Questionnaire
The average reported work ability as measured by the WAI was moderate i.e. 35.01± 7.67 points with 20.5% poor, 30% moderate, 34.5% good and 15% excellent work ability. Patients receiving BT reported statistically significantly higher WAI (36.89 ± 7.8 points) compared to CT group (33.14 ± 7.36 points) (
Table 5).
Associations between sociodemographic, clinical characteristics, and WAI are presented in
Table 6. The distribution of the WAI score varied significantly between the gender and different age, disease duration and number of BTs categories.
Mann–Whitney U Test showed that patients 45 years old and younger had statistically higher WAI than older ones (p<0.05). Additionally, male patients reported significantly higher WAI than female ones (36.05 ± 8.02 in male vs. 33.52 ± 6.81 in females) (p<0.05). Higher WAI scores were found in patients who had low back pain less than a year, than those with disease duration more than a year (36.84 ± 7.13 vs 34.30 ± 7.78). There was a significant difference in WAI between patients who received one and more than one balneotherapy (34.45 ± 7.62 for one balneotherapy and 36.20 ± 7.7 for more than one balneotherapy) (p<0.05).
Distribution of the work ability category between patients treated with conventional protocols and BT is presented in
Figure 2.
3.4. CES-D Scale
There was a statistically significantly lower CES-D score in patients receiving BT compared to CT, thus indicating the better the depression.
The distribution of the CES-D score varied significantly between the gender and age (
Table 8). Mann–Whitney U Test showed that patients 45 years old and younger had statistically lower CES-D score than older ones (p<0.05). Additionally, female patients had significantly higher CES-D than males (16.7 ± 4.11 in female vs. 12.11 ± 2.9 in males) (p<0.05).
3.5. SF-36 Questionnaire
To determine whether there was a statistically significant difference in SF-36 domains and their values in CT and BT groups, Mann-Whitney U test was performed. There were statistically significant difference between patients subjected to BT compared to CT in terms of all domains except general health (p<0.05) (
Table 9).
Association between factors related to patients and total physical health PCS and total psychic health MCS are present in
Table 10. Statistical analysis revealed significant gender differences referring to MCS with higher MCS score (38.78 ± 7.72) in males than females (34.97 ± 7.07). Additionally, there was a significant association between disease duration and both PCS and MCS. In brief, higher scores for PCS were present in patients younger than 45 than older than 45, i.e. 45.91 ± 7.2 and 42.01 ± 6.9 respectively. Similary, MCS scores were significantly elevated in patients ≤ 45 years age (40.9 ± 8.11) in comarison to older than 45 years (36.92 ± 7.5) (p<0.05). Moreover, there was a significant link between number of BT sessions and MCS and increased MCS values were present in patients exposed to more than one BT session.
4. Discussion
In the current study, we observed positive effects of BT on functional state, quality of life and mental health in cLBP patients at mid-life. This study provides comprehensive evidence about multiple aspects that affect patient’s well-being, while available studies so far were oriented mostly on identification of specific impact on pain, functional state and disability [
6,
7]. We provide comprehensively understanding how BT influences physical and mental healthcare indicators which is crucial step for advancing evidence-based practice in pain management. The present study is among the few that specifically examines the influence of BT in cLBP in individuals at mid-life with the demographic characteristics closely resemble those typically seen in BT treatments for cLBP [
15].
EQ-5D-3L descriptive system was used to measure health-related quality of life in patients receiving BT and provide a patient-centered perspective on the benefits of this type of therapy. Our findings suggest that BT improved mobility and usual activities in patients with cLBP which are among essential components of quality of life thus directly regain independence and functionality [
16]. Addressing these core aspects of functional limitations enables patients to experience less pain, perform daily tasks with greater ease and reduce necessity for medication reliance. Additionally, higher EQ-VAS score and lower VAS score in patients receiving BT compared to CT indicates that BT significantly improved health perception and better psychological well-being. These findings undoubtedly serve as a valuable subjective measure of the impact of balneotherapy on overall health in individuals suffering from cLBP.
It was previously reported that BT in elderly people with cLBP led to improvement in functionality assessed through VAS score when implemented in combination with physical therapy [
17]. In line with our data, it was also confirmed that BT can be effective in pain reduction and improvement in functionality, fatigue and sleepiness in patients with knee osteoarthritis [
10,
18]. Other group of authors revealed that BT reduce pain intensity, functional disability perceived self-efficacy, fears and beliefs about physical activity and pain [
4].
It’s not fully clarified so far how the number of balneotherapy sessions affects VAS scores in cLBP, however our data confirmed a reduction in pain with repeated sessions as verified through a decrease in VAS score [
19]. Generally viewed it’s difficult to identify the exact number of BT sessions required for improvement in functional state of patients since treatment response varies widely among individuals and the specific protocol of BT affects clinical outcome. The number of sessions recommended for cLBP can vary based on the severity of the pain and it is often determined on a case-by-case basis by healthcare provider [
20,
21].
WAI questionnaire was also used for data collection in this research in order to provide more detailed understanding about the influence of BT on patients’ ability to work, and predict work disability [
11]. We reveled significantly higher WAI score in patients subjected to BT compared to CT which typically indicates better perceived work ability and functional capacity. In fact, these findings reflects how BT helped patients to alleviate disease-induced limitations in daily working tasks and enhanced the patient's ability to engage in work-related activities. The significantly higher WAI in males with cLBP likely may be explained by the variations in pain perception, coping mechanisms, hormonal influences and functional capacity while males may be less likely to report pain [
22].
Apart from physical manifestations that strongly limits functional state of patients with cLBP, chronic pain conditions are frequently associated with depression. Prolonged pain affects daily life, social interactions and emphasize necessity of providing patients therapy that would also prevent depressive symptoms and improve mental health [
23]. In that sense, we analyzed CES-D score in order to provide comprehensive insight into the benefits of BT, both on physical and psychological aspects. In our study, a decreased CES-D score after BT reflects improved emotional health, reduced depressive symptoms, enhanced quality of life, and a positive response to BT in cLBP. It underscores the holistic benefits of BT in addressing not only physical symptoms but also psychological aspects of chronic pain. Özkuk et al. observed a greater reduction in anxiety following BT and suggested that this could be attributed to the interplay between pain and anxiety [
24]. It’s proposed that BT exerts benefits through stress reduction alteration in salivary cortisol levels in both healthy and diseased individuals [
25]. Moreover, the hydrostatic pressure and warmth of the water may promote endorphins release thus contributing to pain relief which is in accordance with our findings [
26]. We noticed significantly higher CES-D score in females which appears to be logical due to already proven increased vulnerability to mood changes and depressive symptoms in females [
27].
In addition to the aforementioned questionnaires, we also used SF-36 for monitoring the effects of BT comprehensively and revealed that BT impacts not only pain but also broader aspects of health-related quality of life. Significant improvement in physical functioning, role limitations due to physical health, bodily pain, vitality and social functioning indicates the potential of BT as promising strategy for cLBP management via impact on different aspects of a person's life. Improvements in physical and mental health are important because they enhance quality of life, reduce disability, improve treatment adherence [
1,
2].
Both MCS and PCS were significantly elevated in patients with established diagnosis of cLBP for less than a year than longer, while increased number of BT sessions was associated with better MCS. Based on our data we may propose initiating BT earlier to prevent the progression of acute or subacute low back pain into a chronic condition with severe symptoms. However, consulting with a healthcare provider is crucial to determine the most appropriate timing and approach to treatment based on individual circumstances. Greater vulnerability of females to most of the monitored aspects of cLBP revealed in this research emphasizes the importance of implementation of education strategies about the gender differences in cLBP that will contribute to prevention and alleviation of disease progression [
6,
15].
This research provides a valuable information for increasing awareness of healthcare providers regarding the protective effects of BT in, pain management and improvement in functional status and patients’ quality of life. Taking into consideration incidence of depressive symptoms in cLBP patients and improvement in mental health achieved by BT, evidence-based practice should highlight BT along with psychosocial support and resources to address the emotional impact of chronic pain. Moreover, these data should encourage employers to implement strategies such as ergonomic assessments, adjustments to workstations, and education on proper lifting techniques to reduce the risk of developing chronic pain.
5. Conclusions
In summary, our results revealed that BT significantly contributed to reduction of pain, better functionality and disability perception status thus providing evidence for effectively managing low back pain by implementing rehabilitation approach such as BT. Understanding physical and mental healthcare indicators and patients’ health perception affected by BT is essential for optimizing patient care and adjusting treatment frequency, duration, or combining therapies to optimize outcomes.
Author Contributions
Conceptualization, D.T.M., J.B and S.Z.; writing—original draft preparation D.T.M, S.Z., J.B, A.J.S. and S.K., data curation D.T.M, B.J., B.M., Z.D., G.S., V.M., K.P.J., M.D. and D.J. ; writing—review and editing D.T.M., and. S.Z. ; visualization, B.J., B.M., Z.D., G.S., V.M., K.P.J., M.D. and D.J.; supervision, A.J.S. and S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nicol, V.; Verdaguer, C.; Daste, C.; Bisseriex, H.; Lapeyre, É.; Lefèvre-Colau, M.-M.; Rannou, F.; Rören, A.; Facione, J.; Nguyen, C. Chronic Low Back Pain: A Narrative Review of Recent International Guidelines for Diagnosis and Conservative Treatment. J. Clin. Med. 2023, 12, 1685. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M. L.; Katie de Luca; Haile, L. M.; Steinmetz, J. D.; Culbreth, G. T.; Cross, M.; Kopec, J. A.; Ferreira, P. H.; Blyth, F. M.; Buchbinder, R.; Hartvigsen, J.; Wu, A.-M.; Saeid Safiri; Woolf, A.; Collins, G. S.; Ong, K. L.; Stein Emil Vollset; Smith, A. E.; Cruz, J. A.; Kai Glenn Fukutaki. Global, Regional, and National Burden of Low Back Pain, 1990–2020, Its Attributable Risk Factors, and Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021. The Lancet Rheumatology. 2023, 5, e316–e329. [Google Scholar]
- Bailly, F.; Trouvin, A.-P.; Bercier, S.; Dadoun, S.; Deneuville, J.-P.; Faguer, R.; Fassier, J.-B.; KoleckM. ; Lassalle, L.; Le Vraux, T.; Brigitte, L.; Petitprez, K.; Ramond-Roquin, A.; Renard, J.-F.; Roren, A.; Rozenberg, S.; Sebire, C.; Vuides, G.; Rannou, F.; Audrey, P. Clinical Guidelines and Care Pathway for Management of Low Back Pain with or without Radicular Pain. Joint Bone Spine. 2021, 88, 105227. [Google Scholar] [PubMed]
- Raud, B.; Lanhers, C.; Crouzet, C.; Bénédicte Eschalier; François Bougeard; Goldstein, A. ; Pereira, B.; Coudeyre, E. Identification of Responders to Balneotherapy among Adults over 60 Years of Age with Chronic Low Back Pain: A Pilot Study with Trajectory Model Analysis. Int. J. Environ. Res. Public Health. 2022, 19, 14669–14669. [Google Scholar] [CrossRef] [PubMed]
- Ge, L.; Pereira, M. J.; Yap, C. W.; Heng, B. H. Chronic Low Back Pain and Its Impact on Physical Function, Mental Health, and Health-Related Quality of Life: A Cross-Sectional Study in Singapore. Scientific Reports. 2022, 12, 20040. [Google Scholar] [CrossRef]
- Takinacı, Z. D.; Karagülle, M.; İşsever, H.; Karagülle, M. Z. Clinical Efficacy of Spa Therapy (Balneotherapy) for Chronic Low Back Pain: A Randomized Single-Blind Trial. Eur J Integr Med. 2019, 29, 100928. [Google Scholar] [CrossRef]
- Haji, Y.; Taddesse, F.; Serka, S.; Gebretsadik, A. Effect of Balneotherapy on Chronic Low Back Pain at Hot Springs in Southern Ethiopia: Perceived Improvements from Pain. J. Pain Res. 2021, 14, 2491–2500. [Google Scholar] [CrossRef]
- Clark-Kennedy, J.; Kennedy, G.; Cohen, M.; Conduit, R. Mental Health Outcomes of Balneotherapy: A Systematic Review. Int. J. Spa Wellness. 2021, 4, 69–92. [Google Scholar] [CrossRef]
- Onat, Ş. Ş.; Taşoğlu, Ö.; Güneri, F. D.; Özişler, Z.; Safer, V. B.; Özgirgin, N. The Effectiveness of Balneotherapy in Chronic Low Back Pain. Clin. Rheumatol. 2014, 33, 1509–1515. [Google Scholar] [CrossRef]
- Dilekçi, E.; Özkuk, K.; Kaki, B. Effect of Balneotherapy on Pain and Fatigue in Elderly with Knee Osteoarthritis Receiving Physical Therapy: A Randomized Trial. International J. Biometeorol. 2019, 63, 1555–1568. [Google Scholar] [CrossRef]
- Magnavita, N.; Igor Meraglia; Viti, G. ; Borghese, L. The Work Ability Index (WAI) in the Healthcare Sector: A Cross-Sectional/Retrospective Assessment of the Questionnaire. Int. J. Environ. Res. Public Health. 2024, 21, 349. [Google Scholar] [CrossRef] [PubMed]
- Vilagut, G.; Forero, C. G.; Barbaglia, G.; Alonso, J. Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLOS ONE. 2016, 11, e0155431. [Google Scholar] [CrossRef] [PubMed]
- Feyza Nur ÇETİNKAYA; Fatmanur Aybala KOÇAK; Emine Eda KURT; Kenan GÜÇLÜ; Figen TUNCAY; Senem ŞAŞ; Hatice Rana ERDEM. The Effects of Balneotherapy on Oxidant/Antioxidant Status in Patients with Fibromyalgia: An Observational Study. Arch rheumatol. 2020, 35, 506–514.
- Jaroslav Stančiak; Jozef Novotný. The Quality of Life of the Patients with Rheumatoid Arthritis before and after Balneotherapy. J. of Health Science. 2015, 3, 232–240. [Google Scholar]
- Falagas, M. E.; Zarkadoulia, E.; Rafailidis, P. I. The therapeutic effect of balneotherapy: evaluation of the evidence from randomised controlled trials. Int J Clin Pract. 2009, 63, 1068–84. [Google Scholar] [CrossRef] [PubMed]
- Grabovac, I.; Dorner, T. E. Association between Low Back Pain and Various Everyday Performances. Wiener klinische Wochenschrift. 2019, 131, 541–549. [Google Scholar] [CrossRef]
- Ozkuk K, Dilekci E. The effects of balneotherapy in elderly patients with chronic low back pain treated with physicaltherapy: a pilot study. J Ist Faculty Med. 2019, 82, 186–192. [Google Scholar]
- Gaál, J.; Varga, J.; Szekanecz, Z.; Kurkó, J.; Ficzere, A.; Bodolay, E.; Bender, T. Balneotherapy in Elderly Patients: Effect on Pain from Degenerative Knee and Spine Conditions and on Quality of Life. The Israel Medical Association journal: IMAJ. 2008, 10, 365–369. [Google Scholar]
- Dilekçi, E.; Özkuk, K.; Kaki, B. The Short-Term Effects of Balneotherapy on Pain, Disability and Fatigue in Patients with Chronic Low Back Pain Treated with Physical Therapy: A Randomized Controlled Trial. Complementary Therapies in Medicine. 2020, 54, 102550. [Google Scholar] [CrossRef]
- Castelli, L.; Galasso, L.; Mulè, A.; Ciorciari, A.; Fornasini, F.; Montaruli, A.; Roveda, E.; Esposito, F. Sleep and Spa Therapies: What Is the Role of Balneotherapy Associated with Exercise? A Systematic Review. Frontiers in Physiology. 2022, 13, 13:964232. [Google Scholar] [CrossRef]
- Mao, S.-J.; Xiao, K.; Zhou, W.-S.; Xu, H.; Zhang, S. The Impact of Hot Spring Hydrotherapy on Pain Perception and Dysfunction Severity in Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Journal of Pain Research. 2023, 16, 3925–3944. [Google Scholar] [CrossRef] [PubMed]
- Borra, C.; Hardy, R. Differences in Chronic Pain Prevalence between Men and Women at Mid-Life: A Systematic Review Protocol. BMJ Open. 2023, 13, e065497. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Hurwitz, E. L.; Li, J.; de Luca, K.; Tavares, P.; Green, B.; Haldeman, S. Bidirectional Comorbid Associations between Back Pain and Major Depression in US Adults. International Journal of Environmental Research and Public Health. 2023, 20, 4217. [Google Scholar] [CrossRef] [PubMed]
- Özkuk, K.; Uysal, B.; Ateş, Z.; Ökmen, B. M.; Sezer, R.; Dilek, G. The Effects of Inpatient versus Outpatient Spa Therapy on Pain, Anxiety, and Quality of Life in Elderly Patients with Generalized Osteoarthritis: A Pilot Study. International Journal of Biometeorology. 2018, 62, 1823–1832. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, M.; Donelli, D. Effects of Balneotherapy and Spa Therapy on Levels of Cortisol as a Stress Biomarker: A Systematic Review. International Journal of Biometeorology. 2018, 62, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Zamunér, A. R.; Andrade, C. P.; Arca, E. A.; Avila, M. A. Impact of Water Therapy on Pain Management in Patients with Fibromyalgia: Current Perspectives. Journal of Pain Research 2019, 12, 1971–2007. [Google Scholar] [CrossRef]
- Niu, L.; He, J.; Cheng, C.; Yi, J.; Wang, X.; Yao, S. Factor Structure and Measurement Invariance of the Chinese Version of the Center for Epidemiological Studies Depression (CES-D) Scale among Undergraduates and Clinical Patients. BMC Psychiatry. 2021, 21. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).