1. Introduction
Head and neck surgery, including submandibular gland resection, performed under magnification, is rare and still performed with the naked eye, or at most with a loupe [
1]. The main indications for submandibular gland surgery are chronic sialadenitis caused by submandibular gland calculi and tumors. Submandibular gland surgery should avoid damage to the nerves running in the surrounding area, including the marginal mandibular branch of the facial, hypoglossal, and lingual nerves. Injury to the marginal mandibular branch of the facial nerve is more common compared to that to the hypoglossal or lingual nerves, with a transient rate of 1–7% and a permanent rate of approximately 2%, compared with < 2% for the hypoglossal and lingual nerves [
2,
3,
4,
5,
6]. Submandibular duct visibility in level 1 neck dissection, including submandibular gland excision, is as low as 22% [
2]. This can be problematic if there is an adhesion between the lingual nerve and surrounding tissues, such as the submandibular duct, due to inflammation of the surrounding area caused by sialolithiasis.
The exoscope is primarily used as an alternative to the microscope in neurosurgery, microvascular, and otologic surgeries [
7,
8,
9]; however, its use in neck surgery may have a significant impact on surgical outcomes. ORBEYE
TM (Olympus, Tokyo, Japan) is a 4K3D exoscope with a small mirror body and an excellent autofocus function that could be valuable in head and neck surgery to magnify the surgical field and enable precise surgical dissection of the submandibular region to reduce the risk of iatrogenic lesions. It is necessary to introduce equipment that can obtain a magnified field-of-view without stress to preserve the function of the delicate structures mentioned above. We investigated, for the first time, the usefulness of an ORBEYE exoscope in submandibular gland surgery.
2. Materials and Methods
This study included 12 patients with previously untreated submandibular lesions (
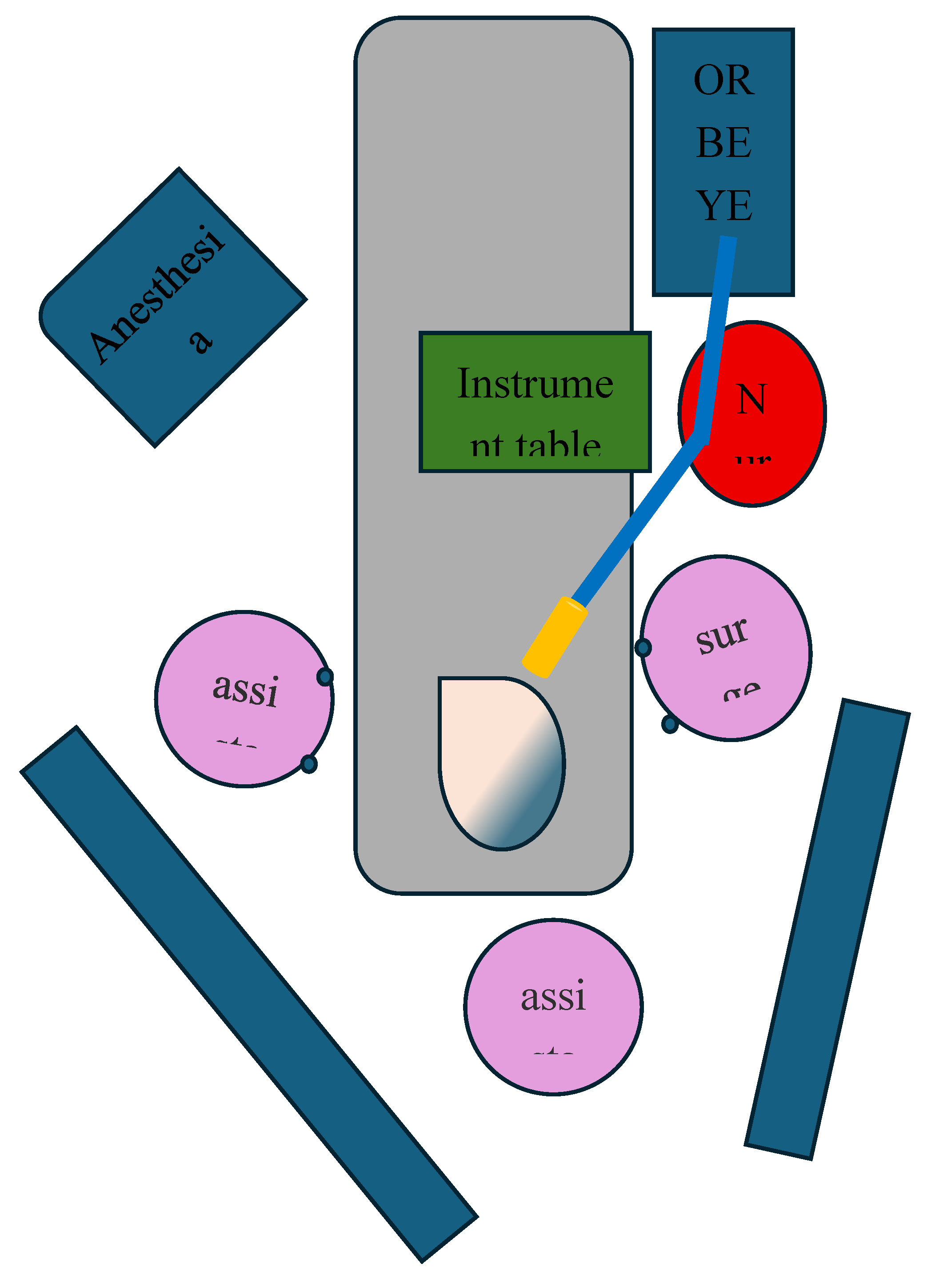
Table 1). This was a retrospective study of patients who underwent submandibular gland excision using ORBEYE at Kansai Medical University (Hirakata, Japan; KMU) between January 2018 and March 2024. We targeted 12 consecutive patients clinically diagnosed with submandibular gland tumors or sialoliths in the submandibular glands and examined the surgical outcomes and complications. On the first postoperative day and several days after the operation, the function of the facial, lingual, and hypoglossal nerves was evaluated by a surgeon different from the one who performed the surgery. We excluded cases with preoperative skin involvement or clinical lymph node metastasis requiring neck dissection other than level I. The layout of the operating room was similar for all cases, as shown in
Figure 1. The main 55-inch 4K 3D monitor was positioned at eye level in front of the surgeon wearing polarizing glasses.
2.1. Surgical Technique
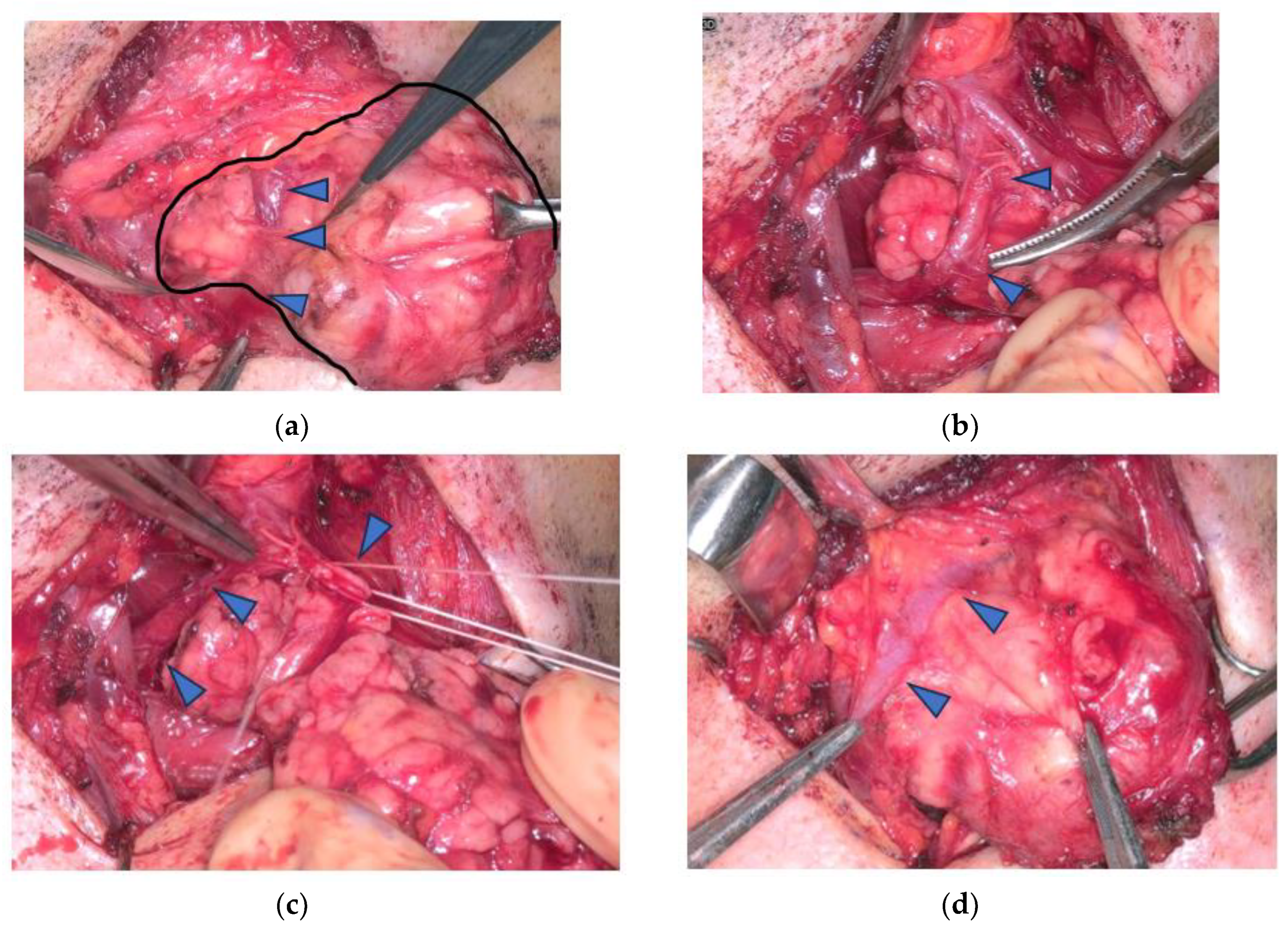
The surgical procedures were performed by two surgeons. A horizontal skin incision was made approximately 3 cm caudal to the inferior border of the mandible, and subplatysmal skin flaps were raised. In two cases, the marginal mandibular branch of the facial nerve was identified and magnified (
Figure 2a). In the other 10 cases, the submandibular gland capsule reached the submandibular end, and dissection of the superficial tissue over the submandibular capsule proceeded cephalad, exposing the submandibular gland without identifying the marginal mandibular branch (
Figure 2b). The facial arteries and veins were preserved by ligation or coagulation of the branches of these vessels toward the submandibular glands (
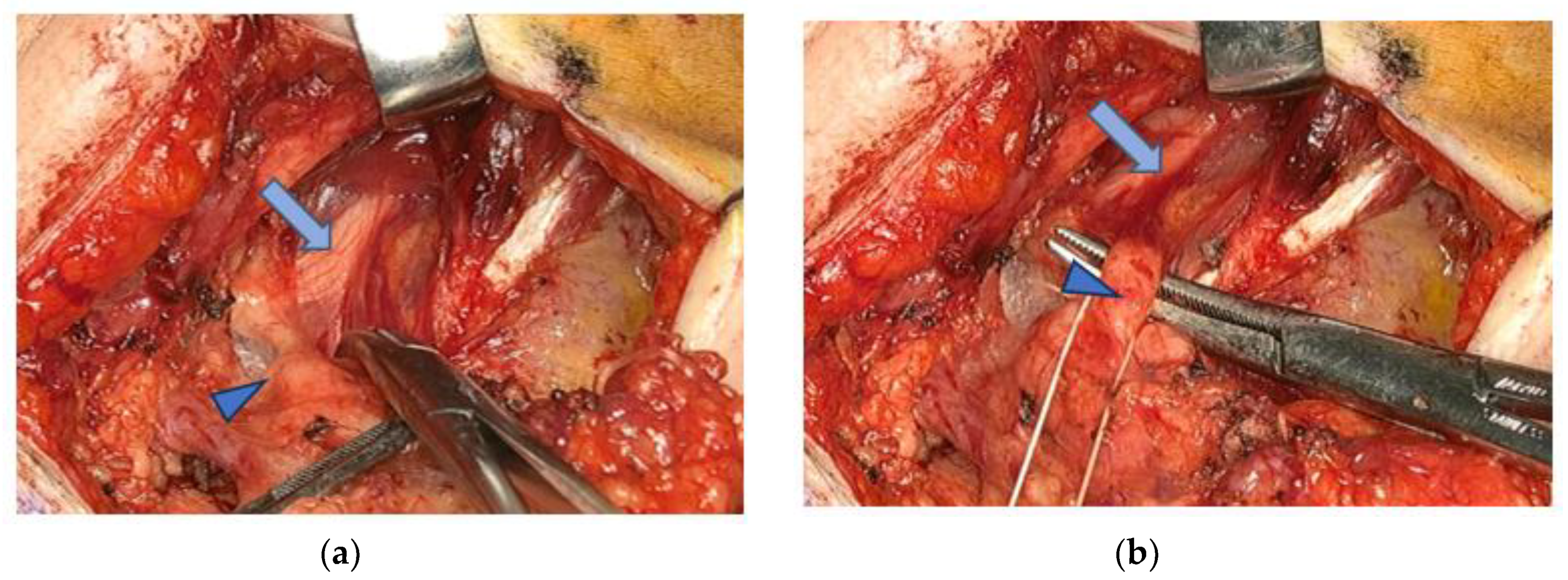
Figure 3). Facial artery and vein were ligated in only one patient (case 2) because neck dissection was performed at level I. Dissection of the submandibular gland’s deep surface was performed to expose the mylohyoid muscle, and retraction of this muscle exposed the lingual nerve (
Figure 4). The lingual nerve was then separated to ligate the submandibular ganglion (
Figure 4 and
Figure 5). The submandibular duct was then ligated (
Figure 4 and
Figure 5).
2.2. Statistical Analysis
Comparative analysis was performed using JMPⓇ13 version (SAS Institute, Cary, NC, USA) for Windows 10.0. Statistical significance was set at p-value ≤ 0.05.
2.3. Ethics
The KMU Ethics Committee and institutional review board approved this study (2020076). The hospital ethics committee waived the requirement for patient consent.
3. Results
In all cases, we used the ORBEYE under monitoring throughout the surgical procedure except for skin incision and skin suture, and no cases were switched to the conventional method. In all cases, structures such as the marginal mandibular, lingual, and hypoglossal nerves, as well as the submandibular duct were confirmed using the ORBEYE under monitoring. The demographic characteristics of the 12 patients (six males and females each) are summarized in
Table 1.
Table 1.
Patient demographics and outcome information (submandibular gland excision).
Table 1.
Patient demographics and outcome information (submandibular gland excision).
| |
Age |
Sex |
Histopathology |
Extent of resection |
Facial artery and vein preservation |
Complication |
Operation time (minutes) |
Blood loss (mL) |
| 1 |
65 |
M |
PA |
S.E. |
Preserved |
None |
127 |
30 |
| 2 |
64 |
F |
Salivary gland carcinoma ex PA |
S.E. with level I ND |
Sacrificed |
None |
118 |
13 |
| 3 |
64 |
M |
Sialolithiasis with chronic inflammation |
S.E. |
Preserved |
None |
118 |
27 |
| 4 |
23 |
M |
PA |
S.E. |
Preserved |
None |
129 |
5 |
| 5 |
35 |
F |
PA |
S.E. |
Preserved |
None |
121 |
31 |
| 6 |
59 |
F |
Lymphadenoma, non-sebaceous type |
S.E. |
Preserved |
None |
85 |
43 |
| 7 |
50 |
F |
PA |
S.E. |
Preserved |
None |
104 |
12 |
| 8 |
72 |
F |
PA |
S.E. |
Preserved |
None |
81 |
6 |
| 9 |
68 |
M |
Sialolithiasis with chronic inflammation |
S.E. |
Preserved |
None |
80 |
13 |
| 10 |
71 |
M |
PA |
S.E. |
Preserved |
None |
96 |
10 |
| 11 |
51 |
F |
PA |
S.E. |
Preserved |
None |
80 |
26 |
| 12 |
83 |
M |
PA |
S.E. |
Preserved |
None |
106 |
24 |
| MEAN |
58.75 |
|
|
|
|
|
104 |
20 |
The mean age of the 12 patients was 58.5 years (23–83 years). The final histopathology showed pleomorphic adenoma in eight cases, non-sebaceous-type lymphadenoma in one case, carcinoma ex pleomorphic adenoma in one case, and sialolithiasis with chronic inflammation in two cases. The extent of resection was submandibular gland excision in 11 cases and level I lymph node dissection (submental and submandibular nodes), including submandibular excision, in one case (Case 2). We performed facial artery and vein sparing, except in one case (Case 2) in which level I neck dissection, including the submandibular gland, was performed. In all cases, the marginal mandibular branches of the facial, hypoglossal, and lingual nerves, as well as submandibular duct were identified and preserved. None of the patients experienced paralysis of the marginal mandibular branches of the facial, hypoglossal, or lingual nerves. No patient experienced postoperative bleeding or infection. The mean operative time was 104 min (80–129 min). The mean volume of blood lost was 20 mL (5–43 mL).
4. Discussion
This retrospective review of 12 cases of submandibular gland resection using an ORBEYE exoscope revealed no postoperative complications, including nerve palsy or vasculature preservation. To the best of our knowledge, this is the first study to examine the usefulness of an exoscope in submandibular gland resection. An exoscope is advantageous because of its ability to perform surgery while viewing high-resolution 3D images under magnification, superior ergonomics with reduced fatigue due to its free viewing angle, and educational significance because of its ability to share screens with the same surgical field of vision as the surgeon [
8,
9,
10,
11]. In head and neck surgery, usually performed with the naked eye, the ORBEYE’s excellent autofocus function and small mirror body allow the surgeon to avoid interference from instruments and secure a smooth surgical field without stress. In addition, its ability to provide a detailed magnification of nerves and blood vessels is extremely useful.
Notably, some of the critical structures for level 1 neck dissection involving submandibular gland excision, such as the marginal mandibular, lingual, and hypoglossal nerves and submandibular duct, may not be identified [
2]. Reportedly, paralysis of the mandibular marginal branch of the facial, lingual, and hypoglossal nerves in submandibular gland surgery occurs in 1–7%, 0.5–4.4%, and 0–1.4% of cases, respectively [
3,
4,
5,
6]. A lack of confirmation can cause these nerve injuries and adhesions between the lingual nerve and the submandibular canal, as seen in sialolithiasis. We believe that these structures were preserved in this study because they could be clearly visualized under ORBEYE.
The facial artery can be preserved by burying it partially in the glandular tissue. This requires careful blunt dissection of submandibular gland along its run, as well as the division of several small arterial branches from the artery to the gland to free it from the gland. We found the exoscope helpful in magnifying the surgical field by delicately dissecting the submandibular gland, detaching the artery, and ligating small arterial branches from the artery to the gland. Facial veins rarely run embedded in the submandibular gland [
12]. However, the veins require ligature of small venous branches, and the benefit of obtaining magnified views in venous processing, which is prone to vascular collapse, is thought to be significant. Cutting and ligation of the facial artery are common in conventional submandibular surgery; its preservation is important because of its role in blood flow to the lower face and platysma muscle. The facial artery should not be routinely ligated and sacrificed because of the significance of preserving it and the fact that it is a crucial recipient vessel in head and neck reconstructive surgery [
12].
Endoscopic and robotic techniques have been reported for submandibular gland surgery, the advantages of which are primarily cosmetic and magnification [
1,
13,
14,
15,
16,
17,
18,
19]. However, they are not widely used, possibly because of the complexity of preparation and cost. In contrast, the ORBEYE exoscope does not require special settings or devices other than drapes, such as ultrasonic coagulation devices, and the surgical instruments are almost similar to those used in conventional surgery. In addition, the difference in the direction of the field of view compared to classical submandibular surgery may also hinder its adoption by surgeons. In this respect, using the exoscope requires familiarity with hand–eye coordination; however, because the direction of the field of view is the same, the hurdle to adoption may be low. In addition, reports of endoscopic and robotic surgery have generally shown promising results in preserving the mandibular marginal branch and other nerves; however, the facial arteriovenous system was ligated, except for robotic resection through a transhairline approach [
14,
15,
16,
17,
18,
19]. The benefits of preserving the facial arteriovenous system remain unknown; it is difficult to imagine that preserving large-diameter vessels is disadvantageous. To the best of our knowledge, there have been no reports on the use of an exoscope.
This preliminary study provides promising results, but there are some limitations that should be noted. The main limitation was the small number of cases, which may affect the results. Therefore, it will be necessary to conduct a prospective study of submandibular gland surgery comparing the conventional method with the ORBEYE exoscope in a larger sample in the future. Visualization of delicate structures, such as nerves and blood vessels, in a greater detail may lead to lower complication rates and educational benefits. Using the ORBEYE exoscope has educational significance for instructors and observers. It is essential to understand anatomical details when learning a surgical technique, and seeing how to handle these structures and surrounding tissues from the surgeon’s perspective can be very helpful in improving the technique. ORBEYE makes this possible.
Author Contributions
Conceptualization, M.Y.; Methodology, M.Y. and T.F.; Formal analysis, K.S.; Investigation, M.Y., M.M., T.U., and M.S; Data curation, M.M. and T.S.; Writing: original draft, M.Y.; Writing: review and editing, K.S. and T.S.; Supervision, H.I.; Project administration, M.Y. and K.S. All authors have read and agreed to the manuscript.
Funding
No funding was received for conducting this study.
Institutional Review Board Statement
The KMU Ethics Committee and institutional review board approved this study (2020076).
Informed Consent Statement
The hospital ethics committee waived the requirement for patient consent.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to thank Editage (
www.editage.jp) for English language editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Beahm, D.D.; Peleaz, L.; Nuss, D.W.; Schaitkin, B.; Sedlmayr, J.C.; Rivera-Serrano, C.M.; Zanation, A.M.; Walvekar, R.R. Surgical approaches to the submandibular gland: a review of literature. Int J Surg 2009, 7, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Nocon, C.C.; Cohen, M.A.; Langerman, A.J. Quality of neck dissection operative reports. Am J Otolaryngol 2016, 37, 330–333. [Google Scholar] [CrossRef]
- de Carvalho, A.S.; Dedivitis, R.A.; de Castro, M.A.; Nardi, C.E. Submandibular gland excision. Rev Col Bras Cir 2015, 42, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Springborg, L.K.; Møller, M.N. Submandibular gland excision: long-term clinical outcome in 139 patients operated in a single institution. Eur Arch Otorhinolaryngol 2013, 270, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Delsing, C.P.; Cillessen, E.; Scheffer, A.; van Hulst, K.; Erasmus, C.E.; van den Hoogen, F.J. Bilateral submandibular gland excision for drooling: our experience in twenty-six children and adolescents. Clin Otolaryngol 2015, 40, 285–290. [Google Scholar] [CrossRef]
- Preuss, S.F.; Klussmann, J.P.; Wittekindt, C.; Drebber, U.; Beutner, D.; Guntinas-Lichius, O. Submandibular gland excision: 15 years of experience. J Oral Maxillofac Surg 2007, 65, 953–957. [Google Scholar] [CrossRef]
- Montemurro, N.; Scerrati, A.; Ricciardi, L.; Trevisi, G. The exoscope in neurosurgery: An overview of the current literature of intraoperative use in brain and spine surgery. J Clin Med 2022, 11, 223. [Google Scholar] [CrossRef]
- Pafitanis, G.; Hadjiandreou, M.; Alamri, A.; Uff, C.; Walsh, D.; Myers, S. The Exoscope versus operating microscope in microvascular surgery: A simulation non-inferiority trial. Arch Plasti Surg 2020, 47, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Tu, N.C.; Doerfer, K.; Costeloe, A.; Sioshansi, P.C.; Babu, S. Educational benefit of the three-dimensional exoscope versus operating microscope in otologic surgery. Otol Neurotol 2024, 45, 150–153. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, J.; Covell, M.M.; Jabeen, S.; Nadeem, A.; Malik, G.H.; Abdus, S.H.; Amin, A.; Salman, Y.; Hafeez, M.H.; Bowers, C.A. Comparative analysis of exoscope-assisted spine surgery versus operating microscope: A systematic review. World Neurosurg 2024, 21, 100258. [Google Scholar] [CrossRef]
- Ricciardi, L.; Chaichana, K.; Cardia, A.; Stifano, V.; Rossini, Z.; Olivi, A.; Sturiale, C.L. The exoscope in neurosurgery: An innovative “Point of View”. A systematic review of the technical, surgical, and educational aspects. World Neurosurg 2019, 124, 136–144. [Google Scholar] [CrossRef]
- Rahman, S.H.; Ali, M.I.; Tariq, A.; Tarafderc, K.H.; Islam, M.R. A modified technique in submandubular salivary gland excision: preservation of facial artery. Mymensingh Med J 2020, 29, 361–365. [Google Scholar] [PubMed]
- Chen, M.K.; Su, C.C.; Tsai, Y.L.; Chang, C.C. Minimally invasive endoscopic resection of the submandibular gland: a new approach. Head Neck 2006, 28, 1014–1017. [Google Scholar] [CrossRef]
- Lee, D.Y.; Jung, K.Y.; Baek, S.K. Endoscopic submandibular gland resection preserving great auricular nerve and periaural sensation. Auris Nasus Larynx 2016, 43, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Song, C.M.; Jung, Y.H.; Sung, M.W.; Kim, K.H. Endoscopic resection of the submandibular gland via a hairline incision: A new surgical approach. Laryngoscope 2010, 120, 970–974. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.L.; Li, H.; Holsinger, F.C.; Koh, Y.W. Submandibular gland resection via the trans-hairline approach: A preclinical study of a novel flexible single-port surgical system and the surgical experiences of standard multiarm robotic surgical systems. Head Neck 2019, 41, 2231–2238. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.W.; Kim, Y.K.; Cha, Y.H.; Koh, Y.W.; Nam, W. Robot-assisted submandibular gland excision via modified facelift incision. Maxillofac Plast Reconstr Surg 2017, 39, 25. [Google Scholar] [CrossRef]
- Lee, H.S.; Park, D.Y.; Hwang, C.S.; Bae, S.H.; Suh, M.J.; Koh, Y.W.; Choi, E.C. Feasibility of robot-assisted submandibular gland resection via retroauricular approach: preliminary results. Laryngoscope 2013, 123, 369–373. [Google Scholar] [CrossRef]
- Yang, T.L. Robotic surgery for submandibular gland resection through a trans-hairline approach: The first human series and comparison with applicable approaches. Head Neck 2018, 40, 793–800. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).