1. Introduction
Breast cancer (BC) is one of the most common malignancies affecting women worldwide, with various subtypes presenting unique diagnostic and therapeutic challenges. [
1,
2] Triple-negative breast cancer (TNBC) accounts for 12 to 17% of all breast cancers and is one of the most aggressive forms of breast cancer. TNBC lacks the expression of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). It is characterized by poor differentiation, high invasiveness, a tendency for both local and distant metastases, poor prognosis, and high recurrence rates. [
3]. Since it does not express hormone receptors or HER2 amplification, its biology remains poorly understood to this day. Because of this, the development of targeted therapies for TNBC has lagged behind other breast cancer subtypes. [
4,
5] This case report details the diagnostic process and multidisciplinary management of a 64-year-old woman who presented with a nodular formation in her left breast, later confirmed as TNBC. The case underscores the importance of comprehensive evaluation, including the role of family history and genetic testing, and highlights an unusual presentation involving multiple organ systems. The findings ultimately suggested a primary pulmonary origin of the malignancy, providing a rare insight into the metastatic pathways and diagnostic intricacies associated with BC.
2. Case Presentation
A 64-year-old woman with no relevant medical history, no drug allergies, and no significant surgical history had noticed in March 2024 a nodular formation in the upper outer quadrant of her left breast during self-examination so she went to a diagnostic center in Genoa where she underwent a follow-up mammogram and subsequently a biopsy. Mammography revealed two formations in the left breast, measuring 7 mm and 8 mm, respectively. Biopsy confirmed triple-negative infiltrating ductal carcinoma with a Ki-67 of 50% and she decided to continue the necessary treatment at the Breast Unit of the San Martino Polyclinic Hospital in Genoa.
A Multidisciplinary Team (MDT) decided on a nipple-sparing mastectomy due to her small breast size, with a biopsy of the sentinel lymph node (
Figure 1).
Figure 1.
Frontal photo of the patient before surgery.
Figure 1.
Frontal photo of the patient before surgery.
Figure 2.
Left and right-side photo of the patient before surgery.
Figure 2.
Left and right-side photo of the patient before surgery.
During the preoperative evaluation, a new formation was found in the lower inner quadrant of the right breast, previously undetected.
Our breast radiologists re-examined the previous mammographic images and they confirmed that the exam on the right side was negative, therefore, they decided to perform a right-sided unilateral breast ultrasound on the patient.
The ultrasound of the right breast revealed a nodular lesion with mixed echogenicity, classified as E4b. The patient had a significant family history of cancer, including leukemia in her father, lung carcinoma in her mother, and breast carcinoma in her paternal aunt. Genetic testing for the BRCA mutation was negative.
Despite her family history, she opted for a bilateral mastectomy without further investigation on the right side.
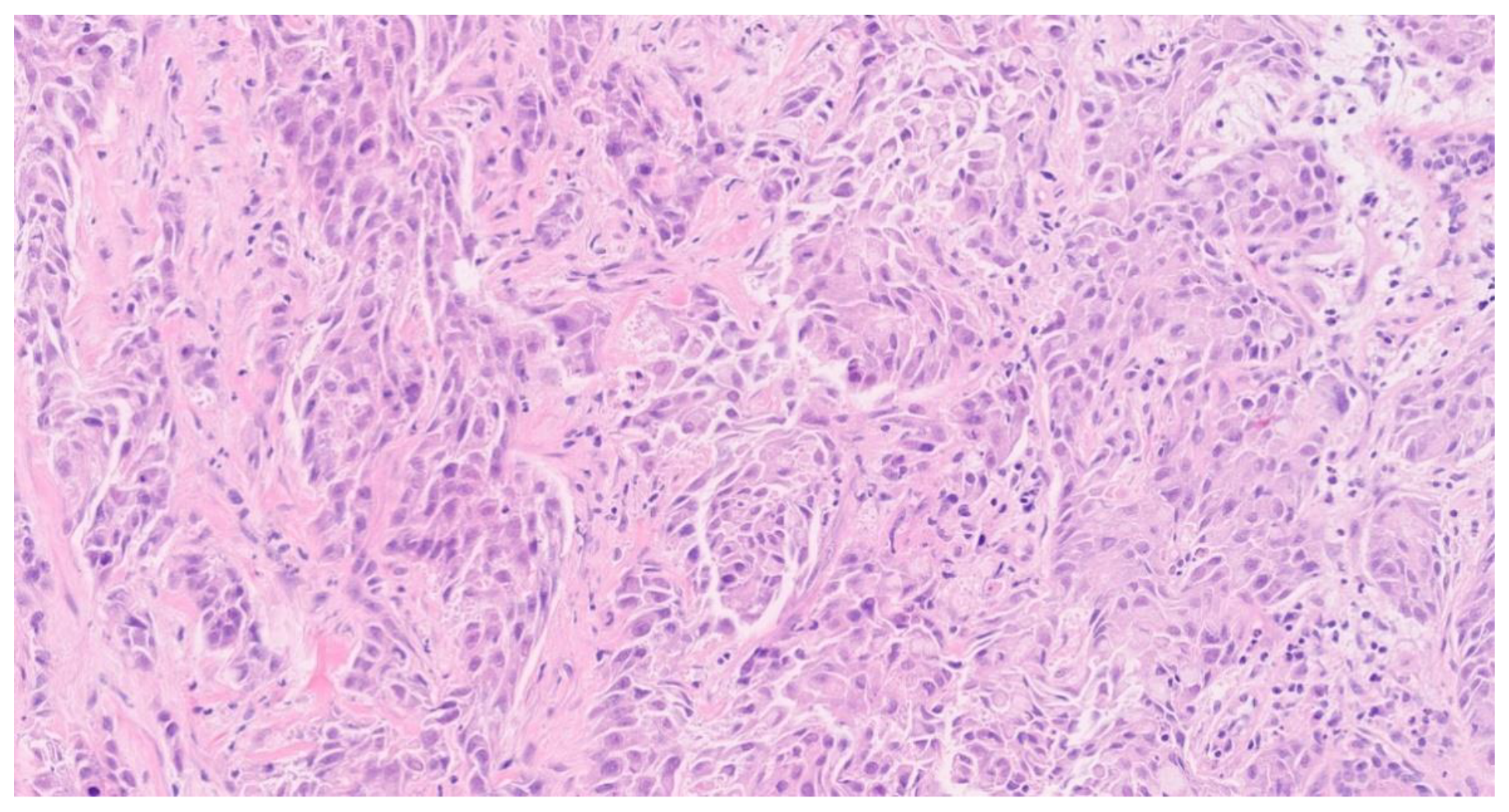
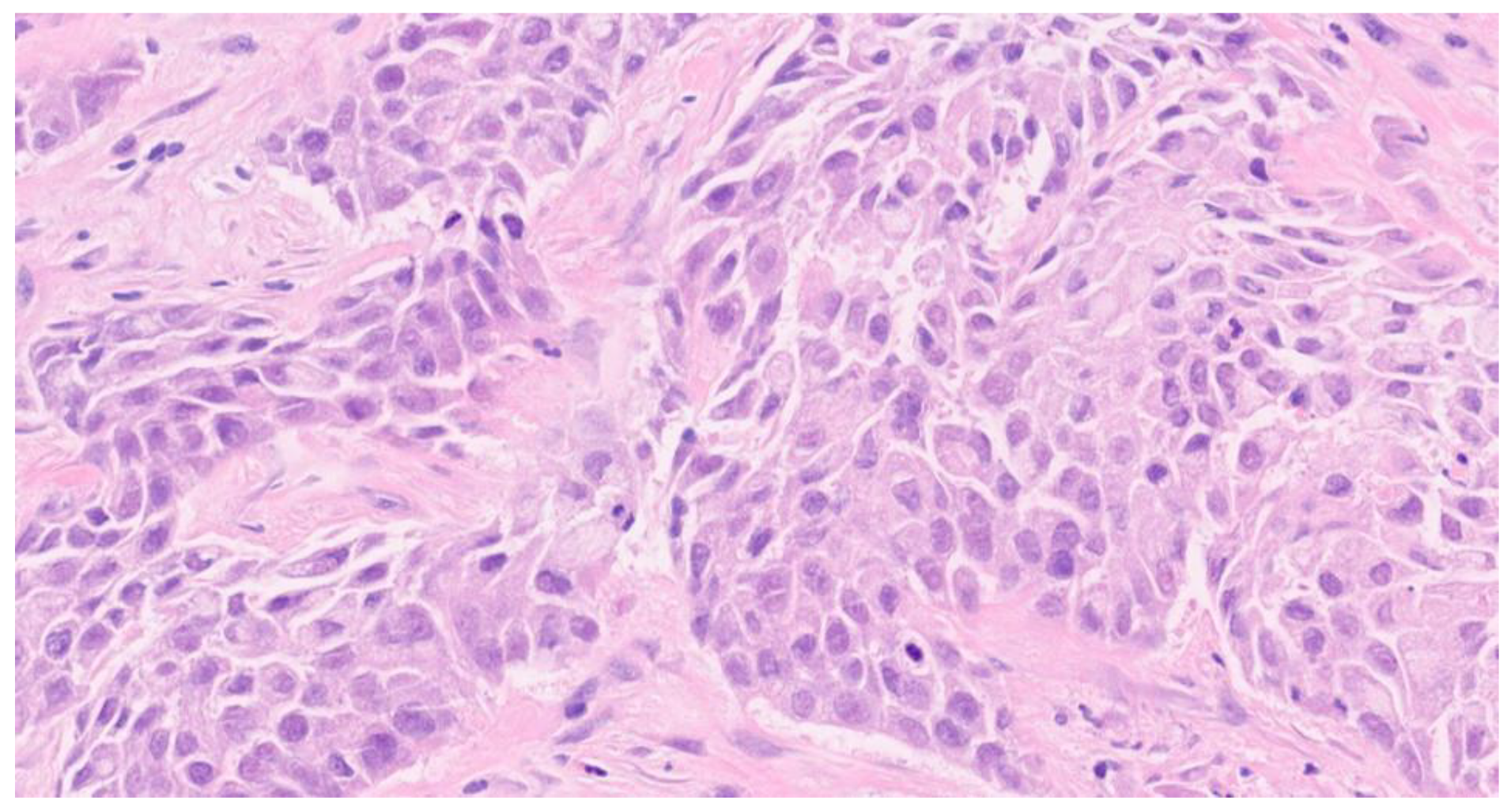
In April 2024, she underwent preoperative tests (blood tests, chest X-ray, and ECG), all of which returned normal results and so she underwent bilateral nipple-sparing mastectomy along with a sentinel lymph node biopsy and immediate breast reconstruction with tissue expanders. Histological examination revealed poorly differentiated neoplasms in the right breast. Histology of the left breast showed invasive ductal carcinoma pT1c/G3/N0, while the right breast showed invasive ductal carcinoma m(2)pT1b/G3/N0.
Post-surgery, she underwent radiological staging examinations for adjuvant chemotherapy.
Staging CT scans revealed multiple hypodense nodules with hyperemic rims, mostly on the left side. Additionally, a spiculated-margin pulmonary nodule that was not visible on the preoperative chest X-ray and an adrenal localization was found. Subcutaneous nodules were biopsied, showing carcinomatous localization with expression of cytokeratin 7 and partial CDX2.
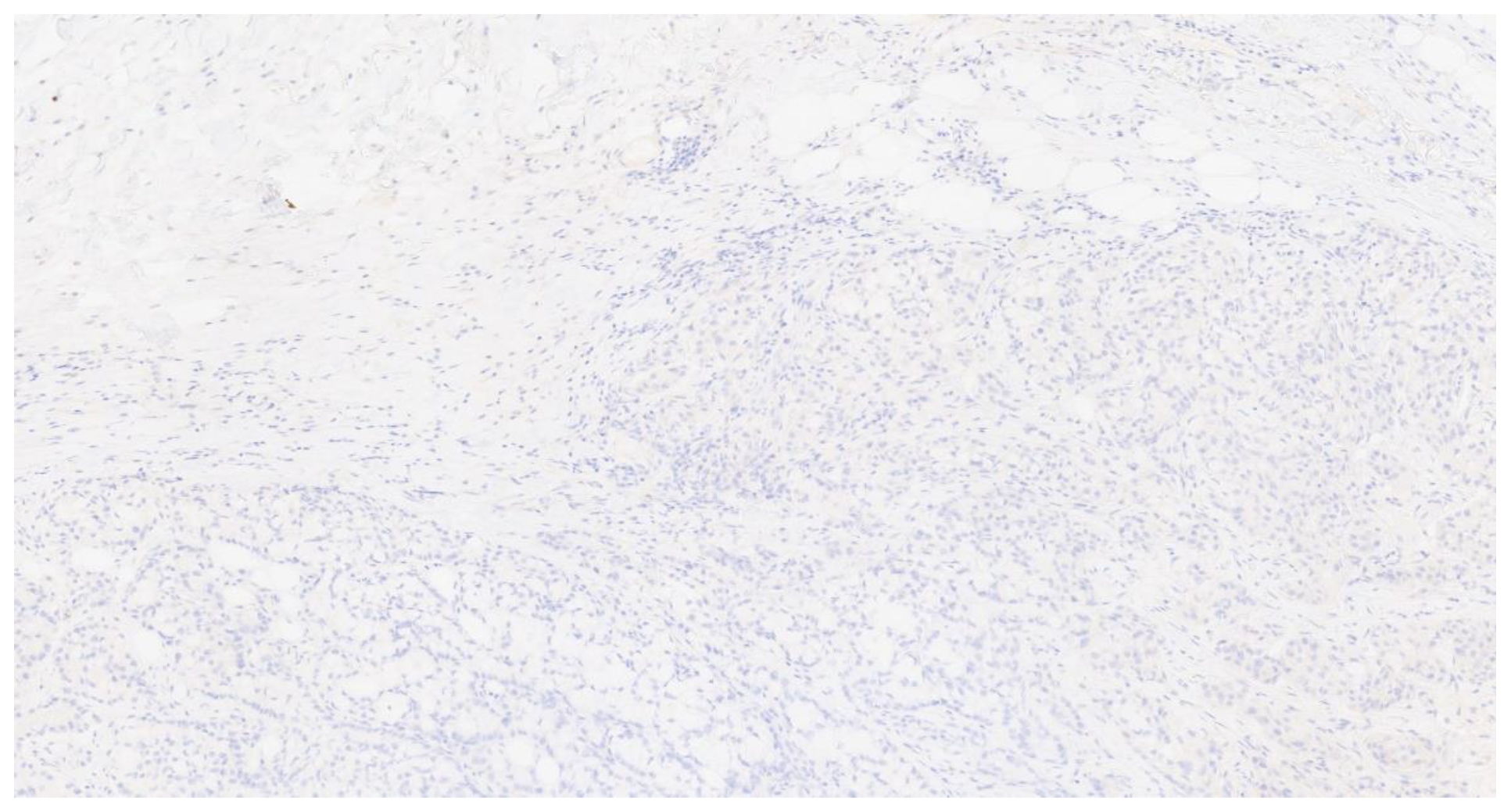
Immunohistochemical staining was negative for various markers. The proliferation index was 70-80%. The histopathological findings did not conclusively determine the neoplasm's origin.
Finally, the patient underwent an endoscopic lung biopsy with multiple cryobiopsies of a subsegmental branch of the right upper lobe bronchus, performed under fluoroscopic guidance and radial endobronchial ultrasound (EBUS).
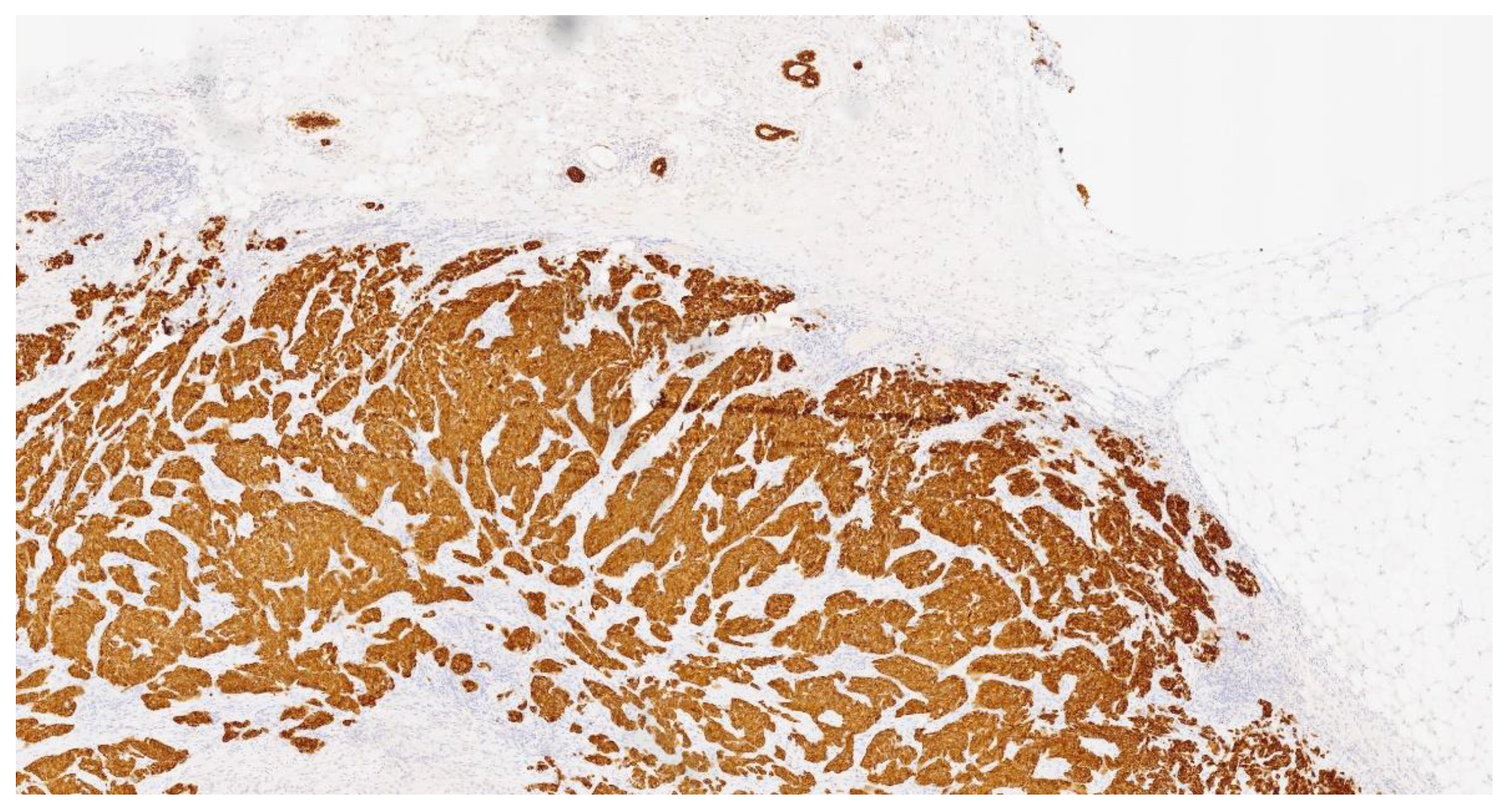
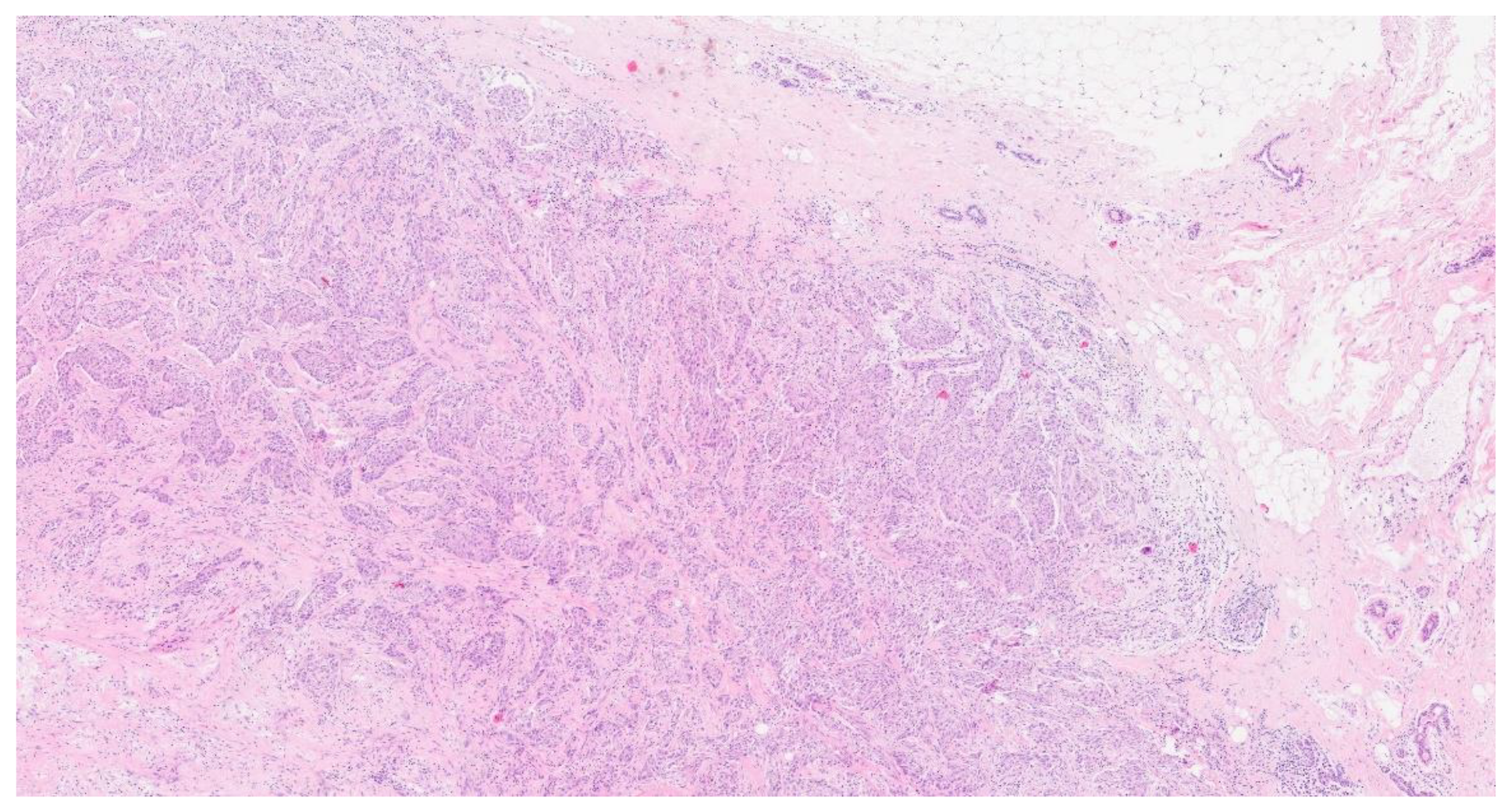
On May 2024, the histological examination revealed the presence of carcinoma, specifically involving the bronchial mucosa, which showed infiltration near the cartilaginous tissue by a neoplasm with solid and glandular growth and widespread expression of cytokeratin 7 (Figure. 3) Overall, the histopathological findings were substantially similar to those of the previous histological examination that involved the breast (
Figure 4,
Figure 5 and
Figure 6). The pathologists performed further examinations on the breast and lung biopsies, testing for TTF1 (Thyroid Transcription Factor-1) commonly tested for in various types of neoplasms, primarily to help in the diagnosis and differentiation of lung and thyroid cancers (specifically TTF1 is used to identify lung adenocarcinomas, small cell lung carcinomas and thyroid carcinomas) (
Figure 7), GATA3 gene commonly involved in various types of cancers, primarily those arising from epithelial tissues (breast carcinoma, urothelial and in general urological carcinomas, lung carcinomas and thyroid carcinoma and certain hematologic malignancies), napsin A which is an aspartic proteinase enzyme encoded by the NAPSA gene, primarily recognized for its expression in specific cancers, specifically lung adenocarcinoma, and P40, a variant of the p63 protein encoded by the TP63 gene, is identified through its immunohistochemical staining, aiding pathologists in distinguishing squamous cell carcinomas from adenocarcinomas in various tissues, including lung, head, and neck. All these examinations came back negative. PD-L1 (Programmed Death-Ligand 1, important target in anticancer therapy) was absent, and ALK (Anaplastic Lymphoma Kinase, involved in some types of small cell lung cancer), EGFR (Epidermal Growth Factor Receptor, implicated in many cancer types, particularly non-small cell lung cancer), ROS1 gene (primarily involved in non-small cell lung cancer), RET gene (involved in various cancer types, for example medullary thyroid carcinoma), METex14 (specific mutation in the MET (Mesenchymal-Epithelial Transition factor) gene involving exon 14 that can be relevant in non-small cell lung carcinoma) , NTRK1/2/3 (Neurotrophic Tyrosine Receptor Kinase family genes involvede in different types of solid tumors and hematologic malignancies), and BRAF (B-Raf Proto-Oncogene, Serine/Threonine Kinase, involved in different types of cancer especially melanoma and others type of solid tumors) were all wild type (wt).
Considering the radiological findings, the histopathological results and the development of the disease again primarily suggest a possible primary pulmonary origin. Therefore, both the breast subcutaneous neoplasms and adrenal metastasis were locations of disease originating from the lungs. Therefore, it was decided to administer the patient a first-line therapy with carboplatin AUC 5, paclitaxel, and pembrolizumab every 3 weeks.
On physical examination, the patient is currently in good general condition, asymptomatic, with a saturation of 97% on room air.
4. Discussion
This case report presents a complex diagnostic and therapeutic challenge involving a 64-year-old woman with triple-negative breast cancer (TNBC). The initial presentation of a nodular formation in the left breast, confirmed as TNBC with a high proliferation index (Ki-67 of 50%), necessitated a multidisciplinary approach. The decision to perform a nipple-sparing mastectomy was influenced by the small breast size and the need for a sentinel lymph node biopsy.
The discovery of a new lesion in the right breast during preoperative evaluation further complicated the clinical picture. Despite negative genetic testing for BRCA mutations, the patient’s significant family history of various cancers raised concerns about potential genetic predispositions and metastatic disease.
Histological findings from both breasts revealed poorly differentiated neoplasms, prompting further radiological staging. The presence of multiple hypodense nodules with hyperemic rims and a spiculated-margin pulmonary nodule on CT scans raised the suspicion of metastatic disease. The subcutaneous nodules biopsied showed carcinomatous localization with cytokeratin 7 (CK7 typically expressed in epithelial cancers such as breast, lung, ovarian, and pancreatic cancers, among others) but the immunohistochemical staining was inconclusive regarding the primary origin of the neoplasm.
The definitive diagnosis came from the endoscopic lung biopsy, which identified a carcinoma involving the bronchial mucosa with infiltration near cartilaginous tissue, displaying both solid and glandular growth patterns. The histopathological findings, which were similar to those seen in the breast tissue, suggested a primary pulmonary origin.
This case highlights several critical points like the complexity of TNBC that is a heterogeneous disease that often require aggressive treatment and comprehensive diagnostic evaluation due to its lack of hormone receptors and HER2 expression [
6]; The role of family history is crucial in understanding potential genetic predispositions, even when genetic testing is negative. This case highlights the importance of considering metastatic pathways from non-mammary primary sites, especially in patients with unusual presentations or multiple lesions. Furthermore, one of the most important aspects is the multidisciplinary approach. Effective management of such complex cases requires a coordinated effort among oncologists, radiologists, pathologists, and surgeons to ensure accurate diagnosis and optimal treatment planning.
This was an extremely rare case that, based on the clinical, radiological, and histological data available to us, could not have been managed differently. However, it emphasizes uncommon clinical presentations, such as the rapid appearance of contralateral neoplasms to those already studied on the left breast.
In the literature, the most recent article we found was a systematic review by Jennifer A. Mirrielees et al. [
7] which identified 41 case reports of patients with synchronous or metachronous breast metastases from primary lung tumors. Except for two cases, all identified breast metastases from primary lung tumors had negative estrogen and progesterone receptors, and HER2 was not amplified. The most common treatment history was chemotherapy (CT) for lung cancer alone (36 %), the 20% received CT + surgery, 16% received surgery alone, 12% received CT + radiotherapy (RT), 4% RT + surgery, 4 % RT alone and the 8 % none. Finally, more non-small-cell lung cancer (NSCLC) metastases have been documented than small-cell lung cancer (SCLC) among published case reports.
5. Conclusions
The diagnosis of a primary pulmonary carcinoma with metastatic involvement of the breasts and subcutaneous tissues is rare but emphasizes the need for thorough and repeated evaluations in atypical presentations of BC. This case contributes to the understanding of metastatic BC and the necessity of considering extramammary origins in differential diagnosis.
Author Contributions
Conceptualization, R.D., F.M. and P.F.; methodology, R.D., P.F. and M.G.; data curation, R.D., L.C., F.M., F.D., C.C., S.F., M.P., S.B., B.M., V.B. and F.P.; writing—original draft preparation, R.D., M.G., F.M. and P.F.; writing—review and editing, R.D., P.F., M.G. and F.M. ,supervision, P.F. and F.D.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this study are available in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhang YN; Xia KR; Li CY; Wei BL; Zhang B. Review of Breast Cancer Pathologigcal Image Processing. Biomed Res Int. 2021; 2021:1994764. [CrossRef]
- Fregatti P; Gipponi M; Diaz R; DE Rosa R; Murelli F; Depaoli F; Pitto F; Baldelli I; Zoppoli G; Ceppi M; Friedman D. The Role of Sentinel Lymph Node Biopsy in Patients with B5c Breast Cancer Diagnosis. In Vivo. 2020 Jan-Feb;34(1):355-359.
- Liu Y; Hu Y; Xue J; Li J; Yi J; Bu J; Zhang Z; Qiu P; Gu X. Advances in immunotherapy for triple-negative breast cancer. Mol Cancer. 2023 Sep 2;22(1)-145. [CrossRef]
- Leon-Ferre RA; Goetz MP. Advances in systemic therapies for triple negative breast cancer. BMJ. 2023 May 30;381:e071674. [CrossRef]
- Bergin ART; Loi S. Triple-negative breast cancer: recent treatment advances. F1000Res. 2019 Aug 2;8:F1000 Faculty Rev-1342. [CrossRef]
- Sharma P. Biology and Management of Patients with Triple-Negative Breast Cancer. Oncologist. 2016 Sep;21(9):1050-62. [CrossRef]
- Mirrielees JA; Kapur JH; Szalkucki LM; Harter JM; Salkowski LR; Strigel RM; Traynor AM; Wilke LG. Metastasis of primary lung carcinoma to the breast: a systematic review of the literature. J Surg Res. 2014 May 15;188(2):419-31.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).