Introduction
The incidence of neurological injury in paediatric and adolescent spinal deformity surgery varies within the literature but is thought to range from 1 to 2% [
1,
2]. Due to the significant variation within this large cohort, the incidence can vary depending on which subgroup of patients are analysed. Specifically, the type and severity of deformity, curve stiffness and curve correction, underlying medical conditions, surgical approach, intraoperative haemodynamic stability, and revision procedures are all thought to have an effect [
1,
2]. In most cases, injury to the spinal cord occurs due to direct trauma or secondary to ischemia. The utilisation of spinal cord monitoring can assist in alerting the operating team that the cord is at risk in the hope to reverse actions to prevent permanent neurological deficit. The method of assessing spinal cord function during deformity surgery has moved from the Stagnara wake-up test to intra-operative neuro-monitoring [
3].
Intraoperative neurophysiological monitoring (IOM) helps assess the integrity of neural structures during surgical procedures. It includes both continuous monitoring of neural tissue, as well as the localization of vital neural structures. IOM methods have evolved from the use of only somatosensory evoked potentials (SSEPs) to the combined approach using SSEPs, motor evoked potentials (MEPs) and free running electromyography (EMG) [
4,
5]. SSEPs monitor the dorsal column–medial lemniscus pathway, which mediates tactile discrimination, vibration, and proprioception. MEPs monitor the motor pathways; transcranial electrical stimulation elicits excitation of corticospinal projections at multiple levels with the electrical potential recorded at the spinal cord or muscles. MEPs are generated and transported via the pyramidal tract. Electromyography (EMG) records myoelectric signals from peripheral musculature to monitor selective nerve root function.
Multimodal IOM has been established as standard method for early detection of an evolving or impending spinal cord deficit during surgical deformity correction of the spine, that will allow timely intervention before permanent neurologic injury occurs (SRS information statement 2019). This combined approach has increased sensitivity and specificity for detecting neurological damage during deformity correction [
4,
6,
7]. Despite this there remains variability in individual practice during utilisation of IOM and in handling of neuro-monitoring alerts [
8]. There is also discrepancy between surgeons with regard to when they discontinue monitoring. 12.7% of surgeons stop monitoring when the anaesthetic is discontinued, 29.2% continue monitoring for 60 minutes after deformity correction or until the wound is closed, and 45.4% continue for 30 minutes after correction or until the wound is closed. Alarmingly, 12.7% of surgeons stop monitoring when the final tightening of implants has been completed.
Continuation of IOM after completion of instrumentation is very important as there is a potential for loss of IOM signals in this period. There is paucity of literature regarding these events. Within our institution we would classify this as a delayed IOM event. We define delayed IOM events as ‘loss of responses, after baseline responses were present upon completion of instrumentation and deformity correction’. The aim of this study is to evaluate the IOM results within our service and specifically investigate this subgroup of delayed events with the aim to assess their incidence and determine the need for continuation of IOM after completion of instrumentation.
Methods
We performed a retrospective study of all paediatric and young adult patients who underwent spinal deformity surgery with instrumentation and intended multimodal IOM within our service between December 2011 and August 2021. Patients under the age of 25 years were included for analysis. Data was collected from the medical, surgical, and IOM records and documented postoperative complications. The primary objective was to identify and investigate those patients who had an IOM event.
IOM Technique
IOM was performed by 2 nationally certified senior clinical physiologists who were present throughout the entire procedure using a 10-channel Medelec© Synergy IOM constant voltage system (2009–2013) and a 24-channel Inomed ISIS IOM constant current system (2014–2021). We aimed for multimodal IOM in all patients, recording of cortical SSEPs, cervical SSEPs, and MEPs. Reference traces were obtained before skin incision.
Somatosensory Evoked Potentials
Sensory evoked potentials were recorded from the brain (cortical SSEP) and spinal cord (cervical SSEP). Responses were evoked by cathodal delivery of 0.2 ms duration, square-wave impulses at a range of 3.7–4.3 Hz to bilateral posterior tibial nerves using pairs of adhesive electrodes. The stimulation intensity was 45 mA. Upper limb SSEPs were introduced in a similar fashion with square wave impulses delivered to bilateral ulnar nerves at 25 mA. Cortical SSEPs were recorded from corkscrew electrodes placed in the scalp at Cz’ and referred to Fz (identified using the 10–20 international head measurement system). Cervical SSEPs were recorded from a needle electrode placed subcutaneously over Cv2 and referred to Fz.
Motor Evoked Potentials
MEPs were recorded bilaterally as compound muscle action potentials (CMAPs) from the tibialis anterior (TA) and abductor hallucis (AH) muscles in the lower extremities (the rectus femoris [RF] was added in 2013) and from the abductor digiti minimi (ADM) muscle in the upper extremities. Bilateral ADM responses were used as controls to differentiate between surgical and nonsurgical loss of limb responses and identify brachial plexus compromise due to patient positioning. MEPs were elicited periodically by delivering an anodal pulse train of 4–7 pulses of 0.5 ms duration and interstimulus interval of 2–4 ms at amplitudes of 200–500 V (fixed voltage system) or 150–220 mA (fixed current system) between two corkscrew electrodes positioned over the motor cortex at C1 and C2. The stimulus strength was optimised to elicit reproducible responses. In patients with grade IV and V spondylolisthesis included in this series we added MEP recording from the anal sphincter and the gastrocnemius to the multimodal technique in order to monitor the sacral nerve roots.
Alarm Criteria
Action was taken when:
Mode 1-cortical SSEPs: unilateral or bilateral responses dropped >50% in amplitude with or without a corresponding increase in latency >10% of reference traces.
Mode 2-cervical SSEPs: unilateral or bilateral responses dropped >50% in amplitude with or without corresponding increase in latency >10% of reference traces.
Mode 3-MEPs: MEP-evoked CMAP responses in any muscle were lost and remained absent. Any sudden drop in amplitude of MEP traces >80% of reference traces was reported and investigated.
Decisions during surgery in response to IOM findings rested with the surgeon. Close collaboration with our anaesthetic and neurophysiology teams was mandatory to secure accurate interpretation of IOM changes, to initiate an immediate response, and prevent neurological damage. In all cases of IOM events, the routine initial check included mean arterial blood pressure that was raised to >80mm Hg and body temperature >36.5°C. Technical problems with the recording system or due to dislodgement of the electrodes were also excluded. Muscle relaxant (atracurium) given during soft tissue dissection had metabolised and another baseline IOM recording was obtained before placement of instrumentation.
IOM Diagnostic Criteria
IOM events were classified by time of onset and by type of event. Time of onset was split into immediate events that occurred immediately after a surgical action or delayed events that we defined as a loss of responses, after baseline traces were present upon completion of instrumentation and correction. Our diagnostic criteria for type of IOM monitoring events are presented in
Table 1 [
11].
Results
We identified 1881 patients (562 male:1319 female) with a mean age of 14.2 years (range 1-25 years). 59.1% (n = 1112) of patients had surgery to treat an Adolescent Idiopathic Scoliosis (AIS). A further breakdown of the primary diagnosis is listed in
Table 2. In total, 1780 patients underwent posterior spinal instrumentation and fusion, 41 patients underwent anterior spinal instrumentation and fusion, and 36 patients underwent a combined anterior release and posterior instrumented fusion. 24 patients had insertion of growing rods. Multimodal monitoring was achieved in 93.9% (1767/1881) of patients. In 0.6% (11/1881) of patients reproducible monitoring responses were unachievable and so intraoperative neuromonitoring was abandoned. Unimodal monitoring was achieved in 2.3% (44/1881) and bimodal monitoring was achieved in 3.1% (59/1881) of patients. Of those patients that multimodal was not achieved, the predominant (75%, 85/114 patients) diagnosis was either neuromuscular or syndromic scoliosis.
Neuro-Monitoring Events
Of the 1870 patients that had intra-operative monitoring for the duration of their surgical procedure, 3% (61/1870) of patients (18 male:43 female) had a positive IOM event meeting the alarm criteria outlined in
Table 3. 2.4% (44/1870) of patients had a true positive event, of which 43 events were transient. 35 patients had acute events and 9 patients had delayed events. 0.9% (17/1870) of patients had a false positive event. 97% (1809/1870) of patients had a true negative IOM. No patient had a false negative IOM. The sensitivity of intraoperative spinal cord monitoring with MEPs and SSEPs for our cohort was 1.0 and the specificity was 0.99. The positive predictive value was 0.73 and the negative predictive value was 1.0.
True Positive Acute Events (Table 2)
There was 1 true positive event and 34 transient true positive events. In the true positive event the change in monitoring was not attributable to a surgical step and failed to improve after reversal of surgical steps including removal of spinal instrumentation. No canal breach was identified and postoperative investigations supported a vascular event to the cord. The patient recovered to baseline neurological function within 3 months of surgery. The transient events were associated with surgical events, with the most common being rod reduction (11 patients, 41%) and screw insertion (10 patients, 37%). Other causes included pedicle hook insertion (3 patients, 11%), sublaminar wire insertion (2 patients, 7%), posterior facetectomy (2 patients, 7%), patient positioning (2 patients, 7%), rod distraction (1 patient, 4%), application of skeletal traction (1 patient, 4%), psoas retraction during an antero-lateral approach (1 patient, 4%) and 1 was undetermined.
True Positive Delayed Events
9 patients (3 male:6 female) had a true positive delayed event after posterior segmental pedicle screw instrumentation. Mean age was 12.5 (2-17) years. 6 patients had idiopathic scoliosis (4 AIS, 2 JIS), 1 patient congenital scoliosis, 1 neuromuscular scoliosis and 1 patient had thoracic kyphosis post-vertebral osteomyelitis. In those patients with scoliosis, the mean thoracic curve angle was 78° (51-94°). Mean estimated blood volume loss was 28%. Titanium beam shaped rods were utilised in 3 patients and 5.5 mm titanium rods in 6. MEPs were lost on average 18 (10-30) minutes after completion of instrumentation. All alarms were Mode 3 alarms; 7 patients had bilateral loss and 2 patients had unilateral loss of MEPs. Sensory evoked potential amplitude was temporarily reduced in 1 patient and was preserved in all other cases. There was a transient latency shift in one another patient. The MEPs returned within 20 minutes of rod release in all patients. The rod was re-contoured to incorporate more scoliosis in 1 patient. 2 patients had beam rods exchanged to 5.5 mm titanium rods. 6 patients had rod removal with retention of pedicle screws and staged completion of instrumentation at mean 5 (1-7) days later. No patients had a postoperative neurological deficit.
False Positive Events
0.9% (17/1870) of patients had a false positive event. 14 of these were acute and 3 were delayed events experienced after completion of instrumentation. 53% (9/17) of false positive events were associated with a reduction in patient blood pressure and resolved with an increase in mean arterial pressure to 85-90 mm Hg. In one patient this hypotension was secondary to intra-operative administration of Clonidine for analgesia. In 1 patient, responses dropped during exposure and recovered before placement of instrumentation. This was attributed to be an acute drop in patient temperature, normalising with patient warming. In 1 patient MEP loss recovered to reproducible baseline after adjustment of stimulus. 1 patient had IOM loss attributed to a technical fault with the monitoring software and confirmed with a normal wake up test. 2 patients had return of baseline monitoring without surgical intervention or identified haemodynamic adjustment. In 2 patients with AIS, removal of instrumentation was done with no change in monitoring. Despite monitoring change, both patients woke with no neurological deficit and normal postoperative imaging. Re-instrumentation and definitive fusion were successfully re-attempted and completed within two weeks of initial surgery.
Discussion
IOM is recommended in procedures where there is risk of neurological injury including scoliosis surgery [
6,
10]. Fehlings et al. [
11], in their systematic review of 32 studies determined that strong evidence exists that multimodal IOM is sensitive and specific for detecting intra-operative neurological injury and recommended the use of such monitoring for spinal deformity correction. Our series shows that multimodal IOM is achievable in 94% of paediatric and adolescent spinal deformity procedures while reproducible neuro-monitoring was not achievable in less than 1% of patients. Furthermore, when used in conjunction with a standardised management algorithm, IOM is highly sensitive (100%) and specific (99%) in the detection of acute intra-operative neurological dysfunction [
9].
Thuet et al. [
6] reported a false negative rate of 0.2% in their 23-year retrospective series of 3436 pediatric patients undergoing spinal surgery using varying IOM methods. This is in contrast to our study where we had 0% false negative IOM events. We feel that this reflects the advancement of monitoring techniques and further development of the skills of the specialised neuro-physiology teams. Fortunately, the incidence of true positive events is low with only 1 patient having sustained IOM loss together with a postoperative deficit that later recovered. The remainder of the acute true positive events were transient with recovery to baseline following surgical intervention. Lee et al. [
12] identified greater preoperative Cobb angle of the major structural curve, number of levels fused, operative time and estimated blood loss as risk factors for spinal cord injury during deformity correction which can cause IOM loss. In our cohort, the most common cause of a transient true positive event was during placement of instrumentation of the spine, accounting for 44% (15/34) of events (29% screw insertion, 9% pedicle hook insertion and 6% sublaminar wire insertion). The second most common cause of transient true positive events was during reduction manoeuvres including rod distraction (35%, 11/34).
In our series, the highest risk of true positive IOM event was seen in syndromic scoliosis (5.5%). The next highest within our cohort was seen in spondylolisthesis (3.7%). However, this only represented a single event in a small sample size (1/27). The next highest was seen in juvenile idiopathic scoliosis and adolescent idiopathic scoliosis. Neuromuscular scoliosis and Scheuermann kyphosis had similar rate of true positive IOM events (
Table 2). This is different from the rate of true positive events reported in the literature [
10,
13,
14,
15]. We found a difference between Scheuermann kyphosis and AIS on the risk of true positive events with event incidence of 2/111 patients (1.8%) in Scheuermann kyphosis versus 23/1112 patients (2.1%) in AIS. Previous studies suggested greater risk of neurological complications in patients with thoracic hyper-kyphosis and those requiring corrective osteotomies [
10,
16,
17]. Although there are differences in sample size, this was not demonstrated in our cohort. The increased rate of events in early onset idiopathic scoliosis is likely representative of curve severity and curve stiffness within this subgroup.
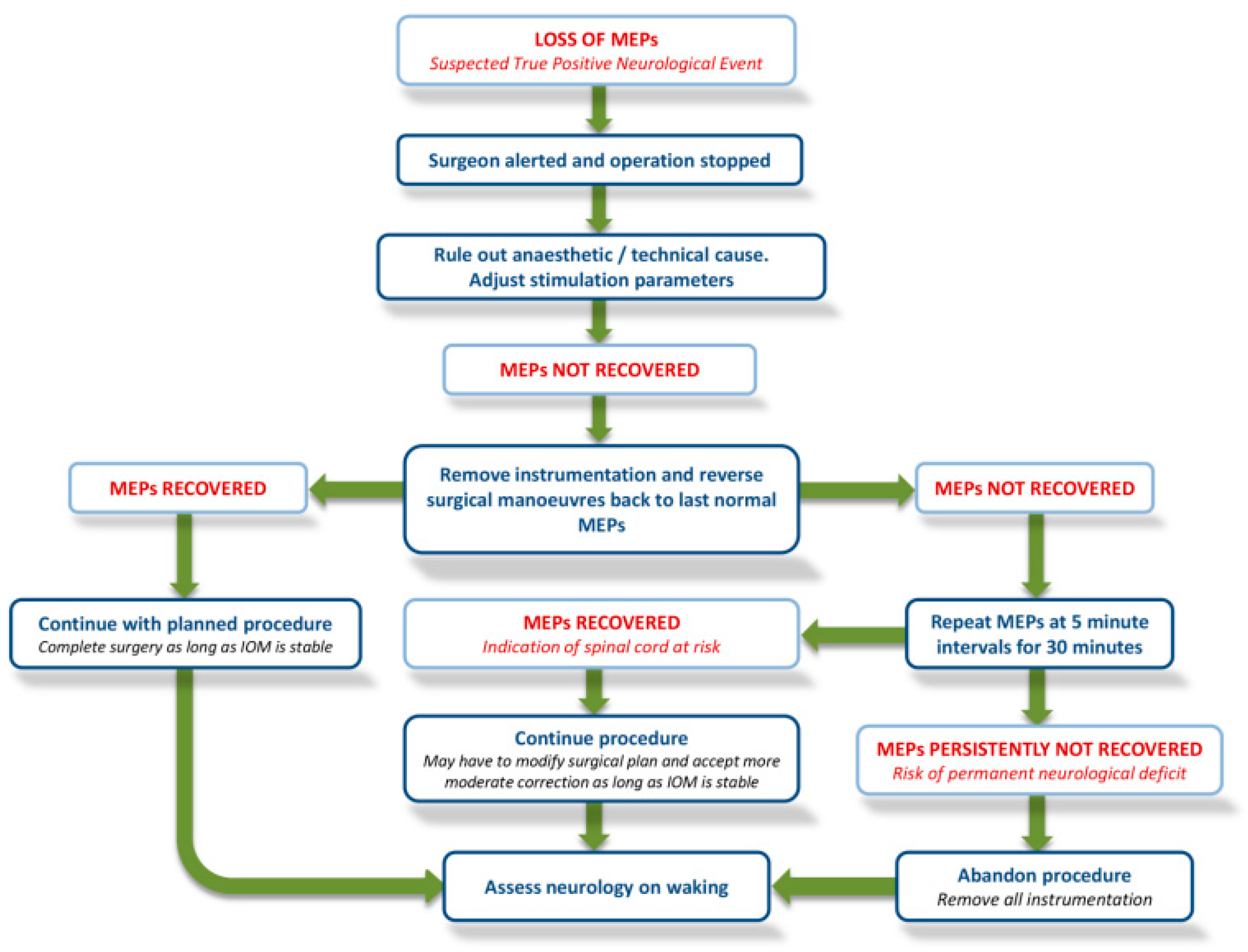
False positive events do continue to occur, however these can only be classified after systematically excluding a direct cause for the event. This is best achieved by following a structured algorithm or cord-at-risk protocol, such as that illustrated in
Figure 1 [
9]. This requires effective working within the multi-disciplinary theatre team and good communication with the anaesthetic team to ensure drug administration, haemodynamic stability and temperature are all appropriate.
Delayed Event
A delayed IOM event is defined as change in IOM after completion of instrumentation. There is lack of information in the literature as far as delayed loss of IOM signals after spinal deformity surgery is concerned. Stöckl et al. [
18] reported 2 cases of delayed motor deficit after posterior scoliosis correction. Both patients improved after removal of instrumentation. Lovi et al. [
19] reported a case of delayed postoperative neurological deficit far from the surgical site in a patient with syndromic scoliosis. The authors concluded that delayed postoperative neurological deficit far from the surgical site can be considered a specific subgroup of these rare complication that can occur several hours after spine surgery, regardless of intraoperative complication. Removal of instrumentation was sufficient to regain full motor recovery caudal to the level of instrumentation.
In our study, there were 9 delayed true positive IOM events. These represented 16% of all true positive IOM events and an overall incidence of 1 in 200 procedures. This emphasises the importance of continuation of monitoring after deformity correction and completion of spinal instrumentation. In our cohort, patients’ MEPs were lost on average 18 minutes after completion of instrumentation with a range of 10-30 minutes. We, therefore, recommend continuing neuro-monitoring for at least 30 minutes after placement of instrumentation or until skin closure; thereby, minimising the period between discontinuing monitoring and the patient being awake to perform a formal neurological evaluation.
We would hypothesise that these delayed events are due to spinal cord ischaemia secondary to segmental artery hypo-perfusion as a result of vessel tension. Meylaerts et al. [
20] showed recovery of MEPs by restoration of spinal cord perfusion during thoraco-abdominal aortic aneurysm repair. Sandhu et al. [
21] also described fluctuations in spinal cord perfusion pressure as cause of delayed paraplegia after thoraco-abdominal aortic repair.
The pathophysiology of intra-operative spinal cord injury during deformity correction was studied by Turner et al. [
22] combining spinal cord perfusion (SCP) with intrathecal pressure and neurological monitoring (MEP). The authors depicted a direct relation between SCP fluctuation and MEPs reduction. As we know hypotension correction is one of the most widely performed general measure following an intra-operative alert, since there is good evidence that even a mild drop in systemic systolic blood pressure can affect the motor potentials profile [
11,
22]. Releasing rods reduces cord/vascular tension and aids cord re-perfusion. MEPs returned within 20 minutes of rod release in all patients.
The stiffness of the rod could be influential in the incidence of delayed events. Within our institution the beam shape rods are utilised in a small percentage of patients, yet these were associated with 33% of the delayed IOM events. Due to the difference in Young’s modulus of elasticity, beam shape rods are stiffer than standard titanium cylindrical rods and, therefore, have reduced capacity to undergo plastic/elastic deformation, thereby potentially leading to increased cord/vascular tension. On review of patient risk factors for delayed events, we identified no significant difference within this subgroup when we looked at age, diagnosis, curve angle and estimated blood loss.
We have proposed an algorithm to allow the surgical team to decide appropriate actions in response to MEP loss (
Figure 1) [
9]. There are existing guidelines, checklists, and algorithms for the prevention, identification, and management of neurological complications in spine surgery [
23,
24,
25,
26]. We advocate the need for close cooperation and continuous communication of the surgical/anaesthetic/neurophysiology teams before, during, and after surgery. In our experience, this coordinated approach has allowed appropriate response to IOM changes and ensured that no patient in this series developed neurological deficits contrary to previous studies which reported risk of permanent neurological injury of 0.1–0.2% [
13,
17]. In the patient consent, we recommend a detailed discussion on IOM and the possible need to abandon surgery depending on IOM findings and complete it in a staged manner at a later date.
Limitations
While we have addressed some of the risk factors for neurological injury/IOM event, further analysis could have been performed looking at curve stiffness and it would also be useful to assess percentage curve correction at the time of IOM event but this is not possible with the patients lying in the supine position and the limited information provided by intra-operative imaging. Additionally, the literature reports the use of pre-operative MRI to assess the risk of intra-operative neuromonitoring data loss and it may have been beneficial utilise this classification in our patients and to correlate this with our findings [
27]. Unfortunately, as we run a tertiary centre, many of the MRI scans are performed at the point of referral, and not at the point of surgery, therefore we did not feel they would accurately represent the curve characteristics at the time of intervention
Conclusions
We present one of the largest cohorts of spinal cord monitoring outcomes in spinal deformity. This provides further support that multimodal IOM is the gold standard of neuro-monitoring during deformity correction with excellent sensitivity and specificity. We feel that this study will aid the surgeons in standardisation of practice and will also facilitate in educating and consenting patients on the risks of monitoring events and neurological injury during spinal deformity surgery. Delayed IOM loss represented 16% of all events with the likely mechanism of increased cord tension and hypo-perfusion. The timing of events emphasises the importance of continued monitoring for at least 30 minutes after completion of instrumentation or until wound closure. Surgeons should be particularly vigilant for delayed events when using stiffer rod constructs.
Author Contributions
Tristan McMillan: writing original draft and review. Atul Vats: writing and editing. Enrique Garrido: review. Ciara Michaelson: review, Athanasios I. Tsirikos: Conceptualization (lead) and review.
Funding
Nothing to declare.
Consent and Institutional Review Board statement
As this is a retrospective analysis of practice and doesn’t involve any clinical encounter, no consent or institutional board approval was needed.
Data availability
Data that supports the study are available from the corresponding author(TM) on request.
Disclosure Statement
The authors did not receive grants or outside funding in support of their research or preparation of this manuscript. They did not receive payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or debit, any benefits to any research fund, foundation, educational institution, or other charitable or non-profit organisation with which the authors are affiliated or associated.
Conflicts of Interest
None.
References
- Diab, M.; Smith, A.R.; Kuklo, T.R.; Spinal Deformity Study Group. Neural complications in the surgical treatment of adolescent idiopathic scoliosis. Spine 2007, 32, 2759–2763. [Google Scholar] [CrossRef]
- Qiu, Y.; Wang, S.; Wang, B.; Yu, Y.; Zhu, F.; Zhu, Z. Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine 2008, 33, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Vauzelle, C.; Stagnara, P.; Jouvinroux, P. Functional monitoring of spinal cord activity during spinal surgery. Clin Orthop Relat Res 1973, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, L.; Lamb, J.; Grevitt, M.; Mehdian, S.M.; Webb, J.K.; Blumhardt, L.D. Combined monitoring of motor and somatosensory evoked potentials in orthopaedic spinal surgery. Clin Neurophysiol 2002, 113, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Nuwer, M.R.; Dawson, E.G.; Carlson, L.G.; Kanim, L.E.; Sherman, J.E. Somatosensory evoked potential spinal cord monitoring reduces neurologic deficits after scoliosis surgery: results of a large multicenter survey. Electroencephalogr Clin Neurophysiol 1995, 96, 6–11. [Google Scholar] [CrossRef]
- Sutter, M.; Deletis, V.; Dvorak, J.; Eggspuehler, A.; Grob, D.; Macdonald, D.; et al. Current opinions and recommendations on multimodal intraoperative monitoring during spine surgeries. Eur Spine J 2007, 16 (Suppl. 2), S232–S237. [Google Scholar] [CrossRef] [PubMed]
- Thuet, E.D.; Winscher, J.C.; Padberg, A.M.; Bridwell, K.H.; Lenke, L.G.; Dobbs, M.B.; et al. Validity and reliability of intraoperative monitoring in pediatric spinal deformity surgery: a 23-year experience of 3436 surgical cases. Spine 2010, 35, 1880–1886. [Google Scholar] [CrossRef] [PubMed]
- Dikmen, P.Y.; Halsey, M.F.; Yucekul, A.; de Kleuver, M.; Hey, L.; Newton, P.O.; Havlucu, I.; Zulemyan, T.; Yilgor, C.; Alanay, A. Intraoperative neuromonitoring practice patterns in spinal deformity surgery: a global survey of the Scoliosis Research Society. Spine Deform 2021, 9, 315–325. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; Duckworth, A.D.; Henderson, L.E.; Michaelson, C. Multimodal Intraoperative Spinal Cord Monitoring during Spinal Deformity Surgery: Efficacy, Diagnostic Characteristics, and Algorithm Development. Med Princ Pract 2020, 29, 6–17. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pastorelli, F.; Di Silvestre, M.; Plasmati, R.; Michelucci, R.; Greggi, T.; Morigi, A.; et al. The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J 2011, 20 (Suppl. S1), S105–S114. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Brodke, D.S.; Norvell, D.C.; Dettori, J.R. The evidence for intraoperative neurophysiological monitoring in spine surgery: does it make a difference? Spine 2010, 35 (Suppl. 9), S37–S46. [Google Scholar] [CrossRef]
- Lee, C.S.; Hwang, C.J.; Lee, D.H.; Cho, J.H.; Park, S. Risk Factors and Exit Strategy of Intraoperative Neurophysiological Monitoring Alert During Deformity Correction for Adolescent Idiopathic Scoliosis. Global Spine J 2023. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Zuccaro, M.; Zuccaro, J.; Samdani, A.F.; Pahys, J.M.; Hwang, S.W. Intraoperative neuromonitoring alerts in a pediatric deformity center. Neurosurg Focus 2017, 43, E8. [Google Scholar] [CrossRef] [PubMed]
- Ghazi, J.; Sparagana, S.; Rampy, P.; Sucato, D.; Johnson, M. Upper extremity neuromonitoring changes are more common than lower extremity during spinal fusion for Scheuermann's kyphosis. Spine Deformity 2023, 11, 1253–1259. [Google Scholar] [CrossRef] [PubMed]
- Kasliwal, M.K.; Smith, J.S.; Shaffrey, C.I.; Saulle, D.; Lenke, L.G.; Polly, D.W., Jr.; Ames, C.P.; Perra, J.H. Short-term complications associated with surgery for high-grade spondylolisthesis in adults and pediatric patients: A report from the scoliosis research society morbidity and mortality database. Neurosurgery 2012, 71, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Lewis, N.D.; Keshen, S.G.; Lenke, L.G.; Zywiel, M.G.; Skaggs, D.L.; Dear, T.E.; et al. The Deformity Angular Ratio: Does It Correlate With High-Risk Cases for Potential Spinal Cord Monitoring Alerts in Pediatric 3-Column Thoracic Spinal Deformity Corrective Surgery? Spine 2015, 40, E879–85. [Google Scholar] [CrossRef] [PubMed]
- Leong, J.J.; Curtis, M.; Carter, E.; Cowan, J.; Lehovsky, J. Risk of Neurological Injuries in Spinal Deformity Surgery. Spine 2016, 41, 1022–1027. [Google Scholar] [CrossRef] [PubMed]
- Stöckl, B.; Wimmer, C.; Innerhofer, P.; Kofler, M.; Behensky, H. Delayed anterior spinal artery syndrome following posterior scoliosis correction. Eur Spine J 2005, 14, 906–909. [Google Scholar] [CrossRef]
- Lovi, A.; Manfroni, F.; Luca, A.; et al. Delayed postoperative cervical spinal cord ischemic lesion after a thoracolumbar fusion for syndromic scoliosis: a case report and systematic review of the literature. Childs Nerv Syst 2022, 38, 1011–1015. [Google Scholar] [CrossRef]
- Meylaerts, S.A.; Jacobs, M.J.; van Iterson, V.; De Haan, P.; Kalkman, C.J. Comparison of transcranial motor evoked potentials and somatosensory evoked potentials during thoracoabdominal aortic aneurysm repair. Ann Surg 1999, 230, 742–749. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sandhu, H.K.; Evans, J.D.; Tanaka, A.; Atay, S.; Afifi, R.O.; Charlton-Ouw, K.M.; Azizzadeh, A.; Miller, C.C., 3rd; Safi, H.J.; Estrera, A.L. Fluctuations in Spinal Cord Perfusion Pressure: A Harbinger of Delayed Paraplegia After Thoracoabdominal Aortic Repair. Semin Thorac Cardiovasc Surg 2017, 29, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Turner, J.D.; Eastlack, R.K.; Mirzadeh, Z.; Nguyen, S.; Pawelek, J.; Mundis, G.M., Jr. Fluctuations in Spinal Cord Perfusion during Adult Spinal Deformity Correction Identify Neurologic Changes: Proof of Concept. World Neurosurgery 2016, 85, 365.E1–365.E6. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.K.; Smith, J.S.; Sansur, C.A.; Glassman, S.D.; Ames, C.P.; Berven, S.H.; et al. Scoliosis Research Society Morbidity and Mortality Committee Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine 2011, 36, 1218–1228. [Google Scholar] [CrossRef] [PubMed]
- Ziewacz, J.E.; Berven, S.H.; Mummaneni, V.P.; Tu, T.H.; Akinbo, O.C.; Lyon, R.; et al. The design, development, and implementation of a checklist for intraoperative neuromonitoring changes. Neurosurg Focus 2012, 33, E11. [Google Scholar] [CrossRef]
- Pahys, J.M.; Guille, J.T.; D'Andrea, L.P.; Samdani, A.F.; Beck, J.; Betz, R.R. Neurologic injury in the surgical treatment of idiopathic scoliosis: guidelines for assessment and management. J Am Acad Orthop Surg 2009, 17, 426–434. [Google Scholar] [CrossRef]
- British Society for Clinical Neurophysiology ANS/BSCN Guidelines for Neurophysiological Recordings of the Spinal Cord during Corrective Spinal Deformity Surgery 2013. 2018. http://www.bscn.org.uk/content.aspx?Group=guidelines&Page=guidelines_IOM.
- Sielatycki, J.A.; Cerpa, M.; Baum, G.; Pham, M.; Thuet, E.; Lehman, R.A.; Lenke, L.G. A novel MRI-based classification of spinal cord shape and CSF presence at the curve apex to assess risk of intraoperative neuromonitoring data loss with thoracic spinal deformity correction. Spine Deform 2020, 8, 655–661. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).