Submitted:
18 July 2024
Posted:
25 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Background
1.2. Objective
1.3. Significance
2. Methods
2.1. Data Collection
2.2. Variables
2.3. Statistical Analysis
2.4. Tools and Techniques
3. Results
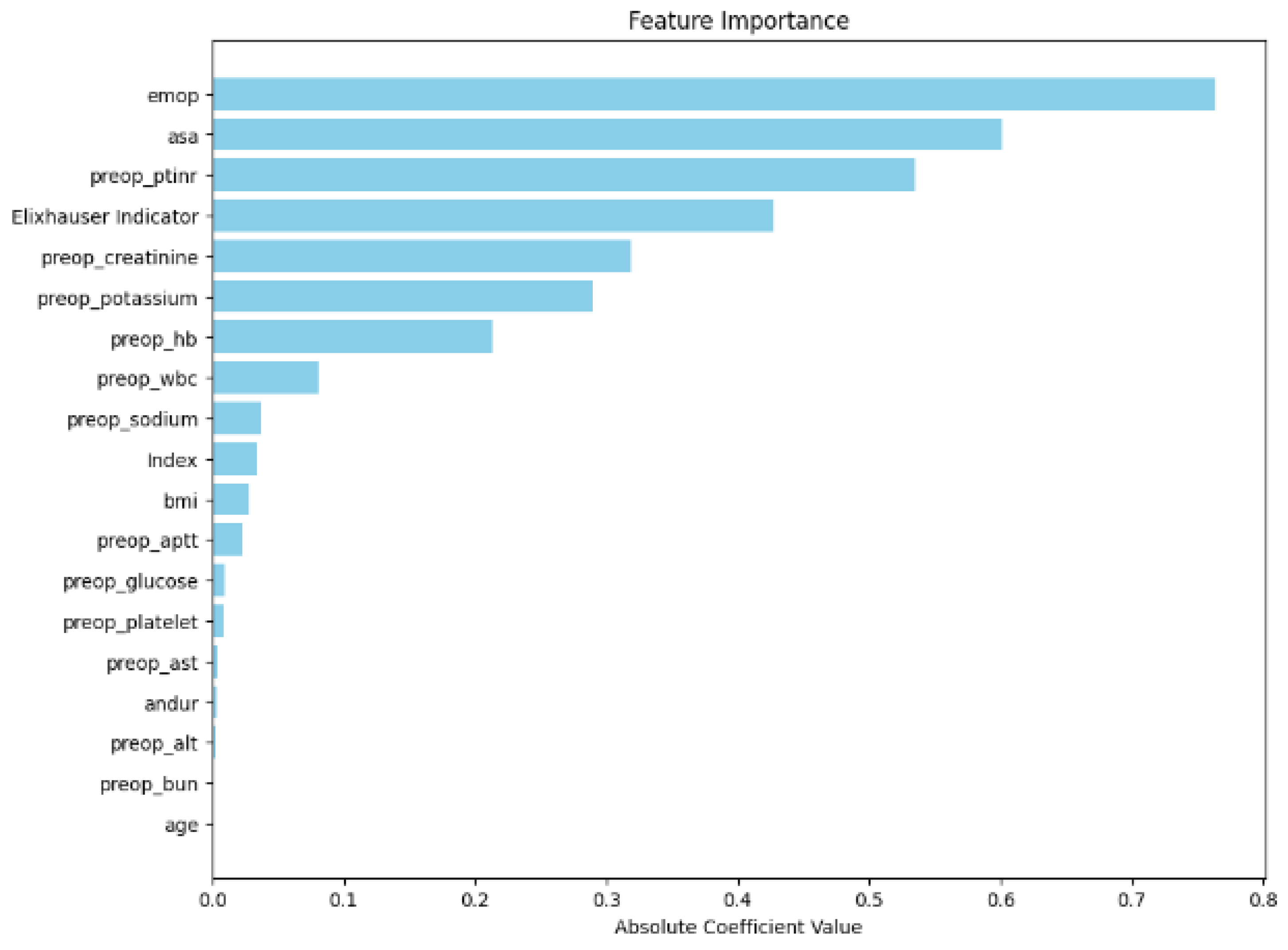
3.1. Feature Importance
3.2. Model Performance
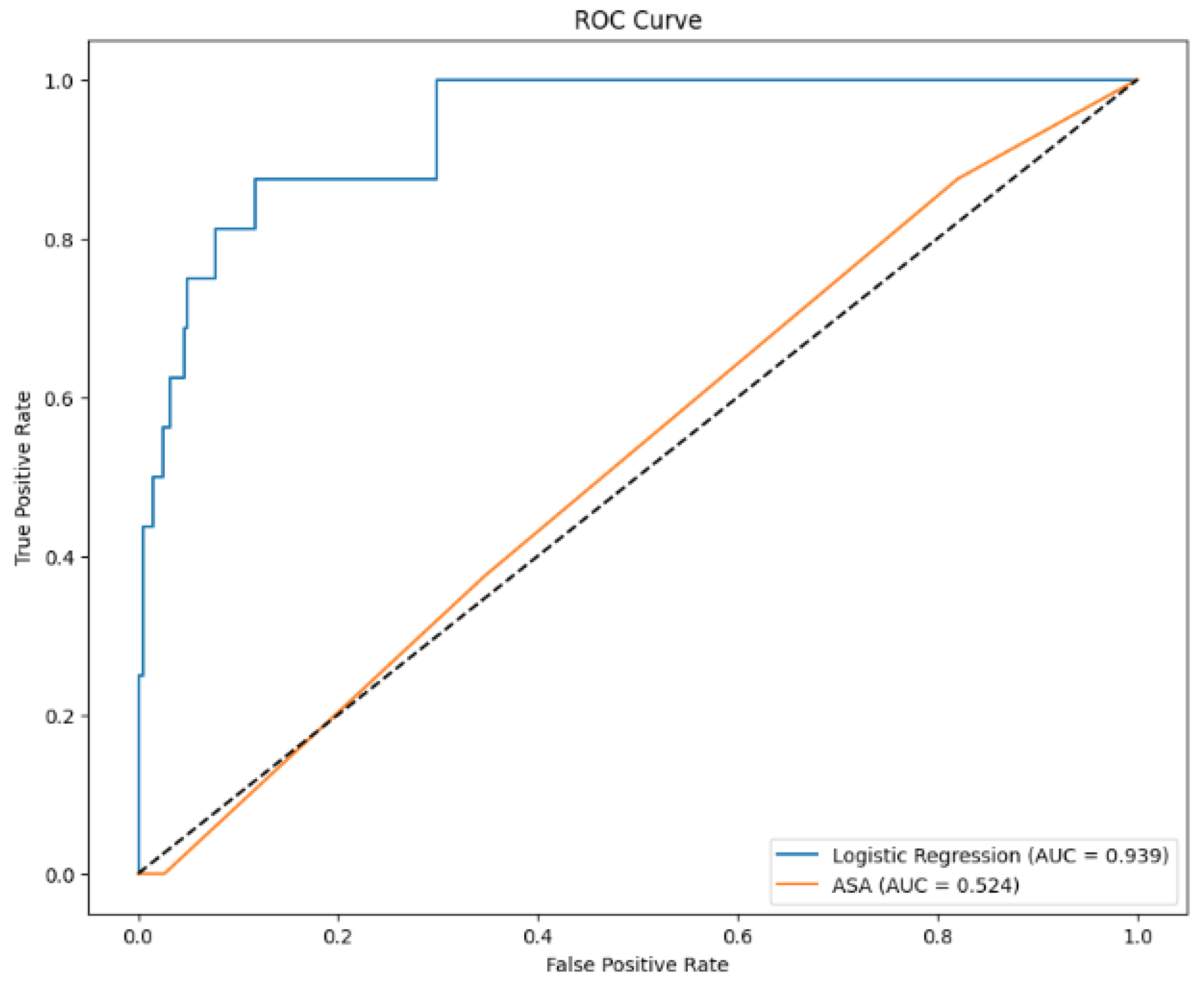
3.3. ROC Curve
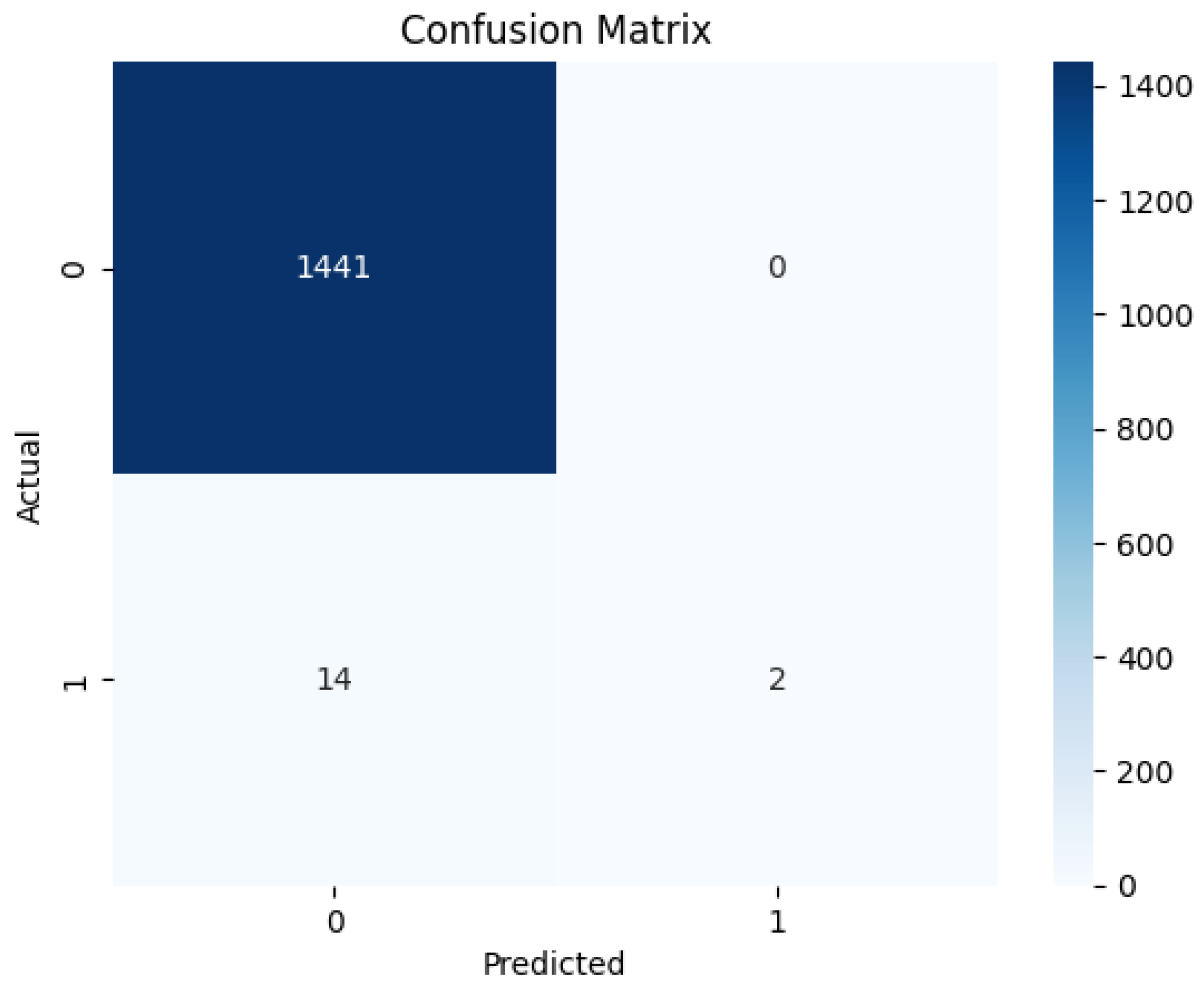
3.4. Confusion Matrix
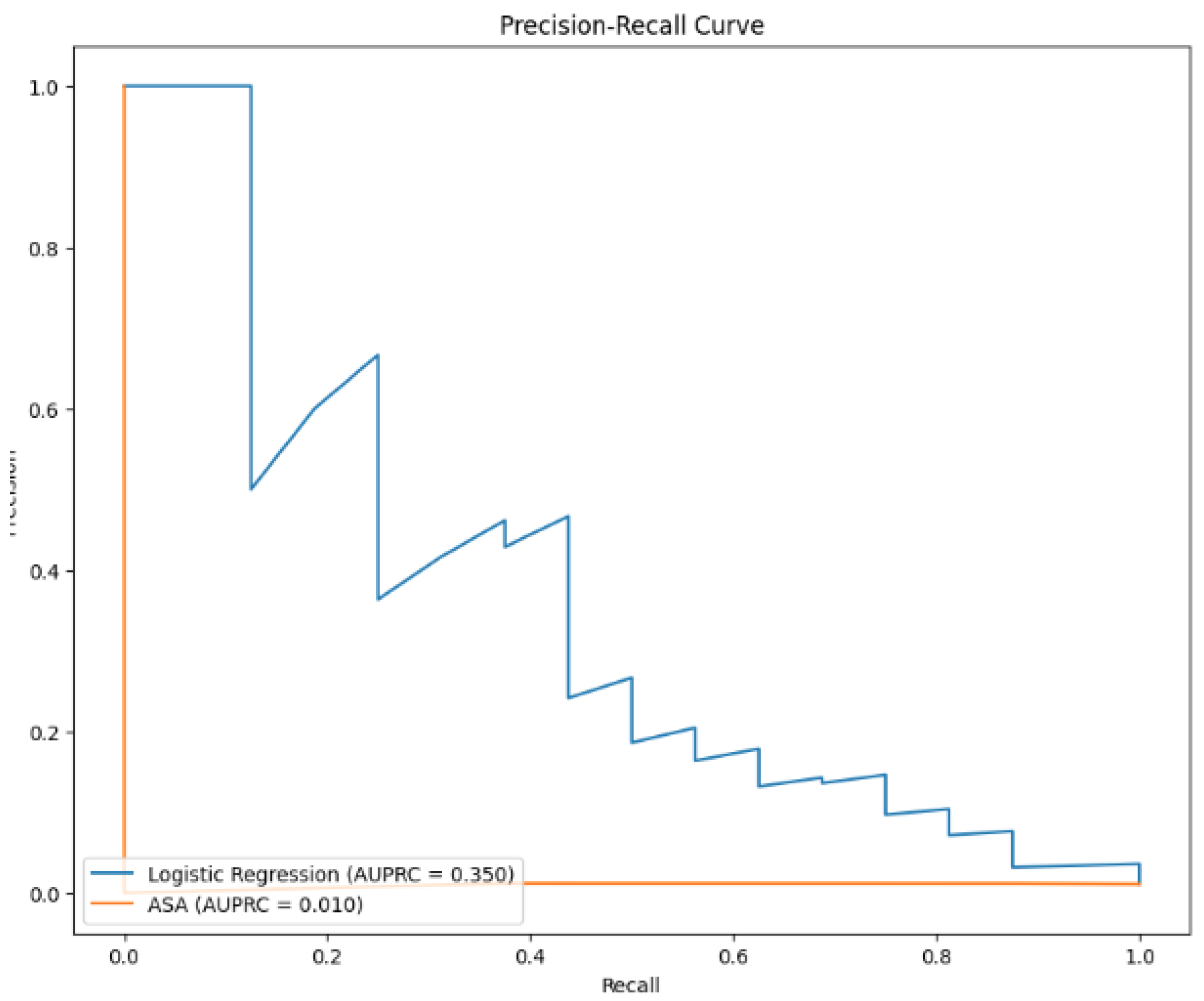
3.5. Precision-Recall Curve
4. Discussion
4.1. Interpretation of Results
4.2. Strengths and Limitations
4.3. Future Work
5. Conclusion
5.1. Summary
5.2. Implications
References
- Benedetto, U., Sinha, S., Lyon, M., Dimagli, A., Gaunt, T. R., Angelini, G., & Sterne, J. (2020). Can machine learning improve mortality prediction following cardiac surgery? European Journal of Cardio-Thoracic Surgery: Official Journal of the European Association for Cardio-thoracic Surgery.
- Brobbey, A., Bruning, J. W., & Cimini, M. (2018). Ensemble-based classification models for predicting post-operative mortality risk in coronary artery disease. Journal of Biomedical Informatics, 78, 39-49.
- Choi, B., Oh, A., Lee, S.-H., Lee, D. Y., Lee, J.-H., Yang, K., Kim, H. Y., Park, R. W., & Park, J. (2022). Prediction model for 30-day mortality after non-cardiac surgeryusing machine-learning techniques based on preoperative evaluation of electronic medical records. Journal of Clinical Medicine, 11, 6487.
- Fan, Y., Dong, J., Wu, Y., Shen, M., Zhu, S., He, X., Jiang, S., Shao, J., & Song, C. (2021). Development of machine learning models for mortality risk prediction after cardiac surgery. Cardiovascular Diagnosis and Therapy, 12(1), 12-23.
- Fernandes, M., Armengol de la Hoz, M. Á., Rangasamy, V., & Subramaniam, B. (2020). Machine learning models with preoperative risk factors and intraoperative hypotension parameters predict mortality after cardiac surgery. Journal of Cardiothoracic and Vascular Anesthesia.
- Fritz, B., Cui, Z., Zhang, M., He, Y., Chen, Y., Kronzer, A., Ben Abdallah, A., King, C., & Avidan, M. (2019). Deep-learning model for predicting 30-day postoperative mortality. British Journal of Anaesthesia.
- Kilic, A., Goyal, A., Miller, J. K., Gjekmarkaj, E., Tam, W., Gleason, T., Sultan, I., & Dubrawksi, A. (2019). Predictive utility of a machine learning algorithm in estimating mortality risk in cardiac surgery. The Annals of Thoracic Surgery.
- Rahmanian, P. B., Adams, D. H., & Castillo, J. G. (2010). Predicting hospital mortality and analysis of long-term survival after major noncardiac complications in cardiac surgery patients. The Annals of Thoracic Surgery, 90(3), 902-909.
- Widyastuti, Y., Khusen, M., Prihartono, J., & Soesastro, Y. (2012). Preoperative and intraoperative prediction of risk of cardiac dysfunction following open heart surgery. The Journal of Thoracic and Cardiovascular Surgery, 143(1), 178-186.
- Yu, Y., Peng, C., Zhang, Z., Shen, K., Zhang, Y., Xiao, J., Xi, W., Wang, P.-Y., Jin, Z., & Wang, Z. (2021). Machine learning methods for predicting long-term mortality in patients after cardiac surgery. Frontiers in Cardiovascular Medicine, 9.
- Zeng, J., Zhang, D., Lin, S., Su, X., Wang, P., Zhao, Y., & Zheng, Z. (2023). Comparative analysis of machine learning versus traditional modeling approaches for predicting in-hospital mortality after cardiac surgery: assessment from temporal and spatial external validation based on a nationwide cardiac surgery registry. European Heart Journal - Quality of Care & Clinical Outcomes.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).



