1. Introduction
Virtual reality (VR) is one of the most promising technologies for neurorehabilitation. The main advantages of this technology are the easiness of use, its safety, the low costs with respect to other technologies, its portability, the embedded sensors that can provide informative data [
1]. However, in many reviews the efficacy of virtual reality has been evaluated including non-immersive interactive video gaming systems into the meta-analysis [
2,
3], despite VR has a specific definition. In fact, VR has been defined as a high-end user-computer interface involving real-time stimulation and interactions of subject embedded into a digital world through multiple sensorial channels in which the subject feels his presence, the ownership of the body of his/her avatar and the possibility to interact with that world [
4,
5].
A critical limitation of the existing literature is that the meta-analysis aggregated studies based solely on VR hardware, disregarding software-specific content and rehabilitative principles. This approach conflates diverse VR applications, including gaming, physical and cognitive exercises, and real-life simulations.
In 2021, we tested the usability of VR for administering a protocol of art-therapy in which patients with stroke could paint a virtual canvas [
6]. A novel aspect of this approach was the potential of VR to induce the illusion in patients that they were perfectly replicating iconic artworks, such as the Creation of Adam of Michelangelo or the Birth of Venus of Botticelli. It combined the advantages of visual art fruition, mainly related to the wide arousal of brain networks activated by the vision of artistic masterpieces [
7], and the active involvement typical of artistic creation [
8].
This approach allowed to discover the “Michelangelo effect”, i.e. healthy subjects and patients perceived less fatigue and were more accurate in the upper limb movements when they had the illusion of painting an art masterpieces with respect to when they were simply asked to colour the digital canvas, highlighting the importance of the content within the required task [
6].
In a previous pilot study, involving 20 patients with stroke in subacute phase (10 treated with this virtual art-therapy protocol and 10 with conventional rehabilitation), we found a statistically significant higher improvement in patients treated with VR in terms of independency in activities of daily living (p=0.021, assessed by Barthel Index). The improvements in upper limb force (Manual Muscle Test) and in reduction of spasticity (Ashworth Scale) only approached the statistically significant threshold (p=0.063 and p=0.055, respectively), suggesting the need to enroll more patients to obtain more consistent results [
9].
In the present study, we expanded the data collection by using the previous protocol [
6], doubling the number of patients with stroke in subacute phase. The aim of this study was to test the efficacy of the proposed virtual reality art-therapy protocol with respect to conventional therapy for patients with stroke. The secondary aim is to test whether the efficacy of VR is correlated with the active participation of patients or to a reduction of fatigue perception in the VR protocol.
2. Materials and Methods
2.1. Participants
The study was conducted in accordance with the ethical standards in the 2013 Declaration of Helsinki, and approved by the Local Ethical Committee. All patients signed written informed consent. Inclusion criteria were: patients admitted to our hospitals for rehabilitation, clinical diagnosis of ischemic or hemorrhagic stroke confirmed by computerized tomography or magnetic resonance, age between 40 and 90. Exclusion criteria were: inability to understand and follow the instructions given by therapists (Mini Mental State Evaluation <24) [
20]; presence of risk of visual epilepsy, unilateral spatial neglect, severe comorbidities.
2.2. Study Protocol
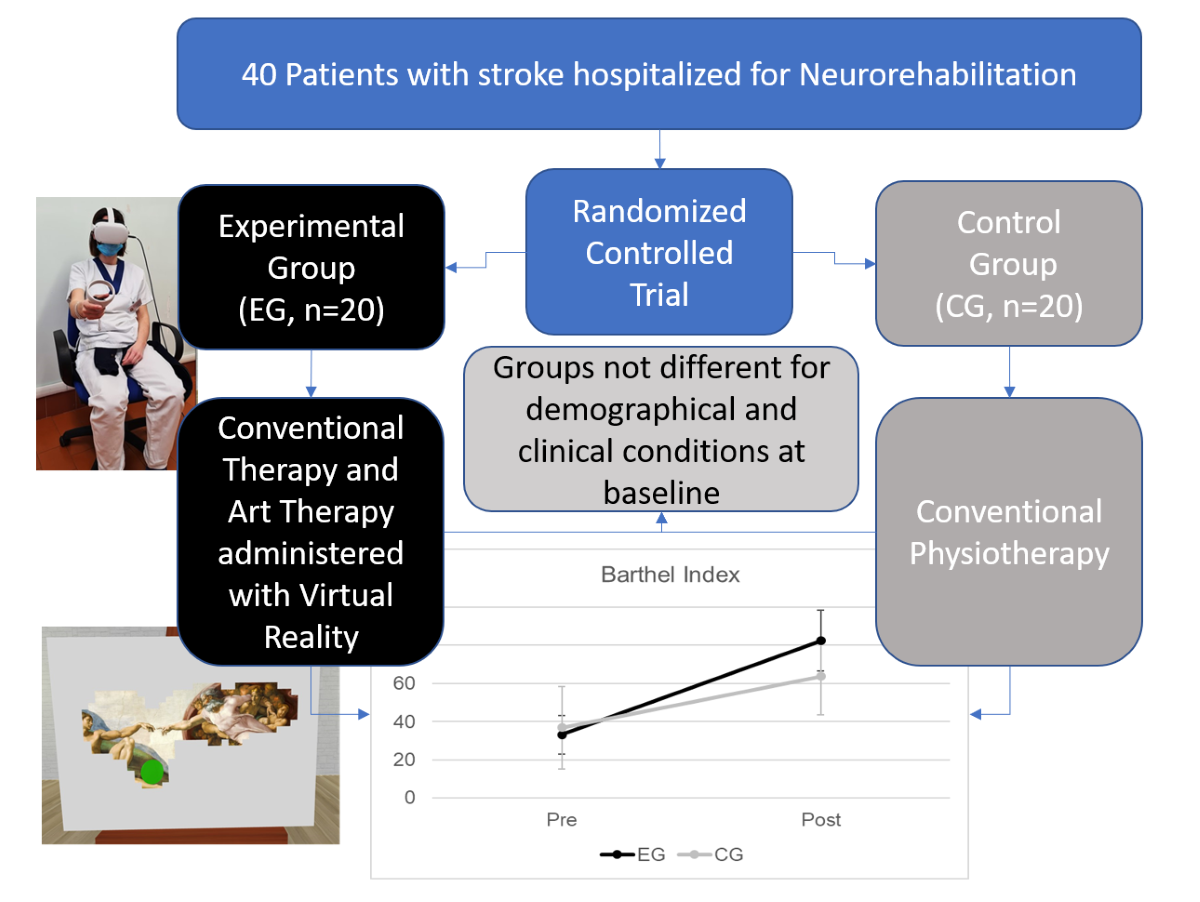
This study consists in a randomized controlled trial (RCT) that completed the enrollment of patients of our previous pilot study [
6]. Patients were randomly assigned to the experimental therapy group (EG) or conventional therapy group (CG) after their enrollment.
Conventional therapy consisted of 3 rehabilitative sessions per day, each one of 1 hour, 6 days per week, for one month (after which our protocol ended, but patients could continuous their therapies). During these 3 daily hours, rehabilitation could include not only physical therapy for upper and lower limbs, posture and balance, but also cognitive therapy, occupational therapy, speech therapy, specific therapy for swallowing, bowel, and bladder dysfunctions according to the clinical needs of the patient. The only difference for patients enrolled in experimental therapy group was that 3 weekly sessions of conventional upper limb physical therapy aiming at arm functional recovery were substituted by art therapy administered by virtual reality for a period of 4 weeks. The amount of time spent in rehabilitation and the typologies of other daily therapies remained analogous between the two groups.
During virtual art-therapy sessions, the patients comfortably sat on a chair when wearing an Head Mounted Display (Oculus Quest 2, Meta) and took into his/her paretic hand the controller which allowed to interact with the virtual stimuli. The virtual environment, designed by using 3ds MAX 2018 and implemented in Unity 2018 game engine software with customized C# scripts, consisted of a room having, in the middle, a white canvas on an easel. The dimensions of the virtual area of the canvas were 40cmx60cm. The subject saw in the virtual environment a spherical brush at the same place of their real hand. Patients were previously informed that the brush can color the canvas when put in contact with it, forming a painting. The illusion to paint an artwork was given thanks to a series of white thin virtual panels (pixels) placed in front of the canvas which occluded the visibility of an underlying paintings. The target pixels were deleted when the subject moved the virtual brush keeping it in touch with the canvas, allowing to see a part of the underlying painting (a masterpiece of history of the art)(see
Figure 1 for an example). Patients performed different trials during the time dedicated to the rehabilitative sessions, unveiling in each trial a different famous painting associated to concept of beauty in previous studies (masterpieces of Michelangelo, Leonardo, Renoir, van Gogh, Caravaggio, etc. were used, abstract art was not included) [
6,
10]. Each trial was performed under the supervision of a trained physiotherapist who monitored that the patient executes the correct movements and maintained the correct posture according to his/her rehabilitation needs. As for conventional therapy, the assistance of the therapist was allowed when needed and the patient could have a rest if needed.
2.3 Assessment
All patients were assessed at baseline (after enrollment) and 1 month later (at the end of this period of therapy) by a clinical assessor blind to the allocation group of the patient. The assessments were performed measuring the independence of the patient into the activities of daily living using the modified version of the Barthel Index (BI) [
11], the upper limb strength using the Manual Muscle Test (MMT) [
12] and the spasticity of the upper limb using the Ashworth scale (AS) [
13]. For the patients of ETG, the participation to each session of therapy was assessed using Pittsburgh Rehabilitation Participation Scale [
14,
15]. After each trial the perceived fatigue was assessed asking to the patient “how much tiring was this trial on a numeric rating scale ranging from 0 (no fatigue), to 10 (maximum possible fatigue)?” [
6].
2.4. Statistical Analysis
Data are reported in terms of mean and standard deviation for continuous measures, or percentage frequencies for nominal variables. The normality of data was tested using Kolgomorov-Smirnov analysis. For normally distributed variables Mixed Analysis of Variance was used to assess the effect of time (Pre vs. Post, within subject parameter), group (EG vs. CG) and their interaction. Effect size (ES) was computed using the partial eta-squared. For not-normally distributed variables non parametric Wilcoxon test for paired comparisons (pre vs. post) and Mann-Whitney u-test for unpaired comparisons between groups (EG vs. CG) were used. The efficacy of the interventions was computed in terms of effectiveness [
16,
17] computed as follows:
The PRPS- and fatigue-scores were averaged (firstly among trials for fatigue) among sessions for each patient and their correlations with other clinical variables were computed using the Spearman coefficient (R). For all the analysis, the level of statistical significance for rejecting the null hypothesis was set at 5%.
3. Results
3.1. Comparison of the Experimental and Control groups
Table 1 shows the demographical and clinical characteristics of the two groups at baseline. No significant differences were noted between groups, but for spasticity that was 0.9 points lower in EG than in CG.
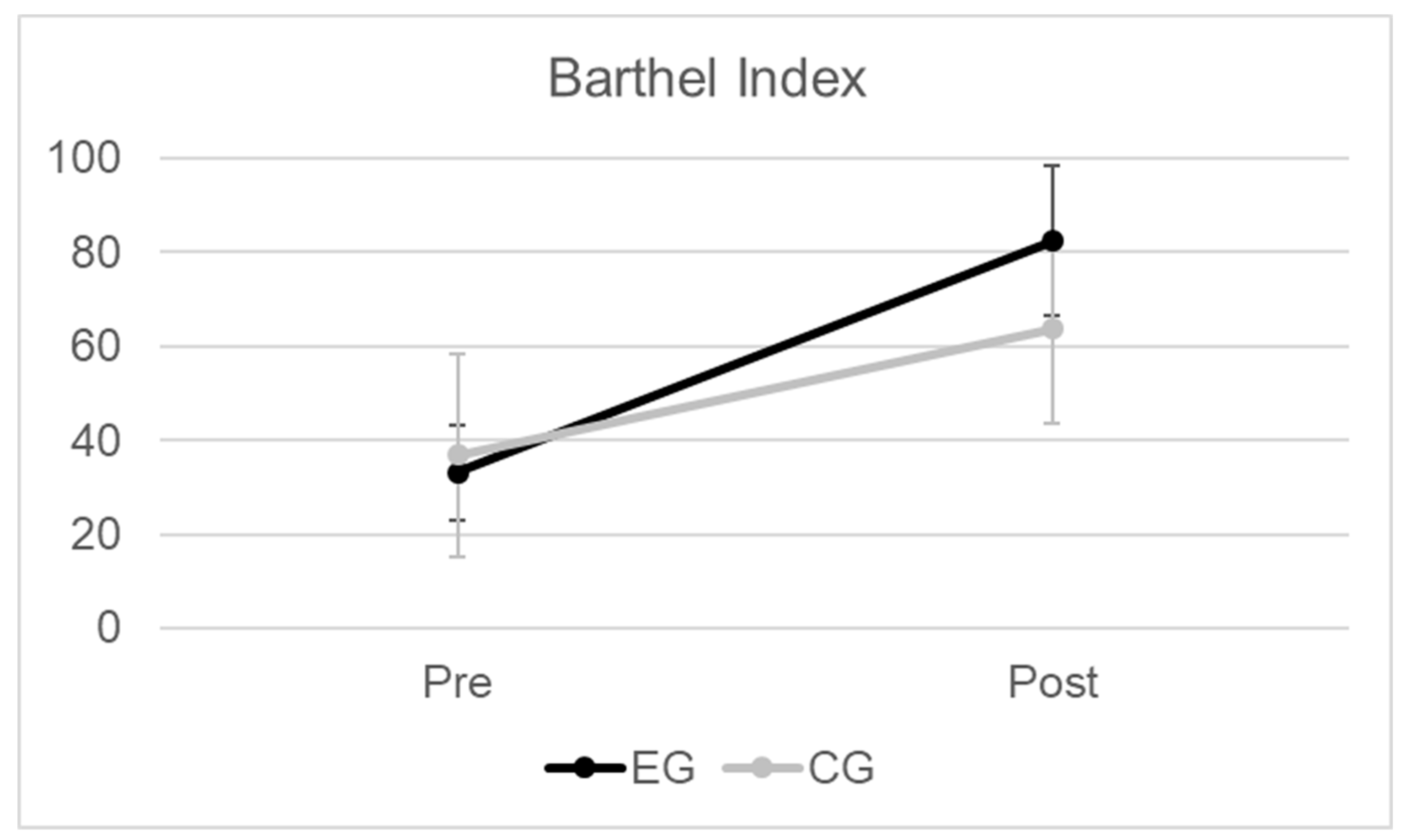
Figure 2 shows the primary outcome (Barthel Index) at baseline and after treatment. Mixed Analysis of Variance highlighted a significant effect of Time (pre vs. post: F(1,38)=129, p<0.001, ES=0.8), a significant interaction Time*Group (F(1,38)=9, p<0.01, ES=0.2), and a not significant effect of group (EG vs. CG: F(1,38)=4, p=0.07, ES=0.1). Non parametric test confirmed the significant differences of BI-score post treatmnt (p=0.001).
The Effectiveness in terms of BI-score was 75±21% in EG and 39±29% in CG (p<0.001).
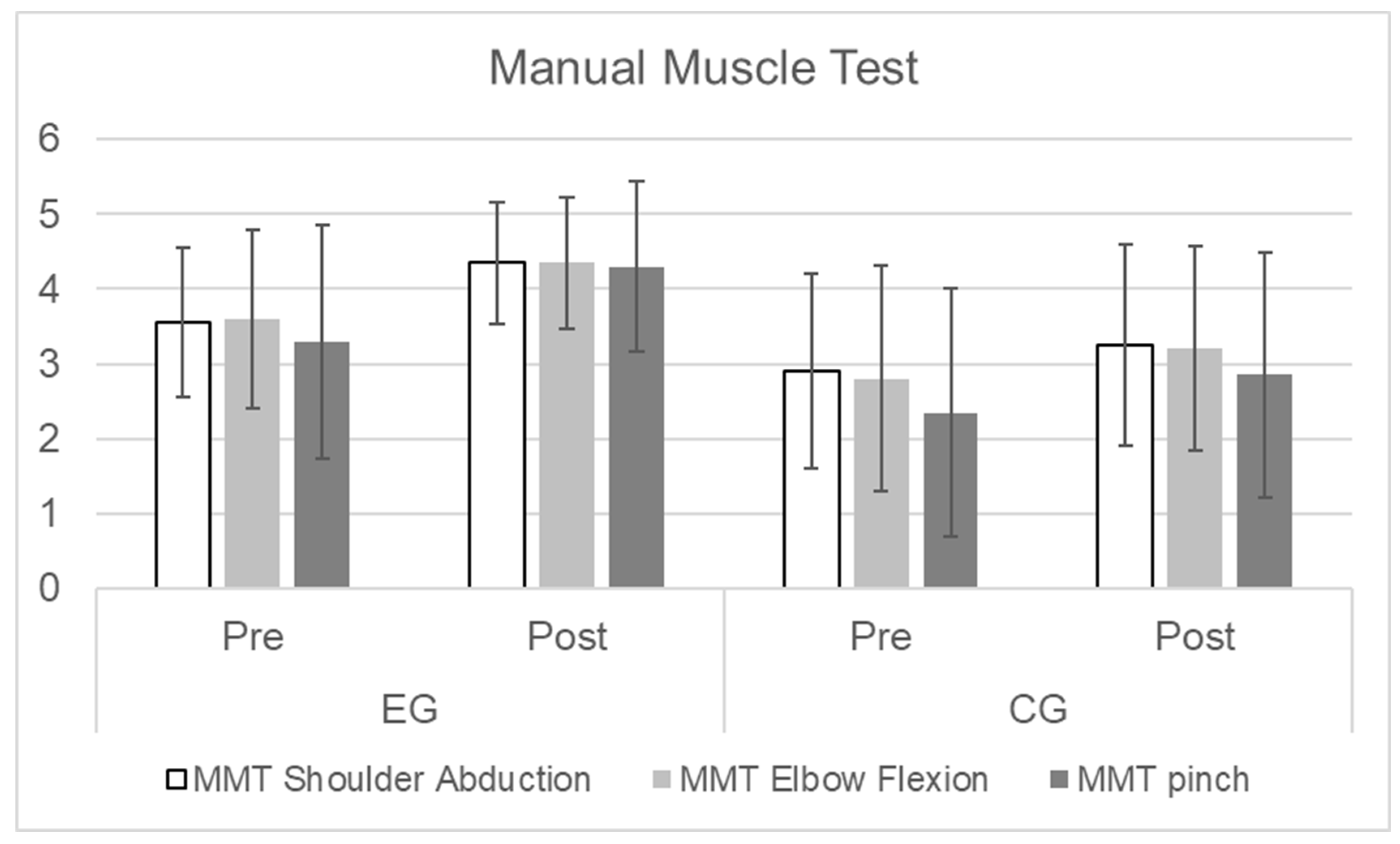
After treatment, also the scores of MMT (
Figure 3) were significant higher (u-test) in EG than in CG for shoulder abduction (p<0.01), elbow flexion (p<0.01) and pinch (p<0.001). The Ashworth scale showed a lower spasticity in EG than in CG (p<0.01).
3.2. Effects of Participation, Motivation and Fatigue on the Experimental Group
The mean values of participation was PRPS=5.5±0.5, of fatigue was 2.2±2.0, of patient’s satisfaction 9.2±0.9, or the therapist’s perceived utility 9.7±0.4.
Significant correlation was found between Effectiveness in terms of BI and participation measured with PRPS averaged among sessions (R=0.45, p≤0.05). Participation was also found significantly correlated with the utility of VR therapy perceived by the therapist (R=0.47) and with the level of satisfaction reported by each patient (R=0.51). Finally, utility perceived by therapist and satisfaction reported by patient were each other significantly correlated (R=0.50). Fatigue negatively but not significantly correlated with Effectiveness, participation, patient’s satisfaction and therapist’s utility perception.
4. Discussion
In recent years, there is a growing body of literature about the advancements of virtual reality and its use in different fields from entertainment to scientific research, from education to rehabilitation, including both physiotherapy and psychotherapy [
18]. However little attention has been given to the potential of virtual reality for art therapy.
Our previous pilot study [
9] was conducted on 20 patients, ten per group, showing a significantly higher improvement in terms of Barthel Index score and pinch strength in patients treated with the adjunction of virtual art therapy with respect to those who received additional conventional therapy. Neither the changes in MMT total score nor in the Asworth spasticity score achieved the significant threshold. According to the sample size calculation already reported in that paper, we increased our samples by including 20 patients per group. As hypothesized, the improvements in subscores of MMT and Ashworth scores resulted statistically significant. It should be noted a slight but significant difference in terms of spasticity in favor of EG at baseline (0.9 point less on average) with respect to CG. In general, EG showed a slight higher upper limb functioning than CG, but also a slight lower independency in the activities of daily living (4 points less on BI-score).
The art-therapy administered by virtual reality resulted more effective than conventional treatment, confirming the first hypothesis of this study.
The analysis conducted within the EG showed a significant correlation between the effectiveness of treatment with the participation of the patient assessed by the therapist using the PRPS. In addition, the utility perceived by the therapist and the level of satisfaction perceived by the patient were significantly correlated with the assessed effectiveness on BI-score.
It is known that fatigue and exertion can be reduced during physiotherapy by listening music [
19], that could also improve muscle activity and motor movements [
20]: our previous studies on Michelangelo effect extend to paintings the arts that could have these benefits on rehabilitation. In the present study, fatigue did not correlate with the efficacy of the intervention, but it should be noted that the therapists, during virtual art therapy (as well as during conventional therapy), adapted the level of difficulty of the exercises to the abilities of the patient. A limit of our study was that patients’ fatigue, participation and satisfaction were not assessed in the CG, but only in EG, not allowing comparisons between groups. Another limit is to have not assessed some other important psychological aspects that may affect rehabilitation. For example, it has been reported that participation in arts activities can reduce depression and improve quality of life, self-efficacy and compliance to treatment in patients with stroke [
21,
22]. Virtual Reality can be combined with art-therapy reducing anxiety and social difficulties especially in adolescents, because they are “digital natives” [
23], but the growing diffusion of digital technologies is increasing the compliance to these approaches also in elderly patients [
24].
According to the recent dual-task approach of rehabilitation, that combines motor and cognitive therapies, it could be important to analyze the impact of art-therapy also on cognitive domains. There are promising results about the exploitation of Michelangelo effect on memory rehabilitation [
25] and more in general on the use of digital technologies, such as virtual reality, and complementary medicine, such as visual art therapy [
25], for the recovery of cognitive functions [
26]. This approach could also be combined with telerehabilitation [
27] for a continuous care of patients with stroke also during chronic phase.
Finally, the fast diffusion of artificial intelligence (AI) may boost the use of digital technologies combined with art-therapies thanks to the easy-to-use generative tools of AI. It has been reported that AI chatbot interactions and AI-generated artworks may facilitate discussions about emotions, encourage self-expression through art creation, and provide cognitive-behavioral therapeutic advice in both verbal and visual ways [
28]. Moreover, AI con be further implemented in our virtual scenario for adapting the level of difficulty for each patients and analyze kinematics data in real-time.
The present study demonstrated that art-therapy combined with virtual reality, capitalizing on the Michelangelo effect in neurorehabilitation, may be an effective approach to enhancing independence in activities of daily living and upper limb muscle strength among stroke patients. The more is the participation of patient to the therapy, the more is the obtained benefit. Both patient and therapist resulted satisfied by this type of intervention. Further studies should include the assessment and treatment of cognitive domains, for which art-therapy showed to be effective [
29,
30], and it could be empowered by new technologies such as virtual reality and artificial intelligence.
Author Contributions
Conceptualization, M.I. and G.T.; methodology, M.I. and A.F.; software, G.T.; validation, R.D.G. and G.A.; formal analysis, M.I.; resources, M.I. and A.F.; data curation, T.M.; patients enrollment, assessment and treatment, F.A., F.G., C.R.; writing—original draft preparation, M.I.; writing—review and editing, M.I., G.T., R.D.G., A.F. G.A.; supervision, M.I.; project administration, M.I.; funding acquisition, M.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Sapienza University of Rome, grant number RM122181675BD4-FF, grant name: Project Michelangelo.
Institutional Review Board Statement
Local Independent Ethical Committee approved this study (approval code: CE/PROG.795, date of approval 2 December 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- De Pasquale, P.; Bonanno, M.; Mojdehdehbaher, S.; Quartarone, A.; Calabrò, R. S. The Use of Head-Mounted Display Systems for Upper Limb Kinematic Analysis in Post-Stroke Patients: A Perspective Review on Benefits, Challenges and Other Solutions. Bioengineering (Basel, Switzerland) 2024, 11(6), p. 538. [CrossRef]
- Laver, K.; George, S.; Thomas, S.; Deutsch, J. E.; Crotty, M. Cochrane review: Virtual reality for stroke rehabilitation. European journal of physical and rehabilitation medicine 2012, 48(3), pp. 523–530.
- Laver, K.; George, S.; Thomas, S.; Deutsch, J. E.; Crotty, M. Virtual reality for stroke rehabilitation: An abridged version of a Cochrane review. European journal of physical and rehabilitation medicine 2015, 51(4), pp. 497–506.
- Burdea, G.; Coiffet, P. Virtual reality technology. Presence: Teleoperators Virtual Environ 2003, 12(6), pp. 663e664.
- Tieri, G.; Morone, G.; Paolucci, S.; Iosa, M. Virtual reality in cognitive and motor rehabilitation: Facts, fiction and fallacies. Exp Rev Med Dev, 2018, 15(2), pp. 107-117.
- Iosa, M.; Aydin, M.; Candelise, C.; Coda, N.; Morone, G.; Antonucci, G.; Marinozzi, F.; Bini, F.; Paolucci, S.; Tieri, G. The Michelangelo Effect: Art Improves the Performance in a Virtual Reality Task Developed for Upper Limb Neurorehabilitation. Front Psychol. 2021, 11, p. 611956.
- Freedberg, D.; Gallese, V. Motion, emotion and empathy in esthetic experience. Trends Cogn Sci, 2007, 11(5), pp. 197-203.
- Fancourt, D.; Finn, S. What is the evidence on the role of the arts in improving health and well-being? A scoping review. Copenhagen: WHO Regional Office for Europe; 2019.
- De Giorgi, R.; Fortini, A.; Aghilarre, F.; Gentili, F.; Morone, G; Antonucci, G.; Vetrano, M.; Tieri, G.; Iosa, M. Virtual Art Therapy: Application of Michelangelo Effect to Neurorehabilitation of Patients with Stroke. Journal of clinical medicine 2023, 12(7), p. 2590. [CrossRef]
- Iosa, M.; Bini, F.; Marinozzi, F.; Antonucci, G.; Pascucci, S.; Baghini, G.; Guarino, V.; Paolucci, S.; Morone, G.; Tieri, G. Inside the Michelangelo effect: The role of art and aesthetic attractiveness on perceived fatigue and hand kinematics in virtual painting. Psych J, 2022, 11(5), pp. 748-754. [CrossRef]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. Journal of clinical epidemiology 1989, 42(8), pp. 703–709. [CrossRef]
- Bohannon R. W. Manual muscle test scores and dynamometer test scores of knee extension strength. Archives of physical medicine and rehabilitation 1986, 67(6), pp. 390–392.
- Ashworth B. Preliminary trial of carisoprodol in multiple sclerosis. The Practitioner, 1964, 192, pp. 540–542.
- Lenze, E.J.; Munin, M.C.; Quear, T.; Dew, M.A.; Rogers, J.C.; Begley, A.E.; Reynolds, C.F. The Pittsburgh Rehabilitation Participation Scale: Reliability and validity of a clinician-rated measure of participation in acute rehabilitation. Arch. Phys. Med Rehabil, 2004, 85, pp. 380–384. [CrossRef]
- Iosa, M.; Galeoto, G.; De Bartolo, D.; Russo, V.; Ruotolo, I.; Spitoni, G.F.; Ciancarelli, I.; Tramontano, M.; Antonucci, G.; Paolucci, S.; Morone, G. Italian Version of the Pittsburgh Rehabilitation Participation Scale: Psychometric Analysis of Validity and Reliability. Brain Sci, 2021, 11(5), p. 626. [CrossRef]
- Vanclay, F. Functional outcome measures in stroke rehabilitation. Stroke, 1991, 22, pp. 105-108.
- Shah, S.; Vanclay, F.; Cooper, B. Efficiency, effectiveness and duration of stroke rehabilitation. Stroke, 1990, 21, pp. 241-246.
- Hacmun, I., Regev, D., & Salomon, R. (2018). The Principles of Art Therapy in Virtual Reality. Frontiers in psychology, 9, 2082. [CrossRef]
- Lim HA, Miller K, Fabian C. The effects of therapeutic instrumental music performance on endurance level, self-perceived fatigue level, and self-perceived exertion of inpatients in physical rehabilitation. J Music Ther. 2011;48(2):124–48. PMID: 21938889.
- Prahm C, Kayali F, Sturma A, Aszmann O. Playbionic: Game-based interventions to encourage patient engagement and performance in prosthetic motor rehabilitation. PM&R. 2018;10(11):1252–60. [CrossRef]
- Morris JH, Kelly C, Joice S, Kroll T, Mead G, Donnan P et al. Art participation for psychosocial wellbeing during stroke rehabilitation: A feasibility randomised controlled trial. Disabil Rehabil. 2019;41(1):9–18. [CrossRef]
- Kongkasuwan R, Voraakhom K, Pisolayabutra P, Maneechai P, Boonin J, Kuptniratsaikul V. Creative art therapy to enhance rehabilitation for stroke patients: A randomized controlled trial. Clin Rehabil. 2015;30(10):1016–23. [CrossRef]
- Shamri Zeevi L. (2021). Making Art Therapy Virtual: Integrating Virtual Reality Into Art Therapy With Adolescents. Frontiers in psychology, 12, 584943. [CrossRef]
- Oliva, A., Iosa, M., Antonucci, G., & De Bartolo, D. (2023). Are neuroaesthetic principles applied in art therapy protocols for neurorehabilitation? A systematic mini-review. Frontiers in psychology, 14, 1158304. [CrossRef]
- Salera, C., Capua, C., De Angelis, D., Coiro, P., Venturiero, V., Savo, A., Marinozzi, F., Bini, F., Paolucci, S., Antonucci, G., & Iosa, M. (2024). Michelangelo Effect in Cognitive Rehabilitation: Using Art in a Digital Visuospatial Memory Task. Brain sciences, 14(5), 479. [CrossRef]
- Li, B., & Shen, M. (2022). The Psychological Recovery of Patients in the Context of Virtual Reality Application by a Complementary Medicine Scheme Based on Visual Art. Evidence-based complementary and alternative medicine : eCAM, 2022, 7358597. [CrossRef]
- Cheng, C., Elamin, M. E., May, H., & Kennedy, M. (2023). Drawing on emotions: The evolving role of art therapy. Irish journal of psychological medicine, 40(3), 500–502. [CrossRef]
- Zubala, A., Kennell, N., & Hackett, S. (2021). Art Therapy in the Digital World: An Integrative Review of Current Practice and Future Directions. Frontiers in psychology, 12, 595536. [CrossRef]
- Eum, Y., & Yim, J. (2015). Literature and art therapy in post-stroke psychological disorders. The Tohoku journal of experimental medicine, 235(1), 17–23. [CrossRef]
- Alwledat, K., Al-Amer, R., Ali, A. M., Abuzied, Y., Adnan Khudeir, F., Alzahrani, N. S., Alshammari, S. R., AlBashtawy, M., Thananayagam, T., & Dehghan, M. (2023). Creative Art Therapy for Improving Depression, Anxiety, and Stress in Patients with Stroke: A Quasi-Interventional Study. SAGE open nursing, 9, 23779608231160473. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).