Submitted:
31 July 2024
Posted:
31 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Sample
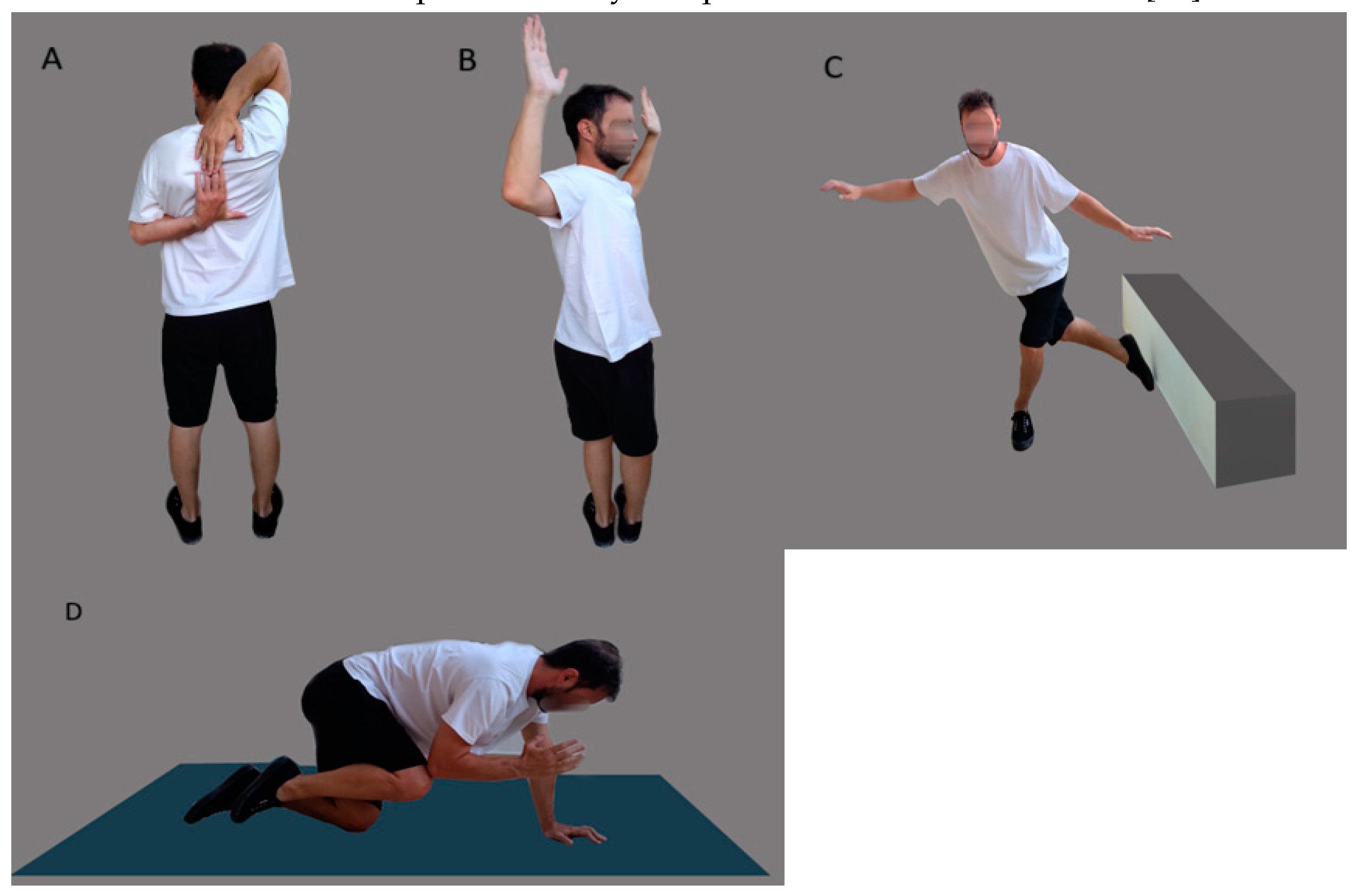
2.2. Modified ACS
2.3. Risk Factors
- True Positive (TP): This was recorded when a participant had at least one shoulder or thoracic mobility risk factor, which was correctly identified by a positive result in the ACS reciprocal shoulder mobility test on either side.
- True Negative (TN): This occurred when the participant passed all goniometric shoulder and thoracic range of motion (ROM) tests and received a negative result on the reciprocal shoulder mobility test for both sides.
- False Positive (FP): This was noted when no shoulder or thoracic risk factors were present, yet the participant tested positive on either side of the reciprocal shoulder mobility test.
- False Negative (FN): This was observed when a participant had at least one shoulder or thoracic risk factor but tested negative on the reciprocal shoulder mobility test for both sides.
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Key Findings
4.2. Sensitivity and Specificity
4.3. Positive and Negative Predictive Values
4.4. Likelihood Ratios and Odds Ratios
4.5. Implications for Screening and Prevention
4.6. Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lucas, J.; van Doorn, P.; Hegedus, E.; Lewis, J.; van der Windt, D. A systematic review of the global prevalence and incidence of shoulder pain. BMC Musculoskeletal Disorders 2022, 23, 1073. [Google Scholar] [CrossRef] [PubMed]
- Bilberg, R.; Nørgaard, B.; Overgaard, S.; Roessler, K.K. Mental health and quality of life in shoulder pain patients and hip pain patients assessed by patient reported outcome. International Journal of Orthopaedic and Trauma Nursing 2014, 18, 81–88. [Google Scholar] [CrossRef]
- Virta, L.; Joranger, P.; Brox, J.I.; Eriksson, R. Costs of shoulder pain and resource use in primary health care: a cost-of-illness study in Sweden. BMC musculoskeletal disorders 2012, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Liaghat, B.; Pedersen, J.R.; Husted, R.S.; Pedersen, L.L.; Thorborg, K.; Juhl, C.B. Diagnosis, prevention and treatment of common shoulder injuries in sport: grading the evidence - a statement paper commissioned by the Danish Society of Sports Physical Therapy (DSSF). Br J Sports Med 2023, 57, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulos, E.; Pamboris, G.M.; Papandreou, M. The Changing Landscape in Upper Limb Sports Rehabilitation and Injury Prevention. Sports 2023, 11, 80. [Google Scholar] [CrossRef] [PubMed]
- Forthomme, B.; Wieczorek, V.; Frisch, A.; Crielaard, J.-M.; Croisier, J.-L. Shoulder pain among high-level volleyball players and preseason features. Medicine and science in sports and exercise 2013, 45, 1852–1860. [Google Scholar] [CrossRef]
- Andersson, S.H.; Bahr, R.; Clarsen, B.; Myklebust, G. Preventing overuse shoulder injuries among throwing athletes: a cluster-randomised controlled trial in 660 elite handball players. British journal of sports medicine 2017, 51, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Paraskevopoulos, E.; Kottaridis, F.-M.; Moutzouri, M.; Koumantakis, G.A.; Antonakis-Karamintzas, D.; Tsolakis, C.; Koulouvaris, P.; Christakou, A.; Papandreou, M. Preliminary Insights into the Diagnostic Accuracy of the Modified Arm Care Screen Test for Overhead Athletes: An On-Field Tool for Injury Prevention. Healthcare 2023, 11, 3046. [Google Scholar] [CrossRef] [PubMed]
- Feijen, S.; Struyf, T.; Kuppens, K.; Tate, A.; Struyf, F. Prediction of Shoulder Pain in Youth Competitive Swimmers: The Development and Internal Validation of a Prognostic Prediction Model. The American Journal of Sports Medicine 2021, 49, 154–161. [Google Scholar] [CrossRef]
- Matsel, K.A.; Hoch, M.C.; Butler, R.J.; Westgate, P.M.; Malone, T.R.; Uhl, T.L. A Field-expedient Arm Care Screening Tool Can Identify Musculoskeletal Risk Factors in Baseball Players. Sports Health 2023, 15, 736–745. [Google Scholar] [CrossRef]
- Torabi, T.P.; Bencke, J.; van den Tillaar, R. The Closed Kinetic Chain Upper Extremity Stability Test (CKCUEST) Performance in Elite Team Handball Players Playing with Shoulder Pain, Previous Pain, or No Pain. Int J Sports Phys Ther 2024, 19, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Matsel, K.A.; Brown, S.N.; Hoch, M.C.; Butler, R.J.; Westgate, P.M.; Malone, T.R.; Uhl, T.L. The intra-and inter-rater reliability of an arm care screening tool in high school baseball coaches. International Journal of Sports Physical Therapy 2021, 16, 1532. [Google Scholar] [CrossRef]
- Plisky, P.J.; Gorman, P.P.; Butler, R.J.; Kiesel, K.B.; Underwood, F.B.; Elkins, B. The reliability of an instrumented device for measuring components of the star excursion balance test. North American journal of sports physical therapy: NAJSPT 2009, 4, 92. [Google Scholar] [PubMed]
- Matsel, K.A.; Hoch, M.C.; Butler, R.J.; Westgate, P.M.; Malone, T.R.; Uhl, T.L. A Field-expedient Arm Care Screening Tool Can Identify Musculoskeletal Risk Factors in Baseball Players. Sports Health 2022, 19417381221125465. [Google Scholar] [CrossRef]
- Barfield, J.W.; Bordelon, N.M.; Wasserberger, K.W.; Oliver, G.D. Preliminary Analysis of Closed Kinetic Chain Upper Extremity Stability Test Differences Between Healthy and Previously Injured/In-Pain Baseball Pitchers. Sports Health 2023, 15, 290–294. [Google Scholar] [CrossRef]
- Goldbeck, T.G.; Davies, G.J. Test-retest reliability of the closed kinetic chain upper extremity stability test: a clinical field test. Journal of Sport Rehabilitation 2000, 9, 35–45. [Google Scholar] [CrossRef]
- Pontillo, M.; Spinelli, B.A.; Sennett, B.J. Prediction of In-Season Shoulder Injury From Preseason Testing in Division I Collegiate Football Players. Sports Health 2014, 6, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Ellenbecker, T.; Manske, R.; Davies, G. Closed kinetic chain testing techniques of the upper extremities. Orthopaedic Physical Therapy Clinics of North America 2000, 9, 219–230. [Google Scholar]
- Bullock, G.S.; Faherty, M.S.; Ledbetter, L.; Thigpen, C.A.; Sell, T.C. Shoulder Range of Motion and Baseball Arm Injuries: A Systematic Review and Meta-Analysis. Journal of athletic training 2018, 53, 1190–1199. [Google Scholar] [CrossRef]
- Shanley, E.; Kissenberth, M.J.; Thigpen, C.A.; Bailey, L.B.; Hawkins, R.J.; Michener, L.A.; Tokish, J.M.; Rauh, M.J. Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. Journal of shoulder and elbow surgery 2015, 24, 1005–1013. [Google Scholar] [CrossRef]
- Shitara, H.; Kobayashi, T.; Yamamoto, A.; Shimoyama, D.; Ichinose, T.; Tajika, T.; Osawa, T.; Iizuka, H.; Takagishi, K. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 2017, 25, 3303–3310. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D., 2nd; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am J Sports Med 2011, 39, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Aune, K.T.; Porterfield, R.A.; Harker, P.; Evans, T.J.; Andrews, J.R. Deficits in glenohumeral passive range of motion increase risk of shoulder injury in professional baseball pitchers: a prospective study. The American journal of sports medicine 2015, 43, 2379–2385. [Google Scholar] [CrossRef] [PubMed]
- Hiramoto, M.; Morihara, T.; Kida, Y.; Matsui, T.; Azuma, Y.; Seo, K.; Miyazaki, T.; Watanabe, Y.; Kai, Y.; Yamada, Y.; et al. Hip, Trunk, and Shoulder Rotational Range of Motion in Healthy Japanese Youth and High-school Baseball Pitchers. Progress in rehabilitation medicine 2019, 4, 20190009. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Imai, K.; Liu, X.; Chen, Z.; Watanabe, E. Assessing the Association of Shoulder Pain Risk with Physical Fitness in Badminton Players at National Tournament Level. Asian J Sports Med 2022, 13, e129916. [Google Scholar] [CrossRef]
- Saito, M.; Kenmoku, T.; Kameyama, K.; Murata, R.; Yusa, T.; Ochiai, N.; Kijima, T.; Takahira, N.; Fukushima, K.; Ishige, N. Relationship between tightness of the hip joint and elbow pain in adolescent baseball players. Orthopaedic journal of sports medicine 2014, 2, 2325967114532424. [Google Scholar] [CrossRef] [PubMed]
- Sekiguchi, T.; Hagiwara, Y.; Yabe, Y.; Tsuchiya, M.; Itaya, N.; Yoshida, S.; Yano, T.; Sogi, Y.; Suzuki, K.; Itoi, E. Restriction in the hip internal rotation of the stride leg is associated with elbow and shoulder pain in elite young baseball players. Journal of shoulder and elbow surgery 2020, 29, 139–145. [Google Scholar] [CrossRef]
- Hamano, N.; Shitara, H.; Tajika, T.; Ichinose, T.; Sasaki, T.; Kamiyama, M.; Miyamoto, R.; Kuboi, T.; Endo, F.; Yamamoto, A.; et al. Relationship between tightness of the hip joint and shoulder/elbow injury in high school baseball pitchers: a prospective study. Scientific reports 2020, 10, 19979. [Google Scholar] [CrossRef]
- Ryman Augustsson, S.; Ageberg, E. Weaker lower extremity muscle strength predicts traumatic knee injury in youth female but not male athletes. BMJ Open Sport Exerc Med 2017, 3, e000222. [Google Scholar] [CrossRef]
- de Noronha, M.; França, L.C.; Haupenthal, A.; Nunes, G. Intrinsic predictive factors for ankle sprain in active university students: a prospective study. Scandinavian journal of medicine & science in sports 2013, 23, 541–547. [Google Scholar]
- Kim, H.-Y. Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restorative dentistry & endodontics 2017, 42, 152–155. [Google Scholar]
- Farrington, D.P.; Loeber, R. Relative improvement over chance (RIOC) and phi as measures of predictive efficiency and strength of association in 2× 2 tables. Journal of Quantitative Criminology 1989, 5, 201–213. [Google Scholar] [CrossRef]
- Trevethan, R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Frontiers in public health 2017, 5, 307. [Google Scholar] [CrossRef] [PubMed]
- Shreffler, J.; Huecker, M.R. Diagnostic testing accuracy: Sensitivity, specificity, predictive values and likelihood ratios. 2020.
- Dhaliwal, G.; Saint, S.; Drazen, J.; Solomon, C. New England Journal of Medicine: Clinical Problem-Solving. 2006.
- Degens, H.; Stasiulis, A.; Skurvydas, A.; Statkeviciene, B.; Venckunas, T. Physiological comparison between non-athletes, endurance, power and team athletes. European journal of applied physiology 2019, 119, 1377–1386. [Google Scholar] [CrossRef] [PubMed]
- Alberg, A.J.; Park, J.W.; Hager, B.W.; Brock, M.V.; Diener-West, M. The use of “overall accuracy” to evaluate the validity of screening or diagnostic tests. J Gen Intern Med 2004, 19, 460–465. [Google Scholar] [CrossRef]
- Schwank, A.; Blazey, P.; Asker, M.; Møller, M.; Hägglund, M.; Gard, S.; Skazalski, C.; Haugsbø Andersson, S.; Horsley, I.; Whiteley, R.; et al. 2022 Bern Consensus Statement on Shoulder Injury Prevention, Rehabilitation, and Return to Sport for Athletes at All Participation Levels. Journal of Orthopaedic & Sports Physical Therapy 2021, 52, 11–28. [Google Scholar] [CrossRef]
| ACS | Risk factors |
|---|---|
| Reciprocal shoulder mobility |
The dominant shoulder exhibited less than 45° of internal rotation passive range of motion at 90° of abduction. [19]. Glenohumeral Internal Rotation Deficit (GIRD) ≥20°: The difference in internal rotation between the non-dominant shoulder and the dominant shoulder was 20° or greater.[20,21]. Shoulder total range of motion deficit (TROM) ≥10°: The total range of motion difference between the dominant and non-dominant shoulders was 10° or greater[19,22]. Shoulder flexion deficit ≥5°: The difference between the dominant shoulder’s flexion PROM and the non-dominant shoulder’s flexion PROM was 5° or greater [23]. Thoracic spine rotation PROM <50°: Either the dominant or non-dominant thoracic rotation PROM, measured in a quadruped position, was less than 50°.[24,25]. |
| Total Body Rotation | Limited hip internal rotation (IR) passive range of motion (PROM) ≤36°: Either the stance or stride hip showed IR PROM of 36° or less when the participant was in the prone position[26,27]. Restricted hip external rotation (ER) passive range of motion (PROM) ≤40°: Either the stance or stride hip exhibited ER PROM of 40° or less with the participant in the prone position[28]. |
| Lower Body Diagonal Reach | Normalized Y Balance Test-Posterior-Lateral (YBT-PL) reach distance: The YBT-PL reach distance was assessed for both the stance and stride legs using the YBT. To adjust for the potential impact of player height on reach distance, the YBT-PL reach was normalized by dividing it by the length of the participant’s dominant lower limb and then multiplying by 100. The average normalized YBT-PL reach distances were calculated for each age group. Reach distances falling below the lower third quartile for the respective age categories—youth (<92 cm), high school (<95 cm), and college (<98 cm)—were identified as risk factors [29]. YBT-PL reach asymmetry: The absolute difference between the YBT-PL reach distances of the stance leg and the stride leg was 5.5 cm or greater [30]. |
| Rotary Stability | Closed Kinetic Chain Upper Extremity Stability test (CKCUES): Subjects who scored below the reference values (18.5 touches for males and 20.5 touches for females from a modified position) were considered to have an increased risk factor [17,18]. |
| Mean Age | 22.7±3.1 | |
| Gender (Male-Female) | 14 – 16 | |
| Height (cm) | 172.7±10.4 | |
| Weight (kg) | 68.4±12.8 | |
| BMI | 23 | |
| Limb dominance (L: Left, R: Right) |
2 L – 28 R |
| Reciprocal Shoulder Mobility | 90/90 Total Body Rotation | Lower Body Diagonal Reach | Core Stability | |||||||||||||
| ≥1 Risk Factor | ≥1 Risk Factor | ≥1 Risk Factor | ≥1 Risk Factor | |||||||||||||
| Shoulder mobility | Yes | No | Total Body Rotation | Yes | No | Diagonal Reach | Yes | No | Rotary Stability | Yes | No | |||||
| Fail | 10 | 2 | Fail | 0 | 3 | Fail | 6 | 0 | Fail | 4 | 0 | |||||
| Pass | 12 | 5 | Pass | 13 | 14 | Pass | 14 | 9 | Pass | 24 | 1 | |||||
| Chi-square for association | p=0.481, Phi=0.12 | p=0.626, Phi=0.089 | p=0.053, Phi=0.354 | p=0.464, Phi=0.134 | ||||||||||||
| ACS Component | Reciprocal shoulder mobility | Total Body Rotation | Lower Body Diagonal Reach | Rotary Stability | ||||
| Statistic | Value | 95% CI | Value | 95% CI | Value | 95% CI | Value | 95% CI |
| Sensitivity | 47,62% | 25,71%-70,22% | 0,00% | 0,00%- 24,71% | 31,58% | 12,58%-56,55% | 14,29% | 4,03%-32,67% |
| Specificity | 55,56% | 21,20%-86,30% | 82,35% | 56,57%-96,20% | 90,91% | 58,72%-99,77% | 100,00% | 15,81%-100,00% |
| Positive Likelihood Ratio | 1,07 | 0,45-2,52 | 0,00 | 3,47 | 0,48-25,22 | |||
| Negative Likelihood Ratio | 0,94 | 0,46-1,92 | 1,21 | 0,97-1,51 | 0,75 | 0,53-1,08 | 0,86 | 0,74-1,00 |
| Disease prevalence | 30% | 30% | 30% | 30% | ||||
| Positive Predictive Value | 31,47% | 16,31%-51,97% | 0,00% | 59,82% | 17,01%-91,53% | 100,00% | 39,76%-100,00% | |
| Negative Predictive Value | 71,22% | 54,82%-83,46% | 65,77% | 60,66%-70,54% | 75,61% | 68,42%-81,60% | 73,13% | 70,06%-76,00% |
| Accuracy | 53,17% | 34,18%-71,52% | 57,65% | 38,35%-75,37% | 73,11% | 53,87%-87,56% | 74,29% | 55,13%-88,40% |
| Odds ratio | 2.08 | 0.33 to 13.14 | 0.15 | 0.007 to 3.254 | 8.51 | 0.428 to 169.46 | 0.55 | 0.019 to 15.78 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





