Submitted:
20 August 2024
Posted:
21 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Approaches and Methods
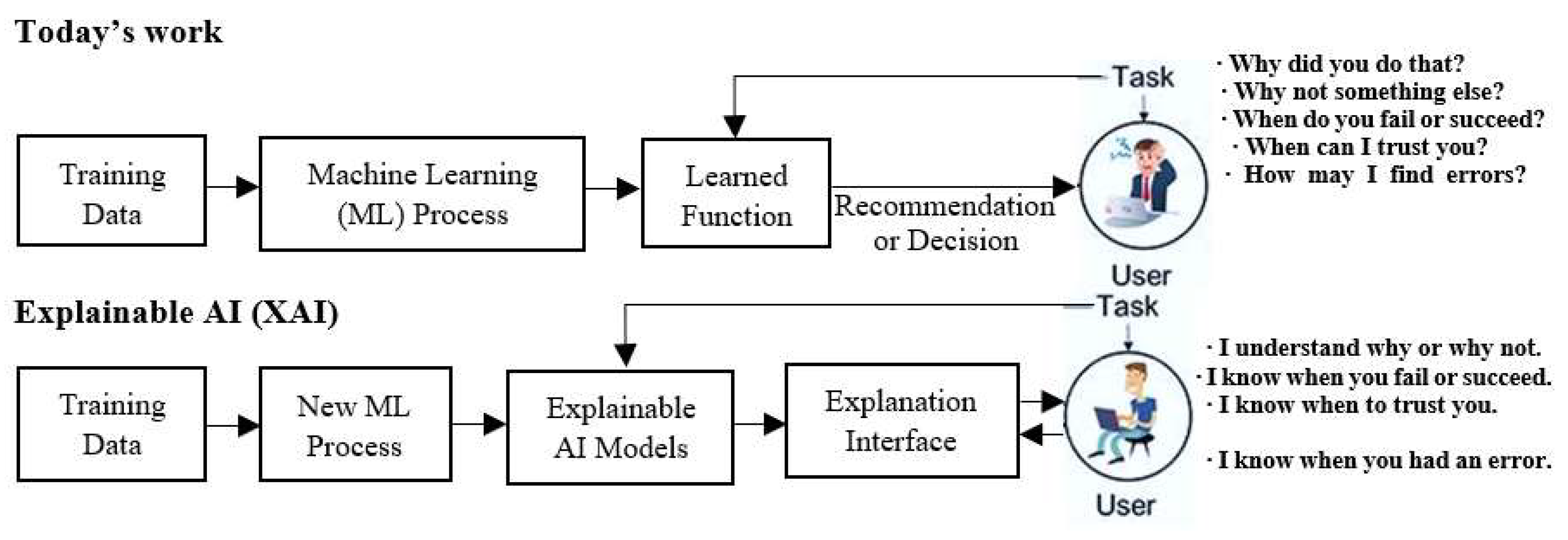
2.1. Fundamental Concepts and Workflow of Explainable AI for Clinical Use
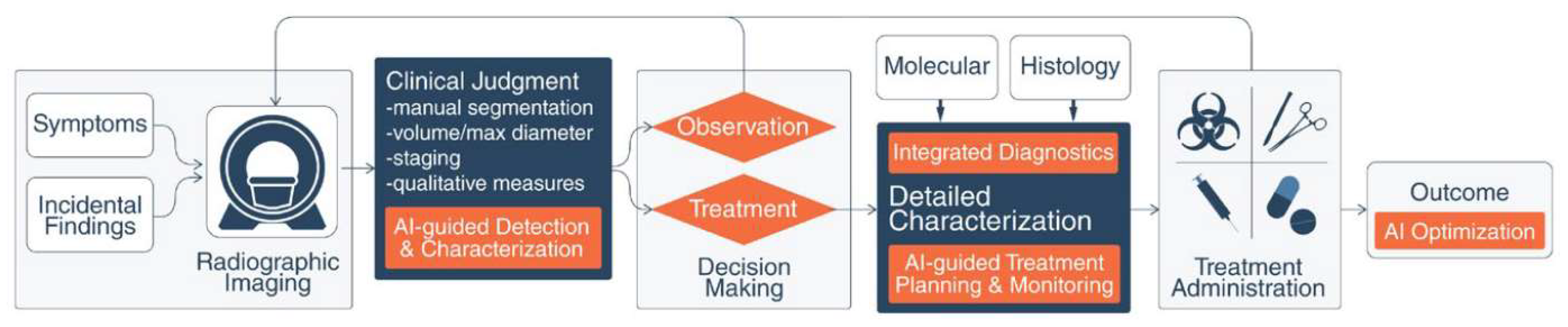
2.2. Preliminary Review of Explainable AI on Diagnosis and Treatment for Gynecological Oncology
3. Recent Advances and Challenging Issues
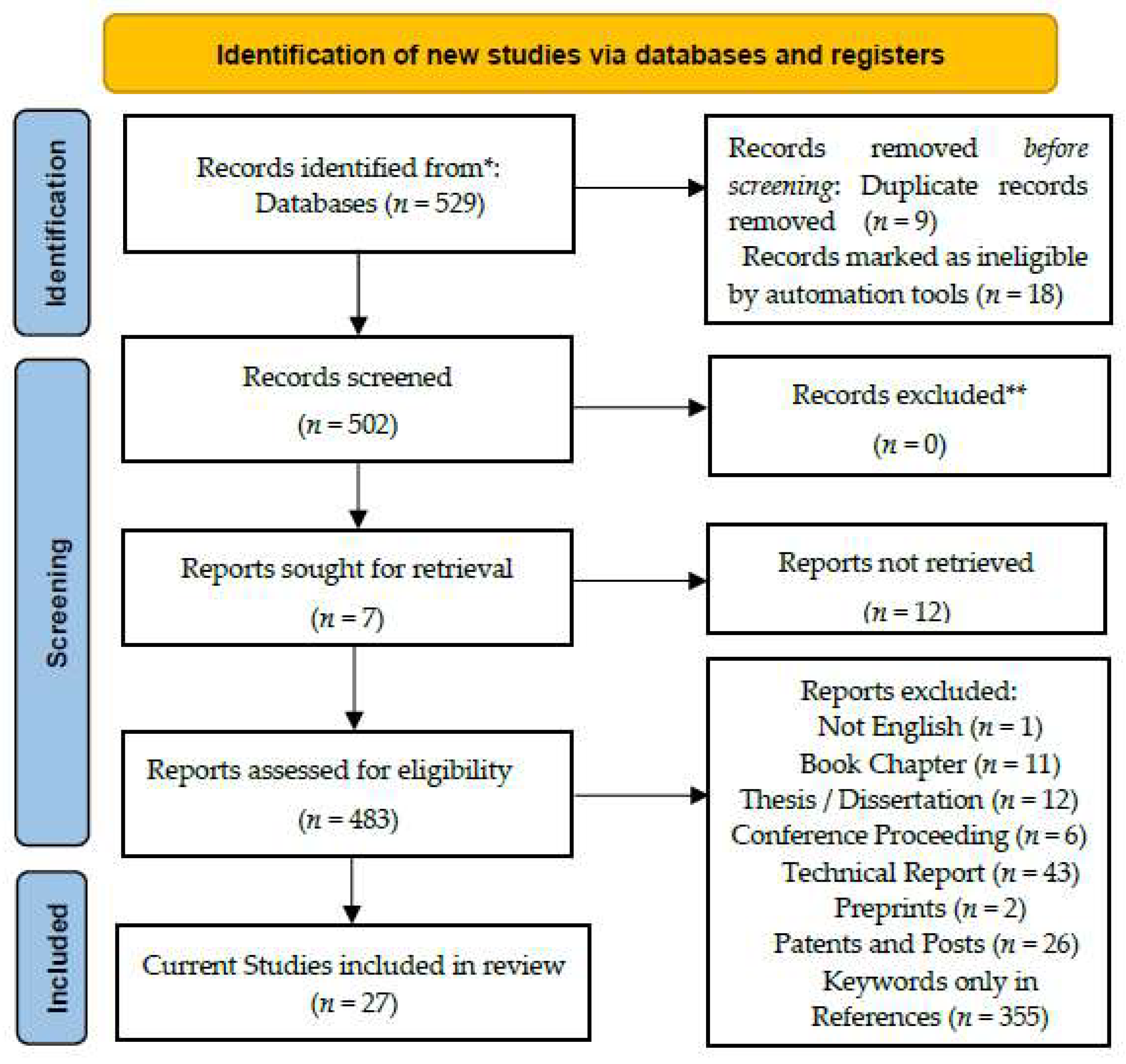
3.1. Application of PRISMA 2020 on Systematic Review of the Proposed Study
3.2. Main Set of the Current Schemes on Applying Explainable AI for Gynecological Oncology
4. Discussion
4.1. Selected Evaluations on Explainable AI-Guided Precise Medicine for Gynecological Tumors
4.2. Brief Summary on Contributions and Limitations of Our Study
5. Conclusions and Future Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duan, R.-F.; Zhang, H.-P.; Yu, J.; Deng, S.-S.; Yang, H.-J.; Zheng, Y.-T.; Huang, Y.-C.; Zhao, F.-H., Yang, H.-Y. Temporal trends and projections of gynecological cancers in China, 2007-2030. BMC Women’s Health. 2023, 23, 346, 1-9. [CrossRef]
- Dahad, N. AI may recognize real intelligence only if understanding the operating style of brains. EE Times China. 2019, 8.
- Bi, W.-Y.; Hosny, A.; Schabath, M. B.; Giger, M. L.; Birkbak, N. J.; Mehrtash, A.; Allison, T.; Arnaout, O.; Abbosh, C.; Dunn, I. F.; Mak, R. H.; Tamimi, R. M.; Tempany, C. M.; Swanton, C.; Hoffmann, U.; Schwartz, L. H.; Gillies, R. J.; Huang, R. Y.; Aerts, H. J. W. L. Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J. Clin. 2019, 0, 1-31. [CrossRef]
- Tang, L.-L; Li, L. Research and applications of big data and artificial intelligence on gynecological malignant tumors. Chin. J. Prac. Gynecol. Obstet. 2019, 35, 720-723.
- Chango, X.; Flor-Unda, O.; Gil-Jiménez, P.; Gómez-Moreno, H. Technology in forensic sciences: innovation and precision. Technologies 2024, 12, 120. [CrossRef]
- Kyrgiou, M.; Pouliakis, A.; Panayiotides, J. G. Personalised management of women with cervical abnormalities using a clinical decision support scoring system. Gynecol. Oncol. 2016, 141, 29-35. [CrossRef]
- Pergialiotis, V.; Pouliakis, A.; Parthenis, C.; Damaskou, V.; Chrelias, C.; Papantoniou, N.; Panayiotides, I. The utility of artificial neural networks and classification and regression trees for the prediction of endometrial cancer in postmenopausal women. Public Health 2018, 164, 1-6. [CrossRef]
- Bora, K.; Chowdhury, M.; Mahanta, L.B.; Kundu, M. K.; Das, A. K. Automated classification of Pap smear images to detect cervical dysplasia. Comput. Methods Prog. Biomed. 2017, 138, 31-47. [CrossRef]
- Patel, T. A.; Puppala, M.; Ogunti, R. O.,Ensor, J. E.; He, T.-C.; Shewale, J. B.; Ankerst, D. P.; Kaklamani, V. G.; Rodriguez, A. A.; Wong, S. T. C.; Chang, J. C. Correlating mammographic and pathologic findings in clinical decision support using natural language processing and data mining methods. Cancers 2017, 123, 114-121. [CrossRef]
- Sato, M.; Horie, K.; Hara, A.; Miyamoto, Y.; Kurihara, K.; Tomio, K.; Yokota, H. Application of deep learning to the classification of images from colposcopy. Oncol. Lett. 2018, 15, 3518-3523. [CrossRef]
- Aramendia-Vidaurreta, V.; Cabeza, R.; Villanueva, A.; Navallas, J.; Alcázar, J. L. Ultrasound image discrimination between benign and malignant adnexal masses based on a neural network approach. Ultrasound Med. Biol. 2016, 42, 742-752. [CrossRef]
- Vu, T. H.; Mousavi, H. S.; Monga, V.; Rao, G.; Rao, UK A. Histopathological image classification using discriminative feature-oriented dictionary learning. IEEE Trans. Med. Imag. 2016, 35, 738-751. [CrossRef]
- Zhang, L.; Le, L.; Nogues, I.; Summers, R. M.; Liu, S.-X.; Yao, J.-H. DeepPap: deep convolutional networks for cervical cell classification. IEEE J. Biomed. Health Inform. 2017, 21, 1633-1643. [CrossRef]
- Sornapudi, S.; Stanley, R. J.; Stoecker, W. V.; Almubarak, H.; Long, R.; Antani, S.; Thoma, G.; Zuna, R.; Shelliane R.; Frazier, S. R. Deep learning nuclei detection in digitized histology images by superpixels. J. Pathol. Inform. 2018, 9, 1-10. [CrossRef]
- Sinno, A.K.; Fader, A.N. Robotic-assisted surgery in gynecologic oncology. Fertil. Steril. 2014, 102, 922-932. [CrossRef]
- Aruni, G.; Amit, G.; Dasgupta, P. New surgical robots on the horizon and the potential role of artificial intelligence. Investig. Clin. Urol. 2018, 59, 221-222. [CrossRef]
- Moussa, H.G.; Husseini, G.A.; Abel-Jabbar, N.; Ahmed, S. Use of model predictive control and artificial neural networks to optimize the ultrasonic release of a model drug from liposomes. IEEE Trans. Nanobiosci. 2017, 16, 149-156. [CrossRef]
- Li, S.; Jiang, Q.; Liu, S.; Zhang, Y.-L.; Tian, Y.-H.; Song, C.; Wang, J.; Zou, Y.-G.; Anderson, G. A.; Han, J.-Y.; Chang, Y.; Liu, Y.; Zhang, C.; Chen, L.; Zhou, G.-B.; Nie, G.-J., Yan, H.; Ding, B.-Q.; Zhao, Y.-L. A DNA nanorobot functions as a cancer therapeutic in response to a molecular trigger in vivo. Nat. Biotechnol. 2018, 36, 258-264. [CrossRef]
- Shamsi, M.; Sedaghatkish, A.; Dejam, M.; Saghafianc, M.; Mehdi Mohammadi, M.; Sanati-Nezhad, A. Magnetically assisted intraperitoneal drug delivery for cancer chemotherapy. Drug Deliv. 2018, 25, 846-861. [CrossRef]
- Du, M.; Liu, X.-X.; Xu, C.-J.; Zhang, X.-Y. Research progress on application of artificial intelligence (AI) in radiotherapy for gynecological malignancy. China J. Radiat. Oncol. 2022, 31, 671-674.
- Quan, Z.-M; Jiang, H. The practice perspective of the internet combining with artificial intelligence in the area of gynecologic tumor management. Fudan Univ. J. Med. Sci. Oncol. 2019, 46, 556-561.
- Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L. H; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500-510. [CrossRef]
- Saw, C. B.; Li, S.; Battin, F.; McKeague, J.; Peters, C. A. External beam planning module of Eclipse for external beam radiation therapy. Med. Dosim. 2018, 43, 195-204. [CrossRef]
- Zhou, J.; Zeng, Z.-Y.; Li, L. Progress of artificial intelligence in gynecological malignant tumors. Cancer Manag. Res. 2020, 12, 12823-12840. [CrossRef]
- Tanabe, K.; Ikeda, M; Hayashi, M.; Matsuo, K.; Yasaka, M.; Machida, H.; Shida, M.; Katahira, T.; Imanishi, T.; Hirasawa, T.; Sato, K.; Yoshida, H.; Mikami, M. Comprehensive serum glycopeptide spectra analysis combined with artificial intelligence (CSGSA- AI) to diagnose early-stage ovarian cancer. Cancers 2020, 12, 2373. [CrossRef]
- Zhang, Y.-D.; Gorris, J. M.; Wang, S.-H. Deep learning in medical image analysis: a review. J. Imag. 2021, 7, 74. [CrossRef]
- Chen, K.-Y.; Wang, Q.-B.; Ma, Y.-T. Cervical optical coherence tomography image classification based on contrastive self-supervised texture learning. Med. Phys. 2022, 49, 3638-3653. [CrossRef]
- Lawton, F. G.; Pavlik, E. J. Perspectives on ovarian cancer: 1809 to 2022 and beyond. Diagnostics 2022, 12, 791. [CrossRef]
- Zimmer-Stelmach, A.; Zak, J.; Pawlosek, A.; Rosner-Tenerowicz, A.; Budny-Winska, J.; Pomorski, M.; Fuchs, T.; Zimmer, M. The application of artificial intelligence-assisted colposcopy in a tertiary care hospital within a cervical pathology diagnostic unit. Diagnostics 2022, 12, 106. [CrossRef]
- Zhang, R.; Zou, Y.; Luo, J. Application of extracellular vesicles in gynecologic cancer treatment. Bioengineering 2022, 9, 740. [CrossRef]
- Maruthi, V.K.; Khazaeli, M.; Jeyachandran, D.; Desouki, M.M. The clinical utility and impact of next generation sequencing in gynecologic cancers. Cancers 2022, 14, 1352. [CrossRef]
- Terlizzi, M.; Minard, V.; Haie-Meder, C.; Espenel, S.; Martelli, H.; Guérin, F.; Chargari, C. Implementation of image-guided brachytherapy for pediatric vaginal cancers feasibility and early clinical results. Cancers 2022, 14, 3247. [CrossRef]
- Youneszade, N.; Marjani, M.; Chong, P.-P. Deep learning in cervical cancer diagnosis: architecture, opportunities, and open research challenges. IEEE Access 2023, 11, 6133-6149. [CrossRef]
- Liu, Y.; Lawson, B.C.; Huang, X.; Broom, B.M.; Weinstein, J.N. Prediction of ovarian cancer response to therapy based on deep learning analysis of histopathology images. Cancers 2023, 15, 4044. [CrossRef]
- Okada, Y.; Ning, Y.-L.; Ong, M.E.H. Explainable AI in emergency medicine: an overview. Clin. Exp. Emerg. Med. 2023, 10, 354-362. [CrossRef]
- Ghnemat, R.; Alodibat, S.; Abu Al-Haija, Q. Explainable artificial intelligence (XAI) for deep learning based medical image classification. J. Imaging 2023, 9, 177. [CrossRef]
- Allahqoli, L.; Hakimi, S.; Laganà, A.S.; Momenimovahed, Z.; Mazidimoradi, A.; Rahmani, A.; Fallahi, A.; Salehiniya, H.; Ghiasvand, M.M.; Alkatout, I.18F-FDG PETMRI and 18F-FDG PETCT for the management of gynecological malignancies: a comprehensive review of the literature. J. Imaging 2023, 9, 223. [CrossRef]
- Sekaran, K.; Varghese, R.P.; Gopikrishnan, M.; Alsamman, A.M.; El Allali, A.; Zayed, H.; Doss C, G.P. Unraveling the dysbiosis of vaginal microbiome to understand cervical cancer disease etiology: an explainable AI approach. Genes 2023, 14, 936. [CrossRef]
- Cheon,W.; Han, M.; Jeong, S.; Oh, E.S.; Lee, S.U.; Lee, S.B.; Shin, D.; Lim, Y.K.; Jeong, J.H.; Kim, H.; Kim, J.K. Feature learning analysis of a deep learning model on predicting late bladder toxicity occurrence in uterine cervical cancer patients. Cancers 2023, 15, 3463. [CrossRef]
- Abuzinadah, N.; Kumar Posa, S.; Alarfaj, A.A.; Alabdulqader, E.A.; Umer, M.; Kim, T.-H.; Alsubai, S.; Ashraf, I. Improved prediction of ovarian cancer using ensemble classifier and shapy explainable AI. Cancers 2023, 15, 5793. [CrossRef]
- Triumbari, E.K.A.; Rufini, V.; Mingels, C.; Rominger, A.; Alavi, A.; Fanfani, F.; Badawi, R.D.; Nardo, L. Long axial field-of-view PETCT could answer unmet needs in gynecological cancers. Cancers 2023, 15, 2407. [CrossRef]
- Margul, D.; Yu, C.; AlHilli, M.M. Tumor immune microenvironment in gynecologic cancers. Cancers 2023, 15, 3849. [CrossRef]
- Pang, J.; Xiu, W.; Ma, X. Application of artificial intelligence in the diagnosis, treatment, and prognostic evaluation of media- stinal malignant tumors. J. Clin. Med. 2023, 12, 2818. [CrossRef]
- Robert, A.; Potter, K.; Frank, L. Explainable AI: interpreting and understanding machine learning models. Artificial Intelligence 2024, 1-18; [Online Available]: https://www.researchgate.net/publication/377844899.
- Wang, Y.-L.; Lin W.-H.; Zhuang, X.-L.; Wang, X.-L., He, Y.-F.; Li, L.-H.; Lyu, G.-R. Advances in artificial intelligence for the diagnosis and treatment of ovarian cancer. Onco. Rep. 2024, 51, 46. [CrossRef]
- Seo, K.; Refai, H.H.; Hile, E.S. Application of dynamic mode decomposition to characterize temporal evolution of plantar pressures from walkway sensor data in women with cancer. Sensors 2024, 24, 486. [CrossRef]
- Jopek, M. A.; Pastuszak, K.; Cygert, S.; Best, M.G.; THOMAS WÜrdinger, T.; Jassem, J.; Żaczek, A.J.; Supernat, A. Deep learning-based multiclass approach to cancer classification on liquid biopsy data. IEEE J. Translation. Health Med. 2024, 12, 306-313. [CrossRef]
- Karalis, V.D. The integration of artificial intelligence into clinical practice. Appl. Biosci. 2024, 3, 14-44. [CrossRef]
- Brandão, M.; Mendes, F.; Martins, M.; Cardoso, P.; Macedo, G.; Mascarenhas, T.; Mascarenhas Saraiva, M. Revolutionizing women’s health: a comprehensive review of artificial intelligence advancements in gynecology. J. Clin. Med. 2024, 13, 1061. [CrossRef]
- Wu, A.-Y.; Remela, R.; Qiao, Y.-L. Progress and challenge of artificial intelligence in diagnosis treatment of cervical lesions. Chin. Gen. Pract. 2022, 25, 2215-2222, 2230. [CrossRef]
- Guha, S.; Kodipalli, A.; Fernandes, S. L.; Dasar, S. Explainable AI for interpretation of ovarian tumor classification using enhanced ResNet50. Diagnostics 2024, 14, 1567. [CrossRef]
- Moltó-Balado, P.; Reverté-Villarroya, S.; Alonso-Barberán, V.; Monclús-Arasa, C.; Balado-Albiol, M.T.; Clua-Queralt, J.; Clua-Espuny, J.-L. Machine learning approaches to predict major adverse cardiovascular events in atrial fibrillation. Technologies 2024, 12, 13. [CrossRef]
- Litjens, G.; Kooi, T.; Bejnordi, B. E.; Setio, A. A. A.; Ciompi, F.; Ghafoorian, M.; Laak, J. A.W.M. van der; Ginneken, B. van; S’anchez, C. I. A survey on deep learning in medical image analysis. Med. Image Anal. 2017, 42, 60-88. [CrossRef]
- Luo, X.-Y.; Qu, L.-H.; Guo, Q.-H.; Song, Z.-J.; Wang, M.-N. Negative instance guided self-distillation framework for whole side image analysis. IEEE J. Biomed. Health Inform. 2024, 28, 964-975. [CrossRef]
- Mahmud, T.; Barua, K.; Habiba, S.U.; Sharmen, N.; Hossain, M.S.; Andersson, K. An explainable AI paradigm for Alzheimer’s diagnosis using deep transfer learning. Diagnostics 2024, 14, 345. [CrossRef]
- Allen, B. The promise of explainable AI in digital health for precision medicine: a systematic review. J. Pers. Med. 2024, 14, 277. [CrossRef]
- Taherdoost, H; Madanchian, M. AI advancements: comparison of innovative techniques. AI 2024, 5, 38-54. [CrossRef]
- Hulsen, T. Artificial intelligence in healthcare: ChatGPT and beyond. AI 2024, 5, 550-554. [CrossRef]
| Reference | Year | General Category | Brief Summary of Kernel Work |
|---|---|---|---|
| [15] | 2014 | Da Vinci Robot assisted system | treating ovarian cancers in early stage |
| [6] | 2016 | NN and AI-based DSSS | histological diagnosis on females |
| [11] | 2016 | AI guidance for pre-surgery | classifying adnexal masses with NN |
| [13] | 2017 | Deep CNN based scheme | liquid-based imaging on cervical cells |
| [8,9,10] | 2017-2018 | CV framework with AI | detecting cervical lesions in colposcopy |
| [17,18,19] | 2017-2018 | AI-aided biochemical therapy | molecular drugs on cancer chemotherapy |
| [7] | 2018 | CNN-based AI | predicting endometrial cancer |
| [16] | 2018 | XAI-related video processing | comprehensive system on telemedicine |
| [22,23] | 2018 | AI-aided radiation oncology | Eclipse and AutoPlan on treating tumors |
| [4] | 2019 | Study and use on AI and big data | AI techniques on gynecological tumors |
| [21] | 2019 | “Internet + AI” based techniques | Prospecting gynecologic tumor management |
| Author | Year | Main Set of Approaches | Publication Title |
|---|---|---|---|
| Zhou et al. | 2020 | AI Progress in gynecological cancers | Cancer Management and Research |
| Tanabe et al. | 2020 | Combining AI to diagnose ovarian cancer | Cancers (MDPI) |
| Zhang et al. | 2021 | Deep learning in medical image analysis | Journal(J.) of Imaging (MDPI) |
| Chen et al. | 2022 | Cervical cancer imaging with contrastive learning | Medical Physics |
| Lawton & Pavlik | 2022 | Prospecting ovarian cancer till 2022 and beyond | Diagnostics (MDPI) |
| Zimmer-Stelmach | 2022 | AI-assisted colposcopy in cervical diagnosis | Diagnostics (MDPI) |
| Zhang et al. | 2022 | Extracellular vesicles and AI for gynecological cancer | Bioengineering (MDPI) |
| Maruthi et al. | 2022 | Next generation testing on gynecological cancer | Cancers (MDPI) |
| Terlizzi et al. | 2022 | Image-guided brachytherapy for pediatric vaginal cancer | Cancers (MDPI) |
| Youneszade et al. | 2022 | Deep learning (DL)-based cervical cancer diagnosis | IEEE Access |
| Liu et al. | 2023 | Inception V3 model on predicting ovarian cancer | Cancers (MDPI) |
| Okada et al. | 2023 | Explainable AI(XAI) in emergency medicine | Clinical and Experimental Emergency Medicine |
| Ghnemat et al. | 2023 | XAI for DL-based medical diagnosis | J. of Imaging (MDPI) |
| Allahqoli et al. | 2023 | PET/MRI, PET/CT to manage gynecological tumors | J. of Imaging (MDPI) |
| Sekaran et al. | 2023 | SHAP and XAI on disease etiology of cervical cancer | Genes (MDPI) |
| Cheon et al. | 2023 | DL on predicting bladder toxicity from cervical cancer | Cancers (MDPI) |
| Abuzinadah et al. | 2023 | Shapely XAI on improving prediction of ovarian cancer | Cancers (MDPI) |
| Triumbari et al. | 2023 | LAFOV PET/CT imaging on gynecological malignancies | Cancers (MDPI) |
| Margul et al. | 2023 | Gynecological tumors with immune microenvironment | Cancers (MDPI) |
| Pang et al. | 2023 | Applying AI in Mediastinal malignant tumors | J. of Clinical Medicine (MDPI) |
| Duan et al. | 2023 | Trending and projecting gynecological cancer in China | BMC Women’s Health |
| Robert et al. | 2024 | Machine learning models for explainable AI | Artificial Intelligence |
| Wang et al. | 2024 | AI advances on diagnosing and treating ovarian cancer | Oncology Reports |
| Seo et al. | 2024 | Emerging AI via walkway sensor data for women with cancer | Sensors (MDPI) |
| Jopek et al. | 2024 | DL and XAI approach to classify gynecological cancers on liquid biopsy data Engineering | IEEE J. of Translational in Health and Medicine |
| Karalis et al. | 2024 | Clinical use of AI such as gynecological oncology | Applied Biosciences (MDPI) |
| Brandão et al. | 2024 | AI advancements in gynecology including differentiating and diagnosing types of malignancies | J. of Clinical Medicine (MDPI) |
| Author | Year | Main AI Scheme | Data Source | Analytical Methods | Performance Metrics |
|---|---|---|---|---|---|
| Sinno & Fader [15] | 2014 | Da Vinci Robot assisted surgery | Number of patients | Review, case report, and cost analysis | Surgical indices, costs, and 5-year survival rates |
| Kyrgiou et al. [6] | 2016 | ANN and DSSS | Clinical data | Prediction via MLP, ANN, and histological diagnosis | Accuracy indices and statistical measures |
| Zhang et al. [13] | 2017 | DeepPap and transfer learning | Pap Smear and HEMLBC datasets | ConvNet learning, cross-validation | Information retrieval (IR), AUC, classification accuracy |
| Pergialiotis et al. [7] | 2018 | ANN and CARTs | Clinical cases | Logistic regression | IR indices, overall accuracy, and prediction values |
| Tang and Li [4] | 2019 | Big data and XAI | Case reports | Systematic review | Not applicable (N/A) |
| Quan and Jiang [21] | 2019 | “Internet + AI” | Clinical data | Systematic review | Not applicable (N/A) |
| Zhou et al. [24] | 2020 | Shallow learning, DL, ensemble classifier | Medical imaging, pathological data | Model performance, Systematic review | C-index, AUC, accuracy, and importance factors |
| Tanabe et al. [25] | 2020 | Deep CNN, CSGSA-AI | Sample patients | CNN with 2D barcodes | ROC-AUC, IR indices |
| Chen et al. [27] | 2022 | Deep CNN and CADx | Clinical study | In-vivo 3D OCT imaging | ROC and IR indices |
| Zimmer-Stelmach [29] | 2022 | CNN-based classification | Sample patients | AI-aided Colposcopy | IR indices and PPV |
| Youneszade et al. [33] | 2022 | CNN, DL-based CAD | Typical image datasets | Systematic review | Stage and IR indices |
| Duan et al. [1] | 2023 | Projected classification Grey model prediction | Statistical data reports | Statistical analysis, graphical visualization | Data metrics and Classification (CI) |
| Liu et al. [34] | 2023 | DL (Inception V3) | TCGA, sample patients | DL, classification, visualization, and prediction | ROC-AUC, OSA, and survival rates |
| Okada et al. [35] | 2023 | XAI and ML models | Clinical case study | Review with visualization | SHAP values |
| Sekaran et al. [38] | 2023 | SHAP and XAI | Cervical cancer samples and healthy samples | k-fold cross-validation, statistical visualization | ROC, residuals, and SHAP values |
| Cheon et al. [39] | 2023 | Multi-variate logistic regression and Lightweight | Sample patients (281 (with cervical cancer) | 5-fold cross validation, statistical classification | Basic IR indices and AUROC, p-value |
| Abuzinadah et al. [40] | 2023 | Shapely XAI and ensemble learning | Ovarian cancer dataset in Soochow university | Feature classification and k-fold cross validation | IR metrics and feature weights |
| Wang et al. [45] | 2024 | AI with radiomics | Sample patient datasets (with ovarian cancer) | Systematic review and visualization | Basic IR metrics and AUC (as narrated) |
| Jopek et al. [47] | 2024 | DL(ResNet) with TEP and XAI (SHAP) | Sample datasets (with multiple cancers) | Binary classification and 5-fold cross validation | Balanced accuracy and other IR metrics |
| Brandão et al. [49] | 2024 | Typical ML and DL models for XAI | Case reports in clinical study and tests | Systematic review Basic IR metrics and AUC (as narrated) | |
| Guha et al. [51] | 2024 | Modified ResNet50 in contrast to XAI | CT image datasets (with ovarian tumors) | Algorithmic proposal and systematic review | Architecture, basic IR metrics, loss and error |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





