1. Introduction
1.1. Background and Motivation
A chronic health condition poses a significant challenge in a patient’s life. Managing it is often difficult, time-consuming, and not always effective, especially since many patients suffer from more than one chronic health issues. Addressing these challenges in community healthcare management requires strategic methodologies that facilitate a personalized care approach for several key reasons. Individuals have diverse healthcare needs, cultural backgrounds, and preferences, necessitating individualized solutions. Furthermore, community healthcare programs frequently encounter limited resource, making efficiency imperative. Additionally, tailored and efficient interventions are more likely to achieve the desired results. Patients who receive personalized care tend to be more involved in their treatment plans, experience better health outcomes, and generally require less intensive interventions [
1]. Furthermore, those who perceive their needs as fully met are more likely to develop greater trust and engagement with the healthcare system [
2,
3]. Consequently, it is crucial to explore how healthcare systems can maintain sustainable practices while ensuring comprehensive coverage and high-quality care services that reflect a patient-directed approach. Indeed, an efficient management of patients, especially those with chronic health conditions, through a well-planned community-based assistance, is essential for both current and future healthcare scenarios.
The integration of Information and Communication Technology (ICT) capabilities with implemented care models allows for the definition of dynamic and adaptive services that meet the needs of citizens and patients while supporting healthcare personnel in managing an increasing number of patients through a 4.0 territorial assistance model. Traditional healthcare models have predominantly been reactive, focusing on treatment after the onset of disease [
4]. However, with the rise of digital health technologies, there is a significant shift towards proactive and preventive approaches that can lead to early detection of potential health issues, allowing for prompt and appropriate actions [
5,
6]. Health community 4.0 embodies this shift, leveraging real-time data and advanced analytics to predict and prevent health issues before they become critical. Furthermore, this type of management, in addition to requiring advanced technologies such as telehealth platforms, remote monitoring devices, and wearable health sensors, also necessitates a well-defined strategy, which we believe should be a bottom-up process. A “one-size-fits-all” approach is widely recognized as inadequate in addressing the complexity and diversity of individuals’ needs, resulting in suboptimal care and potentially excluding people from accessing essential services. In contrast, a bottom-up process begins at the grassroots level and emphasizes the involvement and contribution of individual components in order to build a larger, more complex system [
7]. Unlike a top-down approach driven by centralized authority, the bottom-up method is based on a co-managed model of care and empowers healthcare providers, patients and families, fostering inclusivity by allowing diverse perspectives and ideas to naturally emerge. This approach encourages collaboration and innovation, ensuring that users actively participate in the design and development of systems and services [
8].
When implementing this participative approach, it is essential to consider its adoption among end-users. As stated by the Unified Theory of Acceptance and Use of Technology (UTAUT) [
9], the success of the developed solution relies on active participation and sustained use by the communities involved in its creation [
10]. UTAUT particularly identifies social influence and facilitating conditions as significant factors influencing technology adoption. Social influence represents perceived pressure from others to use technology, which, in the context of community participation in solution creation, can foster ownership and peer support. Facilitating conditions, including resource availability, technical support such as tailored training and ongoing assistance, and clear communication channels, are essential for ensuring that users feel competent and comfortable using the solution effectively.
This methodology represents a transition from traditional to modern medicine through the concept of "super convergence". Modern medicine integrates elements such as social networking, wearable and environmental sensors, and computational power, forming the basis of a new healthcare paradigm centered on advanced technologies and aimed at enhancing patient care. The evolution towards modern medicine recognizes patients as health consumers, emphasizes the importance of home as the primary place for care, and ensures no one is left behind. Patients are more likely to feel supported and understood, knowing that their care is being systematically managed and that they are active participants in their healthcare journey [
11]. Consequently, this streamlining of processes allows for better coordination of care, timely interventions, and personalized treatment plans, leading to increased patient satisfaction [
12,
13]. Education and regulatory frameworks are also essential for ensuring that both patients and healthcare providers are well-informed and compliant to best practices. Guiding principles include homogeneity, balance, and equity, alongside an integrated approach to health pathways and adaptable resource management. Also, fostering a culture of innovation is pivotal for ongoing quality improvement in healthcare. This approach, centered on occurrences and specific needs of patients and caregivers, not only enhances preventive healthcare measures but also significantly contributes to optimizing community healthcare assistance overall [
13,
14,
15].
1.2. Our Contribution
Recently, healthcare management has been undergoing a transformative evolution with the integration of self-monitoring, monitoring, and patient journey tracking into a unified system [
16]. By utilizing real-time data, personalized care plans, and continuous feedback, healthcare providers can significantly enhance patient outcomes, improve operational efficiency, and deliver high-quality, cost-effective care. As healthcare continues to evolve, the adoption of such innovative solutions is essential in meeting the increasing demands and expectations of both patients and providers.
Our work has focused on emphasizing the need for a tool that integrates patient self-monitoring, professional monitoring, and patient care planning. This tool is designed not only to enhance patient management but also to improve actual organizational models based on collected feedback, such as deviations from the planned outcomes. Specifically, we proposed a multidisciplinary bottom-up approach named smartHUB, which emphasizes end-user engagement from the initial stages and throughout the design process. The aim is to implement a 4.0 assistance system capable of effectively addressing future challenges related to citizen health and well-being. This innovative approach has been developed within the framework of the smartHUB project and has been applied to the design and development of new healthcare assistance tools for the Local Health Unit (LHU) Toscana Centro, a component of the Tuscany Health Service known for its highly advanced healthcare system [
17].
To address the variety of territorial needs, we propose a scalable pathway that can be carefully customized as needed. The identified ICT solution, designed to effectively enhance territorial care, consists of an innovative platform that includes a highly tailored mobile app. Such system is specifically planned for health data collection through patient self-monitoring or during home visits by nurses, with the aim to increase patients’ self-awareness regarding their health status and support nurses in the provision of patient-centered care. One of the primary goals of this initiative is to streamline healthcare processes and provide comprehensive support to patients, thereby fostering a more connected and efficient healthcare environment.
The paper is organized as follows: after providing the background context and the motivation behind the need for innovative ICT tools for effective healthcare management (
Section 1), in
Section 2 we describe our multidisciplinary approach called smartHUB, focusing on how it has been conceived to stimulate and support local administrations, social and health institutions, and third sector organisations.
Section 3 outlines the co-designed creation of the system, from users’ needs to system implementation, while
Section 4 offers an overview of the architecture of the proposed solution, the PROASSIST 4.0 system. This is followed by a detailed description of the developed mobile application, PROASSIST 4.0 app, including its profiles and functionalities (
Section 5). Furthermore,
Section 6 highlights the refinement of our App based on initial findings from the system evaluation phase, in addition to detailing upcoming experimental activities intended to validate these app adjustments. Finally,
Section 7 discusses the presented solution and associated challenges, concluding with remarks in Paragraph 8.
2. The smartHUB Approach: An Innovative Multidisciplinary Systemic Methodology
The smartHUB methodology employs a systemic management approach to innovation processes, engaging all stakeholders (users, service providers, companies, researchers, and policymakers) from the initial needs analysis through the entire design process.
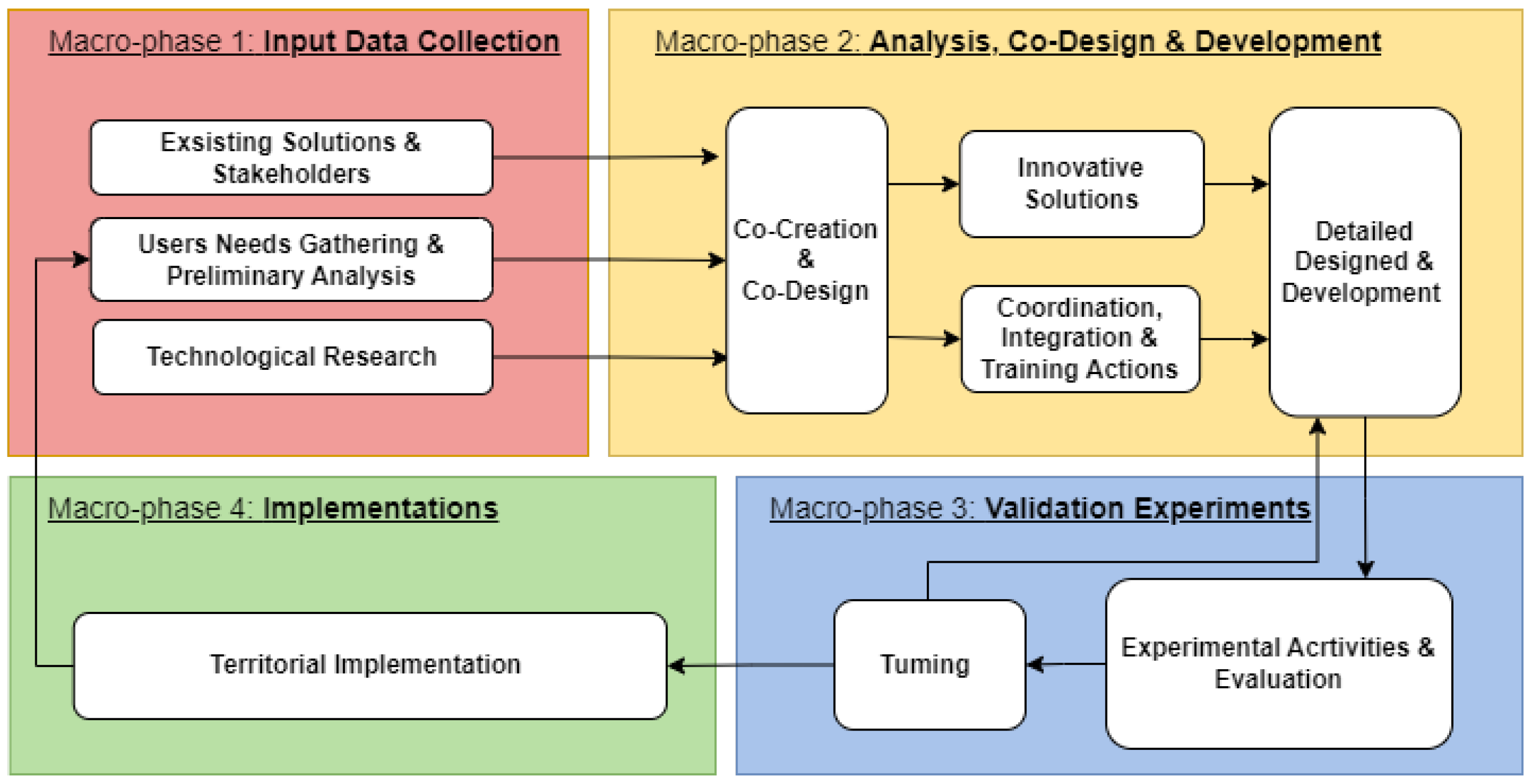
It consists of four macro-phases (
Figure 1), which are briefly described in the following subsections:
- -
Macro-phase 1: Input Data Collection;
- -
Macro-phase 2: Analysis, Co-design and Development;
- -
Macro-phase 3: Validation Experiments;
- -
Macro-phase 4: Implementation.
2.1. Macro-Phase 1: Input Data Collection
The initial macro-phase focuses on data collection, beginning with active community involvement. After determining the application context, the critical step of "listening to the territory’s needs" helps define the final technological solution. Essential participants in social and healthcare service delivery, along with their beneficiaries, play an active role in identifying both current and emerging needs. Moreover, community engagement offers a detailed overview of the implemented solutions, highlighting their advantages and disadvantages concerning operational activities.
Besides performing a preliminary analysis of user needs, existing solutions, and stakeholder feedback, this macro-phase also considers the state-of-the-art in technological research. This is to explore both current and emerging technologies that could be adopted to create innovative solutions addressing the identified needs. Data collection methods employed during this macro-phase include workshops, focus groups, and literature reviews.
2.2. Macro-Phase 2: Analysis, Co-Design and Development
The second macro-phase is composed of three steps: i) co-design and co-creation; ii) identification of innovative solutions for coordination, integration, and training actions; iii) detailed design and development.
The co-design and co-creation phase involves a thorough analysis of the gathered data, with a particular focus on evaluating existing solutions, their potentials, and limitations. This step aims to identify gaps in relation to current and anticipated technological advancements.
By employing a multidisciplinary co-design and co-creation approach that involves frequent interactions with end-users, innovative solutions are identified. Additionally, this approach facilitates the development of coordination, integration, and training actions to enable active experimentation within the community.
The final step of this macro-phase involves the realization of the identified solution. This includes translating the high-level project into a detailed design by defining system requirements and functional components necessary for development and integration. Furthermore, this step encompasses the execution of functionality, integration, and internal validation tests, preparing the solution for real-world testing with end-users.
2.3. Macro-Phase 3: Validation Experiments
The third macro-phase serves as a small-scale experimental validation campaign conducted within the community. Its aim is to achieve preliminary validation and evaluation of the proposed solution in response to emerging needs, through the incremental refinement of the system. This phase is crucial for implementing and standardizing innovative solutions and actions that provide significant value to individual well-being and health, which everyone should be aware of.
This macro-phase comprises two main steps: i) experimental and evaluation activities, and ii) tuning. Experimental activities involve testing the proposed solution in a controlled environment with active participation from end-users, gathering their feedback through interviews and specially designed questionnaires. The tuning step involves adjusting the solution based on the feedback analysis. As illustrated in
Figure 1, this step may require detailed design revisions and/or the addition of new features to enhance the solution. The feedback-tuning cycle may need multiple iterations, depending on the extent of revisions necessary.
2.4. Macro-Phase 4: Implementations
The fourth macro-phase involves implementing the solution within the community, thus concluding one operational cycle and initiating the next. Evolving societal needs and the introduction of innovative solutions can lead to new requirements and changes. Therefore, continuously "listening to the community" is crucial for defining technological systems that effectively support social and healthcare services.
2.5. The smartHUB Approach in the Healthcare Assistance Management Framework
In the healthcare assistance management context, the smartHUB approach has the ultimate goal of improving patient care and quality of life [
14], linking the digital world into the real one to benefit the patient [
15]. One of the primary objective of this initiative is to streamline healthcare processes and offer comprehensive support to patients, fostering a more connected and efficient healthcare environment. Co-design and development phases focus on user-centered principles, creating an intuitive and accessible interface suitable for patients of all ages and technical abilities.
3. The Co-Designed System PROASSIST: from Users’ Needs to System Implementation
3.1. Application Context: Nursing Home Assistance
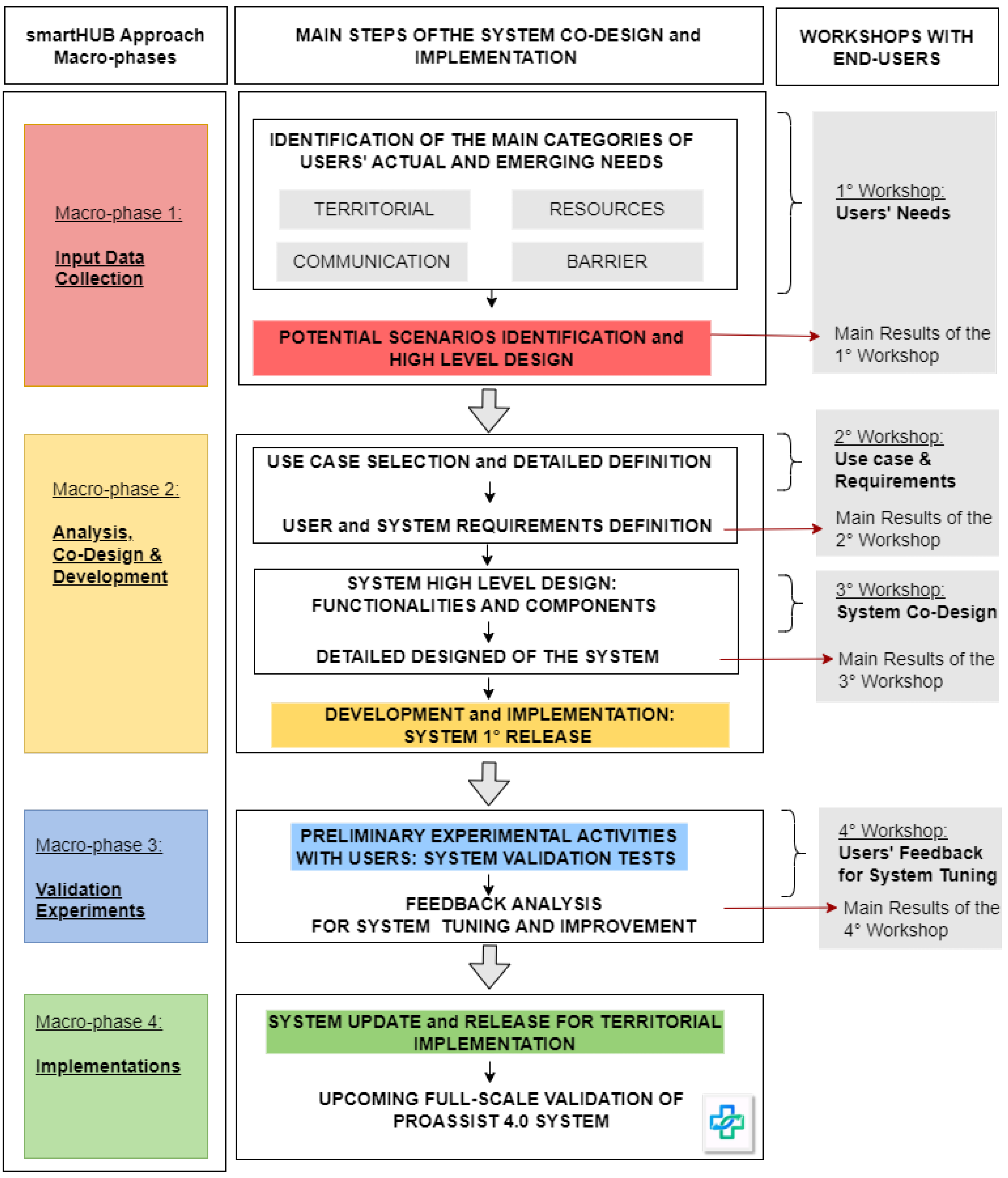
The smartHUB approach has been adopted to design and develop effective ICT tools for improving community healthcare nursing assistance in the LHU Toscana Centro. In particular, the process starting with gathering users’ needs has led to the implementation of PROASSIST 4.0 system, that will be tested, validated and evaluated in a real context. In
Figure 2, an overview of the main steps needed for the system co-design and implementation is provided. These steps are mapped into the smartHUB approach macro-phases (figure left side) and into the co-design workshops held with users (figure right side). We organized four workshops with all end-users (family and community nurses - FCNs, nurse coordinators and patients associations) in an effort to analyse the specific needs of territorial nursing care and provide initial definition of possible improvement strategies for community healthcare management. During each workshop, particular attention was given to the areas of patient care, health monitoring, care pathways and emerging needs. Specifically, the first three sessions (co-design and co-creation workshops) were intended to identify the main actors of territorial nursing care and collect information about the current state of the art of community healthcare assistance, users’ emerging needs, and nurses’ desires related to their work management. Data gathered during the co-design and co-creation activities was then analyzed to define the main user requirements and the most relevant use cases for the solution design. Finally, the last workshop was oriented to expose and evaluate the implemented ICT solution resulted from the previous sessions, in order to collect users’ feedback essential for system tuning. Several processes to system tuning have been conceived and implemented to develop a ICT tool that is functional and effective for the community healthcare nursing services at LHU Toscana Centro. Nevertheless, the proposed solution remains under continuous development and ever more specific improvements will be required to achieve the final implementation.
3.2. Users’ Needs: Identification and Classification
Users’ emerging needs we collected during the co-design and co-creation workshops can be grouped in four main categories:
Territorial needs;
Resources needs;
Communication needs;
Barrier needs.
Within each category, for each specific need, the desired outcomes (how one would wish it to be) were solicited. Based on these inputs, a proposal of functionalities was formulated to satisfy the users’ requirements, always within the specific operational context of reference.
3.2.1. Territorial Needs
Territorial needs arise from the observation that each territory has its own specificities, with central and peripheral zones differing in terms of ease of reaching the patient. Accessing peripheral areas entails a longer time, while in the urban areas, despite distances are limited, traffic represents a significant concern. Territorial needs deal also with the absence of cellular network coverage in some peripheral areas and with the lack of knowledge regarding the services available within the territory. To address these emerging needs, the following functionalities have been proposed: i) location-independent connectivity (e.g., alternative networks); ii) traffic-based route optimization; and iii) territorial map with indications of gathering points and local services.
3.2.2. Resources Needs
Resources needs encompass shortages in personnel, such as a lack of specialized medical staff, as well as deficiencies in technological tools used for management and organization of care programs. Currently, health parameters measurement and data collection during home visits are manually conducted on a paper, with subsequent transcription into the corporate program. In addition, there is a lack of accessible historical patient data and technological tools enabling personalized weekly planning and management of criticalities in patient care. In order to comprehensively respond to these needs, we proposed the development and implementation of the following functionalities: i) direct input of health data into the automated system (via connected devices) or through manual entry or voice assistant; ii) patient data history with graphical reports, shared among all healthcare professionals involved in patient’s care; iii) patient-specific approach for accurate data interpretation and goal assessment; iv) automated planning as initial recommendation for management of patient care; v) proximity-based nurse localization for patients with critical conditions; vi) personalized data correlation algorithms with priority indication; vii) tracking and reminders to ensure therapy adherence; and viii) color notifications to patients for anxiety mitigation and reduced unnecessary communication.
3.2.3. Communication Needs
Communication needs arise from the necessity for a more efficient interaction among all healthcare professionals involved in patient’s care, with the aim of facilitating the management of patient’s health status, particularly in critical conditions. Among communicative needs, there is also the necessity to establish a visual interaction between healthcare workers and the patient, essential for better understanding patient’s non-verbal behaviours and building a relationship based on empathy. Potential functionalities that could support healthcare professionals in their work include: i) real-time communication for effective collaboration among all actors involved; and ii) video calls for direct interactions with the patient and visual management of medical conditions. Proposed functionalities that could help patients consist of: i) opportunity for patients to access to their health data in a modality appropriate for them, fostering their involvement and awareness of their treatment journey while mitigating potential anxiety; ii) possibility for patients to know that nurses are effectively managing their health situation in order to perceive to be actively monitored; and iii) reminders for therapy, healthy lifestyle practices, and appointments.
3.2.4. Barrier Needs
Barrier needs refer to overcoming technological barriers, particularly those faced by individuals who are less familiar with digital tools, as well as linguistic and cultural barriers arising from different cultures and religions. Suggested functionalities that could resolve such needs include: i) the design and development of an inclusive interface with multilingual support, voice assistant, virtual coach sessions, real-time assistance, and translations services; and ii) the provision of training and educational content for health workers, patients, and caregivers to facilitate their the use of technological devices.
3.3. Selected Use Case for System Implementation: Data Gathering, Sharing and Planning
Following the assessment of emerging needs and the subsequent analysis of the desired outcomes and functionalities, three distinct potential use scenarios for the smartHUB approach were identified:
- (1)
Collection of medical data for remote health monitoring, including data sharing among healthcare professionals and support through a virtual coach;
- (2)
Collaboration among FCNs to efficiently manage patients in accordance to the geographical proximity of the healthcare professional to the patient and traffic conditions in urban areas;
- (3)
Multilingual video interpretation service to facilitate communication between patients and healthcare providers from different cultural backgrounds.
Considering the identified necessity for appropriate ICT systems customized to the specific operational demands of healthcare workers involved in territorial care management, encompassing the creation of a comprehensive patient monitoring history, alongside with the well documented increase in life expectancy and the importance of domiciliary care, we decided to prioritize the first scenario. In response to the emerging challenges arising from the exponential growth in the number of patients receiving home-based care, we proposed the development of PROASSIST 4.0 system with the purpose to ensure real-time personalized management of patients for a 4.0 territorial care. Specifically, PROASSIST 4.0 system primarily aims to i) delineate dynamic and adaptive services capable of addressing the needs of citizens and supporting healthcare professionals in managing a progressively growing patient population through a 4.0 territorial care approach, exploiting the potential of ICT solutions by integrating them with the care models already employed in healthcare; and ii) ensuring efficient planning of territorial care in accordance with occurrences and the actual needs of patients and caregivers. With the introduction of these tools, PROASSIST 4.0 system intends to align with new paradigms for complex organizations, requiring flexibility, adaptability, and optimization, and to assure the maintenance and promotion of the well-being and safety of all individuals involved in the process.
4. PROASSIST 4.0 System Architecture Overview
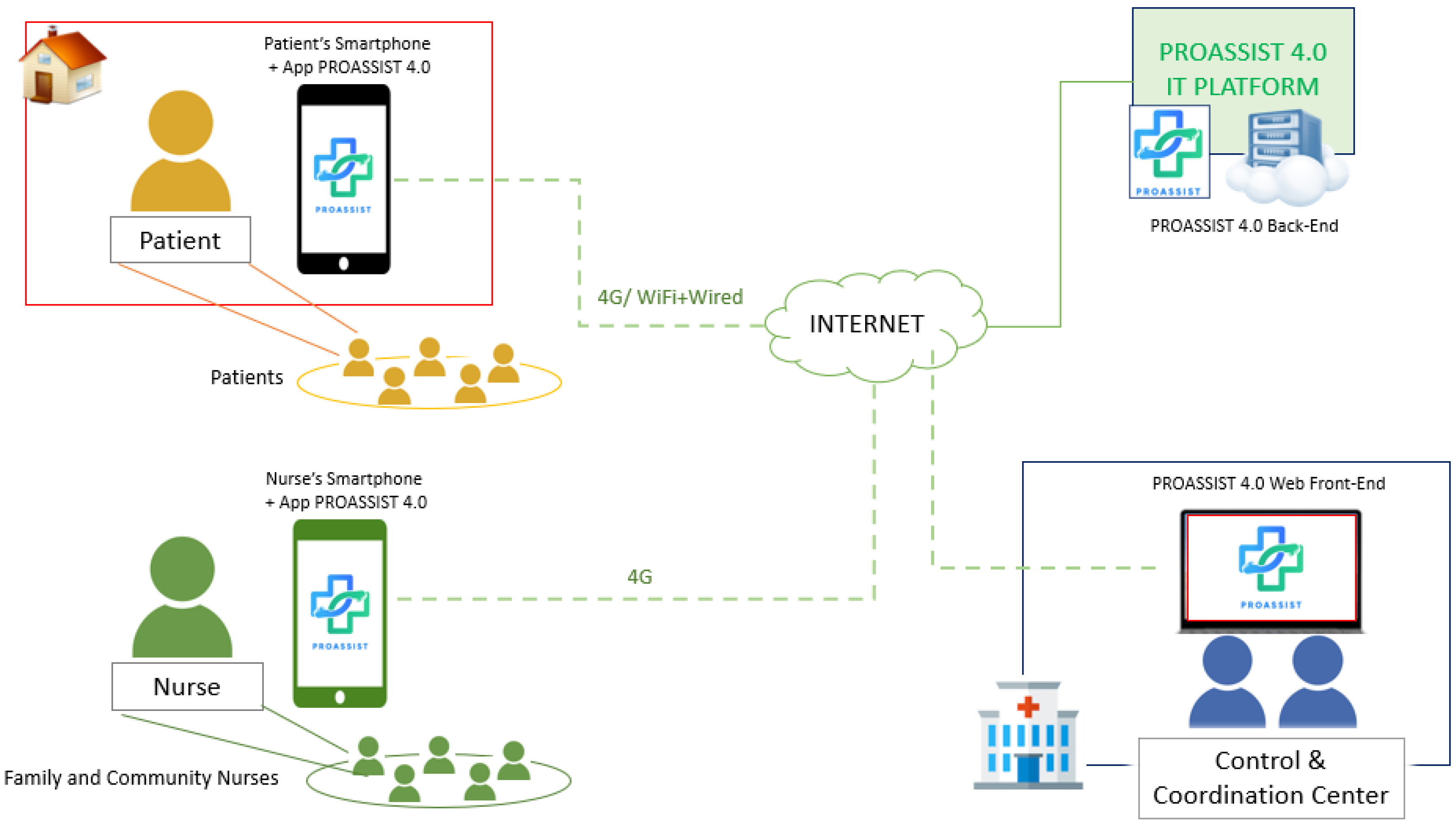
Figure 3 provides a comprehensive overview of PROASSIST 4.0 system’s architecture, highlighting its main components and the interconnections and communication protocols used for data exchange among them.
As detailed in the following sections, PROASSIST 4.0 system facilitates the collection, processing, and storage of health data entered by patients and FCNs. Data can be manually inserted or acquired by wireless wearable sensors used for clinical parameters measurements and monitoring. Through PROASSIST 4.0 app, patients can independently input their health data and access educational content and tutorials to manage their health effectively, fostering self-monitoring. Additionally, nurses are allowed to input health measurements taken during home visits, thereby enhancing home care health services and promoting a more comprehensive patient care.
Privacy and security are paramount. Data entered by users is securely transmitted to the cloud server via the HTTPS protocol for storage and basic processing, including data organization, generation of historical data in graphs, and filtered views tailored to individual user profiles. The cloud deployment of the platform is hosted on Amazon AWS, ensuring compliance with the General Data Protection Regulation (GDPR), AgID certification, and servers located within the European Union. To minimize the risk of data loss, stored data undergoes periodic backups. Furthermore, transparent privacy policies and consent procedures are clearly communicated to users, building trust and confidence in the app’s use.
Notably, PROASSIST 4.0 system has been specifically designed from its inception to be modular, scalable, and open to integration with other platforms. Its architecture is composed of the following interlinked macro-modules:
The web front-end is accessible via a desktop platform by the system administrator for management of users (both patients and nurses). The creation of profiles and the subsequent assignment of patients to their respective nurses allow patients to access and view their own medical data, and nurses to retrieve the data of their patients by the mobile application. All the data processing, management and exchange based on specific permission is provided by the system back-end hosted in cloud (PROASSIST 4.0 IT Platform).
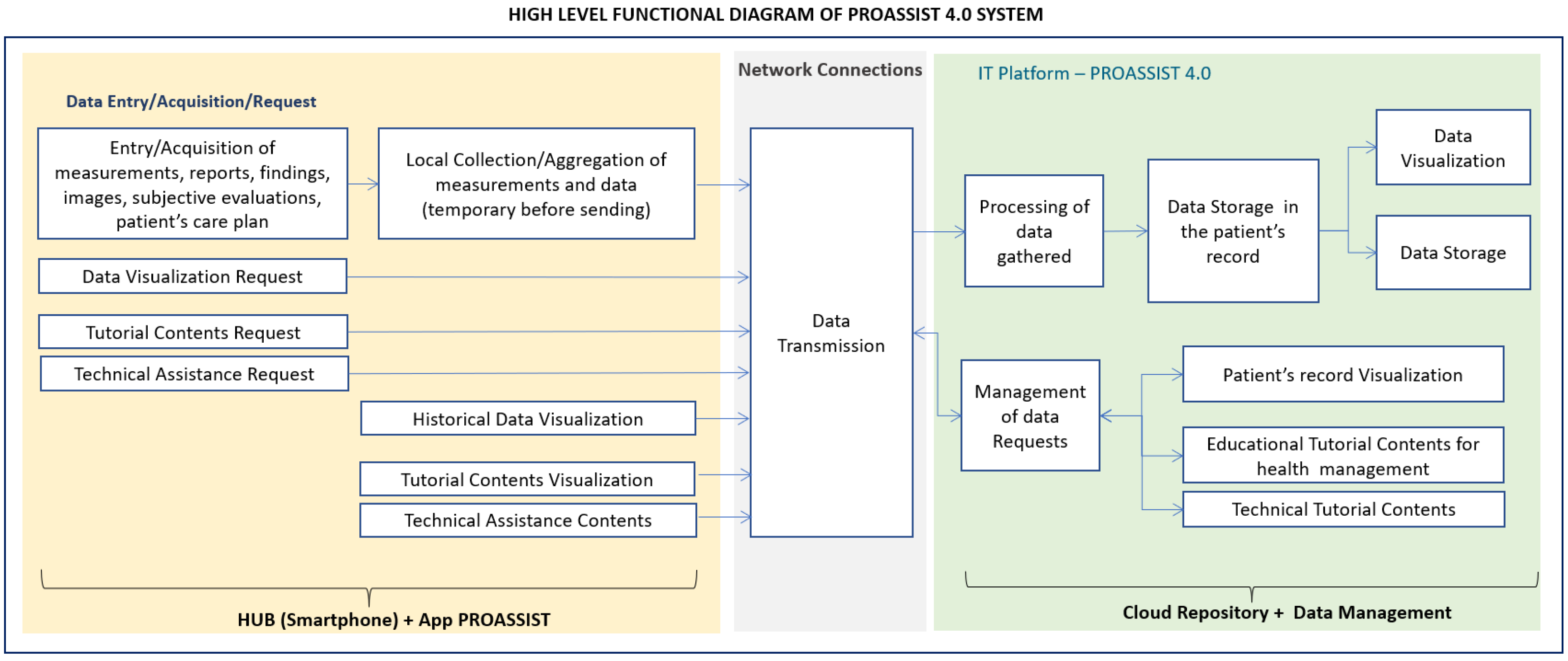
In order to give an overview of the system functionalities, in
Figure 4 the high level functional diagram of PROASSIST 4.0 system is shown, highlighting both the end-users’ side and the IT platform side. A more detailed analyses of end-users’ side functionalities is carried out in the following section, where the macro-functionalities of PROASSIST 4.0 app are described.
5. PROASSIST 4.0 App
PROASSIST 4.0 app constitutes a digital tool for the collection and sharing of information regarding the patient’s health status. Data gathering can occur either through self-monitoring directly conducted by patients in their daily life or during home visits by FCNs, who provide patient assessments, evaluations, and care. In the former case, the developed app aims to support patients in gathering greater awareness and management of their own health, thereby fostering their involvement in the care process. In the latter case, PROASSIST 4.0 app aspires to assist home-visit nurses in providing home care services. A real-time remote monitoring system enables the collection of patients’ health parameters, the identification of unforeseen critical issues, and the subsequent adjustment of family nurses’ visit scheduling, ensuring timely assistance based on emergent priorities.
5.1. Macro-Functionalities
PROASSIST 4.0 app is specifically designed to offer the following macro-functionalities, all available through an internet connection:
Profiles creation and management: the app facilitates the creation and management of users’ profiles, currently limited to patients and nurses. Future updates will expand this macro-functionality to include profiles of other healthcare professionals engaged in patient care. Overall, the app aims to offer a comprehensive and integrated platform that supports a broader range of healthcare services and professionals involved in the patient’s healthcare journey.
Acquisition and visualization of health data: users can input a variety of health data, including vital measurements, medical reports, images, subjective evaluations, as well as information regarding the management of health devices. Both nurses and patients can access their data through textual descriptions and graphical trends, enabling them to effectively monitor and analyze health information over time. This functionality empowers patients to actively monitor their health status and nurses to make informed decisions about patient treatment plans.
Communication: PROASSIST 4.0 app supports one-way communication from nurses to patients. Such feature enables nurses to effectively communicate important information and instructions to patients, even though the latter are currently not allowed to respond directly via the application. Future enhancements may focus on enabling bidirectional communication in order to improve interaction and patient engagement.
Information and training: the "Resources" section of PROASSIST 4.0 app provides users access to video tutorials for using the app and managing health measurements. Many of these resources are specifically customized for nurses and patients, ensuring targeted information. Additionally, technical assistance and training are offered to help users with the correct use of the system. Such functionalities guarantee that users are well-informed about health-related topics while also receiving the necessary guidance for navigating through the application interface, thereby enhancing user experience and promoting better health management.
5.2. Profiles and Related Functionalities
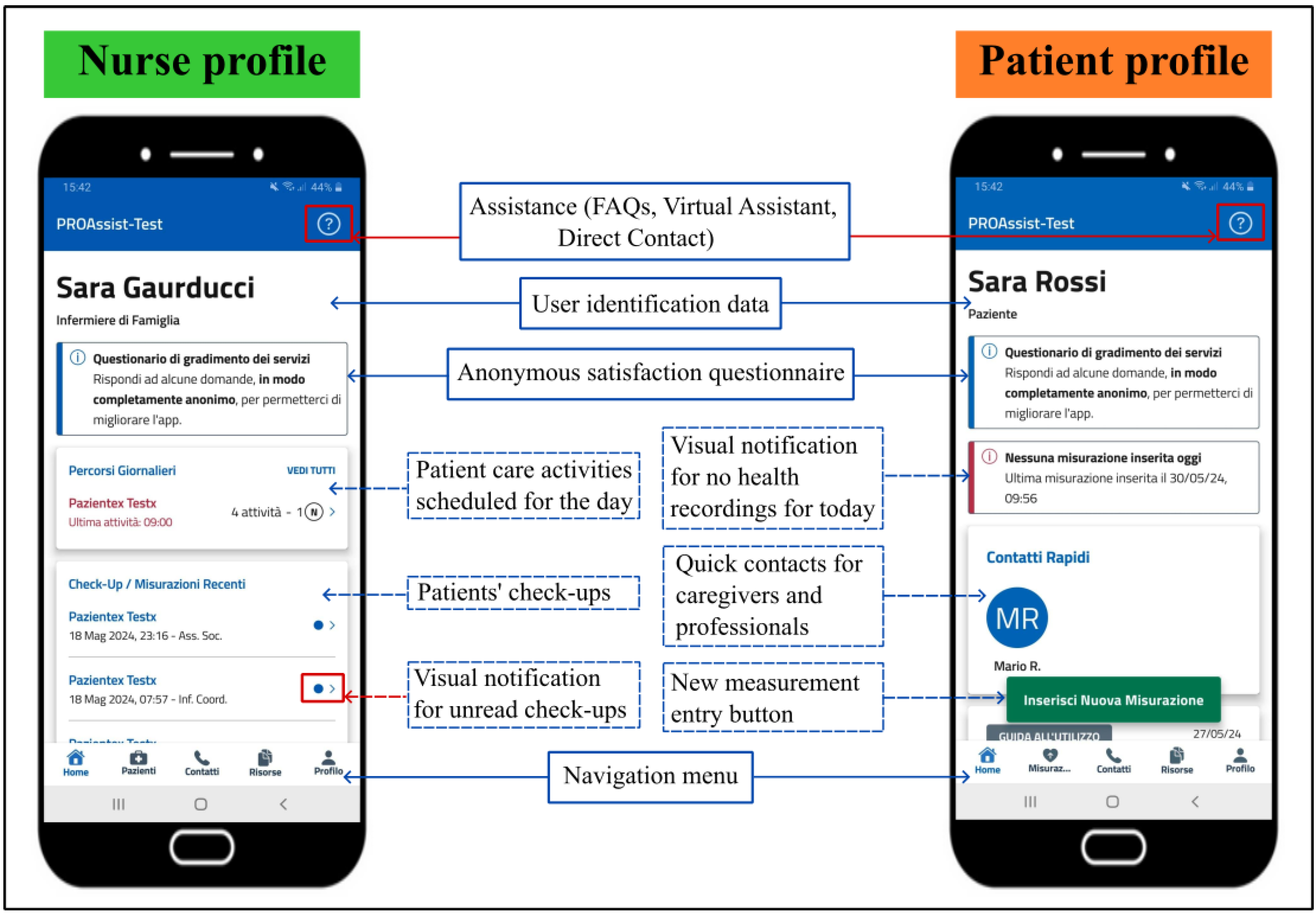
Currently, two distinct profiles have been activated within PROASSIST 4.0 app to deliver services to both patients and nurses (
Figure 5). The patient profile allows patients to insert, view and share their health data, while the FCNs profile offers tailored functionalities for the monitoring and management of patient care. Specifically, in accordance with the necessity for a planning tool for patient care activities emerged from the ongoing dialogue with nurses as app end-users, which constitutes an essential aspect of our smartHUB approach, a patient care planning function has been recently integrated into the nurse profile. Thus, the specific features available include self-monitoring for patients, and professional monitoring and patient care planning for nurses. Below is a more detailed description of these specific functionalities.
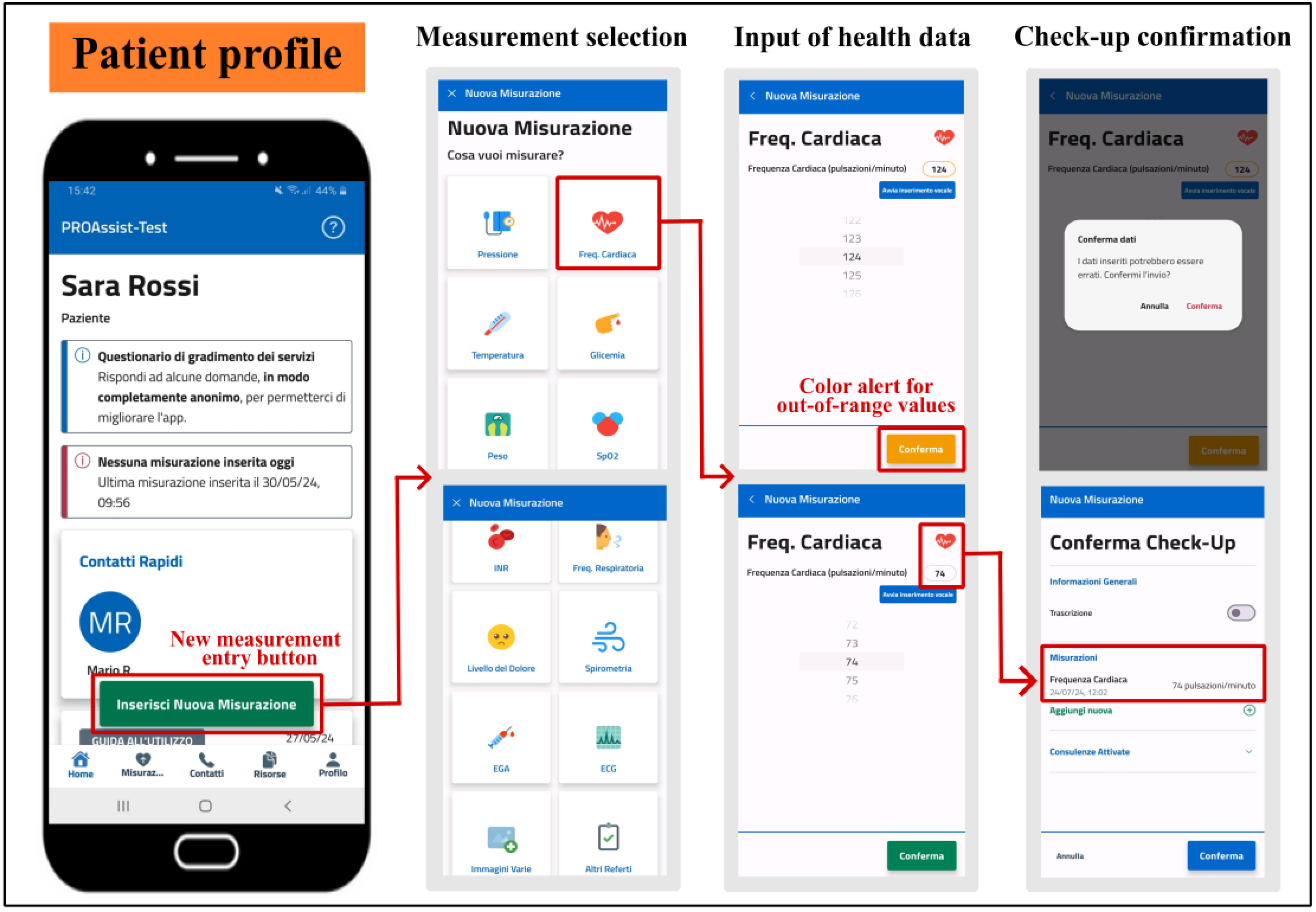
5.2.1. Patient Self-Monitoring
PROASSIST 4.0 app offers several functionalities to support patients in self-monitoring. Health measurements, such as blood pressure, heart rate, body temperature, blood glucose level, body weight, respiratory rate, and oxygen saturation, can be entered in real-time either manually or using voice input, in addition to being recorded through transcription. While inserting a medical measurement, patients are alerted via a color notification if the value entered differs from its physiological range, ensuring immediate awareness of the input of potentially erroneous data (
Figure 6). Additionally, patient self-monitoring check-ups provide the recording of subjective data regarding perceived pain levels, along with the inclusion of medical reports encompassing pulmonary function tests, arterial blood gas analyses, electrocardiograms, and other relevant medical exams or imaging. Information about the management of pressure injuries, wounds and medical devices, either independently or with the assistance of a caregiver, can be also self-reported by the patient in the check-up. Patients are also allowed to graphically view their measurement history containing exclusively self-measurement data, and to apply a time filter to display data ranging from the previous week to the last year. Furthermore, to encourage patient self-assessment, PROASSIST 4.0 app provides visual notifications indicating when no health measurements have been recorded for the day. Finally, the app grants patients access to the contact of their caregivers and healthcare professionals involved in home care. All these features aim to empower patients by facilitating self-monitoring and enhancing their ability to proactively manage their health status.
In this process, nurses have a pivotal role as they act as the primary point of contact with patients and are essential in ensuring the effective adoption and utilization of self-monitoring technologies [
18]. Their close interactions with patients allow them to deliver guidance and support on the optimal use of digital health tools. Furthermore, nurses educate patients on the importance of consistent monitoring and on the accurate interpretation of gathered data. Finally, by fostering a collaborative relationship with patients, nurses promote trust and encourage patient engagement. When patients feel supported and understood, they are more inclined to adhere to their care plans and actively participate in managing their health [
19].
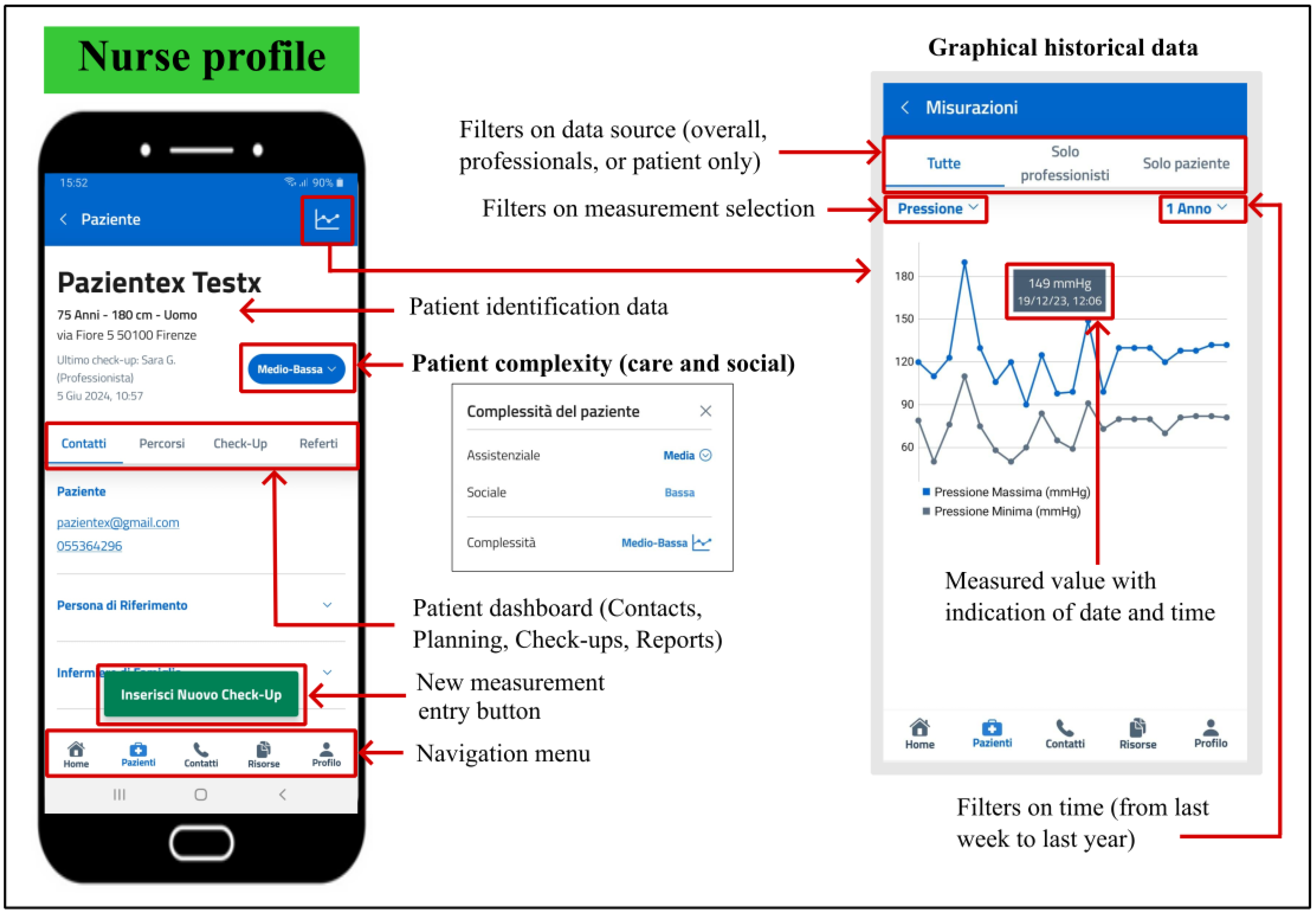
5.2.2. Professional Monitoring
The application we developed provides a large range of functionalities designed specifically for the FCNs profile. After logging in, nurses can view a personalized list of their own patients and access to their profiles and check-ups. Unread check-ups recently conducted by other healthcare professionals, as well as any variations in patient complexity and the number of patient care activities scheduled for the day, are indicated through a visual notification.
When conducting patient check-ups, nurses can enter medical measurements and reports either in real-time, through manual input or voice entry, or via transcription, as those previously described in the patient’s self-monitoring. However, professional check-ups encompass not only such metrics, but also additional notes on the oxygen therapy values, the presence of stoma and tracheostomy tube, the activation of palliative care pathways, along with information about the management of pressure injuries, wounds and specific medical devices (e.g., catheters, vascular access and ventilation devices, PEG, nasogastric or feeding tubes), indicating whether these tasks were conducted with the consultation of another healthcare figure. Professional monitoring check-ups also include a comprehensive subjective assessment of the patient’s overall health condition, as well as an insight into the social context of the patient, regarding the educability and availability of the family or caregiver, and the patient’s autonomy-status (whether autonomous, autonomous with aids, or non-autonomous). Furthermore, interactions that have occurred with other healthcare providers, such as general practitioners or physiotherapists, are also documented in the check-up, which can be entered in real-time or through transcription. For each patient, nurses can visualize historical data in a graphical format, with the option to apply filters on both data source (overall, professionals, or patient only) and time (from last week to last year) (
Figure 7). Finally, PROASSIST 4.0 app provides access to patients’ contacts, including those of caregivers.
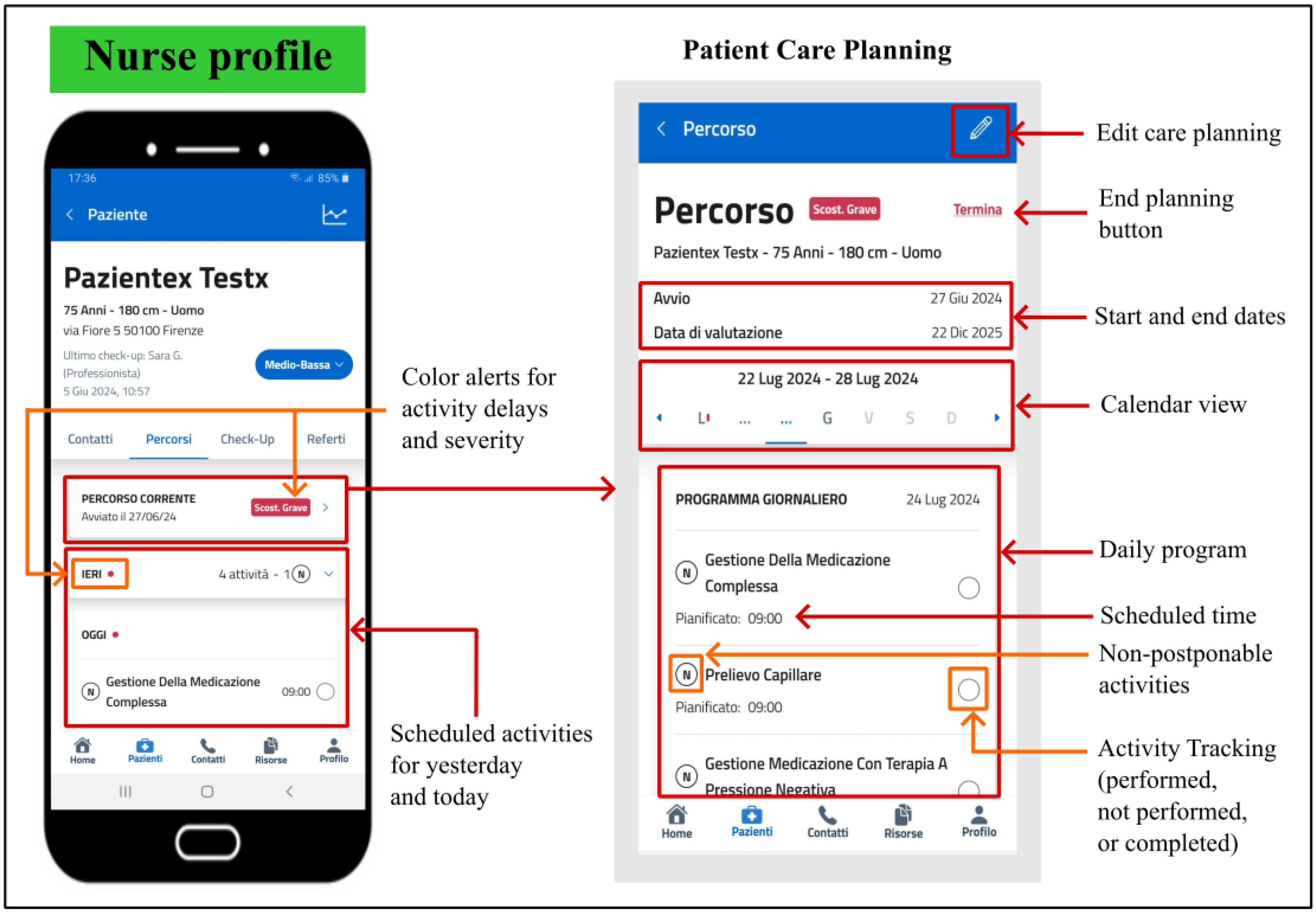
5.2.3. Patient Care Planning
In addition to providing nurses with the capability to collect important information for monitoring patients’ health status, PROASSIST 4.0 app promotes a comprehensive patient care management thought the patient care planning, a specific feature that enables healthcare professionals to create a periodic schedule of all the activities necessary for patient care. Designing home care services involves the challenging task of scheduling patient visits within a planning horizon (typically one week) and determining the daily route for each operator on the number of patients requiring services, their complexity and care load. By monitoring and mapping the patient care journey, the app can offer a detailed overview of completed actions, ongoing tasks, and existing gaps.
For each of their patients, nurses can establish a personalized care pathway by recording all required activities in a calendar, including the designated times and desired frequency for each task. All scheduled activities entered by the nurse appear in the daily program of the patient care pathway, which remains always modifiable and can be interrupted at any time within the app. Specifically, nurses can view the detailed daily program starting from the current week and extending to subsequent weeks, where days with planned activities are marked in a different colour. To facilitate a quick overview of the activities to be performed, each patient card includes a section displaying the scheduled tasks for yesterday, today, and tomorrow. The number of activities that cannot be postponed is indicated. During daily home care, nurses record in the app whether the activity was performed, not performed (specifying the reason), or if they intend to complete the activity and remove it from the periodic schedule. In case of unperformed activities, these can be rescheduled by the nurse according to patient’s needs and nurse’s workload. Furthermore, a color-coded notification indicates if an activity has been completed later than the initially planned time and the severity of the delay is reported (
Figure 8).
All these features aim to provide an efficient automated planning for patient care management with the ultimate goals of minimizing costs, times, and transportation distances for operators; equitably distributing the workload among operators; and maximizing the number of visits conducted and patient preferences.
6. Experimental Activities
6.1. Preliminary Results for System Tuning
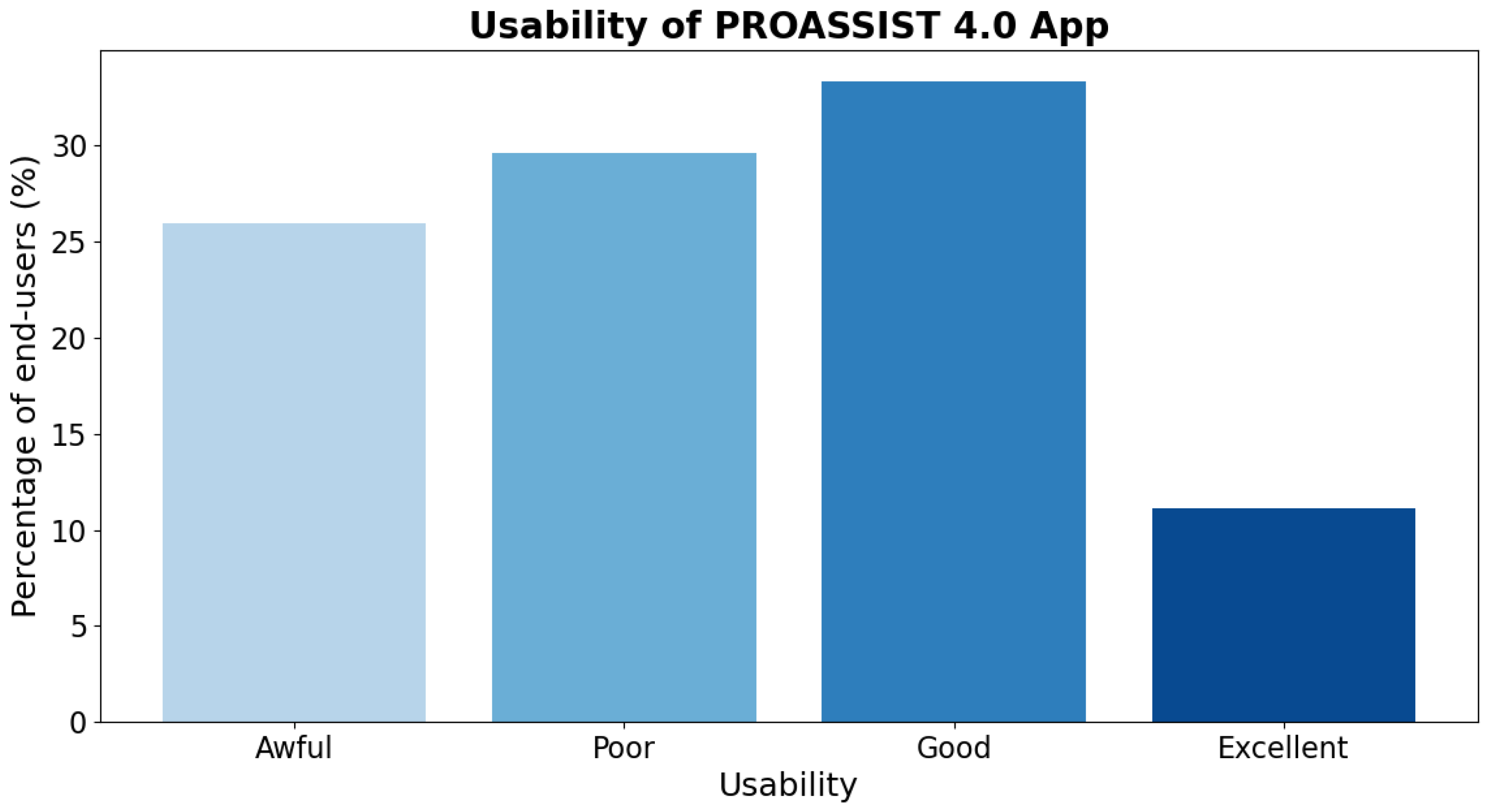
Our initial findings regarding the use of PROASSIST 4.0 app arise from our last workshop with FCNs, during which the initial co-designed version of the app was introduced and assessed. We aimed to collect preliminary feedback on the app’s professional monitoring functionality, which is essential for subsequent system refinements. Early results suggested that, despite still being in a development and refinement phase, PROASSIST 4.0 app demonstrated an overall good functionality [
17]. Specifically, for the majority of nurses involved, the app achieved a good level of usability, with a small percentage of users rating it as excellent. However, some users expressed that there is still potential for improvement in app usability (
Figure 9).
To enhance app usability, we collected feedback on areas for improvement. The desired features identified through discussions with nurses are detailed in
Table 1. Some of theme (i. e., voice data entry, assistance, resources, and in-app questionnaire) have already been implemented into the latest release of the app, which will be used in the next testing phase involving both nurses and patients. For other features (i. e., nurse-to-nurse patient transfer, offline use, system integration and interprofessional communication, and multilingual accessibility), development is planned for the future.
We expect that refining the system based on feedback from nurses will significantly enhance app usability, especially when evaluated in a real operational context — as will be done during the upcoming validation of PROASSIST 4.0 system — rather than during a single workshop session, where time constraints may not afford a comprehensive understanding of the app’s true usability.
6.2. Upcoming Full-Scale Validation of PROASSIST 4.0 System
The first phase of future experimental activities encompasses a validation study that will have a total duration of 60 days. This constitutes a prospective observational pilot study aimed at refining the functionalities of the health digital app we proposed, which, to date, has been developed exclusively within a theoretical testing environment. The final product will serve as a support for healthcare providers and caregivers in assisting patients at their home, and will also be available through territorial services to all those who require it. Specific objectives of this validation study will be as follows:
- (1)
To assess acceptability and usability of PROASSIST 4.0 app in a real-life operational context that involves patients receiving community care services and home-visit nurses;
- (2)
To analyze the feedback collected from patients in order to refine the basic functionalities and enhance usability of the app, thereby increasing acceptability among end-users.
Approximately 120 patients and 20 FCNs of the LHU Toscana Centro will be recruited on a voluntary basis. Patients will be evaluated and enrolled within their living environment during their scheduled home visits as part of their care plan. Inclusion criteria will include: i) being under the care of the identified FCNs district; ii) having a smartphone or tablet with iOS 15+ or Android 8+ and an internet connection; iii) having familiarity with smartphone and app use; iv) being helped by a caregiver capable of entering data in case of patients with limited digital skills; and v) being at least 18 years old. Enrolled patients will provide written informed consent, and FCNs responsible for their care will provide them a prototype of PROASSIST 4.0 app to install on their smartphone or tablet, along with a detailed explanation of its functioning. Patients will be requested to use the app to input their health data throughout the study period and will continue to receive their standard care treatments according to their care plan. It will be emphasized that the experimentation is purely functional and lacks any clinical care aspect. Specifically, it will be highlighted that health data entered by patients will not undergo a clinical evaluation and any anomalies identified during the measurements should be directed to competent healthcare professionals.
PROASSIST 4.0 app functionalities that will be evaluated in this phase are patient self-monitoring and professional monitoring by FCNs. These two features constitute the core capabilities of our app, as they allow health measurements and data monitoring for both patients and nurses. The patient care planning functionality represents a highly customized feature that directly responds to specific healthcare needs and extends beyond basic functionalities. Therefore, this feature will be separately tested in a later phase.
To assess the acceptability and usability of PROASSIST 4.0 app for both patient and nurse interfaces, specific variables will be evaluated: total number of measurements, total measurements per patient, total measurements per parameter, total measurements per parameter per patient, number of support requests, and total registrations. Furthermore, an anonymous in-app questionnaire will be completed by both patients (or caregivers) and nurses in order to collect the following information:
sociodemographic characteristics of app users;
digital literacy of app users, to evaluate their level of knowledge about the use of smartphone and tablet in daily life;
app usability, assessed through the System Usability Scale [
17,
20,
21];
app functionality, evaluated through technical indicators specifically developed to assess specific features of the application, such as data collection, health monitoring, and data visualization.
The questionnaire will be completed in a pseudonymized manner using an alphanumeric code. As previously described, all data will be processed with consistency and responsibility, ensuring full compliance with the GDPR. Information collected will be utilized to evaluate the ease of use, comprehensiveness, and accuracy of PROASSIST 4.0 app. This will support app developers in addressing any issues encountered during the experimentation phase and in the ultimate refinement of the system.
6.3. Future Validation of Patient Care Planning Functionality
Given the recent advancements in the development of our app, particularly with the integration of the patient care planning functionality, and recognizing the importance of this feature for FCNs, we are planning to conduct a series of experimental sessions focused on evaluating both the usability and effectiveness of this new feature.
This preliminary validation will provide valuable insights and feedback, which will be pivotal for the ongoing refinement of the app. The information gathered will play a crucial role in guiding enhancements to ensure that the app effectively meets the real needs of healthcare assistance management.
7. Discussion and Challenges
In this study, we introduced the smartHUB approach, an innovative multidisciplinary systemic methodology designed to address the specific needs of community healthcare assistance of LHU Toscana Centro and ultimately enhance patient care and quality of life. Within the scope of the smartHUB project, PROASSIST 4.0 system has been developed to provide real-time personalized patient management for advanced territorial care. Specifically, PROASSIST 4.0 system includes a mobile application named PROASSIST 4.0 app, designed for the collection and sharing of medical information regarding patients’ health. This app is currently available for both patients and nurses, providing self-monitoring functionalities for patient, as well as professional monitoring and patient care planning functionalities for nurses.
A fundamental aspect of our approach deals with the early engagement of end-users in the developmental of the final solution, from the initial phase of identification and analysis of needs and extending throughout the entire design process. This critical aspect of our methodology stems from the understanding that continuous involvement of end-users in the development and implementation stages is essential for identifying factors that influence app acceptability and practical use [
22,
23]. For example, insufficient app usability can adversely affect the adoption of the technology and potentially compromise patient health. Conversely, enhanced usability is closely associated with user satisfaction, leading to broader adoption of the tool, which can significantly improve community healthcare assistance and the quality of life of patients [
24,
25]. Thus, the development of PROASSIST 4.0 app is guided by users’ feedback to ensure the optimization of app ease of use.
Although initial feedback from nurses revealed that not all end-users were fully satisfied with app functionality [
17], we are confident that our ongoing engagement with nurses and patients will result in improvements that will enhance app utilization and usability in future assessments. Targeted training designed to raise community awareness about the benefits of the customized 4.0 approach will also contribute to foster active participation and ownership of the proposed methodology in both patients and nurses, which is essential for its success. Furthermore, adequate training and support programs will be crucial to empower end-users with the necessary digital literacy and skills to effectively utilize ICT tools.
Successfully implementing the system requires acknowledging and addressing the complex challenges and barriers it presents. Key issues include interoperability among various systems, data security, and infrastructure limitations [
18]. Interoperability is critical for the seamless exchange of patient information across different platforms. Without it, the coordination and continuity of patient care can be compromised. Equally important are robust data security measures to protect sensitive patient information from breaches and cyber threats. Electronic health records are particularly susceptible to cyberattacks, highlighting the need for strong encryption and access controls to maintain data privacy and security, which remains a major concern for the adoption of technological solutions [
26]. Furthermore, inadequate infrastructure, such as outdated hardware, limited bandwidth, or unreliable internet connectivity, can significantly impede the efficient operation of ICT systems. These limitations may cause delays in accessing patient data or lead to system crashes, thereby negatively impacting nurses’ ability to provide timely care. Addressing these technical challenges necessitates concerted efforts in standardization, significant investment in robust IT infrastructure, and ongoing technological advancements.
Ethical complexities are closely interlinked with technical considerations [
18]. Maintaining patient privacy and confidentiality remains a paramount concern in the digital era. Nurses face the delicate challenge of balancing the use of patient data to enhance care outcomes with respecting individual autonomy and privacy rights. To mitigate the risks of data misuse and violations of trust, it is imperative to rigorously adhere to ethical frameworks and guidelines on data sharing and patient consent.
Finally, future efforts will focus not only on developing new features that effectively meet users’ needs but also on integrating innovative technological solutions based on emerging technologies for the remote health monitoring of patients. Different data collection systems, including wearable sensors, could be employed to monitor and record real-time information about physiological signs and physical activity levels [
27]. Integrating these technologies into our system could significantly enhance patient care through continuous monitoring of critical health parameters, enabling the detection and diagnosis of relevant health conditions at their early onset. Also, real-time monitoring could facilitate more accurate and timely interventions. This integration would not only empower patients with greater control over their health status but also enable healthcare providers to deliver more personalized and proactive care programs.
8. Conclusions
In conclusion, we presented the development of an ICT platform called PROASSIST 4.0, specifically designed to enhance community healthcare management of the LHU Toscana Centro. By adopting the smartHUB multidisciplinary methodology, which prioritizes the creation and implementation of ICT tools based on end-users’ needs, we developed a highly customized app that integrates patient monitoring (including self-monitoring), real-time health data collection and processing, patient care planning, and decision support for healthcare professionals. This solution not only increases patients’ awareness of their health status, making them active participants in their care journey, but also supports nurses in delivering patient-centered care. Our work highlights the importance of addressing healthcare needs and challenges with innovative solutions aimed at fostering a more connected and efficient healthcare environment.
Author Contributions
The authors contributed equally to this work based on their background. The paper is a result of co-creation activities carried out following a multidisciplinary approach. Background, motivation and application context, C.B., M.A., M.P. and P.Z.; requirements, system and experimental activities, S.J., S.G., L.M. and S,C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by: the European Telecommunication Standard Institute (ETSI), Smart Body Area Networks (SmartBAN) Technical Committee, the European Union’s Horizon 2020 programme under grants No. 872752 and No. 101017331, and Fondazione Cassa di Risparmio di Firenze (project: smartHUB on Medical & Social ICT for Territorial Assistance).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank the smartHUB partners.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Schmidt, S.; Hemmestad, L.; MacDonald, C.; Langberg, H.; Valentiner, L. Motivation and barriers to maintaining lifestyle changes in patients with type 2 diabetes after an intensive lifestyle intervention (the U-TURN trial): a longitudinal qualitative study. International Journal of Environmental Research and Public Health 2020, 17, 7454. [Google Scholar] [CrossRef] [PubMed]
- Roche, P.; Shimmin, C.; Hickes, S.; Khan, M.; Sherzoi, O.; others. Valuing All Voices: refining a trauma-informed, intersectional and critical reflexive framework for patient engagement in health research using a qualitative descriptive approach. Research Involvement and Engagement 2020, 6, 1–13. [Google Scholar] [CrossRef]
- Islam, S.; Joseph, O.; Chaudry, A.; Forde, D.; Keane, A.; others. “We are not hard to reach, but we may find it hard to trust”… Involving and engaging ‘seldom listened to’ community voices in clinical translational health research: a social innovation approach. Research Involvement and Engagement 2021, 7, 46. [Google Scholar] [CrossRef] [PubMed]
- Wesson, D.; Kitzman, H. How academic health systems can achieve population health in vulnerable populations through value-based care: the critical importance of establishing trusted agency. Academic Medicine 2018, 93, 839–842. [Google Scholar] [CrossRef] [PubMed]
- Meskó, B.; Drobni, Z.; Bényei, E.; Gergely, B.; Győrffy, Z. Digital health is a cultural transformation of traditional healthcare. Mhealth 2017, 3. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.; Yang, S.; Yuan, J.; Xu, L.; Zhao, X.; others. Patients with chronic illness urgently need integrated physical and psychological care during the COVID-19 outbreak. Asian Journal of Psychiatry 2020, 51, 102081. [Google Scholar] [CrossRef] [PubMed]
- Bours, S.; Wanzenböck, I.; Frenken, K. Small wins for grand challenges. A bottom-up governance approach to regional innovation policy. European Planning Studies 2022, 30, 2245–2272. [Google Scholar] [CrossRef]
- Wilde, M.; Garvin, S. A concept analysis of self-monitoring. Journal of advanced nursing 2007, 57, 339–530. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Morris, M.; Davis, G.; Davis, F. User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Barchielli, C.; Marullo, C.; Bonciani, M.; Vainieri, M. Nurses and the acceptance of innovations in technology-intensive contexts: the need for tailored management strategies. BMC Health Services Research 2021, 21, 639. [Google Scholar] [CrossRef]
- Abril-Jiménez, P.; Merino-Barbancho, B.; Fico, G.; Martín Guirado, J.; Vera-Muñoz, C.; others. Evaluating IoT-Based Services to Support Patient Empowerment in Digital Home Hospitalization Services. Sensors 2023, 23, 1744. [Google Scholar] [CrossRef]
- Anik, F.; Sakib, N.; Shahriar, H.; Xie, Y.; Nahiyan, H. ; others. Unraveling a blockchain-based framework towards patient empowerment: A scoping review envisioning future smart health technologies. Smart Health, 1004. [Google Scholar] [CrossRef]
- Mahawan, T.; Luckett, T.; Mielgo, I.; Pornputtapong, N.; Caamaño Gutiérrez, E. Harnessing Predictive Power: Exploring the Crucial Role of Machine Learning in Early Disease Detection. JURIHUM: Jurnal Inovasi dan Humaniora 2023, 1, 302–315. [Google Scholar] [CrossRef]
- Alowais, S.; Alghamdi, S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.; others. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Medical Education 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- François, J.; Audrain-Pontevia, A.; Menvielle, L.; Chevalier, N. Empowering health care consumers in the era of internet of things. International Journal of Consumer Studies 2023, 47, 1060–1075. [Google Scholar] [CrossRef]
- Keys, R.; Marshall, P.; Stuart, G.; O’Kane, A. "I think it saved me. I think it saved my heart": The Complex Journey From Self-Tracking With Wearables To Diagnosis. Proceedings of the CHI Conference on Human Factors in Computing Systems, 2024, pp. 1–15.
- Jayousi, S.; Barchielli, C.; Alaimo, M.; Guarducci, S.; Caputo, S. ; others. Improving Community Healthcare Assistance Through an Innovative and Multidisciplinary Systemic Approach. 18th International Symposium on Medical Information and Communication Technology (ISMICT), 2024.
- Jayousi, S.; Barchielli, C.; Alaimo, M.; Caputo, S.; Paffetti, M.; others. ICT in Nursing and Patient Healthcare Management: Scoping Review and Case Studies. Sensors 2024, 24, 3129. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Carayon, P. Health Care 4.0: A vision for smart and connected health care. IISE Transactions on Healthcare Systems Engineering 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Brooke, J. SUS: A “quick and dirty” usability scale; Taylor & Francis, 1996; pp. 189–194. In: P. W. Jordan, B. Thomas, I. L. McClelland, B. Weerdmeester, eds. Usability evaluation in industry.
- Bangor, A.; Kortum, P.; Miller, J. An empirical evaluation of the system usability scale. International Journal of Human-Computer Studies 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Anderson, K.; Burford, O.; Emmerton, L. Mobile health apps to facilitate self-care: a qualitative study of user experiences. PloS one 2016, 11, e0156164. [Google Scholar] [CrossRef]
- Peng, W.; Kanthawala, S.; Yuan, S.; Hussain, S. A qualitative study of user perceptions of mobile health apps. BMC Public Health 2016, 16, 1158. [Google Scholar] [CrossRef]
- Ebnali, M.; Shah, M.; Mazloumi, A. How mHealth apps with higher usability effects on patients with breast cancer? 2019 International Symposium on Human Factors and Ergonomics in Health Care, 2019, Vol. 8, pp. 81–84. [CrossRef]
- Feng, L.; Wei, W. An empirical study on user experience evaluation and identification of critical UX issues. Sustainability 2019, 11, 1–19. [Google Scholar] [CrossRef]
- Lluch, M. Healthcare professionals’ organisational barriers to health information technologies—A literature review. Int. J. Med. Inform. 2011, 80, 849–862. [Google Scholar] [CrossRef] [PubMed]
- Majumder, S.; Mondal, T.; Deen, M. Wearable Sensors for Remote Health Monitoring. Sensors (Basel) 2017, 17, 130. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).