A 58 year-old female patient presented to the Emergency Department of General Hospital of Katerini in Pieria, Greece, wiht complains of abdominal pain, vomiting and constipation. She reported no history of previous abdominal surgery, had no significant medical history and was not taking any specific medication. Laboratory tests indicated an elevated white blood cell count of 18.24x103/μL and C-reactive protein values of 29.83 mg/dL. Her complete blood count (CBC) at admission is shown in
Table 1. Physical examination revealed abdominal distension, guarding and rebound tenderness.
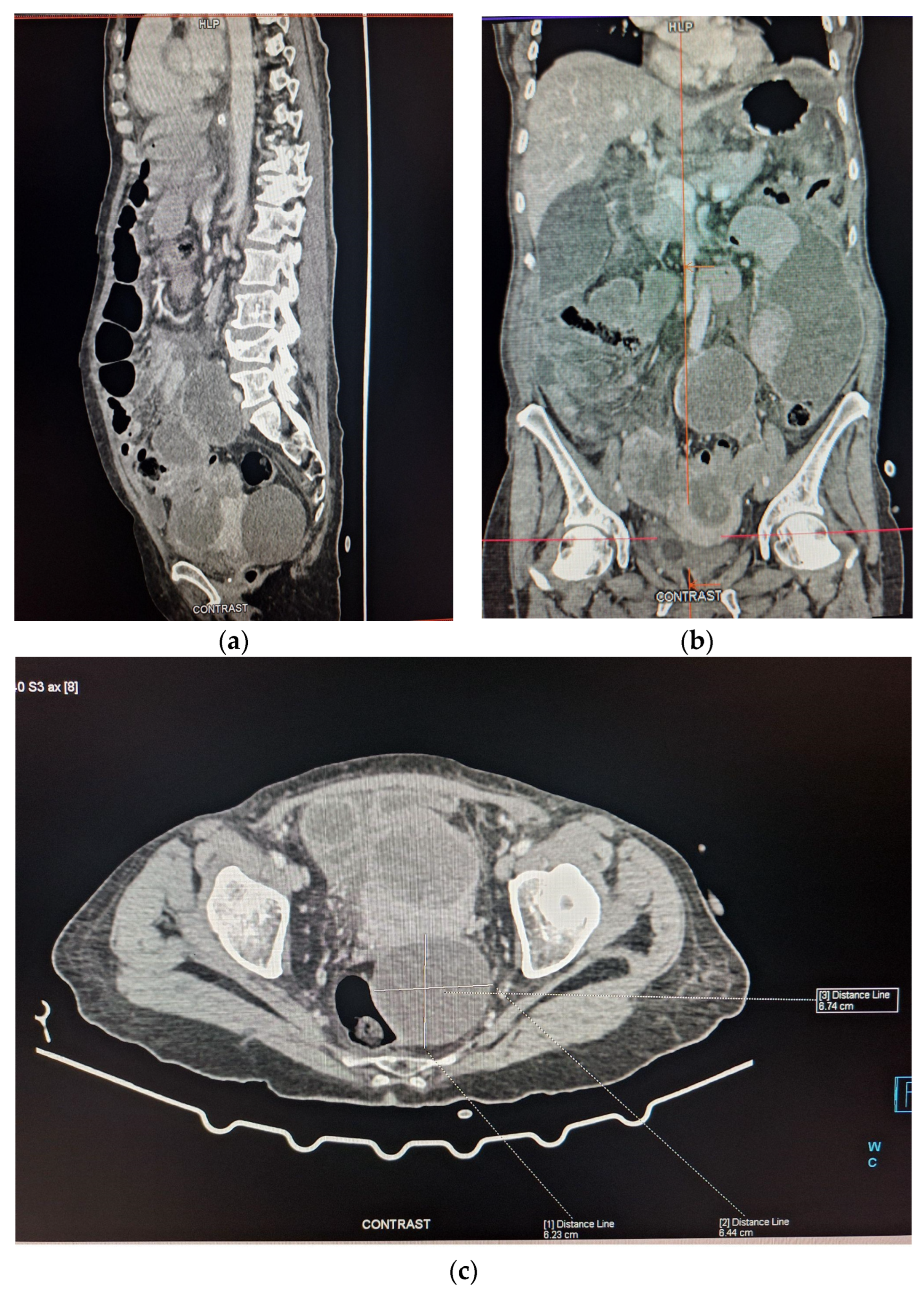
The patient was admitted to the Surgical Ward and underwent a Computered Tomography (CT) scan, with oral Gastrografin contrast, which revealed two abscess cavities - one below the right hemidiaphragm and one in the left paracolic gutter, generalized distension of her small bowel, a large cystic mass in the right ovary and multiple peritoneal implants (
Figure 1a–c). Due to the presence of peritoneal implants a preliminary diagnosis of ovarian cancer with generalized peritoneal carcinomatosis was made. Initial treatment was conservative, consisting of intravenous fluids, a nasogastric tube and antibiotics. Two days later, with no improvement in the patient’s clinical condition, a second abdominal CT scan was performed, again demonstrating distended small bowel loops with no distal contrast passage. Following discussions with the patient and her family, and consultations among the medical, surgical and gynecological teams, the following day, the decision was made to proceed with a laparotomy the following day.
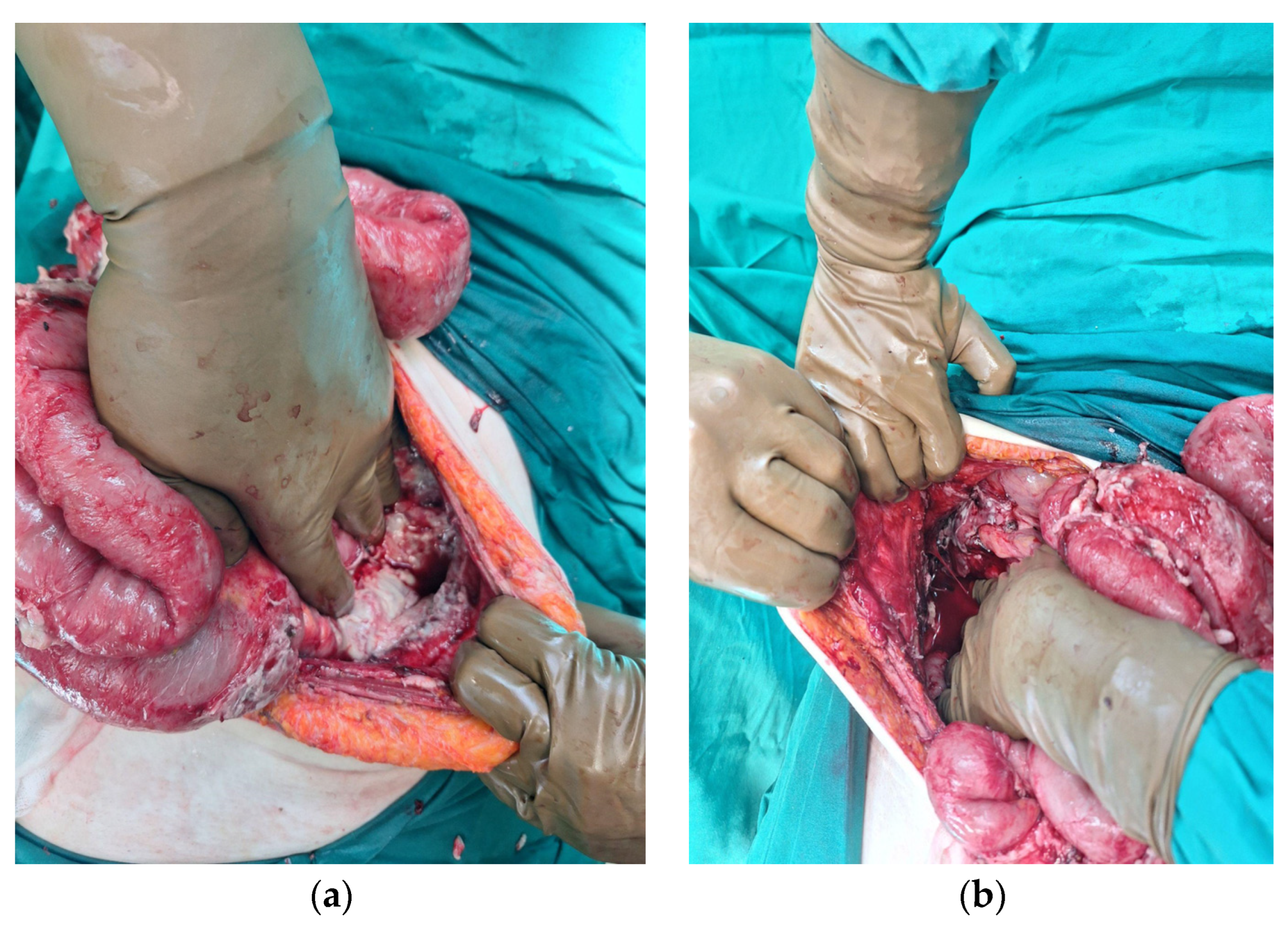
During the laparotomy, generalized peritonitis was observed characterized by a large amount of fibrinous exudate and free purulent fluid. The small bowel was significantly dilated due to obstruction caused by multiple inflammatory adhesions. The adhesions were lysed and the peritoneal cavity was thoroughly explored. No signs of peritoneal carcinomatosis or point of small bowel obstruction were found. However a cystic formation protruding from the right ovary was identified, with a rupture in its wall through which purulent fluid was leaking (
Figure 2).
Two abscess cavities were identified: one located below the right hemidiaphragm and another in the left paracolic gutter (
Figure 3a,b). A lavage of the peritoneal cavity was performed, along with an en-bloc salpingo-oophorectomy and resection of the cystic formation. The cystic formation was submitted for histopathological examination. Due to the excessive small bowel dilation and the presence of small bowel ileus, a prophylactic loop ileostomy was installed in the right abdominal wall.
The patient had an uncomplicated postoperative course and awaited for her histopathology results, which confirmed the presence of a dermoid ovarian cyst. No evidence of malignancy was found.
Discussion
A dermoid ovarian cyst is the most common form of benign ovarian tumor [
1,
2,
3]. These tumors are often asymptomatic and typically cause symptoms only when enlarge or become complicated [
1]. Complicated ovarian cysts can be severe life threatening events, with ovarian torsion (16%) being the most common. Relatively less frequent complications include cystic rupture (1-2%), infection (1%) or malignant transformation (2%) [
1,
2]. A bowel involvement is particularly rare, with only a few cases documented in the literature [
4]. Dermoid ovarian tumors may lead to bowel obstruction or the formation of an entero-ovarian fistula,both of which are infrequently reported in the literature [
1,
4]. A perforated ovarian cyst can cause acute peritonitis and subsequent to obstructive ileus of the small bowel [
2].
Li et al. have reviewed the literature and found that the size of a dermoid ovarian cyst can contribute to cystic rupture, with most ruptured cysts, including the case presented here, being 6 to 10 cm in diameter [
5].
This case report highlights a rare instance of a perforated ovarian cyst with radiological findings that mimic generalized carcinomatosis. A perforated dermoid ovarian cyst can cause peritonitis [
6] which may present either acutely, with symptoms of acute abdomen and shock [
6], or as in this case, chronically [
7,
8]. Chronic peritonitis due to a perforated dermoid ovarian cyst is more challenging to diagnose due to its subtle and non-specific symptoms [
6]. CT scans are useful in diagnosis revealing characteristic hypoattenuating fat-fluid levels in dependent pockets within the peritoneal cavity, typically below the right hemidiaphragm, which is a pathognomonic finding [
6]. In chronic granulomatous peritonitis, multiple small white peritoneal lesions, dense adhesions, and ascites may mimic carcinomatosis or tuberculous peritonitis [
6]. A Magnetic Resonance Imaging (MRI) scan can be helpful for the differential diagnosis [
8].
Dermoid ovarian cysts identified before rupture are usually managed surgically, either laparoscopically or via laparotomy [
9]. The recurrence rate of mature cystic teratomas is less than 3–4%, with malignancy occurring approximately in 1.7% of the cases [
9]. Recent studies indicate that a laparoscopic removal of ovarian dermoid tumors is a safe approach [
10,
11,
12].
For ruptured dermoid ovarian cysts a surgical intervention is the treatment of choice [
11,
12]. Laparoscopic management can be effective for the treatment of ruptured dermoid ovarian cysts but is best performed by experienced surgeons [
11]. Laparotomy remains the preferred treatment of choice in most cases [
5,
11,
12]. In 2023 Takeda et al. reported that laparoscopic management was feasible in 8 of 9 cases of ruptured dermoid ovarian cysts, except for one case with severe adhesion requiring laparotomy [
12]. For generalized peritonitis, surgical treatment involves unilateral salpingo-oophorectomy and abdominal lavage with complete pelvic and abdominal cavity exploration, peritoneal washing and/or sampling of ascites [
8,
13]. Early surgical intervention can reduce complications, prevent new adhesions and nodules and facilitate a faster recovery [
8].
This case report aims to increase awareness among surgeons and gynecologists regarding the rare occurrence of bowel obstruction due to complicated ovarian cysts. The fluid from a ruptured dermoid ovarian cyst can cause purulent peritonitis and peritoneal thickening, potentially leading to misdiagnosis as peritoneal carcinomatosis. It is crucial for healthcare providers to consider this rare cause of bowel obstruction in the differential diagnosis of patients presenting with relevant clinical and radiological findings.
Author Contributions
Conceptualization, Investigation, Writing—Original Draft Preparation: Ismini Kountouri. Writing—Review and Editing: Ismini Kountouri, Christos Gkogkos, Periklis Dimasis, Ioannis Katsarelas, Amyntas Giotas, Eftychia Kokkali, Miltiadis Chandolias, Nikolaos Gkiatas, Dimitra Manolakaki. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained. None of the data in the paper reveal the patient’s identity.
Data Availability Statement
All relevant data are within the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bhasin SK, MalikSM, SharmaG, GuptaSK.Ovarian dermoid presenting as acute intestinal obstruction: a rare case report and review of literature.Int Surg J2015;2:283-5.
- Nitinavakarn B, Prasertjaroensook V, Kularkaew C. Spontaneous rupture of an ovarian dermoid cyst associated with intra-abdominal chemical peritonitis: characteristic CT findings and literature review. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet. 2006 Apr;89(4):513-517. PMID: 16696398.
- Simillis C, Cribb E, Gurtovaya Y, Pawa N. Generalised purulent peritonitis and small bowel obstruction due to a spontaneously perforated ovarian dermoid cyst. BMJ Case Rep. 2019 Oct 23;12(10):e231729. PMID: 31645380; PMCID: PMC6827800. [CrossRef]
- Esterson YB, Gaballah M, Grimaldi GM, Raj MH, Pellerito JS. Ovarian dermoid cyst complicated by small bowel obstruction, entero-ovarian fistula formation, and malignant degeneration. ClinImaging. 2019 Jul-Aug;56:47-51. Epub 2019 Mar 8. PMID: 30878712. [CrossRef]
- Li, Rebecca Yuan, Nikam, Yogesh, Kapurubandara, Supuni, Spontaneously Ruptured Dermoid Cysts and Their Potential Complications: A Review of the Literature with a Case Report, Case Reports in Obstetrics and Gynecology, 2020, 6591280, 9 pages, 2020. [CrossRef]
- Erbay G. Ruptured ovarian dermoid cyst mimicking peritoneal carcinomatosis: CT and MRI. J Clin Anal Med 2016;6:701-3.
- Rai K, Dhakal B, Shahi S, Pant S, Sapkota S, Timilsina B. Ruptured dermoid cyst of ovary developing into chronic peritonitis; a rare complication diagnosed by contrast CT: A case study. Ann Med Surg (Lond). 2022 Sep 15;82:104700. PMID: 36268424; PMCID: PMC9577650. [CrossRef]
- Jane Chua K, Barr A, Prints M, Ruskin R, Brooks R. Management of ruptured ovarian teratoma mimicking advanced ovarian cancer. Gynecol Oncol Rep. 2024 Mar 31;53:101386. PMID: 38596159; PMCID: PMC11001759. [CrossRef]
-
Multani, Jasmine; Multani, Jasmine; Kives, Sari. Dermoid cysts in adolescents. Current Opinion in Obstetrics and Gynecology 27(5):p 315-319, October 2015. |. [CrossRef]
- Târcoveanu E, Vasilescu A, Georgescu S, Dănilă N, Bradea C, Lupascu C, Cotea E, Crumpei F, Vintili D, Motoc-Vieriu R, Dimofte G. Laparoscopic approach to ovarian dermoid cysts. Chirurgia (Bucur). 2012 Jul-Aug;107(4):461-8. PMID: 23025112.
- Rubod C, Triboulet JP, Vinatier D. Kyste dermoïde de l’ovaire compliqué d’une péritonite chimique. A propos d’un cas [Ovarian dermoid cyst complicated by chemical peritonitis. Case report]. Gynecol Obstet Fertil. 2007 Jul-Aug;35(7-8):651-3. French. Epub 2007 Jun 29. PMID: 17602847. [CrossRef]
- Takeda A, Koike W. Clinical characteristics and laparoscopic surgical outcomes of ovarian dermoid cysts complicated by spontaneous rupture: nine cases and a literature review. J Int Med Res. 2023 May;51(5):3000605231171023. PMID: 37138472; PMCID: PMC10161322. [CrossRef]
- Ayoub M, Touihar S, Ouazni M, Sanae A, Hicham N, Soufi M. Perforated degenerated immature teratoma of the ovary: Rare cause of acute peritonitis, case report and review of the literature. Int J Surg Case Rep. 2024 Aug;121:110003. Epub 2024 Jul 4. PMID: 39024992. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).