1. Introduction
The potential applications of internet and communication technologies for healthcare (eHealth) in primary care settings are being increasingly recognized, particularly their potential to improve access to general practice and medical data. The Saudi Arabia 2030 vision makes a transition towards eHealth provision one of its key targets [
1,
2], and recognizes its potential to improve the quality and accessibility of care and empower patients [
3]. Saudi Arabia is a leading country in the field of eHealth among the Gulf countries. Saudi Arabia leads in the percentage of households with an Internet connection and broadband connection and has the highest percentage of people who are regular Internet users and who use eGovernment services. Recent published reviews examined the current status and progress of eHealth applications in Saudi Arabia [
2,
4,
5] and found that eHealth services have been implemented in primary care centers (PCs). Most PCs offered at least one or two eHealth services to their patients by which they could contact their doctors or the general practice, such as booking an online appointment or asking healthcare professionals a question.
Such a transition towards eHealth is anticipated to lead to higher efficiency, better care quality and improved patient satisfaction [
6,
7,
8,
9,
10,
11,
12]. The use of internet-based messaging systems, for instance, has been found to reduce in-person visits, to aid communication between patients and their healthcare providers, and to be received favorably by patients, who find such systems helpful and convenient to use [
11,
13,
14]
Despite these potential benefits of eHealth, research has found that such services are yet to become a routine part of healthcare systems, and that patients do not routinely use or accept them [
15,
16,
17]. In the Saudi context, Alshammari has found that uptake of such systems in healthcare settings is slower than predicted, despite the emphasis the government has placed on their implementation [
2]. Lack of awareness of the application of eHealth services among main users including patients could be considered a factor affecting this low uptake. Patients’ lack of intention to use such technologies also has been proposed as another possible reason for this slow uptake [
2,
7,
18]. It is essential to gain insights into patients’ actual use and intention toward using to improve adoption and use of such services.
To understand how willing patients are to use a particular eHealth service, several factors have to be considered, which may be social, psychological and/or physical, in addition to patients’ particular needs [
15]. Understanding these factors can also help improve the adoption and use of such services in the future [
15].
The technology acceptance model (TAM) is considered the most robust means to assess acceptance of a new technology [
19]. According to the TAM model, potential users' beliefs about perceived usefulness and ease of use are the main factors that can predict users' intention to use a given technology [
19]. Subsequent studies have extended TAM to incorporate additional constructs, most notably the unified theory of acceptance and use of technology (UTAUT), which adds two further constructs: social influence and facilitating conditions, as well as a range of social factors that might influence intention to use [
20]. A review by Or and Karsh (2009) suggests that the influence of patient trust should be further explored, as this has been established as a reliable predictor of acceptance outside of healthcare settings [
15]. In addition, several other studies have also emphasized the importance of considering patient attitudes towards and intention to use a new technology [
21]. This study therefore utilized the UTAUT model, along with considering trust and attitude, to enhance the understanding of technology acceptance factors, as these have been emphasized as important predictors of technology acceptance in previous research [
15,
21].
Despite the adoption of eHealth being prioritized internationally, there have been few studies into patients’ intention to use such technologies in primary care globally [
7,
14], and none specifically examining Saudi Arabia or the wider Gulf region [
2,
4,
22]. Given the multiple potential benefits of eHealth, it is important to invest in this topic. The aim of this research is therefore to investigate Saudi patients’ actual use and awareness of the availability of 7 key eHealth services in PCs and to examine their intention to use such services. The second objective of the study is to explore what factors and characteristics impact on patients’ intention to use eHealth patients’ use of and attitude toward two eHealth services: online appointment booking and asking a question via the care center website or app. These were selected due to their relative simplicity and their potential for common adoption within primary care.
2. Methods
Design and Participants
This research utilized a cross-sectional study design. Questionnaires were given to participants in the main/biggest PC in Riyadh, the capital city of Saudi Arabia, and its largest population center. The PC are open 24 hours per day, 7 days per week and treat patients from across the city.
Participants were recruited from Feb 2022 – Aug 2022, using systematic random sampling, whereby the study researcher spoke with every third person who entered the waiting area at the PC to assess their interest in participating and their suitability. The inclusion criteria were adults, aged 18 years and over, who had contacted their PCs at least once in the year prior to sampling. Prior to their participation, participants’ informed consents were obtained. Ethical approval for conducting this study was obtained (reference#21-518E).
According to statistics from the Saudi Ministry of Health (MOH), the number of Saudi visitors to PCs in Riyadh City was 7,372,405. Given the size of this population the sample size was set at 385 participants, giving a confidence interval of 95%, a 0.05 alpha error, ± 5% accuracy, and power of 80%. This sample size was calculated using the Raosoft Sample Size Calculator. The target sample size for this study, therefore, ranges from 600 to 1200 eligible people, ensuring a higher level of precision and reliability in the findings.
Measurements
Questionnaire
The questionnaire that was used to establish respondents’ actual use of eHealth and their intention to use such services is derived from previous research, where it has been utilized successfully [
7,
14]. It consists of 3 main sections: Participants’ characteristics; Use, Intention to use and Availability of eHealth services; and Factors affecting their intention to use.
The questionnaire was translated into Arabic and then validated according to the WHO Process of translation and adaptation of instruments.
Participants’ Characteristics
Data on participant characteristics were gathered, including their gender, age, education level, geographical location within Riyadh, their internet use, and whether they rate the internet as difficult or easy to use.
Use and Intention to Use and Availability of Internet Services
The questionnaire collected data on participants’ actual use of eHealth, their awareness of the existence and availability of such services, and their intention to use such services when communicating with their healthcare providers about the following:
1) appointment booking using website/app; 2) receiving SMS appointment reminders; 3) asking questions of healthcare professionals using website/app; 4) taking home measurements of vital signs including blood pressure and weight, and sending these to a healthcare professional via website/app; 5) requesting repeat prescriptions via website/app; 6) accessing their medical data online; 7) video consultation via the app/web.
Factors Influencing Intention to Use eHealth Services
To understand which factors influence the participants’ intention to use two eHealth services: (1) appointment booking using website/app and (2) asking questions of healthcare professionals using website/app, participant were asked to rate several items divided according to 6 subscales based on the UTAUT model as well recommendations from studies by Or and Karsh (2009) and Spil and Schuring (2006) [
15,
21]. These subscales were: effort expectancy, trust, attitude, facilitating conditions, social influence, and performance expectancy.
Data Analysis
Descriptive analyses were used to calculate participant characteristics and to examine participants’ actual use, intention toward using, and awareness of availability regarding the 7 eHealth services.
The strong correlations between the six subscales indicate strong multicollinearity (Table 2 and Table 3). As a consequence, a multiple regression analysis is not possible. Instead, a simple linear regression analysis was performed to explore how each subscale and the personal characteristics age, gender and education level relate to the intention to use the two services.
3. Results
Out of 1650 participants approached, 1250 responded to the questionnaire. Among these 1250 respondents, 47 participants were excluded because they did not complete all of the questionnaire items regarding their use, intentions and awareness of the internet services. Therefore, the total number of participants included is 1203. Table 1 shows participant characteristics for the study (n=1203).
Table 1.
Participants Characteristics (n=1203).
Table 1.
Participants Characteristics (n=1203).
| |
Mean (SD) or n (%) |
| Age in years |
43.7(17.1) |
| Gender |
|
| Male |
535(44.5|%) |
| Female |
668(55.5%) |
| Level of education |
|
| Low |
479 (39.8%) |
| Medium |
698 (58.0%) |
| High |
26 (2.2%) |
| Internet usage (years) |
|
| <1 |
201(16.7%) |
| 1-3 |
614 (51.0%) |
| >3 |
388(32.3%) |
Use, Intention to Use, and Awareness of Availability of Internet Services
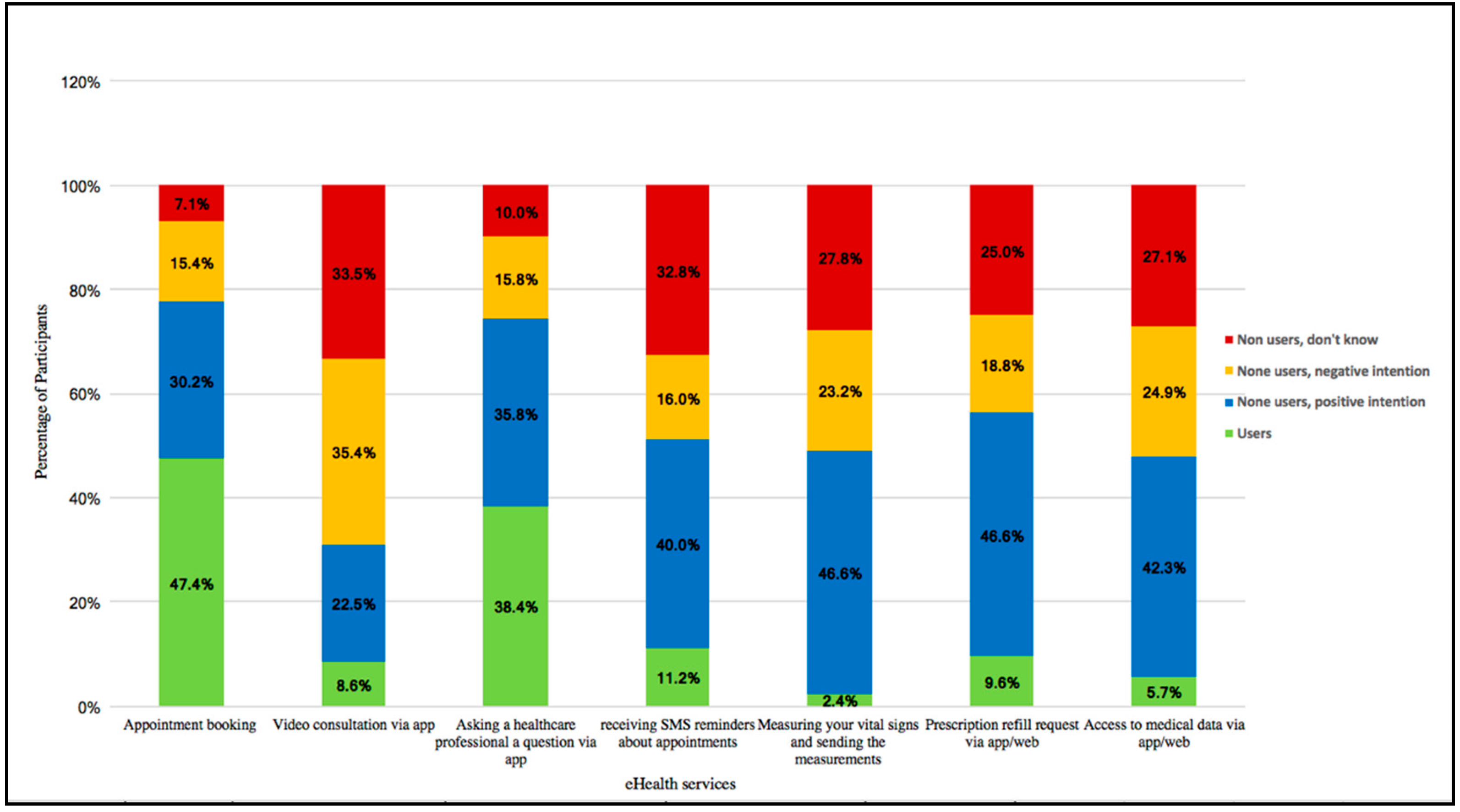
As shown in
Figure 1, the use of most of the eHealth services (5 out of 7) was low. Very few of the participants reported having measured their vital signs and sent the measurement to their health-care professional (2.41%, 29/1203) or having accessed their medical data via app/web (5.74%, 69/1203). A larger number of participants had undertaken a video consultation via the app in the past year (8.56%, 103/1203), requested a prescription refill via app (9.56%, 115/1203) or received SMS reminders about appointments (11.31%, 136/1203). The other two services were used more frequently. Booking an appointment via app/web was the most frequently used (47.4%, 570/1203), followed by asking a healthcare professional a question via the app (38.4%, 462/1203).
Participants were also asked about their intentions to use eHealth services in the future, and these results are also presented in
Figure 1. The highest percentages of participants with a positive intention were found for prescription refill requests (46.63%, 561/1203), measuring their vital signs and sending the measurement (46.55%, 560/1203), followed by having access to medical data (42.31%, 509/1203) and receiving SMS appointment reminders (39.98%, 481/1203). Almost a third of participants reported positive intentions regarding their future use of these services.
The proportion of respondents expressing a negative intention towards future eHealth use ranged from 15.4% for online appointment booking to 35.41% for video consultations. For most services, more than one quarter of respondents said that they did not know whether they would like to use Internet services in the future, ranging from 25.0% for prescription refill requests to 33.50% for video consultations.
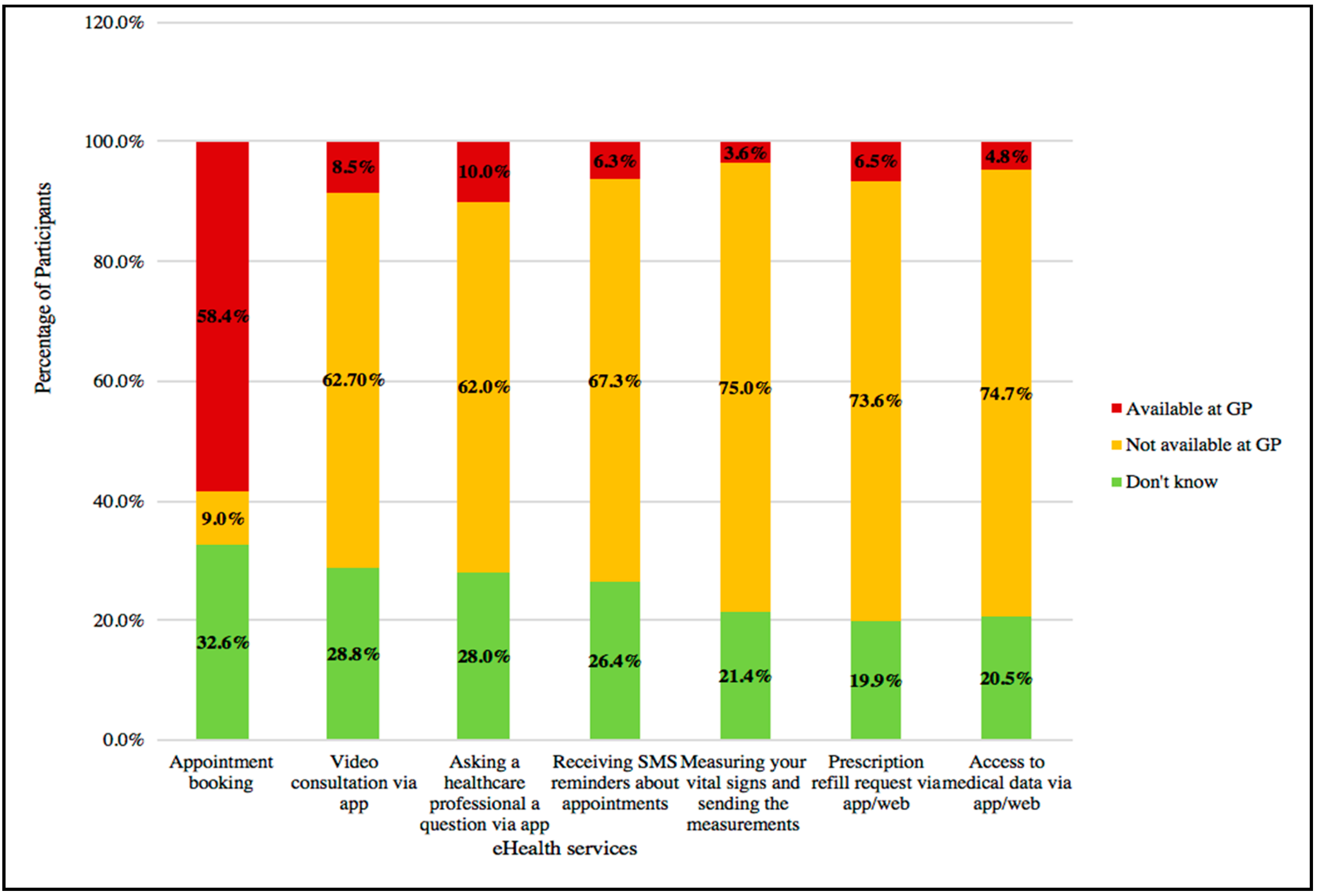
Figure 2 shows participants’ levels of awareness of the availability of each of the internet services at their primary care center. Measurement and transmission of vital signs had the lowest level of awareness (3.57%) whereas online appointment booking had the highest (58.3%). When asked which services they thought were unavailable at their PC, 9.06% reported that online appointments were not possible, and 75.06% reported that it was not possible to measure and share vital signs. Many patients did not know whether any of these online services were available at their PC (around one fifth of respondents for each service).
Relationship between Factors and Intention to Use eHealth Services
Table 4 presents the correlation between the constructs (effort expectancy, attitude, trust, performance expectancy, social influence and, facilitating conditions) and the two selected eHealth services. Correlations between both services and each of the studied constructs were statistically significant, higher than or equal to r=.64 (P<.001). For the constructs that could influence intention to ask questions via app or website, most coefficients were 0.80 or above, as shown in Table 2. In order to assess the interrelatedness of the constructs, variance inflation factors (VIFs) were calculated. All these VIF values were between 5 and 10, indicating strong multicollinearity.
For the constructs that influence participants’ appointment booking, 4 correlation coefficients exceeded the value of 0.80: attitude and effort expectancy (r=.85), and facilitating condition (r=.82), performance expectancy and attitude (r=.84) and facilitating condition (r=.80), each with a VIF value between 5 and 10, indicating high multicollinearity. Consequently, the strong multicollinearity makes multiple regression analysis impossible.
Table 2.
Matrix of linear correlations and variance inflation factor values between the independent constructs that could influence intention to ask healthcare professionals, a question via app/websitea.
Table 2.
Matrix of linear correlations and variance inflation factor values between the independent constructs that could influence intention to ask healthcare professionals, a question via app/websitea.
| Asking healthcare professionals, a question via app/website |
EE |
PE |
TR |
AT |
FC |
VIF value |
| Effort expectancy (EE) |
1 |
|
|
|
|
7.3 |
| Performance expectancy (PE) |
0.84 |
1 |
|
|
|
8.1 |
| Trust (TR) |
0.82 |
0.81 |
1 |
|
|
6.1 |
| Attitude (AT) |
0.85 |
0.84 |
0.82 |
1 |
|
8.1 |
| Facilitating Condition (FC) |
0.82 |
0.87 |
082 |
0.82 |
1 |
7.6 |
| Social Influence (SI) |
0.84 |
0.85 |
0.81 |
0.87 |
0.84 |
8.2 |
Table 3.
Matrix of linear correlations and variance inflation factor values between the independent constructs that could influence intention to book Appointment booking using website/appa.
Table 3.
Matrix of linear correlations and variance inflation factor values between the independent constructs that could influence intention to book Appointment booking using website/appa.
| Appointment booking using website/app |
EE |
PE |
TR |
AT |
FC |
VIF value |
| Effort expectancy (EE) |
1 |
|
|
|
|
5.7 |
| Performance expectancy (PE) |
0.75 |
1 |
|
|
|
5.5 |
| Trust (TR) |
0.70 |
0.72 |
1 |
|
|
4.3 |
| Attitude (AT) |
0.85 |
0.84 |
0.70 |
1 |
|
5.1 |
| Facilitating Condition (FC) |
0.70 |
0.79 |
074 |
0.78 |
1 |
5.7 |
| Social Influence (SI) |
0.72 |
0.76 |
0.64 |
0.78 |
0.74 |
5.1 |
Table 4 presents the simple linear regression analysis results. Each of the studied constructs (effort expectancy, attitude, trust, performance expectancy, social influence, and facilitating conditions) was significantly associated with intention to book appointments via app and to ask healthcare professionals questions via an app/website. For asking healthcare professionals online questions, the R ranged from 0.34 for trust and facilitate condition to 0.45 for performance expectancy. The R for booking appointments via the app/web ranged from 0.24 for trust to 0.36 for attitude.
The characteristics of participants, age, and internet usage showed a significant correlation with intention to use booking online appointment and asking healthcare professionals questions via app or a website. The R for age were 0.48 and 0.56, respectively and the R for Internet usage were 0.28 and 0.21 respectively. In Table 4, the analysis reveals that all six subscales have significant correlations with the intention to use the services, but also that age is the main explaining variable
Table 4.
Simple linear regression of constructs and characteristics with intention toward using booking appointment planning and asking questions via app/websitea.
Table 4.
Simple linear regression of constructs and characteristics with intention toward using booking appointment planning and asking questions via app/websitea.
| |
booking appointment planning |
asking questions via app/website |
| Independent Variable |
R |
Unstandardized B |
P |
R |
Unstandardized B |
P |
| Effort Expectancy |
0.30 |
0.20 |
0.001 |
0.42 |
0.24 |
0.001 |
| Performance Expectancy |
0.32 |
0.20 |
0.001 |
0.45 |
0.25 |
0.00 |
| Trust |
0.24 |
0.15 |
0.014 |
0.34 |
0.19 |
0.001 |
| Attitude |
0.36 |
0.23 |
0.001 |
0.40 |
0.23 |
0.001 |
| Facilitating condition |
0.26 |
0.17 |
0.007 |
0.34 |
0.19 |
0.001 |
| Social Influence |
0.31 |
0.20 |
0.001 |
0.42 |
0.23 |
0.001 |
| Gender |
0.13 |
-0.11 |
0.18 |
0.17 |
-0.13 |
0.08 |
| Age |
0.48 |
-0.01 |
0.001 |
0.56 |
-0.02 |
0.001 |
| Level of education |
0.16 |
-0.12 |
0.105 |
0.15 |
-0.096 |
0.13 |
| Internet usage |
0.28 |
0.18 |
0.003 |
0.37 |
0.21 |
0.001 |
4. Discussion
Participants’ use of and intention to use eHealth services to contact healthcare professionals varied greatly between each of the services studied. Online appointment booking was used most frequently (47.4%) while measuring vital signs and sending the measurement to the health-care professional was least frequent (2.4%). Participants who had not used these services at least once in the past year expressed differing positive intentions towards using them in future, ranging from 46.6% for prescription refill request via app/web and measuring vital signs and sending them to the healthcare professionals to 22.5% for video consultation. Many participants (around a fifth for each service) did not know whether these services were available at their PC center. The study also investigated the participant characteristics and other factors that could influence participants’ intention to use eHealth services to communicate with their primary care center. Several of the studied constructs exerted a significant influence on participants’ intention to use online appointment booking: effort expectancy, performance expectancy, trust, attitude, facilitating conditions, social influence, the characteristics of age, and internet usage. However, the age is the main explanatory variable. Given the relatively small number of participants who reported not knowing about their intentions, combined with the relatively high correlations between the constructs measured, the findings suggest that study respondents had clear and consistent views regarding the use of eHealth services.
Although the findings of previous research [
14,
16] indicate that the use of eHealth services is low, the present study found them to differ from one service to another. One reason for this variance may be that Saudi people were urged to use these services during COVID-19 lockdown [
23,
24], resulting in greater familiarity with these services and their ease of use [
1]. Moreover, the Ministry of Health (MOH) has also encouraged patients to book appointments via an app to reduce their waiting time and to serve them quickly, and to ask a doctor a question via app/website when no appointments are available) [
1,
25]. These drives could explain why these two services are used more than the others.
Our study confirms the findings of previous research, which has concluded that often patients do not know about the existence of eHealth applications or they are not aware of the possibilities of these applications [
2,
26]. Participants’ lack of knowledge about service availability will inevitably influence their usage. In the current study, only 10% of respondents thought that it was possible to ask questions of healthcare professionals online, and many replied that they did not know or that eHealth services were not available when asked about the availability of these eHealth services, despite these being available at a large proportion of primary care centers [
3,
23]. Patients’ awareness and use of eHealth services has greatly increased following the COVID-19 pandemic [
27,
28] with one study reporting that the number of online medical consultations in China was 20 times greater in 2020 than in the previous year [
29]. However, many of the eHealth solutions implemented in Saudi Arabia during this time were temporary, and have been replaced with new ones that patients may not know. Mair et al (2015) highlighted in their review the importance of communicating the purposes, benefits and values of eHealth services to prospective users as a way to improve the implementation of eHealth solutions, further indicating that lack of awareness was likely to have influenced respondents’ use and intentions in the present study [
30].
Although all of the studied constructs were found to exert influence over participants’ use of and intention to use eHealth services, most of the independent constructs exhibited high correlations. A previous study (in the Dutch context) has applied the UTAUT model to examine participants’ intention to use eHealth services [
14], finding moderate to high correlations between constructs, similar to the present study. On the other hand, a few studies have utilized a modified version of the UTAUT model to examine patient’s attitudes towards internet services for patient self-management, and did not report high correlations between independent constructs [
15,
31,
32]. A current research indicated that culture plays a key role on the strength of the relationships among the model constructs [
33].
Patient characteristics have been shown to influence their intention to use eHealth services, and this relationship has been well studied [
34,
35]. The results of the present study show that older participants, and those who reported greater difficulty with internet use in general also expressed more negative intentions regarding eHealth. Most previous studies have reported the same patterns [
36,
37]. Whereas it has been suggested by some researchers that the association between age and technology usage will become less pronounced as this population develops greater familiarity with internet communication technologies [
31], a study by Heart and Kalderon (2011) found that greater adoption of ICT among older participants did not necessarily translate into greater adoption of eHealth services [
38]. Among their study population, the most commonly reported reason not to use eHealth services was that they were perceived to be unnecessary, underscoring the importance of communicating the potential benefits of these technologies [
14].
Strength and Limitation
A strength of this study is that it is the first to investigate participants’ use of and intention to use eHealth services in the context of Saudi Arabia and the wider Gulf Region, therefore providing essential evidence regarding participants’ engagement with these technologies in PC settings. Secondly, a high number of participants (n=1203) between 18 and 74 years of age participated. The findings of the study may have only limited generalizability, but could provide insights into other cultures and contexts similar to Saudi Arabia and the Saudi Ministry of Health.
The questionnaire used in this study was adopted from a previous study, where it was designed to gather data on participants’ intention to make appointments and ask questions online based on the validated UTAUT model. The trust and valuation subscales were not validated, as the intention was not to produce a new validated model predicting patients’ intentions, nor are the factors included claimed to be the only ones informing participants’ intentions to use these services. Instead, the study investigated possible factors influencing the general population’s intentions by using predictors suggested in previous research.
5. Conclusions
The present study found use of and intention to use eHealth services to vary greatly among this study population, depending on the specific service examined. Participants’ awareness of the availability of services was generally limited, which would inevitably influence their use and intentions. While a substantial proportion of respondents expressed positive future intentions, many participants reported an unwillingness to use eHealth services. The findings indicate that greater information regarding the availability and benefits of eHealth services could play a key role in promoting greater engagement with eHealth services in this and other primary care settings.
References
- Alanzi TM, Althumairi A, Aljaffary A, Alfayez A, Alsalman D, Alanezi F, et al. Evaluation of the Mawid mobile healthcare application in delivering services during the COVID-19 pandemic in Saudi Arabia. Int Health. 2021;1–10.
- Alshammari, MH. Electronic-health in Saudi Arabia: A review. Int J Adv Appl Sci. 2021;8(6):1–10.
- MOH. Health Sector Transformation Strategy. Model Archit Pract. 2021;265–7.
- A, N. The Utilization of E-Health in the Kingdom of Saudi Arabia. Int Res J Eng Technol e. 2019;06(09):1229–39.
- Alshahrani A, Stewart D, MacLure K. A systematic review of the adoption and acceptance of eHealth in Saudi Arabia: Views of multiple stakeholders. Int J Med Inform. 2019 Aug 1;128:7–17.
- Curtis F, Burton JO, Butt A, Dhaliwal HK, Graham-Brown MMP, Lightfoot CJ, et al. Lifestyle interventions delivered by eHealth in chronic kidney disease: A scoping review. PLoS One [Internet]. 2024 Jan 1 [cited 2024 Jul 27];19(1). Available from: https://pubmed.ncbi.nlm.nih.gov/38266006/.
- De Veer AJE, Peeters JM, Brabers AEM, Schellevis FG, Rademakers JJDJM, Francke AL. Determinants of the intention to use e-Health by community dwelling older people. BMC Health Serv Res [Internet]. 2015 Mar 15 [cited 2024 Jul 27];15(1). Available from: https://pubmed.ncbi.nlm.nih.gov/25889884/.
- Chaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med [Internet]. 2006 May 16 [cited 2024 Jul 27];144(10):742–52. Available from: https://pubmed.ncbi.nlm.nih.gov/16702590/.
- McGeady D, Kujala J, Ilvonen K. The impact of patient–physician web messaging on healthcare service provision. Int J Med Inform. 2008 Jan 1;77(1):17–23.
- Wallwiener M, Wallwiener CW, Kansy JK, Seeger H, Rajab TK. Impact of electronic messaging on the patient-physician interaction. http://dx.doi.org/101258/jtt2009090111 [Internet]. 2009 Jul 9 [cited 2024 Jul 27];15(5):243–50. Available from: https://journals.sagepub.com/doi/10.1258/jtt.2009.090111.
- Ye J, Rust G, Fry-Johnson Y, Strothers H. E-mail in patient-provider communication: a systematic review. Patient Educ Couns [Internet]. 2010 Nov 13 [cited 2024 Jul 27];80(2):266–73. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/pmid/19914022/?tool=EBI.
- Bergmo TS, Kummervold PE, Gammon D, Dahl LB. Electronic patient–provider communication: Will it offset office visits and telephone consultations in primary care? Int J Med Inform. 2005 Sep 1;74(9):705–10.
- Nguyen PTL, Nguyen TB Le, Pham AG, Duong KNC, Gloria MAJ, Vo T Van, et al. Psychological Stress Risk Factors, Concerns and Mental Health Support Among Health Care Workers in Vietnam During the Coronavirus Disease 2019 (COVID-19) Outbreak. Front public Heal [Internet]. 2021 Mar 19 [cited 2024 Aug 1];9. Available from: https://pubmed.ncbi.nlm.nih.gov/33816419/.
- Huygens MW, Vermeulen J, Friele RD, van Schayck OC, de Jong JD, de Witte LP. Internet Services for Communicating With the General Practice: Barely Noticed and Used by Patients. Interact J Med Res [Internet]. 2015 Nov 24 [cited 2024 Jul 28];4(4):e21. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26601596.
- Or CKL, Karsh BT. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc [Internet]. 2009 Jul [cited 2024 Jul 28];16(4):550–60. Available from: https://pubmed.ncbi.nlm.nih.gov/19390112/.
- Santana S, Lausen B, Bujnowska-Fedak M, Chronaki C, Kummervold PE, Rasmussen J, et al. Online communication between doctors and patients in Europe: Status and perspectives. J Med Internet Res [Internet]. 2010 Jun 15 [cited 2024 Jul 28];12(2):e1281. Available from: https://www.jmir.org/2010/2/e20.
- Tao Z, Cheng Y, Liu J. Hierarchical two-step floating catchment area (2SFCA) method: Measuring the spatial accessibility to hierarchical healthcare facilities in Shenzhen, China. Int J Equity Health. 2020;19(1):1–16.
- Zaman TU, Raheem TMA, Alharbi GM, Shodri MF, Kutbi AH, Alotaibi SM, et al. E-health and its Transformation of Healthcare Delivery System in Makkah, Saudi Arabia. Int J Med Res Heal Sci [Internet]. 2018 May 21 [cited 2024 Aug 1];7(5):76–82. Available from: https://www.ijmrhs.com/abstract/ehealth-and-its-transformation-of-healthcare-delivery-system-in-makkah-saudi-arabia-15024.html.
- Davis, FD. A technology acceptance model for empirically testing new end-user information systems: Theory and results. Management. 1985;Ph.D.(May):291.
- Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: Toward a unified view. MIS Q Manag Inf Syst. 2003;27(3):425–78.
- Spil TAM, Schuring RW. E-health systems diffusion and use: The innovation, the user and the USE IT model. E-Health Syst Diffus Use Innov User USE IT Model. 2006;1–342.
- Almazroi AA, Mohammed F, Al-Kumaim NH, Hoque MR. An empirical study of factors influencing e-health services adoption among public in Saudi Arabia. Health Informatics J [Internet]. 2022 Apr 1 [cited 2023 Nov 8];28(2). Available from: https://journals.sagepub.com/doi/10.1177/14604582221102316?icid=int.sj-full-text.similar-articles.6.
- Alqifari S, Saleh SM, Habboush O, Ibrahim AA. Characteristics of Electronic Health Services in Saudi Arabia During the COVID-19 Pandemic. Cureus [Internet]. 2022 Aug 26 [cited 2023 Oct 16];14(8). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9509694/.
- Alkhalifah JM, Seddiq W, Alshehri BF, Alhaluli AH, Alessa MM, Alsulais NM. The role of the COVID-19 pandemic in expediting digital health-care transformation: Saudi Arabia’s experience. Informatics Med Unlocked [Internet]. 2022;33(July):101097. Available from:. [CrossRef]
- Alali E, Al-Dossary R, Al-Rayes S, Al-Ansary N, Alshawan D, Almulla S, et al. Evaluation of the Patient Experience with the Mawid App during the COVID-19 Pandemic in Al Hassa, Saudi Arabia. Healthcare [Internet]. 2022 Jun 1 [cited 2023 Oct 16];10(6). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9222366/.
- Alpay LL, Henkemans OB, Otten W, Rövekamp TAJM, Dumay ACM. E-health applications and services for patient empowerment: directions for best practices in The Netherlands. Telemed J E Health [Internet]. 2010 Sep 1 [cited 2024 Aug 2];16(7):787–91. Available from: https://pubmed.ncbi.nlm.nih.gov/20815745/.
- Furlepa K, Śliwczyński A, Kamecka K, Kozłowski R, Gołębiak I, Cichońska-Rzeźnicka D, et al. The COVID-19 Pandemic as an Impulse for the Development of Telemedicine in Primary Care in Poland. J Pers Med [Internet]. 2022 Jul 1 [cited 2023 Oct 16];12(7):1165. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9318246/.
- De Witte NAJ, Carlbring P, Etzelmueller A, Nordgreen T, Karekla M, Haddouk L, et al. Online consultations in mental healthcare during the COVID-19 outbreak: An international survey study on professionals’ motivations and perceived barriers. Internet Interv. 2021;25(March).
- Omboni S, Padwal RS, Alessa T, Benczúr B, Green BB, Hubbard I, et al. The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Heal. 2022;7–35.
- Mair FS, May C, O’Donnell C, Finch T, Sullivand F, Murray E. Factors that promote or inhibit the implementation of e-health systems: an explanatory systematic review. Bull World Health Organ [Internet]. 2012 May [cited 2024 Aug 2];90(5):357–64. Available from: https://pubmed.ncbi.nlm.nih.gov/22589569/.
- Philippi P, Baumeister H, Apolinário-Hagen J, Ebert DD, Hennemann S, Kott L, et al. Acceptance towards digital health interventions – Model validation and further development of the Unified Theory of Acceptance and Use of Technology. Internet Interv. 2021;26.
- Walle AD, Jemere AT, Tilahun B, Endehabtu BF, Wubante SM, Melaku MS, et al. Intention to use wearable health devices and its predictors among diabetes mellitus patients in Amhara region referral hospitals, Ethiopia: Using modified UTAUT-2 model. Informatics Med Unlocked [Internet]. 2023;36(December 2022):101157. Available from:. [CrossRef]
- Marikyan, D.& Papagiannidis S. The Unified Theory of Acceptance and Use of Technology. Int J Sociotechnology Knowl Dev. 2023;12(3):79–98.
- Alsharif AH. Attitudes of Patients with Chronic Diseases toward Management eHealth Applications Systems in Post-COVID-19 Times. Int J Environ Res Public Health [Internet]. 2022 Apr 1 [cited 2023 Oct 20];19(7). Available from: https://pubmed.ncbi.nlm.nih.gov/pmc/articles/PMC8998994/.
- Reiners F, Sturm J, Bouw LJW, Wouters EJM. Sociodemographic Factors Influencing the Use of eHealth in People with Chronic Diseases. Int J Environ Res Public Heal 2019, Vol 16, Page 645 [Internet]. 2019 Feb 21 [cited 2023 Oct 20];16(4):645. Available from: https://www.mdpi.com/1660-4601/16/4/645/htm.
- Alessa T, Hawley MS, Alsulamy N, de Witte L. Using a commercially available app for the self-management of hypertension: Acceptance and usability study in Saudi Arabia. JMIR mHealth uHealth. 2021;9(2).
- Uncovska M, Freitag B, Meister S, Fehring L. Patient Acceptance of Prescribed and Fully Reimbursed mHealth Apps in Germany: An UTAUT2-based Online Survey Study. J Med Syst [Internet]. 2023 Dec 1 [cited 2023 Oct 20];47(1):1–14. Available from: https://link.springer.com/article/10.1007/s10916-023-01910-x.
- Heart T, Kalderon E. Older adults: are they ready to adopt health-related ICT? Int J Med Inform [Internet]. 2013 Nov [cited 2024 Aug 2];82(11). Available from: https://pubmed.ncbi.nlm.nih.gov/21481631/.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).