Submitted:
05 August 2024
Posted:
07 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
2.1. Description of the Cohort
2.2. Variants Identified in Nicastrin (NCSTN) Gene
2.3. Variants Identified in Others Genes Involved in γ-Secretase Complex
2.4. Comprehensive Catalog of γ-Secretase Variants
2.5. Variants Identified in Others Genes Described as Being Associated with HS
3. Discussion
4. Materials and Methods
4.1. Sample Collection
4.2. Whole Exome Sequencing
| Cohort | Agilent WES Kit | Protocol | Library size |
| HS1 | SureSelectXT Human All Exon V5+UTR 2 | 2 x 100 bp | |
| HS2 | SureSelectXT Human All Exon V6 | 2 x 150 bp | ~70M |
| CTL | SureSelectXT Human All Exon V4+UTR | 2 x 100 bp | ~60M |
4.3. Variant Calling and Annotation
- CADD Phred-like score ≥ 30: among the 0.1% most deleterious variants
- REVEL ≥ 0.5: deleterious missense
- SIFT < 0.05: deleterious missense
- AlphaMissense > 0.564: possibly deleterious
- PolyPhen-2 ≥ 0.85: probably damaging missense
- SpliceAI ≥ 0.8: variant with the probability of altering splicing
- Pangolin ≥ 0.8: variant with the probability of altering splicing
- PhyloP (mammals) < 1.5: fast evolution of the locus in mammals
4.4. Variant Validation
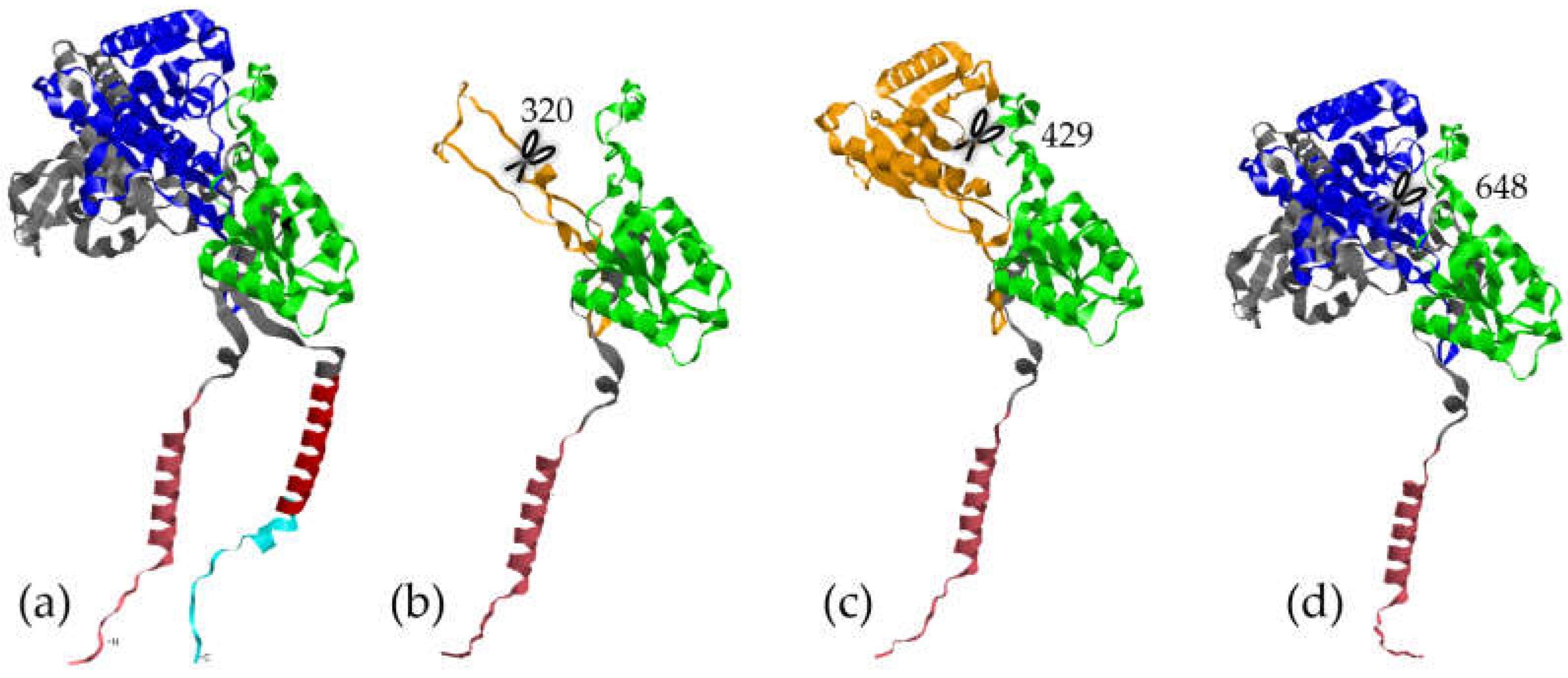
4.5. Protein Folding
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Vinkel, C.; Thomsen, S.F. Hidradenitis Suppurativa: Causes, Features, and Current Treatments. J Clin Aesthet Dermatol 2018, 11, 17–23. [Google Scholar]
- Frew, J.W. Hidradenitis Suppurativa Is an Autoinflammatory Keratinization Disease: A Review of the Clinical, Histologic, and Molecular Evidence. JAAD International 2020, 1, 62–72. [Google Scholar] [CrossRef]
- Akiyama, M.; De Vita, V.; Sugiura, K. Editorial: Autoinflammatory Keratinization Disease (AiKD). Front Immunol 2020, 11, 1753. [Google Scholar] [CrossRef] [PubMed]
- Nikolakis, G.; Kaleta, K.P.; Vaiopoulos, A.G.; Wolter, K.; Baroud, S.; Wojas-Pelc, A.; Zouboulis, C.C. Phenotypes and Pathophysiology of Syndromic Hidradenitis Suppurativa: Different Faces of the Same Disease? A Systematic Review. DRM 2021, 237, 673–697. [Google Scholar] [CrossRef] [PubMed]
- Duchatelet, S.; Miskinyte, S.; Delage, M.; Join-Lambert, O.; Coignard, H.; Lortholary, O.; Nassif, X.; Hovnanian, A.; Nassif, A. Coexistence d’une Acné Fulminante et d’une Hidrosadénite Suppurée : Syndrome ASH, Une Nouvelle Entité ? Annales de Dermatologie et de Vénéréologie 2014, 141, S381–S382. [Google Scholar] [CrossRef]
- Phan, K.; Tatian, A.; Woods, J.; Cains, G.; Frew, J.W. Prevalence of Inflammatory Bowel Disease (IBD) in Hidradenitis Suppurativa (HS): Systematic Review and Adjusted Meta-Analysis. Int J Dermatol 2020, 59, 221–228. [Google Scholar] [CrossRef]
- Moltrasio, C.; Tricarico, P.M.; Romagnuolo, M.; Marzano, A.V.; Crovella, S. Hidradenitis Suppurativa: A Perspective on Genetic Factors Involved in the Disease. Biomedicines 2022, 10, 2039. [Google Scholar] [CrossRef]
- Gasparic, J.; Theut Riis, P.; Jemec, G.B. Recognizing Syndromic Hidradenitis Suppurativa: A Review of the Literature. J Eur Acad Dermatol Venereol 2017, 31, 1809–1816. [Google Scholar] [CrossRef]
- Kjaersgaard Andersen, R.; Clemmensen, S.B.; Larsen, L.A.; Hjelmborg, J.V.B.; Ødum, N.; Jemec, G.B.E.; Christensen, K. Evidence of Gene-Gene Interaction in Hidradenitis Suppurativa: A Nationwide Registry Study of Danish Twins. Br J Dermatol 2022, 186, 78–85. [Google Scholar] [CrossRef]
- Sabat, R.; Jemec, G.B.E.; Matusiak, Ł.; Kimball, A.B.; Prens, E.; Wolk, K. Hidradenitis Suppurativa. Nat Rev Dis Primers 2020, 6, 1–20. [Google Scholar] [CrossRef]
- Wolfe, M.S.; Miao, Y. Structure and Mechanism of the γ-Secretase Intramembrane Protease Complex. Curr Opin Struct Biol 2022, 74, 102373. [Google Scholar] [CrossRef] [PubMed]
- Mintoff, D.; Pace, N.P.; Borg, I. Interpreting the Spectrum of Gamma-Secretase Complex Missense Variation in the Context of Hidradenitis Suppurativa—An in-Silico Study. Front Genet 2022, 13, 962449. [Google Scholar] [CrossRef] [PubMed]
- Pace, N.P.; Mintoff, D.; Borg, I. The Genomic Architecture of Hidradenitis Suppurativa-A Systematic Review. Front Genet 2022, 13, 861241. [Google Scholar] [CrossRef] [PubMed]
- Moltrasio, C.; Cagliani, R.; Sironi, M.; Clerici, M.; Pontremoli, C.; Maronese, C.A.; Tricarico, P.M.; Crovella, S.; Marzano, A.V. Autoinflammation in Syndromic Hidradenitis Suppurativa: The Role of AIM2. Vaccines 2023, 11. [Google Scholar] [CrossRef] [PubMed]
- Tricarico, P.M.; Gratton, R.; Dos Santos-Silva, C.A.; de Moura, R.R.; Ura, B.; Sommella, E.; Campiglia, P.; Del Vecchio, C.; Moltrasio, C.; Berti, I.; et al. A Rare Loss-of-Function Genetic Mutation Suggest a Role of Dermcidin Deficiency in Hidradenitis Suppurativa Pathogenesis. Front Immunol 2022, 13, 1060547. [Google Scholar] [CrossRef] [PubMed]
- Theut Riis, P.; Loft, I.C.; Yazdanyar, S.; Kjaersgaard Andersen, R.; Pedersen, O.B.; Ring, H.C.; Huber, R.; Sultan, M.; Loesche, C.; Saunte, D.M.L.; et al. Full Exome Sequencing of 11 Families with Hidradenitis Suppurativa. J Eur Acad Dermatol Venereol 2021, 35, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, A.S.L.E.; Bloise, G.; Moltrasio, C.; Coelho, A.; Agrelli, A.; Moura, R.; Tricarico, P.M.; Jamain, S.; Marzano, A.V.; Crovella, S.; et al. Transcriptome Meta-Analysis Confirms the Hidradenitis Suppurativa Pathogenic Triad: Upregulated Inflammation, Altered Epithelial Organization, and Dysregulated Metabolic Signaling. Biomolecules 2022, 12, 1371. [Google Scholar] [CrossRef] [PubMed]
- Higgins, R.; Pink, A.; Hunger, R.; Yawalkar, N.; Navarini, A.A. Generalized Comedones, Acne, and Hidradenitis Suppurativa in a Patient with an FGFR2 Missense Mutation. Front Med (Lausanne) 2017, 4, 16. [Google Scholar] [CrossRef]
- Nyquist, G.G.; Mumm, C.; Grau, R.; Crowson, A.N.; Shurman, D.L.; Benedetto, P.; Allen, P.; Lovelace, K.; Smith, D.W.; Frieden, I.; et al. Malignant Proliferating Pilar Tumors Arising in KID Syndrome: A Report of Two Patients. Am. J. Med. Genet. 2007, 143A, 734–741. [Google Scholar] [CrossRef]
- Lazic, T.; Li, Q.; Frank, M.; Uitto, J.; Zhou, L.H. Extending the Phenotypic Spectrum of Keratitis-Ichthyosis-Deafness Syndrome: Report of a Patient with GJB2 (G12R) Connexin 26 Mutation and Unusual Clinical Findings. Pediatr Dermatol 2012, 29, 349–357. [Google Scholar] [CrossRef]
- Bettoli, V.; Forconi, R.; Pezzini, I.; Martinello, R.; Scuderi, V.; Zedde, P.; Schettini, N.; Pacetti, L.; Corazza, M. KID Syndrome and Hidradenitis Suppurativa: A Rare Association Responding to Surgical Treatment. Skin Appendage Disord 2021, 7, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Oliveira Mendonca, L.; Caroli, F. Hidradenitis Suppurativa in KID’s Syndrome: Genetic Characterisation, Clinical and Surgical Intervention; 2019;
- Montgomery, J.R.; White, T.W.; Martin, B.L.; Turner, M.L.; Holland, S.M. A Novel Connexin 26 Gene Mutation Associated with Features of the Keratitis-Ichthyosis-Deafness Syndrome and the Follicular Occlusion Triad. Journal of the American Academy of Dermatology 2004, 51, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Genovese, G.; Moltrasio, C.; Tricarico, P.M.; Gratton, R.; Piaserico, S.; Garcovich, S.; Boniotto, M.; Brandão, L.; Moura, R.; et al. Whole-Exome Sequencing in 10 Unrelated Patients with Syndromic Hidradenitis Suppurativa: A Preliminary Step for a Genotype-Phenotype Correlation. Dermatology 2022, 238, 860–869. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Ceccherini, I.; Gattorno, M.; Fanoni, D.; Caroli, F.; Rusmini, M.; Grossi, A.; De Simone, C.; Borghi, O.M.; Meroni, P.L.; et al. Association of Pyoderma Gangrenosum, Acne, and Suppurative Hidradenitis (PASH) Shares Genetic and Cytokine Profiles With Other Autoinflammatory Diseases. Medicine (Baltimore) 2014, 93, e187. [Google Scholar] [CrossRef] [PubMed]
- Palmroth, M.; Viskari, H.; Seppänen, M.R.J.; Keskitalo, S.; Virtanen, A.; Varjosalo, M.; Silvennoinen, O.; Isomäki, P. IRF2BP2 Mutation Is Associated with Increased STAT1 and STAT5 Activation in Two Family Members with Inflammatory Conditions and Lymphopenia. Pharmaceuticals (Basel) 2021, 14, 797. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, A.; Ebstein, F.; Shamseldin, H.; Prouteau, C.; Krüger, E.; Binamer, Y.M.; Bonneau, D.; Alkuraya, F.S.; Martin, L. Gain-of-Function Variants in the KDF1 Gene Cause Hidradenitis Suppurativa Associated with Ectodermal Dysplasia by Stabilizing IκB Kinase α. Br J Dermatol 2023, 189, 131–132. [Google Scholar] [CrossRef] [PubMed]
- Shamseldin, H.E.; Khalifa, O.; Binamer, Y.M.; Almutawa, A.; Arold, S.T.; Zaidan, H.; Alkuraya, F.S. KDF1, Encoding Keratinocyte Differentiation Factor 1, Is Mutated in a Multigenerational Family with Ectodermal Dysplasia. Hum Genet 2017, 136, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Pedraz, J.; Peñas, P.; Garcia-Diez, A. Pachyonychia Congenita and Hidradenitis Suppurativa: No Response to Infliximab Therapy. Journal of the European Academy of Dermatology and Venereology 2008, 22, 1500–1501. [Google Scholar] [CrossRef]
- Yan, J.; Zhang, G.; Liao, C.; Wang, X.; Shi, L. ALA-iPDT for Follicular Occlusion Tetrad Concomitant with Pachyonychia Congenital Type Ⅱ and Ankylosing Spondylitis. Photodiagnosis and Photodynamic Therapy 2022, 39, 102891. [Google Scholar] [CrossRef]
- Musumeci, M.L.; Fiorentini, F.; Bianchi, L.; Cascella, R.; Giardina, E.; Caputo, V.; Micali, G. Follicular Occlusion Tetrad in a Male Patient with Pachyonychia Congenita: Clinical and Genetic Analysis. J Eur Acad Dermatol Venereol 2019, 33, 36–39. [Google Scholar] [CrossRef]
- Vural, S.; Gündoğdu, M.; Gökpınar İli, E.; Durmaz, C. d.; Vural, A.; Steinmüller-Magin, L.; Kleinhempel, A.; Holdt, L. m.; Ruzicka, T.; Giehl, K. a.; et al. Association of Pyrin Mutations and Autoinflammation with Complex Phenotype Hidradenitis Suppurativa: A Case–Control Study. British Journal of Dermatology 2019, 180, 1459–1467. [Google Scholar] [CrossRef]
- Jfri, A.; Litvinov, I.V.; Netchiporouk, E.; O’Brien, E. Novel Variants of MEFV and NOD2 Genes in Familial Hidradenitis Suppurativa: A Case Report. SAGE Open Med Case Rep 2020, 8, 2050313X20953113. [Google Scholar] [CrossRef]
- Bueno-Molina, R.C.; Hernández-Rodríguez, J.-C.; Zulueta-Dorado, T.; Pereyra-Rodriguez, J.-J. Pyrin-Associated Autoinflammation with Neutrophilic Dermatosis: A Case Report. The Journal of Dermatology 2024, n/a. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.Y.; Keiser, E.; LeBoit, P.; Yeh, I.; Wei, M.L. A Rare Case of Axillary Keratoacanthoma Arising in Hidradenitis Suppurativa. JAAD Case Rep 2022, 21, 49–51. [Google Scholar] [CrossRef] [PubMed]
- Morales-Heil, D.J.; Cao, L.; Sweeney, C.; Malara, A.; Brown, F.; Milam, P.; Anadkat, M.; Kaffenberger, J.; Kaffenberger, B.; Nagele, P.; et al. Rare Missense Variants in the SH3 Domain of PSTPIP1 Are Associated with Hidradenitis Suppurativa. HGG Adv 2023, 4, 100187. [Google Scholar] [CrossRef] [PubMed]
- Marzuillo, P.; Piccolo, V.; Mascolo, M.; Apicella, A.; Argenziano, G.; Della Vecchia, N.; Guarino, S.; Miraglia del Giudice, E.; La Manna, A. Patients Affected by Dent Disease 2 Could Be Predisposed to Hidradenitis Suppurativa. Journal of the European Academy of Dermatology and Venereology 2018, 32, e309–e311. [Google Scholar] [CrossRef] [PubMed]
- García-Gil, M.F.; Monte Serrano, J.; Ramirez-Lluch, M.; Valero Torres, A.; López-Giménez, M.T.; Lezcano Biosca, V. A Novel Mutation in POFUT1 Gene Associated with Dowling-Degos Disease and Hidradenitis Suppurativa. Int J Dermatol 2021, 60, e25–e27. [Google Scholar] [CrossRef] [PubMed]
- González-Villanueva, I.; Gutiérrez, M.; Hispán, P.; Betlloch, I.; Pascual, J. c. Novel POFUT1 Mutation Associated with Hidradenitis Suppurativa–Dowling–Degos Disease Firm up a Role for Notch Signalling in the Pathogenesis of This Disorder. British Journal of Dermatology 2018, 178, 984–986. [Google Scholar] [CrossRef] [PubMed]
- Duchatelet, S.; Clerc, H.; Machet, L.; Gaboriaud, P.; Miskinyte, S.; Kervarrec, T.; Hovnanian, A. A New Nonsense Mutation in the POGLUT1 Gene in Two Sisters with Dowling–Degos Disease. Journal of the European Academy of Dermatology and Venereology 2018, 32, e440–e442. [Google Scholar] [CrossRef]
- Duchatelet, S.; Miskinyte, S.; Join-Lambert, O.; Ungeheuer, M.-N.; Francès, C.; Nassif, A.; Hovnanian, A. First Nicastrin Mutation in PASH (Pyoderma Gangrenosum, Acne and Suppurative Hidradenitis) Syndrome. Br J Dermatol 2015, 173, 610–612. [Google Scholar] [CrossRef]
- Shen, M.; Yeoh, X.L.A.; Wang, D.Y.; Tey, H.L.; Ren, E.C.; Oon, H.H. Genetic Variations in Gamma-Secretase and PSTPIP1 in Hidradenitis Suppurativa in Singaporean Chinese. J Eur Acad Dermatol Venereol 2021, 35, e348–e350. [Google Scholar] [CrossRef] [PubMed]
- Braun-Falco, M.; Kovnerystyy, O.; Lohse, P.; Ruzicka, T. Pyoderma Gangrenosum, Acne, and Suppurative Hidradenitis (PASH)–a New Autoinflammatory Syndrome Distinct from PAPA Syndrome. Journal of the American Academy of Dermatology 2012, 66, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Kotzerke, M.; Mitri, F.; Marbach, F.; Enk, A.; Haenssle, H. A Case of PAPASH Syndrome in a Young Man Carrying a Novel Heterozygote Missense Variant in PSTPIP1. J Eur Acad Dermatol Venereol 2021, 35, e439–e440. [Google Scholar] [CrossRef]
- Hieta, N.; Nuutinen, H.; Roivas, J.; Salminen, K.; Kujari, H.; Talve, L.; Toivonen, M.; Haanpää, M.K. Severe Ulcerative Proctitis, Pyoderma Gangrenosum, Hidradenitis Suppurativa and Fever in a Patient with a Rare Variant of the PSTPIP1 Gene. Clin Exp Dermatol 2021, 46, 1387–1390. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Trevisan, V.; Gattorno, M.; Ceccherini, I.; De Simone, C.; Crosti, C. Pyogenic Arthritis, Pyoderma Gangrenosum, Acne, and Hidradenitis Suppurativa (PAPASH): A New Autoinflammatory Syndrome Associated With a Novel Mutation of the PSTPIP1 Gene. JAMA Dermatology 2013, 149, 762–764. [Google Scholar] [CrossRef] [PubMed]
- Saito, N.; Minami-Hori, M.; Nagahata, H.; Nozaki, H.; Iinuma, S.; Igawa, S.; Kanno, K.; Kishibe, M.; Kanazawa, N.; Ishida-Yamamoto, A. Novel PSTPIP1 Gene Mutation in Pyoderma Gangrenosum, Acne and Suppurative Hidradenitis Syndrome. J Dermatol 2018, 45, e213–e214. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Castrat, X.; Bancalari-Díaz, D.; Román-Curto, C.; Romo-Melgar, A.; Amorós-Cerdán, D.; Alcaraz-Mas, L.A.; Fernández-López, E.; Cañueto, J. PSTPIP1 Gene Mutation in a Pyoderma Gangrenosum, Acne and Suppurative Hidradenitis (PASH) Syndrome. Br J Dermatol 2016, 175, 194–198. [Google Scholar] [CrossRef]
- van Straalen, K.R.; Prens, E.P.; Willemsen, G.; Boomsma, D.I.; van der Zee, H.H. Contribution of Genetics to the Susceptibility to Hidradenitis Suppurativa in a Large, Cross-Sectional Dutch Twin Cohort. JAMA Dermatol 2020, 156, 1359–1362. [Google Scholar] [CrossRef]
- Genin, E.; Redon, R.; Deleuze, J.-F.; Campion, D.; Lambert, J.-C.; Dartigues, J.-F.; Consortium, F. The French Exome (FREX) Project: A Population-Based Panel of Exomes to Help Filter Out Common Local Variants. Genetic Epidemiology 2017, 41, 691. [Google Scholar]
- Herzig, A.F.; Velo-Suárez, L.; Dina, C.; Redon, R.; Deleuze, J.-F.; Génin, E. How Local Reference Panels Improve Imputation in French Populations. Sci Rep 2024, 14, 370. [Google Scholar] [CrossRef]
- Van der Zee, H.H.; Jemec, G.B.E. New Insights into the Diagnosis of Hidradenitis Suppurativa: Clinical Presentations and Phenotypes. J Am Acad Dermatol 2015, 73, S23–26. [Google Scholar] [CrossRef] [PubMed]
- Nishimori, N.; Hayama, K.; Kimura, K.; Fujita, H.; Fujiwara, K.; Terui, T. A Novel NCSTN Gene Mutation in a Japanese Family with Hidradenitis Suppurativa. Acta Derm Venereol 2020, 100, adv00283. [Google Scholar] [CrossRef] [PubMed]
- Ingram, J. r.; Wood, M.; John, B.; Butler, R.; Anstey, A. v. Absence of Pathogenic γ-Secretase Mutations in a South Wales Cohort of Familial and Sporadic Hidradenitis Suppurativa (Acne Inversa). British Journal of Dermatology 2013, 168, 874–876. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Yu, Y.; Yu, G.; Zhang, F. Identification of One Novel Mutation of the NCSTN Gene in One Chinese Acne Inversa Family. Dermatologica Sinica 2014, 32, 126–128. [Google Scholar] [CrossRef]
- Pink, A.E.; Simpson, M.A.; Brice, G.W.; Smith, C.H.; Desai, N.; Mortimer, P.S.; Barker, J.N.W.N.; Trembath, R.C. PSENEN and NCSTN Mutations in Familial Hidradenitis Suppurativa (Acne Inversa). Journal of Investigative Dermatology 2011, 131, 1568–1570. [Google Scholar] [CrossRef] [PubMed]
- Miskinyte, S.; Nassif, A.; Merabtene, F.; Ungeheuer, M.-N.; Join-Lambert, O.; Jais, J.-P.; Hovnanian, A. Nicastrin Mutations in French Families with Hidradenitis Suppurativa. Journal of Investigative Dermatology 2012, 132, 1728–1730. [Google Scholar] [CrossRef] [PubMed]
- Shi, T.-W.; Bai, N.; Zhang, J.-A.; Lu, F.; Chen, X.-B.; Kong, X.-D.; Yu, J.-B. Mutations in the γ-Secretase Genes PSEN1, PSENEN, and NCSTN in a Family with Acne Inversa. Eur J Dermatol 2018, 28, 374–376. [Google Scholar] [CrossRef] [PubMed]
- Duchatelet, S.; Miskinyte, S.; Delage, M.; Ungeheuer, M.-N.; Lam, T.; Benhadou, F.; Del Marmol, V.; Vossen, A.R.J.V.; Prens, E.P.; Cogrel, O.; et al. Low Prevalence of GSC Gene Mutations in a Large Cohort of Predominantly Caucasian Patients with Hidradenitis Suppurativa. Journal of Investigative Dermatology 2020, 140, 2085–2088.e14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Wang, L.; Chen, L.; Ren, W.; Mei, A.; Chen, X.; Deng, Y. Two Novel Mutations of the NCSTN Gene in Chinese Familial Acne Inverse. J Eur Acad Dermatol Venereol 2013, 27, 1571–1574. [Google Scholar] [CrossRef]
- Pink, A.E.; Simpson, M.A.; Desai, N.; Dafou, D.; Hills, A.; Mortimer, P.; Smith, C.H.; Trembath, R.C.; Barker, J.N.W. Mutations in the γ-Secretase Genes NCSTN, PSENEN, and PSEN1 Underlie Rare Forms of Hidradenitis Suppurativa (Acne Inversa). Journal of Investigative Dermatology 2012, 132, 2459–2461. [Google Scholar] [CrossRef]
- Li, C.-R.; Jiang, M.-J.; Shen, D.-B.; Xu, H.-X.; Wang, H.-S.; Yao, X.; Zhang, Y.; Zhou, W.-Q.; Wang, B. Two Novel Mutations of the Nicastrin Gene in Chinese Patients with Acne Inversa. Br J Dermatol 2011, 165, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Nomura, Y.; Nomura, T.; Sakai, K.; Sasaki, K.; Ohguchi, Y.; Mizuno, O.; Hata, H.; Aoyagi, S.; Abe, R.; Itaya, Y.; et al. A Novel Splice Site Mutation in NCSTN Underlies a Japanese Family with Hidradenitis Suppurativa. British Journal of Dermatology 2013, 168, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.; He, Y.; Li, C.; Zhang, X.; Xu, H.; Wang, B. Nicastrin Mutations in Familial Acne Inversa Impact Keratinocyte Proliferation and Differentiation through the Notch and Phosphoinositide 3-Kinase/AKT Signalling Pathways. British Journal of Dermatology 2016, 174, 522–532. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Xu, H.; Li, C.; Zhang, X.; Zhou, P.; Xiao, X.; Zhang, W.; Wu, Y.; Zeng, R.; Wang, B. Nicastrin/miR-30a-3p/RAB31 Axis Regulates Keratinocyte Differentiation by Impairing EGFR Signaling in Familial Acne Inversa. Journal of Investigative Dermatology 2019, 139, 124–134. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Davis, J. w.; Idler, K. b.; Mostafa, N. m.; Okun, M. m.; Waring, J. f. Genetic Analysis of NCSTN for Potential Association with Hidradenitis Suppurativa in Familial and Nonfamilial Patients. British Journal of Dermatology 2016, 175, 414–416. [Google Scholar] [CrossRef] [PubMed]
- Yang, J. -q.; Wu, X. -j.; Dou, T. -t.; Jiao, T.; Chen, X. -b.; Min, M.; Cai, S. -q.; Zheng, M. Haploinsufficiency Caused by a Nonsense Mutation in NCSTN Underlying Hidradenitis Suppurativa in a Chinese Family. Clinical and Experimental Dermatology 2015, 40, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Vural, S.; Baumgartner, M.; Lichtner, P.; Eckstein, G.; Hariry, H.; Chen, W.C.; Ruzicka, T.; Melnik, B.; Plewig, G.; Wagner, M.; et al. Investigation of Gamma Secretase Gene Complex Mutations in German Population with Hidradenitis Suppurativa Designate a Complex Polygenic Heritage. J Eur Acad Dermatol Venereol 2021, 35, 1386–1392. [Google Scholar] [CrossRef] [PubMed]
- Takeichi, T.; Matsumoto, T.; Nomura, T.; Takeda, M.; Niwa, H.; Kono, M.; Shimizu, H.; Ogi, T.; Akiyama, M. A Novel NCSTN Missense Mutation in the Signal Peptide Domain Causes Hidradenitis Suppurativa, Which Has Features Characteristic of an Autoinflammatory Keratinization Disease. British Journal of Dermatology 2020, 182, 491–493. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Gao, M.; Lv, Y.; Yang, X.; Ren, Y.; Jiang, T.; Zhang, X.; Guo, B.; Li, M.; Zhang, Q.; et al. Confirmation by Exome Sequencing of the Pathogenic Role of NCSTN Mutations in Acne Inversa (Hidradenitis Suppurativa). J Invest Dermatol 2011, 131, 1570–1572. [Google Scholar] [CrossRef]
- Li, C.; Xu, H.; Wang, B. Is SAPHO Syndrome Linked to PASH Syndrome and Hidradenitis Suppurativa by Nicastrin Mutation? A Case Report. J Rheumatol 2018, 45, 1605–1607. [Google Scholar] [CrossRef]
- Wu, C.; Yang, J.; Zhang, S.; Li, J.; Jin, H.; Zhang, X. A Novel NCSTN Gene Mutation in a Chinese Family with Acne Inversa. Mol Genet Genomics 2018, 293, 1469–1475. [Google Scholar] [CrossRef]
- Wang, B.; Yang, W.; Wen, W.; Sun, J.; Su, B.; Liu, B.; Ma, D.; Lv, D.; Wen, Y.; Qu, T.; et al. γ-Secretase Gene Mutations in Familial Acne Inversa. Science 2010, 330, 1065–1065. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Xiao, X.; Hui, Y.; Zhang, X.; He, Y.; Li, C.; Wang, B. Phenotype of 53 Chinese Individuals with Nicastrin Gene Mutations in Association with Familial Hidradenitis Suppurativa (Acne Inversa). Br J Dermatol 2016, 174, 927–929. [Google Scholar] [CrossRef]
- Xu, H.; He, Y.; Hui, Y.; Xiao, X.; Zhang, X.; Li, C.; Wang, B. NCSTN Mutations in Hidradenitis Suppurativa/Acne Inversa Do Not Influence Cytokine Production by Peripheral Blood Mononuclear Cells. British Journal of Dermatology 2017, 176, 277–279. [Google Scholar] [CrossRef]
- Chen, S.; Mattei, P.; You, J.; Sobreira, N.L.; Hinds, G.A. γ-Secretase Mutation in an African American Family With Hidradenitis Suppurativa. JAMA Dermatology 2015, 151, 668–670. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Liu, X.; Wang, R.; Chen, L.; Zhao, H.; Zhou, Y. A Novel NCSTN Mutation in a Three-Generation Chinese Family with Hidradenitis Suppurative. J Healthc Eng 2022, 2022, 1540774. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Ge, H.; Fan, Y.; Zhen, Q.; Tang, L.; Sun, L. Novel Mutation of the NCSTN Gene Identified in a Chinese Acne Inversa Family. Ann Dermatol 2020, 32, 237–242. [Google Scholar] [CrossRef]
- Savva, A.; Kanni, T.; Damoraki, G.; Kotsaki, A.; Giatrakou, S.; Grech, I.; Katoulis, A.; Papadavid, E.; Giamarellos-Bourboulis, E. j. Impact of Toll-like Receptor-4 and Tumour Necrosis Factor Gene Polymorphisms in Patients with Hidradenitis Suppurativa. British Journal of Dermatology 2013, 168, 311–317. [Google Scholar] [CrossRef]
- Mintoff, D.; Pace, N.P.; Bauer, P.; Borg, I. A Novel c.671_682del NCSTN Variant in a Family with Hidradenitis Suppurativa: A Pilot Study. Clin Exp Dermatol 2021, 46, 1306–1308. [Google Scholar] [CrossRef]
- Ratnamala, U.; Jhala, D.; Jain, N.K.; Saiyed, N.M.; Raveendrababu, M.; Rao, M.V.; Mehta, T.Y.; Al-Ali, F.M.; Raval, K.; Nair, S.; et al. Expanding the Spectrum of γ-Secretase Gene Mutation-Associated Phenotypes: Two Novel Mutations Segregating with Familial Hidradenitis Suppurativa (Acne Inversa) and Acne Conglobata. Exp Dermatol 2016, 25, 314–316. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, B.; Guo, Y.; Chen, J.; Zheng, S.; Gao, X.; Chen, H.; Xu, X. A Novel Mutation of the NCSTN Gene in a Chinese Hidradenitis Suppurativa Family with Familial Comedones as the Main Clinical Manifestation. Int J Dermatol 2022, 61, e293–e294. [Google Scholar] [CrossRef]
- Xiao, X.-M.; Yang, W.-Z.; Lin, L.-H.; Li, C.-R. Two Novel Nicastrin Mutations in Chinese Families with Acne Inversa. J Dermatol 2020, 47, e449–e451. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Meng, J.; Jiang, M.; Zhao, J. Characterization of a Novel Mutation in the NCSTN Gene in a Large Chinese Family with Acne Inversa. Acta Derm Venereol 2016, 96, 408–409. [Google Scholar] [CrossRef] [PubMed]
- Haines, R.; Common, J.; Teo, D.; Tang, M.; Lane, E. Sequencing of the Gamma-Secretase Complex in Singaporean Patients with Acne Inversa Reveals a Novel Mutation in Nicastrin, but Suggests Other Mechanisms Must Be Present.; April 1 2012; pp. e33–e33.
- Pink, A.E.; Simpson, M.A.; Desai, N.; Trembath, R.C.; Barker, J.N.W. γ-Secretase Mutations in Hidradenitis Suppurativa: New Insights into Disease Pathogenesis. J Invest Dermatol 2013, 133, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Pink, A.E.; Dafou, D.; Desai, N.; Holmes, O.; Hobbs, C.; Smith, C.H.; Mortimer, P.; Simpson, M.A.; Trembath, R.C.; Barker, J.N. Hidradenitis Suppurativa: Haploinsufficiency of Gamma-Secretase Components Does Not Affect Gamma-Secretase Enzyme Activity in Vitro. Br J Dermatol 2016, 175, 632–635. [Google Scholar] [CrossRef] [PubMed]
- Jiao, T.; Dong, H.; Jin, L.; Wang, S.; Wang, J. A Novel Nicastrin Mutation in a Large Chinese Family with Hidradenitis Suppurativa. British Journal of Dermatology 2013, 168, 1141–1143. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.-Y.; Lin, L.-H.; Kang, J.; Li, C.-R.; Xiao, X.-M. Hidradenitis Suppurativa Associated with a Novel NCSTN Mutation and Concomitant Klippel-Trenaunay Syndrome. European Journal of Dermatology 2021, 31, 246–248. [Google Scholar] [CrossRef] [PubMed]
- González-Villanueva, I.; Poveda-Montoyo, I.; Álvarez-Chinchilla, P.; Gutiérrez, M.; Pascual-Ramírez, J.C. Hidradenitis Suppurativa/Dowling-Degos Disease (DDD) Phenotype Associated with Mutations in NCSTN Gene (Poster - Plenary Lectures). Experimental Dermatology 2019, 28, 5–55. [Google Scholar] [CrossRef]
- Qian, Y.-T.; Xiao, M.; Liu, K.; Ma, D.-L.; Zhang, X. Two Novel Mutations of the γ-Secretase Genes in Chinese Acne Inversa (Hidradenitis Suppurativa). Experimental Dermatology 2022, 31, 643–644. [Google Scholar] [CrossRef]
- Faraji Zonooz, M.; Sabbagh-Kermani, F.; Fattahi, Z.; Fadaee, M.; Akbari, M.R.; Amiri, R.; Vahidnezhad, H.; Uitto, J.; Najmabadi, H.; Kariminejad, A. Whole Genome Linkage Analysis Followed by Whole Exome Sequencing Identifies Nicastrin (NCSTN) as a Causative Gene in a Multiplex Family with γ-Secretase Spectrum of Autoinflammatory Skin Phenotypes. J Invest Dermatol 2016, 136, 1283–1286. [Google Scholar] [CrossRef]
- Nomura, Y.; Nomura, T.; Suzuki, S.; Takeda, M.; Mizuno, O.; Ohguchi, Y.; Abe, R.; Murata, Y.; Shimizu, H. A Novel NCSTN Mutation Alone May Be Insufficient for the Development of Familial Hidradenitis Suppurativa. J Dermatol Sci 2014, 74, 180–182. [Google Scholar] [CrossRef]
- Garcovich, S.; Tricarico, P.M.; Nait-Meddour, C.; Giovanardi, G.; Peris, K.; Crovella, S.; Boniotto, M. Novel Nicastrin Mutation in Hidradenitis Suppurativa–Dowling–Degos Disease Clinical Phenotype: More than Just Clinical Overlap? Br J Dermatol 2020, 183, 758–759. [Google Scholar] [CrossRef] [PubMed]
- Vossen, A.R.J.V.; van Straalen, K.R.; Swagemakers, S.M.A.; de Klein, J.E.M.M.; Stubbs, A.P.; Venter, D.J.; van der Zee, H.H.; van der Spek, P.J.; Prens, E.P. A Novel Nicastrin Mutation in a Three-Generation Dutch Family with Hidradenitis Suppurativa: A Search for Functional Significance. J Eur Acad Dermatol Venereol 2020, 34, 2353–2361. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.-J.; Yang, Y.; Liang, Y.-H. Hsa-miR-155 Targeted NCSTN 3′UTR Mutation Promotes the Pathogenesis and Development of Acne Inversa. Int J Clin Exp Pathol 2018, 11, 1878–1889. [Google Scholar]
- de Oliveira, A.S.L.E.; de Siqueira, R.C.; Nait-Meddour, C.; Tricarico, P.M.; Moura, R.; Agrelli, A.; d’Adamo, A.P.; Jamain, S.; Crovella, S.; de Fátima Medeiros Brito, M.; et al. A Loss-of-Function NCSTN Mutation Associated with Familial Dowling Degos Disease and Hidradenitis Suppurativa. Experimental Dermatology 2023, 32, 1935–1945. [Google Scholar] [CrossRef]
- Le Gall, C.; Puca, L.; Madrange, M.; Bal, E.; Choukair, Z.; Hamel, Y.; Fraitag, S.; Brou, C.; Bachelez, H.; Smahi, A. Impairment of Notch 1 Signaling Is a Common Defect in Lesions from Patients with Hidradenitis Suppurativa. J Invest Dermatol 2017, 137, S226. [Google Scholar] [CrossRef]
- Hermasch, M.A.; Schön, M.P.; Frank, J. Comorbid Acne Inversa and Dowling–Degos Disease Due to a Single NCSTN Mutation: Is There Enough Evidence? Br J Dermatol 2021, 184, 374–374. [Google Scholar] [CrossRef]
- Ratnamala, U.; Jain, N.K.; Jhala, D.D.; Prasad, P.V.S.; Saiyed, N.; Nair, S.; Radhakrishna, U. An Updated Mutation Spectrum of the γ-Secretase Complex: Novel NCSTN Gene Mutation in an Indian Family with Hidradenitis Suppurativa and Acne Conglobata. Indian J Dermatol 2023, 68, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Mintoff, D.; Pace, N.P.; Borg, I. NCSTN In-Frame Deletion in Maltese Patients With Hidradenitis Suppurativa. JAMA Dermatol 2023, 159, 939–944. [Google Scholar] [CrossRef]
- Li, A.; Peng, Y.; Taiclet, L.M.; Tanzi, R.E. Analysis of Hidradenitis Suppurativa–Linked Mutations in Four Genes and the Effects of PSEN1-P242LfsX11 on Cytokine and Chemokine Expression in Macrophages. Hum Mol Genet 2019, 28, 1173–1182. [Google Scholar] [CrossRef]
- Ralser, D.J.; Basmanav, F.B.Ü.; Tafazzoli, A.; Wititsuwannakul, J.; Delker, S.; Danda, S.; Thiele, H.; Wolf, S.; Busch, M.; Pulimood, S.A.; et al. Mutations in γ-Secretase Subunit–Encoding PSENEN Underlie Dowling-Degos Disease Associated with Acne Inversa. J Clin Invest 2017, 127, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Kan, T.; Takahagi, S.; Shindo, H.; Tanaka, A.; Kawai, M.; Hide, M. A Unique Clinical Phenotype of a Patient Bearing a Newly Identified Deletion Mutation in the PSENEN Gene along with the Pathogenic Serum Desmoglein-1 Antibody. Clin Exp Dermatol 2018, 43, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Peter, D.C.V.; Smith, F.J.D.; Wilson, N.J.; Danda, S. PSENEN Mutation in Coexistent Hidradenitis Suppurativa and Dowling-Degos Disease. Indian Dermatol Online J 2020, 12, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.-M.; Zhou, P.-J.; Zhu, C.-H.; Lin, L.-H.; Liu, J.-J.; Han, Y. Coexistence of Acne Inversa with Psoriasis and Dowling-Degos Disease Harboring Impaired PSENEN-Notch Signaling. Chin Med J (Engl) 2020, 133, 2383–2385. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Wen, G.-D.; Soe, L.M.; Xu, H.-J.; Du, J.; Zhang, J.-Z. Novel Mutations in PSENEN Gene in Two Chinese Acne Inversa Families Manifested as Familial Multiple Comedones and Dowling-Degos Disease. Chinese Medical Journal 2016, 129, 2834. [Google Scholar] [CrossRef] [PubMed]
- Pavlovsky, M.; Sarig, O.; Eskin-Schwartz, M.; Malchin, N.; Bochner, R.; Mohamad, J.; Gat, A.; Peled, A.; Hafner, A.; Sprecher, E. A Phenotype Combining Hidradenitis Suppurativa with Dowling-Degos Disease Caused by a Founder Mutation in PSENEN. Br J Dermatol 2018, 178, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Li, W.; Xu, H.; Zhang, X.; Su, B.; Zhang, W.; Zhang, X.; Wang, B. PSENEN Mutation Carriers with Co-Manifestation of Acne Inversa (AI) and Dowling-Degos Disease (DDD): Is AI or DDD the Subphenotype? J Invest Dermatol 2017, 137, 2234–2236. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; He, Y.; Xu, H.; Wang, B. First PSENEN Mutation in PASH Syndrome. The Journal of Dermatology 2020, 47, 1335–1337. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Liu, J.; Xu, T.; Guo, Y.; Han, Y.; He, Y.; Lin, L.; Xiao, X. Mutations in γ-Secretase Subunit-Encoding PSENEN Gene Alone May Not Be Sufficient for the Development of Acne Inversa. J Dermatol Sci 2021, 103, 73–81. [Google Scholar] [CrossRef]
- Liu, Y.; Miao, T.; Ma, J.; Shao, L.; Luo, S.; Li, Y.; Liu, Q. PSENEN c.66delG in Sporadic Acne Inversa. Eur J Dermatol 2016, 26, 298–299. [Google Scholar] [CrossRef]
- Chen, A.-W.; Chen, Z.; Bai, X.-M.; Luo, X.-Y.; Wang, H. Successful Treatment of Early-Onset Hidradenitis Suppurativa with Acitretin in an Infant with a Novel Mutation in PSENEN Gene. Indian J Dermatol Venereol Leprol 2022, 88, 445–445. [Google Scholar] [CrossRef]
- Vellaichamy, G.; Dimitrion, P.; Zhou, L.; Ozog, D.; Lim, H.W.; Liao, W.; Hamzavi, I.H.; Mi, Q.-S. Insights from γ-Secretase: Functional Genetics of Hidradenitis Suppurativa. Journal of Investigative Dermatology 2021, 141, 1888–1896. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Yan, Y.; Wang, B. γ-Secretase Genetics of Hidradenitis Suppurativa: A Systematic Literature Review. DRM 2021, 237, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Frew, J.W.; Hawkes, J.E.; Sullivan-Whalen, M.; Gilleaudeau, P.; Krueger, J.G. Inter-Relater Reliability of Phenotypes, and Exploratory Genotype- Phenotype Analysis in Inherited Hidradenitis Suppurativa. Br J Dermatol 2019, 181, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Frew, J.W.; Vekic, D.A.; Woods, J.; Cains, G.D. A Systematic Review and Critical Evaluation of Reported Pathogenic Sequence Variants in Hidradenitis Suppurativa. Br J Dermatol 2017, 177, 987–998. [Google Scholar] [CrossRef] [PubMed]
- Jfri, A.H.; O’Brien, E.A.; Litvinov, I.V.; Alavi, A.; Netchiporouk, E. Hidradenitis Suppurativa: Comprehensive Review of Predisposing Genetic Mutations and Changes. J Cutan Med Surg 2019, 23, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Eble, S.M.; Wisco, O.J.; Boccuto, L.; Laffin, B.; Parker, V.G.; Davis, N.J.; Temples, H.S. Genetic Factors Associated with Hidradenitis Suppurativa, a Literature Review. Int J Womens Dermatol 2024, 10, e158. [Google Scholar] [CrossRef] [PubMed]
- Yudin, A.I.; Generao, S.E.; Tollner, T.L.; Treece, C.A.; Overstreet, J.W.; Cherr, G.N. Beta-Defensin 126 on the Cell Surface Protects Sperm from Immunorecognition and Binding of Anti-Sperm Antibodies1. Biology of Reproduction 2005, 73, 1243–1252. [Google Scholar] [CrossRef]
- Li, Y.; Tang, L.; Yue, J.; Gou, X.; Lin, A.; Weatherbee, S.D.; Wu, X. Regulation of Epidermal Differentiation through KDF1-mediated Deubiquitination of IKKα. EMBO Rep 2020, 21, e48566. [Google Scholar] [CrossRef]
- Körholz, J.; Gabrielyan, A.; Sczakiel, H.L.; Schulze, L.; Rejzek, M.; Laass, M.W.; Leuchten, N.; Tiebel, O.; Aust, D.; Conrad, K.; et al. Novel Mutation and Expanding Phenotype in IRF2BP2 Deficiency. Rheumatology (Oxford) 2023, 62, 1699–1705. [Google Scholar] [CrossRef]
- Sun, Q.; Broadaway, K.A.; Edmiston, S.N.; Fajgenbaum, K.; Miller-Fleming, T.; Westerkam, L.L.; Melendez-Gonzalez, M.; Bui, H.; Blum, F.R.; Levitt, B.; et al. Genetic Variants Associated With Hidradenitis Suppurativa. JAMA Dermatology 2023, 159, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Li, Y.; Xu, H.; Zhang, Y. The γ-Secretase Complex: From Structure to Function. Front Cell Neurosci 2014, 8, 427. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, H.; Li, H.; Kim, B.S.; Shah, S.; Lee, H.-J.; Thinakaran, G.; Kim, T.-W.; Yu, G.; Xu, H. PEN-2 and APH-1 Coordinately Regulate Proteolytic Processing of Presenilin 1. J Biol Chem 2003, 278, 7850–7854. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Morales-Heil, D.J.; Roberson, E.D.O. Nicastrin Haploinsufficiency Alters Expression of Type I Interferon-Stimulated Genes: The Relationship to Familial Hidradenitis Suppurativa. Clin Exp Dermatol 2019, 44, e118–e125. [Google Scholar] [CrossRef] [PubMed]
- Paik, D.; Monahan, A.; Caffrey, D.R.; Elling, R.; Goldman, W.E.; Silverman, N. SLC46 Family Transporters Facilitate Cytosolic Innate Immune Recognition of Monomeric Peptidoglycans. J Immunol 2017, 199, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Hessam, S.; Gambichler, T.; Skrygan, M.; Scholl, L.; Sand, M.; Meyer, T.; Stockfleth, E.; Bechara, F.G. Increased Expression Profile of NCSTN, Notch and PI3K/AKT3 in Hidradenitis Suppurativa. J Eur Acad Dermatol Venereol 2021, 35, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Hessam, S.; Skrygan, M.; Bakirtzi, M.; Kasakovski, D.; Bechara, F.G. NOD2 Signalling in Hidradenitis Suppurativa. Clin Exp Dermatol 2021, 46, 1488–1494. [Google Scholar] [CrossRef] [PubMed]
- Li, H. Aligning Sequence Reads, Clone Sequences and Assembly Contigs with BWA-MEM 2013.
- Li, H. Toward Better Understanding of Artifacts in Variant Calling from High-Coverage Samples. Bioinformatics 2014, 30, 2843–2851. [Google Scholar] [CrossRef]
- Picard Tools - By Broad Institute . Available online: http://broadinstitute.github.io/picard/ (accessed on 14 October 2022).
- Danecek, P.; Bonfield, J.K.; Liddle, J.; Marshall, J.; Ohan, V.; Pollard, M.O.; Whitwham, A.; Keane, T.; McCarthy, S.A.; Davies, R.M.; et al. Twelve Years of SAMtools and BCFtools. GigaScience 2021, 10, giab008. [Google Scholar] [CrossRef]
- Tarasov, A.; Vilella, A.J.; Cuppen, E.; Nijman, I.J.; Prins, P. Sambamba: Fast Processing of NGS Alignment Formats. Bioinformatics 2015, 31, 2032–2034. [Google Scholar] [CrossRef]
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.; Daly, M.; et al. The Genome Analysis Toolkit: A MapReduce Framework for Analyzing next-Generation DNA Sequencing Data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef] [PubMed]
- Poplin, R.; Ruano-Rubio, V.; DePristo, M.A.; Fennell, T.J.; Carneiro, M.O.; Van der Auwera, G.A.; Kling, D.E.; Gauthier, L.D.; Levy-Moonshine, A.; Roazen, D.; et al. Scaling Accurate Genetic Variant Discovery to Tens of Thousands of Samples; Genomics, 2017.
- Quinlan, A.R.; Hall, I.M. BEDTools: A Flexible Suite of Utilities for Comparing Genomic Features. Bioinformatics 2010, 26, 841–842. [Google Scholar] [CrossRef] [PubMed]
- Van der Auwera, G.A.; Carneiro, M.O.; Hartl, C.; Poplin, R.; del Angel, G.; Levy-Moonshine, A.; Jordan, T.; Shakir, K.; Roazen, D.; Thibault, J.; et al. From FastQ Data to High-Confidence Variant Calls: The Genome Analysis Toolkit Best Practices Pipeline. Current Protocols in Bioinformatics 2013, 43, 11.10.1–11.10.33. [Google Scholar] [CrossRef] [PubMed]
- Sherry, S.T.; Ward, M.-H.; Kholodov, M.; Baker, J.; Phan, L.; Smigielski, E.M.; Sirotkin, K. dbSNP: The NCBI Database of Genetic Variation. Nucleic Acids Res 2001, 29, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Cingolani, P.; Platts, A.; Wang, L.L.; Coon, M.; Nguyen, T.; Wang, L.; Land, S.J.; Lu, X.; Ruden, D.M. A Program for Annotating and Predicting the Effects of Single Nucleotide Polymorphisms, SnpEff: SNPs in the Genome of Drosophila Melanogaster Strain w 1118 ; Iso-2; Iso-3. Fly 2012, 6, 80–92. [Google Scholar] [CrossRef] [PubMed]
- Cingolani, P.; Patel, V.M.; Coon, M.; Nguyen, T.; Land, S.J.; Ruden, D.M.; Lu, X. Using Drosophila Melanogaster as a Model for Genotoxic Chemical Mutational Studies with a New Program, SnpSift. Front. Gene. 2012, 3. [Google Scholar] [CrossRef] [PubMed]
- Schubach, M.; Maass, T.; Nazaretyan, L.; Röner, S.; Kircher, M. CADD v1.7: Using Protein Language Models, Regulatory CNNs and Other Nucleotide-Level Scores to Improve Genome-Wide Variant Predictions. Nucleic Acids Res 2024, 52, D1143–D1154. [Google Scholar] [CrossRef] [PubMed]
- Allot, A.; Wei, C.-H.; Phan, L.; Hefferon, T.; Landrum, M.; Rehm, H.L.; Lu, Z. Tracking Genetic Variants in the Biomedical Literature Using LitVar 2.0. Nat Genet 2023, 55, 901–903. [Google Scholar] [CrossRef]
- Steinhaus, R.; Proft, S.; Schuelke, M.; Cooper, D.N.; Schwarz, J.M.; Seelow, D. MutationTaster2021. Nucleic Acids Research 2021, 49, W446–W451. [Google Scholar] [CrossRef]
- Karczewski, K.J.; Francioli, L.C.; Tiao, G.; Cummings, B.B.; Alföldi, J.; Wang, Q.; Collins, R.L.; Laricchia, K.M.; Ganna, A.; Birnbaum, D.P.; et al. The Mutational Constraint Spectrum Quantified from Variation in 141,456 Humans. Nature 2020, 581, 434–443. [Google Scholar] [CrossRef]
- Tordai, H.; Torres, O.; Csepi, M.; Padányi, R.; Lukács, G.L.; Hegedűs, T. Analysis of AlphaMissense Data in Different Protein Groups and Structural Context. Sci Data 2024, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Novati, G.; Pan, J.; Bycroft, C.; Žemgulytė, A.; Applebaum, T.; Pritzel, A.; Wong, L.H.; Zielinski, M.; Sargeant, T.; et al. Accurate Proteome-Wide Missense Variant Effect Prediction with AlphaMissense. Science 2023, 381, eadg7492. [Google Scholar] [CrossRef] [PubMed]
- Hinrichs, A.S.; Karolchik, D.; Baertsch, R.; Barber, G.P.; Bejerano, G.; Clawson, H.; Diekhans, M.; Furey, T.S.; Harte, R.A.; Hsu, F.; et al. The UCSC Genome Browser Database: Update 2006. Nucleic Acids Res 2006, 34, D590–598. [Google Scholar] [CrossRef] [PubMed]
- Jumper, J.; Evans, R.; Pritzel, A.; Green, T.; Figurnov, M.; Ronneberger, O.; Tunyasuvunakool, K.; Bates, R.; Žídek, A.; Potapenko, A.; et al. Highly Accurate Protein Structure Prediction with AlphaFold. Nature 2021, 596, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Buel, G.R.; Walters, K.J. Can AlphaFold2 Predict the Impact of Missense Mutations on Structure? Nat Struct Mol Biol 2022, 29, 1–2. [Google Scholar] [CrossRef]
- Chakravarty, D.; Porter, L.L. AlphaFold2 Fails to Predict Protein Fold Switching. Protein Sci 2022, 31, e4353. [Google Scholar] [CrossRef]
- Valadon, P. RasTop 2007.
- Blum, M.; Chang, H.-Y.; Chuguransky, S.; Grego, T.; Kandasaamy, S.; Mitchell, A.; Nuka, G.; Paysan-Lafosse, T.; Qureshi, M.; Raj, S.; et al. The InterPro Protein Families and Domains Database: 20 Years On. Nucleic Acids Research 2021, 49, D344–D354. [Google Scholar] [CrossRef]
- Bai, X.; Rajendra, E.; Yang, G.; Shi, Y.; Scheres, S.H.W. Sampling the Conformational Space of the Catalytic Subunit of Human γ-Secretase. Elife 2015, 4, e11182. [Google Scholar] [CrossRef] [PubMed]
- Zhou, R.; Yang, G.; Guo, X.; Zhou, Q.; Lei, J.; Shi, Y. Recognition of the Amyloid Precursor Protein by Human γ-Secretase. Science 2019, 363, eaaw0930. [Google Scholar] [CrossRef]
- Burley, S.K.; Bhikadiya, C.; Bi, C.; Bittrich, S.; Chen, L.; Crichlow, G.V.; Christie, C.H.; Dalenberg, K.; Di Costanzo, L.; Duarte, J.M.; et al. RCSB Protein Data Bank: Powerful New Tools for Exploring 3D Structures of Biological Macromolecules for Basic and Applied Research and Education in Fundamental Biology, Biomedicine, Biotechnology, Bioengineering and Energy Sciences. Nucleic Acids Research 2021, 49, D437–D451. [Google Scholar] [CrossRef]
| Individual characteristics | Male | Female | All | ND |
|---|---|---|---|---|
| N | 36 | 64 | 100 | - |
| Age (mean ± sd) | 33.8 ± 12.2 | 34.6 ± 11.1 | 34.0 ± 11.5 | 2 |
| BMI (mean ± sd) | 26.1 ± 4.5 | 27.1 ± 5.1 | 26.8 ± 4.8 | 4 |
| Smoking status | 21 (67.7%) | 44 (72.1%) | 65 (70.6%) | 8 |
| Familial case | 7 (36.8%) | 21 (37.5%) | 28 (37.3%) | 25 |
| IBD history | 0 | 1 (1.8%) | 1 (1.3%) | 25 |
| Rhumatological history | 0 | 2 (3.6%) | 2 (2.7%) | 25 |
| Hurley | ||||
| I (mild) | 4 (12.5%) | 11 (17.2%) | 15 (15.6%) | 4 |
| II (moderate) | 12 (37.5%) | 30 (46.9%) | 42 (43.7%) | |
| III (severe) | 16 (50.0%) | 23 (35.9%) | 39 (40.6%) | |
| Gene | ID | Position (GRCh38) | Ex. | c/p.HGVS | Eff. | rsID | R. | Or. | F/S | Association |
|---|---|---|---|---|---|---|---|---|---|---|
| APH1A (ENST00000369109) | 1 | 1:150267780 | 3 | p.D98E | mis|spl | rs996158631 | 0 | div. | – | – |
| APH1B (ENST00000261879) | 2°N | 15:63277702 | 1 | p.T27A | mis | rs77834210 | 0 | FR* | S | – |
| 3°N | 15:63279258 | 2 | p.L71V | mis | – | 0 | FR* | S | – | |
| 4 | 15:63302375 | 5 | p.H170R | mis | rs139355584 | 2 | div. | F | – | |
| 5°N | 15:63302416 | 5 | p.K185Sfs*10 | fs | rs745918508 | 0 | FR* | S | – | |
| 6 | 15:63305770 | 6 | p.R255C | mis | rs142676640 | 0 | div. | – | – | |
| NCSTN (ENST00000294785) | 7 | 1:160343408 | 1 | p.G6Vfs*22 | fs | rs1266104510 | 0 | div. | – | – |
| 8 | 1:160343434 | 1 | p.G13Efs*15 | fs | – | 3 | DE | S | AC | |
| 9°N | 1:160343443 | 1 | p.L17Sfs*30 | fs | – | 0 | FR* | S | – | |
| 10 | 1:160344733 | 2 | p.G33R | mis|spl | – | 6 | JP | F | – | |
| 11 | 1:160344767 | 2 | p.L44* | non | – | 0 | BR | F | DDD | |
| 12 | 1:160344818 | 2 | p.G61V | mis | – | 3 | FR*|MT* | F | – | |
| 13 | 1:160349018 | 3 | p.V72Yfs*16 | fs | rs1243425689 | 10 | CN | F | – | |
| 14 | 1:160349031 | 3 | p.V75I | mis | rs12045198 | 10 | CN | F | – | |
| 15° | 1:160349039 | 3 | p.E77D | mis | rs35603924 | 0 | div.|FR* | S | – | |
| 16 | 1:160349086 | 3 | p.P93Lfs*15 | fs | – | 8 | CN | FS | SAPHO | |
| 17 | 1:160349578 | 4 | p.T115Nfs*20 | fs | – | 9 | FR* | – | PASH | |
| 18 | 1:160349583 | 4 | p.R117* | non | rs387906896 | 10 | CN|US*|AfUS | F | – | |
| 19 | 1:160349799 | 4-5 | c.436+129A>G | int | rs2274184 | 0 | SG | FS | – | |
| 20 | 1:160350115 | 5 | p.N150Ifs*52 | fs | – | 2 | CN | F | – | |
| 21 | 1:160350118 | 5 | p.S151Qfs*48 | fs | – | 4 | CN | F | – | |
| 22 | 1:160350145 | 5 | p.C159* | non | – | 9 | CN|GR* | F | – | |
| 23 | 1:160350150 | 5 | p.I162Yfs*40 | fs | – | 1 | IT* | S | PASH/SAPHO | |
| 24 | 1:160350155 | 5 | p.Q163Sfs*39 | fs | – | 10 | FR | F | – | |
| 25 | 1:160350165 | 5 | p.S166* | non | – | 6 | CN | F | – | |
| 26 | 1:160350221 | 5 | p.D185N | mis | rs201293070 | 9 | GB* | S | Diab | |
| 27 | 1:160350251 | 5-6 | c.582+1del(G) | spl* | – | 10 | JP | F | – | |
| 28 | 1:160350251 | 5-6 | c.582+1G>A | spl | rs1373027391 | 0 | SG | FS | – | |
| 29 | 1:160351256 | 6 | p.S206* | non | – | 7 | CN* | F | – | |
| 30 | 1:160351271 | 6 | p.P211R | mis | – | 10 | CN | S | – | |
| 31 | 1:160351286 | 6 | p.Q216P | mis | – | 9 | CN|MT* | F | – | |
| 32 | 1:160351310 | 6 | p.V224_T227del | del | – | 3 | MT | F | – | |
| 33 | 1:160351325 | 6 | p.C230Pfs*32 | fs | – | 8 | CN|IN | F | AC | |
| 34 | 1:160351713 | 7 | p.L251Vfs*2 | fs | – | 3 | CN | F | Com | |
| 35 | 1:160351755 | 7 | p.T265Nfs*8 | fs | – | 2 | CN | F | – | |
| 36 | 1:160352097 | 8 | p.E296G | mis | rs758910156 | 7 | CN|MT* | F | – | |
| 37°N | 1:160352104 | 8 | p.A300Wfs*20 | fs | – | 0 | FR* | F | – | |
| 38 | 1:160352154 | 8 | p.A315V | mis | rs1553210405 | 9 | CN | F | – | |
| 39 | 1:160352188 | 8 | p.M326Ifs*31 | fs | – | 5 | SG | – | – | |
| 40 | 1:160352207 | 8-9 | p.E333Q367del(x9) | spl* | – | 5 | GB | F | – | |
| 41 | 1:160352213 | 8-9 | c.996+7G>A | int | rs202046846 | 9 | GB*|FR* | S | AC|Diab | |
| 42 | 1:160352992 | 9-10 | c.1101+1G>A | spl | rs1347055289 | 10 | GB | F | – | |
| 43 | 1:160353001 | 9-10 | c.1101+10A>G | int | rs1048828525 | 9 | GB* | S | – | |
| 44 | 1:160353198 | 10 | p.D381Sfs*7 | fs | – | 1 | IT* | S | PAPASH | |
| 45° | 1:160354113 | 10-11 | c.1180-5C>G | int | rs7528638 | 5 | GB|FR* | F | – | |
| 46 | 1:160354167 | 11 | p.A410V | mis | rs147225198 | 6 | US* | S | – | |
| 47° | 1:160354187 | 11 | p.N417Y | mis | rs143039637 | 0 | div.|FR* | S | – | |
| 48 | 1:160354190 | 11 | p.Q418* | non | – | 0 | div. | – | – | |
| 49 | 1:160354196 | 11 | p.Q420* | non | – | 10 | CN|SG|div. | F | – | |
| 50° | 1:160354223 | 11 | p.R429* | non | rs771414318 | 5 | JP|FR* | F | – | |
| 51 | 1:160354232 | 11 | p.R432* | non | – | 3 | CN* | FS | KTS | |
| 52 | 1:160354238 | 11 | p.R434* | non | rs1085307081 | 10 | CN|ES*|FR | F | DDD | |
| 53 | 1:160354263 | 11 | p.D443Lfs*6 | fs | – | 3 | ES* | – | DDD | |
| 54 | 1:160354291 | 11-12 | c.1352+1G>A | spl | – | 9 | CN | F | – | |
| 55 | 1:160354194 | 11 | c.1381del(C) | fs | – | 2 | FR* | F | – | |
| 56 | 1:160355941 | 13 | p.Q512* | non | – | 3 | CN* | F | – | |
| 57 | 1:160355959 | 13-14 | p.A486_T517del(x13) | spl* | rs1553210984 | 9 | CN | F | – | |
| 58 | 1:160356263 | 14 | p.T519Nfs*10 | fs | – | 3 | CN | S | – | |
| 59 | 1:160356343 | 14 | p.Y545* | non | – | 8 | IR | F | PASH | |
| 60 | 1:160356655 | 15 | p.Y565* | non | – | 10 | CN | F | – | |
| 61 | 1:160356662 | 15 | p.Q568* | non | – | 9 | JP | F | – | |
| 62 | 1:160356687 | 15 | p.G576V | mis | – | 3 | FR*|MT* | F | – | |
| 63 | 1:160356707 | 15 | p.R583* | non | – | 3 | IT* | F | DDD | |
| 64 | 1:160356712 | 15 | p.E584Dfs*44 | fs | rs1553211087 | 10 | CN | F | – | |
| 65 | 1:160356728 | 15 | p.S590G/p.S590Afs*3 | mis|spl | – | 10 | FR | F | – | |
| 66 | 1:160357046 | 16 | p.Y600* | fs | – | 6 | CN|IN | FS | AC | |
| 67 | 1:160357122 | 16 | p.R626* | non | – | 3 | ES*|IN | F | DDD|AC | |
| 68 | 1:160357161 | 16 | p.Q639Gfs*31 | fs | – | 5 | NL | F | – | |
| 69°N | 1:160357189 | 16 | p.W648* | non | – | 0 | FR* | S | – | |
| 70 | 1:160358788 | 3’ | c.*517_*518del(CA) | utr | rs141849450 | 4 | CN | S | – | |
| PSEN1 (ENST00000324501) | 71 | 14:73186897 | 6 | p.S178Ffs*10 | fs | rs1174374799 | 0 | div. | – | – |
| 72 | 14:73192820 | 7 | p.P242Lfs*11 | fs | rs1595035030 | 10 | CN | F | – | |
| 73° | 14:73198145 | 8-9 | c.868+16G>T | int | rs165932 | 4 | CN|div.|FR* | S | Ps | |
| 74° | 14:73206470 | 9 | p.E318G | mis|spl | rs17125721 | 8 | GB|div.|FR* | F | – | |
| 75°N | 14:73211786 | 10 | p.Q325E | mis | – | 0 | FR* | S | – | |
| 76 | 14:73217163 | 11 | p.S390Efs*20 | fs | – | 3 | FR* | F | Crohn | |
| 77° | 14:73217252 | 11-12 | c.1248+8T>C | int | rs362382 | 0 | div.|FR* | S | – | |
| PSEN2 (ENST00000366783) | 78°N | 1:226882007 | 4 | p.G34S | mis | rs200636353 | 0 | FR* | S | – |
| 79 | 1:226894073 | 12 | p.T380K | mis | rs143912759 | 0 | div. | – | – | |
| PSENEN (ENST00000587708) | 80 | 19:35745943 | 2 | p.R5* | non | – | 3 | CN | F | – |
| 81 | 19:35745965 | 2 | p.L12* | non | rs1555738763 | 5 | DE | – | DDD | |
| 82 | 19:35745973 | 2 | p.C15Pfs*101 | fs | – | 5 | JP | F | AC | |
| 83 | 19:35746418 | 2-3 | p.G21_Y56del(x3) | spl* | rs1555738836 | 4 | IN | F | DDD | |
| 84 | 19:35746418 | 2-3 | c.62-1G>T | spl | – | 5 | IN* | F | DDD | |
| 85 | 19:35746423 | 3 | p.F23Vfs*98 | fs | rs1555738837 | 10 | GB*|FR* | FS | DDD | |
| 86 | 19:35746423 | 3 | p.F23Lfs*46 | fs | rs1555738837 | 10 | CN | FS | DDD|Ps | |
| 87 | 19:35746441 | 3 | p.L29Sfs*92 | fs | – | 3 | TH | F | DDD | |
| 88 | 19:35746472 | 3 | p.R39* | non | – | 5 | DE | – | DDD | |
| 89 | 19:35746525 | 3-4 | p.G21_Y56del(x3) | spl* | rs1970575677 | 5 | FR | F | DDD | |
| 90 | 19:35746706 | 3-4 | c.167-2A>G | spl | rs1555738903 | 7 | CN | F | DDD | |
| 91 | 19:35746709 | 4 | p.Y56* | non | rs751542345 | 8 | Jash|FR* | F | DDD|IBD|PS | |
| 92 | 19:35746735 | 4 | p.L65R | mis | rs1555738906 | 7 | CN | F | Com|DDD | |
| 93 | 19:35746756 | 4 | p.S73Pfs*72 | fs | – | 1 | DE | – | DDD | |
| 94 | 19:35746769 | 4 | p.I77Hfs*45 | fs | – | 1 | CN | F | PASH | |
| 95 | 19:35746770 | 4 | p.I77Tfs*45 | fs | – | 4 | CN* | F | DDD | |
| 96 | 19:35746812 | 4 | p.Y91Tfs*54 | fs | – | 2 | div. | F | – | |
| 97 | 19:35746819 | 4 | p.F94Sfs*51 | fs | rs1555738943 | 9 | CN | F | – | |
| 98 | 19:35746833 | 4 | p.L98Wfs*47 | fs | – | 2 | div. | F | – | |
| 99 | 19:35746845 | 4 | p.*102Rxt*50 | elg | – | 3 | FR* | – | DDD|Diab |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





