1. Introduction
Decompressive craniectomy (DC) is a surgical procedure used to alleviate increased intracranial pressure (ICP) in patients with severe brain injury. It involves the removal of a portion of the skull to allow a swollen brain to expand without being compressed [
1]. This procedure is typically employed in cases of Traumatic Brain Injury (TBI), stroke, or other forms of acquired brain injury where medical management of ICP fails [
2]. Cranioplasty (CP) is the surgical procedure to repair the skull defect created during DC [
3]. It involves replacing the removed bone flap or using synthetic materials to cover the opening. The primary goals are to protect the brain, restore the normal appearance of the skull, and potentially improve neurological function [
4].
Through the restoration of normal vascular circulation and cerebrospinal fluid, CP is successful in lowering mortality and improving clinical outcomes [
2]. However, despite being a routine neurosurgical treatment, CP has a high likelihood of complications [
5]. Up to 34% of CP procedures have complications [
6]. Infection, hygroma, hydrocephalus, seizures, reoperations, cerebral bleeding, bone resorption, flap depression, and wound dehiscence are some of these problems. For this reason, Considering the high complication rates of cranioplasty, the definition of the best timing of cranioplasty after DC is mandatory. Nowadays, there is no definitive association between the time intervals between CP intervention and clinical outcomes. Routinely, a delayed scheduling of CP (after 3 months from DC) is conventionally performed, but many surgeons have questioned the benefits of cranial repair at an early stage (1-3 months after DC) [
7]. However, until now there is a large disagreement persisting about what constitutes "early" CP [
4].
Relevant specialists came to an agreement at the most recent International Neurotraumatology Progress Conference [
8] and suggested that the time of CP be described in four phases starting from after craniotomy and decompression:
Ultra-Early: <6 weeks;
Early: from 6 weeks to 3 months; Intermediate: 3–6 months; Late: >6 months. This has led many clinicians to draw attention to the disparities in outcomes between the ultra-early or early interventions, although consistent findings have never reported that could suggest prescribing earlier or later CP in order to increase the likelihood of clinical recovery [
4,
5]. For instance, Aloraidi et al., [
5] reported no differences in clinical outcome between early or late CP, whereas for Xu et al., [
4], early CP can only shorten the amount of time needed for surgery, but it cannot lessen patient complications.
Therefore, to better delineate the consequence of CP in late TBI, in this study we describe, for the first time, the clinical characteristics and course of a patient with TBI after 19 months from DC and 6 months after CP intervention.
2. Case Report History
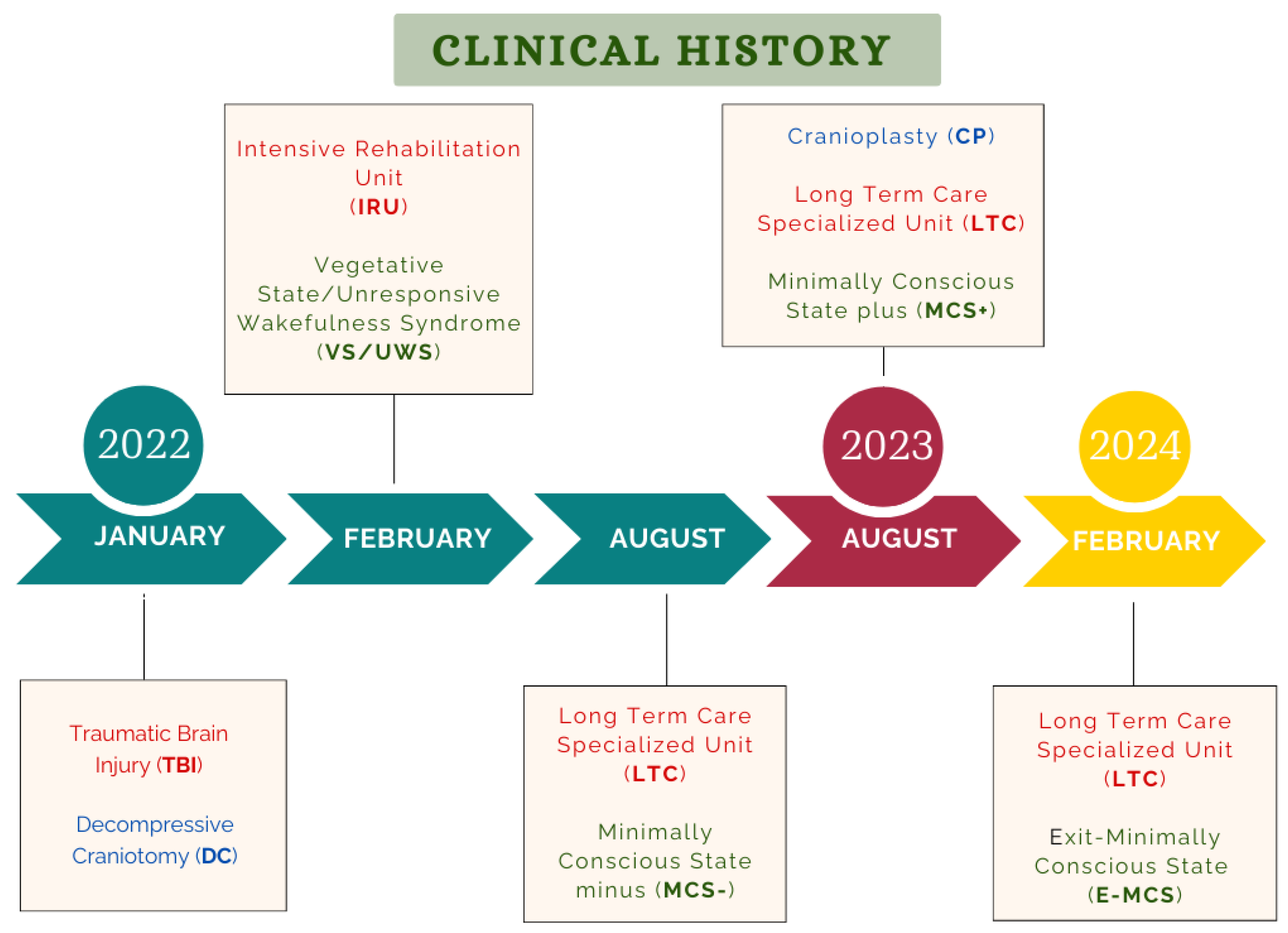
Clinical history and treatment have been described in
Figure 1. On January 1st, 2022, a 26-year-old man fell from a height of four floors due to an intentional attempt. His past medical history was unremarkable except for a referred cocaine abuse. He was immediately brought to the emergency facility in an unresponsive consciousness state (Glasgow Coma Scale-GCS= 4), requiring intubation and hemodynamic support. He underwent an urgent right fronto-temporo-parietal DC because of intracranial hypertension. The patient was later transferred to the Intensive Care Unit (ICU) of the City Hospital with the diagnosis of Vegetative State/Unresponsive Wakefulness Syndrome (VS/UWS; Level of Cognitive Functioning-LCF= 2). The legal representative gave written informed consent.
On February 21st, 2022, the patient was admitted to the Intensive Rehabilitation Unit (IRU). At admission, the patient was awake with no signs of awareness (VS/UWS). He breathed through a tracheostomy. A percutaneous gastrostomy was present to ensure proper caloric intake and internal hydration. Craniectomy scar showed no signs of dehiscence with optimal healing. However, a brain bulging through the craniectomy window was observed.
The legal representative gave written informed consent. The study was approved by the Central Area Calabria Region in Catanzaro (Protocol No. 343. Oct. 21, 2021).
Admission Computer Tomography (CT) scan revealed evidence of a right fronto-parietal hygroma, a pathological enlargement of the ventricular system, particularly on the right at the occipital horn, protrusion of the brain parenchyma at the craniectomy site, a hypodense area that affected the right thalamus.
During the neurorehabilitation stay, the patient underwent daily passive mobilization, respiratory rehabilitation with prone position and copping, and unimodal sensitive stimulations. The neurologic state was monitored weekly. He was gradually weaned from tracheostomy.
The patient demonstrated a shift from VS/UWS to a Minimally Conscious State (MCS; LCF:3) during the six-month IRU stay. In this period, patient’s caregivers disagreed with cranioplasty intervention, due to fear of complications from surgery. For this reason, in addition with urinary recurrent infections, the patient was not treated with reconstructive cranioplasty.
On August 9, 2022, the patient was moved to a Long-Term Care Specialized Unit (LTC), in agreement with his caregivers. During the LTC stay, the patient underwent the following rehabilitative treatments: multiprofessional nursing, including activities like monitoring vital signs, giving medications, managing and treating gastrostomy to maintain proper hydration and nutritional intake, etc.; respiratory physiotherapy and mobilization; speech therapy and observation for maintaining and enhancing bucco-lingual-facial muscle tonicity; recovering the automatism of swallowing. Additionally, depending on the level of cognitive functioning, laryngeal shield stimulations, global stimulations, gustatory stimulations, and specific and non-specific neurosensory stimulations of the oral cavity and peri-buccal area are given. Multisensory stimulation protocol, including visual, auditory, tactile and emotional stimulations created ad hoc with the caregiver’s assistance. This treatment was performed twice a week according to Wood’s protocol [
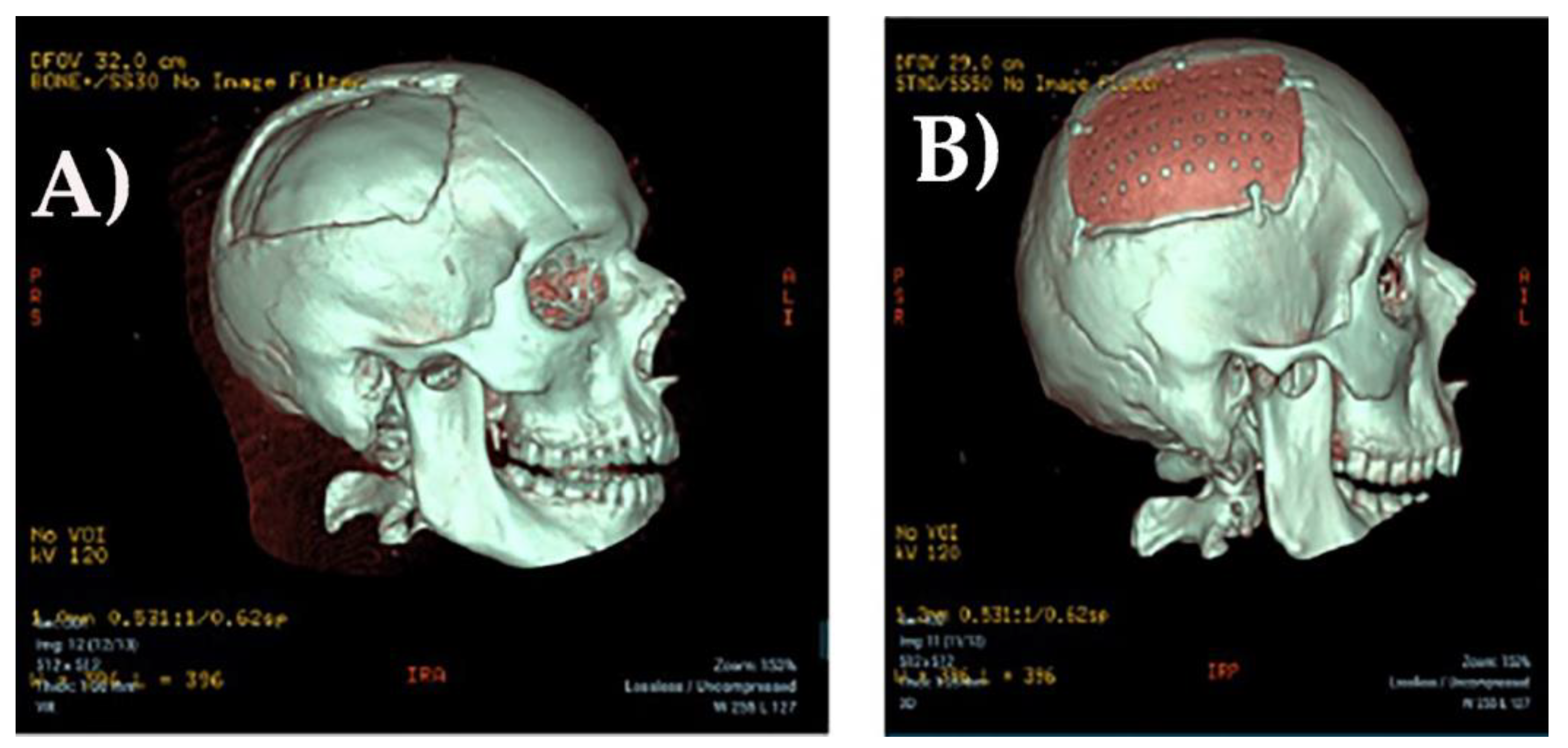
9]. The multiprofessional team who was responsible for patient care, including physician, physiotherapist and psychologist, persuaded the family for neurosurgery reintervention. Thus, one year after LTC admission, on August 17th 2023, the patient received a custom-made CP implant.
Cranioplasty Intervention
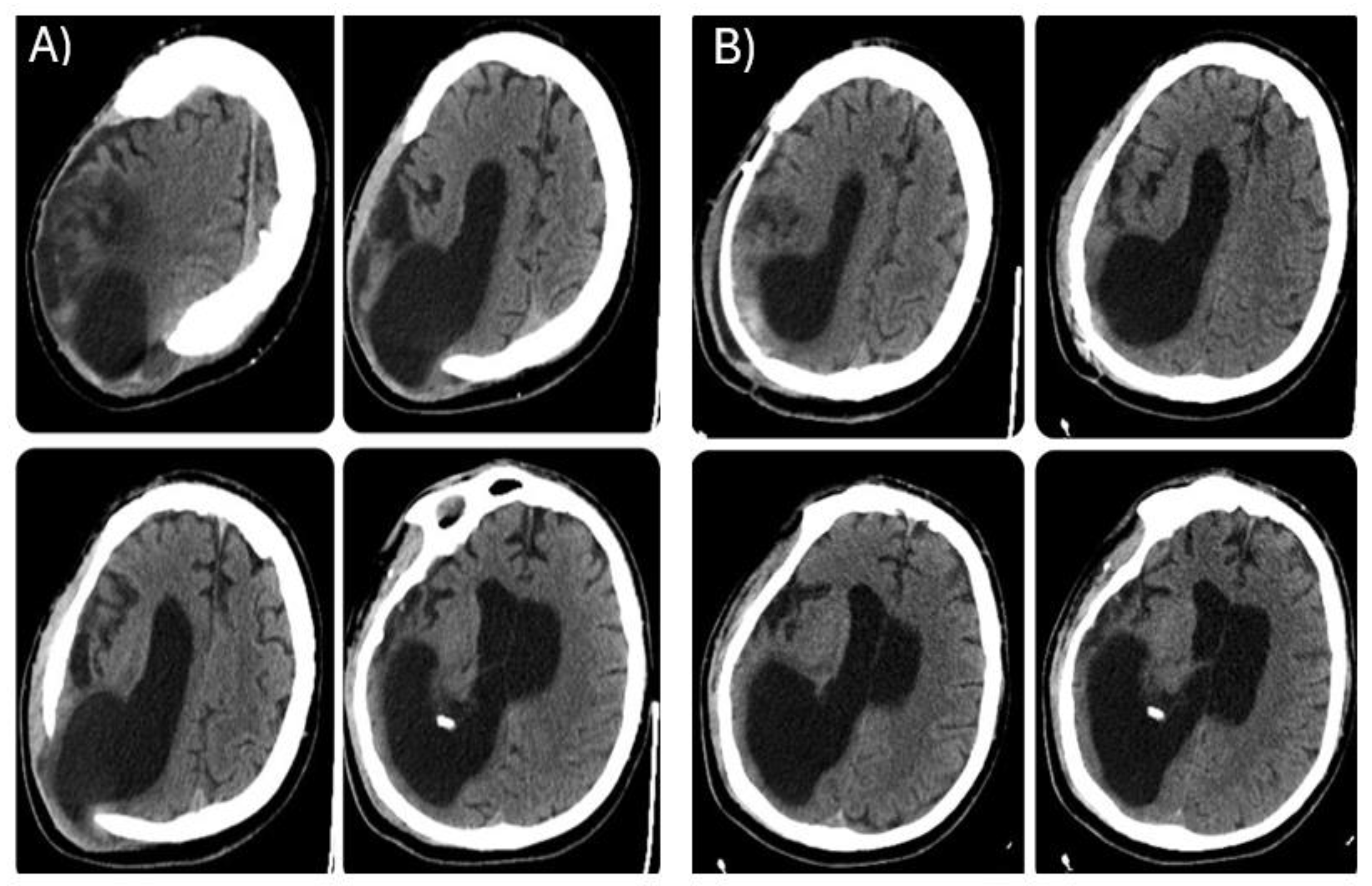
During the LTC stay, the patient was monitored with repeated CT scans. The last brain CT carried out before reconstructive cranioplasty (
Figure 2A), showed further right occipital horn enlargement with persistence of brain parenchyma protrusion at the craniectomy site. One month after CP, a CT scan was repeated revealing patches of blood-type hyperdensity in the cortico-subcortical location corresponding to the posterior horn of the right lateral ventricle at the surgical site with persistent significant right ventricle dilatation (
Figure 2B).
Clinical Assessment
Four distinct time points were used for clinical and behavioural evaluations of the level of consciousness: at IRU admission and during LTC stay, before CP, following CP and 6-month follow-up after CP. Clinical battery included: a) Levels of Cognitive Functioning-Revised (LCF-R); b) Glasgow Outcome Scale-Extended (GOSE-E); c) Disability Rating Scales (DRS); d) Barthel Index (BI); e) Early Rehabilitation Barthel Index (ERBI); f) Glasgow Coma Scale (GCS); g) Brief Post-Coma Scale (BPCS); h) Coma Recovery Scale-Revised (CRS-R); i) Wessex Head Injury Matrix (WHIM); l) Nociception Coma Scale (NCS).
3. Results
Table 1 reported the clinical assessments before and after the CP during the clinical course.
Overall, the patient's clinical condition improved after CP, as demonstrated by LCF, CRS-R, NCS, GCS, WHIM and BPCS measurements. This result is in line with the ability of the aforementioned scales in specifically investigating consciousness and cognitive functioning. He was able to interact with the outside world, albeit less erratically and fluctuating, and they exhibit behavioral signs of awareness and response. Consequently, Exit-SMC is the diagnosis made following CP, according to Bruno et al., [
10].
We were able to distinguish between VS/UVRS and MCS in the patient with reduced consciousness thanks to the BPCS evaluation. Because of the patient's poor eye tracking and visual attention before CP, he doubles his value (from 1.5 to 3) after CP. After the neurosurgical procedure, eye tracking and visual fixation were completely recovered, however spontaneous movements at the upper and/or lower limbs remained unaltered.
According to the results of the CRS-R assessment, the patient was able to carry out repetitive actions, recognize objects, give voluntary, automatic reactions, vocalize and move their mouth, communicate purposefully, and show signs of awareness and attention.
The NCS evaluation showed a rise in scores from 5 to 8. In particular, the motor response changed from abnormal posturing (slow, stereotyped flexion or extension of the upper and/or lower extremities) to flexion withdrawal (there is isolated flexion withdrawal of at least one limb, the limb must move away from the point of stimulation) in response to the proprioception of pain, while the facial expression remained unchanged. The auditory response shifted from groaning (which is defined as groans that aren't spontaneous) to vocalization/oral movement (that is, from at least one instance of non-reflexive oral movement or vocalization in response to stimulation), and the visual response shifted from eye movements (which are anarchical eye movements in response to noxious stimulation) to fixation (which is defined as shifting from the initial fixation point and fixating the examiner for longer than two seconds).
The WHIM examination also confirmed an increase in the score from 49/30 to 57/41. The patient has proven that he can disregard distractions (such as averting his attention from a conversation to attend to someone else), mimic a gesture when asked to do so, and indicate understanding by nodding his head or making other movements while accurately responding to nine out of ten questions; Find a specific playing card from a group of four and select it, answering properly to nine out of ten questions; report the time of day using binary answers of yes and no; use your eyes to point between two images, real objects, or cards that have the right answers to nine out of ten questions.
No evident clinical improvements were instead detected by Barthel, DRS, ERBI and GOS-E scales. This observation was also predictable, because these are predominantly disability scales that score patient motor functional capability. The patient was able to interact with the outside world, albeit erratically and with fluctuations, and exhibited behavioural signs of awareness and response.
4. Discussion
In this study, we observed that even after more than 19 months from DC, a late CP may induce a relevant functional recovery with emergence from an MCS. In particular, the clinical and cognitive improvement was characterized by a meaningful functional recovery with emergence from a minimally conscious state and a more focused and defined response (avoidance of pain, blinking at intense light stimulation, head turning toward sound, fixing and following with one's gaze); reactions to uncomfortable situations (exhibit oppositional attitudes and more pertinent facial expressions); and ability to comply with both simple and complex commands. The clinical variation we noted was mainly a cognitive variation with a severe residue motor disability. In fact, albeit emerging from MCS, the patient was persistently dependent on daily living activities.
Our study confirmed the consensus about the lack of definitive association between the time intervals of CP intervention and clinical outcomes [
8]. Research has shown that cranioplasty can be performed weeks or months following craniectomy. In general, cranioplasty is carried out 3-6 months after DC, or longer if the surgical site becomes infected [
11]. We confirmed that a late CP intervention should be performed in a patient with a severe TBI who has had the injury for a long time [
12]. The similarity in neurological outcome between TBI patients underwent early versus late CP has been reported by Aloraidi [
5], who described not statistically significant differences in the rates of overall postoperative complications between early versus late CP. Iaccarino et al., [
8] confirmed this finding, highlighting that the odds of infections, reoperations, intracranial haemorrhage, and seizures did not appear different between early and late cranioplasty. Similarly, Corallo et al., (2015) demonstrated no significant difference between patients early with respect to delayed CP. This later finding contrasts with other studies that suggested prescribing earlier CP in order to increase the likelihood of clinical recovery (Malcolm et al., 2018; Ozoner, 2021). Despite, Archavlis et al., [
13] found that deep wound infections and osteomyelitis seem to be more common in people with early CP and several concomitant illnesses.
5. Conclusions
Our results suggest that delayed post-DC cranioplasty can improve long-term MCS patients’ functional recovery. CP may still help improve clinical outcomes several months after the traumatic event, in contrast to previous studies that emphasised the significance of this type of treatment mainly in the early phases of the clinical course of patients with VS/UWS or MCS.
Author Contributions
Conceptualization, M.C., F.S., and M.E. P.; methodology, M.C., F.S., M.E.P..; investigation, M.C., F.S., M.E.P., M.G.R.; F.L.L.; data curation, M.C., F.S.; writing—original draft preparation, M.C., F.S., M.E.P. and A.C.; writing—review and editing, M.C., F.S., M.E.P. and A.C.; supervision, M.G.R.; F.L.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ethical Committee of the Central Area Regione Calabria of Catanzaro (Protocol n. 343. October 21, 2021). All procedures performed in this study involving human participant were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Written informed consent has been obtained from the legal representative to publish this paper.
Acknowledgments
Nothing to declare.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Mraček, J.; Mork, J.; Dostal, J.; Tupy, R.; Mrackova, J.; Priban, V. Complications following decompressive craniectomy. J Neurol Surg A Cent Eur Neurosurg. 2021, 82, 437–45. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Xue, Q.; Chen, J.; Dong, Y.; Hou, L.; Jiang, Y.; Wang, J. Decompressive craniectomy in the management of intracranial hypertension after traumatic brain injury: a systematic review and meta-analysis. Sci Rep 2017, 7, 8800. [Google Scholar] [CrossRef] [PubMed]
- Ozoner, B. Cranioplasty following severe traumatic brain injury: role in neurorecovery. Curr Neurol Neurosci Rep. 2021, 21, 62. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Niu, C.; Fu, X.; Ding, W.; Ling, S.; Jiang, X.; Ji, Y. Early cranioplasty vs. late cranioplasty for the treatment of cranial defect: A systematic review. Clin Neurol Neurosurg. 2015, 136, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Aloraidi, A.; Alkhaibary, A.; Alharbi, A.; Alnefaie, N.; Alaglan, A.; AlQarni, A.; Elarjani, T.; Arab, A.; Abdullah, J.M.; Almubarak, A.O.; Abbas, M.; Khairy, I.; Almadani, W.H.; Alowhaibi, M.; Alarifi, A.; Khairy, S.; Alkhani, A. Effect of cranioplasty timing on the functional neurological outcome and postoperative complications. Surg Neurol Int. 2021, 12, 264. [Google Scholar] [CrossRef] [PubMed]
- Gooch, M.R.; Gin, G.E.; Kenning, T.J.; German, J.W. Complications of cranioplasty following decompressive craniectomy: Analysis of 62 cases. Neurosurg Focus. 2009, 26, E9. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, K.M.; Kashuk, J.; Moore, E.E.; Bolles, G.; Rabb, C.; Seinfeld, J.; Szentirmai, O.; Sauaia, A. Cranioplasty after postinjury decompressive craniectomy: is timingof the essence? J Trauma 2010, 69, 270–4. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, C.; Kolias, A.; Adelson, P.D.; Rubiano, A.M.; Viaroli, E.; Buki, A.; Cinalli, G.; Fountas, K.; Khan, T.; Signoretti, S.; Waran, V.; Adeleye, A.O.; Amorim, R.; Bertuccio, A.; Cama, A.; Chesnut, R.M.; De Bonis, P.; Estraneo, A.; Figaji, A.; Florian, S.I.; Formisano. R.; Frassanito, P.; Gatos, C.; Germanò, A.; Giussani, C.; Hossain, I.; Kasprzak, P.; La Porta, F.; Lindner, D.; Maas, A.I.R.; Paiva, W.; Palma, P.; Park, K.B.; Peretta, P.; Pompucci, A.; Posti, J.; Sengupta, S.K.; Sinha, A.; Sinha, V.; Stefini, R.; Talamonti, G.; Tasiou, A.; Zona, G.; Zucchelli, M.; Hutchinson, P.J.; Servadei, F. Consensus statement from the international consensus meeting on post-traumatic cranioplasty. Acta Neurochir (Wien) 2021, 163, 423–440. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.; Winkowski, T.B.; Miller, J.L.; Tierney, L.; Goldman, L. Evaluating sensory regulation as a method to improve awareness in patients with altered states of consciousness: a pilot study. Brain Injury 1992, 6, 411–8. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.A.; Vanhaudenhuyse, A.; Thibaut, A.; Moonen, G.; Laureys, S. From unresponsive wakefulness to minimally conscious PLUS and functional locked-in syndromes: recent advances in our understanding of disorders of consciousness. J Neurol 2011, 258, 1373–84. [Google Scholar] [CrossRef] [PubMed]
- Corallo, F.; Calabrò, R.S.; Leo, A.; Bramanti, P. Can cranioplasty be effective in improving cognitive and motor function in patients with chronic disorders of consciousness? A case report. Turk Neurosurg 2015, 25, 193–6. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Xiaofeng, Y.; Weiguo, L.; Gang, S.; Xuesheng, Z.; Fei, C.; Gu, L. Cranioplasty of large cranial defect at an early stage after decompressive craniectomy performed for severe head trauma. J. Craniofac Surg 2007, 18, 526–32. [Google Scholar] [CrossRef] [PubMed]
- Archavlis, E.; Carvi YNievas, M. The impact of timing of cranioplasty in patients with large cranial defects after decompressive hemicraniectomy. Acta Neurochir (Wien). 2012, 154, 1055–62. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).