Introduction
Long COVID is a condition that
occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis [
1]
. Long COVID is associated with poor quality of life due to persistent symptoms such as fatigue, dyspnoea, anosmia, sleep disturbances and worsening of mental health [
2]
.
As the population with long COVID is growing, this becomes a significant impact on health care systems. An estimation of 2.0 million people in the UK (3.0% of the population) were experiencing long COVID and 380,000 (19%) reporting that their ability to undertake their day-to-day activities had been ‘limited a lot’ [
3]
.
Assessment and management by multidisciplinary teams play a key role in rehabilitation of long COVID patients [
4,
5,
6]
. Therefore, it is crucial for the long COVID services to perform holistic assessments and monitor symptoms’ progression, in order to provide more efficient support by addressing patients’ needs.
Several tools have been developed to assess severity and progress of long COVID symptoms such as Symptom Burden Questionnaire for Long COVID (SBQ-LC) [
7], My Long COVID Needs [
8], and the COVID-19 Yorkshire Rehabilitation Score (
C19-YRS) which was developed by a multidisciplinary team of rehabilitation research professionals from the University of Leeds
in June 2020 to assess the severity of the symptoms and rehabilitation process of long COVID patients [
9]
. C19-YRS is clinically useful and satisfied standard psychometric criteria. Furthermore C19-YRS has demonstrated good internal consistency, a satisfactory scaling and targeting assumptions [
10], and the ability to demonstrate patterns of clinical severity of LC [
11] . C19-YRS is also recommended by National Health Service in England (NHSE) [
12], and National Institute for Health and Care Excellence (NICE)[
13]. However, there is currently little evidence on the feasibility of the C19-YRS in tracking symptoms before and after a LC-specific rehabilitation intervention, and as such little data is available on how symptoms of LC sufferers may change as a result.
This study was set within a LC rehabilitation clinic in Manchester, UK. The clinic is supported by two general practitioners (GPs) with special interest in LC, two respiratory consultants, physiotherapists, occupational therapists, therapy assistants, and specialist nurses, with pathways linked to psychology service, speech and language therapists and dietitians. The clinic also arranges investigations such as blood tests and pulmonary function tests. Patients who have complex and persistent symptoms after physiotherapy and other support interventions at clinic are referred to LC multidisciplinary team meeting where specialists such as respiratory physicians with special interest in long COVID, cardiologists, endocrinologists and psychiatrists are involved.
Methods and Study Population
This is a retrospective analysis as part of service improvement of the C19-YRS assessments submitted digitally via ELAROS application [
14], by patients who attended the LC Rehabilitation clinics during 18-month period (June 2021 to November 2022).
Inclusion criteria
1.Patients referred to the LC Rehabilitation clinic, downloaded and used the ELAROS Application and completed the initial assessment, AND
2.have completed at least one further follow up assessment, using the ELAROS application at least 6 weeks after the initial assessment (patients have undergone LC rehabilitation during this period).
Exclusion criteria
1.patients who did not meet the inclusion criteria
2.Patients who met the inclusion criteria but their submitted assessments had significantly missing data (>25%)
The original version of C19-YRS was used in this study, with 22 patient-reported outcome measures on numerical scale of 0 to 10.
16 patient-reported outcomes of a total of 22 items were assessed – breathlessness at rest, breathlessness on dressing, breathlessness on walking up a flight of stairs, cough/ throat sensitivities, difficulty in swallowing, fatigue, continence issue, pain/ discomfort, problems with cognition, anxiety, depression, PTSD screen, communication problems, issues with personal care, issues with ADLS, issues with caring for family/ social life and overall health. The study did not meet the criteria for needing ethical approval.
A total of 50 patients have submitted 186 assessments during their attendance, and eligible initial and final assessments (100) were analysed.
Results
Patients were referred by GP, respiratory clinics, and some self-referred. The interval between index infection and the first C19-YRS assessment was 4 – 107 weeks (mean of 33.6 weeks). The majority of patients were white British females, from the Salford area in Greater Manchester, UK. The mean age was 48.82 years (
Table 1).
Majority of the patients (70%) completed their final C19-YRS assessment within 26 weeks from their initial assessment (mean 24.82).On the initial assessments, 82% of patients reported worsening of their overall health conditions after acquiring COVID-19 infection. On the second assessment (which was after completing LC rehabilitation intervention), 46% of patients have seen improvement in their overall health and 28% had no change in symptoms.
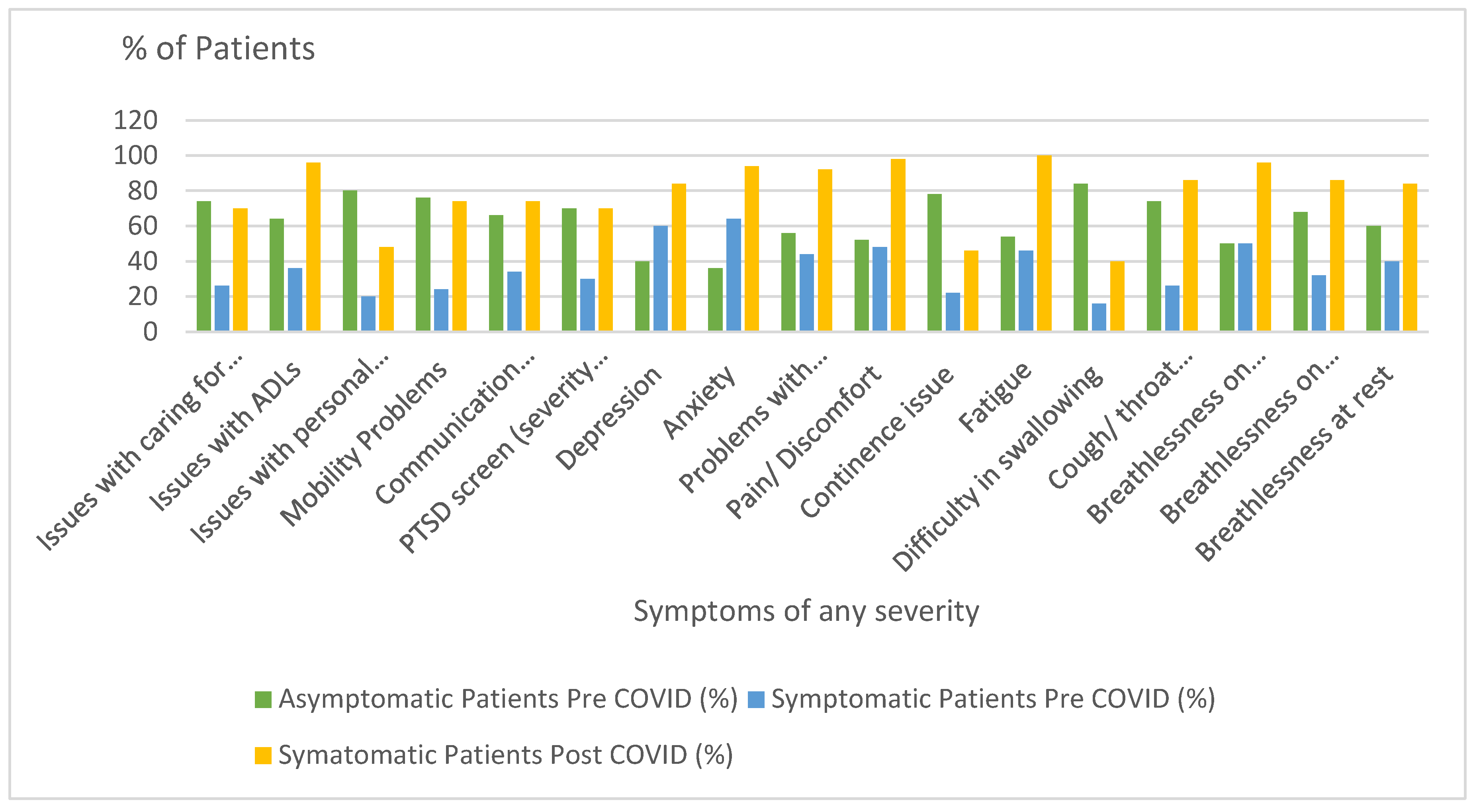
There was variation in pre-COVID symptoms in patients ranging from 16% for problems with swallowing to 64% for anxiety. However, following COVID-19 infection, the number of patients who reported new symptoms or worsening of their baseline symptoms has increased (
Figure 1). Fatigue was the most common symptom in this sample.
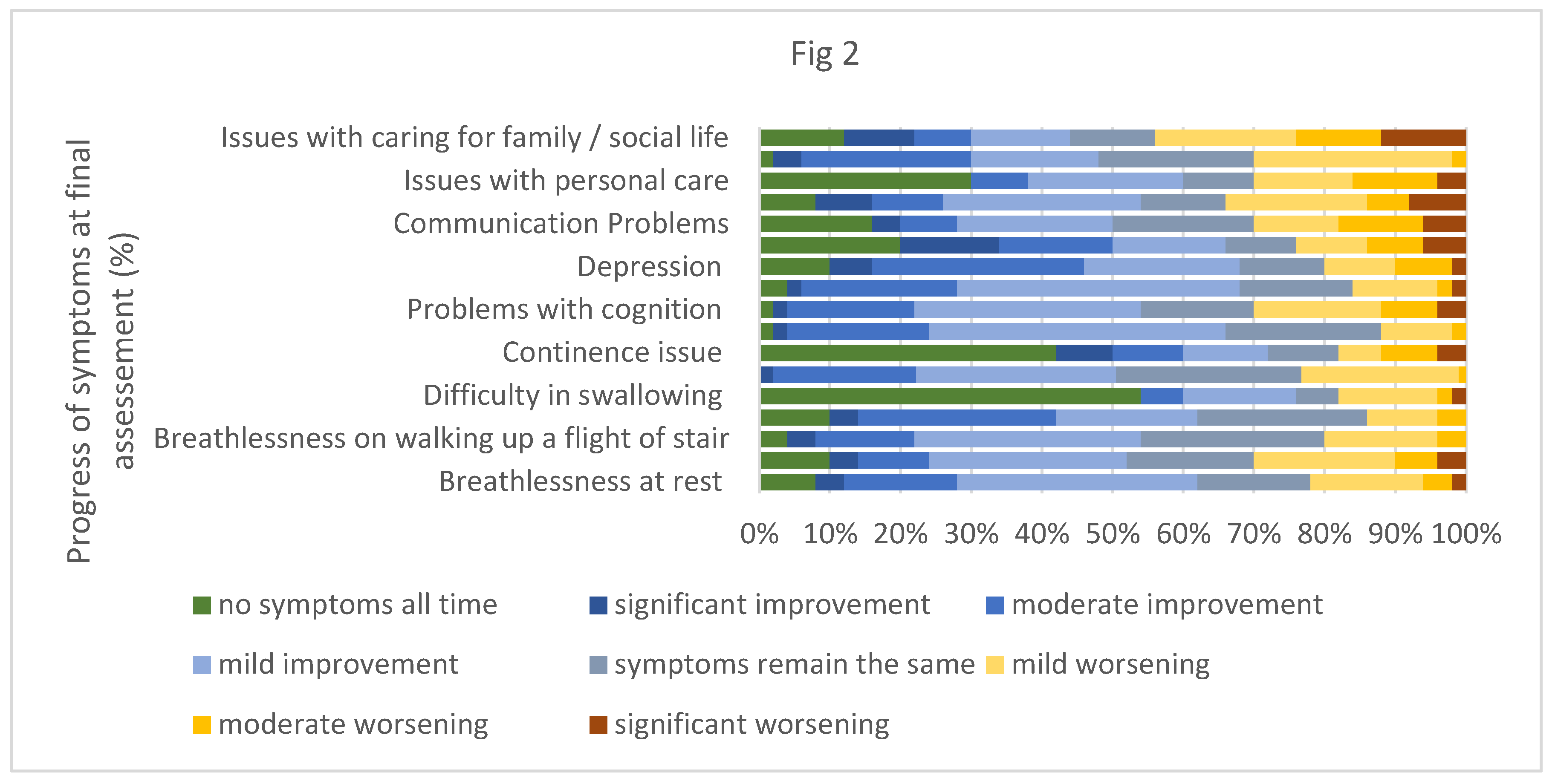
At the final assessment, a significant proportion of the patients reported improvement in their symptom severity (
Table 2 and
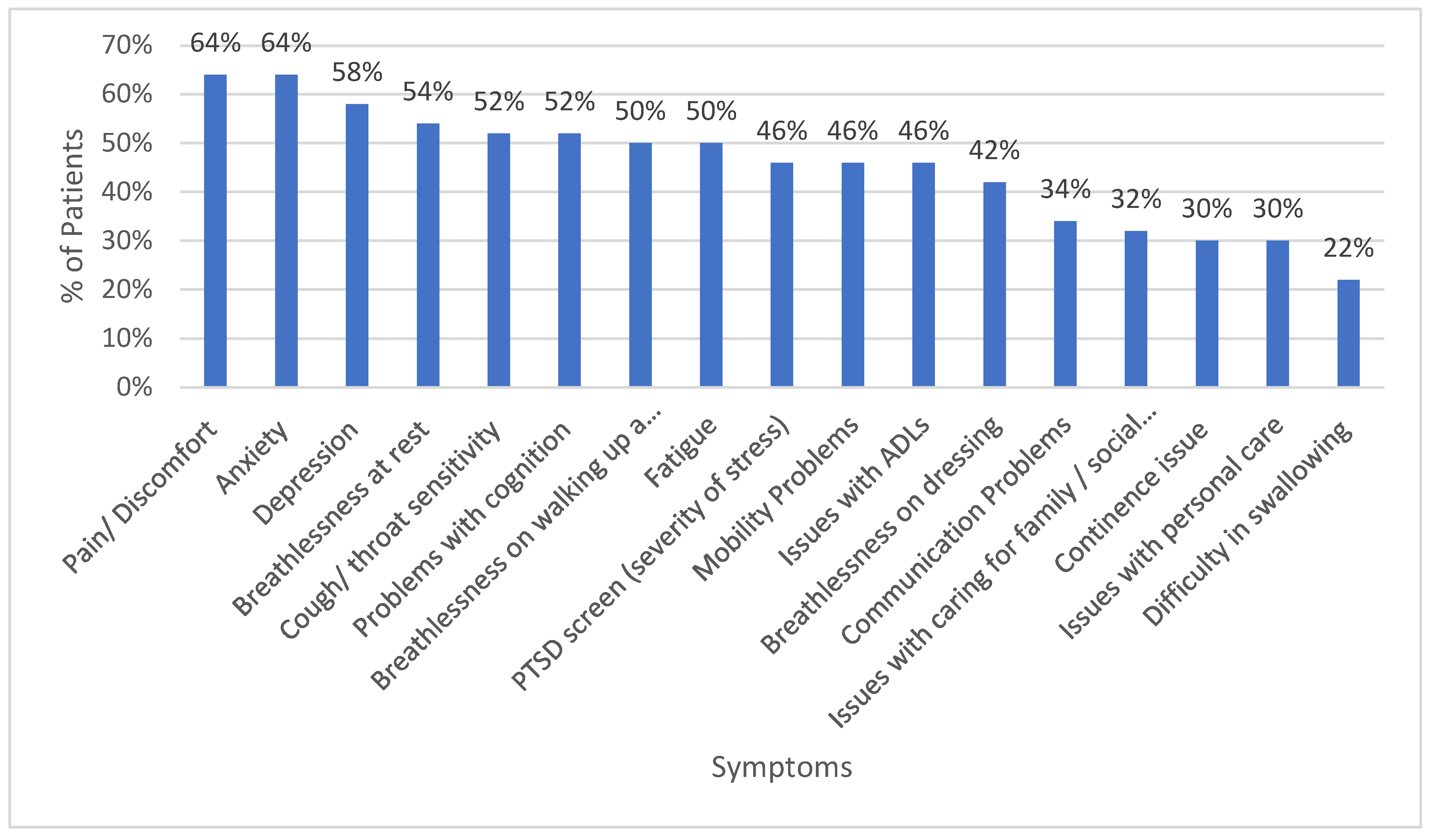
Figure 2). Many common symptoms (including pain, anxiety, breathlessness, fatigue and impaired cognition) responded well to rehabilitation, with more than 50% people reporting improvement (
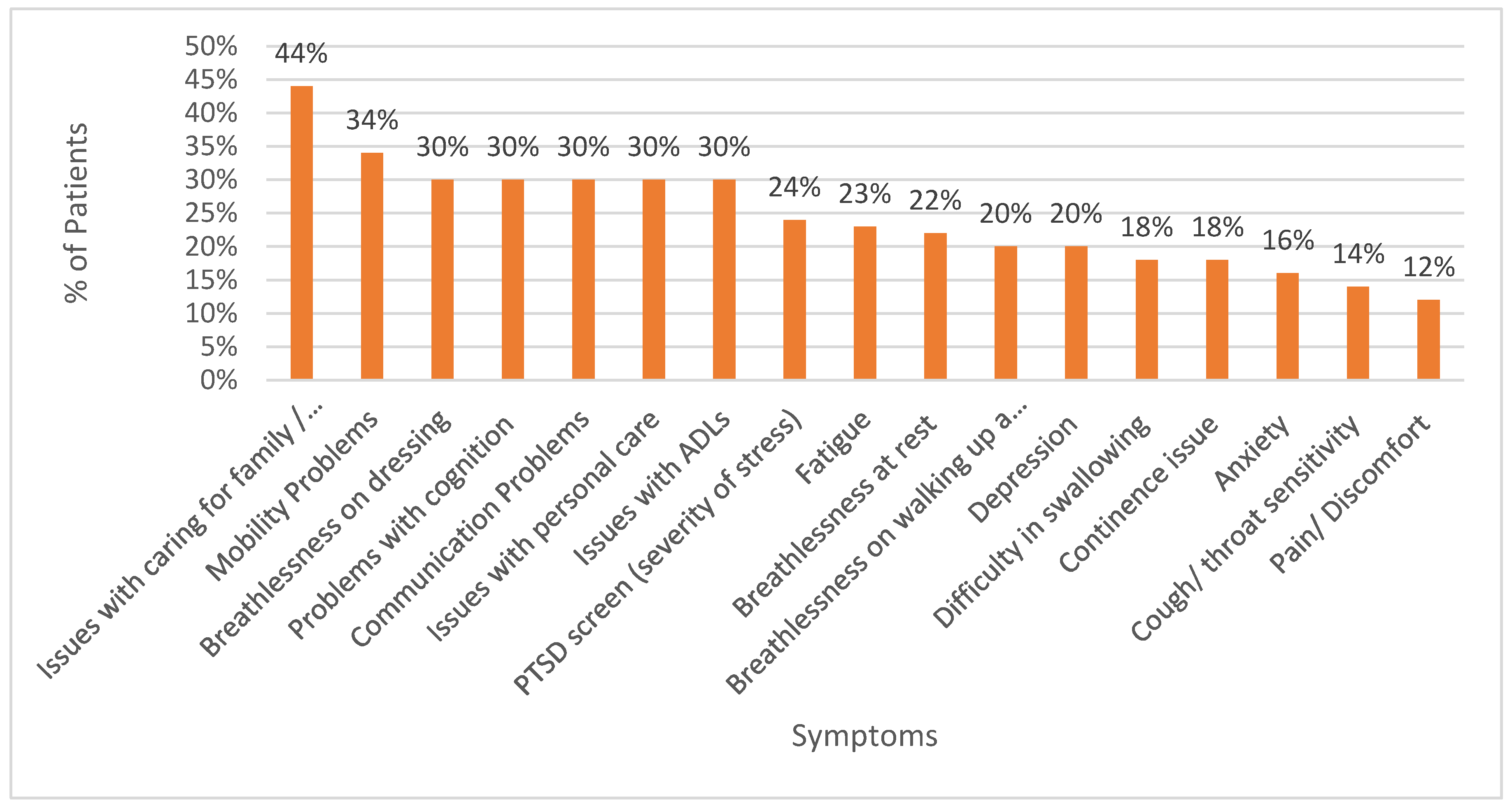
Figure 3). Difficulty in swallowing responded the least, with only 22% of patients affected by this reporting improvement post rehabilitation. Conversely, some patients reported worsening of some symptoms despite interventions provided in the LC rehabilitation clinic. This was highest for issues of caring for family/ social life, where 44% of sufferers reported worsening at final assessment (
Figure 4)
Discussion
Long COVID is a diverse condition that is underpinned by multiple pathophysiologies which are not fully understood [
15]. Given that there is evidence to support many competing theories, it is likely that long COVID is not a single disease entity and different mechanisms operate in different patients [
16]. In the absence of a consensus for the underlying biology, designing and testing disease modifying treatments will likely be slow to deliver any patient benefit. Clinical services have therefore taken the pragmatic approach to offering rehabilitation focussed on practical help and guidance tailored to the individual needs of each patient. To this end, post COVID services were established in the UK in December 2020 [
17] and the latest National Health Service (NHS) plan of improving long COVID services was launched in July 2022 for further investment in services, training programmes and research [
18]. As such, multi-disciplinary rehabilitation programmes for LC are now embedded in the delivery of care for LC patients supported by national and international guidelines [
19,
20].
In this study, we have used the C19-YRS tool to track symptoms across a multi-disciplinary rehabilitation program for the first time in the UK. We demonstrated that patients attending the rehabilitation service experience improvements in many symptoms, most notably anxiety and pain. As this study was observational, it did not have a control arm to assess the natural progression of long COVID symptoms in the absence of our rehabilitation intervention. However, in another study in survivors of COVID-19 admitted to hospital, here were little change in reported symptoms up to 12 months after acute COVID-19 [
21]. Moreover, a randomised control trial in preparation will formally assess the benefit of rehabilitation in LC [
22], although, unlike our study, it will only include patients with long COVID who were admitted to hospital during their acute infection.
We note the prevalence of some pre-existing symptoms in our study population to be higher than those reported in the UK population during the COVID-19 pandemic, and in the national evaluation of the C19-YRS [
23,
24]. We have selected patients who completed their C19-YRS (>75% completion) as per our inclusion/ exclusion criteria, which may have pre-selected those who had more health issues upfront and as such, more likely to have been committed to completing their questionnaires. Unlike the national evaluation for the ELAROS platform, we have not reported pre-COVID co-morbidity as part of this study. In the national evaluation for LC outcomes using digital C19-YRS collected via ELAROS platform, co-morbidity prior to acquiring COVID-19 was around 7% nationally (3.1% for mental health); however, the symptom burden for our cohort prior to acquiring COVID was not insignificant; for example, 64% reported pre-COVID symptoms of anxiety as we have considered any score above 0 on the C19-YRS to be positive although a score of 1 or 2 could represent mild symptoms only without the diagnosis of anxiety.[
24]
Some symptoms did not improve with rehabilitation, particularly swallowing difficulty. Both intubated COVID patients [
25,
26] and non-intubated COVID patients [
27] can experience various degrees of swallowing problems. The underlying causes are hypothesised to be related to pulmonary function changes, direct viral action on neurons [
27] and changes in smell and taste [
28]. However, further research to explore underlying causes and treatment options would be beneficial. The differential response to rehabilitation for different symptoms will be important to consider when assessing which patients are most likely to benefit from this service and in the long-term will help to direct efforts towards improving rehabilitation for the symptoms that responded the least.
Conclusions
It is feasible to monitor symptoms of patients with Long COVID ongoing rehabilitation programmes through utilising the C19-YRS. The digitalised version of C19-YRS via the ELAROS application allows gratifying tracking of symptoms overtime.
Symptoms which are most and least likely to improve with LC rehabilitation clinic intervention have been identified. Pain and anxiety symptoms are most likely to improve after intervention at long COVID clinic whereas swallowing difficulty is least likely to improve. Some issues, most notably issues with caring for family/ social life got worse for several people during the course of rehabilitation. Long COVID services will need to consider service provision and support for patients with clinical problems that are least likely to improve or likely to deteriorate so patients’ needs are addressed. Further research with a larger population and ethnic variety is warranted to establish a more definitive symptom response. Future research will need to explore the reasons leading some patients’ symptoms to deteriorate rather than improve despite rehabilitation.
References
- A clinical case definition of post COVID-19 condition by a Delphi consensus. 2021.
- Malik P, Patel K, Pinto C, et al. Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)—A systematic review and meta-analysis. J Med Virol. 2022;94:253–62. [CrossRef]
- Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK - Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/alldatarelatingtoprevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk (accessed 29 July 2023).
- Nurek M, Rayner C, Freyer A, et al. Recommendations for the recognition, diagnosis, and management of long COVID: a Delphi study. British Journal of General Practice. 2021;71:e815–25. [CrossRef]
- Crook H, Raza S, Nowell J, et al. Long covid—mechanisms, risk factors, and management. BMJ. 2021;n1648. [CrossRef]
- Ostrowska M, Rzepka-Cholasińska A, Pietrzykowski Ł, et al. Effects of Multidisciplinary Rehabilitation Program in Patients with Long COVID-19: Post-COVID-19 Rehabilitation (PCR SIRIO 8) Study. J Clin Med. 2023;12:420. [CrossRef]
- Hughes SE, Haroon S, Subramanian A, et al. Development and validation of the symptom burden questionnaire for long covid (SBQ-LC): Rasch analysis. BMJ. 2022;e070230. [CrossRef]
- My Long COVID Needs | My Long COVID. https://mylongcovid.org.uk/# (accessed 7 July 2024).
- Sivan M, Halpin S, Gee J. Assessing long-term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool). Advances in Clinical Neuroscience & Rehabilitation. 2020;19:14–7. [CrossRef]
- O’Connor RJ, Preston N, Parkin A, et al. The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): Application and psychometric analysis in a post-COVID-19 syndrome cohort. J Med Virol. 2022;94:1027–34. [CrossRef]
- Sivan M, Smith AB, Osborne T, et al. Long COVID Clinical Severity Types Based on Symptoms and Functional Disability: A Longitudinal Evaluation. J Clin Med. 2024;13:1908. [CrossRef]
- NHS England » Commissioning guidance for post-COVID services for adults, children and young people. 2024.
- Overview COVID-19 rapid guideline: managing the long-term effects of COVID-19 Guidance NICE. 2020.
- Home - C19-YRS. https://c19-yrs.com/ (accessed 7 July 2024).
- Diar Bakerly N, Smith N, Darbyshire JL, et al. Pathophysiological Mechanisms in Long COVID: A Mixed Method Systematic Review. Int J Environ Res Public Health. 2024;21:473. [CrossRef]
- Davis HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023;21:133–46. [CrossRef]
- NHS England. Post-COVID syndrome (long COVID). https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/. 2023.
- NHS England » The NHS plan for improving long COVID services. 2024.
- COVID-19 rapid guideline: managing the long-term effects of COVID-19.
- Clinical management of COVID-19. https://www.who.int/teams/health-care-readiness/covid-19 (accessed 7 July 2024).
- Evans RA, Leavy OC, Richardson M, et al. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. Lancet Respir Med. 2022;10:761–75. [CrossRef]
- Daynes E, Baldwin M, Greening NJ, et al. The effect of COVID rehabilitation for ongoing symptoms Post HOSPitalisation with COVID-19 (PHOSP-R): protocol for a randomised parallel group controlled trial on behalf of the PHOSP consortium. Trials. 2023;24:61. [CrossRef]
- Jia R, Ayling K, Chalder T, et al. The prevalence, incidence, prognosis and risk factors for symptoms of depression and anxiety in a UK cohort during the COVID-19 pandemic. BJPsych Open. 2022;8:e64. [CrossRef]
- Sivan MGDSARLROTGM. National Evaluation of Long COVID Services Outcomes Using ELAROS Data. Leeds 2023.
- Frajkova Z, Tedla M, Tedlova E, et al. Postintubation Dysphagia During COVID-19 Outbreak-Contemporary Review. Dysphagia. 2020;35:549–57. [CrossRef]
- Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post-acute phase. ‘Instant paper from the field’ on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56:323–6. [CrossRef]
- Grilli GM, Giancaspro R, Del Colle A, et al. Dysphagia in non-intubated patients affected by COVID-19 infection. Eur Arch Otorhinolaryngol. 2022;279:507–13. [CrossRef]
- Vergara J, Lirani-Silva C, Brodsky MB, et al. Potential Influence of Olfactory, Gustatory, and Pharyngolaryngeal Sensory Dysfunctions on Swallowing Physiology in COVID-19. Otolaryngology–Head and Neck Surgery. 2021;164:1134–5. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).