Submitted:
13 August 2024
Posted:
15 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Study Protocol
2.2.1. Laboratory Assessment
2.2.2. Coagulation Profile Evaluation Tests
2.2. Evaluation of Liver Fibrosis
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. General characteristics of the study population
3.2. Evolution of virological parameters, liver function and the degree of liver fibrosis in the studied group
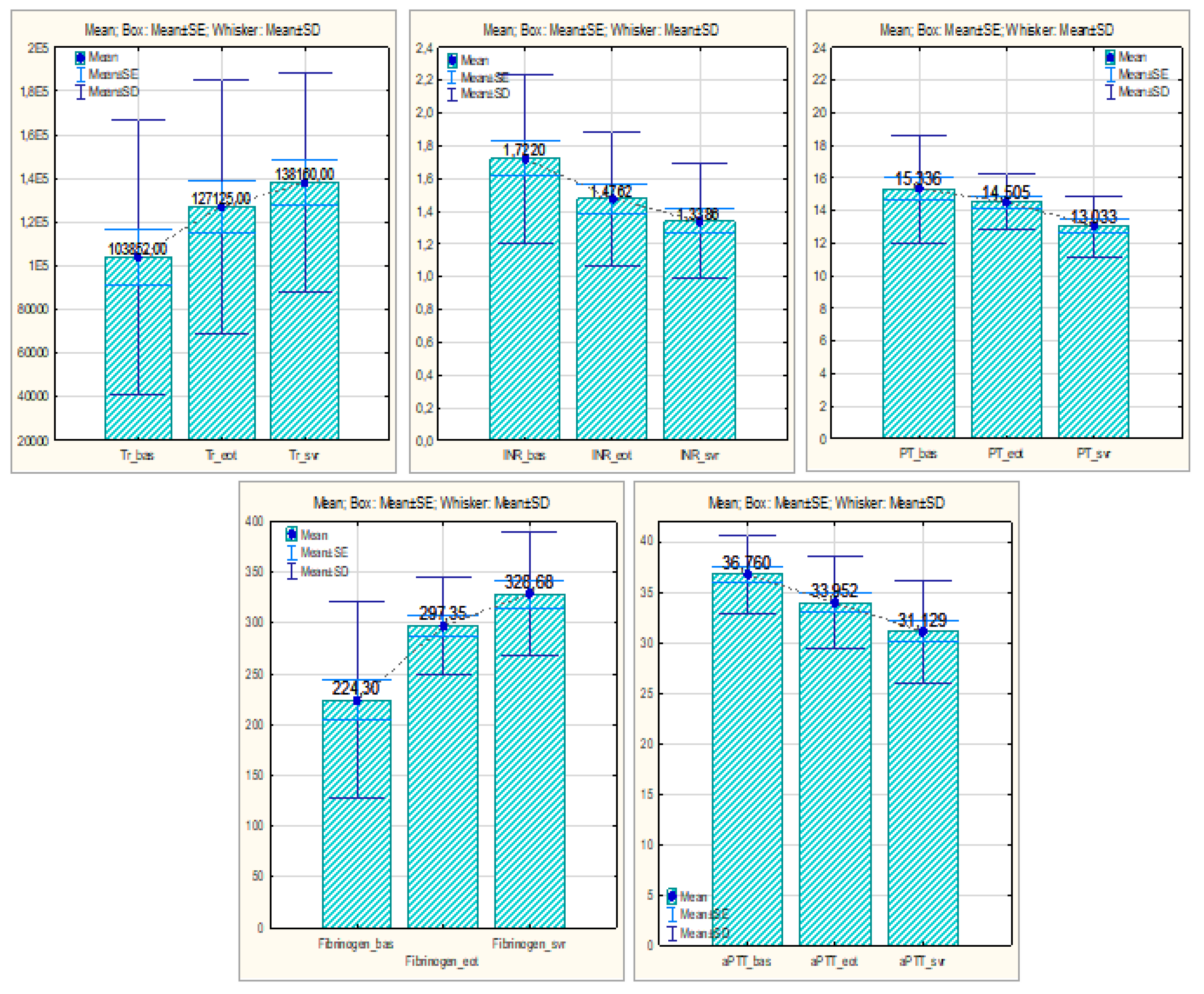
3.3. Evaluation of routine coagulation parameters in patients with HCV-related liver cirrhosis treated with DAAs and SVR
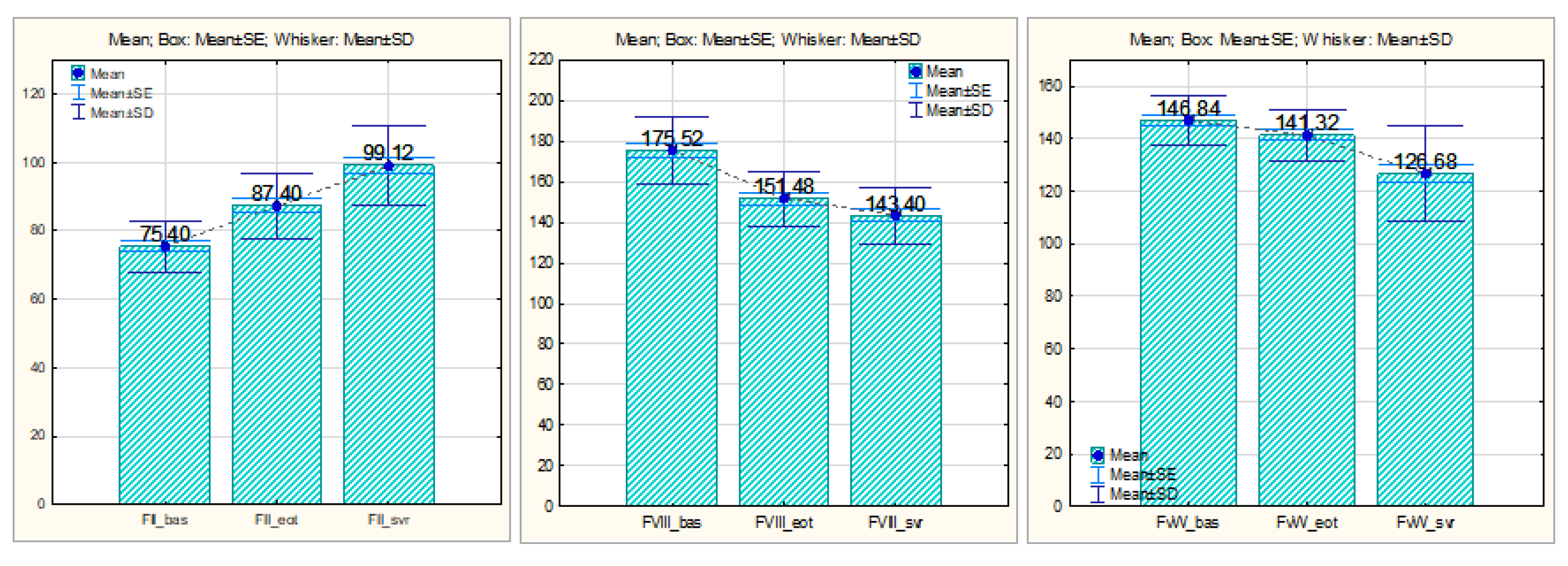
3.4. Evaluation of procoagulant factors in patients with HCV-related liver cirrhosis treated with DAAs and SVR
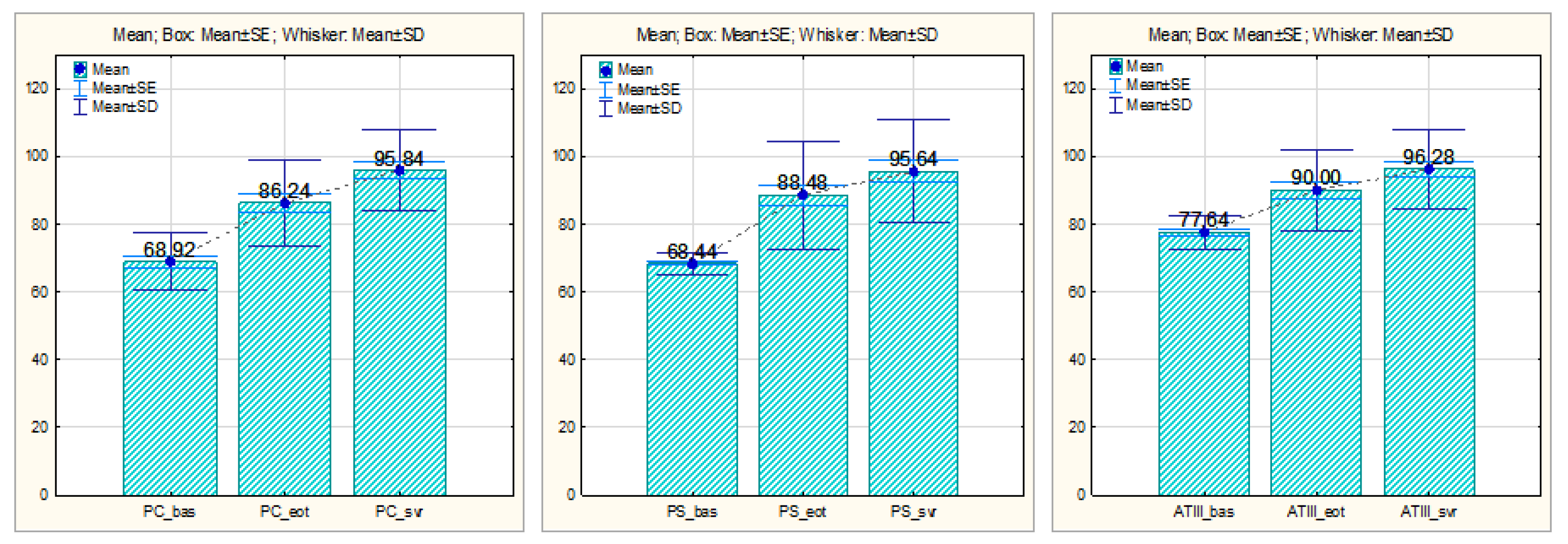
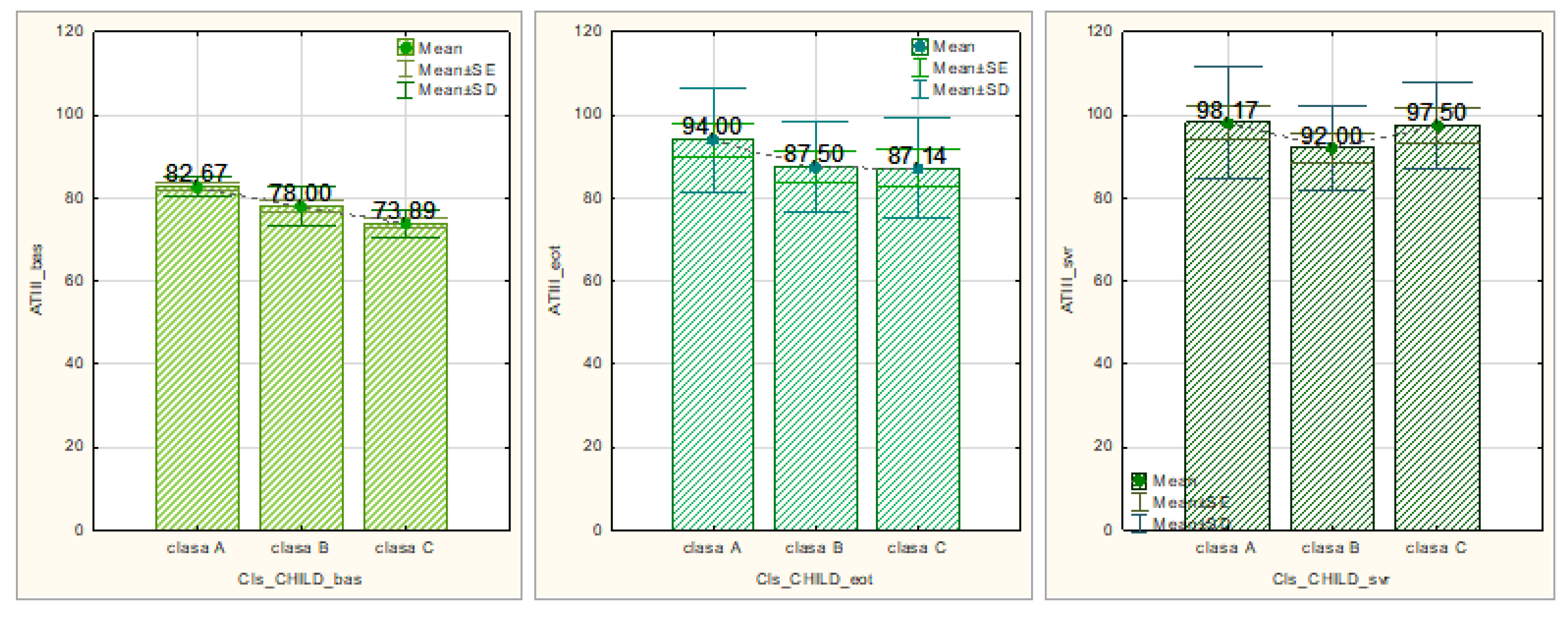
3.5. Evaluation of anticoagulant factors in patients with HCV-related liver cirrhosis treated with DAAs and SVR
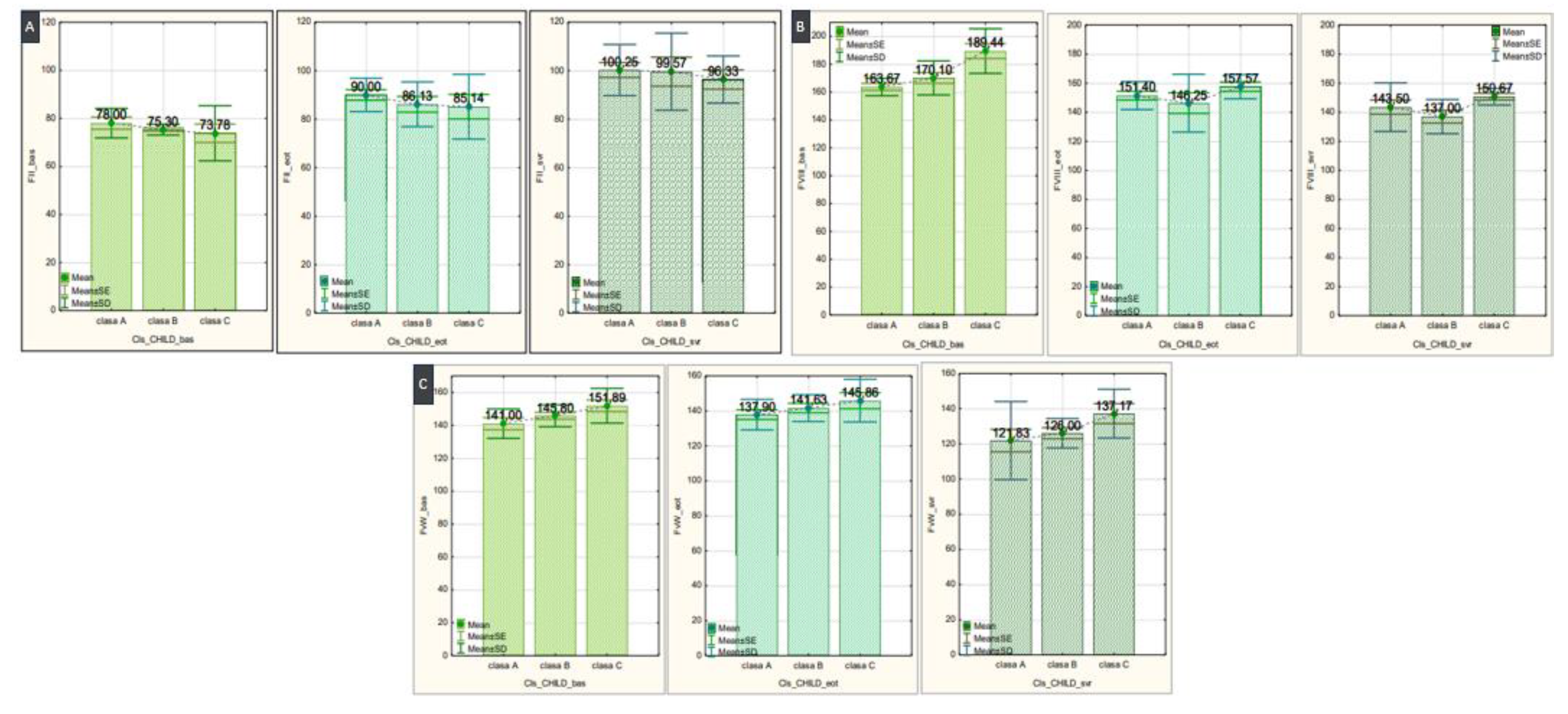
3.6. Evaluation of the Relationship between the Severity of Liver Cirrhosis and Changes in Coagulation Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Masetti, C.; Lleo, A.; Colombo, M.; Colombo, M.; Aghemo, A. Postsustained Virological Response Management in Hepatitis C Patients. Semin Liver Dis 2020, 40, 233–239. [Google Scholar] [CrossRef]
- Reiberger, T.; Lens, S.; Cabibbo, G.; Nahon, P.; Zignego, A.L.; Deterding, K.; Elsharkawy, A.M.; Forns, X. EASL position paper on clinical follow-up after HCV cure. J Hepatol. 2024, 81, 326–344. [Google Scholar] [CrossRef]
- Cheng, C.H.; Chu, C.Y.; Chen, H.L.; et al. Direct-acting antiviral therapy of chronic hepatitis C improves liver fibrosis, assessed by histological examination and laboratory markers. J Formos Med Assoc. 2021, 120, 1259–1268. [Google Scholar] [CrossRef]
- Tripodi, A.; D’Ambrosio, R.; Padovan, L.; et al. Evaluation of coagulation during treatment with directly acting antivirals in patients with hepatitis C virus related cirrhosis. Liver Int. 2017, 37, 1295–1303. [Google Scholar] [CrossRef] [PubMed]
- Russo, F.P.; Zanetto, A.; Campello, E.; et al. Reversal of hypercoagulability in patients with HCV-related cirrhosis after treatment with direct-acting antivirals. Liver Int. 2018, 38, 2210–2218. [Google Scholar] [CrossRef] [PubMed]
- Azer, A.; Kong, K.; Basta, D.; Modica, S.F.; Gore, A.; Gorman, E.; Sutherland, A.; Tafesh, Z.; Horng, H.; Glass, N.E. Evaluation of coagulopathy in cirrhotic patients: A scoping review of the utility of viscoelastic testing. Am J Surg 2024, 227, 34–43. [Google Scholar] [CrossRef]
- González-Reimers, E.; Quintero-Platt, G.; Martín-González, C.; et al. Thrombin activation and liver inflammation in advanced hepatitis C virus infection. World J Gastroenterol 2016, 22, 4427–4437. [Google Scholar] [CrossRef]
- Zanetto, A.; Campello, E.; Senzolo, M.; Simioni, P. The evolving knowledge on primary hemostasis in patients with cirrhosis: A comprehensive review. Hepatology 2024, 79, 460–481. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Racila, A.; Muir, A.; et al. Long-term Patient-Centered Outcomes in Cirrhotic Patients With Chronic Hepatitis C After Achieving Sustained Virologic Response. Clin Gastroenterol Hepatol. 2022, 20, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Northup, P.G.; Caldwell, S.H. Coagulation in liver disease: a guide for the clinician. Clin Gastroenterol Hepatol 2013, 11, 1064–1074. [Google Scholar] [CrossRef]
- Nielsen, N.S.; Jespersen, S.; Gaardbo, J.C.; et al. Impaired Platelet Aggregation and Rebalanced Hemostasis in Patients with Chronic Hepatitis C Virus Infection. Int J Mol Sci 2017, 18, 1016. [Google Scholar] [CrossRef]
- Ioannou, G.N.; Feld, J.J. What Are the Benefits of a Sustained Virologic Response to Direct-Acting Antiviral Therapy for Hepatitis C Virus Infection? Gastroenterology 2019, 156, 446–460. [Google Scholar] [CrossRef] [PubMed]
- Pearlman, B.L. Direct-Acting Antiviral Therapy for Patients with Chronic Hepatitis C Infection and Decompensated Cirrhosis. Dig Dis Sci 2024, 69, 1551–1561. [Google Scholar] [CrossRef]
- Young, K.; Liu, B.; Bhuket, T.; et al. Improved liver transplant waitlist mortality and lower risk of disease progression among chronic hepatitis C patients awaiting liver transplantation after the introduction of direct-acting antiviral therapies in the United States. J Viral Hepat. 2019, 26, 350–361. [Google Scholar] [CrossRef]
- Pol, S.; Parlati, L. Treatment of hepatitis C: the use of the new pangenotypic direct-acting antivirals in “special populations”. Liver Int. 2018, 38, 28–33. [Google Scholar] [CrossRef]
- Bachofner, J.A.; Valli, P.V.; Kroger, A.; et al. Direct antiviral agent treatment of chronic hepatitis C results in rapid regression of transient elastography and fibrosis markers fibrosis-4 score and aspartate aminotransferase-platelet ratio index. Liver Int. 2017, 37, 369–376. [Google Scholar] [CrossRef]
- Elsharkawy, A.; Samir, R.; El-Kassas, M. Fibrosis regression following hepatitis C antiviral therapy. World J Hepatol 2022, 14, 1120–1130. [Google Scholar] [CrossRef]
- Bethea, E.D.; Gaj, K.; Gustafson, J.L.; et al. Pre-emptive pangenotypic direct acting antiviral therapy in donor HCV-positive to recipient HCV-negative heart transplantation: an open-label study. Lancet Gastroenterol Hepatol 2019, 4, 771–780. [Google Scholar] [CrossRef]
- Hutchinson, S.J.; Valerio, H.; McDonald, S.A.; et al. Population impact of direct-acting antiviral treatment on new presentations of hepatitis C-related decompensated cirrhosis: a national record-linkage study. Gut. 2020, 69, 2223–2231. [Google Scholar] [CrossRef]
- Tosetti, G.; Degasperi, E.; Farina, E.; et al. Decompensation in Direct-Acting Antiviral Cured Hepatitis C Virus Compensated Patients With Clinically Significant Portal Hypertension: Too Rare to Warrant Universal Β-Blocker Therapy. Am J Gastroenterol 2021, 116, 1342–1344. [Google Scholar] [CrossRef]
- Calvaruso, V.; Craxi, A. Hepatic benefits of HCV cure. J Hepatol 2020, 73, 1548–1556. [Google Scholar] [CrossRef]
- Trifan, A.; Stanciu, C.; Gheorghe, L.; et al. Efficacy and safety of paritaprevir/ritonavir, ombitasvir, and dasabuvir with ribavirin for the treatment of HCV genotype 1b compensated cirrhosis in patients aged 70 years or older. Medicine 2017, 96, e9271. [Google Scholar] [CrossRef]
- Krassenburg, L.A.P.; Maan, R.; Ramji, A.; et al. Clinical outcomes following DAA therapy in patients with HCV-related cirrhosis depend on disease severity. J Hepatol. 2021, 74, 1053–1063. [Google Scholar] [CrossRef]
- Foster, G.R.; Irving, W.L.; Cheung, M.C.; et al. Impact of direct acting antiviral therapy in patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol 2016, 64, 1224–31. [Google Scholar] [CrossRef]
- Pons, M.; Rodríguez-Tajes, S.; Esteban, J.I.; et al. Non-invasive prediction of liver-related events in patients with HCV-associated compensated advanced chronic liver disease after oral antivirals. J Hepatol. 2020, 72, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Maynard, S.; Marrinan, E.; Roberts, L.; Stanworth, S. Does the Use of Viscoelastic Hemostatic Assays for Periprocedural Hemostasis Management in Liver Disease Improve Clinical Outcomes? Transfus Med Rev. 2024, 38, 150823. [Google Scholar] [CrossRef]
- Koh, C.; Heller, T.; Haynes-Williams, V.; et al. Long-term outcome of chronic hepatitis C after sustained virological response to interferon-based therapy. Aliment Pharmacol Ther. 2018, 37, 887–894. [Google Scholar] [CrossRef] [PubMed]
- Quaranta, M.G.; Ferrigno, L.; Tata, X.; D’Angelo, F.; Coppola, C.; et al. Liver function following hepatitis C virus eradication by direct acting antivirals in patients with liver cirrhosis: data from the PITER cohort. BMC Infect Dis 2021, 21, 413. [Google Scholar] [CrossRef]
- Poordad, F.; Castro, R.E.; Asatryan, A.; Aguilar, H.; Cacoub, P.; et al. Long-term safety and efficacy results in hepatitis C virus genotype 1-infected patients receiving ombitasvir/paritaprevir/ritonavir + dasabuvir ± ribavirin in the TOPAZ-I and TOPAZ-II trials. J Viral Hepat. 2020, 27, 497–504. [Google Scholar] [CrossRef]
- Airola, C.; Pallozzi, M.; Cerrito, L.; Santopaolo, F.; Stella, L.; Gasbarrini, A.; Ponziani, F.R. Microvascular Thrombosis and Liver Fibrosis Progression: Mechanisms and Clinical Applications. Cells. 2023, 12, 1712. [Google Scholar] [CrossRef]
- Wilson, S.; Joseph, J.; Danta, M.; Rabbolini, D.J. Viscoelastometry to Manage Bleeding in Liver Disease. Cureus. 2023, 15, e41401. [Google Scholar] [CrossRef] [PubMed]
- Campello, E.; Radu, C.M.; Zanetto, A.; et al. Changes in plasma circulating microvesicles in patients with HCV-related cirrhosis after treatment with direct-acting antivirals. Liver Int. 2020, 40, 913–920. [Google Scholar] [CrossRef] [PubMed]
| Parameters | Patients, N=52 |
|---|---|
|
Sex male, n (%) female, n (%) |
17 (32%) 35 (68%) |
| Age (years) | 63,88 ± 9,387 |
|
Child-Pugh class class A, n (%) class B, n (%) class C, n (%) |
12 (24%) 21 (40%) 19 (36%) |
|
MELD score < 15 ≥ 15 |
21 (40%) 31 (60%) |
|
Treatment DAA PrOD, n (%) LED / SOF, n (%) |
12 (24%) 40 (76%) |
| Experienced / naïve to IFN, n (%) | 15 (28%) / 37 (72%) |
| Ribavirin, n (%) | 15 (28%) |
| Antecedents of decompensation, n (%) | 29 (56%) |
| History of esophageal varices, n (%) | 35 (68%) |
| Fibroscan, kPa | 26 |
| SVR, n (%) | 52 (100%) |
| Protein C | |||
|---|---|---|---|
| CHILD class | N | Media ±SD | p |
| Baseline | 0,001** | ||
| class A | 14 | 75,50 ± 3,146 | |
| class B | 20 | 71,30 ± 3,129 | 0,075 |
| class C | 18 | 61,89 ± 9,993 | 0,010* |
| EOT | 0,002** | ||
| class A | 22 | 87,30 ± 10,253 | |
| class B | 17 | 95,50 ± 10,433 | 0,102 |
| class C | 13 | 74,14 ± 9,582 | 0,015* |
| SVR | 0,164 | ||
| class A | 24 | 96,75 ± 11,395 | |
| class B | 16 | 100,71 ± 12,392 | 0,474 |
| class C | 12 | 88,33 ± 10,328 | 0,156 |
| Protein S | |||
|---|---|---|---|
| CHILD class | N | Media ±SD | p |
| Baseline | 0,005** | ||
| class A | 13 | 71,83 ± 2,787 | |
| class B | 21 | 67,60 ± 2,011 | 0,005** |
| class C | 18 | 67,11 ± 3,018 | 0,002** |
| EOT | 0,665 | ||
| class A | 20 | 90,10 ± 3,018 | |
| class B | 19 | 90,63 ± 19,835 | 0,947 |
| class C | 13 | 83,71 ± 10,484 | 0,437 |
| SVR | 0,781 | ||
| class A | 25 | 96,75 ± 15,184 | |
| class B | 15 | 97,14 ± 18,898 | 0,959 |
| class C | 12 | 91,67 ± 12,910 | 0,527 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





