1. Introduction
The increasing survival rate of newborns with low and extremely low birth weights, along with the rising percentage of preterm births, has heightened the significance of the problem of intracranial hemorrhage. This condition is one of the leading causes of neonatal morbidity and, at times, even mortality. Preterm birth interrupts normal growth and development, causing the brain to develop outside the womb under conditions different from the physiological norm. The brain of a preterm infant is vulnerable due to its anatomical and physiological characteristics, and, in cases of perinatal asphyxia or trauma, there is an increased risk of intracranial hemorrhage. Complications in other organ systems can adversely affect the further development of the central nervous system.
The vulnerable and immature anatomy, hemodynamic instability, and tendency to bleed—which are intrinsic factors in preterm infants—lead to germinal matrix and intraventricular hemorrhage (GMH-IVH). On the other hand, based on a large number of routine sonographic examinations, it has been shown that most GMH-IVH cases are asymptomatic, and the diagnosis of hemorrhage cannot be based solely on clinical presentation. Undiagnosed intracranial hemorrhage does not rule out the possibility of later sequelae in these children, which can be very serious. Just as it is important to diagnose intracranial hemorrhage in a timely manner, it is also crucial to regularly visualize and monitor the size of the ventricular system through ultrasonographic examinations after hemorrhage resorption. Neurosonography has been proven to be helpful in neonatal brain diagnoses [
1]. Although there are other classifications of intracranial hemorrhage in newborn [
2], the classification of Papile et al. is most commonly used [
3]. Globally, rates of grades GMH-IVH I-IV have been reported with considerable variation between different regions of the world [
4].
Simple ultrasonographic monitoring of these children, analyzing the degree of hemorrhage and the size of the right and left lateral ventricles, provides many prognostic indicators. The Brunet–Lezine scale is used in Serbia for the assessment of psychomotor development. It is easy to administer, requires a short time to apply, and has low costs for acquisition and training.
In this study, we aimed to determine whether the sizes of the left and right lateral ventricles after the resorption of intracranial hemorrhage affect the values obtained in the psychomotor development assessment of children at the age of 3 years, using the Brunet–Lezine scale.
2. Materials and Methods
The study was conducted at the Institute for Child and Youth Health Care of Vojvodina in Novi Sad, and included prematurely born infants who were hospitalized in the Department of Neonatology, Intensive Care, and Therapy of the Institute. Parents of the prematurely born children were also included in the study. The parents received written information about the study and completed consent forms prior to testing.
The study was prospective and included 120 prematurely born infants with diagnosed intracranial hemorrhage, as detected through ultrasound examination of the central nervous system. The echographic examinations of the central nervous system were performed using a Siemens ultrasound machine with convex probes of 3 and 5 MHz frequencies and linear probes of 5 and 7.5 MHz frequencies. Standardization of the evaluation of neonatal central nervous system echograms was based on the Papile classification [
5]. Prematurely born infants were classified by gestational weeks into 4 groups: Group 1 (25–29 6/7 weeks), Group 2 (30–32 6/7 weeks), Group 3 (33–34 6/7 weeks), and Group 4 (35–37 weeks).
The study did not include newborns with intrauterine growth restriction, those with major congenital malformations, or newborns from twin pregnancies. Prematurely born children were regularly monitored at the neonatology clinic of the Institute for Child and Youth Health Care of Vojvodina in Novi Sad until the age of 3 years, at which point their psychomotor development was assessed using the Brunet–Lezine scale.
Statistical data analysis was performed using appropriate modules within the SPSS 23.0 for Windows software package. To determine whether there were differences among subjects with different degrees of hemorrhage in relation to gender and the bilaterality of the hemorrhage, Pearson’s ꭓ2 test was applied.
To determine whether there were differences among subjects with different degrees of hemorrhage in relation to their average birth weight, average Apgar scores, average gestational age, average size of the right lateral ventricle, average size of the left lateral ventricle, and average values of the global development quotient (QR scores), one-way analysis of variance (ANOVA) was applied.
3. Results
In this study, the biological data yielded the following results (described as mean ± standard deviation): the average body weight of preterm infants with grade I hemorrhage was 1915.67 g, while the average body weight of children with grade IV hemorrhage was 1442.17 g. The research results suggest that there were no differences in gender among subjects with different degrees of intracranial hemorrhage. The value of the chi-square test was not statistically significant, amounting to χ2 = 3.35 (df = 3, p = 0.34).
The average Apgar score at birth in Group 1 was 6.43, while in Group 4, it was 3.90. The value of the F-test was statistically significant at the p < 0.01 level, amounting to F = 10.74 (df = 118, p = 0.00). The research results suggest that the differences in Apgar scores at birth among the groups of subjects with different degrees of intracranial hemorrhage were greater than the differences within each group.
The average Apgar score at five minutes after birth for preterm infants with grade I hemorrhage was 7.77, and for subjects with the most severe (i.e., grade IV) hemorrhage, it was 5.97. The value of the F-test was statistically significant at the p < 0.01 level, amounting to F = 8.90 (df = 118, p = 0.00). The differences in Apgar scores at five minutes after birth among the groups of subjects with different degrees of intracranial hemorrhage were greater than the differences within each group. In particular, the average Apgar scores after five minutes were higher in subjects from Group 1, and then further decreased.
The average gestational age in Group 1 was 33 4/7 weeks, while in Group 4, it was 29 5/7 weeks. The value of the F-test was statistically significant at the p < 0.01 level, amounting to F = 9.48 (df = 119, p = 0.00). The differences in gestational age among the groups of subjects with different degrees of intracranial hemorrhage were greater than the differences within each group. The values of the average gestational age decreased with an increase in the degree of intracranial hemorrhage.
The bilaterality of intracranial hemorrhage in prematurely born infants with different degrees of hemorrhage was analyzed. The results are presented in
Table 1. Of all unilateral hemorrhages, 45.9% occurred in prematurely born infants with grade IV hemorrhage.
The value of the F-test was statistically significant at the p < 0.01 level, with F = 52.48 (df = 116, p = 0.00). The research results suggest that the differences in QR scores among groups of subjects with varying degrees of intracranial hemorrhage were greater than the differences within each group. The average QR scores were above 90 for subjects in Groups 1 and 2, while the average QR score for the group of subjects with Grade IV intracerebral hemorrhage (Group 4) was below 70.
In order to achieve a comprehensive analysis of the correlations between the ultrasound findings and subsequent neurodevelopmental characteristics, the following charts present two-dimensional functions of the dependent variables (i.e., motor skills, coordination, speech, and sociability) with respect to the independent variables (i.e., intracranial hemorrhage with the dimensions of the left and right lateral ventricles).
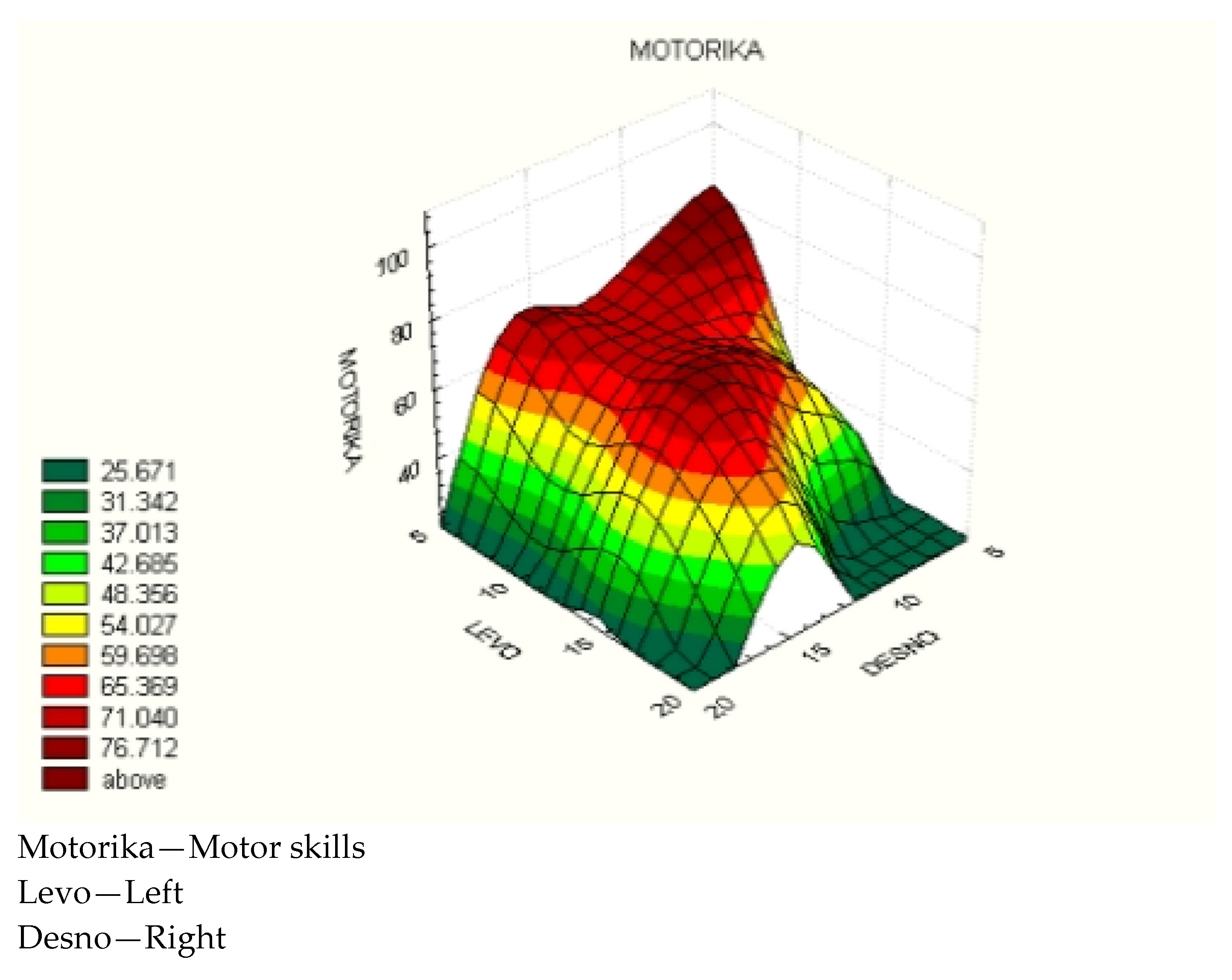
In the case of
motor skills, the influence of asymmetry in the size of the left and right lateral ventricles was pronounced. With a small value of the right lateral ventricle size and values over 10 mm for the left lateral ventricle, motor skill values were at their minimum, which manifested as unilateral motor deficits (
Figure 1).
It should be noted that the main ridge (or the inflection point of the function), located at around 15 mm of the right lateral ventricle size, indicates that with large values of the left lateral ventricle size, an increase in the right lateral ventricle size up to 15 mm still results in increasing motor skills. Beyond 15 mm of the right lateral ventricle size, there is a general decline in motor skill values.
It should also be noted that there are three local maxima for motor skills:
At small values of the left and right lateral ventricle sizes;
At small values of the left lateral ventricle size and a value of 15 mm for the right lateral ventricle size;
At bilateral values of 15 mm for both lateral ventricles.
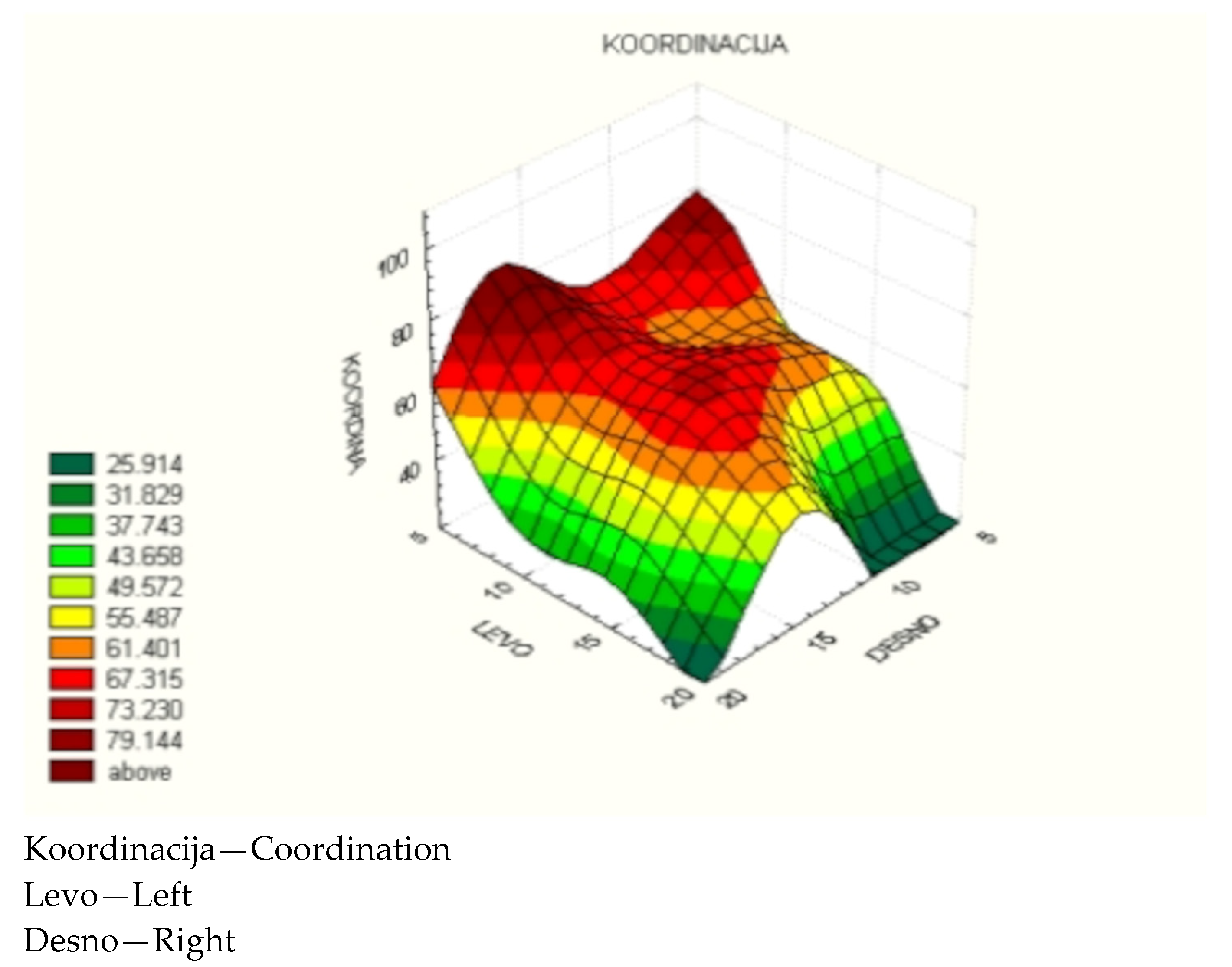
The analysis of coordination yielded similar results to motor skills, with a distinct difference found in tolerance for the left lateral ventricle size, from 10 to 15 mm, and at small values of the right lateral ventricle size, where there was no intense degradation of coordination, as was the case with motor skills (
Figure 2).
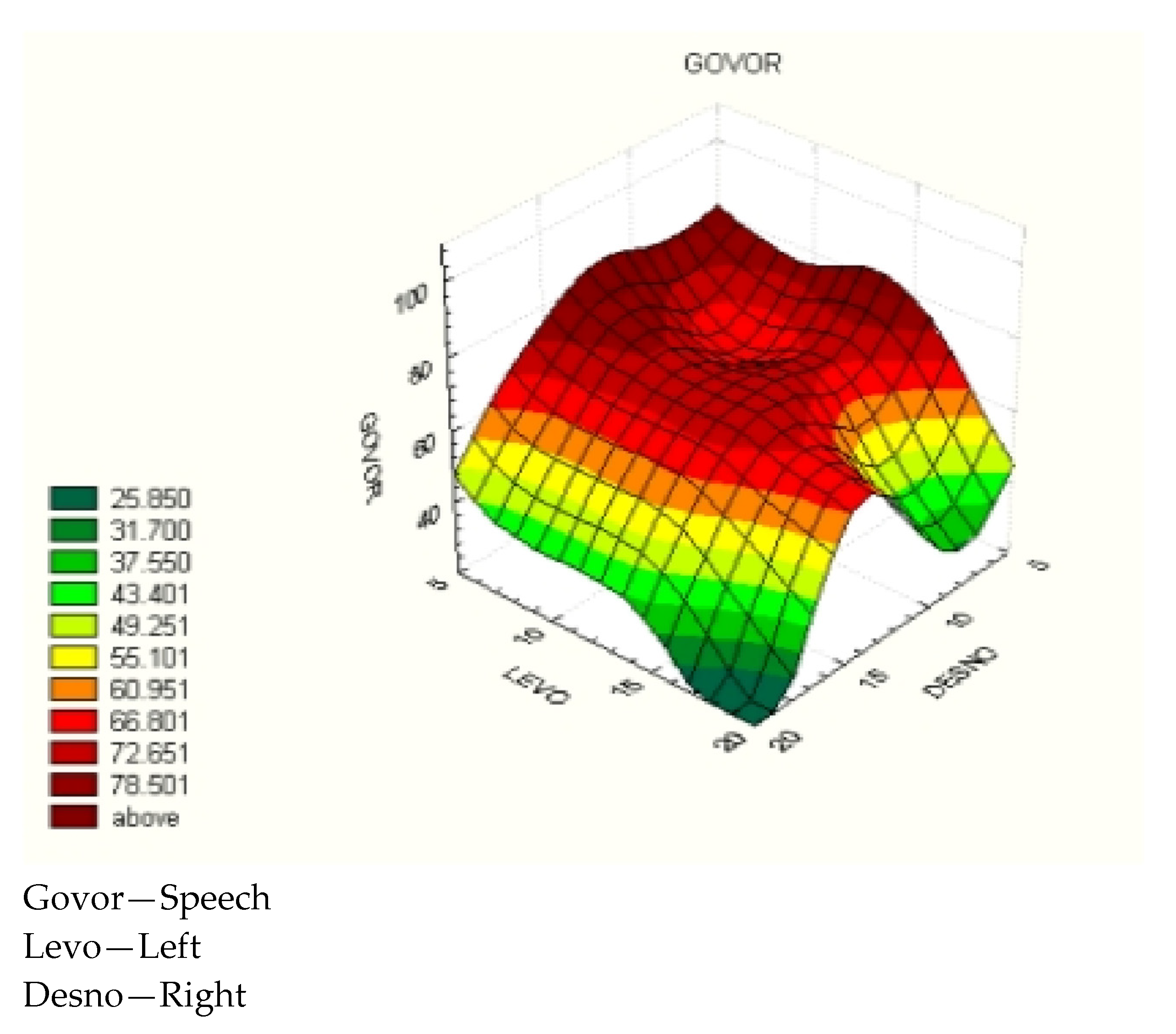
In the case of speech, the overall bilateral tolerance improved in favor of the size of the left lateral ventricle. There is a general zone where, with bilateral sizes of the lateral ventricles below 15 mm, satisfactory speech values were achieved. However, with bilateral sizes of the lateral ventricles exceeding 15 mm, there was a marked degradation in speech scores (
Figure 3).
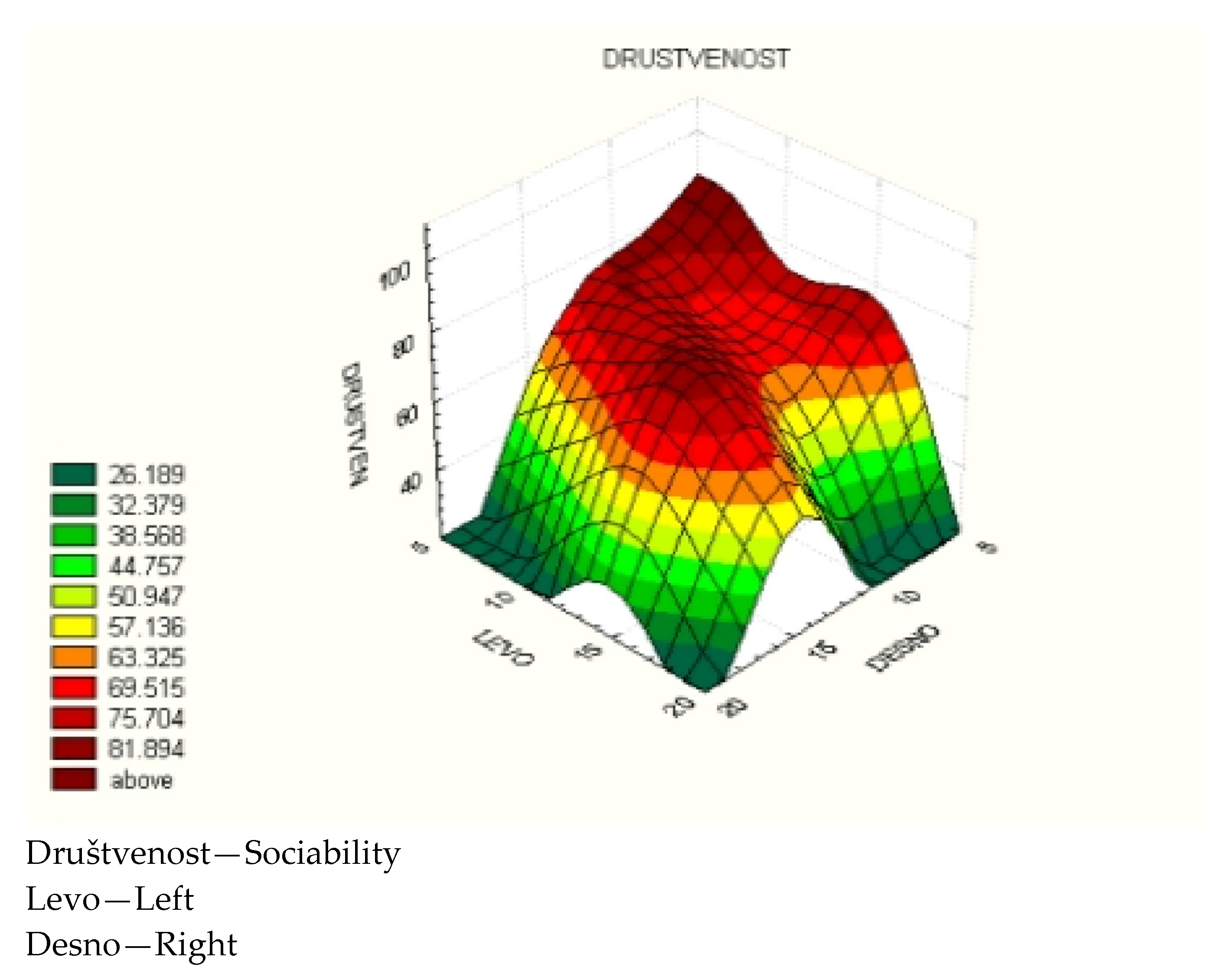
As expected, the results for sociability were similar to those for speech. The only difference was a weaker tolerance for values around 10 mm of the right lateral ventricle size and around 15 mm of the left lateral ventricle size (
Figure 4).
For analysis of the impact of the lateral ventricle sizes, the values of the global psychological development quotient (QR), motor skills, coordination, speech, and sociability variables were divided into three factors:
Factor I, which denotes larger dimensions of the left lateral ventricle.
Factor II, which denotes equal sizes of the left and right lateral ventricles.
Factor III, which denotes larger dimensions of the right lateral ventricle.
The analysis revealed a significant difference in the width of the left lateral ventricle, compared to that of the right lateral ventricle, which partially favors the size of the left lateral ventricle and its influence on the selected random variables.
The following tables present the mean values of the selected variables, as well as the results of the dispersion analysis focused on the impacts of the mentioned factors on the selected variables in the groups.
In premature infants
with Grade I intracranial hemorrhage (
Group 1), 23 out of 30 patients had hemorrhaged to a greater extent on the left side, with a larger dimension of the left lateral ventricle, and 4 out of 5 minimum values of the selected variables (motor skills, coordination, sociability, speech, QR) were associated with the left side. The difference in motor skills values is concerning, as patients with a larger dimension of the left lateral ventricle had significantly reduced
motor skills (
Table 2). Therefore, it is necessary to intensify work on motor skills in patients with Grade I intracranial hemorrhage and a larger dimension of the
left lateral ventricle.
In premature infants
with Grade II intracranial hemorrhage (Group 2), 14 out of 30 patients had a more pronounced hemorrhage on the left side and a wider left lateral ventricle. However, two minima for coordination and speech were significant influenced by a larger right lateral ventricle. This fact should be highlighted, as the size of the right lateral ventricle is generally significantly smaller than that of the left, and all minimal parameters were expected on the left side. Despite this, Fisher’s analysis issued a warning at
the coordination level. In Group 2, the level of coordination in patients with more intense hemorrhage on the right side and a wider right lateral ventricle did not show a significant difference; however, this difference is concerning, and some patients with a larger right lateral ventricle presented a significant reduction in coordination (
Table 3). Therefore, it is necessary to intensify work on coordination in patients with Grade II intracranial hemorrhage and a larger dimension of the
right lateral ventricle.
In premature infants with
Grade III intracranial hemorrhage (Group 3), while there was a dominance of the frequency of a wider left lateral ventricle, the set of minima for the selected variables was associated with a wider right lateral ventricle. However, the differences in all variables did not provide significant indications or warnings (
Table 4).
In premature infants
with Grade IV intracranial hemorrhage (Group 4), all minima were under the significant influence of the size of the left lateral ventricle. Fisher’s analysis at all levels provided strong warnings, and, in the case of speech, there was a significant impact (
Table 5). In the group of premature infants with parenchymal hemorrhage, greater dilation of the left lateral ventricle resulted in significantly greater speech impairments.
4. Discussion
The goal of perinatal medicine is to reduce mortality, improve health-related quality of life, and enhance neurodevelopmental outcomes [
6]. Advances in perinatal medicine have led to improved survival rates for high-risk newborns, but not as much to a reduction in morbidity.
The increased survival of preterm infants has led to a rise in the total number of children with potential neurodevelopmental impairments. Various dysfunctions that may occur in these children do not appear in isolation. At an early age, it is difficult to determine whether these problems are transient and a result of recovery or the catch-up phenomenon, due to the negative effects of premature birth, or if they are signs of permanent disability, making it necessary to monitor and follow up with these children.
Intracranial hemorrhage is one of the most important causes of neonatal morbidity and, sometimes, mortality [
7].
Despite earlier beliefs that preterm infants with Grade I, subependymal, or Grade II intraventricular hemorrhage have good neurodevelopmental outcomes, recent studies have shown that they can also have poor development, particularly in the area of cognitive development, with increasing reports of psychiatric disorders in these children [
8,
9].
Intraventricular hemorrhage of Grade III or intraparenchymal hemorrhage of Grade IV is associated with the least encouraging neurodevelopmental outcomes.
Children with developmental delay should not be left without a diagnosis. The earlier the intervention begins, the better the prognosis [
10].
The monitoring programs for preterm infants with biological risk vary among individual departments and clinical programs, which decide on the possible combination of levels and frequency of monitoring these children. However, all aim for the early recognition of deficits in children and the application of early therapy.
Every scale used is not ideal, as confirmed in the literature, indicating that there is no perfect scale for assessing child development [
11]. While the Bayley Scale is the gold standard, studies in the literature have shown that there is a good correlation in some areas (e.g., speech) between the Bayley III Scale and the Brunet–Lézine Scale [
12]. On the other hand, the Brunet–Lézine Scale has been shown to have high values of specificity in all areas of development, meaning that it can help to identify children in a timely manner.
Regarding the size of the ventricular system, our research results suggested that the differences in the size of the right lateral ventricle among groups of subjects with varying degrees of intracranial hemorrhage were greater than the differences within each group. In particular, the size of the right lateral ventricle was consistent among subjects in Groups 1 and 2, then significantly increased with the severity of the hemorrhage (Groups 3 and 4). These findings indicate that the height of the body of the left lateral ventricle is also within normal limits in newborns from Groups 1 and 2, while an increase in the size of the left lateral ventricle occurs in preterm infants from Groups 3 and 4. It is known that findings regarding the height of the body of the lateral ventricles in different degrees of hemorrhage correspond to the classification of intracranial hemorrhage [
13].
Preterm infants with intracranial hemorrhage were assessed for early childhood psychological development by a clinical psychologist using the Brunet–Lézine scale. Global developmental quotients (DQ) and partial developmental quotients were observed. The differences in DQ scores among groups of subjects with varying degrees of intracranial hemorrhage were greater than the differences within each group; in particular, the average DQ scores were above 90 in subjects from Groups 1 and 2, while the average DQ score for subjects in Group 4 was below 70.
Regarding motor skills, the average scores on the Brunet–Lézine scale were above 90 in subjects from Groups 1 and 2, while the average score for Group 4 was around 60. The assessment of coordination across all examined groups yielded almost identical results to the motor skills assessment.
An assessment of the speech of preterm infants up to the age of 3 years following intracranial hemorrhage, using the Brunet–Lézine scale, revealed that an increase in the severity of the hemorrhage led to a lower score on the speech assessment scale. Additionally, the average scores in the assessment of sociability in preterm children also decreased with increasing severity of the hemorrhage.
In Group 1, among patients with Grade I intracranial hemorrhage, the difference in the motor function variable with a larger dimension of the left lateral ventricle was found to be concerning. Fisher’s analysis also highlighted a warning at the level of coordination in Group 2, with a wider right lateral ventricle. In Group 3, there was a predominance of minimal values of the selected variables with a wider right lateral ventricle, but the differences did not provide significant guidance or warnings. In Group 4, greater dilation of the left lateral ventricle resulted in significantly greater speech impairments.
5. Conclusions
Although there is a lack of data in the literature on the impact of the size of the ventricular system following intracranial hemorrhage in preterm infants on subsequent psychomotor development, this factor should certainly be taken into account. In addition to size, the unilaterality of lateral ventricle dilation also influences the further characteristics of these children, primarily motor skills. In cases where the Bayley Scale cannot be used, it is essential to utilize available assessment instruments, in order to identify at-risk children in a timely manner, such that appropriate therapy can be applied as early as possible to achieve the best possible outcome.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Institute for child and youth health care Vojvodina (173/19.09.2019).
Informed Consent Statement
All subjects i.e., their parents or guardians gave their informed consent for inclusion before they participated in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to privacy and ethical reasons.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Maller, V.V.; Cohen, H.L. Neurosonography: Assessing the Premature Infant. Pediatr Radiol. 2017, 47, 1031–1045. [Google Scholar] [CrossRef] [PubMed]
- Volpe, J.J. Intracranial hemorrhage: Germinal matrix-intraventricular hemorrhage of the premature infant. In Neurology of the Newborn; Saunders: Philadelphia, PA, USA, 1995. [Google Scholar]
- Patra, K.; Wilson-Costello, D.; Taylor, H.G.; Mercuri-Minich, N.; Hack, M. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: Effects on neurodevelopment. J. Pediatr. 2006, 149, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Siffel, C.; Kistler, K.D.; Sarda, S.P. Global incidence of intraventricular hemorrhage among extremely preterm infants: A systematic literature review. J. Perinat. Med. 2021, 49, 1017–1026. [Google Scholar] [CrossRef] [PubMed]
- Papile, L.A.; Munsick-Bruno, G.; Schaefer, A. Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J. Pediatr. 1983, 103, 273–277. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, T.M.; Preisser, J.S.; Klinepeter, K.L.; Dillard, R.G. Trends in mortality and cerebral palsy in a geographically based cohort of very low birth weight neonates born between 1982 to 1994. Pediatrics 1998, 101, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Pape, K.E.; Wiglesworth, J.S. Haemorhage, ishaemia and the perinatal brain. Clin. Dev. Med. 1979, 69–70. [Google Scholar]
- Yaghini, O.; Majidinezhad, M.; Ghehsareh Ardestani, A.; Riahinezhad, M.; Maracy, M.R. The Effect of Low-Grade Intraventricular Hemorrhage on the Neurodevelopment of Very Low Birth Weight Infants. Iran. J. Child Neurol. 2022, 16, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Pfahl, S.; Hoehn, T.; Lohmeier, K.; Richter-Werkle, R.; Babor, F.; Schramm, D.; Sabir, H. Long-term neurodevelopmental outcome following low grade intraventricular hemorrhage in premature infants. Early Hum. Dev. 2018, 117, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Heineman, K.R.; Hadders-Algra, M. Evaluation of neuromotor function in infancy—A systematic review of available methods. J. Dev. Behav. Pediatr. 2008, 29, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.L.; Harris, S.R. Psychometric Properties and Standardization Samples of Four Screening Tests for Infants and Young Children: A Review. Pediatr. Phys. Ther. 2005, 17, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, F.G.C.; Formiga, C.K.M.R.; Bizinotto, T.; Tessler, R.B.; Neto, R.F. Concurrent Validity of the Brunet-Lézine Scale with the Bayley Scale for Assessment of the Development of Preterm Infants up to Two Years. Validade Concorrente da Escala Brunet-Lézine com a Escala Bayley para Avaliação do Desenvolvimento de Bebês Pré-Termo até Dois Anos. Rev. Paul. Pediatr. 2017, 35, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Volpe, J.J. Neurological evaluation; Hypoxic-ischemic encephalopathy; and Intracranial hemorrhage. In Neurology of the Newborn, 3rd ed.; Volpe, J.J., Ed.; W.B. Sounders Company: Philadelphia, PA, USA, 1995; pp. 95–463.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).