2. Methods:
Prospectively, 2,922 American patients in Metropolitan Detroit submitted stool in a CRC prospective screening study from 1996 to 2013. We used an stool ELISA and western blotting as described previously [
7] to detect p87, a product of the innate immune system to prospectively detect lung cancer in a cohort of patients at high risk for colorectal cancer. Controls were selected on the basis of criteria of no diagnosed lung, other cancer or family history of cancer. Other criteria used were non-smokers, no alcohol intake and non-diabetic patients. Patients and controls were approximately 50–80 years old and the male to female ratios were similar (5:1 and 10:1). Sixty- seven percent of patients and 45 % of controls were African American. Immunohistochemical (IHC) staining of lung tissues of 28 patients with lung cancer from patients seen at the Karmanos Cancer Institute collected retrospectively and the IHC were performed as described previously [
8]. Commercially available lung tissue arrays with malignant and benign tissues were stained with anti-p87 monoclonal Adnab-9 and ELISA of tissue extracts from 3 bronchoalveolar (lepidic spread) cell lines (a kind gift of Dr. Galli Hilman) was performed.
Results: 112 Lung cancers were detected on follow-up, 8.25±5.63years before the clinical diagnosis. These data were available in 52 patients (46%). The sensitivity was 60% vs 38% in 44 controls and the difference was significant (OR2.19[1.06-4.53];p=0.045). In the group who submitted stool samples, 20 were adenocarcinomas; 31 were squamous cell cancers; 9 were small cell; 7 were large cell; 4 were non- small cell; 4 were metastatic; 1 was indeterminate; and 1 had lepidic spread features; data was unavailable in 35 patients. (29%). Patients are summarized in
Table 1.
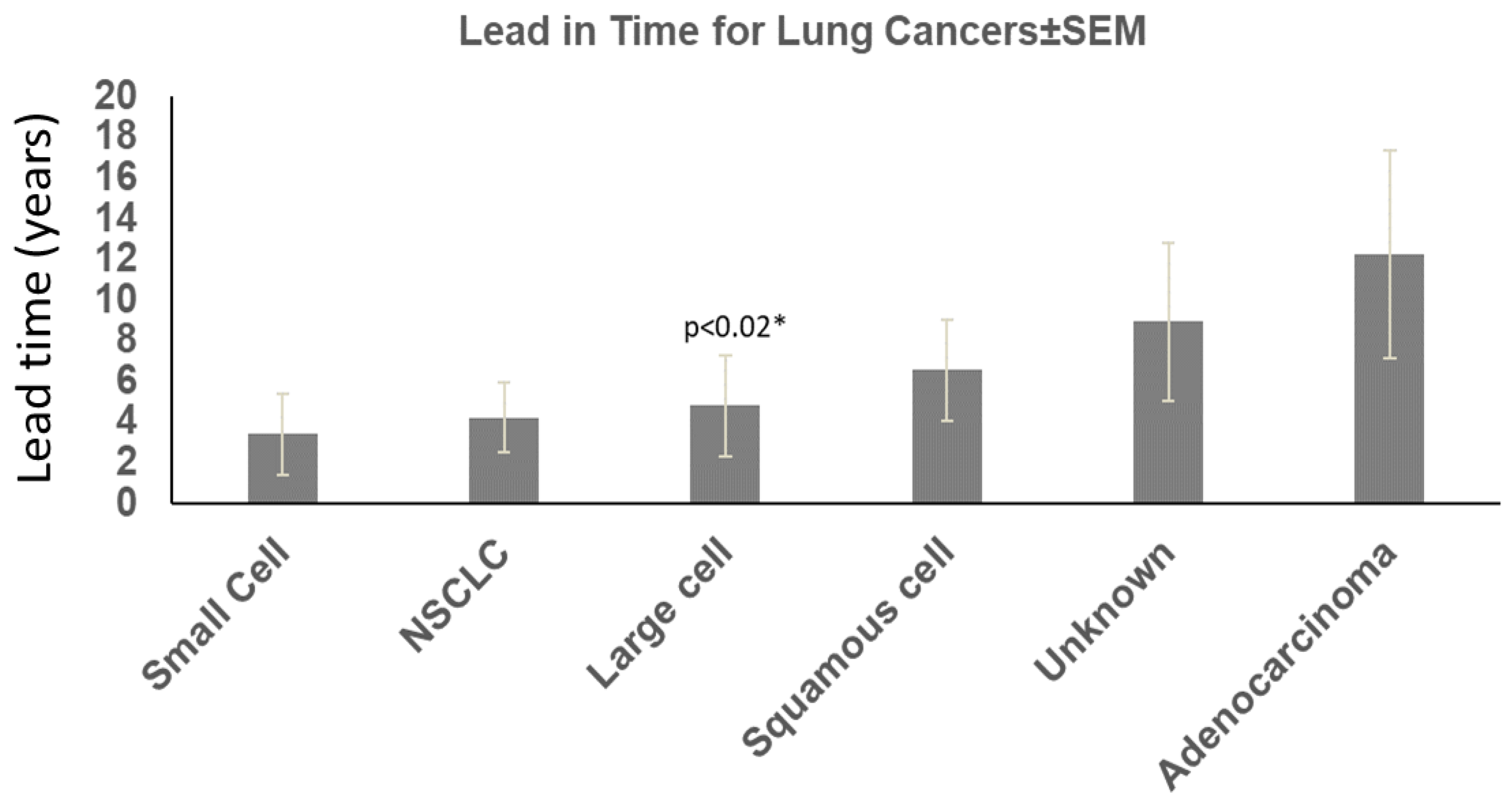
Of these 112 patients, 51 (46%) had prospective stool Adnab-9 binding tests testing. We found that about half the patients ultimately diagnosed with lung cancer had either stool ELISA or Western blot positivity for Adnab-9 compared to 14 patients were alive and 48 had expired (22.6% survival). 74 were black and 37 white and 1 unknown. 101 were male and 9 were females (2 unknown); average age was 63.78±10.82 years at time of enrollment. 49 were actively smoking and 26 were not. Quantitively, data were available in over half the patients: 6 had quit, 24 had <30pyh, 14 <60pyh 12<100pyh and 15>100pyh. 58 had a BMI<28kg/m and 24 were greater where available. 21 did not have a second cancer diagnosis. According to tumor type adenocarcinoma lead in time from test to diagnosis was 10.96±6.41 years (age 57.77±9.43); large cell 4.09±3.39 Years (age 65.20±8.08); non-small cell cancer 4.55±4.20 years (age 65.00±7.53); squamous cell cancer 8.38±6.53 years (age 64.15±11.72); small cell cancer 3.31±3.00 years (age 72.33±7.79) . 9.46± 5.34 years was the lead in time where the type of cancer was unknown (age 65.93±10.4).
Figure 1.
Lead-in Time and Lung Cancer Types.
Figure 1.
Lead-in Time and Lung Cancer Types.
The “*” shows the significance when comparing lead in time for adenocarcinoma versus large cell cancers. The other significant differences between cancer cases and controls were: age where patients with cancer over 50 years of age predominated over control cases (78% versus 62%; 2.16(1.37-3.40) chi-square with Yates correction; Black African ancestry (67 vs 52%;1.83[1.22-2.75]; p<0.005; less obesity (BMI<80m/Kg2 in the lung cancer group (29 vs 51%; 0.39[0.24- 0.64];p<0.0002); smoking 65 vs 36% (3.34[2.05-5.46];p<0.0001); more additional malignancies 81% versus 71% (p<0.037, Yates correction); and family history of lung cancer in 2% versus 0.11% in controls <0.02, 16.69[2.33-119.70] by Fishers Exact test. The results are summarized in
Table 1.
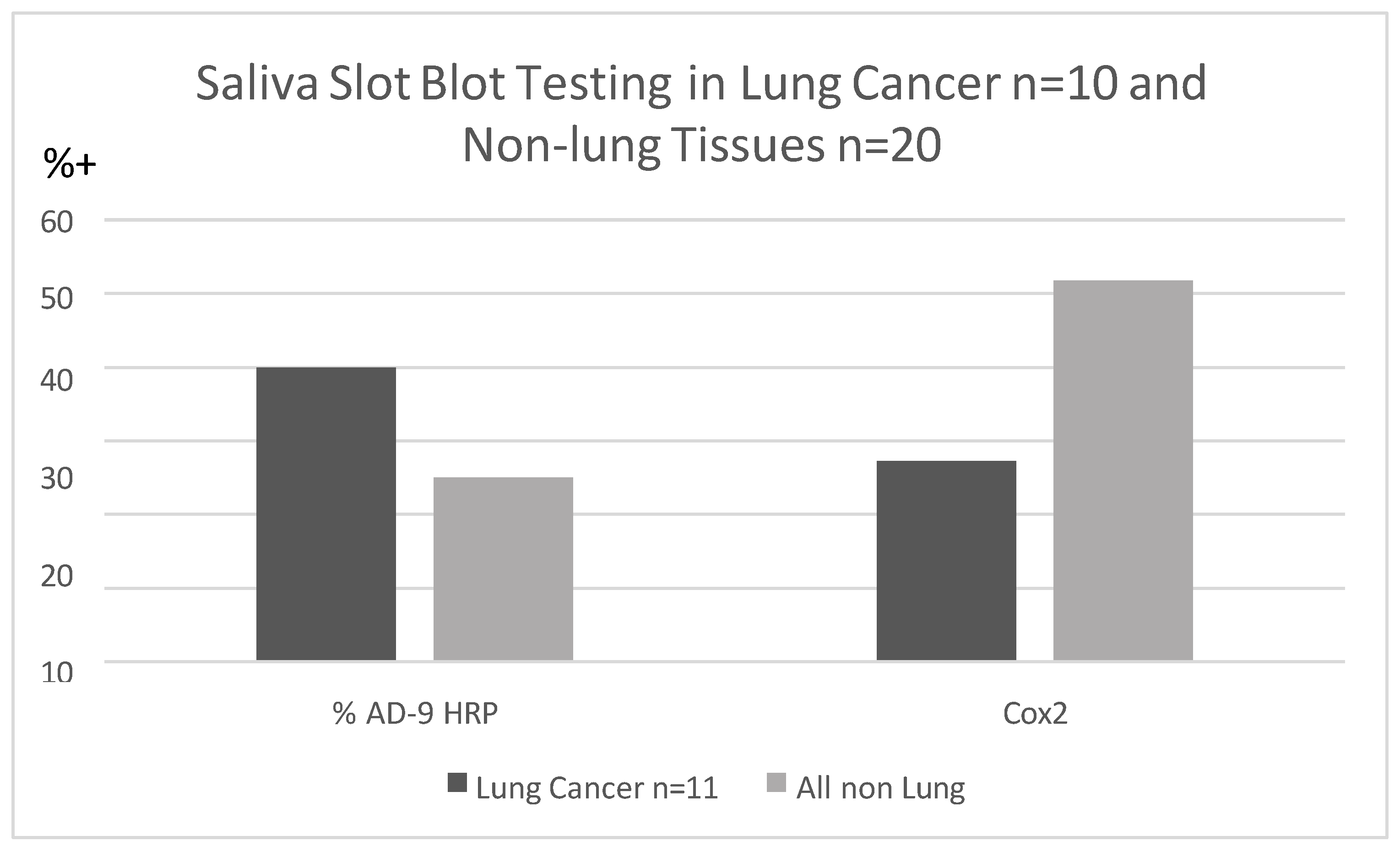
Saliva specimens collected before lung cancer diagnosis were reacted with p87 and OSN [
9], for innate immune and adoptive immune systems but were not found to be clinically useful when standardized by protein contrast saliva peroxidase activity difference between patients and controls was significantly different despite relatively small numbers. Inherent salivary peroxidase activity in the LC group was significantly lower (OD<0.05/1 µg protein) less (P<0.05) than in controls (64.3% positive). Although not significantly different we did find that Ad-9 bound to saliva of lung cancer patients more that non-lung controls and Cox2 antibody binding using horse-radish peroxidase to detect substrate, showed an inverse relationship (
Figure 2).
Figure 2 shows saliva binding of Adnab-9 in slot blots are more sensitive in patient with lung cancer than Cox-2 antibody binding but inferior to historic stool and effluent binding as noted above.
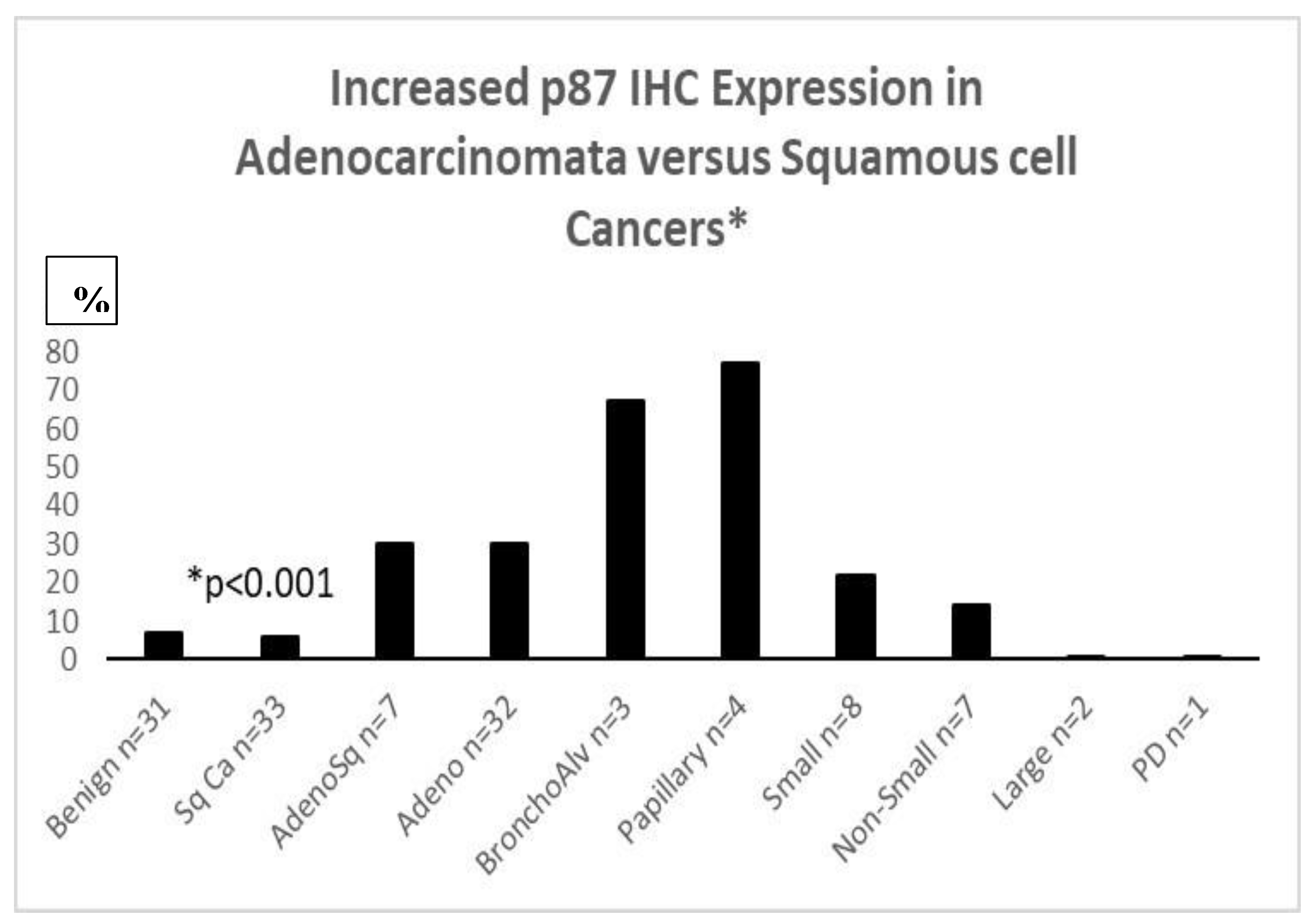
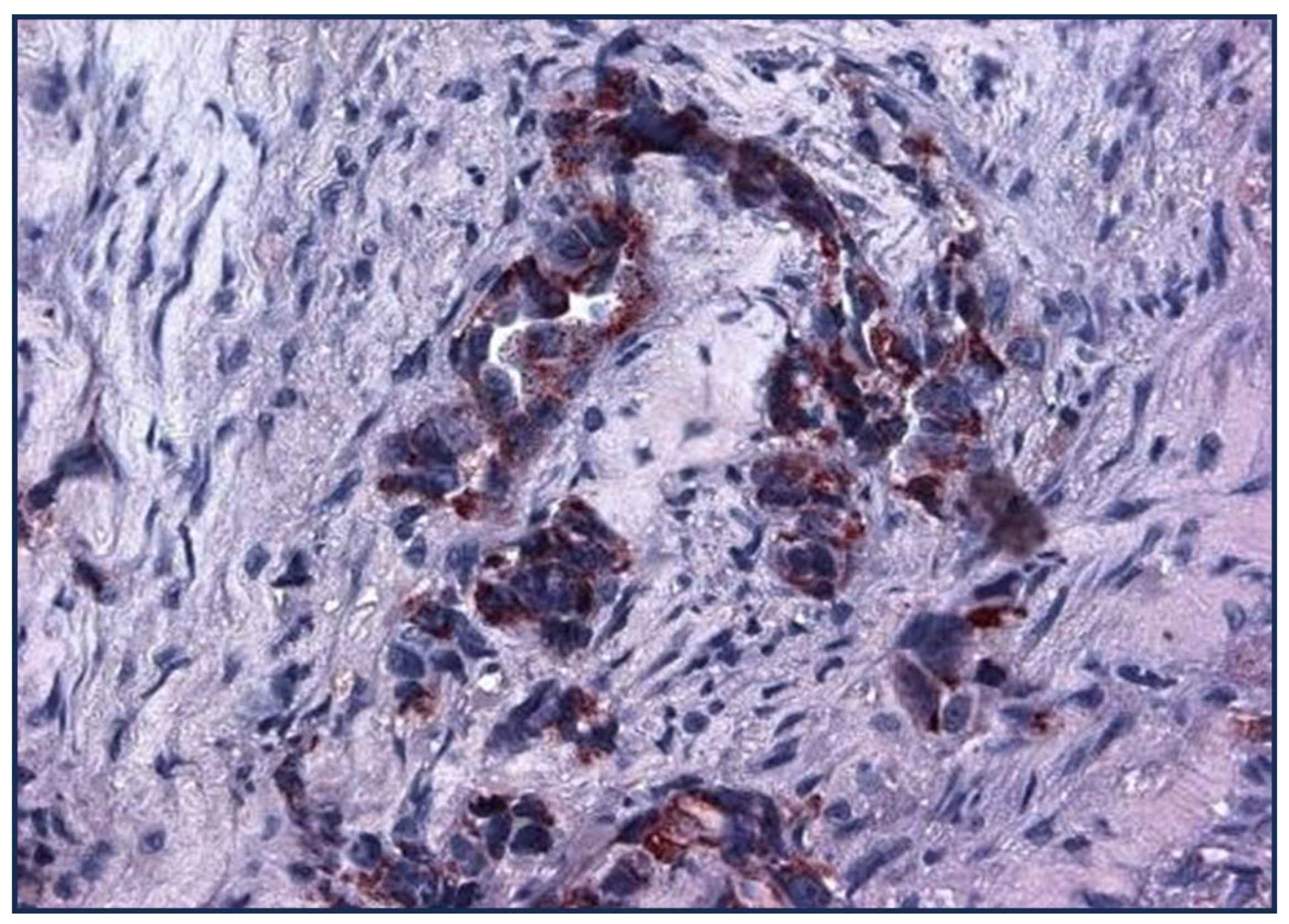
IHC for p87 favors certain phenotypes (
Figure 3) and also shares an inverse relation with prognosis in the higher graded tumors (
Figure 4). Of seven lung cancer IHC samples, 3 were positive, 4 were negative. Only 1 of 27 normal lung samples were positive (OR11.6[CI1.04-128.97;p<0.049]), see
Figure 3 for a summary of the entire IHC group and individual cancers. All of the lung cancer KCI patients had a family history of lung cancer.
Figure 3: Bar Diagram Showing Percentage of Various Lung Cancer Phenotypes Labeling with anti-p87, Adnab-9. Bronchoalveolar (lepidic-spread) and papillary cancers were positive for labeling in over 60%.
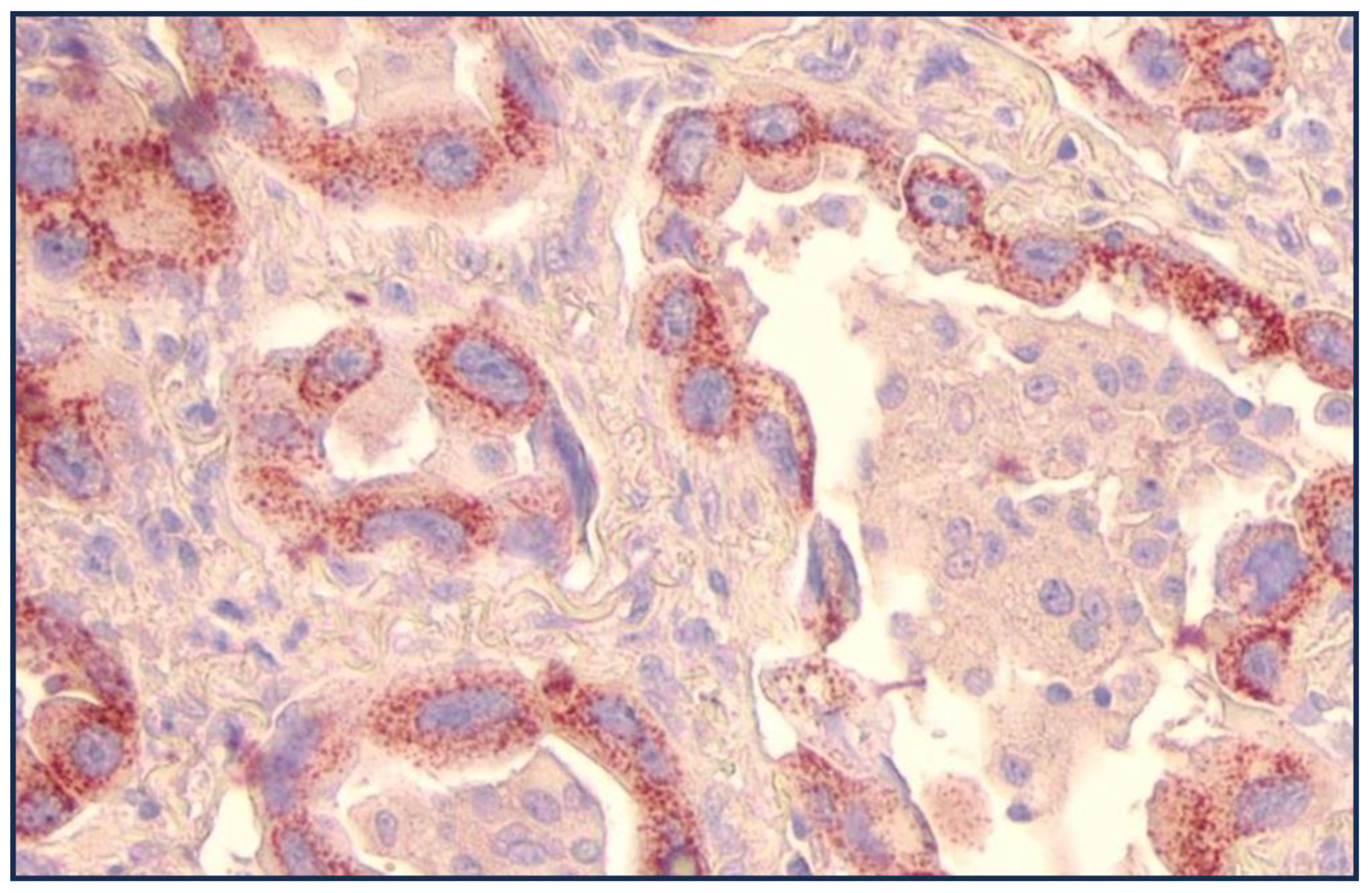
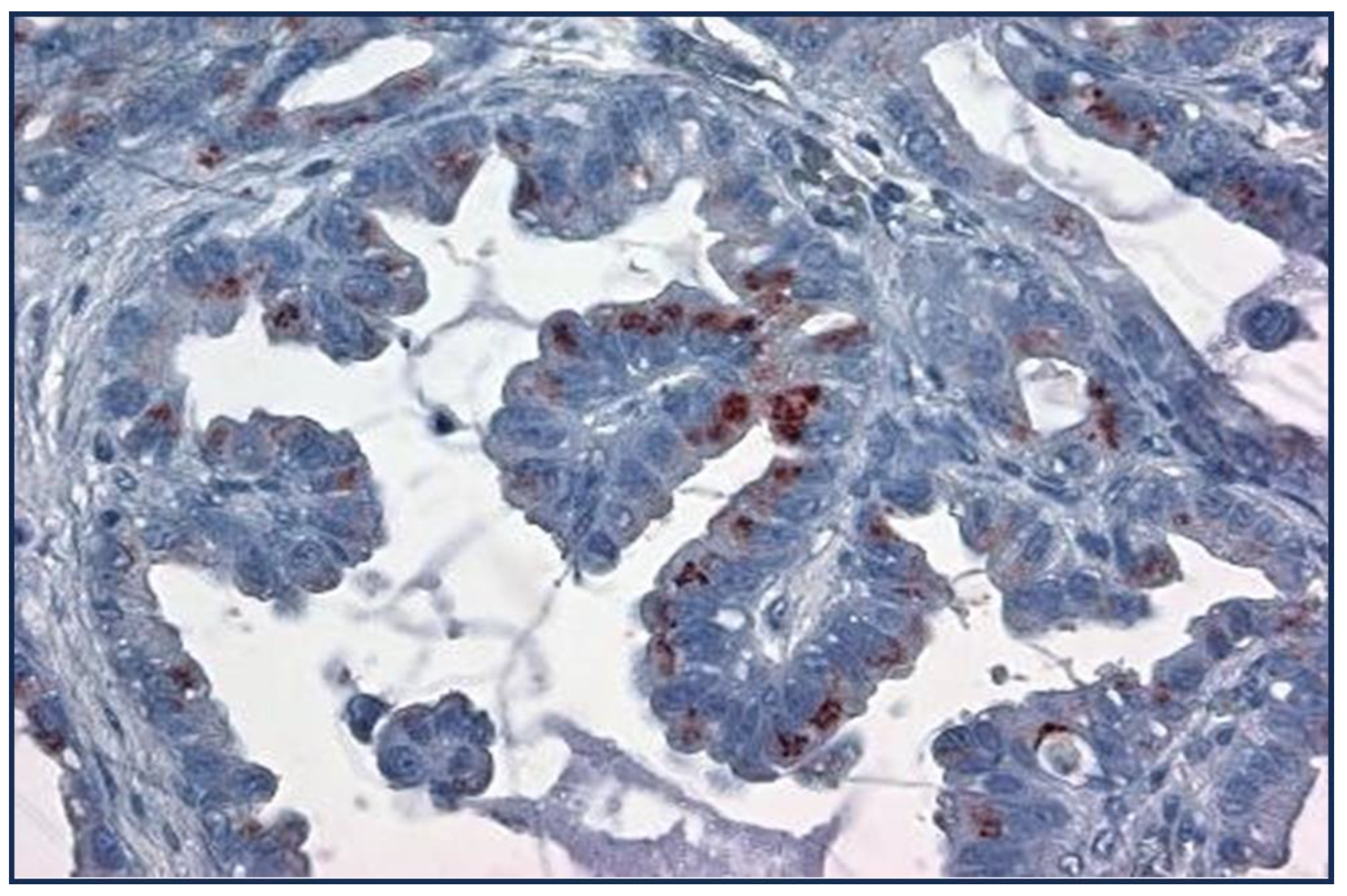
Figure 4,
Figure 5,
Figure 6,
Figure 7 and
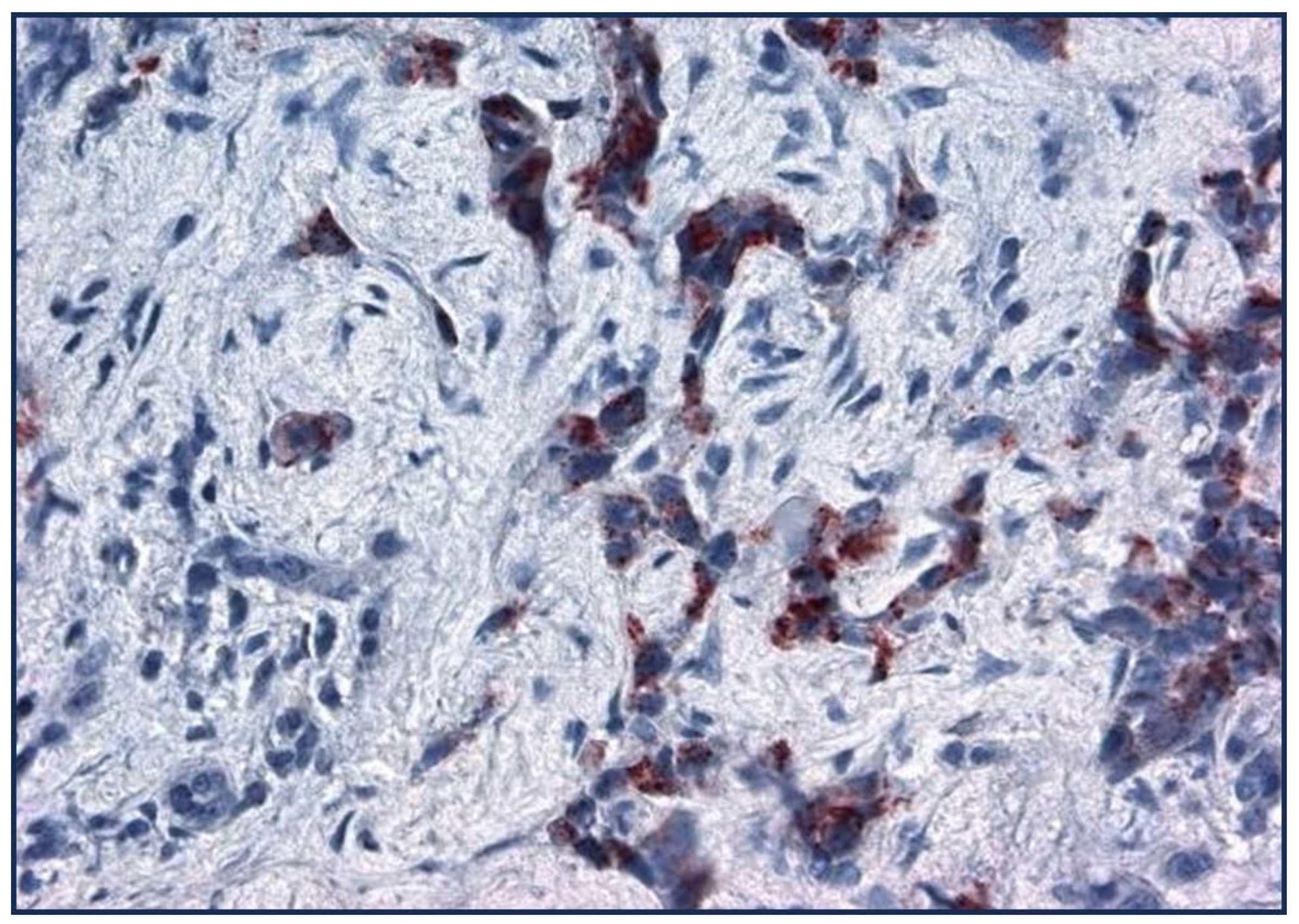
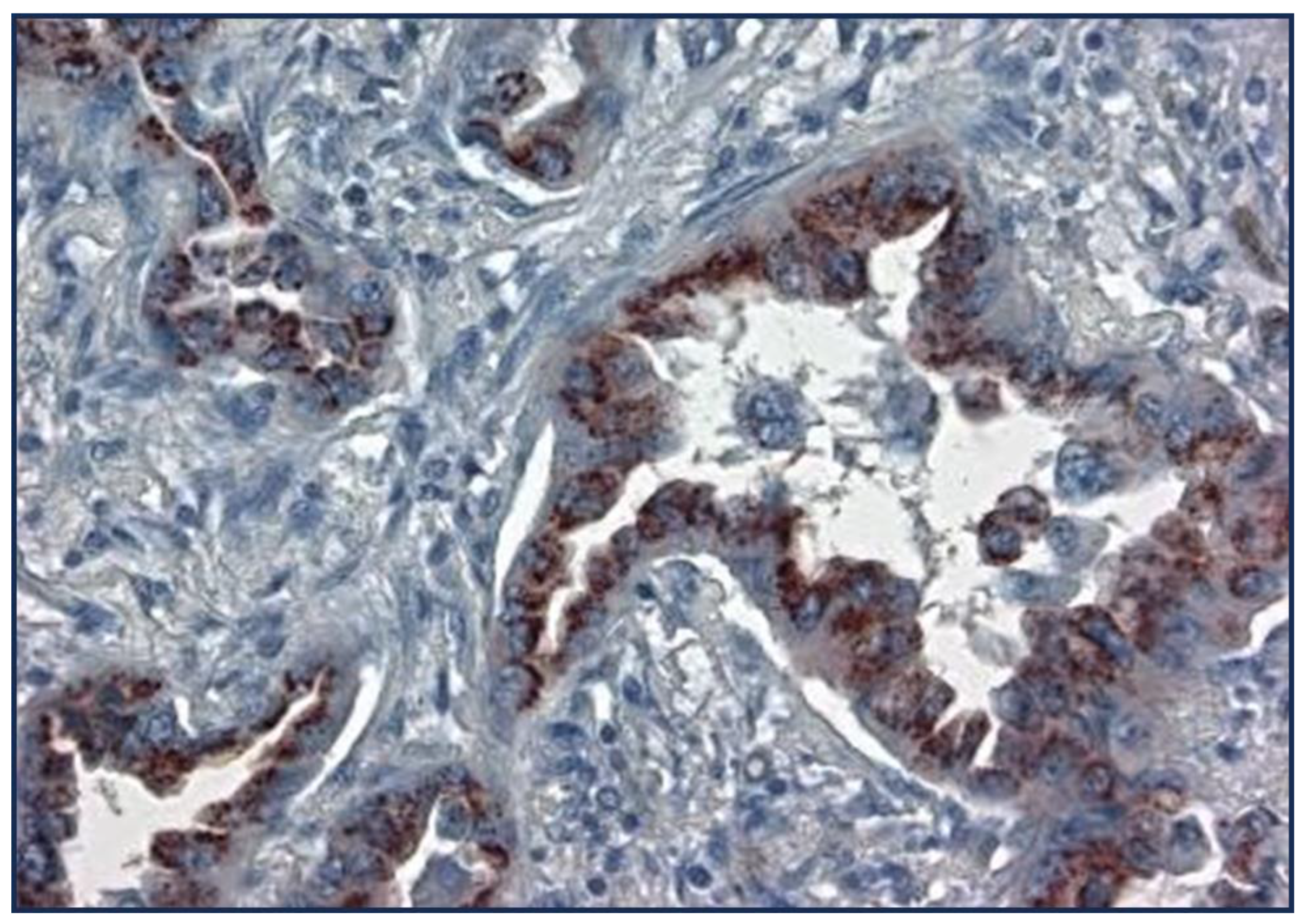
Figure 8 are photomicrographs showing Adnab-9 labeling of representative sections of various forms of lung cancers.
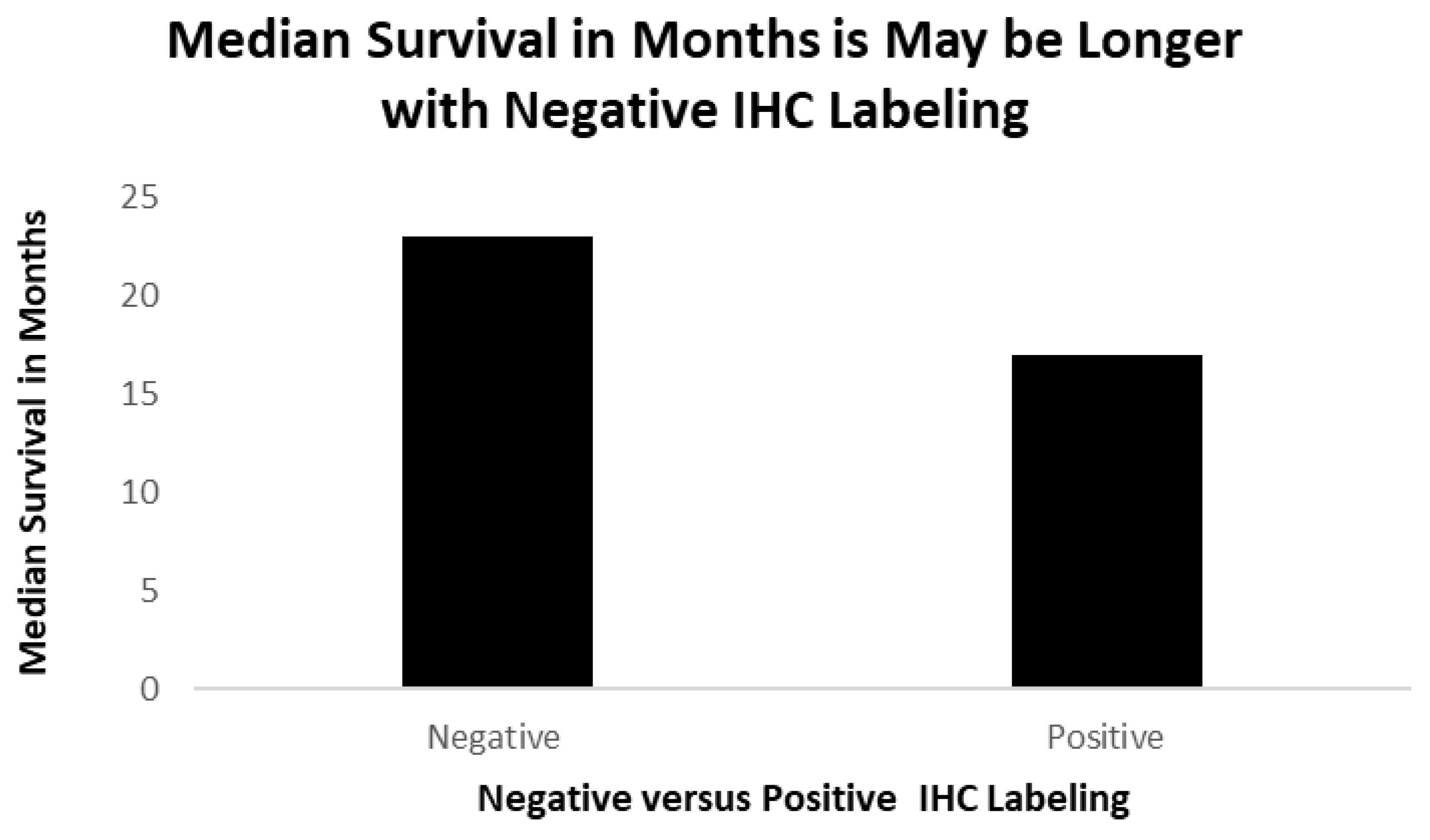
Figure 9 depicts survival in patients with positive IHC labeling versus those without.
Figure 4 shows a view of a lung adenocarcinoma with golgi staining and a lepidic form of infiltration. The substate is ethylaminocarbazine (EAC) which when present is reddish-brown in color.
A papillary lung cancer at high power is seen to stain the golgi apparatus with reddish brown substrate but not uniformly.
Dense, focal dark, reddish p87 cytoplasmic deposits are seen in this invasive focus of NSCLC with a fibroblastic response.
The figure shows golgi staining in an adenocarcinoma with a less fibrocystic response.
Figure 8 shows that while the NSCLC cancer cells are positive most of the non-cancer tissue does not take up the antibody.
The positive cases had on average 8.3 months survival (one case is still alive and un-staged now, one had local disease, one distant disease) while the negative cases averaged 23 months of survival, depicted in
Figure 8, (two with regional disease and 2 with distant disease)
Figure 9: A Bar Diagram showing Survival Times of 51 Lung Cancer Patients, Formalin’ Fixed and Paraffin Embedded Slides, Staining for p87 (positive) and those without (negative).
When comparing primary lung cancer patients who had negative stool testing (n=25) to those with positive testing (n=26) there were no differences in demographics, or survival (p=0.35). Significant differences were seen in historic ferritin levels (358±314 versus 149±129;p<0.034). Higher levels of native antigens in extracts of colonoscopy biopsies were found in the cecum and ascending colon in patients with negative p87 stool tests (cecum 0.132±0.014 versus 0.055±0.031; p<0.035 and ascending colon 0.203±0.059 versus 0.042±0.023; p<0.008) suggestion a lack of shedding from the right side of the colon that harbors Paneth cells reflected in the stool findings. The ratio of historic blood ferritin:fecal p87 (FERAD ratio) thought to reflect the activity of the InImS was found to be commensurately high in patients with very low fecal p87 and higher ferritin levels(179,882±302,992 versus 2,987±3492; P<0.048). The patients with a negative stool and higher FERAD levels tended to survive longer that those with positive p87 stools but lower FERAD indices (10.6±4.8 versus 7.3±4.4 years, p=0.35). The results are summarized in
Table 3.
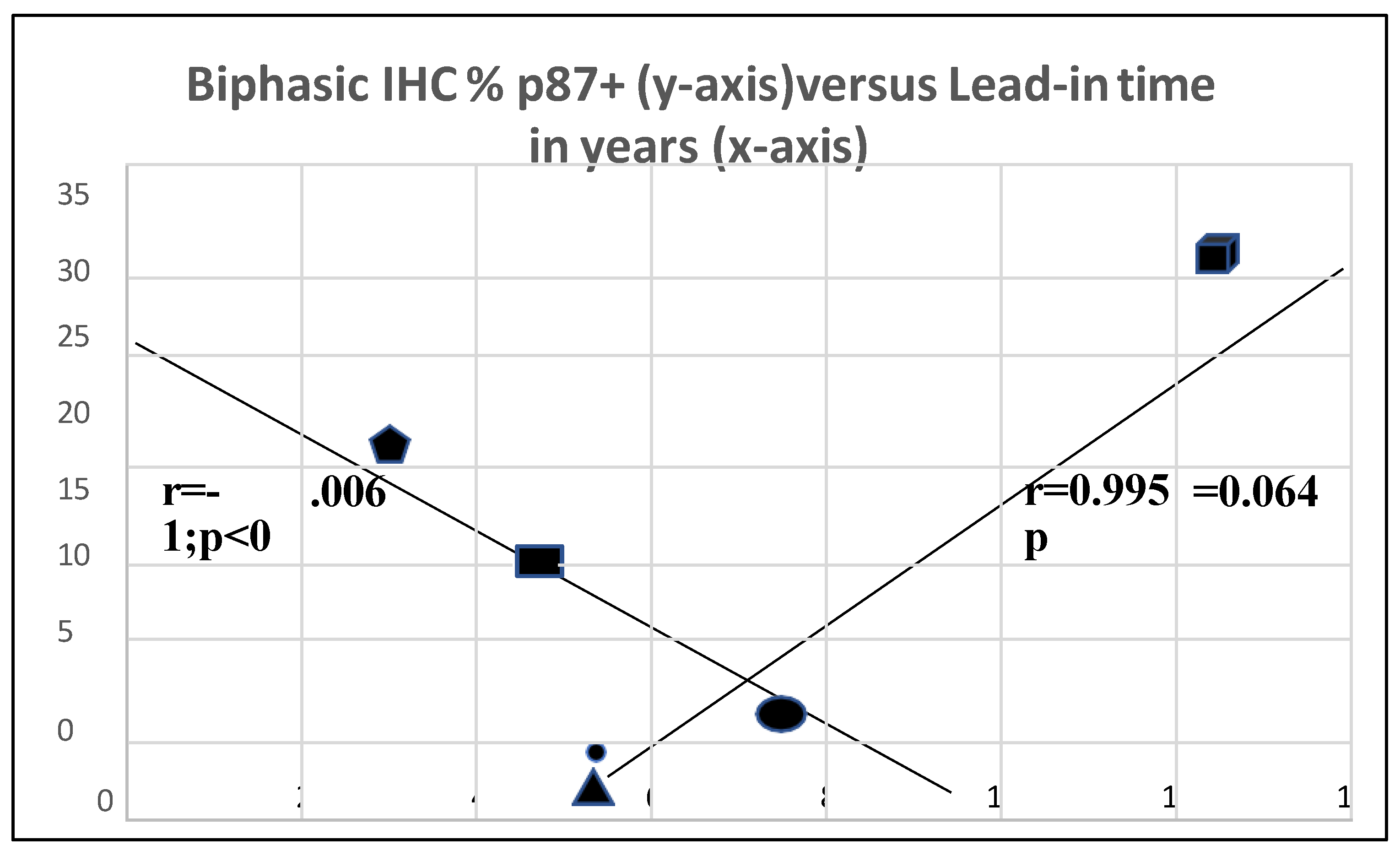
The interrelationship between p87 staining and lead-in time is quite complex and appears to be biphasic (
Figure 8). The 2 axes interest with the coordinates for squamous cell cancer at the intersection (oval symbol) and a strong trend to a direct correlation of adenocarcinoma (faceted square) and large cell carcinoma (triangle) and a highly significant inverse correlation with NSLC at the upper end (pentagram) and small cell cancer (rectangle) at the lower end. This suggests that for some p87+ cancers prognosis is better and for others, worse. This is not unusual for lung cancers [
11] where morphologic characteristics are of profound importance for type of treatment and hence prognosis. Certain assumptions were made that p87 % stain was uniform for type of cancer since the data was derived from 2 different populations of patients.
Figure 10. symbols show a solid block square for adenocarcinoma,

; solid rectangle for NSCLC,

; a solid circle for squamous cell,

; ;a solid triangle for a large cell,

; a solid pentagram for small cell,

.
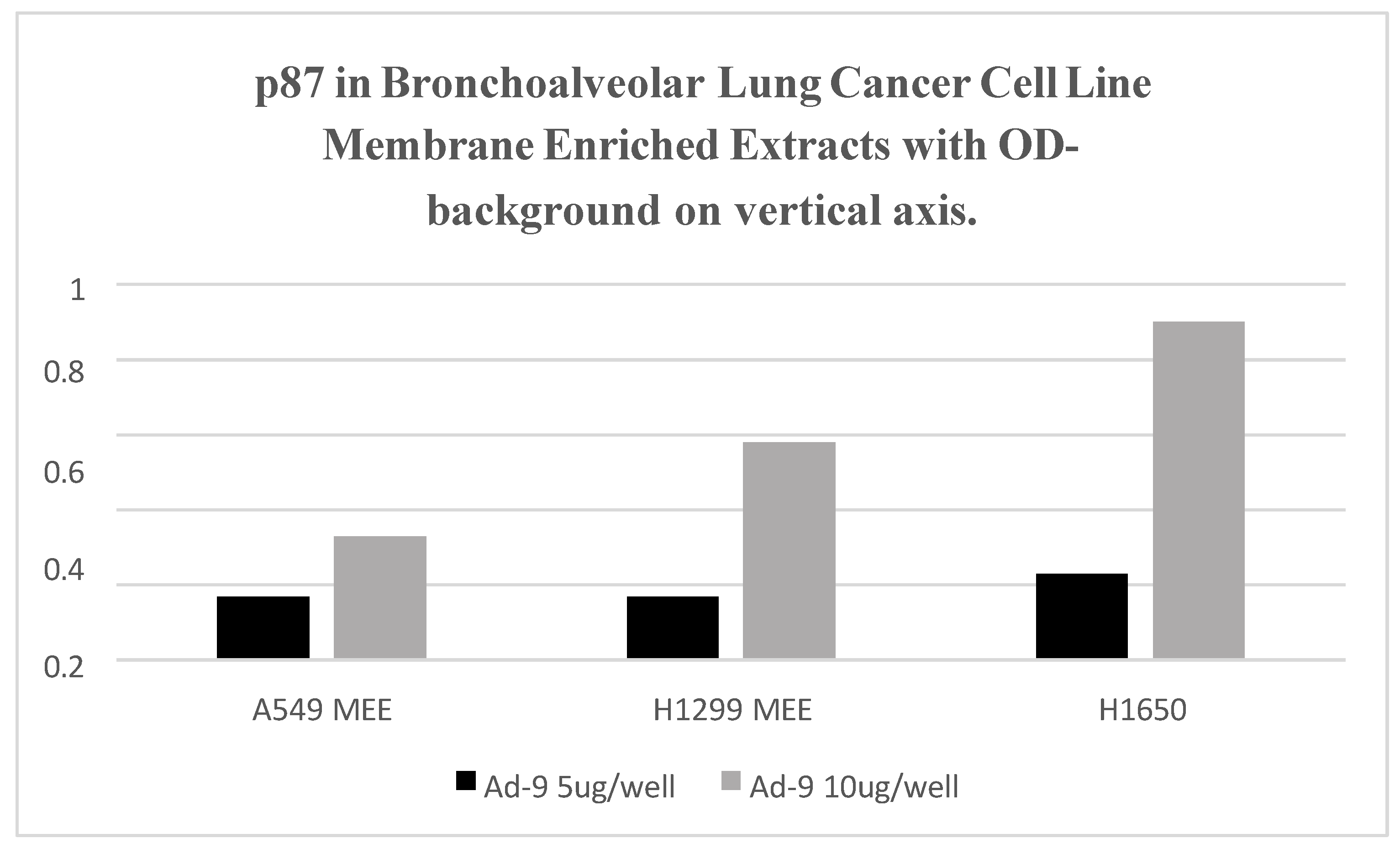
Figure 11 shows increase of binding with increase of protein content in 3 Lepidic Spread Lung Adenocarcinoma cell lines. H1650 p87 binding is equivalent to the positive control (data not shown).
Adnab-9 treated lepidic bronchoalveolar cancer cell lines is antiproliferative further supporting our observations (data not shown).
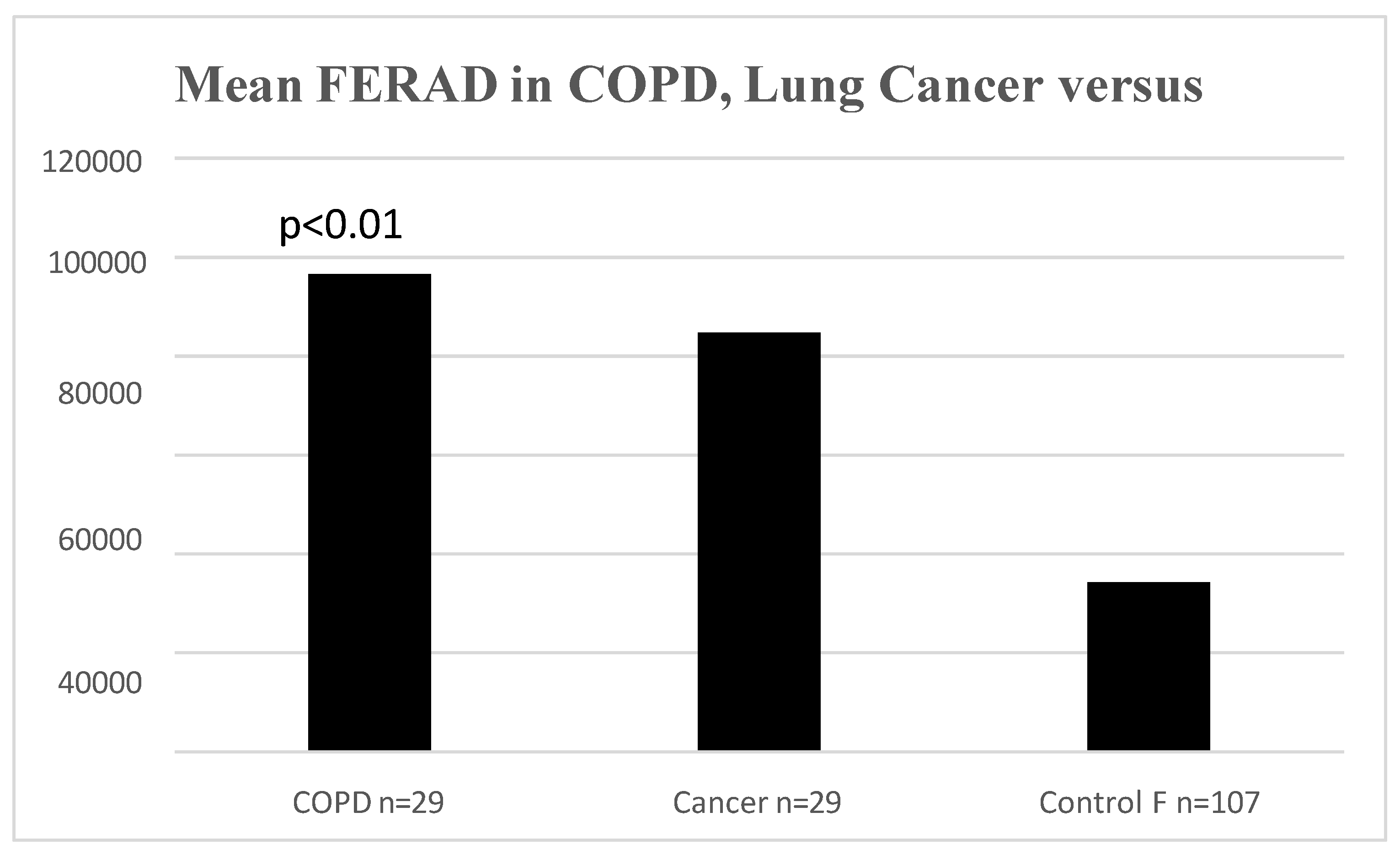
We found that there was a statistically significant difference between the FERAD ratio in patients with COPD and controls (
Figure 12).
There is a statistical difference between COPD patients and controls (p<0.011) in
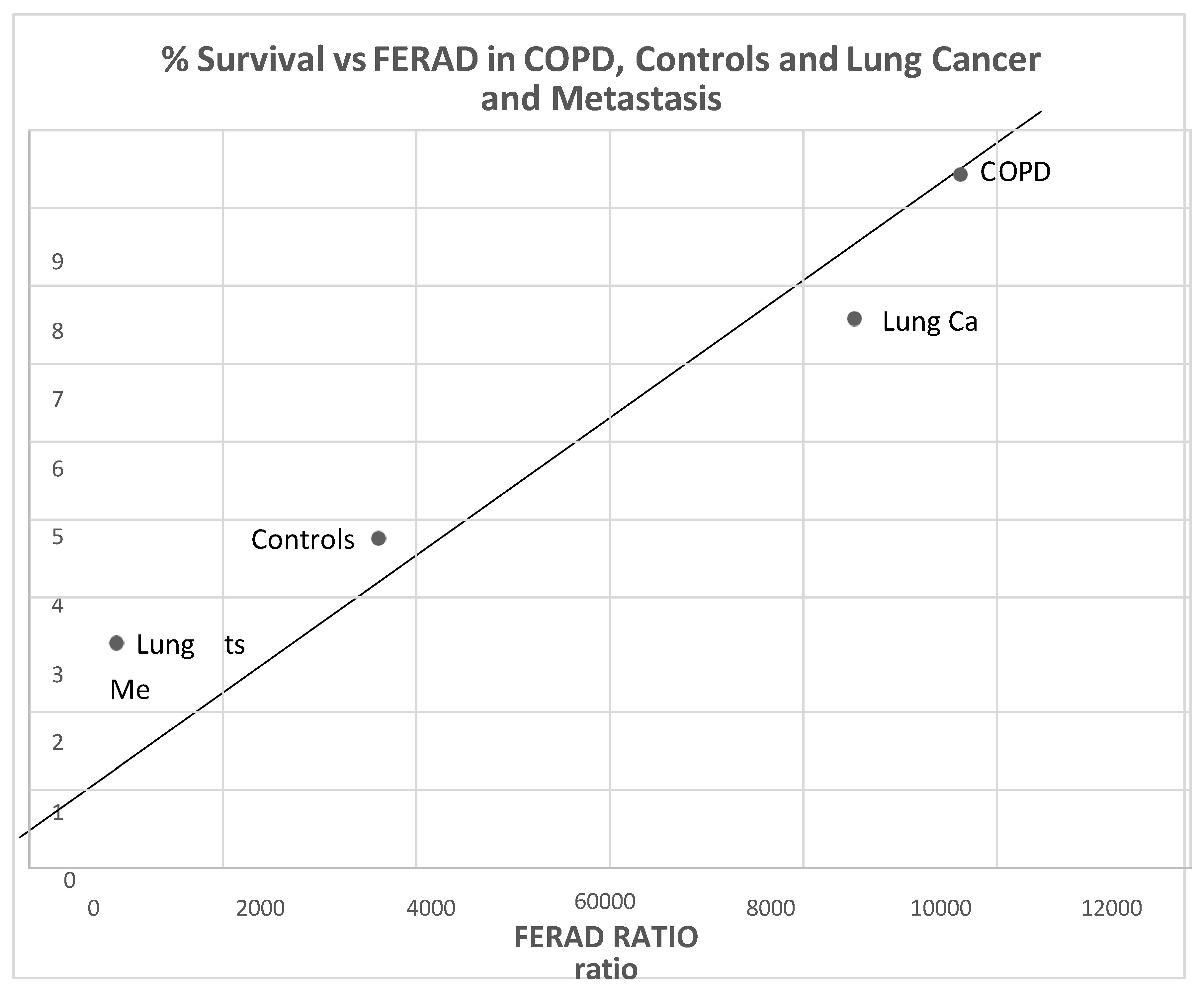
Figure 12. Interestingly there is also a statistically significant positive correlation between survival in lung cancer patients both primary and metastatic, and those with COPD and controls (
Figure 13).
From left to right the dots designate cancer metastatic (Mets) to lungs; primary lung cancer; COPD patients and controls.
3. Discussion:
p87 can detect cancers up to 12 years before they are diagnosed with reasonable sensitivity and specificity for most common forms of lung cancer. This strategy can select out patients at high- risk who could undergo radiologic imaging leading to a much earlier diagnosis that could currently achieved. The p87 biomarker appears to identify the patients with a poorer prognosis and thus aiding in detection in these tumors at a very early stage will allow for effective intervention. Hopefully this approach will reduce mortality from this common organ cancer site. p87 staining suggests a differential stain in lung cancer as opposed to normal tissues. Conceptually, Adnab-9 recognizes the p87 antigen [
8], a constituent of putatively activated pulmonary type 2 pneumocytes and particularly lung cancer cells. The p87 antigen is likely shed into sputum and swallowed may represent a useful potential tumor marker detectable by the Adnab-9 stool test. Of note is the fact that both α- Defensin5 and p87 are both Paneth cell secretory products yet the former is not expressed in the lung. However, β-defensins are secreted in the lung and earlier studies did find an cancer association of overexpression in about 40-50% in common forms of lung cancer but no association of human β-defensins (HBD) type 1.2 and 4 mRNA levels with histological type, tumor grade or stage of disease or suman levels of the peptide [
12]. Earlier, others [
13] had shown a correlation of HBD1 and 2 with lung cancer with an estimated sensitivity of 76.4% and specificity of 94% pre-surgery but no prospectively with respect to cancer diagnosis which was known at the time of venesection. A later summary of the data for HBD1,2 and 3 cautioned against generalization with different cancer types but allowed the association with tumor progression [
14]. The same caveats may be applied to p87 but the lead-in time for diagnosis is for now, unparalleled. Despite a similar cellular source as defensins, p87 outside of the lung does not usually label cancers but has been shown to be retrospectively diagnostic and prognostic in stool in both colorectal cancer (CRC), IPMN pancreatic subtype, and gastric cancer [
3,
15,
16,
17,
18] and prospective in the common form of pancreatic cancer [
19] where the lead-in time was 2.3 years. This and other work conform to biomarker standards proposed in 2018
[
11] such as objective measuring to which our standardized ELISA aligns, evaluated as usual biological process (product of the innate immune system); influence clinical decisions minimizing harm (p87 estimation is non-invasive, risk-free, and predictive); the biomarker must be stable and reproducible (p87 is stable for more than 10years [
19] in cold storage with a high correlation coefficient); must be sensitive and specific (while p87 is only moderately sensitive and specific ~60% for both), its lead-in time more than compensates but the algorithm for use has thus far not been developed definitively). Adnab-9 has been confirmed to be prognostic by an independent laboratory [
20], does not disrupt workflow and reduces cost and harm. p87 is an inexpensive, cost-effective ELISA-based test and envisaged follow-up would be down to top to minimize costs by allying the stool test with salivary peroxidase to increase specificity and both could be sent in the mail on fecal occult blood cards which has been shown to be acceptable and effective in large-scale [
10] CRC screening trials) . The medium should be convenient such as lung sources (exhaled breath or sputum) but blood [
21], saliva and urine are also convenient (p87 could be co-opted onto the organ specific neoantigen (OSN) urine test [
9] which we also used in this study in limited numbers (data not shown). Low dose computerized tomographic (LDCT) screening has been shown to reduce disease-specific mortality from lung cancer by 20% and all-cause by 7% but this has come at a cost of poor specificity with one quarter of screened patients exhibiting lesions with 96% proving to be false-positive associated with many drawbacks [
22]. They conclude that new modalities are promising but do not satisfy current goals to qualify as biomarkers of proven utility.
There are many pitfalls even with morphology used to characterize the type of lung cancer, for example, lepidic growth patterns a more unusual characteristic of invasive mucinous lung adenocarcinoma (
Figure 12) can be mistaken for metastatic pancreatic cancer [
23,
24]. Molecular testing, sometimes yielding similar results for both types of cancer, may confound the differential diagnosis [
25].
Table 1 shows interesting differences, some can be explained by lifestyle differences such as smoking and effects of being overweight but others are more challenging. Fewer “other cancers” is somewhat counter-intuitive. Black ethnicity is significantly more prevalent but this may be a normal inner-city distribution. The lethality of lung cancer despite significant advances is still imposing. Family history differences may suggest familial commonality of risk factors.
While
Table 2 shows no increased mortality based on p87 expression the differences may be explained by increased shedding particularly from the right colon where the colonic Paneth cells are distributed. If the numbers could be increased the current trend to increased mortality in p87+ patient may become significant. The innate immune system as defined by the FERAD ration suggests a significant reduction in p87+ patients which may have associated adverse events. The H1650 cell line has a EGFR mutation in exon 19 but is very resistant to EGFR-directed inhibitor treatment despite seeing responses in other cell lines showing the same mutation [
26]. It does express p87 and using anti-p87 Adnab-9 monoclonal, proliferation is reduced. This monoclonal should be considered in treatment trials of cancers with positive EGFR mutations yet showing anti-EGFR resistance.
 ; solid rectangle for NSCLC,
; solid rectangle for NSCLC,  ; a solid circle for squamous cell,
; a solid circle for squamous cell,  ; ;a solid triangle for a large cell,
; ;a solid triangle for a large cell,  ; a solid pentagram for small cell,
; a solid pentagram for small cell,  .
.