Submitted:
19 August 2024
Posted:
20 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
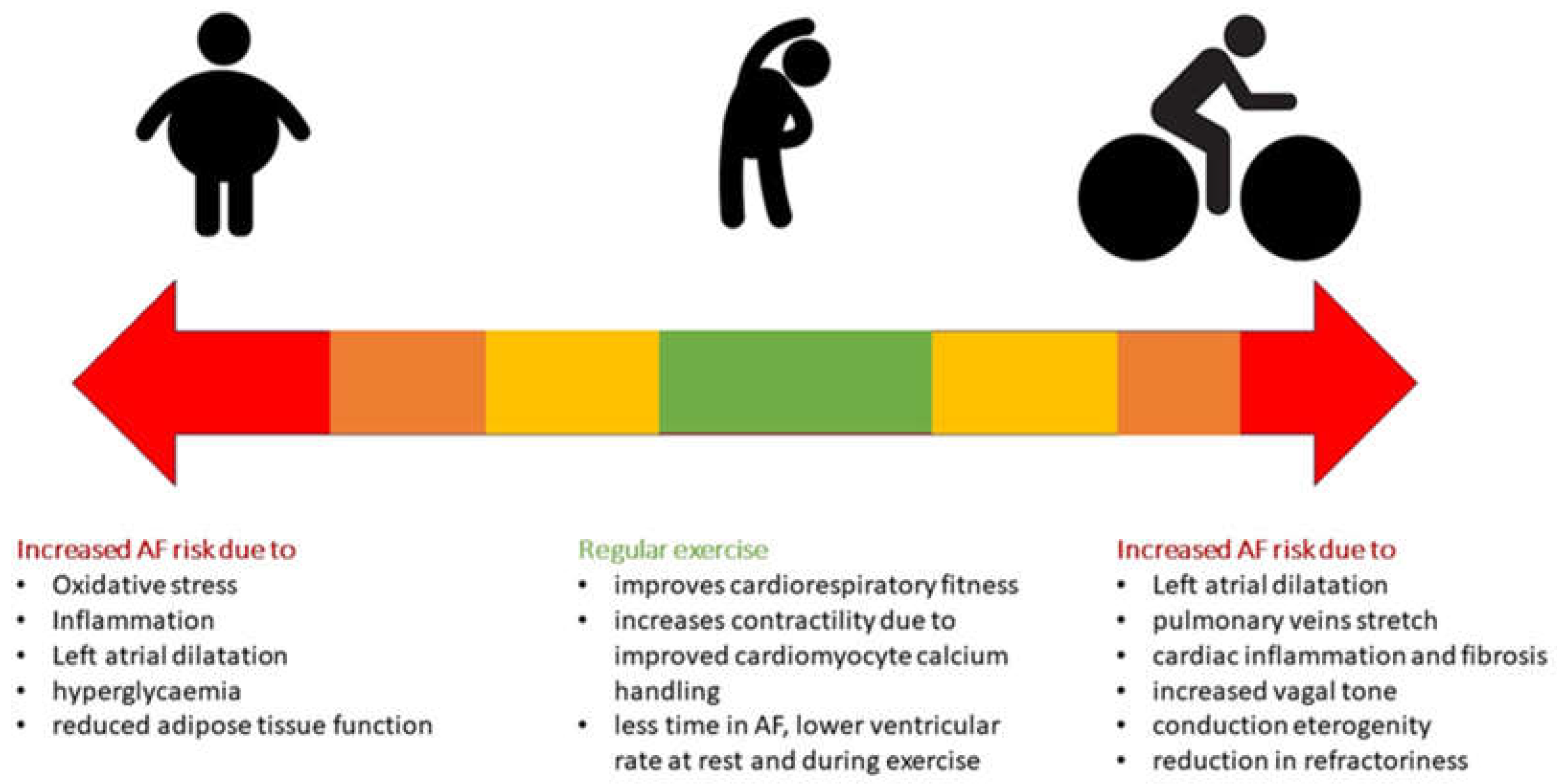
2. Epidemiology and Predisposal Factors
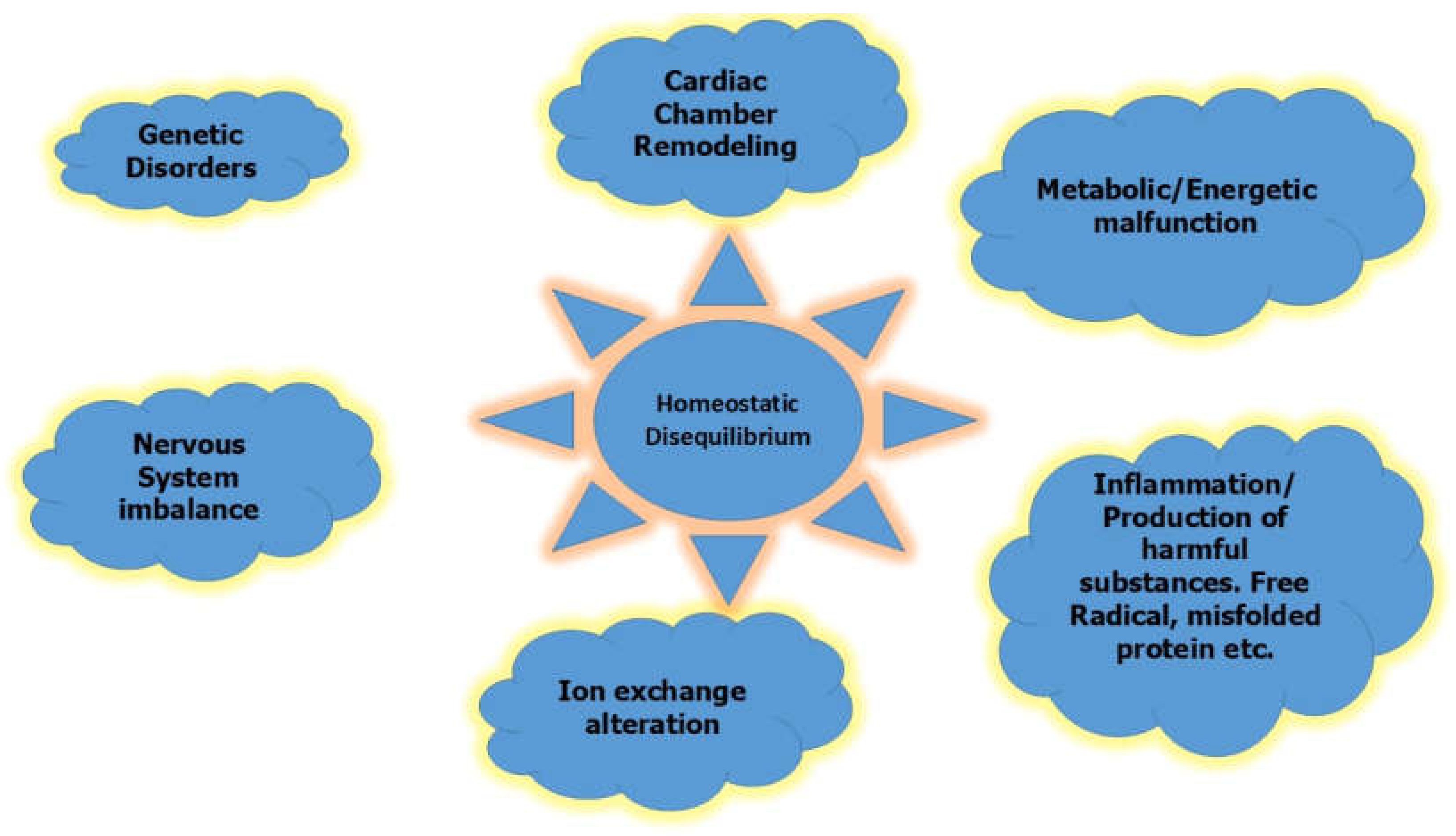
3. Pathophysiology
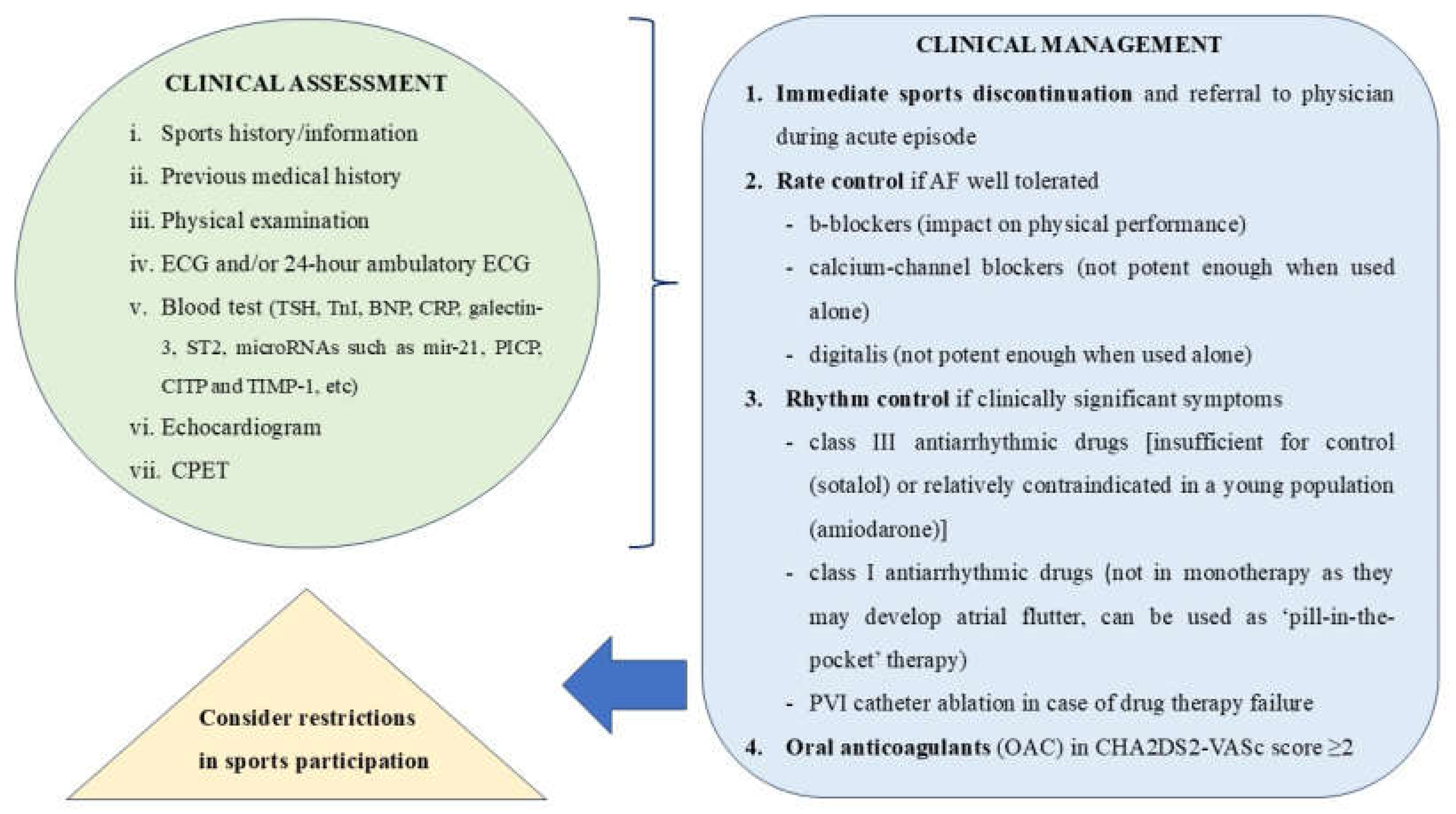
4. Clinical Significance, Screening and Management
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Abed HS, Wittert GA, Leong DP, Shirazi MG, Bahrami B, Middeldorp ME, Lorimer MF, Lau DH, Antic NA, Brooks AG, et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA. 2013;310(19):2050-60.
- Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, Stanford FC, Kohl HW 3rd, Blair SN. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124(23):2483-90.
- Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64(5):472-81.
- Turagam MK, Velagapudi P, Kocheril AG. Atrial fibrillation in athletes. Am J Cardiol. 2012;109(2):296-302.
- Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis. Europace. 2009;11(9):1156-9.
- Wilhelm M, Roten L, Tanner H, Wilhelm I, Schmid JP, Saner H. Atrial remodeling, autonomic tone, and lifetime training hours in nonelite athletes. Am J Cardiol. 2011;108(4):580-5.
- Mont L, Tamborero D, Elosua R, Molina I, Coll-Vinent B, Sitges M, Vidal B, Scalise A, Tejeira A, Berruezo A, et al. Physical activity, height, and left atrial size are independent risk factors for lone atrial fibrillation in middle-aged healthy individuals. Europace. 2008;10(1):15-20.
- Myrstad M, Nystad W, Graff-Iversen S, Thelle DS, Stigum H, Aarønæs M, Ranhoff AH. Effect of years of endurance exercise on risk of atrial fibrillation and atrial flutter. Am J Cardiol. 2014;114(8):1229-33.
- Elliott AD, Mahajan R, Pathak RK, Lau DH, Sanders P. Exercise Training and Atrial Fibrillation: Further Evidence for the Importance of Lifestyle Change. Circulation. 2016;133(5):457-9.
- Pelliccia A, Fagard R, Bjørnstad HH, Anastassakis A, Arbustini E, Assanelli D, Biffi A, Borjesson M, Carrè F, Corrado D, et al. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(14):1422-45.
- Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, Collet JP, Corrado D, Drezner JA, Halle M, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42(1):17-96.
- Estes NAM 3rd, Madias C. Atrial Fibrillation in Athletes: A Lesson in the Virtue of Moderation. JACC Clin Electrophysiol. 2017;3(9):921-928.
- Sanchis-Gomar F, Perez-Quilis C, Lippi G, Cervellin G, Leischik R, Löllgen H, Serrano-Ostáriz E, Lucia A. Atrial fibrillation in highly trained endurance athletes - Description of a syndrome. Int J Cardiol. 2017;226:11-20.
- Andersen K, Farahmand B, Ahlbom A, Held C, Ljunghall S, Michaëlsson K, Sundström J. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. Eur Heart J. 2013;34(47):3624-31.
- Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 2008;118(8):800-7.
- Ofman P, Khawaja O, Rahilly-Tierney CR, Peralta A, Hoffmeister P, Reynolds MR, Gaziano JM, Djousse L. Regular physical activity and risk of atrial fibrillation: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2013;6(2):252-6.
- Mohanty S, Mohanty P, Tamaki M, Natale V, Gianni C, Trivedi C, Gokoglan Y, DI Biase L, Natale A. Differential Association of Exercise Intensity With Risk of Atrial Fibrillation in Men and Women: Evidence from a Meta-Analysis. J Cardiovasc Electrophysiol. 2016;27(9):1021-9.
- Petrungaro M, Fusco L, Cavarretta E, Scarà A, Borrelli A, Romano S, Petroni R, D’Ascenzi F, Sciarra L. Long-Term Sports Practice and Atrial Fibrillation: An Updated Review of a Complex Relationship. J Cardiovasc Dev Dis. 2023;10(5):218.
- Morseth B, Graff-Iversen S, Jacobsen BK, Jørgensen L, Nyrnes A, Thelle DS, Vestergaard P, Løchen ML. Physical activity, resting heart rate, and atrial fibrillation: the Tromsø Study. Eur Heart J. 2016;37(29):2307-13.
- Sciarra L, Cavarretta E, Siciliani S, Sette A, Scarà A, Grieco D, DE Ruvo E, Palamà Z, Nesti M, Romano S, et al. Managing athletes with palpitations of unknown origin with an external loop recorder: a cohort study. J Sports Med Phys Fitness. 2022;62(4):554-559.
- La Gerche A, Schmied CM. Atrial fibrillation in athletes and the interplay between exercise and health. Eur Heart J. 2013;34(47):3599-602.
- Johansen KR, Ranhoff AH, Sørensen E, Nes BM, Heitmann KA, Apelland T, Bucher Sandbakk S, Wilsgaard T, Løchen ML, Thelle DS, et al. Risk of atrial fibrillation and stroke among older men exposed to prolonged endurance sport practice: a 10-year follow-up. The Birkebeiner Ageing Study and the Tromsø Study. Open Heart. 2022;9(2):e002154.
- Svedberg N, Sundström J, James S, Hållmarker U, Hambraeus K, Andersen K. Long-Term Incidence of Atrial Fibrillation and Stroke Among Cross-Country Skiers. Circulation 2019;140(11):910–920.
- Boraita A, Santos-Lozano A, Heras ME, González-Amigo F, López-Ortiz S, Villacastín JP, Lucia A. Incidence of Atrial Fibrillation in Elite Athletes. JAMA Cardiol. 2018;3(12):1200-1205.
- Newman W, Parry-Williams G, Wiles J, Edwards J, Hulbert S, Kipourou K, Papadakis M, Sharma R, O’Driscoll J. Risk of atrial fibrillation in athletes: a systematic review and meta-analysis. Br J Sports Med. 2021;55(21):1233-1238.
- Wernhart S, Halle M. Atrial fibrillation and long-term sports practice: epidemiology and mechanisms. Clin Res Cardiol. 2015;104(5):369-79.
- Calvo N, Ramos P, Montserrat S, Guasch E, Coll-Vinent B, Domenech M, Bisbal F, Hevia S, Vidorreta S, Borras R, et al. Emerging risk factors and the dose-response relationship between physical activity and lone atrial fibrillation: a prospective case-control study. Europace. 2016;18(1):57-63.
- Drca N, Larsson SC, Grannas D, Jensen-Urstad M. Elite female endurance athletes are at increased risk of atrial fibrillation compared to the general population: a matched cohort study. Br J Sports Med. 2023;57(18):1175-1179.
- Myrstad M, Johansen KR, Sørensen E, Løchen ML, Ranhoff AH, Morseth B. Atrial fibrillation in female endurance athletes. Eur J Prev Cardiol. 2024;31(5):e27-e29.
- Wilhelm M, Roten L, Tanner H, Wilhelm I, Schmid JP, Saner H. Gender differences of atrial and ventricular remodeling and autonomic tone in nonelite athletes. Am J Cardiol. 2011;108(10):1489-95.
- Sanchis L, Sanz-de La Garza M, Bijnens B, Giraldeau G, Grazioli G, Marin J, Gabrielli L, Montserrat S, Sitges M. Gender influence on the adaptation of atrial performance to training. Eur J Sport Sci. 2017;17(6):720-726.
- Shoemaker MB, Shah RL, Roden DM, Perez MV. How Will Genetics Inform the Clinical Care of Atrial Fibrillation? Circ Res. 2020;127(1):111-127.
- Norby FL, Benjamin EJ, Alonso A, Chugh SS. Racial and Ethnic Considerations in Patients With Atrial Fibrillation: JACC Focus Seminar 5/9. J Am Coll Cardiol. 2021;78(25):2563-2572.
- Gomez SE, Fazal M, Nunes JC, Shah S, Perino AC, Narayan SM, Tamirisa KP, Han JK, Rodriguez F, Baykaner T. Racial, ethnic, and sex disparities in atrial fibrillation management: rate and rhythm control. J Interv Card Electrophysiol. 2023;66(5):1279-1290.
- Chalazan B, Freeth E, Mohajeri A, Ramanathan K, Bennett M, Walia J, Halperin L, Roston T, Lazarte J, Hegele RA, et al. Genetic testing in monogenic early-onset atrial fibrillation. Eur J Hum Genet. 2023;31(7):769-775.
- Yoneda ZT, Anderson KC, Quintana JA, O’Neill MJ, Sims RA, Glazer AM, Shaffer CM, Crawford DM, Stricker T, Ye F, et al. Early-Onset Atrial Fibrillation and the Prevalence of Rare Variants in Cardiomyopathy and Arrhythmia Genes. JAMA Cardiol. 2021;6(12):1371-1379.
- Hateley S, Lopez-Izquierdo A, Jou CJ, Cho S, Schraiber JG, Song S, Maguire CT, Torres N, Riedel M, Bowles NE, et al. The history and geographic distribution of a KCNQ1 atrial fibrillation risk allele. Nat Commun. 2021;12(1):6442.
- Lampert R, Chung EH, Ackerman MJ, Arroyo AR, Darden D, Deo R, Dolan J, Etheridge SP, Gray BR, Harmon KG, et al. 2024 HRS expert consensus statement on arrhythmias in the athlete: Evaluation, treatment, and return to play. Heart Rhythm. 2024:S1547-5271(24)02560-8.
- https://www.wada-ama.org/sites/default/files/2022-01/2022list_final_en_0.pdf. Accessed on 13th August, 2024.
- Lau DH, Stiles MK, John B, Shashidhar, Young GD, Sanders P. Atrial fibrillation and anabolic steroid abuse. Int J Cardiol. 2007;117(2):e86-7.
- Seifert SM, Schaechter JL, Hershorin ER, Lipshultz SE. Health effects of energy drinks on children, adolescents, and young adults. Pediatrics. 2011;127(3):511-28.
- Di Rocco JR, During A, Morelli PJ, Heyden M, Biancaniello TA. Atrial fibrillation in healthy adolescents after highly caffeinated beverage consumption: two case reports. J Med Case Rep. 2011;5:18.
- Steinke L, Lanfear DE, Dhanapal V, Kalus JS. Effect of “energy drink” consumption on hemodynamic and electrocardiographic parameters in healthy young adults. Ann Pharmacother. 2009;43(4):596-602.
- Elliott AD, Mahajan R, Lau DH, Sanders P. Atrial Fibrillation in Endurance Athletes: From Mechanism to Management. Cardiol Clin. 2016;34(4):567-578.
- Nattel S, Harada M. Atrial remodeling and atrial fibrillation: recent advances and translational perspectives. J Am Coll Cardiol. 2014;63(22):2335-45.
- La Gerche A, Inder WJ, Roberts TJ, Brosnan MJ, Heidbuchel H, Prior DL. Relationship between Inflammatory Cytokines and Indices of Cardiac Dysfunction following Intense Endurance Exercise. PLoS One. 2015;10(6):e0130031.
- Sugama K, Suzuki K, Yoshitani K, Shiraishi K, Miura S, Yoshioka H, Mori Y, Kometani T. Changes of thioredoxin, oxidative stress markers, inflammation and muscle/renal damage following intensive endurance exercise. Exerc Immunol Rev. 2015;21:130-42.
- Aschar-Sobbi R, Izaddoustdar F, Korogyi AS, Wang Q, Farman GP, Yang F, Yang W, Dorian D, Simpson JA, Tuomi JM, et al. Increased atrial arrhythmia susceptibility induced by intense endurance exercise in mice requires TNFα. Nat Commun. 2015;6:6018.
- Baggish, AL. Mechanisms underlying the cardiac benefits of exercise: Still running in the dark. Trends Cardiovasc Med. 2015;25(6):537-9.
- Pelliccia A, Maron BJ, Di Paolo FM, Biffi A, Quattrini FM, Pisicchio C, Roselli A, Caselli S, Culasso F. Prevalence and clinical significance of left atrial remodeling in competitive athletes. J Am Coll Cardiol. 2005;46(4):690-6.
- Turagam MK, Flaker GC, Velagapudi P, Vadali S, Alpert MA. Atrial Fibrillation In Athletes: Pathophysiology, Clinical Presentation, Evaluation and Management. J Atr Fibrillation. 2015;8(4):1309.
- Mont L, Elosua R, Brugada J. Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace. 2009;11(1):11-7.
- Lindsay MM, Dunn FG. Biochemical evidence of myocardial fibrosis in veteran endurance athletes. Br J Sports Med. 2007;41(7):447-52.
- Wilson M, O’Hanlon R, Prasad S, Deighan A, Macmillan P, Oxborough D, Godfrey R, Smith G, Maceira A, Sharma S, et al. Diverse patterns of myocardial fibrosis in lifelong, veteran endurance athletes. J Appl Physiol (1985). 2011;110(6):1622-6.
- Swanson, DR. Atrial fibrillation in athletes: implicit literature-based connections suggest that overtraining and subsequent inflammation may be a contributory mechanism. Med Hypotheses. 2006;66(6):1085-92.
- Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation. 2002;105(23):2753-9.
- Grimsmo J, Grundvold I, Maehlum S, Arnesen H. High prevalence of atrial fibrillation in long-term endurance cross-country skiers: echocardiographic findings and possible predictors--a 28-30 years follow-up study. Eur J Cardiovasc Prev Rehabil. 2010;17(1):100-5.
- Carpenter A, Frontera A, Bond R, Duncan E, Thomas G. Vagal atrial fibrillation: What is it and should we treat it? Int J Cardiol. 2015;201:415-21.
- Grundvold I, Skretteberg PT, Liestøl K, Erikssen G, Engeseth K, Gjesdal K, Kjeldsen SE, Arnesen H, Erikssen J, Bodegard J. Low heart rates predict incident atrial fibrillation in healthy middle-aged men. Circ Arrhythm Electrophysiol. 2013;6(4):726-31.
- Swanson, DR. Running, esophageal acid reflux, and atrial fibrillation: a chain of events linked by evidence from separate medical literatures. Med Hypotheses. 2008;71(2):178-85.
- Collings KL, Pierce Pratt F, Rodriguez-Stanley S, Bemben M, Miner PB. Esophageal reflux in conditioned runners, cyclists, and weightlifters. Med Sci Sports Exerc. 2003;35(5):730-5.
- Soffer EE, Merchant RK, Duethman G, Launspach J, Gisolfi C, Adrian TE. Effect of graded exercise on esophageal motility and gastroesophageal reflux in trained athletes. Dig Dis Sci. 1993;38(2):220-4.
- Choi SC, Choi SJ, Kim JA, Kim TH, Nah YH, Yazaki E, Evans DF. The role of gastrointestinal endoscopy in long-distance runners with gastrointestinal symptoms. Eur J Gastroenterol Hepatol. 2001;13(9):1089-94.
- Kunz JS, Hemann B, Edwin Atwood J, Jackson J, Wu T, Hamm C. Is there a link between gastroesophageal reflux disease and atrial fibrillation? Clin Cardiol. 2009;32(10):584-7.
- Proietti M, Boriani G, Laroche C, Diemberger I, Popescu MI, Rasmussen LH, Sinagra G, Dan GA, Maggioni AP, Tavazzi L, et al. Self-reported physical activity and major adverse events in patients with atrial fibrillation: a report from the EURObservational Research Programme Pilot Survey on Atrial Fibrillation (EORP-AF) General Registry. Europace. 2017;19(4):535-543.
- Nortamo S, Ukkola O, Lepojärvi S, Kenttä T, Kiviniemi A, Junttila J, Huikuri H, Perkiömäki J. Association of sST2 and hs-CRP levels with new-onset atrial fibrillation in coronary artery disease. Int J Cardiol. 2017;248:173-178.
- Fashanu OE, Norby FL, Aguilar D, Ballantyne CM, Hoogeveen RC, Chen LY, Soliman EZ, Alonso A, Folsom AR. Galectin-3 and incidence of atrial fibrillation: The Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2017;192:19-25.
- McManus DD, Tanriverdi K, Lin H, Esa N, Kinno M, Mandapati D, Tam S, Okike ON, Ellinor PT, Keaney JF Jr, et al. Plasma microRNAs are associated with atrial fibrillation and change after catheter ablation (the miRhythm study). Heart Rhythm. 2015;12(1):3-10.
- Hättasch R, Spethmann S, de Boer RA, Ruifrok WP, Schattke S, Wagner M, Schroeckh S, Durmus T, Schimke I, Sanad W, et al. Galectin-3 increase in endurance athletes. Eur J Prev Cardiol. 2014;21(10):1192-9.
- Roca E, Nescolarde L, Lupón J, Barallat J, Januzzi JL, Liu P, Cruz Pastor M, Bayes-Genis A. The Dynamics of Cardiovascular Biomarkers in non-Elite Marathon Runners. J Cardiovasc Transl Res. 2017;10(2):206-208.
- Baggish AL, Hale A, Weiner RB, Lewis GD, Systrom D, Wang F, Wang TJ, Chan SY. Dynamic regulation of circulating microRNA during acute exhaustive exercise and sustained aerobic exercise training. J Physiol. 2011;589(Pt 16):3983-94.
- Luo N, Merrill P, Parikh KS, Whellan DJ, Piña IL, Fiuzat M, Kraus WE, Kitzman DW, Keteyian SJ, O’Connor CM, et al. Exercise Training in Patients With Chronic Heart Failure and Atrial Fibrillation. J Am Coll Cardiol. 2017;69(13):1683-1691.
- Rienstra M, Hobbelt AH, Alings M, Tijssen JGP, Smit MD, Brügemann J, Geelhoed B, Tieleman RG, Hillege HL, Tukkie R, et al. Targeted therapy of underlying conditions improves sinus rhythm maintenance in patients with persistent atrial fibrillation: results of the RACE 3 trial. Eur Heart J. 2018;39(32):2987-2996.
- Malmo V, Nes BM, Amundsen BH, Tjonna AE, Stoylen A, Rossvoll O, Wisloff U, Loennechen JP. Aerobic Interval Training Reduces the Burden of Atrial Fibrillation in the Short Term: A Randomized Trial. Circulation. 2016;133(5):466-73.
- Kemi OJ, Wisløff U. Mechanisms of exercise-induced improvements in the contractile apparatus of the mammalian myocardium. Acta Physiol (Oxf). 2010;199(4):425-39.
- Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, Alasady M, Hanley L, Antic NA, McEvoy RD, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol. 2014;64(21):2222-31.
- Elliott AD, Verdicchio CV, Mahajan R, Middeldorp ME, Gallagher C, Mishima RS, Hendriks JML, Pathak RK, Thomas G, Lau DH, et al. An Exercise and Physical Activity Program in Patients With Atrial Fibrillation: The ACTIVE-AF Randomized Controlled Trial. JACC Clin Electrophysiol. 2023;9(4):455-465.
- AbuElkhair A, Boidin M, Buckley BJR, Lane DA, Williams NH, Thijssen D, Lip GYH, Barraclough DL. Effects of different exercise types on quality of life for patients with atrial fibrillation: a systematic review and meta-analysis. J Cardiovasc Med (Hagerstown). 2023;24(2):87-95.
- Zipes DP, Link MS, Ackerman MJ, Kovacs RJ, Myerburg RJ, Estes NAM 3rd. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 9: Arrhythmias and Conduction Defects: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2015;66(21):2412-2423.
- Alboni P, Botto GL, Baldi N, Luzi M, Russo V, Gianfranchi L, Marchi P, Calzolari M, Solano A, Baroffio R, et al. Outpatient treatment of recent-onset atrial fibrillation with the “pill-in-the-pocket” approach. N Engl J Med. 2004;351(23):2384-91.
- Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50(5):e1-e88.
- Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018;39(16):1330-1393.
- Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275-e444.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




