1. Introduction
Dysphagia in older people is a well-known risk factor for aspiration pneumonia and poor quality of life [
1]. Dysphagia is not only caused by neurological diseases such as stroke and neurodegenerative diseases, but also by sarcopenia in older people [
2,
3]. Dysphagia caused by sarcopenia has recently been defined as sarcopenic dysphagia, which is swallowing dysfunction due to sarcopenia in both appendicular skeletal muscles and swallowing-related muscles [
3]. Sarcopenia is now widely recognized as a common health problem, with a systematic review suggesting that approximately 10% of community-dwelling older people have sarcopenia [
4]. Similarly, a recent meta-analysis of dysphagia in older people suggested that approximately 20% of community-dwelling older people may have dysphagia [
5]. Therefore, dysphagia in older people associated with sarcopenia should be recognized by health professionals as a common health problem that requires care and prevention.
Assessment of swallowing-related muscle function is essential for the management and prevention of sarcopenic dysphagia. The published diagnostic criteria for sarcopenic dysphagia [
3] and oral hypofunction [
6] have proposed tongue pressure measurement to assess swallowing-related muscle strength. Tongue pressure measurement has been reported to be associated with sarcopenia [
7], appendicular skeletal muscle mass and strength [
8,
9], and geniohyoid and pharyngeal muscle mass [
10]. It has also been suggested that middle-aged and older people with aspiration pneumonia may have reduced tongue pressure [
11]. Therefore, it may be reasonable to assess tongue pressure as an index of swallowing-related muscle strength. However, tongue pressure measures the strength of the tongue, not the strength of the suprahyoid muscle group directly, which is involved in opening the pharyngoesophageal segment [
12] and may contribute to improved swallowing function [
13].
Chin tuck against resistance exercise has recently been reported as an effective therapeutic exercise for dysphagia rehabilitation [
14]. The chin tuck maneuver involves tucking the chin toward the manubrium sterni, and adding isometric or isokinetic resistance to the chin tuck maneuver has been reported to increase suprahyoid muscle activation [
15]. In addition, previous studies of the chin tuck against resistance exercise have reported improvements in tongue pressure [
16] and swallowing function [
14]. Therefore, it is hypothesized that measuring the strength of the chin tuck maneuver (chin tuck strength) is an effective and reasonable assessment of swallowing-related muscle strength. However, no previous study could be found that investigated chin tuck strength, and a method to measure the strength of the chin tuck maneuver has not been established. We developed a method to measure chin tuck strength and examined the reliability and validity of chin tuck strength measurement in community-dwelling older adults.
2. Materials and Methods
2.1. Participants
The participants were 233 community-dwelling older adults aged ≥65 years. They were volunteers recruited through local newspapers in Sagamihara City, Japan. Recruitment and data collection took place between August 2023 and February 2024. Inclusion criteria were as follows: age ≥65 years, independence in activities of daily living (ADL), and without suspected dysphagia. Institutionalized older adults, those younger than 65 years, those with disability in ADL, those with a history of stroke, those with Parkinson’s disease, those with cervical myelopathy and cervical disc herniation, and those with neck pain were excluded from this study. Independence in ADL was confirmed by the certification of care needs levels for long-term care insurance in Japan [
17], and those with the presence of any care needs level were excluded. Suspected dysphagia was confirmed using the Functional Oral Intake Scale (FOIS) [
18], and those with an FOIS level less than 7 were excluded. The presence of a history of stroke or Parkinson’s disease was confirmed by a self-administered questionnaire. The presence of cervical myelopathy, cervical disc herniation, and neck pain was confirmed in a face-to-face interview by trained researchers.
This study was approved by the institutional review board of the School of Allied Health Sciences at Kitasato University (Approval No. 2023-008). Written, informed consent was obtained from all participants.
2.2. Device for measuring chin tuck strength
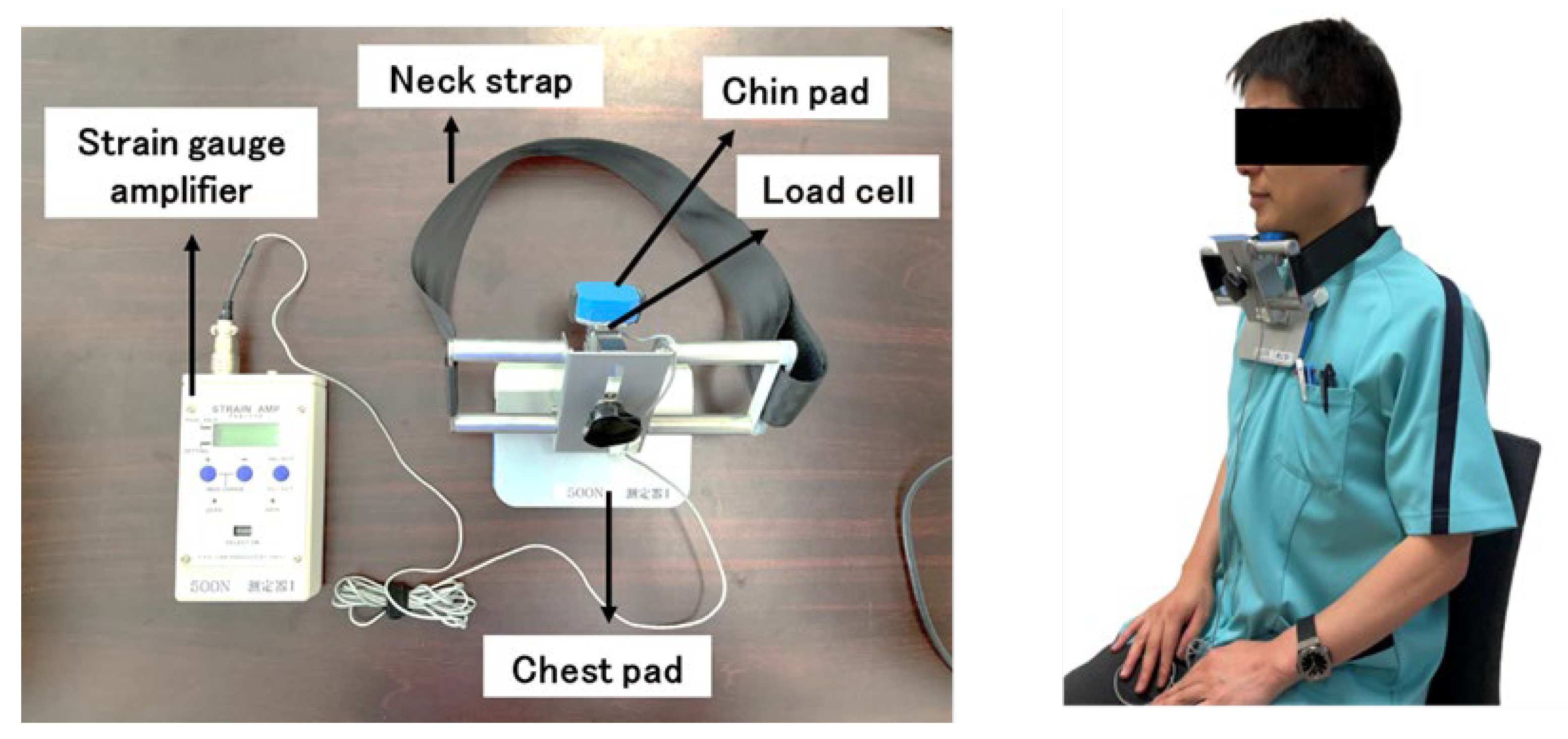
The device shown on the left side of
Figure 1 was developed in the present study to measure chin tuck strength. It consisted of a strain gauge amplifier (T.K.K. 1268, SANKA Co., Ltd., Niigata, Japan) and the instrument for holding the neck with chin pad, chest pad, and neck strap, and the load cell (TU-MXR2(T)500N-G3, TEAC Co., Ltd., Tokyo, Japan) was embedded under the chin pad of the instrument. Participants attached the instrument to the front of their neck with the chin pad and chest pad positioned at the chin and sternum, respectively, while sitting on a chair with a backrest. It was secured with the neck strap at the neutral position of the neck (flexion and extension at zero degrees) (
Figure 1, right).
Participants were asked to rest their back against the backrest of the chair and tuck their chin toward the manubrium sterni with a maximal isometric contraction for 5 seconds. The maximum force generated during chin tuck was recorded as chin tuck strength using the measuring device. Chin tuck strength was measured two consecutive times with an appropriate rest period. Then, the two measurements were used for reproducibility analysis, and the mean of the two measurements was used for validity analysis.
2.3. Swallowing-Related Muscle Function
Maximum tongue pressure (MTP) was measured as an index of swallowing-related muscle strength, and oral diadochokinesis (ODK) was measured as an index of lip-tongue motor function [
6]. MTP data were collected using a tongue pressure measuring device with a disposable probe inserted into the oral cavity on the anterior side of the tongue (TPM-01, JMS Co., Ltd., Hiroshima, Japan) [
19], and measurements were taken three consecutive times with appropriate rest periods. The mean of the three measurements was used for further statistical analysis. In addition, tongue pressure less than 30 kPa was defined as low tongue pressure according to the diagnostic criteria for oral hypofunction [
7]. ODK was assessed by three different sounds (i.e.
, “pa”, “ta”, “ka”) using a device (T.K.K.3351, SANKA Co., Ltd., Niigata, Japan), and the number of sounds produced per second for each sound was recorded.
2.4. Muscle Strength of the Upper and Lower Limbs, Skeletal Muscle Mass, and Physical Performance
Muscle strength of the upper and lower limbs was measured by grip strength and knee extension strength, respectively. Grip strength was measured using a Smedley-type dynamometer (T.K.K.5401, SANKA Co., Ltd.) with the dominant hand in a standing position. Knee extension strength was measured using a handheld dynamometer (μ-Tas F-1; Anima Inc., Tokyo, Japan) on the right side in a sitting position with the knee and hip joint flexed at 90 degrees.
Appendicular skeletal muscle mass was measured using a bioimpedance analysis method (InBody 430; InBody Japan Inc., Tokyo, Japan). Appendicular skeletal muscle mass was divided by the square of the body height, and the appendicular skeletal muscle mass index (SMI) was calculated and used for further statistical analysis.
For the timed up and go test (TUGT), participants were asked to stand up from a chair without hand support, walk 3 m as quickly as possible, turn around, walk back, and then sit down again [
20], and the time required to complete this task was measured.
2.5. Covariates
Body mass index (BMI), number of prescribed medications, and number of comorbidities were included as covariates. Height and weight were measured using a height rod and weight scale, respectively, and BMI was calculated. The number of prescribed medications and number of comorbidities were confirmed using a self-administered questionnaire. For the number of prescribed medications, participants were asked about the number of types of oral medications prescribed by the physician. For the number of comorbidities, they were asked if a doctor had diagnosed any of the following diseases: hypertension, diabetes mellitus, cancer, chronic lung disease, heart attack, congestive heart failure, angina, asthma, arthritis, stroke, Parkinson’s disease, and kidney disease. Those who responded that they had stroke or Parkinson’s disease were excluded from this study. The number of other diseases they had was counted and used for analysis.
2.6. Statistical Analysis
To verify reliability, the reproducibility of the two measurements of chin tuck strength was assessed by the intraclass correlation coefficient (ICC) with a two-way mixed model based on single measurement. An ICC of 0.75 or more was then defined as good reliability [
21]. For validity, the relationships between chin tuck strength and MTP, ODK, grip strength, knee extension strength, and SMI were examined using Pearson’s product-moment correlation coefficient and multiple regression analysis with chin tuck strength as the dependent variable. Statistical analysis was performed using R Statistical Analysis Software Version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria), with significance set at 5%.
3. Results
The basic characteristics of the participants and the descriptive statistics of the variables measured in this study are presented in
Table 1.
For the reproducibility of chin tuck strength measurements, the ICC was 0.890 (95% confidence interval [CI]: 0.826-0.926) for the total sample, 0.817 (95%CI: 0.726-0.879) for males, and 0.865 (95%CI: 0.704-0.927) for females.
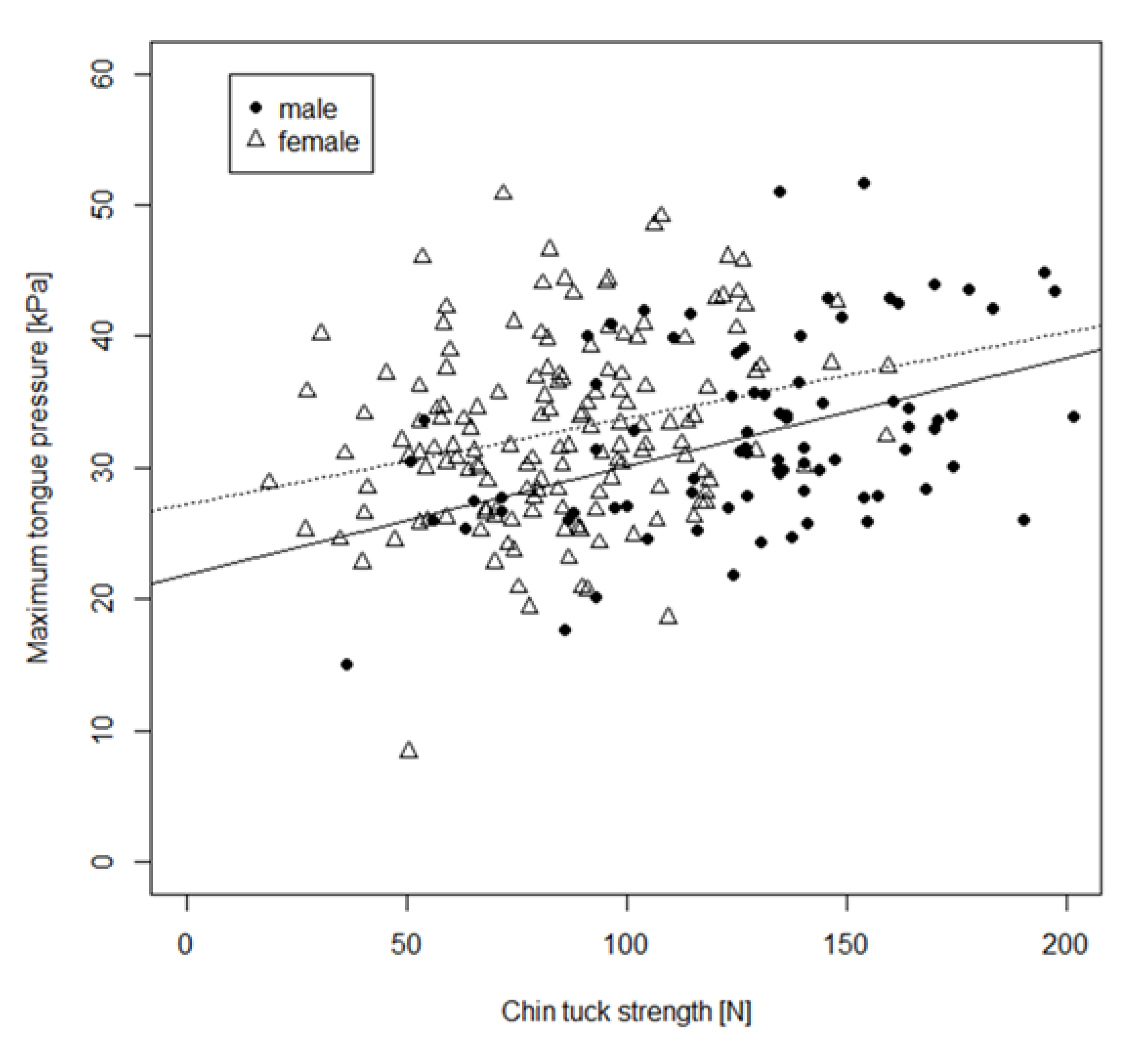
The results of the correlation analysis between chin tuck strength and swallowing-related muscle functions and upper and lower limb muscle functions are presented in
Table 2. Furthermore, for the relationship between chin tuck strength and MTP, which is an index of swallowing-related muscle strength, the scatter plots for male and female participants are shown in
Figure 2. Chin tuck strength was significantly related to MTP, grip strength, knee extension strength, SMI, and TUGT. Furthermore, these relationships remained significant when the analysis was stratified by sex. For MTP, even when MTP data were treated as categorical variables (low tongue pressure or normal tongue pressure), subjects with low tongue pressure had significantly weaker chin tuck strength than those with normal tongue pressure (
Figure 3). However, significant correlations between chin tuck strength and ODK were not found, except for the correlation between chin tuck strength and ODK of “ka” in females. For the covariates, chin tuck strength was significantly related to BMI in the total sample (r=0.257, p<0.001), in males (r=0.263, p<0.001), and in females (r=0.215, p<0.001). In addition, in females only, significant relationships were found between chin tuck strength and age (r=-0.21, p=0.01) and number of prescribed medications (r=0.16, p=0.046). However, these correlations were weak overall.
Finally, multiple regression analysis adjusted for age and sex was performed to determine the associations of chin tuck strength with MTP, SMI, and upper and lower extremity muscle function. Chin tuck strength was significantly associated with MTP, grip strength, knee extension strength, and TUGT (
Table 3).
4. Discussion
Recently, it has been reported that chin tuck against resistance exercise is effective for dysphagia rehabilitation [
14]. Therefore, measuring the muscle strength of the chin tuck maneuver may be useful as an indicator of muscle strength of swallowing-related muscles, but the method for measuring chin tuck strength has not been established. In this study, a method for measuring chin tuck strength was developed, and the reliability and validity of chin tuck strength measurement were examined in community-dwelling older adults.
In terms of reliability, the measurement reproducibility of chin tuck strength obtained in the present study was examined using the ICC, and it was found to range from 0.82 to 0.89. Therefore, this result showed that the chin tuck strength measured in the present study had good reliability [
21]. In previous studies, the ICC of tongue pressure was reported to be 0.96 to 0.99 [
22], and the ICC of physical function tests such as grip strength, knee extension strength, and TUG was 0.88 to 0.96 [
23]. Therefore, the method of measuring chin tuck strength in the present study appeared to have comparable results to the widely used swallowing-related muscle strength and physical function tests.
Regarding the validity of the chin tuck strength measurement, chin tuck strength in the present study was significantly associated with MTP. Since MTP has been reported to be associated with muscle thickness of the geniohyoid muscle [
10], it is used clinically as an index of swallowing-related muscle strength. Furthermore, MTP has also been reported to be associated with whole-body sarcopenia [
7], appendicular skeletal muscle mass [
8], and grip strength [
9], suggesting that MTP reflects not only swallowing-related muscle strength, but also whole-body muscle mass and strength. The finding that chin tuck strength was associated with MTP suggested that chin tuck strength has validity as an index of swallowing-related muscle strength. In particular, the chin tuck was previously reported to increase muscle activity of the suprahyoid muscles [
15]. Therefore, it is assumed that chin tuck strength in the present study reflects the strength of the suprahyoid muscles involved in opening the pharyngoesophageal segment during swallowing [
12]. In addition, multiple regression analysis also showed that chin tuck strength was associated with MTP independently of physical functions such as grip strength, knee extension strength, and TUGT. This result indicated the robustness of the association between chin tuck strength and MTP. In addition, chin tuck strength was also associated with grip strength, knee extension strength, TUGT, and SMI. Therefore, chin tuck strength was shown to be related to whole body muscle functions and skeletal muscle mass, which was suggested to be a characteristic similar to tongue pressure. However, chin tuck strength was not related to ODK. ODK is generally an assessment of the frequency and consistency of repetitive movements of the oral articulators [
24], rather than an indicator of muscle strength. Because chin tuck strength was considered an index of swallowing-related muscle strength, it may not be related to ODK, which is an index of oral articulator function.
As for the assessment of suprahyoid muscle function, measurement of muscle thickness by ultrasound has been reported [
10]. However, measurement of muscle thickness by ultrasound generally requires skill of the examiner, and it cannot directly assess the strength of the suprahyoid muscle. The assessment of chin tuck strength in the present study may be more convenient than suprahyoid muscle assessment by ultrasound. In addition, we believe that the results of the present study, which demonstrated the reliability and validity of chin tuck strength measurement as an assessment of suprahyoid muscle strength, are novel.
The present study had several limitations that should be considered when interpreting the results. First, the reliability of chin tuck strength measurement was only examined for the reproducibility of two measurements. Therefore, the examination of reliability may not be sufficient. Further investigation of reliability, such as inter-rater reliability, is required. Second, the chin tuck strength measured in this study is assumed to assess suprahyoid muscle strength. However, muscle activity and contraction were not directly assessed during chin tuck strength measurement in this study, and assessment of muscle activity and contraction during chin tuck strength measurement using surface electromyography is needed. Third, participants in this study were recruited from community-dwelling older adults who did not have dysphagia. Therefore, the association between chin tuck strength and dysphagia could not be clearly demonstrated, and further studies are needed.
5. Conclusions
This study developed a method for measuring the strength of the chin tuck maneuver in older adults. The chin tuck strength obtained in this study had good reliability. In addition, chin tuck strength was associated with tongue pressure, whole-body muscle functions, and skeletal muscle mass. Therefore, chin tuck strength had validity as an index of swallowing-related muscle strength. Further studies are needed, but the chin tuck strength measurement method developed in this study may be a simple and useful assessment of swallowing-related muscle strength of older adults.
6. Patents
Dr. Kamide and Dr. Murakami are the inventors of the chin tuck strength measuring device (Patent No. 7495133), which is registered with the Japan Patent Office.
Author Contributions
NK and TM contributed to the study conception and design, acquisition of subjects and data, analysis and interpretation of data, and preparation of the manuscript. MA, TS, WH, and MS contributed to acquisition of subjects and data, and interpretation of data. The first draft of the manuscript was written by NK, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive a specific grant from any agency in public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by the institutional review board of the School of Allied Health Sciences at Kitasato University (Approval No. 2023-008).
Informed Consent Statement
Written, informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Conflicts of Interest
In this study, the development of the chin tuck strength measuring device was supported in part by SANKA Co., Ltd. The company had no role in the design of the study; in the collection, analysis, or interpretation of the data; in the writing of the manuscript; or in the decision to publish the results. Dr. Kamide and Dr. Murakami are the inventors of the chin tuck strength measuring device (Patent No. 7495133), which is registered with the Japan Patent Office.
References
- Madhavan, A. Preclinical dysphagia in community dwelling older adults: What should we look for?. Am. J. Speech. Lang. Pathol. 2020, 30; 833-843. [CrossRef]
- Kuroda, Y.; Kuroda, R. Relationship between thinness and swallowing function in Japanese older adults: Implications for sarcopenic dysphagia. J. Am. Geriatr. Soc. 2012, 60, 1785-1786. [CrossRef]
- Fujishima, I.; Fujiu-Kurachi, M.; Arai, H.; Hyodo, M.; Kagaya, H.; Maeda, K.; Mori, T.; Nishioka, S.; Oshima, F.; Ogawa, S.; et al. Sarcopenia and dysphagia: Position paper by four professional organizations. Geriatr. Gerontol. Int. 2019, 19, 91-97. [CrossRef]
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J. Diabetes. Metab. Disord. 2017, 16, 21. [CrossRef]
- Rech, R.S.; de Goulart, B.N.G.; Dos Santos, K.W.; Marcolino, M.A.Z.; Hilgert, J.B. Frequency and associated factors for swallowing impairment in community-dwelling older persons: a systematic review and meta-analysis. Aging. Clin. Exp. Res. 2022, 34, 2945-2961. [CrossRef]
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology. 2018, 35, 317-324. [CrossRef]
- Maeda, K.; Akagi, J. Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia. 2015, 30, 80-87. [CrossRef]
- Murakami, T.; Kamide, N.; Ando, M.; Hata, W.; Sakamoto, M. Association between tongue pressure and skeletal muscle mass and muscle function in community-dwelling older people without sarcopenia. Eur. Geriatr. Med. 2022, 13, 649-653. [CrossRef]
- Buehring, B.; Hind, J.; Fidler, E.; Krueger, D.; Binkley, N.; Robbins, J. Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J. Am. Geriatr. Soc. 2013, 61, 418-422. [CrossRef]
- Nakao, Y.; Uchiyama, Y.; Honda, K.; Yamashita, T.; Saito, S.; Domen, K. Age-related composition changes in swallowing-related muscles: a Dixon MRI study. Aging. Clin. Exp. Res. 2021,33, 3205-3213. [CrossRef]
- Chen, Y.C.; Ku, E.N.; Lin, C.W.; Tsai, P.F.; Wang, J.L.; Yen, Y.F.; Ko, N.Y.; Ko, W.C.; Lee, N.Y. Tongue pressure during swallowing is an independent risk factor for aspiration pneumonia in middle-aged and older hospitalized patients: An observational study. Geriatr. Gerontol. Int. 2024, 24, 351-357. [CrossRef]
- Singh, S.; Hamdy, S. The upper oesophageal sphincter. Neurogastroenterol. Motil. 2005, 17(Suppl.1), 3-12. [CrossRef]
- Shaker, R.; Easterling, C.; Kern, M.; Nitschke, T.; Massey, B.; Daniels, S.; Grande, B.; Kazandjian, M.; Dikeman, K. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002, 122,1314-1321. [CrossRef]
- Park, J.S.; Hwang, N.K. Chin tuck against resistance exercise for dysphagia rehabilitation: a systematic review. J. Oral. Rehabil. 2021, 48, 968-977. [CrossRef]
- Yoon, W.L.; Khoo, J.K.P.; Richard Liow, S.J. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a shaker-type exercise. Dysphagia. 2014, 29, 243-248. [CrossRef]
- Kilinç, H.E.; Arslan, S.S.; Demir, N.; Karaduman. The effects of different exercise training on suprahyoid muscle activation, tongue pressure force and dysphagia limit in healthy subjects. Dysphagia. 2020, 35, 717-724. [CrossRef]
- Tsutsui, T.; Muramatsu, N. Care-needs certification in the long-term care insurance system of Japan. J. Am. Geriatr. Soc. 2005, 53, 522–527. [CrossRef]
- Crary, M.A.; Mann, G.D.; Groher, M.E. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch. Phys. Med. Rehabil. 2005,86, 1516-1520. [CrossRef]
- Yoshikawa, M.; Yoshida, M.; Tsuga, K.; Akagawa, Y.; Groher, M.E. Comparison of three types of tongue pressure measurement devices. Dysphagia. 2011, 26, 232-237. [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys. Ther. 2000, 80, 896–903. [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2017, 15, 155-163. [CrossRef]
- Takahashi, M.; Koide, K.; Suzuki, H.; Satoh, Y.; Iwasaki, S. Evaluation of reliability of perioral muscle pressure measurements using a newly developed device with a lip piece. Acta. Bioeng. Biomech. 2016, 18, 145-153. [CrossRef]
- Suzuki, Y.; Kamide, N.; Kitai, Y.; Ando, M.; Sato, H.; Shiba, Y.; Sakamoto, M. Absolute reliability of measurements of muscle strength and physical performance measures in older people with high functional capacities. Eur. Geriatr. Med. 2019, 10, 733-740. [CrossRef]
- Wang, Y.T.; Kent, R.D.; Duffy, J.R.; Thomas, J.E. Analysis of diadochokinesis in ataxic dysarthria using the motor speech profile program. Folia. Phoniatr. Logop. 2009, 61, 1–11. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).