Submitted:
21 August 2024
Posted:
22 August 2024
You are already at the latest version
Abstract
Keywords:
Introduction
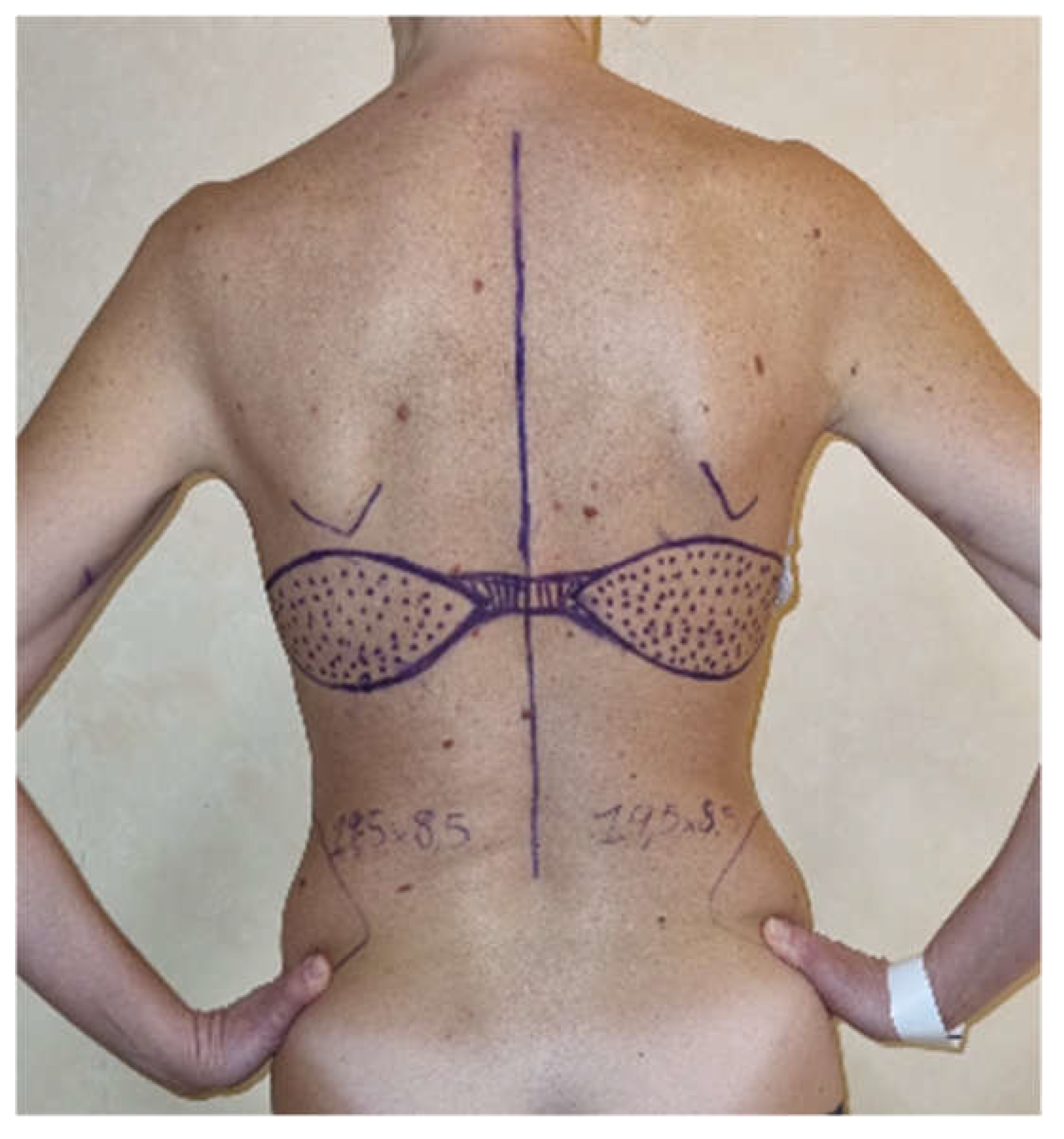
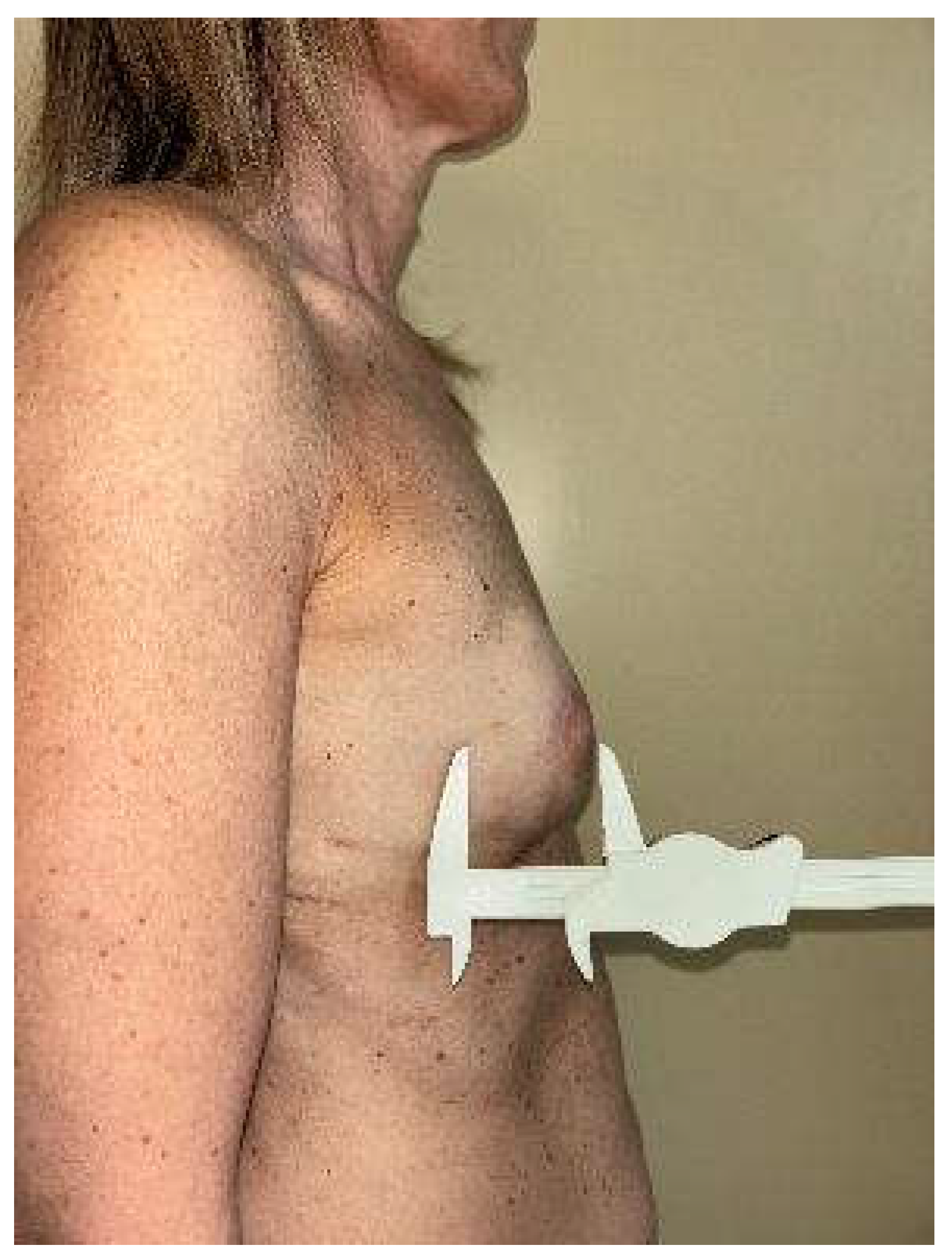
Patients and Methods
Study Endpoints
Statistical Analysis
Results
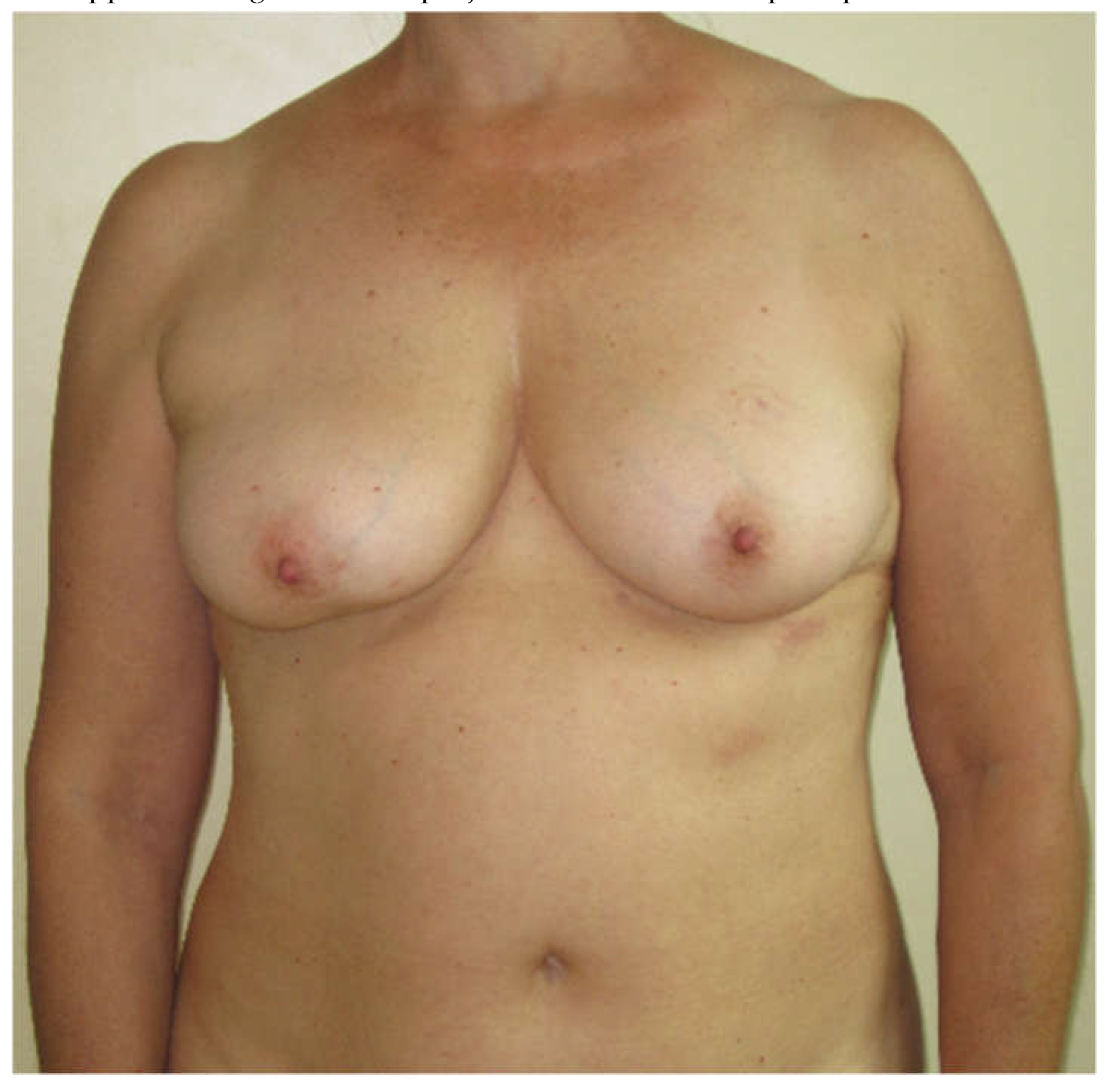
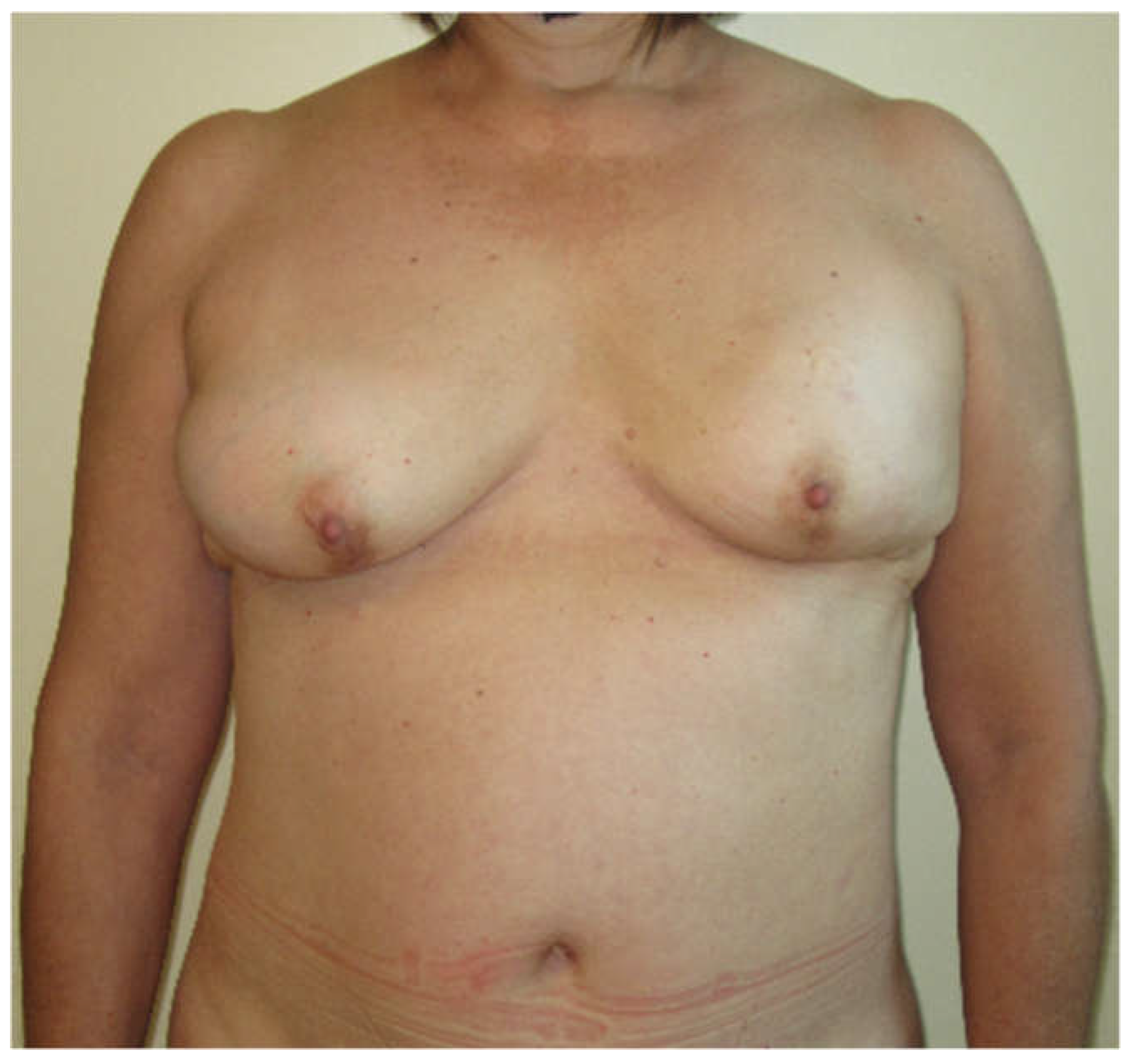
Aesthetic Outcome
Discussion
Conclusion
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest disclosure statement
References
- Demiri EC, Tsimponis A, Pagkalos A, et al. Fat-Augmented Latissimus Dorsi versus Deep Inferior Epigastric Perforator Flap: Comparative Study in Delayed Autologous Breast Reconstruction. J Reconstr Microsurg. 2021;37(3):208-215. [CrossRef]
- Longo, B., D’orsi, G., Orlando, G., Giacalone, M. and Cervelli, V. 2022. Recurrent dermatofibrosarcoma protuberans of the clavicular region: radical excision and reconstruction with Latissimus Dorsi myocutaneous flap. Plastic Reconstructive and Regenerative Surgery. 1, 1 (Jul. 2022), 14–19. [CrossRef]
- Longo B, D’Orsi G, Vanni G, Gagliano E, Buonomo CO, Cervelli V. Fat-Augmented Latissimus Dorsi Flap for Secondary Breast Reconstruction in Small to Medium-Sized Irradiated Breasts. Plast Reconstr Surg. 2023;152(6):1165-1173. [CrossRef]
- Herbst, I. and Saltvig, I. 2022. Cannula tip breakage inside adipose tissue during liposuction – a rare case report. Plastic Reconstructive and Regenerative Surgery. 1, 2 (Nov. 2022), 76–78. [CrossRef]
- Longo B, D’Orsi G, Farcomeni A, et al. The FALD-V: A predictive formula for preoperative volume assessment of adipose tissue transplantation in FALD flap. J Plast Reconstr Aesthet Surg. 2024;90:25-34. [CrossRef]
- Longo B, D’Orsi G, Giacalone M, et al. The Ergonomic FALD Flap for One-stage Total Breast Reconstruction. Plast Reconstr Surg Glob Open. 2023;11(9):e5262. Published 2023 Sep 18. [CrossRef]
- Longo B, D’Orsi G, Farcomeni A, et al. The LD-V: An innovative formula for latissimus dorsi flap volume assessment. J Plast Reconstr Aesthet Surg. Published online July 14, 2024. [CrossRef]
- Longo B, Timmermans FW, Farcomeni A, et al. Septum-Based Mammaplasties: Surgical Techniques and Evaluation of Nipple-Areola Sensibility. Aesthetic Plast Surg. 2020;44(3):689-697. [CrossRef]
- Mazzocchi, M., Sigorini, G., Cerciello, E. and Barberini, F. 2022. The use of Exashape (TM) Bioshield Pocket in prepectoral breast reconstruction: a preliminary experience. Plastic Reconstructive and Regenerative Surgery. 1, 2 (Nov. 2022), 51–57. [CrossRef]
- Longo B, Farcomeni A, Ferri G, Campanale A, Sorotos M, Santanelli F. The BREAST-V: a unifying predictive formula for volume assessment in small, medium, and large breasts. Plast Reconstr Surg. 2013;132(1):1e-7e. [CrossRef]
- Garbay JR, Rietjens M, Petit JY. Résultats esthétiques de la reconstruction mammaire après amputation pour cancer. A propos de 323 cas [Esthetic results of breast reconstruction after amputation for cancer. 323 cases]. J Gynecol Obstet Biol Reprod (Paris). 1992;21(4):405-412. [PubMed]
- Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg. 2008;60(5):568-572. [CrossRef]
- Harris JR, Levene MB, Svensson G, Hellman S. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979;5(2):257-261. [CrossRef]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educational and Psychological Measurement. 1960;20(1):37-46. [CrossRef]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [PubMed]
- Geraci M, Farcomeni A. Mid-quantile regression for discrete responses. Stat Methods Med Res. 2022;31(5):821-838. [CrossRef]
- Russo, A., Farcomeni, A., & Geraci, M. (2024). Mid-quantile regression for discrete panel data. Journal of Statistical Computation and Simulation, 1–18. [CrossRef]
- D’Orsi G, Giacalone M, Calicchia A, et al. BIA-ALCL and BIA-SCC: Updates on Clinical Features and Genetic Mutations for Latest Recommendations. Medicina (Kaunas). 2024;60(5):793. Published 2024 May 10. [CrossRef]
- Bottosso S, Sidoti GB, Vita L, et al. A Multi-Center Retrospective Observational Analysis of Three-Year Experience of Our Protocol for Prevention and Monitoring of Surgical Site Infections in Implant-Based Breast Reconstruction. Cancers (Basel). 2024;16(13):2439. Published 2024 Jul 2. [CrossRef]
- Liu L, Kim L, Teotia SS, Haddock NT. Long-term Implications of Cosmetic Breast Surgeries on Subsequent Breast Reconstruction. Aesthet Surg J. Published online June 24, 2024. [CrossRef]
- Longo B, Di Napoli A, Curigliano G, et al. Clinical recommendations for diagnosis and treatment according to current updated knowledge on BIA-ALCL. Breast. 2022;66:332-341. [CrossRef]
- Meier EL, Ulrich DJO, Hummelink S. Projected augmented reality in DIEP flap breast reconstruction: Projecting perforators on the skin using dynamic infrared thermography. J Plast Reconstr Aesthet Surg. 2024;94:83-90. [CrossRef]
- Longo B, Alberti FB, Pomahac B, et al. International consensus recommendations on face transplantation: A 2-step Delphi study. Am J Transplant. 2024;24(1):104-114. [CrossRef]
- Longo, B., Pistoia, A., D’Orsi, G., Gagliano, E., Vannucchi, L. and Cervelli, V. 2023. Lympho-diep flap transfer perfused by reverse-flow thoracodorsal artery: a case report. Plastic Reconstructive and Regenerative Surgery. 2, 1-2 (Oct. 2023), 20–24. [CrossRef]
- Longo B, D’Orsi G, La Padula S, et al. Narrow inferior-central septum-based pedicle: A safe technique to improve aesthetic outcomes in breast reduction. J Plast Reconstr Aesthet Surg. 2023;85:226-234. [CrossRef]
- Schonauer, F., Cavaliere, A., Pezone, G., D’Andrea, F., Longo, B., D’Orsi, G. and Cervelli, V. 2022. Thoraco-acromial artery perforator (TAAP) flap for reconstruction of a recurrent dermatofibrosarcoma protuberans of the clavicular region. Plastic Reconstructive and Regenerative Surgery. 1, 2 (Nov. 2022), 79–81. [CrossRef]
- D’Andrea, F., Errico, C., D’Andrea, L. and Zaffiro, A. 2023. The treatment of capsular contracture after breast surgery with implants using Capsulase®. Plastic Reconstructive and Regenerative Surgery. 2, 1-2 (Jul. 2023), 49–54. [CrossRef]
- Longo, B., Giacalone, M., Iundusi, R., D’Orsi, G., Gagliano, E., Vannucchi, L., Gargari, T., Tarantino, U. and Cervelli, V. 2023. Calcaneal hybrid reconstruction with femur head allograft enriched with bone marrow and ALT flap. Plastic Reconstructive and Regenerative Surgery. 2, 3 (Dec. 2023), 98–103. [CrossRef]
- Demiri EC, Dionyssiou DD, Tsimponis A, Goula CO, Pavlidis LC, Spyropoulou GA. Outcomes of Fat-Augmented Latissimus Dorsi (FALD) Flap Versus Implant-Based Latissimus Dorsi Flap for Delayed Post-radiation Breast Reconstruction. Aesthetic Plast Surg. 2018;42(3):692-701. [CrossRef]
- Economides JM, Song DH. Latissimus Dorsi and Immediate Fat Transfer (LIFT) for Complete Autologous Breast Reconstruction. Plast Reconstr Surg Glob Open. 2018;6(1):e1656. Published 2018 Jan 23. [CrossRef]
- Longo, B., Vannucchi, L., D’Orsi, G., Pistoia, A., Giacalone, M., Gagliano, E., Ventimiglia, M., Piscitelli, L., Di Giacomo, G., Vanni, G., Buonomo, O.C. and Cervelli, V. 2024. Shoulder function assessment after FALD flap breast reconstruction: comparing ultrasound results and patients’ self perception. Plastic Reconstructive and Regenerative Surgery. 3, 1 (May 2024), 9–16. [CrossRef]
- Otani N, Tomita K, Kuroda K, Taminato M, Kubo T. Effects of Temporary and Permanent Muscle Denervation on Fat Graft Retention in the Latissimus Dorsi Muscle: An Experimental Study in Rats. Aesthetic Plast Surg. 2022;46(4):1942-1949. [CrossRef]
- Escandón JM, Manrique OJ, Christiano JG, et al. Breast reconstruction with latissimus dorsi flap: a comprehensive review and case series. Ann Transl Med. 2023;11(10):355. [CrossRef]
- Taminato M, Tomita K, Nomori M, et al. Fat-augmented latissimus dorsi myocutaneous flap for total breast reconstruction: A report of 54 consecutive Asian cases. J Plast Reconstr Aesthet Surg. 2021;74(6):1213-1222. [CrossRef]
- Felici, N., Delle Femmine, P.F., Tosi, D., Ornelli, M., Mori, F.L.R., Turriziani, G. and Amadei, F. 2022. Common peroneal nerve injuries at the knee: outcomes of nerve repair. Plastic Reconstructive and Regenerative Surgery. 1, 1 (Jul. 2022), 6–13. [CrossRef]
- Messana, F., Lucchetta, G. , Bassetto, F. and Tiengo, C. 2024. Comparative evaluation of neurotubules and autologous nerve grafts for peripheral nerve repair: a retrospective case series. Plastic Reconstructive and Regenerative Surgery. 3, 1 (May 2024), 32–38. [CrossRef]

| Subscale | Category 0 | Category 1 | Category 2 |
| Volume of breast mound | Marked discrepancy relative to contralateral side | Mild discrepancy relative to contralateral side | Symmetrical volume |
| Shape of breast mound | Marked shape deformity | Mild shape deformity | Natural or symmetrical shape |
| Placement of breast mound | Marked displacement | Mild displacement | Symmetrical and aesthetic placement |
| IMF | Poorly defined/not identified | Defined but with asymmetry or lack of medial definition | Defined and symmetrical |
| Skin texture | Marked discrepancy relative to contralateral side | Mild discrepancy relative to contralateral side | Natural texture |
| Scar location | More noticeable | Less noticeable | Well hidden |
| Category 4 | Category 3 | Category 2 | Category 1 |
|---|---|---|---|
| Excellent: treated breast nearly identical to opposite breast | Good: treated breast only slightly different from opposite breast | Fair: treated breast clearly different from opposite breast but not seriously distorted | Poor: treated breast severely distorted |
| Group A | Group B | P value | |
|---|---|---|---|
| Flaps number | 32 | 31 | |
| Patients number | 23 | 25 | |
| Mean Age [y] | 50.5 (SD 9.51, range 33-70) | 50.42 (SD 9.66, range 40-80) | 0.796 |
| Mean BMI [kg/m2] | 23.93 (SD 3.58, range 18.9-35.8) | 23.08 (SD 2.69, range 18.6-30.4) | 0.495 |
| Smoking history | 6 (26.1 %) | 7 (28.0 %) | 0.882 |
| Laterality | Unilateral: 14 (60.9 %) Bilateral: 9 (39.1 %) |
Unilateral: 19 (76.0 %) Bilateral: 6 (24.0 %) |
0.259 |
| Timing of reconstruction | Immediate: 18 (56.2%) Delayed: 14 (43.8%) |
Immediate: 14 (45.2%) Delayed: 17 (54.8%) |
0.378 |
| Mastectomy type | SSM: 9 (28.1 %) NSM: 13 (40.6 %) Secondary: 10 (31.3 %) |
SSM: 4 (12.9 %) NSM: 11 (35.5 %) Secondary: 16 (51.6 %) |
0.177 |
| Preoperative breast volume [cc] | 298.74 (SD 99.69, range 120-520) | 288.75 (SD 78.81, range 130-430) | 0.549 |
| Preoperative Breast Projection [cm] | 6.38 (SD 0.74; range 5 - 8) | 6.42 (SD 0.77; range 5 - 8.5) | 0.408 |
| Preoperative Breast Width [cm] | 11.36 (SD 0.77; range 10 – 13) | 11.21 (SD 0.95; range 9.5 – 13) | 0.247 |
| Preoperative Breast Height [cm] | 11.13 (SD 1.16; range 9 – 13) | 11.37 (SD 1.01; range 9.5 – 13) | 0.147 |
| Group A | Group B | BminusA | CIlow | CIup | P value | |
|---|---|---|---|---|---|---|
| Flaps number | 32 | 31 | ||||
| Patients number | 23 | 25 | ||||
| Post-operative Breast Projection [cm] | 6.05 (SD 0.56; range 5.5 – 7.5) | 5.60 (SD 0.65; range 4.5 – 7) | -0.795 | -1.102 | -0.488 | < 0.0001 |
| Post-operative Breast Width [cm] | 11. 00 (SD 0.84; range 9.5 – 12.5) | 11.03 (SD 0.74; range 9.5 – 12) | 0.165 | -0.287 | 0.617 | 0.477 |
| Post-operative Breast Height [cm] | 10.63 (SD 1.22; range 8.5 – 13) | 10.47 (SD 0.96; range 9 – 13) | -0.281 | -0.916 | 0.355 | 0.390 |
| Group A | Group B | BminusA | CIlow | CIup | p-value | |
|---|---|---|---|---|---|---|
| Volume | 1.75 | 1.71 | -0.104 | -0.316 | 0.108 | 0.335 |
| Shape | 1.75 | 1.39 | -0.454 | -0.711 | -0.198 | 0.001 |
| Placement of breast mound | 1.72 | 1.52 | -0.232 | -0.476 | 0.011 | 0.061 |
| IMF | 1.69 | 1.61 | -0.107 | -0.341 | 0.128 | 0.374 |
| Skin texture | 1.69 | 1.58 | -0.093 | -0.333 | 0.146 | 0.445 |
| Scar | 1.66 | 1.51 | -0.171 | -0.417 | 0.075 | 0.174 |
| Total score | 10.25 | 9.32 | -0.500 | -3.853 | 2.353 | 0.752 |
| Global score | 3.44 | 3.06 | -0.509 | -0.858 | -0.160 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





