1. Introduction
The World Health Organization estimates premature births at 15 million worldwide, with varying rates from 5% to 18% of all births [
1,
2]. Premature infants require long-term hospitalization and neonatal follow-up (NFU) programs are essential to prevent serious health problems that may affect their later life [
3,
4,
5]. NFU programs play an integral and crucial role in long-term care of high-risk infants focusing on neurodevelopmental impairment [
6,
7,
8,
9], family counseling and support, optimal and continuous monitoring for health problems, and early intervention [
4,
9]. High-risk neonates for NFU are preemies (≤ 32 weeks and/or ≤ 1500g), with hypoxic ischemic encephalopathy, convulsions, Central Nervous System disorders, congenital infections, genetic syndromes, MRI pathological imaging, major morbidities, shock requiring inotropic support, severe hypoxemic episode, hypoglycemia, hyperbilirubinemia treated with exchange blood transfusion, Small for Gestational Age, mechanical ventilation support > 24 hours, feto-fetal transfusion, metabolic diseases, abnormal neurological examination at discharge, surgical treatment during Neonatal Intensive Care Unit (NICU) hospitalization and low socio-economic family status [
8,
10]. The interdisciplinary teams providing NFU programs mainly consist of Neonatologists, Physiotherapists, and Speech Therapists [
10,
11].
Attrition or loss to NFU has a significant impact on long-term health and specifically neurodevelopmental outcome of high-risk infants [
12,
13,
14,
15,
16,
17]. Consequently, reasons for non-participation in NFU programs [
6,
18] and strategies implemented for achieving higher attendance rates are of major importance [
19]. Several studies highlight the importance of defining reasons for non-attendance in NFU programs, planning and implementing certain strategies [
6,
18,
20,
21,
22,
23,
24,
25,
26,
27,
28,
29]. The COVID-19 pandemic has caused a decline in access to health services [
30] leading to limitation or even interruption of services provision, and even an increase in waiting time for prevention and rehabilitation health care [
30,
31]. The Greek health system was not an exception as it received enormous pressure [
32]. The SARS-COV-2 pandemic had a severely negative impact on maternal and infant health care programs [
33,
34], highlighting the necessity of defining strategic plans both at national and international level to restore the pre-pandemic levels of health services [
35]. To date, there is no published study investigating potential changes in reported reasons for non-attendance before and after the spread of COVID-19 and the impact on access to NFU programs. This study aims to investigate the impact of the COVID-19 pandemic on access to a NICU NFU program, to determine any changes in parent-reported reasons for non-attendance and predictors for non-compliance. The present study also examines any changes in the reported reasons or potential factors that led to abstaining from the NFU program before and after the spread of COVID-19. We hypothesized that attendance rates and reasons for discontinuation of a follow-up program at a Regular Outpatient Neonatology Clinic will differ before and after the onset of the COVID-19 pandemic.
2. Materials and Methods
We conducted a retrospective observational study using a questionnaire to collect data from families whose newborns were scheduled to participate in a NFU program at the Papageorgiou Hospital Outpatient Clinics before and during the SARS-CoV-2 pandemic in Greece. The data for this study was obtained from two sources: firstly, from the hospital's Systems Applications and Products Software (SAP system), which provided data of high risk infants hospitalized in the NICU, and secondly, through a structured questionnaire, answered by parents of newborns either discontinuing or not attending the NFU program, through a telephone contact. The questionnaire consisted of closed-ended questions, some of which allowed multiple answers, as well as open-ended questions. The closed-ended questions focused on participation in the monitoring program, while the open-ended questions on any obstacles or factors that may have influenced parents' experience during the visits (
Appendix A).
In particular, demographic characteristics of the families and research participants were obtained from the SAP and questionnaires. This information included the age of the father/mother, number of adults/children in the family, single parenthood, working hours, work status of the caregiver, daily work of the caregiver, education level, gender of the research participant, number of visits to the Hospital's Outpatient Clinic, nationality, and Hospital accessibility data such as distance, transport time, and number of tolls. The hospital's SAP system was used to search and retrieve information notes for all newborns, if available. This allowed for the recording of various clinical characteristics of the perinatal period. Specifically, the following parameters were recorded: birth weight (BW), gestational age (GA), method of delivery (vaginal or cesarean section), gender, age of the mother, multiple births, gestational diabetes or hypertension, antenatal steroid administration (ASA), multiparity, intrauterine growth, intrauterine growth restriction (IUGR), presence of early or late septicemia, and jaundice. Additionally, major morbidity factors such as Respiratory Distress Syndrome (RDS), bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), and retinopathy of prematurity (ROP) were also recorded.
Before conducting the research, permission was requested and obtained from Papageorgiou Hospital, and approval was obtained from the Ministry of Health. Anonymity was ensured, and participants were informed of their right to recall their data. Finally, the researcher digitally forwarded the consent form.
2.1. Data Collection
The sample comprises two groups of mother-infant pairs. The first group included newborns who were monitored before the onset of the COVID-19 pandemic, with at least one scheduled appointment between 12/02/2019 and 29/02/2020 (with no appointments scheduled beyond February 29, 2020). The second group included newborns after the onset of the COVID-19 pandemic who had at least one scheduled appointment between 03/01/2020 and 17/11/2021. Each group was divided into three subgroups: Group G1, which included families of neonates who did not miss any scheduled visit; Group G2, who visited the outpatient clinic at least once and discontinued follow-up; and Group G3 who never visited outpatient clinics. Finally, the reported reasons that led participants to discontinue follow-up were grouped by relevance, as shown below (
Table 1).
2.2. Statistical Analysis
Data was collected in Excel spreadsheets and statistical analysis was performed using SAS for Windows (version 9.4). Descriptive statistics for the arithmetic data were presented as median and 1st-3rd quartiles, while normality was evaluated by the Kolmogorov–Smirnov test. For categorical data, frequency and relevant percentages were used. For comparisons between groups, for arithmetic data, the Mann–Whitney U test or the Kruskal–Wallis test was used, the latter for more than two groups; for categorical data, the chi-square test and if required the Fisher’s exact test was used. Multivariable analysis was based on logistic regression models. The significance level for the study was set to p<0.05 and all tests were two-sided.
3. Results
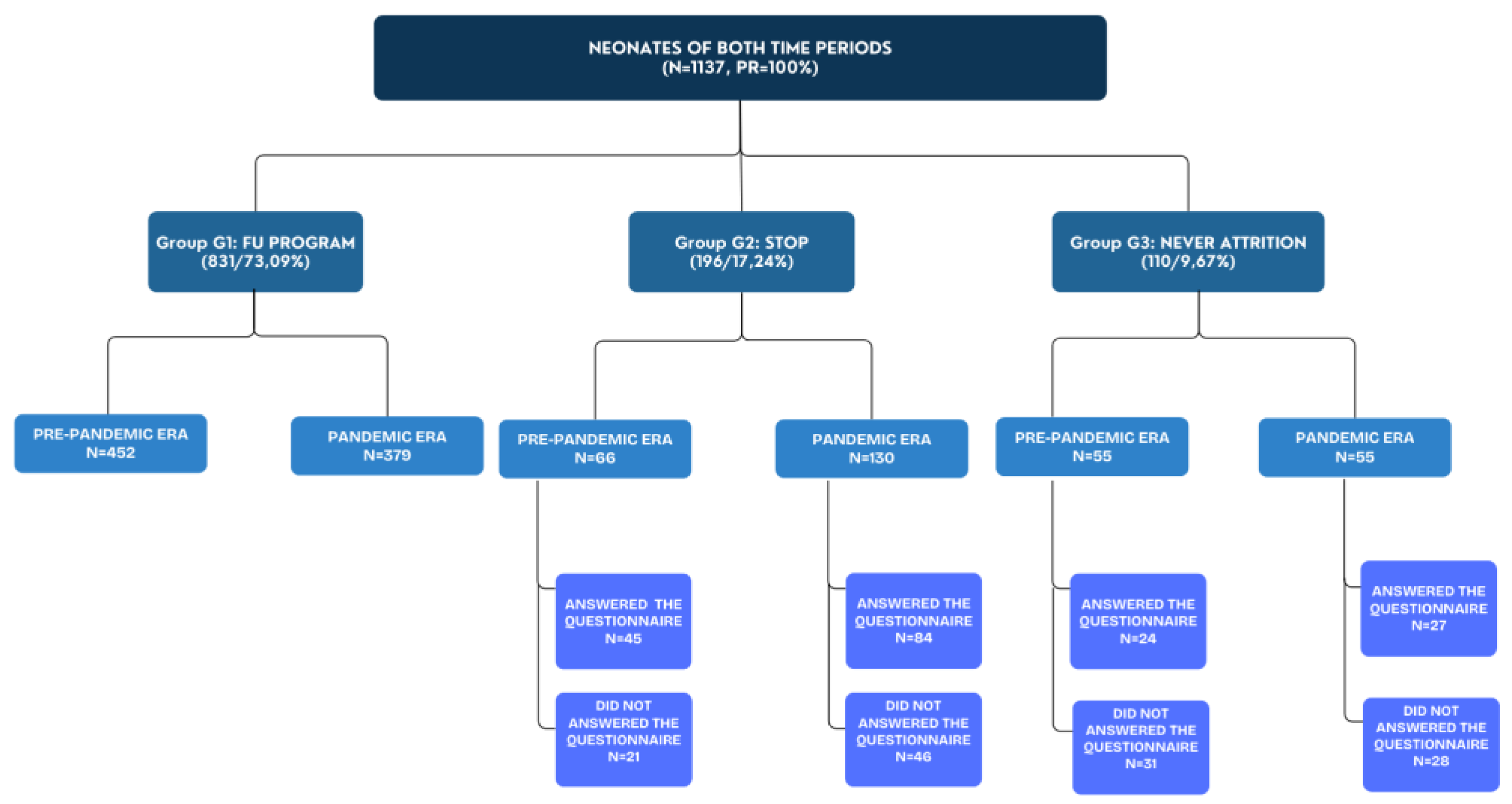
A total sample of 1137 high-risk newborns with 2254 scheduled appointments were recorded. Particularly, 831 newborns (73.08%) consistently participated in the follow-up program (group G1), while 196 (17.24%) discontinued the follow-up (group G2), and 110 (9.67%) did not attend any planned visits (group G3) (
Scheme 1). Out of 306 parents who discontinued or did not attend the NFU program (group G2+G3), 180 responded to the questionnaire (total response rate 58,8%), 69 from the pre-COVID-19 time period and 111 from the COVID-19 time period (
Scheme 1).
During the study period before the onset of the COVID-19 pandemic, 573 newborns were recorded with 452 included in the G1 group, 66 in the G2 group, and 55 in the G3 group (
Scheme 1). After the onset of COVID-19 pandemic, 564 neonates were recorded:, with 379 included to G1 group, 130 to G2 group, and 55 to G3 group (
Scheme 1). Additionally, before the onset of COVID-19 period, a total of 1132 scheduled appointments were recorded, with 143 (12.6%) not being carried out, either being postponed or "lost". During the COVID-19 period, a total of 1122 scheduled appointments were recorded, with 323 (28.8%) not being carried out, either being postponed or "lost". It is important to acknowledge that outpatient clinics were universally closed for 5.5 months during the pandemic [
32]. Therefore, the number of appointments in the COVID-19 period was numerically less than those carried out in the previous period.
3.1. Clinical and Demographic Characteristics before and after the Onset of COVID-19
Birth weight of newborns with scheduled visits after the onset of COVID-19 pandemic was found lower by an average of 260 grams than those before the pandemic (p=0.0005). Also, infants with scheduled visits during COVID-19 pandemic had a mean gestational age of 33.1 weeks (Q1-Q3: 31.4-35.7), while those who attended before COVID-19 pandemic had a mean gestational age of 34.6 weeks (Q1-Q3: 32-37.3), indicating a reduction in pregnancy duration by 3.5 weeks. Also, gestational diabetes and Respiratory Distress Syndrome were more common in the group of infants after the onset of COVID-19 pandemic. On the other hand, more infants appeared to have developed early onset sepsis before the onset of COVID-19 pandemic (
Table 2).
3.2. Attendance Rates before and after the Onset of COVID-19
During the study time period, 989 scheduled appointments were appointments completed at outpatient clinics before the COVID-19 pandemic (from 12/02/2019 to 29/02/2020, a period of 12.5 months) and 799 after COVID-19 onset (from 01/03/2020 to 17/11/2021, a period of 15.5 months). Additionally, 28.8% of appointments scheduled in the COVID-19 period were postponed or did not take place, much higher than the period before the onset of the pandemic (12.6%).
3.2.1. Reasons for Non-Attendance
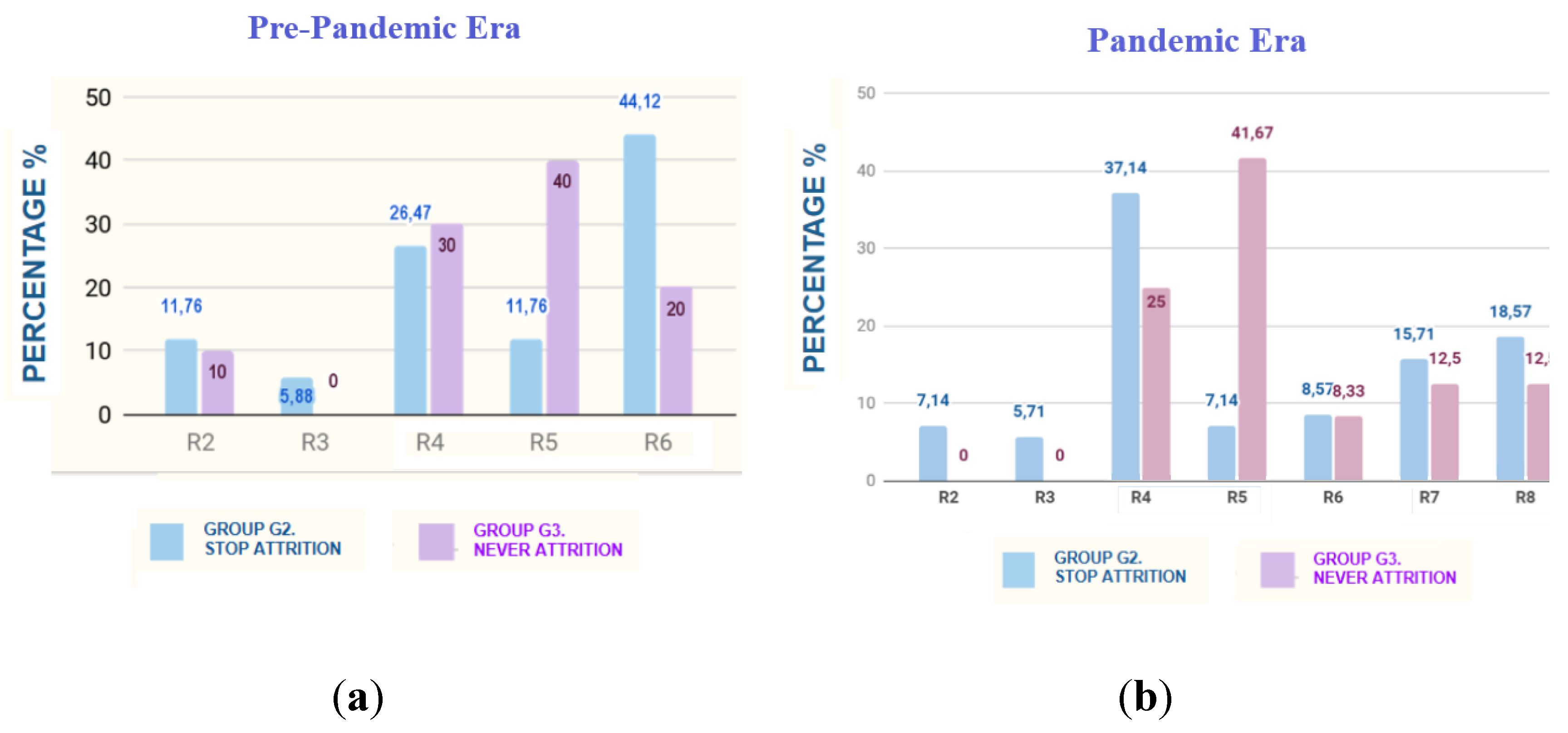
With regards to G2 group, during pre COVID-19 period, the main reported reasons for discontinuing NFU program before the onset of the pandemic were the perception that it was not necessary to maintain participation in the program (R6), at a rate of 44.12%, provider-related barriers (R4) at 26.47%, accessibility-related barriers (R2) and negligence (R5) at 11.76%. In addition, the parents did not mention any health issue or death in the family (R7), as well as possible feelings of insecurity about the hospital environment (R8). In the COVID-19 period, provider-related obstacles (R4) at 37,14%, fear of exposure (R8) at 18,57% and health issues or death in the family (R7) at 15,71% were recorded as the main reasons.
With regards to G3 group, reasons for non-participating at the NFU program during pre-COVID 19 period, were negligence (R5) at 40%, provider-related obstacles (R4) at 30% and perception that it was not necessary to maintain participation in the program (R6) at 20%. In addition, in the COVID-19 period, parental negligence (R5) at 41,67%, provider-related obstacles (R4) at 25%, health issues (R7) and fear of disease exposure (R8) at 12,5% were the main reasons. (
Figure 1).
3.2.2. Comparisons between Groups before the Onset of COVID-19
In order to identify factors related to NFU program participation we compared all three groups (G1, G2 & G3). Regarding the period before COVID-19, significant differences in birth weight, gestational age, antenatal steroid administration, multiparity, jaundice, respiratory distress syndrome, and nationality were recorded (
Table 3). Specifically, morbidity (hyperbilirubinemia (OR, 2.7; CI, 1.47-5, p=0.0016), RDS (OR, 2.33; CI, 1.02-5.26, p=0,00493)), ASA (OR, 4.76; CI, 1.37-16.67, p=0.007), multiple gestation (OR, 2.94; CI, 1.35-6.25, p=0,0047), nationality (OR, 3.13; CI, 1.56-6.25, p=0.0037) acted as incentives for participating to outpatient clinics to NFU program (
Table 3). Of note, infants who discontinued NFU program (group G2), were the most immature (gestational age 32,9 (29.7-35.6) wk) and of lowest BW (1750 (1355-2400 gr)) (
Table 3).
3.2.3. Comparisons between Groups after the Onset of COVID-19
Regarding the COVID-19 time period, comparison between three groups showed a statistically significant difference for morbidities (LOS , NEC, Jaundice, RDS) (
Table 4). Particularly, when comparing groups G1 & G2, LOS (OR, 0.48; CI, 0.28-0.82, p=0.078) and NEC (OR, 0.32; CI, 0.11-0.93, p=0.0467) did not act as incentives for program completion; otherwise, appeared to have a positive effect on joining the NFU program but not on maintaining participation in it. The comparison of groups G1 and G3 showed that more immature neonates, of lower birth weight with morbidities (jaundice (OR, 3.45; CI, 1.82-6.67, p=0.0001), LOS (OR, 4.17; CI, 0.97-16.67, p=0.0372), RDS (OR, 2.44; CI, 1,2-5, p=0.0155)) participated the NFU program.
3.2.4. Multiple Regression Analysis
Multiple regression analysis showed that multiple gestation birth was the only factor in continuing the NFU program in the COVID-19 time period. Neonates of multiple pregnancies appeared to be four times more likely to continue follow-up in the COVID-19 period (OR, 4.04; CI, 1.09-14.9). Additionally, before the COVID-19 time period, no factors were found to potentially lead to participation in the NFU program.
4. Discussion
Improving attendance to NFU programs and addressing barriers to participation are key priorities for enhancing the quality of neonatal care [
6,
36,
37,
38]. However, the impact of the COVID-19 pandemic on access to NFU programs and the potential barriers to family participation have not been thoroughly studied. Our research reveals significant differences for reasons of participation in a NFU program before and after the onset of the pandemic, highlighting the need for further exploration. Additionally, morbidities (RDS, jaundice, NEC, LOS), ASA, multiple gestation and nationality were significant factors for participation in the NFU program.
Kondilis et al.'s study reveals that the utilization of essential public hospital services in Greece during COVID-19 pandemic (from January to November 2020) compared to the 2017-2019 time period, decreased significantly [
32]. Specifically, visits to non-emergency public hospital departments decreased by 33.3% (95% CI: 16.0%–50.5%) [
32]. In our study, the non-attendance rate significantly increased by 2.5-fold during the COVID-19 pandemic (28.8% compared to 12.6%). This is also in line with Panda et al's study. (2021), which underlines that in the USA 43% of programs showed a decrease in attendance rates even one year after the onset of COVID-19 pandemic [
39].
Newborns that did not attend any visits (G3 group) before and after the onset of COVID-19, tended to be more mature and healthier (without morbidities: RDS, jaundice, NEC, LOS), without ASA, of immigrant families, having had more children. Also, newborns that attended the program but did not continue follow up (group G2) had morbidities such as LOS or NEC, which appears to have a positive effect on joining the NFU program but not on maintaining participation.
Most of the findings of this research support international literature. Researchers have shown that families with clinically ill neonates during hospitalization, were more likely to adhere to a NFU program [
20,
22,
26,
27,
28,
40]. According to Patra et al. 's research, very low birth weight, small gestational age, multiple gestation, and Chronic Lung Disease were factors significantly associated with follow-up visits attendance [
6]. Additionally, Harmon and Sweringen et al. studies, showed that longer duration of oxygen hospitalization and mild chronic lung disease were associated with greater and lower odds of NFU compliance, respectively [
20,
22]. Moreover, Swearingen et al. study, showed an inverse relationship of neonates’ gestational age with participation in the program, findings similar with the present research [
22]. Of note, Perenyi et al. comments that parents of neonates with severe health issues or longer hospital stay, have more opportunities to understand their infant’s condition leading to better compliance [
17]. Additionally, neonates of singleton pregnancies were four times more likely to discontinue their participation in the follow-up program after the onset of COVID-19. This is in line to Kim et al.'s study, which suggests that the attendant group had higher rates of multiple pregnancies [
28]. It is important to note that several parents (group G2) highlighted the difficulty during their waiting time in outpatient clinics due to the hospitals’ policy to allow the presence of only one parent per family due to measures against coronavirus spread.
During the period before the onset of the pandemic, the main reported reason for discontinuing follow-up (group G2) was the perception that it was not necessary to maintain participation in the program (R6), while the second most common reason, was related to obstacles caused by the provider (R4).Conversely, the main reason for stopping follow-up in the period after the onset of the pandemic was barriers related to the provider (R5), while the second most common reason, was fear of exposure to disease (COVID-19 or other diseases) (R8), following closely by illness (or death) within the family (R7). With regards to the G3 group, the main reported reason for abstaining from the NFU program both in the period before and after the onset of the pandemic was parental neglect (R5). The second main reason for abstaining from the NFU program was various barriers related to the provider itself (R4), in both periods. Notably, references to a busy parental/family work schedule (R3) as a cause did not significantly differ between the two time periods.
The perception that participation in the NFU is unnecessary if their newborn does not develop health problems has also been reported as a reason for avoiding appointments (R6) by Ballantyne et al. and Duarte et al. studies [
24,
25]. Additionally, Tang et al. study highlights key barriers to family attendance, such as parental work schedules (R3), the parent's perceptions of the child's health status and lack of follow-up (R6) [
18]. Swearingen et al. study found scheduling issues on the part of providers as the second most frequently reported barrier to participation (R4) [
22]. Also, accessibility and distance from the clinic (R2) were highlighted as barriers to attendance by Tang et al. and Ballantyne et al. [
18,
25]. In the present research, barriers related to access and distance from the hospital were identified mainly before the onset of COVID-19 time period.
Also, DeMauro et al. study suggests that larger households are more likely to leave the program (23), while Ballantyne et al. [
25] suggests that limited financial resources act as a barrier to participation in the program. As previously reported larger families did not participate in the NFU program, mainly before COVID-19 time period.
Several studies have emphasized that difficulties with insurance coverage (R1) are a key factor leading to non-adherence to the follow-up program [
6,
18,
20,
40]. Fortunately, in this survey, none of the participating parents mentioned insurance coverage as a barrier to maintaining their participation.
Several studies underline the role of telemedicine for multidisciplinary developmental follow-up after NICU discharge, in comparison to in person meetings [
23]. Watson et al.'s study showed that telemedicine was associated with an increased attendance rate in a twelve-month follow-up program for preterm infants [
41]. In contrast to other similar NFU programs in other countries such as the USA, Canada, and Italy, which tried to exploit the potential benefits of telemedicine by conducting remote appointments with the participation of multidisciplinary teams during the pandemic [
39,
42], in the current NFU program under study nothing similar was implemented. Of note, our NICU did not develop any strategy of enhanced support for parents who faced difficulties attending the program. This lack of a specific strategy for attending NFU program has also been referred to by other studies. Tang et al.'s study indicates that 54% of NFU programs lack a specific strategic plan for attrition [
18].
It is of extreme importance for NICUs employees (physicians, nurses, and administrative staff) to effectively communicate with parents about the importance of the NFU program and the potential benefits of maintaining participation in the program. In conclusion, staff members should encourage the parents to be in contact for any difficulties, concerns, or questions about the follow-up schedule. This will allow appointments to be rescheduled immediately and prevent low attrition rates. Additionally, continuous feedback on the barriers faced by the parents should be provided so that any adopted strategies can be redefined by the provider as needed [
43].
4.1. Limitations
There are some limitations to be underlined. Researchers collected clinical data available only in the SAP digital system; The researchers couldn't investigate the reasons for non-adherence or abstention specifically from refugees' population groups. The present research did not examine specific clinical variables during hospitalization (oxygen administration, oxygen at discharge, length of stay, surgery requirement, breast feeding, and maternal drug use).
5. Conclusions
In conclusion, this study has revealed several key factors associated with adherence to a NFU program during pre and COVID-19 time periods. It is imperative to implement targeted strategies such as patient education, reminder phone calls, and a systematic approach to increase attendance rate in NFU programs. These measures should be focused on families at risk for non-compliance. All of the above significantly contribute to better long-term patient care and neurodevelopmental outcomes through early detection and intervention programs.
Author Contributions
Conceptualization, Evdoxia Nantsi and Ilias Chatziioannidis; methodology, Evdoxia Nantsi, Ilias Chatziioannidis and Elias Kondilis; validation, Evdoxia Nantsi, Ilias Chatziioannidis; formal analysis, Abraham Pouliakis; investigation, Evdoxia Nantsi; resources, Ilias Chatziioannidis; data curation, Evdoxia Nantsi; writing—original draft preparation, Evdoxia Nantsi; writing—review and editing, Evdoxia Nantsi and Ilias Chatziioannidis; visualization, Evdoxia Nantsi supervision, Ilias Chatziioannidis and Georgios Mitsiakos; project administration, Evdoxia Nantsi. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted and approved by Papageorgiou Hospital Scientific Council (341st meeting, April 21, 2021, Thessaloniki, Greece), with reference code 118.
Informed Consent Statement
Consent was obtained from parents involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author due to privacy reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
QUESTIONNAIRE
Research: Attendance in a neonatal follow up program before and in the time of COVID-19 pandemic
1. Participant Code (filled in by the researcher): _________________________
Demographics
2. Guardian Gender (Mark only one answer): Man ____ Woman ____
3. Age: ____________
4. Nationality: ____________
5. Marital Status (Mark only one answer): With a partner ____ Without a partner ____
6. Number of adults living together at home (and taking care of the newborn): __________
7. Number of Children: ____________
8. Professional Status: ________________________
9. Hours of work per week: ____________
10. Work on a daily basis (Mark only one answer): Yes ____ No ____
11. Educational level: _______________________
12. Place of permanent residence: ________________________
Special Questions (Choose the answer that best suits your situation)
13. Was there a recommendation from the pediatrician to stop the program / referral to another clinic? (Mark only one answer): Yes ____ No ____
14. We skipped the visit, due to:
(You can highlight more than one answer and prioritize them.)
_____ lack of insurance coverage
_____ the distance of the clinic from the permanent residence
_____ lack of means of transport
_____ change of residence / move (to another region / country)
_____ a busy parental / family work schedule
_____ limited availability during clinic hours
_____ that I/we judged that it was not necessary, our child was fine
_____there was no specific reason
_____ Other reason
15. If you answered "other" in the previous question, please briefly state the reason that led to the omission of the visit?
______________________________________________________________________________________________________________________________________________________________________
16. Is there anything in particular that made your experience participating in the follow-up program difficult or challenging that you would like recorded?
______________________________________________________________________________________________________________________________________________________________________
References
- Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. The Lancet. 2012 Jun;379(9832):2162–72. [CrossRef]
- World Health Organization. Preterm birth [Internet]. 2023 [cited 2023 May 28]. Available from: https://www.who.int/news-room/fact-sheets/detail/preterm-birth.
- McCormick MC, Litt JS, Smith VC, Zupancic JAF. Prematurity: An Overview and Public Health Implications. Annu Rev Public Health. 2011 Apr 21;32(1):367–79. [CrossRef]
- Litt JS, Campbell DE. High-Risk Infant Follow-Up After NICU Discharge. Clin Perinatol. 2023 Mar;50(1):225–38. [CrossRef]
- Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. 2016 Dec;40(8):542–8. [CrossRef]
- Patra K, Greene MM, Perez B, Silvestri JM. Neonatal high-risk follow-up clinics: How to improve attendance in very low birth weight infants. EJ Neonatal Res. 2014;4(1):3–12.
- McGowan EC, Vohr BR. Neurodevelopmental Follow-up of Preterm Infants. Pediatr Clin North Am. 2019 Apr;66(2):509–23. [CrossRef]
- Purdy IB, Melwak MA. Who Is at Risk? High-Risk Infant Follow-up. Newborn Infant Nurs Rev. 2012 Dec;12(4):221–6. [CrossRef]
- Orton J, Spittle A, Doyle L, Anderson P, Boyd R. Do early intervention programmes improve cognitive and motor outcomes for preterm infants after discharge? A systematic review: Early Intervention for Preterm Infants. Dev Med Child Neurol. 2009 Nov;51(11):851–9. [CrossRef]
- LW, Anderson PJ, Battin M, Bowen JR, Brown N, Callanan C, et al. Long term follow up of high risk children: who, why and how? BMC Pediatr. 2014 Dec;14(1):279. [CrossRef]
- Ayala L, Winter S, Byrne R, Fehlings D, Gehred A, Letzkus L, et al. Assessments and Interventions for Spasticity in Infants With or at High Risk for Cerebral Palsy: A Systematic Review. Pediatr Neurol. 2021 May;118:72–90. [CrossRef]
- Kuppala VS, Tabangin M, Haberman B, Steichen J, Yolton K. Current state of high-risk infant follow-up care in the United States: results of a national survey of academic follow-up programs. J Perinatol. 2012;32(4):293–8. [CrossRef]
- Tang B. The State of Neonatal Follow-Up Programs. In: Needelman H, Jackson BJ, editors. Follow-Up for NICU Graduates: Promoting Positive Developmental and Behavioral Outcomes for At-Risk Infants [Internet]. Cham: Springer International Publishing; 2018 [cited 2024 Jun 12]. p. 337–41. Available from. [CrossRef]
- Vohr BR, O’Shea M, Wright LL. Longitudinal multicenter follow-up of high-risk infants: why, who, when, and what to assess. Semin Perinatol. 2003 Aug 1;27(4):333–42. [CrossRef]
- Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJS. Cognitive and Behavioral Outcomes of School-Aged Children Who Were Born Preterm: A Meta-analysis. JAMA. 2002 Aug 14;288(6):728. [CrossRef]
- Maitre NL, Duncan AF. Neurologic and Developmental Outcomes of High-Risk Neonates. Clin Perinatol. 2023 Mar;50(1):xxi–xxii. [CrossRef]
- Perenyi A, Katz J, Flom P, Regensberg S, Sklar T. Analysis of compliance, morbidities and outcome in neurodevelopmental follow-up visits in urban African-American infants at environmental risk. J Dev Orig Health Dis. 2010 Dec;1(6):396–402. [CrossRef]
- Tang B, Lee H, Gray E, Gould J, Hintz S. Programmatic and Administrative Barriers to High-Risk Infant Follow-Up Care. Am J Perinatol. 2018 Aug;35(10):940–5. [CrossRef]
- Ballantyne M, Stevens B, Guttmann A, Willan AR, Rosenbaum P. Transition to Neonatal Follow-up Programs: Is Attendance a Problem? J Perinat Neonatal Nurs. 2012;26(1):90–8. [CrossRef]
- Harmon SL, Conaway M, Sinkin RA, Blackman JA. Factors associated with neonatal intensive care follow-up appointment compliance. Clin Pediatr (Phila). 2013;52(5):389–96. [CrossRef]
- Brady JM, Pouppirt N, Bernbaum J, D’Agostino JA, Gerdes M, Hoffman C, et al. Why do children with severe bronchopulmonary dysplasia not attend neonatal follow-up care? Parental views of barriers. Acta Paediatr. 2018 Jun;107(6):996–1002. [CrossRef]
- Swearingen C, Simpson P, Cabacungan E, Cohen S. Social disparities negatively impact neonatal follow-up clinic attendance of premature infants discharged from the neonatal intensive care unit. J Perinatol. 2020 May;40(5):790–7. [CrossRef]
- DeMauro SB, Bellamy SL, Fernando M, Hoffmann J, Gratton T, Schmidt B, et al. Patient, Family, and Center-Based Factors Associated with Attrition in Neonatal Clinical Research: A Prospective Study. Neonatology. 2019;115(4):328–34. [CrossRef]
- Duarte ED, Tavares TS, Cardoso IVL, Vieira CS, Guimarães BR, Bueno M. Factors associated with the discontinuance of outpatient follow-up in neonatal units. Rev Bras Enferm. 2020;73(3):e20180793. [CrossRef]
- Ballantyne M, Benzies K, Rosenbaum P, Lodha A. Mothers’ and health care providers’ perspectives of the barriers and facilitators to attendance at Canadian neonatal follow-up programs. Child Care Health Dev. 2015 Sep;41(5):722–33. [CrossRef]
- Hintz SR, Gould JB, Bennett MV, Lu T, Gray EE, Jocson MAL, et al. Factors Associated with Successful First High-Risk Infant Clinic Visit for Very Low Birth Weight Infants in California. J Pediatr. 2019 Jul;210:91-98.e1. [CrossRef]
- Ballantyne M, Stevens B, Guttmann A, Willan AR, Rosenbaum P. Maternal and infant predictors of attendance at Neonatal Follow-Up programmes. Child Care Health Dev. 2014;40(2):250–8. [CrossRef]
- Kim NH, Youn YA, Cho SJ, Hwang JH, Kim EK, Kim EAR, et al. The predictors for the non-compliance to follow-up among very low birth weight infants in the Korean neonatal network. Gurgel RQ, editor. PLOS ONE. 2018 Oct 1;13(10):e0204421. [CrossRef]
- Nehra V, Pici M, Visintainer P, Kase JS. Indicators of compliance for developmental follow-up of infants discharged from a regional NICU. J Perinat Med. 2009;37(6):677–81. [CrossRef]
- Tuczyńska M, Matthews-Kozanecka M, Baum E. Accessibility to Non-COVID Health Services in the World During the COVID-19 Pandemic: Review. Front Public Health. 2021 Dec 16;9:760795. [CrossRef]
- De Biase S, Cook L, Skelton DA, Witham M, ten Hove R. The COVID-19 rehabilitation pandemic. Age Ageing. 2020 Aug 24;49(5):696–700. [CrossRef]
- Kondilis E, Tarantilis F, Benos A. Essential public healthcare services utilization and excess non-COVID-19 mortality in Greece. Public Health. 2021 Sep;198:85–8. [CrossRef]
- Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020 Jul;8(7):e901–8. [CrossRef]
- Erdei C, Liu CH. The downstream effects of COVID-19: a call for supporting family wellbeing in the NICU. J Perinatol. 2020 Sep;40(9):1283–5. [CrossRef]
- Fazzi E, Galli J. New clinical needs and strategies for care in children with neurodisability during COVID-19. Dev Med Child Neurol. 2020 Jul;62(7):879–80. [CrossRef]
- Fraiman YS, Edwards EM, Horbar JD, Mercier CE, Soll RF, Litt JS. Racial Inequity in High-Risk Infant Follow-Up Among Extremely Low Birth Weight Infants. Pediatrics. 2023 Feb 1;151(2):e2022057865. [CrossRef]
- Fuller MG, Lu T, Gray EE, Jocson MAL, Barger MK, Bennett M, et al. Rural Residence and Factors Associated with Attendance at the Second High-Risk Infant Follow-up Clinic Visit for Very Low Birth Weight Infants in California. Am J Perinatol. 2023 Apr;40(05):546–56. [CrossRef]
- Attar MA, Gates MR, Iatrow AM, Lang SW, Bratton SL. Barriers to Screening Infants for Retinopathy of Prematurity after Discharge or Transfer from a Neonatal Intensive Care Unit. J Perinatol. 2005 Jan 1;25(1):36–40. [CrossRef]
- Panda S, Somu R, Maitre N, Levin G, Singh AP. Impact of the Coronavirus Pandemic on High-Risk Infant Follow-Up (HRIF) Programs: A Survey of Academic Programs. Children. 2021 Oct 6;8(10):889.Roberts HJ, Harris RM, Krehbiel. [CrossRef]
- C, Banks B, Jackson B, Needelman H. Examining disparities in the long term follow-up of Neonatal Intensive Care Unit graduates in Nebraska, U.S.A. J Neonatal Nurs. 2016 Oct;22(5):250–6. [CrossRef]
- Watson L, Woods CW, Cutler A, DiPalazzo J, Craig AK. Telemedicine Improves Rate of Successful First Visit to NICU Follow-up Clinic. Hosp Pediatr. 2023 Jan 1;13(1):3–8. [CrossRef]
- Caporali C, Pisoni C, Naboni C, Provenzi L, Orcesi S. Challenges and opportunities for early intervention and neurodevelopmental follow-up in preterm infants during the COVID-19 pandemic. Child Care Health Dev. 2021 Jan;47(1):140–1. [CrossRef]
- Christner LP, Irani S, McGowan C, Dabaja E, Dejong C, Attar MA. Previous missed visits and independent risk of loss to follow-up in the high-risk neonatal follow-up clinic. Early Hum Dev. 2023 Aug;183:105813. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).