1. Introduction
Digital health, a rapidly increasing field at the intersection of healthcare and technology, holds immense potential for transforming healthcare delivery in Nigeria's remote communities [
1]. These areas face numerous challenges, including limited access to quality healthcare, inadequate infrastructure, and geographical isolation [
1]. Recognizing these issues, there is a growing need to explore innovative solutions that can bridge the existing gaps and improve overall health outcomes [
2].
A comprehensive understanding of the role of digital health in addressing healthcare challenges in Nigeria's remote communities is provided in this paper [
3]. The specific objectives include but not limited to;
Firstly, delving into the various components of digital health, such as telehealth, mobile health applications, and electronic health records, to understand their potential impact on healthcare delivery [
3].
Secondly, analysing the challenges associated with implementing digital health solutions in remote areas and proposing viable solutions to overcome these obstacles [
2].
Thirdly
, investigating existing government initiatives and policies that support the integration of digital health in remote communities and assessing their effectiveness [
2].
Also, showcasing grassroots advocacy initiatives aimed at promoting digital health awareness and adoption at the community level [
3].
Finally, discussing emerging technologies and envisioning the future of digital health in Nigeria's remote regions, considering both technological advancements and policy developments [
1].
The significance of digital health in Nigeria's remote communities cannot be overstated [
1]. Digital health interventions can bridge the geographical gap, providing residents in remote areas with easier access to healthcare services through telemedicine and mobile health applications [
3].
By facilitating electronic health records and data-driven decision-making, digital health ensures a more streamlined and efficient healthcare delivery system, thereby improving the quality of care [
2].
Digital health empowers communities by fostering health literacy, enabling self-care, and facilitating active participation in healthcare decisions [
1]. With real-time health monitoring and early detection capabilities, digital health can contribute to timely interventions and preventive measures, reducing the burden of diseases in remote areas [
3].
2. Contextualizing Healthcare Challenges in Nigeria's Remote Areas
Access to quality healthcare in Nigeria's remote areas is flawed by a multifaceted back-and-forth of factors that contribute to healthcare disparities [
3].
Understanding the landscape of challenges is essential to developing targeted interventions and policies that address the unique needs of these regions [
4]. Like healthcare infrastructure, workforce distribution, and the availability of essential medical resources [
2].
These disparities are often worsened by geographical remoteness, making it challenging for residents to access timely and adequate healthcare services [
4].
Remote areas commonly lack well-equipped healthcare facilities, leading to a shortage of medical personnel, diagnostic tools, and essential medications [
2]. This inadequacy significantly hinders the provision of comprehensive healthcare services [
4].
Preventive healthcare measures, including vaccination programs and health education, face challenges in reaching remote populations due to infrastructural limitations and difficulties in communication [
5].
2.1. Consequences of Limited Healthcare in Remote Regions
Limited access to healthcare leads to delayed medical interventions, contributing to the progression of diseases and worsening health outcomes [
3].
In addition, the absence of timely and adequate healthcare services is often associated with higher mortality rates, particularly among vulnerable populations such as infants, pregnant women, and the elderly [
5].
Moreover,
the poor health outcomes in remote regions have economic repercussions, with communities grappling with increased healthcare costs, lost productivity, and a diminished workforce due to preventable health issues and the Nigeria ‘Japa’ syndrome that is causing Nigeria to loose most of his best hands [
6].
Furthermore, limited access to quality healthcare perpetuates a cycle of poverty in remote areas, as individuals and communities struggle with the financial burden of treating preventable illnesses, further limiting their economic opportunities [
4].
This contextualization of healthcare challenges sets the stage for understanding the urgency and importance of digital health interventions in Nigeria's remote regions [
7]. Addressing these challenges requires a comprehensive approach that leverages technology, policy changes, and community engagement to improve healthcare accessibility and outcomes [
8].
2.2. Key Components of Digital Health Interventions
Digital health interventions encompass a range of technologies and applications aimed at revolutionizing healthcare delivery [
8]. Understanding the key components is crucial for appreciating the transformative impact these innovations can have, particularly in Nigeria's remote communities [
5].
Firstly, understanding telehealth and telemedicine [
2]. This involves the delivery of healthcare services remotely using telecommunications technology [
8]. This encompasses virtual consultations, remote monitoring, and the exchange of medical information over secure networks [
8].
Telehealth facilitates real-time interactions between healthcare providers and patients, overcoming geographical barriers [
4]. This is especially crucial in remote areas where access to in-person healthcare is limited [
8].
Telemedicine extends to remote diagnostics and medical imaging [
1], allowing healthcare professionals to assess and diagnose conditions without the need for patients to travel to specialized facilities [
3].
Also, telehealth ensures continuity of care by enabling follow-up consultations and ongoing medical monitoring, improving the overall management of chronic conditions in remote communities [
8].
Secondly, mobile health (mHealth) applications leverage mobile devices, such as smartphones and tablets, to provide access to health information, resources, and services [
9]. This is particularly impactful in regions with limited physical infrastructure [
5].
Mobile health applications play a vital role in health education, delivering information about preventive measures, nutrition, and general wellness directly to users' devices, fostering a culture of health awareness [
9].
In addition, mHealth apps enable remote monitoring of vital signs and health parameters [
9]. In cases of irregularities or emergencies, these applications can generate alerts, prompting timely interventions [
10].
Therefore, enhancing healthcare accessibility because mHealth applications often include features for scheduling appointments and sending reminders, ensuring that individuals in remote areas can plan and adhere to their healthcare appointments [
8].
Thirdly, electronic health records (EHR) systems which help in digital and centralise patient health records, providing a comprehensive and easily accessible repository of medical information [
2]. This is especially valuable in remote areas where paper-based records may be prone to loss or damage [
9].
EHR systems helps in facilitating seamless communication and data sharing among healthcare providers [
9]. This enhances coordination of care, critical for ensuring that patients in remote regions receive comprehensive and well-coordinated healthcare services [
1].
Moreover, EHR systems enable healthcare
providers leverage data analytics, to make informed decisions based on trends and patterns in patient health [
1]. This promotes proactive and personalized healthcare strategies [
2].
Therefore, patients in remote communities can actively engage in their healthcare by accessing their electronic health records, fostering a sense of empowerment and encouraging adherence to treatment plans [
8].
In conclusion, understanding these key components underscores the versatility and potential of digital health interventions to address healthcare challenges in Nigeria's remote areas [
8]. By integrating these technologies, it becomes possible to overcome geographical barriers and enhance the quality and accessibility of healthcare services in these regions [
7].
2.3. Defining Digital Health in the Nigerian Context
In the Nigerian context, digital health refers to the integration of technology, information, and communication tools into healthcare delivery [
11]. This includes electronic health records, telehealth, mobile health applications, and other innovative solutions aimed at improving healthcare accessibility, efficiency, and outcomes [
4].
Digital health in Nigeria is tailored to address the unique challenges and opportunities within the country's healthcare system [
8]. This involves considerations of cultural diversity, linguistic variations, and specific health challenges prevalent in different regions, including remote communities [
8].
It also encompasses the involvement of government bodies, policies, and regulations that guide the implementation and integration of digital health technologies into the national healthcare framework [
11].
2.3.1. Historical Overview of Digital Health Initiatives
Nigeria has seen the gradual adoption of digital health initiatives over the past two decades [
8]. Early efforts involved pilot programs focused on electronic health record systems in urban areas, with a subsequent expansion into more remote regions [
11].
The proliferation of mobile technology and improved telecommunication infrastructure has played a pivotal role in the historical development of digital health initiatives [
11]. This has facilitated the growth of mobile health applications and telemedicine services across the country [
12].
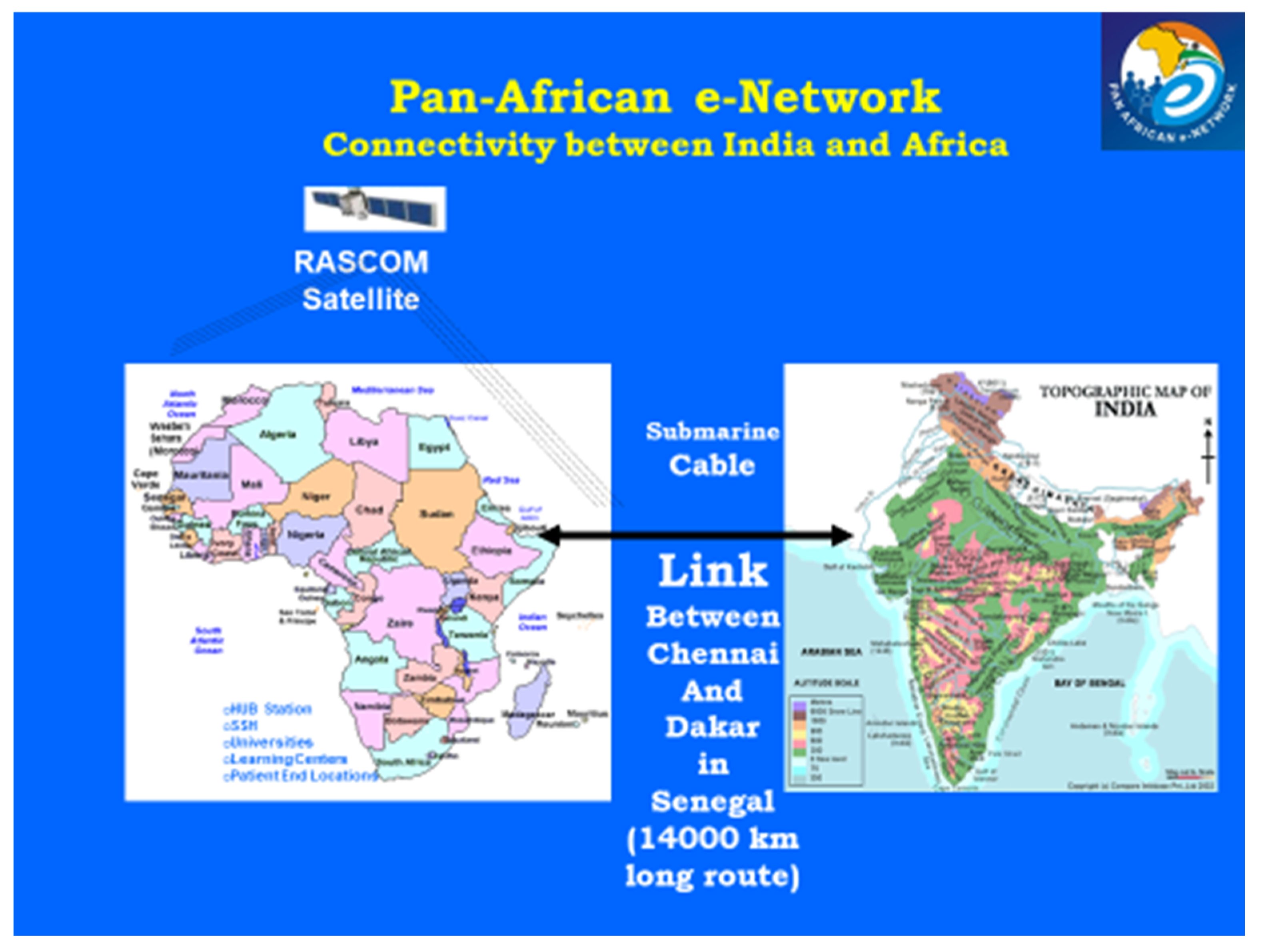
One of those early initiatives in history is the Pan-African e-Network Project, a practical example of south-south cooperation [
13]. Initiative of government of India in collaboration with African Union. A non-commercial project, funded by the Govt. of India at a budgetary cost of
$150 Million [
14].
Dr. A P J Abdul Kalam, the former President of India during his inaugural address to the African Parliament in Johannesburg on 16th Sep. 2004, proposed to connect all 53 AU member countries with Indian institutions with a satellite and fibre-optic network to share India’s expertise in the fields of education and health care for accelerated socio-economic development of Africa [
15].
AU accepted the Indian proposal and signed an umbrella MOU with government of India (through ministry of external affairs – nodal ministry) [
13].
Government of India appointed TCIL as the turnkey implementing agency of the project network, the network primarily provide e-services with priority on tele-education, tele-medicine, and VVIP connectivity (video-conferencing and VOIP) among the heads of African states [
16].
Figure 1.
Pan-African e-Network Connectivity between India and Africa (Source: TCIL) [
16]
.
Figure 1.
Pan-African e-Network Connectivity between India and Africa (Source: TCIL) [
16]
.
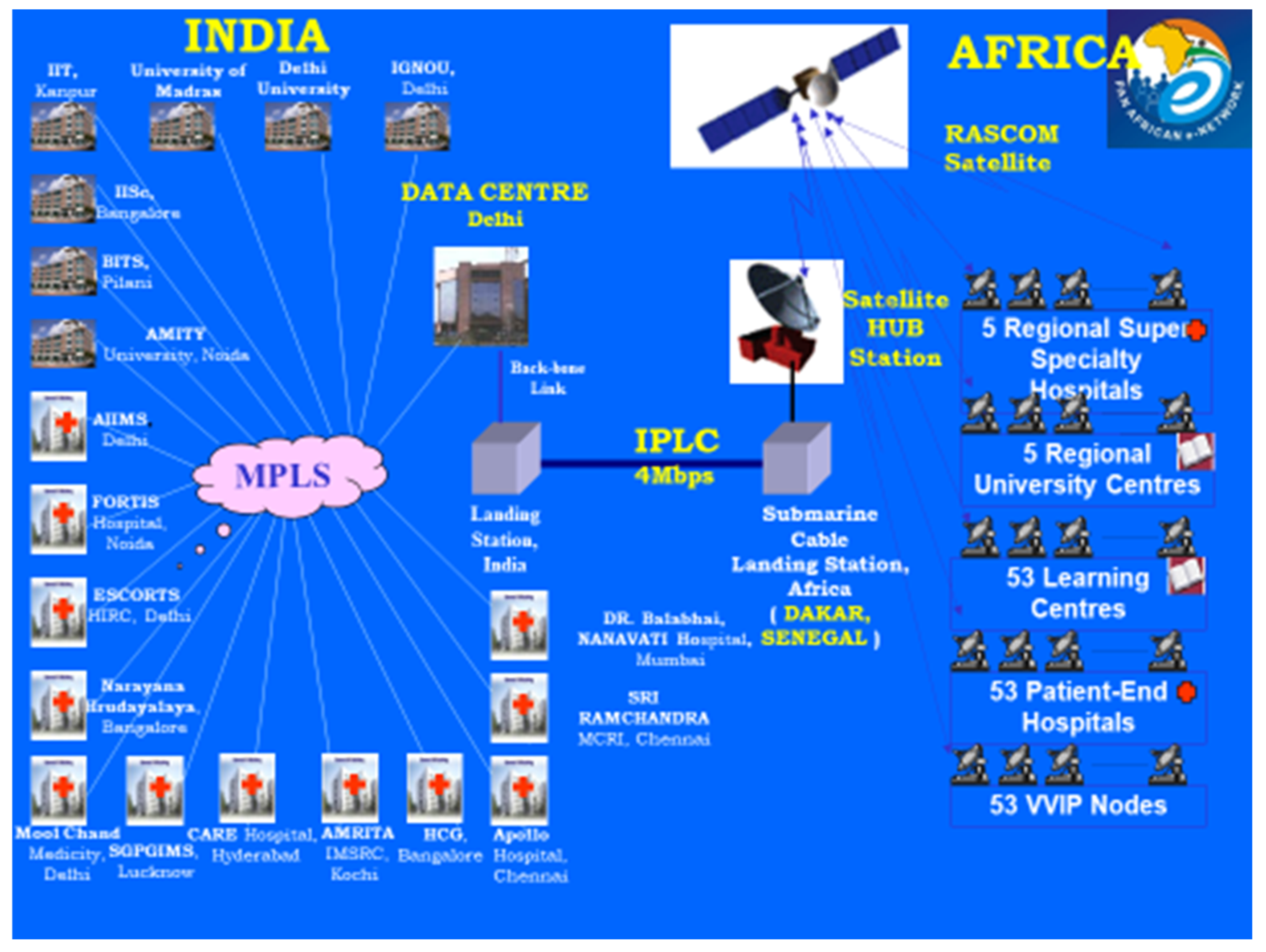
The Pan African telemedicine network involved University College Hospital as a regional coordinating centre, super specialist hospital and Lagos University Teaching Hospital as a patient end location [
16]. This was connected among fifty three African countries, twelve Indian super specialist hospital.
Figure 2.
architecture of Pan-African e-network (Source TCIL) [
16]
.
Figure 2.
architecture of Pan-African e-network (Source TCIL) [
16]
.
The Nigerian government initiated several programs to digitize healthcare delivery, including the National Health Management Information System (NHMIS) and the National Electronic Health Policy [
16]. These initiatives aim to create a digital ecosystem that enhances healthcare services nationwide [
15].
The second initiative in early history in Nigeria is the implementation of remote telemedicine with the initiative of an equipped bus [
17]. The initiative of the Federal Ministry of Science and Technology through its agency, the Nigerian National Space Research and Development Agency (NASRDA) collaborated with the Federal Ministry of Health for the use of the bus for mobile telemedicine [
18].
Telemedicine was one of the target applications of the Nigerian Communications Satellite which carries Hughes VSAT equipment, Polycom video equipment and AMD telemedicine (NOC) [
19]. The pilot project sub-networks integration commenced in March 2007 with the Network Operation Centre. The initial plan was for the integration of the sub-network to include Eight Remote Terminals and One Mobile Unit commissioned in January 2008 [
19].
The remote terminals are in Bayelsa, Benin Kebbi, Ibadan, Gombe, Maiduguri, Makurdi, Owerri, and Owo, spread across the geopolitical zones in the country [
19]. The remote terminals and mobile bus are equipped with basic diagnosis equipment such as Cameras (General Examination Camera, Image & Illumination System) and Diagnostic Scopes (Electronic Stethoscope –Ear, Nose & Throat (ENT) Scope, Ophthalmoscope and Derma-scope) [
19].
Figure 3.
The Nigerian Communications Satellite which carries Hughes VSAT equipment, Polycom video equipment and AMD telemedicine.
Figure 3.
The Nigerian Communications Satellite which carries Hughes VSAT equipment, Polycom video equipment and AMD telemedicine.
2.4. Global and Regional Influences on Digital Health Adoption
Nigeria's digital health landscape is influenced by global best practices and successful case studies from other countries [
8]. Collaborations with international organizations and partnerships with global technology providers contribute to the transfer of knowledge and expertise [
11].
In addition, digital health initiatives in Nigeria are also influenced by collaborations with neighbouring African countries [
17]. Shared challenges and regional health priorities contribute to the exchange of ideas, technologies, and collaborative efforts to address common healthcare issues [
8].
Furthermore, emerging technological innovation hubs in major Nigerian cities serve as catalysts for the development and implementation of digital health solutions [
8]. These hubs foster collaboration between technology experts, healthcare professionals, and policymakers, driving innovation in the digital health space [
17].
Therefore, understanding the nuances of the digital health landscape in Nigeria provides a foundation for exploring how these technologies can be effectively leveraged to address healthcare challenges in remote communities [
11]. The integration of global best practices and regional collaborations contributes to the ongoing evolution of digital health initiatives in the country [
8].
2.4.1. Challenges and Solutions in Implementing Digital Health
Implementing digital health interventions comes with its fair share of challenges, but innovative solutions are reshaping the landscape [
11]. One major hurdle is limited access to technology and infrastructure, particularly in remote or underserved areas [
8]. To address this, low-tech solutions like SMS-based interventions or utilizing community health workers as intermediaries have proven effective [
8]. Partnerships with telecommunications companies can also expand network coverage in remote communities [
11].
Privacy and security concerns pose another challenge. Safeguarding patient data and ensuring compliance with data protection regulations are critical [
20]. Robust data encryption, secure cloud storage, and adherence to privacy regulations such as GDPR and HIPAA are essential [
17]. Regular security audits and user education about data protection can enhance trust in digital health solutions [
20].
Low digital literacy among healthcare providers and patients is a barrier to effective use of digital health tools [
21]. Comprehensive training programs for healthcare workers and user-friendly interfaces for patients can improve digital literacy and engagement [
11]. Incorporating user feedback in the design process ensures that digital tools meet the needs of end-users [
20].
Interoperability between different digital health systems and platforms is crucial for seamless healthcare delivery [
22]. Adopting standardized data formats and protocols, such as HL7 and FHIR, promotes interoperability [
23]. Developing open APIs allows different systems to communicate and share data seamlessly [
22].
The initial cost of implementing digital health solutions and ensuring their long-term sustainability can be prohibitive, especially in resource-constrained settings [
23]. Adopting scalable and cost-effective technologies, such as open-source software and mobile applications, can reduce costs. Public-private partnerships and government support can also ensure the sustainability of digital health initiatives [
8].
Resistance to change among healthcare providers and patients can impede the adoption of digital health solutions [
8]. Providing incentives for healthcare providers to embrace digital health, such as improved efficiency and patient outcomes, can motivate adoption [
11]. Engaging patients in the design and implementation process can also increase acceptance and usage [
22].
Ensuring the quality and safety of digital health solutions, as well as regulatory compliance, is a complex challenge [
22]. Establishing clear quality assurance standards and regulatory frameworks specific to digital health can ensure the safety and efficacy of these technologies [
22]. Collaboration between regulatory bodies, industry stakeholders, and healthcare providers is key to developing and implementing these standards [
23].
In conclusion, addressing these challenges through innovative solutions and collaborative efforts can enhance the implementation of digital health, leading to improved healthcare access, quality, and outcomes [
22].
2.5. Policy Implications and Advocacy for Sustainable Change
Effective policies and advocacy efforts play a pivotal role in ensuring the sustained integration of digital health into Nigeria's remote communities [
22].
Policy implications and advocacy play crucial roles in ensuring the sustainable implementation of digital health solutions [
8]. As digital health continues to evolve, policymakers must navigate complex issues to maximize its potential while minimizing risks and ensuring equitable access for all [
1].
One key policy area is the regulation of digital health technologies [
11]. Policymakers must develop regulatory frameworks that balance innovation with patient safety and privacy [
11]. Clear guidelines are needed for the development, deployment, and use of digital health tools to ensure they meet high standards of quality and effectiveness [
8]. This includes establishing standards for data security, interoperability, and ethical use of health data [
22].
Another important policy consideration is the integration of digital health into existing healthcare systems. Policymakers must work to ensure that digital health technologies complement traditional healthcare services and do not create additional barriers to access. This may involve investing in infrastructure to support digital health, such as broadband internet access and training for healthcare workers.
Policymakers also have a role to play in promoting digital health literacy among healthcare providers and patients [
22]. This includes educating healthcare workers about the benefits and limitations of digital health technologies and empowering patients to make informed decisions about their healthcare [
2]. Policymakers can support initiatives that promote digital health literacy, such as public awareness campaigns and training programs [
22].
In addition to regulatory and infrastructure considerations, policymakers must also address the broader social and ethical implications of digital health [
4]. This includes ensuring that digital health technologies are accessible to marginalized communities and do not exacerbate existing health disparities [
6]. Policymakers can support research and advocacy efforts that aim to address these issues and promote health equity [
22].
Advocacy is another key component of driving sustainable change in digital health [
22]. Advocates can raise awareness about the benefits of digital health, mobilize support for policy changes, and hold policymakers and industry stakeholders accountable for their actions [
8,
22]. Advocacy efforts should be inclusive, engaging a wide range of stakeholders, including patients, healthcare providers, policymakers, and industry representatives [
11].
One example of successful advocacy in digital health is the push for telemedicine reimbursement policies [
22]. Advocates have worked to convince policymakers to expand reimbursement for telemedicine services, making it easier for patients to access care remotely [
8]. This has been particularly important during the COVID-19 pandemic, when in-person healthcare visits were limited [
17].
In conclusion, policy implications and advocacy are critical for ensuring the sustainable implementation of digital health solutions [
22]. Policymakers must develop clear regulatory frameworks, support infrastructure development, promote digital health literacy, and address social and ethical considerations [
11,
22].
Advocates play a vital role in raising awareness, mobilizing support, and holding stakeholders accountable [
22]. By working together, policymakers and advocates can help realize the full potential of digital health to improve healthcare access, quality, and outcomes for all [
8].
2.6. Measuring Impact: Data-Driven Insights
Measuring the impact of digital health interventions is essential to understand their effectiveness and drive continuous improvement [
24]. By leveraging data-driven insights, policymakers, healthcare providers, and other stakeholders can make informed decisions to enhance healthcare delivery and patient outcomes [
24].
2.6.1.a. Quantitative and Qualitative Assessments
Quantitative assessments involve the use of numerical data to measure the impact of digital health interventions [
22]. This may include metrics such as the number of patients served, the reduction in healthcare costs, or the improvement in health outcomes [
24]. Quantitative data provides valuable insights into the effectiveness of interventions and can help identify areas for improvement [
20,
24].
Qualitative assessments, on the other hand, involve gathering non-numerical data, such as patient testimonials or healthcare provider feedback [
24]. Qualitative data provides a more nuanced understanding of the impact of digital health interventions, capturing the experiences and perspectives of those involved [
22]. By combining quantitative and qualitative assessments, stakeholders can gain a comprehensive understanding of the impact of digital health interventions [
24].
2.6.2.b. Monitoring Health Outcomes and Patient Satisfaction
Monitoring health outcomes is a key component of measuring the impact of digital health interventions [
8,
22]. This may involve tracking indicators such as the improvement in disease management, the reduction in hospital readmissions, or the increase in preventive care services [
22]. By monitoring health outcomes, stakeholders can assess the effectiveness of interventions and make data-driven decisions to improve patient care [
22].
Patient satisfaction is another important metric to consider when measuring the impact of digital health interventions [
11]. This may involve gathering feedback from patients about their experience with digital health tools, such as ease of use, convenience, and overall satisfaction [
8]. By understanding patient satisfaction, stakeholders can identify areas for improvement and ensure that digital health interventions meet the needs of patients [
24].
2.6.3.c. Learning from Data for Continuous Improvement
Data-driven insights can also be used to drive continuous improvement in digital health interventions [
24]. By analysing data, stakeholders can identify trends, patterns, and areas for improvement [
24]. This may involve identifying best practices, refining intervention strategies, or developing new interventions based on data-driven insights [
22].
One example of learning from data for continuous improvement is the use of predictive analytics to identify patients at risk of developing complications [
24]. By analysing data, healthcare providers can identify patients who may benefit from early intervention, such as medication adjustments or lifestyle modifications [
22]. This can lead to improved health outcomes and reduced healthcare costs [
24].
In conclusion, measuring the impact of digital health interventions through data-driven insights is essential for improving healthcare delivery and patient outcomes [
24]. By leveraging quantitative and qualitative assessments, monitoring health outcomes and patient satisfaction, and learning from data for continuous improvement, stakeholders can make informed decisions to enhance the effectiveness of digital health interventions [
22,
24].
2.7. Voices from the Communities: Perspectives of Stakeholders
Interviews with healthcare providers can offer valuable insights into the impact of digital health interventions on healthcare delivery [
8]. Providers can share their experiences using digital tools, highlighting the benefits and challenges they encounter [
22]. These interviews can provide a deeper understanding of how digital health is transforming healthcare delivery from the perspective of those on the front lines [
11].
Healthcare providers may discuss how digital tools have improved their ability to deliver care, such as by enabling remote consultations, streamlining administrative tasks, or enhancing communication with patients [
2]. They may also share challenges they face, such as technological barriers, workflow disruptions, or concerns about patient privacy [
7]. These insights can inform efforts to address barriers and improve the implementation of digital health interventions [
5].
In addition, testimonials from patients and caregivers offer a first-hand perspective on the impact of digital health interventions on health outcomes and quality of life [
9]. Patients can share their experiences using digital tools, highlighting how these tools have changed their healthcare experience [
13].
Patients may discuss how digital tools have improved their access to care, enabled them to better manage their health conditions, or enhanced their communication with healthcare providers [
3]. They may also share challenges they face, such as difficulty using the technology, concerns about privacy, or limitations in the scope of services offered [
22]. These testimonials can provide valuable insights into the usability and effectiveness of digital health interventions from the perspective of those receiving care [
11].
Therefore, Community leaders play a critical role in advocating for improved healthcare services and addressing the unique needs of their communities [
9]. By engaging community leaders in discussions about digital health, stakeholders can gain insights into the specific challenges and opportunities facing different communities [
13].
Community leaders may advocate for increased access to digital health services, improved infrastructure to support digital health initiatives, or culturally sensitive approaches to healthcare delivery [
11]. Their advocacy can help shape policies and programs that better meet the needs of underserved communities and ensure that digital health interventions are inclusive and equitable [
8].
In conclusion, capturing the perspectives of stakeholders through interviews, testimonials, and advocacy efforts can provide valuable insights into the impact of digital health interventions on healthcare delivery and patient outcomes [
12]. These insights can inform efforts to improve the implementation and effectiveness of digital health interventions, ultimately leading to better health outcomes for all [
22].
2.8. Government Initiatives and Policies Supporting Digital Health
Government initiatives and policies play a crucial role in shaping the landscape of digital health and driving sustainable change [
12]. Policymakers can enact regulations and provide funding to support the adoption and integration of digital health technologies into healthcare systems [
22].
One key policy area is the development of standards and guidelines for digital health technologies [
8]. Governments can establish frameworks for the evaluation and approval of digital health products, ensuring that they meet high standards of safety, efficacy, and data privacy [
11]. Additionally, governments can incentivize the adoption of digital health technologies through reimbursement policies and grants for healthcare providers [
22].
Government initiatives can also support the development of infrastructure for digital health, such as broadband internet access and electronic health record systems [
13]. By investing in these areas, governments can improve the accessibility and effectiveness of digital health technologies, particularly in underserved communities [
11].
Grassroots advocacy plays a critical role in promoting the integration of digital health into healthcare systems [
12]. Local communities and organizations can advocate for policies and programs that support the adoption of digital health technologies and address barriers to access [
22].
Grassroots advocacy efforts can include raising awareness about the benefits of digital health, mobilizing support from community members and stakeholders, and engaging with policymakers to promote policy changes [
22]. By amplifying the voices of local communities, grassroots advocacy can drive sustainable change and ensure that digital health technologies meet the needs of the people they serve [
12].
Collaborations between the public and private sectors are essential for driving sustainable change in digital health [
13]. Public-private partnerships can leverage the strengths of both sectors to develop innovative solutions and overcome challenges in implementing digital health technologies [
17].
Public-private collaborations can involve joint research and development efforts, shared infrastructure, and collaborative policy-making [
13]. By working together, the public and private sectors can accelerate the adoption of digital health technologies and improve healthcare outcomes for all [
22].
In conclusion, government initiatives, grassroots advocacy, and collaborations between the public and private sectors are essential for driving sustainable change in digital health [
22]. By working together, stakeholders can overcome challenges, promote the adoption of digital health technologies, and improve healthcare delivery and outcomes for all [
11].
2.9. Emerging Technologies Shaping the Future of Digital Health
The future of digital health is being shaped by a range of emerging technologies that have the potential to revolutionize healthcare delivery. One such technology is artificial intelligence (AI), which can analyse large datasets to identify trends and patterns that can inform clinical decision-making [
24]. AI-powered tools can assist healthcare providers in diagnosing diseases, personalizing treatment plans, and predicting health outcomes [
23].
Another emerging technology is the Internet of Things (IOT), which involves connecting devices to the internet to collect and share data [
23]. IOT devices, such as wearable fitness trackers and remote monitoring devices, can provide real-time health information to both patients and healthcare providers, enabling proactive management of health conditions [
22].
Block chain technology is also gaining traction in the healthcare industry due to its ability to secure and share sensitive health information [
12]. Block chain can ensure the integrity and privacy of health data, enabling secure sharing of electronic health records (EHRs) and improving interoperability between different healthcare systems [
11].
2.10. Opportunities for Global and Local Partnerships
Global and local partnerships are essential for driving innovation and advancing digital health [
25]. Collaboration between countries and organizations can facilitate the sharing of best practices, resources, and expertise, leading to the development of more effective digital health solutions [
25].
At the global level, organizations such as the World Health Organization (WHO) and the International Telecommunication Union (ITU) are working to promote digital health initiatives and facilitate collaboration between countries [
22]. These organizations provide a platform for sharing knowledge and resources, enabling countries to learn from each other's experiences and leverage each other's strengths [
11].
In addition, at the local level partnerships between healthcare providers, technology companies, and government agencies can drive innovation and improve healthcare delivery [
8]. By working together, these stakeholders can develop tailored solutions that address the specific needs of local communities and improve health outcomes [
22].
Therefore, research and development (R&D) play a crucial role in advancing digital health by driving innovation and developing new technologies [
22]. R&D efforts focus on improving the effectiveness, accessibility, and affordability of digital health solutions, ultimately improving healthcare delivery and patient outcomes [
11].
One area of R&D focus is the development of new digital health technologies, such as AI algorithms, IOT devices, and block chain solutions [
8]. Researchers are exploring how these technologies can be applied to healthcare to improve diagnosis, treatment, and prevention of diseases [
12].
Another area of R&D focus is the evaluation of digital health interventions to assess their impact on healthcare delivery and patient outcomes [
8]. Researchers conduct clinical trials and studies to determine the effectiveness of digital health technologies and identify areas for improvement [
22].
In conclusion, embracing emerging technologies, fostering partnerships, and investing in research and development are critical steps in shaping the future of digital health in Nigeria [
24]. These strategies contribute to a dynamic and adaptive digital health ecosystem that can effectively address evolving healthcare challenges and opportunities [
22].
3. Conclusions
In conclusion, digital health has the potential to transform healthcare delivery in Nigeria's remote communities, bridging gaps and improving access to quality care [
24].
Looking ahead, there is a need for continued investment in digital health infrastructure and capacity building in remote communities [
11]. Governments, healthcare providers, and other stakeholders must work together to develop policies and programs that support the integration of digital health into existing healthcare systems [
8]. This includes ensuring the interoperability of digital health technologies, addressing privacy and security concerns, and promoting digital literacy among healthcare providers and patients [
22].
Additionally, there is a need for ongoing research and evaluation to assess the impact of digital health interventions and identify areas for improvement. By leveraging emerging technologies, global partnerships, and research and development efforts, Nigeria can achieve sustainable healthcare transformation in its remote communities, ensuring that all citizens have access to quality care.
Funding
“This research received no external funding”
Conflicts of Interest
There is conflict of interest.
References
- Owusu-Ansah, E. D. G. J., Avuglah, R. K., & Kyere, Y. A. (2024). Quantum Leap and Uptake for Technological Advances in Africa in the Era of the COVID-19 Crisis. Examining the Rapid Advance of Digital Technology in Africa, 238-269.
- Rivetti, C., Allen, T. E., Brown, J. B., Butler, E., Carmichael, P. L., Colbourne, J. K., ... & Campos, B. (2020). Vision of a near future: Bridging the human health–environment divide. Toward an integrated strategy to understand mechanisms across species for chemical safety assessment. Toxicology In Vitro, 62, 104692. [CrossRef]
- Owoyemi, A., Osuchukwu, J. I., Azubuike, C., Ikpe, R. K., Nwachukwu, B. C., Akinde, C. B., ... & Olaniran, S. (2022). Digital solutions for community and primary health workers: lessons from implementations in Africa. Frontiers in Digital Health, 4, 876957. [CrossRef]
- Anyanwu, E. C., Maduka, C. P., Ayo-Farai, O., & Chinaemelum, C. (2024). Maternal and child health policy: A global review of current practices and future directions. [CrossRef]
- Morelli, S., D’Avenio, G., Daniele, C., Grigioni, M., & Giansanti, D. (2024, March). Under the Tech Umbrella: Assessing the Landscape of Telemedicine Innovations (Telemechron Study). In Healthcare (Vol. 12, No. 6, p. 615). MDPI. [CrossRef]
- Dzinamarira, T., Iradukunda, P. G., Saramba, E., Gashema, P., Moyo, E., Mangezi, W., & Musuka, G. (2024). COVID-19 and mental health services in Sub-Saharan Africa: A critical literature review. Comprehensive Psychiatry, 152465. [CrossRef]
- Lawal, R. (2023). Transformative Potential of IoT on Smart Healthcare and Remote Patient Monitoring in Nigeria: A Literature Review. environments, 20(27), 28.
- Egenti, B. N., Chukwudi, F. T., Igweagu, C. P., Ubajaka, C. F., & Adogu, P. O. U. E-HEALTH AND TELEMEDICINE PRACTICE IN NIGERIA (1999-2017): CHALLENGES AND PROSPECTS.
- Omoloja, A., & Vundavalli, S. (2021). Patient generated health data: Benefits and challenges. Current problems in pediatric and adolescent health care, 51(11), 101103.
- Ullah, M., Hamayun, S., Wahab, A., Khan, S. U., Rehman, M. U., Haq, Z. U., & Naeem, M. (2023). Smart technologies used as smart tools in the management of cardiovascular disease and their future perspective. Current Problems in Cardiology, 48(11), 101922. [CrossRef]
- Ekuri, S. O. (2020). IMPLEMENTING DIGITAL HEALTH FOR MATERNAL HEALTH IN NIGERIA: A LITERATURE REVIEW.
- Chika, E. U., Dike Ujunwa Precious, B., Ahuchaogu King-David, B., Gabriel Ezenri, B., Nneji Tobechukwu Okechukwu, B., Chidozie, C., & Madubugwu, R. (2024). Digital Healthcare Tools in Nigeria: Strengthening Public Health and Pandemic Preparedness-Insights from the COVID-19 Crisis. Telehealth and Medicine Today, 9(1). [CrossRef]
- DaSilva-Glasgow, D., & Pile, M. D. India in the Development Assistance Global Landscape: Reflections from the Caribbean Sub Region. Editorial Note.
- https://www.mea.gov.in/Portal/LegalTreatiesDoc/NA09B2850.pdf.
- https://www.peaceau.org/en/article/first-progress-report-of-the-chairperson-of-the commission-on-the-pan-african-e-network-on-tele-education-and-tele-medicine.
- https://www.mea.gov.in/Portal/LegalTreatiesDoc/NA09B2850.pdf.
- Alenoghena, C. O., Ohize, H. O., Adejo, A. O., Onumanyi, A. J., Ohihoin, E. E., Balarabe, A. I., ... & Alenoghena, B. (2023). Telemedicine: A survey of telecommunication technologies, developments, and challenges. Journal of Sensor and Actuator Networks, 12(2), 20. [CrossRef]
- Dodoo, J. E., Al-Samarraie, H., & Alsswey, A. (2022). The development of telemedicine programs in Sub-Saharan Africa: progress and associated challenges. Health and technology, 12(1), 33-46. [CrossRef]
- https://www.google.com/url?client=internal-element-cse&cx=a3f3408b7d24d8336&q=https://spacewatchafrica.com/improved-healthcare-services-in-nigeria-through-the-use-of-web-based-ict-initiative/&sa=U&ved=2ahUKEwjij7z-3e6EAxVNWkEAHabZBo0QFnoECAQQAg&usg=AOvVaw2USjyYSlXV1ABgT_ifa_4_.
- Aderigbigbe, T., & Adegbile, T. (2023). The gods are not to Blame: A Review of the Right to Health for Universal Health Coverage through Telehealth in Nigeria. Redeemer's University Journal of Jurisprudence and International Law, 3(1).
- Faux-Nightingale, A., Philp, F., Chadwick, D., Singh, B., & Pandyan, A. (2022). Available tools to evaluate digital health literacy and engagement with eHealth resources: a scoping review. Heliyon, 8(8). [CrossRef]
- Abernethy, A., Adams, L., Barrett, M., Bechtel, C., Brennan, P., Butte, A., ... & Valdes, K. (2022). The promise of digital health: then, now, and the future. NAM perspectives, 2022. [CrossRef]
- Nan, J., & Xu, L. Q. (2023). Designing interoperable health care services based on fast healthcare interoperability resources: Literature review. JMIR Medical Informatics, 11(1), e44842. [CrossRef]
- Cancela, J., Charlafti, I., Colloud, S., & Wu, C. (2021). Digital health in the era of personalized healthcare: opportunities and challenges for bringing research and patient care to a new level. Digital Health, 7-31.
- Odone, A., Gianfredi, V., Sorbello, S., Capraro, M., Frascella, B., Vigezzi, G. P., & Signorelli, C. (2021). The use of digital technologies to support vaccination programmes in Europe: state of the art and best practices from experts’ interviews. Vaccines, 9(10), 1126. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).