Submitted:
30 August 2024
Posted:
02 September 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study Design and Theoretical Underpinning
2.2. Study Setting
2.3. Study Population
2.4. Recruitment
2.5. Phase 1: Quantitative
2.5.1. Patient Survey
2.5.2. Training of Data Collectors
2.5.3. Sample Size Calculations
2.5.4. Data Collection
2.5.5. Data Analysis
2.6. Phase 2: Qualitative Interviews
2.6.1. Sampling and Recruitment
2.6.2. Data Collection
2.6.3. Sample Size Determination
2.6.4. Data Analysis
2.7. Reflexivity
2.8. Triangulation and Integration of Findings
3. Results
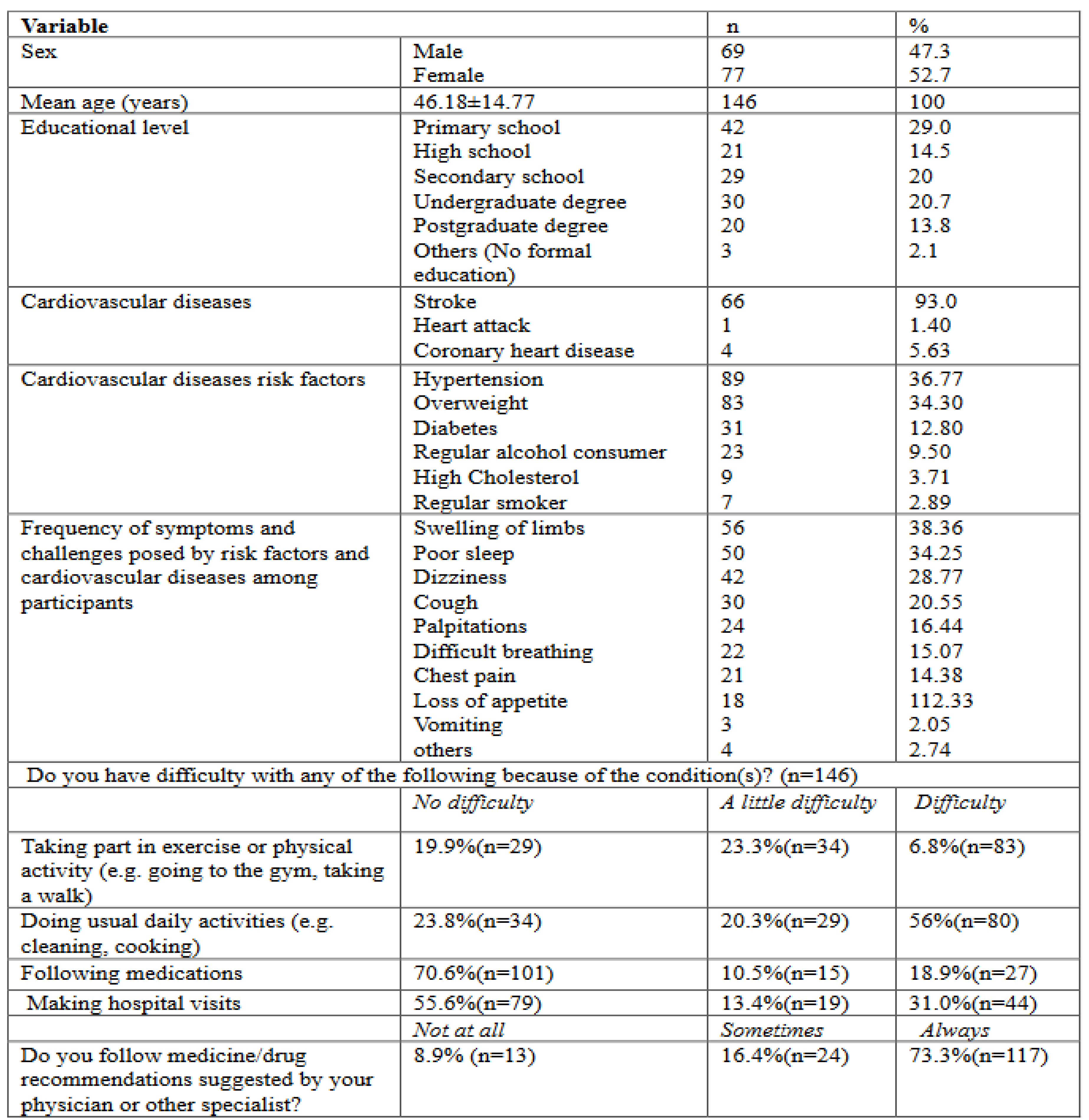
3.1. Participant Characteristics
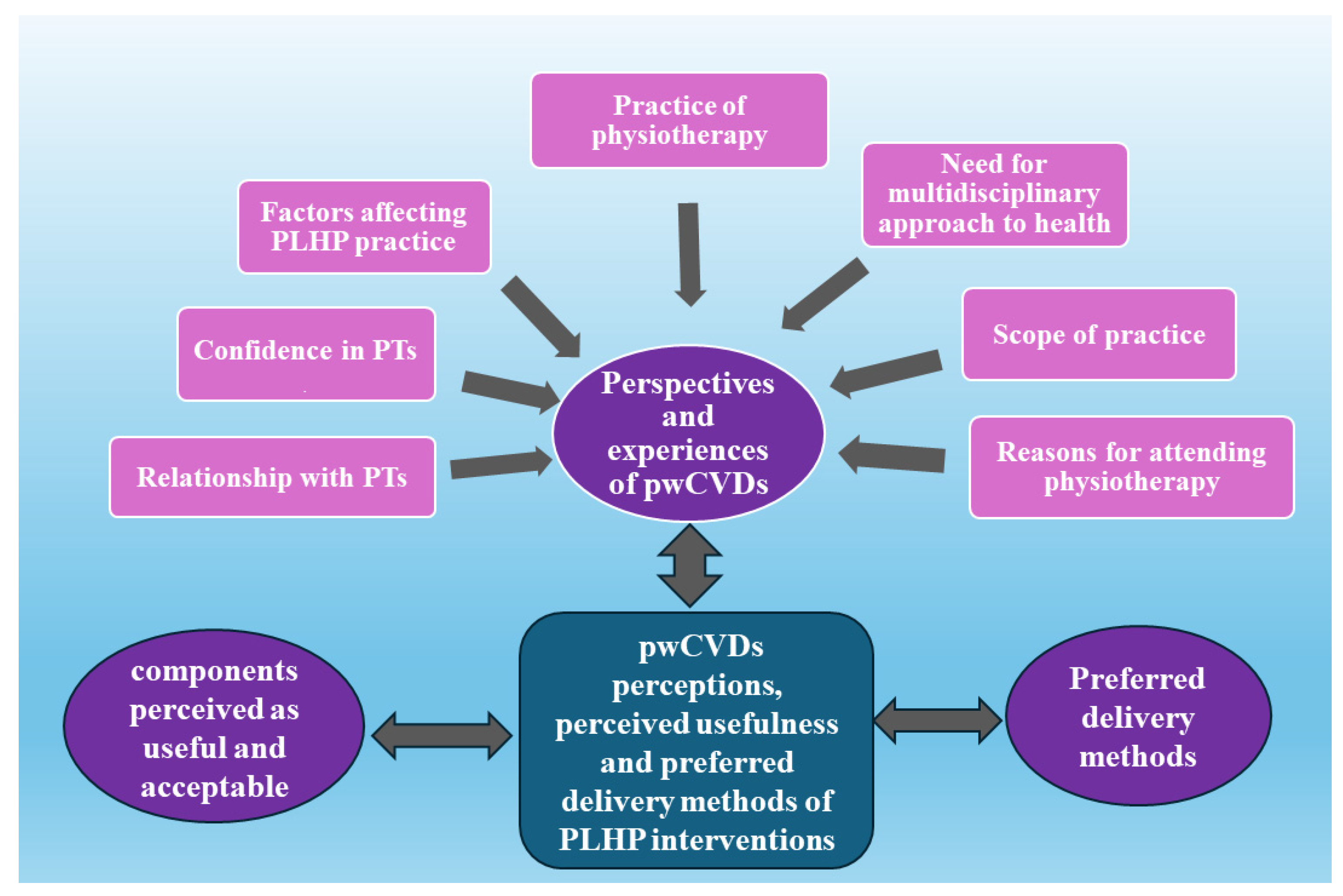
3.2. Synthesised Findings
3.3. Perspectives and Experiences of pwCVDs on PLHP
3.3.1. Reasons for Attending Physiotherapy
3.3.2. Scope of PLHP Practice
3.3.3. Relationship with Physiotherapists
3.3.4. Practice of Physiotherapy
3.3.5. Need for a Multidisciplinary Approach to Health
3.3.6. Factors Affecting PLHP Practice
3.3.7. Confidence in Physiotherapists
3.4. Perceived Usefulness and Acceptability of PLHP
3.4.1. Components Found to Be Useful
3.4.2. Components Found to More Acceptable
3.5. Preferred Methods of PLHP Delivery
4. Discussion
4.1. Implications for Practice, Training and Research
Practice
Training
Research
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, J.; Bu, X.; Wei, L.; Wang, X.; Lai, L.; Dong, C.; Ma, A.; Wang, T. Global Burden of Cardiovascular Diseases Attributable to Hypertension in Young Adults from 1990 to 2019. J. Hypertens. 2021, 39, 2488–2496. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Druetz, T. Integrated Primary Health Care in Low- and Middle-Income Countries: A Double Challenge. BMC Med. Ethics 2018, 19, 48. [Google Scholar] [CrossRef]
- Mudie, K.; Jin, M.M.; Tan; Kendall, L.; Addo, J.; dos-Santos-Silva, I.; Quint, J.; Smeeth, L.; Cook, S.; Nitsch, D.; et al. Non-Communicable Diseases in Sub-Saharan Africa: A Scoping Review of Large Cohort Studies. J. Glob. Health 2019, 9, 020409. [Google Scholar] [CrossRef]
- Nkoke, C.; Jingi, A.M.; Makoge, C.; Teuwafeu, D.; Nkouonlack, C.; Dzudie, A. Epidemiology of Cardiovascular Diseases Related Admissions in a Referral Hospital in the South West Region of Cameroon: A Cross-Sectional Study in Sub-Saharan Africa. PLOS ONE 2019, 14, e0226644. [Google Scholar] [CrossRef]
- Appiah, L.T.; Sarfo, F.S.; Agyemang, C.; Tweneboah, H.O.; Appiah, N.A.B.A.; Bedu-Addo, G.; Opare-Sem, O. Current Trends in Admissions and Outcomes of Cardiac Diseases in Ghana. Clin. Cardiol. 2017, 40, 783–788. [Google Scholar] [CrossRef]
- Keates, A.K.; Mocumbi, A.O.; Ntsekhe, M.; Sliwa, K.; Stewart, S. Cardiovascular Disease in Africa: Epidemiological Profile and Challenges. Nat. Rev. Cardiol. 2017, 14, 273–293. [Google Scholar] [CrossRef]
- Dzudie, A.; Fourie, J.M.; Scholtz, W.; Scarlatescu, O.; Nel, G.; Kingue, S. PASCAR and WHF Cardiovascular Diseases Scorecard Project. 2020, 31, 8. [Google Scholar] [CrossRef]
- Dessie, G.; Mulugeta, H.; Amare, D.; Negesse, A.; Wagnew, F.; Getaneh, T.; Endalamew, A.; Adamu, Y.W.; Tadesse, G.; Workineh, A.; et al. A Systematic Analysis on Prevalence and Sub-Regional Distribution of Undiagnosed Diabetes Mellitus among Adults in African Countries. J. Diabetes Metab. Disord. 2020, 19, 1931–1941. [Google Scholar] [CrossRef]
- IDF Atlas 9th Edition and Other Resources. Available online: https://www.diabetesatlas.org/en/resources/ (accessed on 14 August 2020).
- Noubiap, J.J.; Bigna, J.J.; Nansseu, J.R.; Nyaga, U.F.; Balti, E.V.; Echouffo-Tcheugui, J.B.; Kengne, A.P. Prevalence of Dyslipidaemia among Adults in Africa: A Systematic Review and Meta-Analysis. Lancet Glob. Health 2018, 6, e998–e1007. [Google Scholar] [CrossRef]
- WHO | World Health Statistics 2016: Monitoring Health for the SDGs. Available online: http://www.who.int/gho/publications/world_health_statistics/2016/en/ (accessed on 15 August 2020).
- Akono, M.N.; Simo, L.P.; Agbor, V.N.; Njoyo, S.L.; Mbanya, D. The Spectrum of Heart Disease among Adults at the Bamenda Regional Hospital, North West Cameroon: A Semi Urban Setting. BMC Res. Notes 2019, 12, 761. [Google Scholar] [CrossRef]
- Nkoke, C.; Makoge, C.; Dzudie, A.; Mfeukeu, L.K.; Luchuo, E.B.; Menanga, A.; Kingue, S. A Predominance of Hypertensive Heart Disease among Patients with Cardiac Disease in Buea, a Semi-Urban Setting, South West Region of Cameroon. BMC Res. Notes 2017, 10, 684. [Google Scholar] [CrossRef]
- Nkoke, C.; Jingi, A.M.; Makoge, C.; Teuwafeu, D.; Nkouonlack, C.; Dzudie, A. Epidemiology of Cardiovascular Diseases Related Admissions in a Referral Hospital in the South West Region of Cameroon: A Cross-Sectional Study in Sub-Saharan Africa. PLOS ONE 2019, 14, e0226644. [Google Scholar] [CrossRef]
- Global Action Plan for the Prevention and Control of NCDs 2013-2020. Available online: https://www.who.int/publications-detail-redirect/9789241506236 (accessed on 8 March 2022).
- Owen, L.; Pennington, B.; Fischer, A.; Jeong, K. The Cost-Effectiveness of Public Health Interventions Examined by NICE from 2011 to 2016. J. Public Health 2018, 40, 557–566. [Google Scholar] [CrossRef]
- Supervia, M.; Turk-Adawi, K.; Lopez-Jimenez, F.; Pesah, E.; Ding, R.; Britto, R.R.; Bjarnason-Wehrens, B.; Derman, W.; Abreu, A.; Babu, A.S.; et al. Nature of Cardiac Rehabilitation Around the Globe. EClinicalMedicine 2019, 13, 46–56. [Google Scholar] [CrossRef]
- Meissner, H.; Creswell, J.; Klassen, A.C.; Plano, V.; Smith, K.C. Best Practices for Mixed Methods Research in the Health Sciences. 61.
- Dean, E.; Greig, A.; Murphy, S.; Roots, R.; Nembhard, N.; Rankin, A.; Bainbridge, L.; Anthony, J.; Hoens, A.M.; Garland, S.J. Raising the Priority of Lifestyle-Related Noncommunicable Diseases in Physical Therapy Curricula. Phys. Ther. 2016, 96, 940–948. [Google Scholar] [CrossRef]
- Dean, E.; Skinner, M.; Myezwa, H.; Mkumbuzi, V.; Mostert, K.; Parra, D.C.; Shirley, D.; Söderlund, A.; de Andrade, A.D.; Abaraogu, U.O.; et al. Health Competency Standards in Physical Therapist Practice. Phys. Ther. 2019, 99, 1242–1254. [Google Scholar] [CrossRef]
- McLean, S.; Charlesworth, L.; May, S.; Pollard, N. Healthcare Students’ Perceptions about Their Role, Confidence and Competence to Deliver Brief Public Health Interventions and Advice. BMC Med. Educ. 2018, 18, 114. [Google Scholar] [CrossRef]
- Rawlinson, G. Health Promotion in Physiotherapy Services Using NHS Health and Diabetes Checks. Br. J. Healthc. Manag. 2019, 25, 22–31. [Google Scholar] [CrossRef]
- Bombard, Y.; Baker, G.R.; Orlando, E.; Fancott, C.; Bhatia, P.; Casalino, S.; Onate, K.; Denis, J.-L.; Pomey, M.-P. Engaging Patients to Improve Quality of Care: A Systematic Review. Implement. Sci. 2018, 13, 98. [Google Scholar] [CrossRef]
- Hargraves, I.; LeBlanc, A.; Shah, N.D.; Montori, V.M. Shared Decision Making: The Need For Patient-Clinician Conversation, Not Just Information. Health Aff. (Millwood) 2016, 35, 627–629. [Google Scholar] [CrossRef]
- Puhl, R.; Peterson, J.L.; Luedicke, J. Motivating or Stigmatizing? Public Perceptions of Weight-Related Language Used by Health Providers. Int. J. Obes. 2013, 37, 612–619. [Google Scholar] [CrossRef]
- Allison, K.; Delany, C.; Setchell, J.; Egerton, T.; Holden, M.; Quicke, J.; Bennell, K. A Qualitative Study Exploring the Views of Individuals with Knee Osteoarthritis on the Role of Physiotherapists in Weight Management: A Complex Issue Requiring a Sophisticated Skill Set. Musculoskeletal Care 2019, 17, 206–214. [Google Scholar] [CrossRef]
- Berry, L.L.; Parish, J.T.; Janakiraman, R.; Ogburn-Russell, L.; Couchman, G.R.; Rayburn, W.L.; Grisel, J. Patients’ Commitment to Their Primary Physician and Why It Matters. Ann. Fam. Med. 2008, 6, 6–13. [Google Scholar] [CrossRef]
- Heine, M.; Fell, B.L.; Robinson, A.; Abbas, M.; Derman, W.; Hanekom, S. Patient-Centred Rehabilitation for Non-Communicable Disease in a Low-Resource Setting: Study Protocol for a Feasibility and Proof-of-Concept Randomised Clinical Trial. BMJ Open 2019, 9, e025732. [Google Scholar] [CrossRef]
- University of Arkansas; Venkatesh, V.; Brown, S.; University of Arizona; Sullivan, Y.; State University of New York, Binghamton. Guidelines for Conducting Mixed-Methods Research: An Extension and Illustration. J. Assoc. Inf. Syst. 2016, 17, 435–494. [Google Scholar] [CrossRef]
- Cameroon Society of Physiotherapy. Available online: https://world.physio/membership/cameroon (accessed on 20 June 2022).
- Physiotherapy Practice Start up, Cameroon. Available online: https://www.indiegogo.com/projects/1307213 (accessed on 8 July 2022).
- Sample Size Calculator. Available online: https://www.calculator.net/sample-size-calculator.html?type=1&cl=95&ci=5&pp=50&ps=400&x=44&y=23 (accessed on 15 August 2023).
- Gogovor, A.; Visca, R.; Ware, M.A.; Valois, M.-F.; Bartlett, G.; Hunt, M.; Ahmed, S. Determinants Of Patient Experience With Low Back Pain Interdisciplinary Care: A Pre-Post Interventional Study. J. Pain Res. 2019, Volume 12, 3203–3213. [Google Scholar] [CrossRef]
- Kariburyo, M.F.; Xie, L.; Teeple, A.; Tan, H.; Ingham, M. Predicting Pre-Emptive Discussions of Biologic Treatment: Results from an Openness and Preference Survey of Inflammatory Bowel Disease Patients and Their Prescribers. Adv. Ther. 2017, 34, 1398–1410. [Google Scholar] [CrossRef]
- Knisely, B.M.; Vaughn-Cooke, M. A Comprehensive Survey of Preference for Personal Health Record Features in Patients with Diabetes. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2020, 9, 171–175. [Google Scholar] [CrossRef]
- Rutakumwa, R.; Mugisha, J.O.; Bernays, S.; Kabunga, E.; Tumwekwase, G.; Mbonye, M.; Seeley, J. Conducting In-Depth Interviews with and without Voice Recorders: A Comparative Analysis. Qual. Res. 2020, 20, 565–581. [Google Scholar] [CrossRef]
- Ngeh, E.N.; Lowe, A.; Garcia, C.; McLean, S. Physiotherapy-Led Health Promotion Strategies for People with or at Risk of Cardiovascular Diseases: A Scoping Review. Int. J. Environ. Res. Public. Health 2023, 20, 7073. [Google Scholar] [CrossRef]
- DiCicco-Bloom, B.; Crabtree, B.F. The Qualitative Research Interview. Med. Educ. 2006, 40, 314–321. [Google Scholar] [CrossRef]
- McLellan, E.; MacQueen, K.M.; Neidig, J.L. Beyond the Qualitative Interview: Data Preparation and Transcription. Field Methods 2003, 15, 63–84. [Google Scholar] [CrossRef]
- Smith, J.; Flowers, P.; Larkin, M. Interpretative Phenomenological Analysis: Theory, Method and Research; 2009; Vol. 6, ISBN 978-1-4129-0834-4. [Google Scholar]
- Sadler, E.; Wolfe, C.D.A.; Jones, F.; McKevitt, C. Exploring Stroke Survivors’ and Physiotherapists’ Views of Self-Management after Stroke: A Qualitative Study in the UK. BMJ Open 2017, 7, e011631. [Google Scholar] [CrossRef]
- Bernard, H. Social Research Methods : Qualitative and Quantitative Approaches, 2nd ed.; Sage: Thousand Oaks CA, 2013; ISBN 978-1-4129-7854-5. [Google Scholar]
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample Size in Qualitative Interview Studies: Guided by Information Power. Qual. Health Res. 2016, 26, 1753–1760. [Google Scholar] [CrossRef]
- Guest, G.; Namey, E.; Chen, M. A Simple Method to Assess and Report Thematic Saturation in Qualitative Research. PLOS ONE 2020, 15, e0232076. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Reflecting on Reflexive Thematic Analysis. Qual. Res. Sport Exerc. Health 2019, 11, 589–597. [Google Scholar] [CrossRef]
- Best Qualitative Data Analysis Software for Researchers | NVivo. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed on 24 April 2022).
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for Reporting Qualitative Research: A Synthesis of Recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Olmos-Vega, F.M.; Stalmeijer, R.E.; Varpio, L.; Kahlke, R. A Practical Guide to Reflexivity in Qualitative Research: AMEE Guide No. 149. Med. Teach. 2023, 45, 241–251. [Google Scholar] [CrossRef]
- Carter, N.; Bryant-Lukosius, D.; DiCenso, A.; Blythe, J.; Neville, A.J. The Use of Triangulation in Qualitative Research. Oncol. Nurs. Forum 2014, 41, 545–547. [Google Scholar] [CrossRef]
- Sarfo, F.; Acheampong, J.; Appiah, L.; Oparebea, E.; Akpalu, A.; Bedu-Addo, G. The Profile of Risk Factors and In-Patient Outcomes of Stroke in Kumasi, Ghana. Ghana Med. J. 2014, 48, 127. [Google Scholar] [CrossRef]
- Mastwyk, S.; Taylor, N.F.; Lowe, A.; Dalton, C.; Peiris, C.L. Metabolic Syndrome Is Prevalent and Undiagnosed in Clients Attending Private Practice Physiotherapy: A Cross-Sectional Study. Physiotherapy 2024, 124, 116–125. [Google Scholar] [CrossRef]
- Dean, E.; Moffat, M.; Skinner, M.; Dornelas de Andrade, A.; Myezwa, H.; Söderlund, A. Toward Core Inter-Professional Health Promotion Competencies to Address the Non-Communicable Diseases and Their Risk Factors through Knowledge Translation: Curriculum Content Assessment. BMC Public Health 2014, 14, 717. [Google Scholar] [CrossRef]
- Gona, J.; Newton, C.R.; Geere, J.-A.; Hartley, S. Users’ Experiences of Physiotherapy Treatment in a Semi-Urban Public Hospital in Kenya. Available online: https://www.rrh.org.au/journal/article/2210/ (accessed on 9 July 2024).
- Del Baño-Aledo, M.E.; Medina-Mirapeix, F.; Escolar-Reina, P.; Montilla-Herrador, J.; Collins, S.M. Relevant Patient Perceptions and Experiences for Evaluating Quality of Interaction with Physiotherapists during Outpatient Rehabilitation: A Qualitative Study. Physiotherapy 2014, 100, 73–79. [Google Scholar] [CrossRef]
- Severin, R.; Wang, E.; Wielechowski, A.; Phillips, S.A. Outpatient Physical Therapist Attitudes Toward and Behaviors in Cardiovascular Disease Screening: A National Survey. Phys. Ther. 2019, 99, 833–848. [Google Scholar] [CrossRef]
- Physicians and Physiotherapists in the EU: How Many? Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/w/ddn-20230818-1 (accessed on 14 August 2024).
- Kossi, O. Training, Care Delivery, and Research in Physiotherapy in Sub-Saharan French-Speaking Africa. South Afr. J. Physiother. 2023, 79. [Google Scholar] [CrossRef]
- Elley, C.R. Effectiveness of Counselling Patients on Physical Activity in General Practice: Cluster Randomised Controlled Trial. BMJ 2003, 326, 793–793. [Google Scholar] [CrossRef]
- Grandes, G. Effectiveness of Physical Activity Advice and Prescription by Physicians in Routine Primary CareA Cluster Randomized Trial. Arch. Intern. Med. 2009, 169, 694. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and Evaluating Complex Interventions: The New Medical Research Council Guidance. BMJ 2008, a1655. [Google Scholar] [CrossRef]
- Griffiths, C.; Foster, G.; Ramsay, J.; Eldridge, S.; Taylor, S. How Effective Are Expert Patient (Lay Led) Education Programmes for Chronic Disease? BMJ 2007, 334, 1254–1256. [Google Scholar] [CrossRef]
| Participants | Age/years | Gender | Profession | Academic Qualification | Risk Factor (S) and/or Cardiovascular Condition |
|---|---|---|---|---|---|
| P1 | 79 | M | Retired School Administrator | Postgraduate Degree | Hypertension, Diabetes, Stroke, High Cholesterol, CHD |
| P2 | 49 | F | Agricultural engineer | Postgraduate degree | Overweight |
| P3 | 64 | M | Community development Officer | Undergraduate Degree | Insomnia, hypertension and overweight |
| P4 | 68 | F | Retired Civil Servant | Undergraduate Degree | Stroke, Hypertension, Overweight, High Cholesterol |
| P5 | 37 | M | Unemployed | No formal Education | Stroke, hypertension |
| P6 | 56 | M | Business | High School | Hypertension, Overweight, Stroke and High Cholesterol |
| P7 | 39 | F | Translator | Postgraduate degree | Overweight |
| P8 | 65 | M | Business | High School | Overweight |
| P9 | 46 | F | Teacher | Postgraduate degrees | Overweight |
| P10 | 60 | F | Retired nurse | Undergraduate Degree | Hypertension, Diabetes, Overweight, High Cholesterol |
| P11 | 46 | M | Business | Diploma | Overweight |
| P12 | 63 | M | Retired physical education and sport teachers | Undergraduate Degree | Hypertension, Diabetes, Overweight |
| P13 | 60 | F | Retired civil servant | Undergraduate degrees | Overweight, Diabetes, hypertension, physical inactivity, Stroke |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




